Professional Documents
Culture Documents
Immun Record
Uploaded by
NonofYaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Immun Record
Uploaded by
NonofYaCopyright:
Available Formats
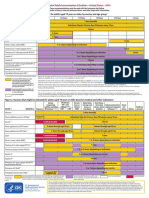
SAMPLE IMMUNIZATION RECORD
PART I
Name
Last Name
First Name
Address
Street
Date of Entry
/
M
Status
City
Date of Birth
Part-time
State
Social Security Number
Zip
/-/
/-/
M D Y
Full-time
Graduate
Undergraduate
Professional
PART II TO BE COMPLETED AND SIGNED BY YOUR HEALTH CARE PROVIDER.
All information must be in English.
A.
M.M.R. (Measles, Mumps, Rubella) (Two doses required.)
1.
Dose 1 given at age 12-15 months or later
#1
/
M
2.
B.
Dose 2 given at age 4-6 years or later, and at least one month after first dose .
#2
/
M
Y
TETANUS-DIPHTHERIA (Primary series with DTaP or DTP and booster with Td in the last ten years meets requirement. Refer to ACIP for details.)
1.
Primary series of four doses with DTaP or DTP:
#1
2.
/
#2
/
#3
/
#4
/
M Y
M Y
M Y
M Y
Tetanus-Diphtheria (Td) booster within the last ten years
/
M
C.
POLIO (Primary series in childhood meets requirement; three primary series schedules are acceptable. Refer to ACIP for details.)
1.
OPV alone (oral Sabin three doses): ...
#1
/
M
2.
IPV/OPV sequential:
IPV #1
3.
IPV alone (injected Salk four doses): ..
#2
Y
#1
#2
M
#2
Y
#3
Y
/
M
/
M
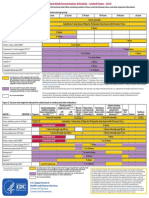
D.
#3
Y
/
M
/
M
#3
Y
#4
Y
/
M
Varicella antibody
/
M
3.
/
M
#4
Y
Y
/
Reactive
Non-reactive
Immunization
a. Dose # 1 # 1
/
M Y
b. Dose # 2, given at least one month after first dose, if age 13 years or older # 1
/
M Y
HEPATITIS B (Three doses of vaccine or two doses of adult vaccine in adolescents 11-15 years of age, or a positive Hepatitis B surface antibody meets
the requirement.)
1.
Immunization (Hepatitis B)
a. Dose # 1
/
b. Dose # 2
/
c. Dose # 3
/
M Y
M Y
M Y
2.
Immunization (Combined Hepatitis A and B Vaccine)
a. Dose # 1
3.
F.
VARICELLA (Either a history of chicken pox, a positive Varicella antibody, or two doses of vaccine given at least one month apart if immunized at the
age of 13 or older meets the requirement.)
1.
History of Disease
Yes
No
2.
E.
/
M
/
b. Dose # 2
/
M Y
M Y
Hepatitis B surface antibody
Date
/
M
Y
c. Dose # 3
Result:
/
M Y
Reactive
HEPATITIS A
1.
Immunization (Hepatitis A)
a. Dose # 1
/
b. Dose # 2
/
M Y
M Y
2.
Immunization (Combined Hepatitis A and B Vaccine)
a. Dose # 1
/
M
b. Dose # 2
Y
/
M
c. Dose # 3
Y
/
M
Non-reactive
G.
PNEUMOCOCCAL POLYSACCHARIDE VACCINE (One dose for members of high-risk groups. Refer to ACIP for details.)
Date
/
M
H.
INFLUENZA (Annual immunization recommended for members of high-risk groups and to avoid disruption to academic activities.)
Date
M
I.
/
Y
M Y
/
M
/
Y
M Y
M Y
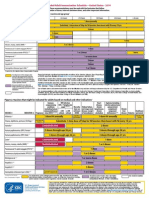
MENINGOCOCCAL VACCINE (One dose recommended for college freshmen living in dormitories/residence halls, persons with terminal
complement deficiencies or asplenia, laboratory personnel with exposure to aerosolized meningococci, and travelers to hyperendemic or endemic areas of
the world. Non-freshmen college students under 25 years of age may choose to be vaccinated to reduce their risk of meningococcal disease.)
Date ____/____
M Y
Meningococcal conjugate (preferred; data for revaccination pending):
Meningococcal polysaccharide (acceptable alternative if conjugate not
available; revaccinate every 3-5 years if increased risk continues):
J.
/
M Y
Date ____/____
M Y
____/____
M
TUBERCULOSIS SCREENING
1.
Does the student have signs or symptoms of active tuberculosis disease?
Yes
No
If No, proceed to 2. If Yes, proceed with additional evaluation to exclude active tuberculosis disease including tuberculin skin testing, chest x-ray
and sputum evaluation as indicated.
2.
Is the student a member of a high-risk group or is the student entering the health professions?
Yes
No
If No, stop. If Yes, place tuberculin skin test (Mantoux only: Inject 0.1 ml of purified protein derivative [PPD] tuberculin containing 5 tuberculin
units [TU] intradermally into the volar [inner] surface of the forearm.) A history of BCG vaccination should not preclude testing of a member of a
high-risk group.
3.
Tuberculin Skin Test:
Date Given:
/
M
/
D
Date Read:
Y
/
D
/
Y
Result:
(Record actual mm of induration, transverse diameter; if no induration, write 0)
Interpretation (based on mm of induration as well as risk factors): positive
negative
4.
Chest x-ray (required if tuberculin skin test is positive) result: normal
Date of chest x-ray:
abnormal
/
/
M D Y
HEALTH CARE PROVIDER
Name
Address
Signature
Phone (
PART III ONLY COMPLETED AND SIGNED BY STUDENT (OR PARENT/GUARDIAN FOR STUDENT UNDER THE AGE OF 18) IF THE
STUDENT DOES NOT HAVE VALID VACCINATION FOR MENINGOCOCCAL DISEASE CHECK BOX
I have (for students under the age of 18: My child has) read, or have had explained to me, the information regarding meningococcal meningitis disease.
I understand the risks of not receiving the vaccine. I have decided that I (my child) will not obtain immunization against meningococcal meningitis disease.
Signed
Date
Student (Parent / Guardian if student is a minor)
1 The American College Health Association has published guidelines on tuberculosis screening of college and university students. These guidelines are based
on recommendations from the Centers for Disease Control and the American Thoracic Society. For more information, visit www.acha.org or refer to the CDCs
Core Curriculum on Tuberculosis available at state health departments or at the following website: www.cdc.gov/nchstp/pubs/corecurr/.
2 Categories of high-risk students include those students who have arrived within the past 5 years from countries where TB is endemic. It is easier to identify
countries of low rather than high TB prevalence. Therefore, students should undergo TB screening if they have arrived form countries EXCEPT those on the
following list: Canada, Jamaica, Saint Kitts and Nevis, Saint Lucia, USA, Virgin Islands (USA), Belgium, Denmark, Finland, France, Germany, Greece,
Iceland, Ireland, Italy, Liechtenstein, Luxemborg, Malta, Monaco, Netherlands, Norway, San Marino, Sweden, Switzerland, United Kingdom, American
Samoa, Australia, or New Zealand. Other categories of high-risk students include those with HIV infection, who inject drugs, who have resided in, volunteered
in, or worked in high-risk congregate settings such as prisons, nursing homes, hospitals, residential facilities for patients with AIDS, or homeless shelters; and
those who have clinical conditions such as diabetes, chronic renal failure, leukemias or lymphomas, low body weight, gastrectomy and jejunoileal by-pass,
chronic malabsorption syndromes, prolonged corticosteroid therapy (e.g., prednisone 15 mg/d for 1 month) or other immunosuppressive disorders.
Adapted from ACHAs Vaccine-Preventable Disease Task Force
You might also like
- IMMUNIZATION RECORD CERTIFICATEDocument2 pagesIMMUNIZATION RECORD CERTIFICATEanusdasari100% (10)
- IMMUNIZATION RECORD CERTIFICATEDocument2 pagesIMMUNIZATION RECORD CERTIFICATEanusdasari100% (10)
- Medical Record FormDocument4 pagesMedical Record FormДария КоваленкоNo ratings yet
- John Jay Immunization FormDocument3 pagesJohn Jay Immunization FormIsam BoukattayaNo ratings yet
- Communicablediseases 110227001506 Phpapp02 PDFDocument30 pagesCommunicablediseases 110227001506 Phpapp02 PDFCrystal Ann Monsale TadiamonNo ratings yet
- Infectious Disease Medical Behavioral Screens AmendedDocument6 pagesInfectious Disease Medical Behavioral Screens AmendedHengkyNo ratings yet
- Immunization Record: Form Is Due at OrientationDocument3 pagesImmunization Record: Form Is Due at OrientationCasey JonesNo ratings yet
- Immunization Report PDFDocument2 pagesImmunization Report PDFJag UnathNo ratings yet
- Univ of Florida ImmunisationDocument2 pagesUniv of Florida ImmunisationPavan Kumar MangipudiNo ratings yet
- PSW6 - PPHFDocument16 pagesPSW6 - PPHFanishthNo ratings yet
- Immunization Letter NB FORM RevisedDocument6 pagesImmunization Letter NB FORM RevisedUddhavendra Pal SinghNo ratings yet
- An Important FormDocument3 pagesAn Important FormRachel ColeNo ratings yet
- Figure 1. Recommended Immunization Schedule For Adults Aged 19 Years or Older, by Vaccine and Age GroupDocument2 pagesFigure 1. Recommended Immunization Schedule For Adults Aged 19 Years or Older, by Vaccine and Age GroupmsarasNo ratings yet
- Adult Immunization Schedule and RecommendationsDocument3 pagesAdult Immunization Schedule and RecommendationsdrmanojvimalNo ratings yet
- Immunizations Page Effective Spring 2010 Guidelines For Completing Immunization InformationDocument7 pagesImmunizations Page Effective Spring 2010 Guidelines For Completing Immunization InformationShubham TrivediNo ratings yet
- Adult Immunization ScheduleDocument3 pagesAdult Immunization ScheduleBryan Mae H. DegorioNo ratings yet
- Pre Entrance Immunization FormDocument3 pagesPre Entrance Immunization FormsmithwesNo ratings yet
- 2024 VPD FormFINAL 16012024Document5 pages2024 VPD FormFINAL 16012024dkid9876No ratings yet
- Immunization Submission FormDocument3 pagesImmunization Submission Formdimpiu11No ratings yet
- Immreq15 16Document2 pagesImmreq15 16api-234991765No ratings yet
- Pre-Registration Nursing Information For Prospective StudentsDocument4 pagesPre-Registration Nursing Information For Prospective StudentsbthangarajNo ratings yet
- ScheduleDocument2 pagesScheduleapi-286634335No ratings yet
- Epi and Cold ChainDocument3 pagesEpi and Cold ChainShadrackNo ratings yet
- Adult Schedule 11x17Document2 pagesAdult Schedule 11x17lcmurilloNo ratings yet
- Adult Pocafeket SizeDocument2 pagesAdult Pocafeket SizedadfNo ratings yet
- Health History and Immunization Form: University of Valley Forge - Health CenterDocument4 pagesHealth History and Immunization Form: University of Valley Forge - Health CenterBernard AmetepeNo ratings yet
- Recommended Immunization - Canadian Immunization Guide - Seventh Edition - 2006Document2 pagesRecommended Immunization - Canadian Immunization Guide - Seventh Edition - 2006Maja MudriNo ratings yet
- 01CIM 01 - Clinical Pathway Managing TB CasesDocument10 pages01CIM 01 - Clinical Pathway Managing TB Casesyin sNo ratings yet
- Immunization Programs For Infants, Children, Adolescents, and Adults: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument24 pagesImmunization Programs For Infants, Children, Adolescents, and Adults: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaEugene YeboahNo ratings yet
- Immunization Requirement Form - UpdateDocument2 pagesImmunization Requirement Form - UpdateManojkumar ANo ratings yet
- Good Health in the Tropics: Advice to Travellers and SettlersFrom EverandGood Health in the Tropics: Advice to Travellers and SettlersNo ratings yet
- "Expanded Program On Immunization": Angeles University FoundationDocument12 pages"Expanded Program On Immunization": Angeles University FoundationJaillah Reigne CuraNo ratings yet
- Adult Combined ScheduleDocument5 pagesAdult Combined SchedulelcmurilloNo ratings yet
- Immunization History FormDocument1 pageImmunization History FormMohammad ShoiabNo ratings yet
- Standing Orders For Administering Tdap/Td To Adults: (Name of Practice or Clinic)Document1 pageStanding Orders For Administering Tdap/Td To Adults: (Name of Practice or Clinic)selvie87No ratings yet
- TUBERCULOSIS TB RISK ASSESSMENT FORM Created March 12 2018 1Document2 pagesTUBERCULOSIS TB RISK ASSESSMENT FORM Created March 12 2018 1Jimmy MountNo ratings yet
- FIU Immunization Documentation FormDocument2 pagesFIU Immunization Documentation FormMO MONo ratings yet
- Health Immunization Clearance Form: Section A: ImmunizationsDocument3 pagesHealth Immunization Clearance Form: Section A: ImmunizationsFaith SetikNo ratings yet
- Recommended Immunizations FS enDocument2 pagesRecommended Immunizations FS enirfanmajeed1987No ratings yet
- Reading VaccineImmunizationDocument13 pagesReading VaccineImmunizationelztly4694No ratings yet
- CUB - Immunisation FormDocument2 pagesCUB - Immunisation FormArcane BeingNo ratings yet
- Health Information FormDocument13 pagesHealth Information FormArtero-Cavallaro PabloNo ratings yet
- ImmunizationDocument40 pagesImmunizationHilyaJae-heeNo ratings yet
- Preventing Illness and Living With Ill HealthDocument11 pagesPreventing Illness and Living With Ill HealthMonique MavronicolasNo ratings yet
- Running Head: Tdap Education and The Proper Administration 1Document4 pagesRunning Head: Tdap Education and The Proper Administration 1api-402463634No ratings yet
- St. Paul University PhilippinesDocument7 pagesSt. Paul University PhilippinesAngelica Mae Kidang RositeNo ratings yet
- Adult ScheduleDocument3 pagesAdult SchedulelcmurilloNo ratings yet
- GOVT.MODEL AYURVED COLLEGE STUDENT'S COMPILATION ON TYPHOID FEVER EPIDEMIOLOGY, SYMPTOMS AND CONTROLDocument16 pagesGOVT.MODEL AYURVED COLLEGE STUDENT'S COMPILATION ON TYPHOID FEVER EPIDEMIOLOGY, SYMPTOMS AND CONTROLArc MuNo ratings yet
- Population Growth Drives Disease SpreadDocument44 pagesPopulation Growth Drives Disease Spreadganesh8sundaresanNo ratings yet
- ImmunizationCertificate PDFDocument2 pagesImmunizationCertificate PDFAnonymous kq5iEDxxhrNo ratings yet
- Form PD1 Medical Examination ReportDocument9 pagesForm PD1 Medical Examination ReportSyazwi BaharuddinNo ratings yet
- COVID 19 Consent FormDocument2 pagesCOVID 19 Consent FormfvdssfdNo ratings yet
- Vietnamese Student Health Exam GuidelinesDocument6 pagesVietnamese Student Health Exam GuidelinesKita 09No ratings yet
- Rutgers Immunization FormDocument3 pagesRutgers Immunization Formruhayl khanNo ratings yet
- Form G Health Examination Report International StudentDocument6 pagesForm G Health Examination Report International StudentVictor OjukwuNo ratings yet
- Dalhousie Dentistry Immunization RequirementsDocument3 pagesDalhousie Dentistry Immunization Requirementsabhinav guptaNo ratings yet
- Immunization Requirement - Student Health Center - The University of UtahDocument2 pagesImmunization Requirement - Student Health Center - The University of Utahmithun916No ratings yet
- Your Name Institution/organization Meeting DateDocument42 pagesYour Name Institution/organization Meeting DateMochammad Fariz AmsalNo ratings yet
- Undertaking Declaration PD2022 - 030Document2 pagesUndertaking Declaration PD2022 - 030MejoNo ratings yet
- EPIDocument7 pagesEPIheng_gutierrezNo ratings yet
- A Statistical Inquiry Into the Nature and Treatment of EpilepsyFrom EverandA Statistical Inquiry Into the Nature and Treatment of EpilepsyNo ratings yet
- Immunization RecordDocument2 pagesImmunization RecordNonofYaNo ratings yet
- Immunization RecordDocument1 pageImmunization RecordNonofYaNo ratings yet
- Immunization RecordDocument2 pagesImmunization RecordNonofYaNo ratings yet