Professional Documents
Culture Documents
24 Antioxidants and Multistage Carcinogenesis in Mouse Skin
Uploaded by
aribniminnakCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
24 Antioxidants and Multistage Carcinogenesis in Mouse Skin
Uploaded by
aribniminnakCopyright:
Available Formats
Free Radical Biology & Medicine, Vol. 7, pp.
377-408, 1989
Printed in the USA. All rights reserved.
0891-5849/89 $3.00+ .00
1989 PergamonPress plc
Review Article
ANTIOXIDANTS
AND MULTISTAGE CARCINOGENESIS IN MOUSE SKIN
JEAN-PIERRE PERCHELLET* a n d ELISABETH M . PERCHELLET
Anti-Cancer Drug laboratory, Division of Biology, Kansas State University, Ackert Hall, Manhattan, KS 66506, U.S.A.
(Received 21 April 1988; Revised and accepted 1 September 1988)
Abstract--The two-step initiation-promotion protocol for the induction of skin tumors in mice is a convenient
model to elucidate what molecular events are involved in the multistage process of carcinogenesis and how they
can be modulated. The current theories concerning the mechanisms of skin tumor initiation, stages 1 and 2 of
tumor promotion, and tumor progression are reviewed. Because chemical carcinogens and tumor promoters may,
directly or indirectly, generate reactive oxygen species (ROS) and because various antioxidants inhibit effectively
some of the biochemical and biological events linked to tumor initiation, promotion and/or progression, it is
conceivable that different sequences and levels of free radical-induced macromolecule damage may contribute to
the evolution of the epidermal target cells from the preneoplastic stage to the malignant stage.
Keywords--Carcinogenesis, Free radical, Antioxidants, Skin tumors, Initiation, Promotion, Progression
daughter cells. 1-4 Genetic and somatic mutations, as
well as epigenetic alterations, may result in neoplastic
transformation.
The presence of irreversible DNA damage or altered
proto-oncogenes increases the probability that the initiated cell might not respond to the regulatory signals
for normal growth and differentiation and, after neoplastic transformation and a postulated period of dormancy, might then proliferate into a benign or
malignant tumor. Because it is impossible to monitor
continually the level of DNA lesions/repair in individual stem cells, it appears difficult to predict if and
when such irreversible initiation and transformation of
a single precursor cell might occur and, therefore, to
determine at the cellular level when carcinogenesis
really begins.
The early diagnosis of cancer, which is crucial to
the efficacy of cancer management, is unfortunately
delayed by the extended period of time between the
initial interaction of physical, chemical or biologic carcinogens at the cellular level and the appearance of a
neoplasm. In most systems studied, there is no evidence of neoplastic growth through much of the latency
period. 3 Then, approximately 30 cell doublings are required for most neoplasms to grow exponentially from
a single transformed cell to about 109 tumor cells, the
estimated limit of clinical or radiologic detection in
human, s-7 After only 10 further doublings in volume,
INTRODUCTION
According to the multihit theory for the monoclonal
origin of cancer, neoplasia arises when the stem cells
of the human tissues that are the random targets of an
undetermined number and sequence of inherited, acquired and/or spontaneous cell-damaging events accumulate nonlethal, unrepaired, irreversible, defects
that can be transmitted to successive generations of
*Author to whom correspondence should be addressed.
Jean-Pierre (PhD, 1974) and Elisabeth (PhD, 1973) Perchellet
were trained in Endocrinology under Dr. A. Jost (Laboratory of
Comparative Physiology, University Paris VI). After serving in the
French Army, Jean-Pierre did postdoctoral work in Biochemistry
with Dr. R. K. Sharma (University of Tennessee Center for the
Health Sciences, Memphis) and in Oncology with Dr. R. K. Boutwell (McArdle Laboratory for Cancer Research, University of Wisconsin, Madison). He is now Associate Professor at Kansas State
University where he directs the Anti-Cancer Drug Laboratory and
teaches graduate courses in Human Oncology and Cancer Therapy.
His research concerns the biochemistry of mouse skin carcinogenesis
and focuses on the molecular mechanisms by which oxidants, antioxidants, and anthracycline antibiotics modulate the multi-stage
process of tumor promotion. His wife and collaborator, Elisabeth,
held full- and part-time Research Associate positions in Gastroenterology with Dr. J.-J. Bernier (INSERM-U54, St. Lazare Hospital,
Paris), in Biochemistry with Dr. R. K. Sharma (University of Tennessee, Memphis) and in Gastroenterology with Dr. W. A. Olsen
(Veteran Administration Hospital, University of Wisconsin, Madison) while raising 3 children. Both authors enjoy hiking in National
Parks, playing bridge, and visiting art, history, and science museums.
377
378
J.-P. PERCHELLETand E. M. PERCHELLET
the tumor burden may become lethal to the host. As
illustrated by the current cancer survival statistics, 7
eradicating by combination therapy 100% of the cells
resulting from this long preclinical growth of human
tumors is a very difficult task. The incidence of cancer
at any age seems directly proportional to the number
of initiated stem cells accumulated at that a g e ? Since
it is impossible to pinpoint the time of tumor cell initiation, there is no way to know how long the progenitor cell remained dormant in the tissue before it
started proliferating. Furthermore, it is difficult to
extrapolate from doubling times in the clinic to preclinical circumstances in order to estimate the time at
which the tumor started growing in the patient before
it was detected.
THE NEED FOR EXPERIMENTAL MODELS
OF CARCINOGENESIS
A skin papilloma (Pa) becomes visible when the
clonal expansion of the initiated epidermal cell reaches
a size of 105-106 cells. In classic animal experiments
where the complete carcinogenesis or the initiationpromotion treatments are applied directly to mouse epidermis, the first skin tumors appear after 5-7 (benign)
and 16-18 (malignant) weeks, s These time intervals
represent about 5 and 12% of a mouse's life. If we can
extrapolate this in terms of a human life lasting 75
years, these lag periods become 4 and 9 years. Because
the stem cells of the human tissues are unlikely to be
exposed to such drastic carcinogenic treatments, and
for other reasons, the whole process of carcinogenesis
in humans may take much longer, it should be noted
that a small percentage of the mice whose skins are
exposed to these potent carcinogenic treatments never
develop any visible neoplasms. It is postulated that
many more skin cells are initiated than finally transformed into neoplastic cells and that populations of
initiated and dormant tumor cells may exist in organisms for a lifetime without ever expressing their potential for neoplastic transformation and exponential
growth? The dormancy of malignant neoplastic cells
has clearly been demonstrated, indicating that further
stimuli are required to trigger their proliferation. 9
Epidemiological and tumor cell kinetics studies sugest that populations of initiated or dormant tumor cells
may exist in the human tissues for several decades
before they are, respectively, transformed or triggered
into a hyperplastic behavior leading to the diagnosis
of a neoplasm? However, most human tumors have a
mean cell cycle time of about 2 days but a mean volume
doubling time of about 50 days because of the small
proportion of proliferating tumor cells (growth frac-
tion) and the high rate of tumor cell death. 3'5'6"~'~LThe
growth of most neoplasms is regarded as an exponential
function limited by an exponential retardation. Since
mass and doubling time are increasing concomitantly,
the rate of tumor growth decellerates because the
growth fraction decreases, the cell loss factor increases
and sometimes the duration of the cell cycle lengthens.
These tumor growth kinetics suggest that it should take
only a few months or years for the selected transformed
cell to proliferate into a tumor reaching the critical
mass of clinical detection. The process of tumorigenesis in humans, therefore, may be characterized by a
relatively long period of latency, which is postulated
to comprise an undetermined period of dormancy preceding the preclinical portion of the theoretic Gompertzian growth curve (Fig. 1).
The hypothetical model in Figure 1 suggests that
the cells that are sequentially subjected to genetic mutation and phenotypic transformation by years of exposure to carcinogenic hazards, including tumor
initiators and promoters, may remain dormant, that is,
maintain their normal rate of self-renewal, for a part
of the latency period of the carcinogenic process until
one of them finally acquires a proliferative advantage
over its neighbor stem cells. In addition to the unknown
stimuli triggering proliferation, the dormant neoplastic
cells may have to overcome immunologic and other
defense mechanisms of the host and induce sufficient
vascularization to support their exponential expansion.
Thus, after going through occult carcinogenic changes
at the molecular level for several months or years, a
transformed human cell may all of a sudden speed up
its rate of renewal with the result that, within a few
more months or years, both patient and physician become finally aware of the presence of a neoplasm. By
using experimental tumor models, the long-term objective of fundamental cancer research is to elucidate
the molecular events specifically involved in the preclinical portion of the neoplastic process (Fig. 1). Earlier detection and modulation of such events should
provide valuable information to design novel cancer
therapies applicable in clinical oncology.
THE MOUSE SKIN SYSTEM FOR
MULTISTAGE CARCINOGENESIS
Experimental carcinogenesis in mouse skin was pioneered by the works of Mottram 12and Berenblum and
Shubik,~3 and studied extensively by Boutwell.~4 The
initiating and promoting elements in skin tumor production have been characterized. 1415 The demonstration of the multistep nature of chemical carcinogenesis
in mouse skin was greatly facilitated by the synthesis
Antioxidants and skin carcinogenesis
o~1014 -tl . . . . .
II . . . . . . . . . . . . .
Maximum Moss Compatible with Ufe
o~
o 1012
. I . . 7. .
Limit of Clinical Detection
~ IOi
Io 8
II . . . . .
379
10 6
},
.~_ 104
Tumor
Initiation
Tumor Promotion
I
I
.
c ~
~ ' ~
Stem Cell
Stem Cell
Initiation
--27
Neoplastic Cell
Transformation Prolif,ercdion /
l
-II ' '
_
"
. Ii .
,
,.
,~ '
,.
1
"6
I
Postulated Period of
Dormancy
/ i
/~,
/I
/
i
'l
i ....
I ,~'~x~L"Y
~
i u~.t=
u,
I
,I ~
',_T_,',e_
, . . . . . . . . . . ,
>
,,P od of t_ rfi
of
'a~
Prior to, Clinical
,
Deteclim
),
Growth
Period of Leten~;y
I<
Pt~iod of ~ 1
)'
Gl~th
Fig. 1 Hypothetical growth of a human neoplasm.
of pure polycyclic aromatic hydrocarbon (PAH)
carcinogens ~6such as 7,12-dimethylbenz[a]anthracene
(DMBA) and the isolation of the potent tumor-promoting agent from croton oil, T M 12-0-tetradecanoylphorbol-13-acetate (TPA). Moreover, the breeding of
promotion-sensitive SENCAR mice has provided an
excellent model system to pursue studies on the mechanisms of multistage skin carcinogenesis. '4,19 The ex-
perimental induction of tumors in mouse skin is
believed to comprise a sequence of initiation, promotion (conversion + propagation), and progression
(Table 1). The various treatments "painted" to the
shaved backs of the mice during the initiation-promotion protocols 14'15,20and the complete carcinogenesis
processesS.2~.22 commonly used for the induction of skin
Pa and carcinomas (Ca) are depicted in Table 1.
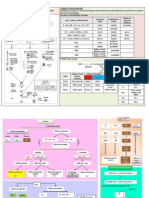
Table 1. Protocols for Multistage Carcinogenesis in Mouse Skin
Description of Treatments (Duration)*
Number
Initiation
1. DMBA
(0.1/~mol; ix)
Initiation
2. DMBA
(0.1 ~tmol; ix)
Initiation
3. DMBA
(0.1/lmol; Ix)
4. DMBA
(0.1 pmol; ix)
5. DMBA
Agents Administered (Dose/Applications; Total Number of Applications)f
Complete Promotion (40 wk)
TPA
(8.5 nmol; 80x)
Two-Stage Promotion (40 wk)
Stage 1 (2 wk)
Stage 2 (38 wk)
TPA
(8.5 nmol; 4x)
Promotion (20 wk)
TPA
(8.5 nmol; 40x)
TPA
(8.5 nmol; 40x)
TPA
(0.1/lmol; ix)
(8.5 nmol; 40x)
Complete Carcinogenesis (40 wk)
MEZ
(8.5 nmol; 76x)
Progression (20 wk)
BPx
(20 mg, 40x)
; then TPA
ENU
(8.5 nmol; 36x)
(10 ,umol; 4x)
; then TPA
MNNG
(8.5 nmol; 36x)
(1/~mol; 4x)
6. DMBA
(3.6/tmol; ix)
7. DMBA
(0.1/tmol; 80x)
*All treatments are applied topically in 0.2 ml of acetone to the same shaved dorsal area of the skin.
tDosages vary with strain. Data are for Charles River CD-1 mice; the frequency of application for repeated treatments is 2x/wk.
380
J.-P. PERCHELLETand E. M. PERCIqELLET
Tumor initiation
A single subcarcinogenic dose of DMBA [Table 1
(Protocol 1)] produces no tumors during the life-span
of the animals but, after metabolic activation, the electrophilic ultimate carcinogen interacts covalently with,
and damages, critical macromolecules, presumably epidermal DNA, 23 to initiate skin carcinogenesis. When
the DNA template is replicated before it is repaired,
the initiating genetic damage becomes irreversible and
,34
heritable.New evidence suggests that the c - r a s m
proto-oncogene is the target of the initiating mutation
in mouse skin carcinogenesis: 25 .~2 1) the activated cr a s Ha oncogene has been isolated from skin Pa; 2) the
introduction of mutated r a s m oncogene into epidermal
cells can substitute for DMBA initiation in two-stage
mouse skin carcinogenesis; and 3) the keratinocytes
derived from DMBA-initiated skins and/or resistant to
Ca2+-induced terminal differentiation contain an activated c - r a s m oncogene and form squamous Pa in skin
grafts on athymic nude mice. A single base substitution
activates the c - r a s m proto-oncogene. The frequency of
this mutation is dependent on the initiating agent. Over
90% of mouse skin tumors initiated with DMBA have
a point mutation (specific A---~T transversion) at the
2nd nucleotide in codon 61 of c - r a s m . Other initiators
may induce a point mutation (specific G--~A transition)
at the 2nd nucleotide in codon 12 of c - r a s m .
Although epigenetic theories are also plausible,; tumor initiation is generally regarded as a permanent
alteration of the cell genotype with no neoplastic phenotype. ~533 Epidermal cells initiated with the v - r a s H~
oncogene remain dormant within the skin in the absence of tumor promotion and require TPA treatments
to form Pa, suggesting that DMBA-induced point mutation and activation of the c - r a s H~ proto-oncogene represents an initiating event, which is insufficient for
skin tumorigenesis unless amplification of the mutated
oncogene is triggered by tumor promoters. The persistence of latent initiated cells with the potential to
give rise to future neoplasms has been demonstrated. 14.34.35The mechanism by which the c - r a s H~ oncogene induces transformation is unknown. Initiated
cells are uniformly resistant to Ca2+-induced terminal
differentiation. The correlation between tumor initiation and resistance of epidermal cells to signals for
terminal differentiation suggests, therefore, that the
initiating event in skin carcinogenesis causes a genetic
alteration in the program of terminal differentiation 36 3s
Complete
tumor promotion
Repetitive applications of the most potent phorbol
ester tumor promoter TPA [Table 1 (Protocol 1)] are
required to trigger molecular events leading the immediate progeny of the DMBA-initiated epidermal
cells to the formation of growing skin tumors and
achieve complete tumor promotion ~5,~3 It is theorized
that TPA stimulates the expression of the abnormal
genetic information within the initiated cells which,
because of their altered program of differentiation, acquire a neoplastic phenotype and a proliferative advantage over their normal neighbors. 3'~ Promoting
agents by definition are neither mutagenic nor carcinogenic and, therefore, incapable of initiation or complete carcinogenesis by themselves. Moreover, they
cannot promote tumor formation in the absence of
preexisting initiated cells, as indicated by the experiments in which the sequence initiation-promotion is
reversed. H The occasional neoplasms resulting from
lifetime treatment of mouse skin with large doses of
TPA alone are likely attributable to the promotion of
initiated or dormant tumor cells of spontaneous origin. ~4.33The experiments in which promotion precedes
initiation or the frequency of TPA application is decreased produce no tumors, suggesting that the promoting effects of individual TPA treatments are
transient and, to a certain degree, reversible. ~4 Although the events critical for the selective clonal expansion of initiated cells to form a neoplasm are poorly
understood, the evidence that the tumor promoters interact with membranes, stimulate and alter genetic
expression and eventually increase the rate of cell proliferation has been reviewed. 33~ 44 TPA has been
shown to produce a series of pleiotropic cellular effects
including the induction of protein kinase C (PKC) activity. 45'46 phospholipid synthesis 47 and prostaglandin
(PG) release, 4~ the synthesis and phosphorylation of
epidermal histones, ~ the increase in protease activity, 5 the production of ROS, 5t the overexpression of
tumor-specific, promotion sensitive, transforming or
cellular proto-oncogenes, 252'~ 32.52.53 the induction of
the polyamine biosynthetic pathway 54 followed by
sequential increases in RNA, protein, and DNA synthesis, 55 with concomitant alterations in cellular
morphology,56 mitotic rate, 44 and degrees of metabolic
~7
cooperationand terminal differentiation. 4 4 ,-5 8 A major
problem is to identify the critical responses which mediate specifically the early and late events required for
two-stage tumor promotion. H59.~'
Multistage
tumor promotion
One to four applications of TPA are sufficient to
trigger the 1st, partially irreversible, stage of promotion called " c o n v e r s i o n " [Table 1 (Protocol 2)]. Multiple applications of the ineffective promoter mezerein
(MEZ) are then required to achieve the 2nd stage of
Antioxidants and skin carcinogenesis
promotion called "propagation" and complete the promotion process. 6~ Neither treatment alone is sufficient
Overall, the tumor response elicited by the initiationtwo stage promotion protocol [Table 1 (Protocol 2)] is
significantly lesser than that observed when TPA is
used as a complete promoter [Table 1 (Protocol 1)].
The long-lasting effects of TPA that are essential
for stage 1 promotion persist for almost 2 months before declining whereas those of MEZ in stage 2 promotion are rapidly reversible and require a certain
frequency of application in order to induce tumors.
The sequential inductions of ornithine decarboxylase
(ODC) activity, macromolecule synthesis and epidermal cell proliferation are undoubtedly involved in the
2nd stage of tumor promotion. 59 For instance, following DMBA initiation and stage 1 promotion with TPA,
the 2nd stage of skin tumor promotion can be completed if only 4 applications of the potent ODC inducer
MEZ, which by themselves are ineffective in completing the two-stage promotion process, are followed
by repetitive treatments with ethyl phenylpropiolate
(EPP), a nonpromoting epidermal hyperplastic agent
unable to induce ODC activity. 59 Interestingly, only
those phorbol esters which induce the sequential transient expression of the proto-oncogenes c - l o s and cm y c and the ODC gene in mouse skin in vivo cause
rapid induction of epidermal hyperplasia, inflammation and stage 2 promotion. 62 The reversibility of complete tumor promotion, therefore, is linked to the 2nd
rather than the 1st stage and reflects the reversibility
of epidermal hyperplastic transformation induced by
TPA.63
The converting activity of TPA in the 1st stage is
slowly reversible, requires undisturbed DNA synthesis, 64 and is characterized by the early occurrence of
dark basal keratinocytes. 56 An observation that may be
relevant to the 1st stage is that the hyperplasia of the
epidermis, dermis and hair follicles and the dark basal
cells are maximal after the 4th TPA treatment. 65 One
theory is that limited applications of TPA in the 1st
stage might only trigger the expression of the altered
genetic information of the DMBA-initiated cells,
which would acquire a neoplastic phenotype but remain
dormant. Then, the 2nd stage of tumor promotion may
simply involve a selection and clonal expansion of neoplastic cells.
Interestingly, the presence of initiated cells is not a
prerequisite to establish stage 1 promotion since the
specific events responsible for conversion by TPA may
be " f i x e d " in normal epidermal cells several weeks
before their initiation with DMBA. 66-68Thus, both normal and initiated epidermal cells exhibit a long-lasting
but not permanent " m e m o r y " for stage 1 promoting
effects of TPA that may complement the past or future
381
irreversible alterations of tumor initiation. 66,68It is not
known whether the ability of a few TPA treatments to
induce DNA damage, chromosomal aberrations and
aneuploidy69 st is linked to their stage 1 tumor-promoting activity. In analogy with the two-hit theory for
the monoclonal origin of most neoplasms and the
mechanism of viral carcinogenesis involving at least 2
mutational events, the cumulative cell-damaging
events triggered by the combinations initiation--stage
1 promotion or stage 1 promotion--initiation may shift
the epidermis into a state of increased promotability, 67
in agreement with the report that TPA enhances viral
transformation.82
When the start of complete tumor promotion by TPA
or the anthrone derivative chrysarobin is delayed 10
weeks after DMBA initiation, the development of skin
tumors is faster and sometimes greater than when promotion immediately follows initiation. 83,84 Moreover,
when the repetitive treatments with the stage 2 promoter MEZ alone are delayed 10 weeks after DMBA
initiation, their effectiveness in promoting skin tumors
becomes equal to that of the two-stage promotion protocol [Table 1 (Protocol 2 ) ] . 83 These findings suggest
that, because tumor initiation provides indirectly the
initiated cells with a proliferative advantage over normal surrounding cells on the basis of their resistance
v e r s u s commitment to terminal differentiation, more
of the initiated cells have had the time in these initiation/delayed promotion experiments to slowly expand
their progeny at the expense of the non-initiated cells
until their clone size reaches a critical threshold of
promotability. 83 This implies that, by stimulating cell
proliferation and differentiation, the few applications
of TPA in the 1st stage may accelerate the differentiation and migration of the non-initiated cells out of the
basal layer, thereby providing space along the basement membrane to favor indirectly the expansion of
the initiated cells resistant to signals of terminal differentiation. 83 Such theory is substantiated by the ability of stage 1 promoters to induce the accumulation of
dark basal and suprabasal cells resembling fetal-type
dedifferentiated keratinocytes. 56 Therefore, the clonal
expansion of the initiated basal keratinocytes at the
expense of the normal cells still committed to differentiation, maturation and degeneration may occur
spontaneously with time after initiation, but much more
slowly then after exposure to a 1st stage tumor promoter. 83 Moreover, in addition to favoring initiated
cells over normal cells on the basis of their resistance
v e r s u s commitment to terminal differentiation, the toxicity of TPA and other promoters may select rapidly
growing initiated cells over more slowly growing initiated or normal epidermal cells. 85 Similarly, it has
been postulated that SENCAR mice are more respon-
382
J.-R PERCHELLET and E. M. PERCHELLET
sive to the various initiation-multistage promotion protocols because populations of constitutively altered
epidermal cells develop spontaneously in these animals
and their skins contain a greater proportion of promotable initiated cells than the skins of other less sensitive strains. 37
As opposed to modulating the hyperplastic events
responsible for the late propagation of the neoplastic
epidermal cells in stage 2 promotion, a breakthrough
in understanding the key molecular events involved in
the early initiation and conversion phases of skin carcinogenesis would appear more likely to stimulate new
ideas for the development of novel methods of cancer
detection or effective therapies to prevent, block or
inhibit the neoplastic process in humans. However,
most in vivo studies on experimental skin carcinogenesis are devoted to the analysis of promotion only (over
60%) with surprisingly few concerned with initiation
alone (13%). 86 Recent findings indicate that all
DMBA-initiated skin Pa possess a point mutation in
the 61st codon of one c-ras Ha allele irrespective of
whether complete tumor promotion is achieved with
benzoyl peroxide (BPx), TPA or the combination stage
1 TPA-stage 2 MEZ. ~7 This mutation is detected
uniquely in the skin Pa as early as 9 weeks after starting
promotion and not in the other epidermal cells of the
dorsal skin that surround the tumors and are also exposed to the promotion treatment. These data reinforce
the theory that the point mutation coincides with the
initiating event and that any type of promoting regimen
can select these mutation-bearing initiated epidermal
cells and induce their transformation and clonal expansion into skin tumors.
Tumor progression
After a relatively short induction period, the twostage system of tumorigenesis [Table 1 (Protocol 1)]
produces mostly benign skin Pa which may either persist, regress or later develop into invasive Ca. The
development of malignant skin Ca from preexisting Pa
is a relatively rare (approximately 5-10% of Pa progress to Ca) and late event (20-40 weeks after the start
of promotion) 88 and its frequency appears to be promoter-independent. Experiments with Pa-bearing mice
demonstrate that this low frequency of malignant conversion of Pa to Ca is unaffected by the continued
application of TPA 89,9 but can be significantly increased by treatments with the free radical generator
BPx or the tumor initiators ethylnitrosourea (ENU) and
l-methyl-3-nitro- 1-nitrosoguanidine (MNNG) [Table 1
(Protocols 3-5)]. 89,91-94 A balance between the promoting and cytotoxic effects of chronic TPA treatments
has been proposed to explain the fact that increasing
the dose and duration of promotion with this agent
adversely affects the yield of Ca. 20New studies provide
strong evidence that the dose of carcinogen used as
initiator plays a critical role in determining which initiated cells will progress to malignancy during or after
promotion. 95 Tumor progression, therefore, is proposed to involve a number of genetic alterations. It is
theorized that subpopulations of epidermal cells may
acquire potentially malignant chromosomal changes at
any time before or after their initiation, conversion or
propagation. 96 Subsequently, those benign neoplastic
cells that have accumulated additional sublethal genetic alterations, besides those associated with tumor
initiation, may be selected to develop malignant characteristics. Interestingly, BPx is a weak complete promoter of mouse skin tumors but neither a tumor
initiator nor a complete carcinogen. 97 The genotoxic
effects of this free radical-generating peroxide may not
be sufficient to produce critical initiation lesions but
may contribute to certain DNA damage or chromosomal aberrations accelerating the progression of benign epidermal tumor cells toward a higher degree of
aneuploidy and malignancy. 93'94
Complete carcinogenesis
Skin tumors can be induced by either a single application of a carcinogenic dose [Table 1 (Protocol 6)]
or repeated applications of a subcarcinogenic dose [Table 1 (Protocol 7)] of DMBA. The tumors that arise
in these protocols are theoretically the result of both
the initiating and promoting abilities of DMBA. Thus,
the irreversible and cumulative effects of multiple subcarcinogenic doses of DMBA [Table 1 (Protocol 7)]
can achieve tumor initiation, conversion, propagation
and progression. In contrast to the DMBA-initiation
TPA-promotion regimen [Table 1 (Protocol 1)], complete carcinogenesis by DMBA [Table 1 (Protocols 6,
7)] is characterized by the late occurrence of fewer Pa
but the Ca develop much earlier. In the DMBA protocols, therefore, the yield of skin tumors is lower but
they have a higher frequency of malignancy and progress to Ca more rapidly. ~
The facts that the glutathione (GSH) peroxidase and
ODC responses to TPA and MEZ are different from
those to DMBA, and that antioxidant and retinoid treatments inhibit ODC induction and skin tumor promotion
by TPA and MEZ but not by DMBA, suggest that the
nature and mechanism of tumor promotion by the phorbol esters and related diterpenes may be different from
those of the promoting component of DMBA carcin-
Antioxidants and skin carcinogenesis
ogenesis. 8,gs-l The magnitude and time course of in-
duction of epidermal ODC activity by the anthracenederived tumor promoters chrysarobin and anthralin are
considerably different from those characterizing the
ODC responses to TPA and MEZ but resemble the
effects of DMBA on ODC induction, ll'm2 Moreover,
the lower tumor incidence, the longer latency of Pa
development and the greater ratio of Ca:Pa observed
with chrysarobin and anthralin as opposed to TPA suggest that the mechanism of ODC induction and skin
tumor promotion by chrysarobin and anthralin is different from that of TPA and more like the promoting
stage which occurs during complete carcinogenesis
w i t h D M B A . 84'11'12 Although it is not clear whether
tumor formation accomplished by the complete carcinogenesis process involves a promoting component
with a mechanism analogous to TPA, DMBA, and the
anthrone promoters may promote the expression of a
subclass of Pa with a high probability of progressing
to Ca. The overall tumorigenicity of various compounds or protocols may reflect major differences in
their ratios of initiating : promoting ability. 103Although
distinct underlying mechanisms may be responsible for
these different kinetics of tumor development, the process of skin carcinogenesis by either of these protocols
is likely to involve the same basic sequence of cellular
alterations (Table 1).
383
THE ROLE OF OXIDANTS IN MULTISTAGE
SKIN CARCINOGENESIS
Cellular prooxidant states appear to play an important role at critical steps of the process of skin carcinogenesis. 104-110Epidermal cells treated with chemical
carcinogens and/or tumor promoters may overproduce
ROS and be deficient in their ability to destroy them.
Increased levels of potentially damaging oxidants are
associated with neoplastic cells but it is unclear
whether free radical reactions are a major cause of
cellular lesions or merely a consequence of them. Increased radical formation may simply result from the
release of intracellular, non-protein bound metal catalysts within damaged cells, ll~
Production of ROS
Much research linking free radicals and neoplastic
transformation has focused on the intermediates of 02
reduction. The sequential formation of the various
types of O2-centered free radicals 112is illustrated (Table
2). The reduction of the molecule of ground-state 02
by a single electron produces the superoxide anion radical 02 ~ (reaction a). It should be noted that 02 ~ exists
in e q u i l i b r i u m with a protonated form, perhydroxyl
radical HO2", which is a more reactive radical then is
02 ~ in aqueous solution. Spontaneous dismutation of
Table 2. Production and Detoxification of Reactive 02 Species
Reaction
Radical Generation
02 + e
~ 02;
02- + H +
' HO2"
2 02: + 2 H +
~ H202 + 02
H202 + Fe2+
, Fe3+ + -OH + OH
H202 + 02 ~ catalyst
Fesalt) 02 + -OH + OHLH + .OH
, L. + H20
L" + 02
, LO2'
LO2' + LH
, L" + LOOH
2 LOOH ~complexes LO" + LO2" + H20
LO. + LH
~ L. + LOH
Radical Degradation
Fe3+-Desferrioxamine complex
aTH + L(O)O.
~ aT. + L(O)OH
aT. + L(O)O.
, Termination products
2 02- + 2H + SOD H202 + 02
2 GSH + H202
CAW
~ 2 H20 + G S S G ~
G
+ LOOH S~-d~.d.tGSHperoxide LOH + H20 + GSSG
(a)
(b)
(c, Fenton)
(d, Haber-Weiss)
(e)
(f)
(g)
(h)
(i)
(J)
(k)
(I)
(m)
(n)
Se-independent GSH peroxidase
GSH S-transferases
GSSG-R
NADP~
.~NADPH
Glucose-6-Phosphate Dehydrogenase
Glucose-6-Phosphate
:~,,~
6-Phosphoglucolactone
384
J.-P. PERCHELLETand E. M. PERCHELLET
two molecules of O2 ~- in aqueous solution generates
H202 (reaction b). The H202 so formed can be reduced
by various metal salts present in tissues to form the
hydroxyl radical -OH (Fenton reaction c). 02- and
H202 may also interact in vivo to form .OH only if the
overall equation is catalyzed by traces of transition
metal ions (iron-catalyzed Haber-Weiss reaction d).
Because of its extreme reactivity, .OH will immediately react with molecules near the site of its generation. ironically, the less reactive 02 ~ and U20/ may
be more damaging because they can diffuse away from
their site of generation and induce .OH production in
remote cellular locations. In contrast to 02 ~ , U202 can
even cross cell membranes and damage other cells.
Therefore, the biological damage done by 02"- and
H202 that is mediated by .OH formation depends
largely on the location of the metal ion complexes
catalytically active in reactions c and d.~l~ Low concentrations of H202 induce DNA damage in vivo and
in vitro, possibly through ferryl radicals generated by
the fenton reaction. ~3
The highly reactive .OH may abstract a hydrogen
atom from an unsaturated fatty acid LH to form a lipid
radical L. (reaction e) and, therefore, initiate a rapid
autocatalytic chain reaction leading to the formation
of lipid hydroperoxides (LOOH). After rearrangement
of the double bonds to form a conjugated diene, the
stabilized lipid molecule containing a carbon radical
rapidly reacts with molecular 02 to give a peroxyl radical LO 2" (reaction f), which can then abstract a hydrogen atom from an adjacent lipid molecule to
produce a LOOH (reaction g) and so continue the chain
reaction of lipid peroxidation. ~2 The decomposition of
these lipid hydroperoxides in the presence of transition
metal ions yields alkoxyl (LO.) and peroxyl (LO2")
radicals (reaction h), which may themselves abstract
further hydrogen atoms and contribute to the initiation
and progapation of new chain reactions of lipid peroxidation (reactions g and i). The small "transit" pool
of non-protein bound iron moving between transferrin,
cell cytoplasm, mitochondria and ferritin could provide
the catalyst required for .OH formation and chain-propagation of lipid peroxidation (reactions c, d, and h). l~t
The lipid peroxyl radicals LO2" may be the major
O2-centered free radicals generated in a cell as a result
of 02 reduction or lipid peroxidation. Compared with
other O2-centered free radicals, LO2" are more stable
species capable of diffusing to cellular loci distant from
the site of their generation. Therefore, their role in
interacting directly or indirectly with DNA and/or
other macromolecules and producing cellular lesions
associated with carcinogenesis may be more important
than that of .OH. l J4 However, lipid peroxidation seems
to occur at a late stage in the injury process and may
contribute little to it. ~J5Nucleic acids and proteins may
also be oxidized and/or converted to free radical forms,
which in turn are highly reactive and may create crosslinks. One of the current hypothesis is that such an
oxidative challenge might contribute significantly to
the induction, promotion and/or progression of skin
tumors. For instance, the role of O2-derived free radicals in mediating ionizing radiation-induced DNA
damage and cytotoxicity is well established. ~16'~7 The
genetic material is undoubtedly the primary target of
oxidant attack in v i v o 1SA9tlSA18"t19 since the above
ROS consistently induce mutations, DNA adducts and
strand breaks, and clastogenic effects in cells subjected
to oxidative stress. The possibility has been suggested
that the initiating and promoting components of carcinogenesis may be triggered by qualitatively and
quantitatively different levels of primary and secondary oxidizing agents causing different levels of mutation, DNA damage and chromosomal aberration.~4
Detoxification of ROS
The major intracellular antioxidant defense relies
on enzymatically removing O2- and H202 hopefully
before they reach the iron catalysts and form "OH and
ferryl radicals. Conversely, an experimental means of
antioxidant protection is to decrease the availability of
metal catalysts required for the damaging free radical
reactions c, d, and h. For example, the specific and
powerful iron chelator desferrioxamine methanesulfonate (Desferal; C1BA-GEIGY) may protect against
OH generation and lipid peroxidation by preventing
complexes of iron salts from participating as catalysts
in radical reactions (j). ~ In addition to the detoxifying
enzymes superoxide dismutase (SOD), catalase (CAT),
and GSH peroxidase, the cells maintain a multi-level
protective system against free radical generation and
lipid peroxidation including both lipid-soluble membrane scavengers such as cx-tocopherol (o~TH, vitamin
E) and water-soluble cytoplasmic antioxidants such as
GSH (Table 2). 12
At the membrane level where the concentration of
the natural cellular antioxidant GSH is probably minimal, the lipid-soluble free radical scavenger o~TH may
play an important role in preventing oxidative processes from taking place. Effective antioxidant protection by oLTHappears to be due to efficient inhibition
of lipid oxy-radical propagation in the bilayer rather
than to interception of initiating 02 radicals. 121 Concentrations of c~TH increasing above the threshold of
0.2 mole percent (based on phospholipid content of
liposomes) decrease the average radical chain length
and the ratio of LO2" to LO. in the bilayer and induce
Antioxidants and skin carcinogenesis
termination of lipid oxy-radical propagation (reactions
k and 1).
Other types of antioxidants may spontaneously and/
or enzymatically prevent the formation of the dangerous OH radicals by reducing U202 before it can react
further. The endogenous antioxidant GSH ~22meets this
requirement because it is present at relatively high concentrations in the aqueous part of the cells where reactions a-d are likely to occur. Moreover, reduction
of oxidative stress is also accomplished by the action
of the following enzymes which control the cellular
level of H202 (Table 2).~2 Native SOD or SOD-mimicking compounds such as Cu(II)-(3,5-diisopropylsalicylate)2 (CuDIPS) accelerate the removal of 02;
radicals (reaction m). In addition to CAT activity, the
detoxification of H202 in the cytoplasm is accomplished largely by the GSH peroxidase-glutathione
reductase (GSSG-R) couple, a NADPH-consuming
system which is extremely specific for GSH and requires adequate concentrations of glucose and Se to
work. 122 Unlike CAT, the Se-dependent form of GSH
peroxidase containing selenocysteine at its catalytic
site is capable of rapidly detoxifying both U202 and
lipid hydroperoxides (reactions n and o). In contrast,
non-Se dependent GSH peroxidase uses organic
hydroperoxides but not H202 as substrates and has
been shown to be associated with another family of
protective enzymes, the GSH S-transferases (reaction 0). 123 125There are multiple forms of GSH S-transferases located principally in the cytosol.~26 Although
conjugation of GSH to certain xenobiotics may be accomplished to some degree by spontaneous non-enzymatic reactions, conjugation with GSH catalyzed by
the GSH S-transferases is an important process for the
cellular detoxification of hydrophobic agents bearing
electrophilic sites. 122.127Thus, the GSH peroxidase activity of the GSH S-transferase (reaction o) may be of
paramount importance to protect from lipid hydroperoxide damage the biological systems that have no or
very little Se-dependent GSH peroxidase, even though
such protection may not be the primary action of this
closely related group of enzymes.~28 In mouse epidermis in vivo and in vitro, Na2SeO3-dependent GSH peroxidase activity represents about 65-75% of the total
GSH peroxidase activity.129
Free radicals in tumor initiation
Although increased free radical generation can lead
to DNA damage and is potentially carcinogenic, the
role of ROS in tumor initiation is not well documented.
Transition metal ions, such as iron, are involved in the
O2~--dependent formation of more reactive radicals and
may affect the initiation of neoplasia. ~2 The free rad-
385
ical-generating agents BPx, lauryl peroxide and H202
may be inactive as skin tumor initiators because the
doses of peroxides capable of inducing irreversible
DNA lesions may be too toxic to permit the survival
of a population of initiated epidermal cells large
enough to be promoted.~3
The essential step in the process of skin tumor initiation is the metabolic activation of DMBA by
NADPH- and cytochrome P448-dependent TM microsomal mixed-function oxidases that are induced in the
epidermis 132,~33 and generate highly reactive electrophilic derivatives, which covalently modify DNA and
other cellular macromolecules.134 A sequence of three
monooxygenase-, epoxide hydratase- and monooxygenase-catalyzed reactions affecting the angular benzo
ring adjacent to the " b a y region ''135 converts the
"procarcinogenic" PAH parent molecule DMBA into
mutagenic oxidation products often called the
" p r o x i m a t e " and "ultimate" forms of the carcinogen:
the initial non-K-region epoxide is then hydrated to
give a dihydrodiol, and finally the oxidation of the
double bond adjacent to the dihydrodiol grouping
yields the " b a y region" vicinal diol-epoxide that is
probably the 3,4-diol 1,2-oxide of DMBA. 136 Thus,
the efficiency of tumor initiation in mouse skin is related both to the dose of DMBA applied and to the
extent of induction of the epidermal microsomal aryl
hydrocarbon hydroxylase (AHH) activities necessary
to catalyze the formation of the electrophilic " b a y region" diol epoxide mutagens in the presence of a
NADPH-cytochrome P448 electron transport system. 132.133,137142Genetic studies suggest that, in different strains of mice, high AHH inducibility leads to
increased susceptibility to PAH-induced tumors.143
In addition to the formation of electrophilic ultimate carcinogens directly inducing DNA lesions, the
metabolic activation/degradation of PAHs may proceed through quinone derivatives and free radical intermediates, thereby producing ROS that may indirectly contribute to the persistence of unrepaired
DNA damage resulting in initiation of the affected
cells.144 14s An O2-dependent metabolic pathway has
been described, in which semiquinone intermediates
of PAHs participating in redox cycles are oxidized to
quinone metabolites with concomitant reductive generation of 027 subsequently triggering H202 and .OH
formation. ~49.150Since ionizing radiations are known to
damage DNA either directly or indirectly through free
radical generation, ~7 it is interesting to note that a
single subtumorigenic dose of ionizing radiations mimics the initiating activity of DMBA in the two-stage
initiation-TPA promotion protocol in mouse skin. TM
Moreover, the increased generation of ROS by leukocytes during skin inflammation is clearly implicated
386
J.-P. PERCHELLETand E. M. PERCHELLET
in the metabolic activation of PAHs in mouse skin. 152
The oxidative challenge produced by the polymorphonuclear (PMN) leukocytes that are recruited and
subsequently activated by two pre-treatments of the
skin with TPA 16 h before and immediately prior to
initiation has been shown to enhance the metabolic
activation of the penultimate carcinogen benzo[a]pyrene (BP) 7,8-dihydrodiol to genotoxic and chemiluminescent metabolites through myeloperoxidase-dependent pathways.~53 Therefore, it is conceivable that
the oxidative burst induced by the metabolically stimulated leukocytes infiltrating the sites of inflammation
in mouse skin could facilitate or enhance either directly
or indirectly the tumor-initiating activity of DMBA.
The possible link between inflammation and cancer has
been reviewed. ~52,~53The free radicals may act as tumor
initiators by direct damaging interaction with DNA,
indirect formation of clastogenic factors, or induction
of cooxygenation in carcinogen metabolism.
The relevance of arachidonic acid metabolism to
skin tumor initiation is sugested by the finding that
PAH dihydrodiols are cooxidized to mutagenic derivatives during PG biosynthesis.~54'~55 PG endoperoxide
synthetase contains both fatty acid cyclooxygenase and
hydroperoxide activities, which catalyze the biosynthesis of hydroxy endoperoxides from arachidonic
acid. ~56 The peroxidative oxidation mediated by the
enzyme PG H synthetase in the presence of arachidonic
acid may simultaneously trigger the cooxidation of
PAH carcinogens. 157 Arachidonic acid treatment prior
to DMBA stimulates tumor initiation, an effect which
is abolished by the simultaneous administration of the
inhibitor of PG synthesis, indomethacin. 154The mechanism of PG endoperoxide synthetase-dependent cooxygenation, therefore, may play an important role in the
oxidative activation of carcinogenic metabolites in tissues with low NADPH-dependent mixed-function oxidase activity. ~54 The excellent correlation observed
between LOz" and diol-epoxide formation m suggests
that the LOz" generated during arachidonic acid metabolism may be the oxidants that epoxidize the penultimate dihydrodiol metabolite of DMBA to the
ultimate diol-epoxide form of the carcinogen. 1~4However, recent studies with isolated epidermal cells suggest that the major source of LOz" may be lipid
peroxidation rather than the enzymes of arachidonic
acid oxygenation. ~4 During metabolic activation of
DMBA, the LOz" radicals play no role in the first epoxidation reaction, which is catalyzed solely by inducible
microsomal monooxygenases. In contrast, both LOz"
and P448-dependent enzymic reactions may contribute
to the terminal step of the pathway of metabolic activation of the initiator DMBA. The kinetics of mixedfunction oxidase induction or inhibition, DNA adduct
formation and skin tumor initiation suggest that, in
intact epidermal cells, LOz'-dependent epoxidation of
dihydrodiols to diolepoxides may be an effective alternative to cytochrome P448-dependent epoxidation
since the induction of the latter enzymic pathway is
not absolutely required for the metabolic activation of
low tumor-initiating doses of DMBA in mouse skin. 114
In conclusion, the catalytic action of microsomal cytochrome P448-dependent monooxygenases is not
exclusively involved in tumor initiation. The tumorinitiating diol epoxides may be formed as well by oxidation of the penultimate metabolites of PAHs through
LOz" or other free radicals generated during lipid
peroxidation ~59 or the oxidative burst accompanying
the state of inflammation, ~52~53 or by the peroxidase
component of PG synthetase. 154,L55.157,158
Free radicals in tumor promotion
The relationships between cellular prooxidant states
and tumor promotion have been reviewed. 5L~4-~1'16.~61
The role of Oz-centered free radicals in tumor promotion is supported indirectly by the obvservations that
1) tumor promoters increase the generation and decrease the degradation of ROS; 2) certain organic peroxides and free radical-generating systems exhibit
tumor-promoting activities and mimic or enhance some
of the molecular events linked to tumor promotion; and
3) various antioxidants and free radical scavengers inhibit the biochemical and biological effects of the tumor promoters. The latter point is developed in the
following section. Since tumor promoters are not mutagenic and do not interact directly with DNA, it is
postulated that their reported effects on aneuploidy ,70,71
chromosomal aberration, 69.7z-75 sister chromatid exchange,76 80 DNA strand breakage, 81 and gene
amplification 3'3zSz'53"Sv are indirect and may be mediated through ROS generated in the TPA-treated epidermal cells themselves and/or released by the
activated phagocytic cells infiltrating the skin during
inflammation. The fact that TPA does not inhibit
gamma radiation-induced DNA repair in resting lymphocytes argues against the hypothesis that tumor promotion is the result of impaired repair of potentially
mutagenic lesions in DNA.~62
One of the current hypotheses is that an increased
generation of free 02 radicals coupled with a defective
antioxidant protective system could explain some of
the mechanisms of tumor promotion and progression.
Although different interpretations have been proposed
to explain these observations, ~63 the activities of the
detoxifying enzymes SOD and CAT seem to be significantly depressed by the tumor promoters, 164.165
Antioxidants and skin carcinogenesis
240-,
220
.
,
A.
e~6 16c
14C
120
I01
I
:,=
160
120
BI
moo
Ct
so
:E.,-
6o
40
:~0.. , .
-=
2
5
Time (hours)
Fig. 2. Time-response curves for the effects of 1 #M TPA on the
level of hydroperoxide (A) GSH peroxidase activity (B) and the
intracellular GSH:GSSG ratio (C) in suspensions of disrupted (A)
or intact (B,C) mouse epidermal cells freshly isolated by trypsin
digestion. '72 The total volume of the incubation mixture was 1 ml;
2 x 106 epidermal cells were resuspended in 0.8 ml of modified
Eagle's HeLa cell medium containing 25 mM Hepes buffer, pH 7.0,
and 10% bovine serum, and the reagents were added in a total volume
of 0.2 ml. Dimethyl sulfoxide (DMSO) was used as a vehicle for
TPA; its final concentration in the medium was 0.5%. At the end
of each incubation period, 1 ml of 20% trichloroacetic acid (TCA)
was added to the cell-free systems and the whole acid-soluble supernatant was collected by centrifugation and mixed with 0.6 ml of
ferrithiocyanate assay reagents? 73=74The absorption of the red ferrithiocyanate complex formed in the presence of peroxide was measured against a reagent blank at 480 nm in a Shimadzu-160 double-beam spectrophotometer and compared to H202 standards. The
soluble epidermal extracts containing GSH peroxidase activity were
prepared from the intact cells and total GSH peroxidase activity was
determined with 1.5 mM cumene hydroperoxide as described previously. ,29.,79-~82The enzymic determination of the intracellular levels
387
w h e r e a s c e r t a i n c l a s s e s o f r e a c t i v e 02 i n h i b i t o r s inc l u d i n g C A T and v a r i o u s S O D - m i m i c k i n g c o m p o u n d s
g e n e r a l l y i n h i b i t s o m e o f the b i o c h e m i c a l and b i o l o g ical e f f e c t s o f the t u m o r p r o m o t e r s . 99'166-169 R e c e n t l y ,
w e h a v e e s t a b l i s h e d the s e q u e n t i a l r e l a t i o n s h i p s bet w e e n the e f f e c t s o f T P A on h y d r o p e r o x i d e f o r m a t i o n ,
G S H p e r o x i d a s e a c t i v i t y and the i n t r a c e l l u l a r ratio o f
reduced glutathione (GSH): oxidized glutathione
(GSSG).
O u r c u r r e n t studies i n d i c a t e that T P A rapidly stimulates h y d r o p e r o x i d e p r o d u c t i o n in intact e p i d e r m a l
cell and c e i l - f r e e s y s t e m s i n c u b a t e d in the p r e s e n c e or
a b s e n c e o f e n z y m i c and n o n e n z y m i c g e n e r a t o r s o f
R O S . 170"171 E p i d e r m a l c e l l s (2 x 106 c e l l s / m l ) f r e s h l y
i s o l a t e d f r o m m o u s e skin by trypsin d i g e s t i o n 172 w e r e
d i s r u p t e d by s o n i c a t i o n and i n c u b a t e d for v a r i o u s periods o f t i m e in the p r e s e n c e or a b s e n c e o f 1 ktM T P A
(Fig. 2 A ) . T h e h y d r o p e r o x i d e c o n t e n t s o f the acids o l u b l e s u p e r n a t a n t s c o l l e c t e d at the end o f the incub a t i o n w e r e a s s a y e d at acid p H by a m o d i f i c a t i o n 173 o f
the f e r r i t h i o c y a n a t e m e t h o d . 174 In this T P A - s t i m u l a t e d
e p i d e r m a l s y s t e m , the s t e a d y - s t a t e l e v e l o f h y d r o p e r o x i d e s i n c r e a s e s r a p i d l y and s t e a d i l y for a b o u t 2 h and
r e m a i n s at 2 2 4 % o f the basal l e v e l up to 4.5 h (Fig.
2 A ) . A f t e r i n c u b a t i o n for 5 h in the p r e s e n c e o f 1 # M
concentrations of DMBA, TPA, phorbol- 12,13-didecanoate, MEZ, phorbol- 12,13-dibenzoate, 4-0-methyl
T P A , p h o r b o i and EPP, the l e v e l s o f h y d r o p e r o x i d e s
are, r e s p e c t i v e l y , 2 3 5 , 2 2 4 , 186, 175, 162, 137, 102,
and 9 8 % o f the c o n t r o l l e v e l , s u g g e s t i n g that the hydroperoxide-inducing activities of these agents correlate with their t u m o r - p r o m o t i n g or c a r c i n o g e n i c activities. 170.171 A l t h o u g h the t i m e - c o u r s e and m a g n i t u d e
o f the h y d r o p e r o x i d e r e s p o n s e to T P A are i d e n t i c a l ,
the v a l u e s o f the basal and T P A - s t i m u l a t e d l e v e l s o f
h y d r o p e r o x i d e s m e a s u r e d in s u s p e n s i o n s o f intact epi d e r m a l cells are about 5 0 % s m a l l e r than t h o s e o b t a i n e d
with the e p i d e r m a l c e l l - f r e e s y s t e m . S i m i l a r results
w e r e o b t a i n e d , but at a m u c h l o w e r l e v e l , u s i n g the 4a m i n o a n t i p y r i n e / p h e n o l r e a g e n t and h o r s e r a d i s h per-
of GSH and GSSG was performed in samples deproteinized in 5%
TCA/0.01 N HCI. ,79-,82Hydroperoxide level was expressed as n mol
H202/2 106 disrupted cells/ml, GSH peroxidase activity as ,umol
of NADPH oxidized in 1 min/ 2 106 cells and the levels of GSH
and GSSG as ng/2 x 106 cells. Blank reactions with enzyme source,
glutathione, or hydroperoxide samples replaced by buffer were substracted from the data. Results are expressed at each point as % of
the basal level of H~O2, GSH peroxidase activity or GSH:GSSG
ratio in cells incubated in the absence of TPA. Each point in the
graph is the mean value SD of 6 replications from 2 different
experiments. The mean values of the basal levels of hydroperoxides
(8.6 +- 0.4 nmol H202/ml; 100 --- 5%), the basal GSH peroxidase
activities (0.167 0.014 k~mol of NADPH oxidized/min/2 x 106
cells; 100 --- 8%) and the basal GSH:GSSG ratios (24.3 --- 1.8;
100 --- 7%) at each point in control incubations have been indicated
by the hatched areas.
388
J.-P. PERCHELLETand E. M. PERCHELLET
oxidase, an enzymic assay performed at physiological
pH and which is specific for H202 .175 177 In other in
vivo experiments, groups of mice received either acetone, 1, or 2 topical applications of 8.5 nmol of TPA
at 24 h interval and were killed i 2 h after the last TPA
treatment. When incubated in vitro in the presence or
absence of 5 mM NAN3, the levels of hydroperoxides
in the homogenates prepared from the skins treated
once or twice with TPA were 1.5- and 3-fold higher,
respectively, than the control levels in the homogenates
from the skins treated with acetone only. 171Phagocytic
cells may contribute to the H202 responses in the homogenates prepared from skins pretreated with TPA or
DMBA in vivo. The fact that similar H202 responses
are detected in epidermal cells and homogenates,
which are isolated or prepared from non-treated skins
and then incubated directly with TPA or DMBA,~7'~7~
suggests that the increasing levels of H202 are generated largely by the TPA-and DMBA-treated keratinocytes and cannot reflect entirely the oxidative burst of
activated leukocytes infiltrating the skin. Indeed, the
keratinocytes may be the major source of H202 in the
epidermis. ~TX
The sequential and dose-dependent relationships between the decreasing effects of TPA on the intracellular
G S H : G S S G ratio and GSH peroxidase activity in
mouse epidermis in vivo and in vitro suggest that the
GSH-dependent detoxifying system cannot fully protect the epidermal cells for an extended period of time
against the oxidative challenge caused by the tumor
promoter. 1'129179-t~3As shown in Figure 2 (B and C),
the incubation of intact epidermal cells with TPA leads
within about 20 min to a rapid, transient increase in
GSH peroxidase activity, which is concomitant with a
dramatic fall in the GSH : GSSG ratio. This is followed
after 1 h by a prolonged inhibition of GSH peroxidase
activity while the G S H : G S S G ratio remains low.
Taken together, the time-dependent studies presented
in Figure 2 (A, B, and C) suggest that the increased
generation of peroxides by TPA initially stimulates the
activity of the GSH-dependent detoxifying system. Although an undetermined amount of spontaneous, nonenzymatic GSH oxidation is likely to occur, the early
and transient induction of GSH peroxidase activity in
the TPA-treated, H202-producing cells may be responsible for the rapid elevation of GSSG and decline in
the intracellular GSH : GSSG ratio. The phenomena observed 2-4.5 h after TPA may be crucial in understanding the cause and prevention of some of the
molecular events of tumor promotion. At these times,
the TPA-treated cells are still accumulating hydroperoxides but their GSH peroxidase activity is now inhibited and their GSH : GSSG ratio remains abnormally
low. Whether it is due to the continual challenge caused
by the presence of TPA in the incubation medium or
to the now depleted intracellular level of GSH, it is
postulated that, a couple of hours after TPA treatment,
the endogenous GSH antioxidant system of the epidermal cells cannot reduce the excessive level of peroxidation possibly triggering macromolecule-damaging events linked to the tumor-promoting activity
of TPA.
Increased peroxidation is easier to detect when hydroperoxide decomposition is inhibited. ~v4'~84For example, whole skin homogenates incubated for 5 h in
the presence of NaN3 contain 4 times more hydroperoxides than in its absence (Table 3). The increased
accumulation of peroxides is also observed in epidermal systems incubated in the presence of 3-amino1,2,4-triazole, diethyl maleate (DEM), l-chloro-2,4dinitrobenzene (CDNB) and L-buthionine-SR-sulfoximine, the compounds that inhibit CAT activity or decrease the availability of GSH. 171 The enzymic and
nonenzymic generation of hydroperoxides in mouse
skin homogenates incubated for 5 h at 37C in 50 mM
potassium phosphate buffer, pH 7.4, containing 118
mM NaCI, 5.36 mM KCI, 1 mM CaCI2, 0.85 mM
MgSO4 and 5 mM dextrose under a 95% 02-5% CO2
atmosphere is reported in Table 3. TPA is equally effective in stimulating hydroperoxide production in control and NaN3-treated homogenates. TPA enhances the
hydroperoxide responses to various enzymic systems
including NADPH, glucose (G)/glucose oxidase (GO)
and xanthine (X)/xanthine oxidase (XO). Moreover,
TPA can also stimulate the nonenzymic, NADPH-independent production of peroxides promoted by ascorbic acid (ASC, vitamin C) or the FeCI~/FeSO4/
EDTA complex. These results suggest that TPA may
increase the levels of peroxidation and cellular damage
in mouse epidermis through the stimulation of the
prooxidant activities of various endogenous enzymic
and nonenzymic sources of ROS.
Our results are consistent with the observations that
TPA stimulates the generation of ROS in leukocytes
and provokes a chemiluminescence (CL) response
that peaks and persists after 5 - 3 0 min. ~5 As early as
1976, DeChatelet et al. ~86have shown that TPA rapidly
increases the cellular production of H202. The cytotoxic potential of activated macrophages and granulocytes has also been demonstrated to correlate with
their ability to release H202 in response to TPA. I87
Several phorbol ester derivatives with various tumorpromoting activities have been shown to stimulate the
generation of H202 by macrophages during a 60-rain
incubation period. ~88Moreover, TPA has already been
reported to stimulate H202 production in mouse skin
in vivo after 30 min.~89 In murine epidermis, TPA induces the specific activity of XO, ~9 a O2~-generating
Antioxidants and skin carcinogenesis
389
Table 3. Enzymic and NonenzymicGeneration of Hydroperoxidesin Mouse Skin (epidermis +
dermis) HomogenatesTreated with TPA
Hydroperoxide Formationt
Incubation System*
Control (no addition)
+NAN3
+NAN3 + N A D P H
+NAN3 + glucose/glucose oxidase
+NAN3 + xanthine/xanthine oxidase
+NAN3 + ascorbate
+NAN3 + FeCIflFeSO4/EDTA
TPA (1 pM)
+NAN3
+NAN3 + N A D P H
+NAN3 + glucose/glucose oxidase
+NAN3 + xanthine/xanthine oxidase
+NAN3 + ascorbate
+ NaN3 + FeC13/FeSOJEDTA
nmol/mg
Protein/5 h r : ~
10.6 -+ 0.4
46.0 _+ 1.9
100.5 +- 4.6
128.3 _+ 5.8
149.4 _+ 7.1
84.6 - 3.2
130.3--- 5.2
23.0 +- 0.9
94.7 _+ 3.7
188.5 -+ 8.3
293.5 -+ 15.3
255.3-+ 12.3
114.1 _+ 4.6
216.7 _+ 10.0
% of
Control
% of Respective
Incubate
Without TPA
100
434
948
1210
1410
798
1229
217
893
1778
2769
2408
1076
2044
217
206
188
229
171
135
166
*Thc volume of each incubate was 1 ml with a protein concentration of 1.5 mg/ml. The concentrations used
were: 2.5 mM NAN3; 1 mM NADPH; 2.5 mM glucose/0.5 munit glucose oxidase; 1.0 mM xanthine/0.5 munit
xanthine oxidase; 0.2 mM ascorbate; 0.1 mM FeClfl0.1 mM FeSOd0,1 mM EDTA.
tDetermined after incubation for 5 h at 37C; ice-cold blanks containing all the components of the incubation
mixtures were subtracted from each value.
SMean + SD of 6 replicates in 2 different experiments.
system shown to mimic the effects of TPA on ODC
induction TM and promotion of cell transformation.192
The tumor-promoting activity of TPA may be related
to its peroxisome proliferative activity.193 In analogy
with TPA, the peroxisome proliferators are not mutagenic and do not covalently interact with DNA but may
modulate gene expression and function as tumor promoters in a two-stage carcinogenesis model. 194,195Peroxisome proliferators stimulate the production of H202
and other ROS and decrease the enzymic defense
against peroxidative damage.196 The resultant oxidant
stress may cause DNA damage either directly or by
initiating lipid peroxidation.
Since ROS, when present in excess, trigger lipid
peroxidation of membranes and cellular damage, it
would be logical to assume that the early imbalance
between hydroperoxide production and degradation observed after TPA in our studies is accompanied by
epidermal lipid peroxidation. However, using the thiobarbituric acid assay, a decline in epidermal lipid peroxidation has been described 4-22 h after TPA treatment in v i v o . 197 In this study, lipid peroxidation
increased whereas GSH peroxidase activity decreased
with the aging of mouse epidermis. However, it might
be critical to re-assess the effects of TPA on microsomal lipid peroxidation at shorter time intervals and
after multiple TPA treatments using the diene conjugation procedure. The level of lipid peroxidation might
not necessarily parallel the H202 response to TPA. In
liver homogenate in vitro prepared from mice treated
in vivo for 14 days with peroxisome proliferators, the
steady-state level of H202 is increased whereas both
GSH peroxidase activity and lipid peroxidation are decreased.198 Interestingly, the tissue level of GSH peroxidase appears to be sensitive to the level of lipid
peroxides. Because the cells maintain a multi-level defense against lipid peroxidation, the sequential transient increase and prolonged decrease in epidermal
GSH peroxidase activity that we observed after TPA
might be linked more directly to the fluctuation of lipid
peroxides than to that of H202. Therefore, a decrease
in lipid peroxidation ~97 and GSH peroxidase activity 100.129,179-183several hours after TPA might not necessarily indicate a decrease in oxidative stress to the
cell. Although the levels of H202 and lipid peroxides
might evolve differently at later times because of different levels of detoxification, both H202 generation
and lipid peroxidation might be implicated in the early
oxidative challenge altering the GSH-dependent antioxidant system during TPA treatment.
The increased level of peroxidation and the decreased efficacy of the GSH protective system may be
characteristic of the tumor growth process. 199 However, it is not known whether increased peroxidation
is indicative of the benign or malignant state of the
skin during carcinogenesis. Inflammatory macrophages from promotion-sensitive SENCAR mice secrete 4 times more H202 than the corresponding cells
from promotion-resistant C57BL/6 mice. 2 Theoretically, if increased peroxidation mediates to some ex-
390
J.-P. PERCHELLETand E.
tent tumor promotion, the skins of these mice should
elicit peroxidative responses to TPA related to their
different sensitivities to tumor promotion by TPA. ROS
mediate nonenzymic, NADPH-supported, and XO-catalyzed lipid peroxidation in microsomal preparations
from whole skin, dermis or epidermisfl ~ NADPH-dependent H20 2 formation in microsomes is mainly due
to NADPH oxidase while about 1/3 may arise from
the autoxidation of cytochrome P450.174'j84 Skin microsomes incubated with NADPH, FeCI3/ADP or low
concentrations of ASC form lipid peroxides. Moreover, the nonenzymic catalysts FeCI3 and ADP enhance
remarkably the enzymic generation of lipid peroxides
in epidermal microsomes. 2~ The nonenzymic FeSO4/
ADP-supported rate of lipid peroxidation has been
studied in epidermal homogenates prepared after the
very heat treatment used in our laboratory. 22 The tumor-promoting activities of the phorbol esters in mouse
skin correlate well with their abilities to induce ODC
activity and DNA synthesis in epidermal cells. 23 Since
the levels of peroxidation in control and TPA-treated
epidermal samples may be several folds greater in the
presence of NAN3, NADPH, G/GO, X/XO, ASC and
FeC13/FeSOg/EDTA than in their absence (Table 3),
one would expect these enzymic and nonenzymic stimulators of lipid peroxidation to enhance as well the
sequential effects of TPA on GSH metabolism, ODC
induction and macromolecule synthesis. By magnifying the effects of TPA, these enzymic and nonenzymic
oxidant-generating systems might provide valuable
tools to elucidate the role of peroxidation in the molecular mechanism of tumor promotion. Indeed, our
preliminary studies (unpublished data) indicate that
concentrations of NaN3 (1-10 pM), CDNB (1-5/~M)
and/or NADPH (0.01-0.1 mM) and G / G O (0.01-0.25
munit/ml) several folds lower than those shown to inc r e a s e hydroperoxide accumulation in skin homoge-
M. PERCHELLET
nates (Table 3) can enhance the ODC-inducing activity
of TPA in suspensions of intact epidermal cells ~72 or
in cultures of intact skin explants, z4 Interestingly, it
has been suggested that mouse skin sensitivity or resistance to TPA as a hyperplasiogen and as a tumor
promoter is likely to be explained on the basis of oxidant generation and 8-1ipoxygenase induction rather
than ODC induction. 25
The significance of increased production of ROS
and elevated peroxidation to the multistage process of
skin tumor promotion is purely speculative. Some of
the major issues to be addressed have been depicted
(Fig. 3). The relevance of PKC induction to the level
of peroxidation/GSH-dependent detoxification during
tumor promotion remains to be determined. The potential role of PKC in stimulus-response coupling has
been reviewed. 45'46,26 PKC is probably a prime target
of several chemically unrelated tumor promoters which
mimic the membrane perturbations caused by diacylglycerol. There is sufficient evidence to suggest that
PKC induction mediates, at least partially, the molecular mechanism by which tumor promoters alter gene
expression. PKC induction has been implicated in the
elaboration of ROS by neutrophils, leukocytes and inflammatory cells. 27-218 Moreover, exogenous diacylglycerols stimulate O2 ~ production, suggesting that
endogenous diacylglycerols may function as messengers for this biological response. 28,2~,2~,2j~ However,
the primary involvement of this enzymic activity in
modulating the production and/or detoxification of
peroxides in epidermal systems treated with TPA has
yet to be demonstrated. In intact cells, phorbol esters
activate NADPH oxidase, the en'zyme system responsible for the oxidative burst. The phorbol ester
promoters similarly activate the oxidase in a reconstituted system which includes a membrane fraction,
ATP, phospholipids, NADPH and either a cytosolic
+ Protein Kinase C
Induction .~.,~iGenerotio n
lf Reactive ._~ Resulting --']
Agent with
~
~. 102 Sl~cies 7 Free Radical[
oae o
Tumor-Promoting
~/
Challenge[
Dam_._ t_
Activity
and I ?
Mocromo~cules, ?
+ l Detoxification[ Increased [ ~ Membranes, DNA,"~-~
~ ] o f
Reactive ] Level of
l
Chromosomes
_ Natural Antioxidon
f
t [ Oz Species [ Peroxidation_.J
Protective Systems
:;~ +
Multistage
_
lumor.
Promohon
and
Progression
Chemotherapy ?
Fig. 3. Postulatedrole of free radicals and epidermal peroxidationin the process of skin tumor promotion and/or progression.
Antioxidants and skin carcinogenesis
fraction or purified P K C . 46 Incidentally, the non-TPA
type tumor promoters palytoxin and thapsigargin,
which do not bind to phorbol ester receptors or activate
PKC, also stimulate O2 ~-formation in neutrophits, suggesting that these compounds activate the NADPH
oxidase system of the cells by different signal transduction mechanisms. 219 TPA stimulates xanthine dehydrogenase (XD) synthesis and the conversion of existing and newly synthesized XD to XO. 19 Several
antibiotics that suppress skin inflammation prevent
H202 production by inhibiting the cell systems generating ROS.22 Moreover, the ability of TPA to induce
peroxisomal enzyme activities and H202 generation is
inhibited by cycloheximide, suggesting that these effects of TPA may be largely the result of de novo
protein synthesis. ~93 New findings suggest that the induction of XO by TPA is a consequence of the hyperplasia induced by the tumor promoter rather than the
cause of it. 22~
In contrast to non-tumor promoters and purely hyperplastic agents, TPA stimulates the accumulation of
hydroperoxides in epidermal cells and cell-free systems
in vitro (Fig. 2, Table 3) 170'171 but the significance of
H202 production, lipid peroxidation and GSH-dependent detoxification to the modulation of gene expression during skin tumor promotion by TPA is not
known. In relation with their weak skin tumor-promoting activities, 97 the peroxides mimic some of the
effects of TPA on PKC induction, 222 cell transformation, 223 single strand break in DNA, 224GSH peroxidase inhibition and ODC induction, 1 but at doses
considerably higher than those of TPA. However, the
peroxides enhance the progression phase of carcinogenesis. 93'94 In accord with our findings on GSH
m e t a b o l i s m, 1'18'~8Hs3 structure function studies indicate that the ability of different phorbol esters
to stimulate the generation of ROS and inhibit
their degradation, and damage DNA and chromosomes correlates with their potency as tumor
promoters. 72"15"18"164'188"19 However, the relevance of
these events to a specific stage of tumor promotion is
not clear: different promoters produce single strand
breaks in DNA of mouse epidermal cells in relation
with their complete and stage 2 tumor-promoting
activities 224 but they stimulate H202 formation and
DNA base modification in relation with their potency
as stage 1 tumor promoters. 225 It has been postulated
that H202-induced damage might be responsible for the
" m e m o r y " effect induced by stage 1 tumor prorooters. 225 On the other hand, PKC induction and generation of 02; do not appear to be of critical importance
for stage 1 conversion. 66,169In agreement with the identical effects of TPA and MEZ on GSH metabolism and
ODC induction observed in our studies, l.18,181.ls3the
391
stage 2 tumor promoter MEZ is at least as potent as
TPA in increasing the generation and decreasing the
detoxification of ROS. 105,108,164A88A90However, the hydroperoxide response to TPA is greater than that induced by MEZ in epidermal cell and cell-free
systems. 170.171In general, purely inflammatory or hyperplastic agents and compounds with no or only stage
1 tumor-promoting activity produce none of these effects. Our findings that peroxides, complete and stage
2 tumor promoters concomitantly deplete the level of
GSH, inhibit GSH peroxidase activity and induce polyamine biosynthesis suggest that the accumulation of
nondetoxified ROS in the epidermis may be one of the
components of the later stages of skin tumor promotion
and progression. Other evidence suggests that an oxidative challenge is involved in the 2rid rather than the
1st stage of skin tumor promotion: treatments with butylated hydroxyanisole (BHA), etTH + GSH, or a SOD
analogue inhibit both the ODC-inducing and complete
tumor-promoting activities of TPA but fail to inhibit
skin tumor promotion when applied in combination
with TPA in the 1st stage. 1,18,169In mouse skin, the
free radical-generating peroxides have been shown to
induce dark basal cells, a characteristic of complete
and stage 1 tumor promoters. 56,13 In SENCAR mice,
retinoic acid (RA), which triggers CL and the development of dark cells, elicits stage 1 and complete tumor-promoting activities. 226 Since the luminescence
response is believed to be due to 02 free radical generation, the data suggest that the ability of RA to promote tumors and induce dark basal keratinocytes may
be due to initial oxidative reaction at the cell membrane.
It is not known whether the increased level of peroxidation in mouse epidermis contributes significantly
to the induction of DNA and chromosome damage during skin tumor promotion and progression and if it
would be possible to prevent TPA-induced genetic lesions by boosting the natural antioxidant protective
systems of the epidermal cells. Since tumor promoters
are reactive 02 generators whose action appears to be
mediated to a certain degree by free radical production,
peroxidation and DNA strand break, 71-73.75,81.166.227-23it
is important to establish whether H202-mediated oxidation of macromolecules is accompanied by DNAdamaging events associated largely with certain stages
of tumor promotion or progression. Sister chromatid
exchanges 76-8 may be implicated in the partially irreversible I st stage of promotion. Moreover, the stage
1 tumor-promoting activity of H202 may be linked to
its ability to induce DNA lesions leading to chromosome-type as well as chromatid-type aberrations. TM
Therefore, it is fundamental to assess whether the different potencies of various compounds during tumor
392
J.-P. PERCHELLETand E. M. PERCHELLET
initiation, stage 1 and 2 promotion, and progression
could be explained on the basis of different levels of
peroxidation causing different levels of DNA damage
(Fig. 3).
Free radicals in tumor progression
When applied to the skin of Pa-bearing mice, the
free radical generators BPx and H,O2 are more potent
than TPA in stimulating the malignant progression of
skin tumorsd 3'94 It is not known whether chemically unrelated compounds such as TPA, chrysarobin,
DMBA, BPx, MNNG and ENU increase the epidermal
levels of peroxidation and genetic lesions in relation
with their potency in tumor progression. As pointed
out before, DMBA does not mimic the effects of TPA
and MEZ on epidermal GSH peroxidase and ODC
activities ~~ and some antioxidant inhibitors of skin
tumor promotion by TPA and MEZ fail to inhibit
DMBA-induced ODC activity and carcinogenesis
by a single large dose or by repeated small doses of
DMBA.~.~ t0o.232However, in our preliminary studies,
DMBA appeared at least as potent as TPA in inducing
hydroperoxide accumulation in the epidermal system. 17lTj In contrast to TPA, the effects of both BPx
and DMBA on mouse skin are characterized by direct
production of single strand breaks in DNA, induction
of a high Ca:Pa ratio and resistance to inhibition by
RA, suggesting that the promoting component of BPx
may resemble more the promoting component of
DMBA carcinogenesis than that of TPA. 233 Moreover,
strains of mice refractory to promotion by phorbol esters in two-stage initiation-promotion protocols respond to promotion by BPx and to complete skin
carcinogenesis protocols.
The induction of single strand breaks by phorbol
esters in vitro may be related to the induction of terminal differentiation. 224Therefore, phorbol ester tumor
promoters would induce DNA strand breaks and accelerate terminal differentiation in normal non-initiated
basal epidermal cells but not in the initiated progenitor
cells resistant to phorbol ester-mediated DNA strand
breaks and signals of terminal differentiationf133 To
explain the mechanism of tumor promotion by BPx, it
has been postulated that this free radical generator
might induce extensive DNA strand breaks and cytotoxic effects in normal epidermal cells and, therefore,
favor indirectly the clonal expansion of the initiated
epidermal cells that are more resistant to BPx-induced
genetic lesions and cytotoxicity. Furthermore, the initiated or benign neoplastic keratinocytes sustaining
and surviving limited DNA damage due to their relative
resistance to the potent effects of BPx, MNNG, or
ENU, might accumulate sufficient additional genetic
lesions to progress towards malignancy. The oxidative
challenge caused by TPA in the epidermis may not be
sufficient to cause such malignant conversion in preneoplastic or neoplastic keratinocytes resistant to TPAinduced DNA strand breaks.
THE EFFECTS OF ANTIOXIDANTS ON MULTISTAGE
SKIN CARCINOGENESIS
The anticarcinogenic activity of antioxidants in various tumor systems has been reviewed. 234-237 With a
few exceptions, most antioxidant treatments tested inhibit the multistage process of skin carcinogenesis
(Table 4). The process of anticarcinogenesis by these
compounds remains obscure. The mechanisms of antioxidant protection elicited by different classes of inhibitors, such as free radical scavengers, thiol delivery
systems, compounds enhancing or mimicking enzymic
activities involved in detoxification, retinoids and inhibitors of arachidonic acid metabolism, are varied and
likely to alter in a different manner and to a different
degree the effects of different categories of skin carcinogens and tumor promoters.
Antioxidants in tumor initiation and
complete carcinogenesis
The mechanisms by which antioxidants may prevent
the generation of carcinogenic compounds, block their
interaction with critical target sites in epidermal cells
and/or suppress the neoplastic process elicited by carcinogenic agents have not been clearly elucidated. 235
During initiation or complete carcinogenesis by a single large dose or repeated small doses of a carcinogen,
antioxidants may alter the enzymic activities involved
in metabolic activation, degradation and detoxification
of the PAHs and/or scavenge free radical species directly or through the enhancement of the host defense
systems. Modifying the metabolism of PAH carcinogens is complicated in that the microsomal monooxygenase system can both activate and detoxify those
compounds. It is postulated that antioxidants exert
chemoprotective effects against neoplasia in laboratory
animals largely through selective induction of phase II
detoxification pathways which facilitate the enzymic
activation and clearance of activated metabolites
through conjugation reactionsf175 In addition to the
inhibition of the oxidative metabolic activation of
procarcinogens to ultimate electrophiles, the data
reviewed in Table 4 suggest that various reducing
agents and electron scavengers can inhibit the processes of skin carcinogenesis and tumor initiation by
trapping the reactive electrophilic ultimate forms of
chemical carcinogens and the free radicals generated
during skin irradiation, thereby preventing their mu-
Table 4. Effects of Antioxidants on Multistage Skin Carcinogenesis*
Treatments (Mode of
Administration)t
Initiation
{ DMBA 238-24
IvDMBA 239"240
Ellagic acid (top)
Quercetin (top)
Garlic oil (top)
Ajoene (top)
Onion oil (top)
Propenyl sulfide (top)
Indomethacin (top)
Flurbiprofen (top)
{ BP, BP-diol-epoxide 2~s
Flurbiprofcn + arachidonic acid (top)
Phenidone (top)
ETYA (top)
ETYA + arachidonic acid (top)
Lipoxygenase inhibitor AA861 (top)
3,4,2' ,4'-Tetrahydroxychalcone (top)
RA (top; orally)
{ MC244~
~, BP 245
~ DMBA 238"24
{ DMBA 239
{ DMBA 239
~, DMBA247; - - O - - D M B A 99
{ DMBA
$ BP 2s
BP, ---O--DMBA TM
{BP,
~,TPA 99,16s
,~TPA 242
{ CRO 241
,LTPA 1~'2'~2
{ TPA 100
{ TPA 183
~,TPA; ~, BPx
ENU/TPA; $ MNNG/TPA
~,TPA 249
TPA TM
$ TPA z52
{ TPA TM
~,TPA 252
{ TPA253'254; 1' TPA 255
T TPA2S5
T TP A252
1"TPA 252
$ TPA 48
{ TPA 48
~ BP TM
{ BP TM
{ TPA 256
{ TPA z56
~,TPAg8.257; { CRO 258
Anthralin 259
{ TPA98257; { CRO 26
Anthralin 259
{ TPAZ61; 1' TPA26111
--4)---DMBA z61
Initiation
Na2SeO3 (i.p.) + aTH (top)
CuDIPS (top)
GSH (i.p.) + aTH (top)
DDTC (i. p. )
Garlic oil (top)
Onion oil (top)
lndomethacin (top)
RA (top)
13-cis-RA (top)
Progression
B p----diol,---O---D MB A ~54
~, BP, BP---dioP s4
RA analogs (retinoids) (top; orally; i.p.)
DMSO (top)
Complete Promotion
~, CRO238'241:~; { TPA nX'-242
TPA 243; - - O - - C R O 238
~, TPA 243
{ CRO TM
TPA 2~; --O---TPA 24s
~, CRO 238,241
{ CRO23~; ~, TPA lc~/
TPA lc~j
{ TPA 1
TPA lc
aTH (top)
ASC (top)
ASC analogs (top)
aTH + ASC + BHT + GSH (diet)
Se (dw)
Na2Se (top; diet)
Na2SeO3 (diet; i.p.)
Na2SeO3 + GSH (i.p.)
Na2SeO3 (i.p.) + aTH (top)
Na2SeO3 + GSH (i.p.) + aTH (top)
BHA (top)
BHT (top)
CuDIPS (top)
Cys (i.p.)
Cysteamidc (top)
GSH (i.p.)
GSH (i.p.) + ctTH (top)
DDTC (i.p.)
Two-Stage Promotion
Stage 1
T TPAm
--O---TPA 169
- - O - - T P A 1~
J, TPA 183
{ TPA
{ TPA
T TPA48
{ TPA262; - - O - - T P A ~69
{ CRO 25~
{ CRO 26
Stage 2
{ MEZm
{ MEZ I~
~ MEZ 183
{ MEZ
{ MEZ
~, MEZ 262
~ TPA 263
Complete Carcinogenesis#
aTH (top; orally)
ASC (diet)
aTH + ASC + BHT + GSH (diet)
Na2Se (top; diet)
Na2SeO3 (diet; dw)
Na2SeO3 (i.p.) + ctTH (top)
CuDIPS (top)
Cysteamide (top)
GSH (i.p.) + aTH (top)
ODTC (i.p.)
Ellagic acid (top; dw)
Garlic oil (top)
Onion oil (top; top + dw)
RA (top; i.p.)
13-cis-RA (orally)
IS-carotene (top)
DMSO (top)
MC (rsd)238; $ DMBA (rsd) 2~,265.266.*
{ UV-light (rsd) 267
{ UV-light (rsd) 22.26s
{ MC (rsd); ~ BP (rsd) 23s
BP (rsd)238; ,~ UV-light (rsd) 269
----<N-DMBA (sld), 1' DMBA (rsd) 1
DMBA (sld), ~ DMBA (rsd) 99
], MC (rsd) 238
--O---DMBA (sld), 1' DMBA (rsd) m
DMBA (sld), ~, DMBA (rsd)
MC (rsd) 270'271
,~ DMBA (sld)
~, DMBA (rsd) 272.*
---O---DMBA (sld), -4)---DMBA (rsd) 98
- - O - - M C (rsd), 1' DMBA (rsd), I' BP (rsd) 8
{ DMBA (rsd) 273~.274"*
J, M e (rsd) 238
'~ BP (rsd) 261
*Enhancing effect ( I' ); Inhibitory effect ( $ ); No significant effect (--O---)
tTreatments administered by topical application to the skin (top), by intraperitoneal injection (i.p.), in drinking water (dw), orally or in the diet.
~tCRO, croton oil; MC, 3-methylcholanthrene
Perchellet, J. P. unpublished data.
IlTopical application to the skin but at a site remote from initiation and TPA treatments.
Belman, S.; Perchellet, J. P. unpublished data.
#Treatment with either a single large dose (sld) or repeated small dose (rsd) of a carcinogen.
**Hamster buccal pouch mucosa carcinogenesis.
ttHamster lingual mucosa carcinogenesis.
394
J.-P. PERCHELLETand E. M. PERCHELLET
tagenic interaction with epidermal DNA. The reducing
agents, therefore, may act as nucleophiles competing
with nucleophilic sites on DNA for the created radicals.
As demonstrated during the photocarcinogenic
response of mouse skin, free radical reactions, specifically chain propagation of epidermal lipid peroxidation, may play a major role in carcinogenesis. 22 Modulation of the level of epidermal lipid peroxidation and
skin carcinogenesis appears possible through treatments
that alter the polyunsaturated lipid:antioxidant ratio.
A major function of oLTHis to inhibit both enzymic and
nonenzymic lipid peroxidation and prevent the spread
of damaging lipid radicals through membranes, o~TH
may also prevent the formation of proximal carcinogens.239 In the standard model for hamster buccal pouch
carcinogenesis, repeated applications of I 0 mg of aTH
on alternate days to those when 0.5% DMBA
solutions are painted thrice a week can not only inhibit
DMBA carcinogenesis but may entirely prevent tumor
development when less potent 0.1% DMBA solutions
a r e u s e d . 266 The important intracellular reducing agent
ASC has been suggested to be a protective agent against
development of cancer. However, the controversy surrounding the efficacy of this agent on cancer chemotherapy comes from the fact that, under certain
conditions, the free radicals generated during the oxidation of ASC may mediate DNA strand scissions and
potentiate the mutagenic effects of carcinogens. 276 In
vitro, ASC exerts opposite effects at different concentrations: at concentrations < 1 raM, ASC has a prooxidant effect on lipid peroxidation, whereas at concentrations >1 mM it fails to promote peroxidation and
generally functions as an antioxidant. 277
The pronounced chemoprotective role, as well as
the adverse effects, of the synthetic phenolic antioxidants butylated hydroxytoluene (BHT) and BHA
commonly used in the food industry to scavenge 02containing radicals and prevent the oxidative deterioration of many food products has been reviewed thoroughly. 237 Electron spin resonance studies in vitro
show that BHT scavenges the .OH and .MNNG formed
by the interaction of H202 with MNNG by reacting
with these labile free radicals and forming a stable
phenoxyl free radical of BHT. 27~The scavenging effect
of BHT on .OH, therefore, may be related to its effect
in lowering carcinogenesis. The chemoprotective action of BHA, BHT and ethoxyquin requires intact cells
to be operational and has been associated with an indirect effect on the epidermal metabolizing system
which leads to a decrease in covalent binding of carcinogens to D N A . 239'279 The protective effects of these
antioxidants may be accounted for, at least in part, by
their ability to elevate the GSH S-transferases. 28 Preliminary results indicating that the inhibitors of PG
endoperoxide synthetase inhibit mouse skin initiation
by BP and BP-7,8-diol but not by DMBA suggest the
possible involvement of PG biosynthesis in BP and
BP-7,8-diol tumor initiation, perhaps by a cooxygenation mechanism.154 However, BHA, an inhibitor of
LO2"-dependent metabolism, but not the modifiers of
PG H synthetase activity, significantly inhibits the
LO2.-dependent epoxidation, which is the major pathway of BP-7,8-diol oxidation in skin cells prepared
from animals that are not treated with inducers of
mixed-function oxidase. ~s~
Since the SOD biomimetic agent CuDIPS is a potent
inhibitor of initiation of SENCAR skins 247 and inhibits
complete carcinogenesis in CD- 1 mice by a single large
dose or multiple small doses of DMBA, 99 it is possible
that, in contrast to SENCAR mice, the requirement for
a high dose of DMBA for initiation of CD- 1 skins and
the lower CuDIPS : DMBA ratio applied on CD- 1 skins
might have masked the anti-initiating activity of
CuDIPS in these mice. 99 The covalent binding of 3HDMBA to epidermal DNA is remarkably reduced by
CuDIPS pretreatment, suggesting that the anti-carcinogenic properties of this compound may reflect a perturbation in O2--dependent metabolic activation of
DMBA. 99 As an alternative explanation, copper complexes could interact with the microsomal electron
transport system and inhibit mixed-function oxidation
reactions through mechanisms independent of their
SOD-like chemical reactivity. This hypothesis is substantiated by the observation that CuDIPS and CuSO4,
but not bovine liver SOD, inhibit BP-dependent mutagenesis and cytochrome P450 reductase activity. The
in vitro antimutagenic activity of CuDIPS as scored in
the Ames assay, therefore, seems independent of its
salicylate structure and is mediated through a copperdependent but non-SOD-associated inhibition of P450
reductase activity. 2~
Thiols, sulfides and synthetic sulfur-rich chemicals
have been shown to inhibit successfully the effects of
several carcinogens, presumably by blocking their metabolic activation and/or by inducing enzyme systems
known to aid in their detoxification. The inhibitory
effects of L-cysteine (Cys) on the mutagenic activities
of several carcinogens have been described. 282 In vitro
treatments with GSH alone and GSH + cytosol or
purified GSH S-transferases are active in inhibiting
DNA binding of reactive metabolites of BP z83 as well
as the cytotoxicity and mutagenicity of these carcinogens in mammalian cells. 284 The dithiolthiones may
inhibit tumor development by increasing cellular thiol
levels and inducing enzymes concerned with the maintenance of GSH pools as well as enzymes important
to electrophile detoxification. 279 Dially sulfide, the
thioether that occurs naturally in garlic, can modify
Antioxidants and skin carcinogenesis
hepatic mixed-function oxidase and stimulate hepatic
sulfate conjugation reactions leading to eventual detoxification and elimination of the electrophile mutagenic forms of the carcinogens. 285 In addition, the
endogenous thioredoxin/thioredoxin reductase system,
a thioenzyme which reduces radicals at the surface of
the skin, may play an important role in preventing free
radical-induced cell damage during skin carcinogenesis.286 Moreover, various intracellular thiols may protect DNA-modifying enzymes such as DNA methylase
from carcinogen damage. 287
The antioxidant effects of disulfiram and its reduction product, diethyldithiocarbamate (DDTC), have
been described. 234.288Both compounds inhibit chemical
carcinogenesis in the gastrointestinal tract. Because of
the chelating properties of its sulfhydryl moieties,
DDTC is a rather nonspecific inhibitor of several
metal-containing enzymes, including SOD. 28~ Although the inhibition of P450-dependent microsomal
enzyme activities may be involved, the GSH peroxidase-like and free radical-quenching activities of
DDTC are likely to explain some of the remarkable
inhibitory effects elicited by this compound during
complete and multistage skin carcinogenesis. ~82j83 It
has been suggested that CS2, a metabolite of disulfiram, may be the chemical species responsible for the
carcinogen-inhibiting effects brought about by disulfiram and DDTC. TM A recent study indicates that
DDTC protects mouse tissues from hyperoxic injury. 29
The data suggest that the mechanism of this antioxidative property is indirect and involves the delayed
increase in the GSH enzyme levels following DDTC
injection. 29~ It has been postulated that DDTC is effective in protecting against lipid peroxidation of microsomal membranes in the nM range because of its
hydrophobicity, whereas the effects of other hydrophilic thiol-containing molecules such as GSH and cysteamine are observed in the mM range only. 288
Mixed results have been published concerning the
potential anticarcinogenicity and/or mutagenicity of
G S H . 292-294 A model of an indirect mechanism of GSH
mutagenesis involving ROS is described in which
cleavage of GSH by 2t-glutamyltranspeptidase, followed by auto-oxidation of the resulting cysteinylglycine may produce free radicals, which lead to the
penultimate mutagen H202 .295 The role of Se in tumorigenesis has been extensively reviewed 296 and its
possible action on both the initiating and promoting
components of chemical carcinogenesis has been disc u s s e d . 297 The anticarcinogenic properties of Se may
be attributed, at least partially, to its ability to maintain
the integrity of the Se-dependent enzyme GSH peroxidase, which detoxifies peroxides. The synergistic
effects of o~TH and Se in the chemoprevention of car-
395
cinogenesis have been described. 298,299Our recent finding that Na2SeO3 + a T H and GSH + aTH, the
combined treatments that inhibit complete and stage 2
tumor promotion in the multistage protocols, fail to
inhibit the carcinogenicity of a single large dose of
DMBA and even enhance the induction of skin tumors
by repeated applications of subcarcinogenic doses of
DMBA is intriguing. ~ The discrepancies between
some of the effects of aTH, Se and GSH on skin carcinogenesis presented in Table 4 have been discussed
previously. 100
The antineoplastic activity of ellagic acid has been
reviewed. 3 The inhibition of skin tumor initiation and
carcinogenesis by ellagic acid 248,27,271may result from
decreased metabolic activation and increased conjugation reactions, as indicated by the findings that ellagic acid inhibits epidermal AHH activity, induces
epidermal GSH S-transferase activities, and decreases
the formation and covalent binding of ultimate carcinogens to epidermal DNA. 271'31'32 Ellagic acid binds
to DNA and it has been suggested that this binding
may be a mechanism by which ellagic acid inhibits
mutagenesis and carcinogenesis. 33 Apparently, ellagic
acid can also scavenge the ultimate carcinogenic
form of BP. 34 Surprisingly, the antitumor-promoting
activity of this interesting antioxidant has not been
studied.
Vitamin A is required for the maintenance and function of differentiation of epithelial cells. Vitamin A
and its analogs (retinoids) are capable of inhibiting the
development of Ca induced by chemical carcinogens
in various organs. The role of retinoids in the modification of multistage skin carcinogenesis is well documented, 8"9~'23z'25~'262'263"35 The RA-binding protein
may be involved in the expression of biological and
antitumorigenic activities of the retinoids. Since the
retinoids have been demonstrated to stimulate cellmediated immunity, there is some suggestion that retinoids may also retard carcinogenesis by serving to
enhance the organism's immune response. 36 The discrepancy between some of the effects of the retinoids
on complete skin carcinogenesis may be related to their
variable chemical reactivity toward free radicals. Incubation of 13-cis-RA with peroxidase and hydroperoxides or with LOz--generating systems leads to rapid
02 uptake, retinoid oxidation and formation of oxygenated products. ~J4The conflicting reports concerning
the effects of retinoids on complete and multistage skin
carcinogenesis, therefore, may be explained by the
fact that the retinoids are not only efficient at trapping
reactive oxidants, thereby lowering the steady-state
oxidant concentration, but that, under certain conditions, they can actually enhance LO2" and LO. formation. 114
396
J.-P. PERCHELLETand E. M PERCHELLET
The fact that our understanding of the mechanism
of tumor promotion is itself still evolving increases the
difficulty of trying to explain how antioxidants may
be affecting this process. Reviewing the effects of the
numerous modifiers of tumor promotion is a monumental task but a survey of the literature reveals clearly
the relevance of ROS to the mechanism of tumor promotion. Basically, these findings can be classified in
three categories.
various cell systems. 169,310,314,316.317For example, retinal
has been shown to decrease PKC induction and H202
formation in TPA-treated neutrophils. 2~3 Several adrenal steroids shown to inhibit skin tumor promotion
by TPA also inhibit the ability of TPA to stimulate
02- production in leukocytes. 3~8.3~9 Furthermore, the
Ca 2+ channel and calmodulin antagonists shown to
inhibit PKC induction by TPA are also capable of inhibiting the CL response in epidermal cells 3t and the
production of 02- and H202 in leukocytes stimulated
by TPA. 21~'-~16'217
Antioxidative effects of anti-tumor promoters. Various
agents which decrease the biological and biochemical
events linked to skin tumor promotion also inhibit the
ability of TPA to induce the generation of ROS. For
instance, a protease inhibitor such as tosyl phenylalanine chloromethyl ketone is effective against complete and stage 1 skin tumor promotion 59'37 and a
number of protease inhibitors from various sources,
specially those active against chymotrypsin, block the
production of 02 ~ and H202 and the CL response by
TPA-activated PMN leukocytes. 3~ 311 However, the
SOD-inhibitory activity of the protease inhibitors may
be independent from their anti-proteolygic activity. 3~2
Not surprisingly, CuDIPS inhibits the TPA-induced
CL response in mouse epidermal cells 313 and the ability of TPA-stimulated PMN leukocytes to generate
oxidants ~69 and enhance the metabolic activation of
PAH carcinogens. ~52 The O j response and toxicity of
TPA-stimulated leukocytes or the CL observed in TPAtreated epidermal cells are inhibited to various degrees
by SOD, 314 quercetin, J69 7,8-benzoflavone and ASC. 31
Although they do not react directly with 02- the phenolic antioxidant BHA 3~ and several of its analogs, 3~5
which inhibit TPA-stimulated O2- formation and CL
in PMN leukocytes or epidermal cells, also inhibit
ASC-initiated lipid peroxidation in relation with their
ability to inhibit TPA-induced ODC activity in mouse
epidermis. The results imply that BHA and its lipophilic analogs may scavenge free-radical derivatives
of 02: more directly involved in the promotional stage
of carcinogenesis. 3~5 In addition, the specific lipoxygenase inhibitors and agents with dual cyclooxygenaselipoxygenase inhibitory activities shown to inhibit skin
tumor promotion in different strains of mice also block
the TPA-induced 02 ~ release from leukocytes ~6~ and
CL response in mouse epidermal cells, 313 whereas the
specific cyclooxygenase inhibitors are ineffective.
These data suggest that at least a major part of the
TPA-induced CL response is due to the increased metabolism of arachidonic acid, most probably by the
lipoxygenases. 3~3 Moreover, another class of anti-promoting agents, the retinoids, also inhibits the oxidative
challenge caused by TPA, MEZ, or teleocidin B in
Antitumor-promoting effects of antioxidants. The direct quenching reactivity of cellular antioxidants
against specific free radicals has been reviewed. 32 The
various antioxidant treatments, which decrease the oxidative challenge caused by TPA, also inhibit the other
biochemical events linked to the skin tumor-promoting
activity of this compound. While cupric sulfate and
diisopropylsalycylic acid are ineffective, t6~ SOD,
CuDIPS, or other copper complexes with potent SOD
mimetic activities inhibit the ability of TPA to induce
ODC activityfl ~'t~7~6~ DNA synthesis and mitosisfl 2~
sister chromatid exchanges, chromosomal aberration
and polyploidization 72,79 and the promotion of neoplastic transformation in vitro 322 324 and to decrease the
13-adrenergic responsiveness of lymphocytes. 325In contrast, CuD1PS does not inhibit DMBA-induced ODC
activity, suggesting that the mechanism by which
DMBA induces this enzymic marker of stage 2 tumor
promotion is different from that of TPA. 99 Most of the
effects of TPA described above are also inhibited by
CAT and various antioxidants and free radical scavengers, including BHA, BHT, mannitol, a T H , disulfiram, selenous acid and the synthetic lipophilic
derivative of ASC, ascorbyl palmitate, j67,24:~'321-329 in
addition, a T H inhibits TPA-stimulated deacylation of
cellular lipids, PG production and altered cell morphology in vitro. 33 Interestingly, the inhibitor of tumor
promotion quercetin inhibits epidermal lipoxygenase
activity and the induction of ODC activity but not the
stimulatory effect of TPA on DNA synthesis. 24~
The complex effects of the inhibitors of arachidonic
acid metabolism on PG synthesis, ODC induction,
DNA synthesis, and skin tumor promotion in different
strains of mice treated with TPA have been excellently
reviewed. 4~'253 Both the cyclooxygenase/endoperoxidase pathway of PG synthesis and the lipoxygenase
pathway of hydroperoxy (HPETE)- and hydroxy-eicosatetraenoic (HETE) acid formation play a mediatory
role in TPA-induced inflammation, ODC activity,
DNA synthesis, cell differentiation, in vitro promotion
of neoplastic transformation and skin tumor formation. 254"255"323"329"331"332 Specific lipoxygenase inhibitors
Antioxidants in tumor promotion
Antioxidants and skin carcinogenesis
and agents with dual cyclooxygenase-lipoxygenase
inhibitory activities consistently antagonize the tumorpromoting effects of TPA. In contrast, the antitumorpromoting activities of specific cyclooxygenase inhibitors are variable. 254.255 In certain strains of mice and
under certain conditions, the cyclooxygenase inhibitors
indomethacin and flurbiprofen may shunt arachidonic
acid metabolism into the alternate lipoxygenase pathway and enhance the tumor-promoting activity of TPA,
suggesting that the HPETEs and other products of the
lipoxygenase pathway play an important role in the
mechanism of ODC induction by TPA and may be more
intimately involved in promotion than the PGs. 48.332
The generation of ROS and the induction of the lipoxygenase pathway producing reactive oxidized metabolites of arachidonic acid, therefore, appears to be
essential to the molecular mechanism of skin tumor
promotion by TPA. Specific lipoxygenase inhibitors
lacking PKC inhibitory effects strongly suppress TPAinduced ODC activity and skin tumor formation. 256
The effectiveness of RA and 2 1 retinoids as inhibitors of TPA -35328or anthralin-induced ODC activity 259
in mouse epidermis in vivo has been demonstrated. In
vitro, RA or its analogs also inhibit the enhancing effects of TPA on DNA synthesis, mitosis, and the
transformation of 3-methylcholanthrene(MC)-treated
c e l l s . 321'326 Cutaneous RA pretreatments inhibit by almost 100% TPA-increased epidermal GSSG-R activity, an event postulated to decontrol the availability of
deoxyribonucleotides for DNA biosynthesis. 333 However, the potent inhibitor of ODC induction and skin
tumor promotion by TPA, RA, fails to inhibit and,
under some experimental conditions, significantly enhances ODC induction and tumor formation by
DMBA. 87-Bromomethylbenz[a] anthracene (BrMBA),
a structural analogue of DMBA, is a weak mouse skin
tumor-initiating agent and a weak complete carcinogen
but a good tumor promoter when applied repeatedly to
DMBA-initiated mouse skin.l3 The doses of RA and
dexamethasone which inhibit skin tumor promotion by
TPA, also inhibit epidermal ODC induction and skin
tumor promotion by BrMBA. 232 In contrast, 7,8-benzoflavone, which does not inhibit TPA-induced ODC
activity, inhibits the ODC and tumor responses to
DMBA but neither ODC induction nor tumor promotion by BrMBA. 232The discrepancy between the effects
of these various compounds on the induction of skin
tumors by different protocols might result from different levels of genetic lesions and hyperplastic, cytostatic or cytotoxic activities in the TPA-and DMBAtreated epidermis. In some cases, the inhibitory effects
that some agents exert on the propagating activities of
TPA or MEZ could be masked by equal or greater
stimulatory effects on the other stages theoretically
397
involved in complete carcinogenesis by DMBA. For
instance, RA inhibits the overall TPA-induced responses but has the ability to act as either a weak 1st
stage or complete tumor promoter in the initiationpromotion system for skin carcinogenesis in SENCAR
m i c e . 226
Our results indicate that the inhibitory effects of
Cys, GSH, and o~TH on ODC induction are proportional to their abilities to prevent the decrease in the
GSH :GSSG ratio caused by TPA and inhibit the incidence of skin tumors in the initiation-promotion prot o c o l . 242 In mouse epidermis in vivo and in vitro, the
inhibitory effects of combined treatments with Cys or
GSH, Na2SeO3 or selenocystamine and ~TH on TPAdecreased GSH peroxidase activity are additive, in
relation with their additive inhibitory effects on TPAinduced ODC activity, t,~29 A number of thiol-containing molecules that are readily transported and/or
enzymatically converted to GSH intracellularly are
more effective than GSH treatment in increasing the
intracellular thiol level of various tissues. In mouse
epidermis in vivo and in vitro, the monoethyl and monomethyl esters of GSH, N-acetyl-L-cysteine and L-2oxothiazolidine-4-carboxylate are all significantly
more effective than GSH in inhibiting the sharp decline
in the intracellular G S H : G S S G ratio, the prolonged
decrease in GSH peroxidase activity and the induction
of ODC activity caused by TPA. ~2"~s3 Moreover,
DDTC, which prevents totally the initial drop in the
G S H : G S S G ratio of TPA-treated epidermal cells and
is more potent that 16 other antioxidants in inhibiting
TPA-decreased GSH peroxidase activity, is also the
most potent thiol delivery agent to inhibit TPA-induced
epidermal ODC activity in vitro and in v i v o . 182'183 In
addition, garlic oil, onion oil and dipropenyl sulfide,
a constituent of onion oil, all inhibit to diverse degrees
the effects of TPA on the GSH-dependent detoxifying
system in relation with their abilities to inhibit TPAinduced ODC activity in mouse epidermis in vitro and
in vivo. ls~'z52 The GSH peroxidase-like activity of
garlic oil has been shown. It should be noted that these
inhibitors of skin tumor promotion also inhibit soybean
and mouse epidermal lipoxygenase activities. 251'252'334
Although DMSO may scavenge free radicals, it is
difficult to find a common explanation for the range
of effects of DMSO on experimental tumorigenesis. 261
When DMSO is used as the solvent instead of acetone,
it enhances complete skin carcinogenesis by BP, does
not alter initiation by DMBA, and inhibits skin tumor
promotion by TPA. Interestingly, DMSO applied topically to the skin before each TPA treatment inhibits
skin tumor promotion when it is administered to the
initiated back of the mouse but increases skin tumor
promotion when it is applied on the non-initiated ab-
398
J.-P. PERCHELLETand E. M. PERCHELLET
domen. 26t Without modifying the initiating event,
DMSO could enhance complete skin carcinogenesis by
increasing the penetration, metabolism and DNA-damaging effects of carcinogenic doses of PAHs. Perhaps,
DMSO alters specifically the promoting components
of carcinogenesis. That the effects of DMSO on skin
tumor promotion depend on the site of its administration in relation to TPA treatment suggests that the intact
DMSO molecules affecting the initiated epidermal
cells following direct penetration through the skin and
the DMSO metabolites affecting the same cells indirectly through the circulation exert opposite effects on
the mechanism of TPA promotion. 26~
Tumor-promoting effects of pro-oxidants. The treatments that worsen the oxidative challenge caused by
TPA enhance the events linked to skin tumor promotion
by TPA. For instance, the promotional activity of
methyl ethyl ketone peroxide, a potent lipid-peroxidizing agent, is potentiated by DEM which is known
to deplete intracellular GSH, suggesting that lipid peroxidation may be important in skin tumor promotion. 335
Chronic treatment of skin Pa with the GSH-depleting
agent DEM also enhances markedly their malignant
conversion to C a . 336 Similarly, the treatments with
NaN3 plus NADPH, G / G O or X/XO that enhance
the hydroperoxide response to TPA in our recent
experiments 17.j7~ also increase, although to a lesser
degree, TPA-induced epidermal ODC activity in mouse
skin explants. Moreover, the H2Oz-generating enzyme
GO mimics the inhibitory effects of several liver tumor
promoters on gap junctional intercellular communication, an event which is inhibited by several antioxidants including SOD and otTH. 337 In mouse epidermis
in vivo, topical adriamycin (ADR, doxorubicin) treatments enhance ODC induction and skin tumor promotion by TPA. In epidermal cells incubated in the
presence of ADR, the tumor promoter causes a greater
sequential rapid increase and prolonged decrease in
GSH peroxidase activity accompanied by a greater decrease in the GSH :GSSG ratio. 179 Since free radical
generation and lipid peroxidation may be associated
with ADR toxicity, these data suggest that the enhancement of the ODC-inducing and tumor-promoting
activities of TPA by ADR may be the result of an
increased oxidative challenge altering to a greater degree than TPA alone the GSH-dependent antioxidant
protective system of the epidermal cells.
CONCLUSION
The review of the inhibitory effects of the antioxidants in the mouse skin tumor system confirms the
important role of 02 metabolites in the multistage pro-
cess of carcinogenesis. Although the anti-carcinogenic
and/or antitumor-promoting activities of some of these
compounds may be caused to a certain degree by mechanisms independent from their antioxidant properties,
it is likely that their effectiveness as inhibitors of tumor
formation is due largely to their ability to scavenge,
reduce and detoxify, directly or indirectly and through
spontaneous or enzyme-catalyzed reactions, the various unstable electrophile intermediates affecting the
epidermal cells during the sequential phases of skin
carcinogenesis. The results of these animal tumor experiments suggest that, if increased levels of peroxidation coupled with decreased antioxidant protection
play a major role during the long and multistage process of neoplasia, the antineoplastic activity of the
natural SOD, CAT and GSH-dependent detoxifying
systems might be preserved and ameliorated through
chemotherapeutic intervention and the use of antioxidant systems that complement each other. For instance,
the mechanisms of antioxidant protection by the GSHdependent detoxifying system and ~xTH are independent, complementary, and protect each other. Treatments or diets that would enhance on a life-long basis
the natural antioxidant protection of the organism,
therefore, might be valuable in cancer chemoprevention by decreasing the risk, increasing the threshold
and delaying the advent of tumor initiation. Our research suggests that free radical scavengers, GSH
level-raising agents, Se-containing compounds and
thiol delivery systems that prevent the decline in the
GSH : GSSG ratio and maintain GSH peroxidase activity stimulated for extended periods of time may facilitate a more complete destruction of peroxides during
TPA treatment, in relation with their effectiveness as
inhibitors of ODC induction, hyperplasia and skin tumor promotion and progression. The ultimate goal is
to determine whether the protective effects of these
antioxidant treatments are sufficient to block the
growth or induce the regression of skin tumors that
have already developed. This information is of importance to assess the potential use of antioxidants in
the management of certain human neoplasms resistant
to conventional therapy.
Acknowledgements--The authors gratefully acknowledge the financial support of the NIH (Grant CA-40083 awarded by the National
Cancer Institute, Department of Health and Human Services), the
American Cancer Society (Grant BC-600), the Wesley Foundation
of Wichita (Wesley Scholar Program: Molecular Biology and Cell
Growth Regulation), and the Center for Basic Cancer Research,
Kansas State University
REFERENCES
1. Moolgavkar, S. H.; Knudson, A. G. Jr. Mutation and cancer:
a model for human carcinogenesis. J. Natl. Cancer Inst.
66:1037-1052; 1981.
Antioxidants and skin carcinogenesis
2. Nowell, P. C. The clonal evolution of tumor cell populations.
Science 194:23-28; 1976.
3. Pitot, H. C. Fundamentals of oncology. New York: Marcel
Dekker; 1986.
4. Phillips, R. A. The genetic basis of cancer. In: Tannock, 1.
F.; Hill, R. P., eds. The basic science ofoncology. Elmsford,
NY: Pergamon Press; 1987:24-51.
5. Schabel, F. J. Jr.; Simpson-Herren, L. Tumor growth kinetics
and drug treatment of cancer. In: Kuemmerle, H. P., ed. Clinical chemotherapy, Vol. 3: Antineoplastic chemotherapy. New
York: Thieme-Stratton; 1984:16-34.
6. Tannock, 1. F. Tumor growth and cell kinetics. In: Tannock,
1. F.; Hill, R. P., eds. The basic science ofoncology. Elmsford,
NY: Pergamon Press; 1987:140-159.
7. DeVita, V. T. Jr. Principles of chemotherapy. In: DeVita, V.
T. Jr.; Hellman, S.; Rosenberg, S. A., eds. Cancer--Principles and practice of oncology. Philadelphia: J. B. Lippincott
Company; 1985:257-285.
8. Verma, A. K.; Conrad, E. A.; 13outwell, R. K. Differential
effects of retinoic acid and 7,8-benzoflavone on the induction
of mouse skin tumors by the complete carcinogenesis process
and by the initiation-promotion regimen. Cancer Res. 42:
3519-3525; 1982.
9. Fisher, B.; Fisher, E. R. Experimental evidence in support of
the dormant tumor cell. Science 130:918-919: 1959.
10. Steel, G. G. Growth kinetics oftumours. Oxford: Oxford University Press; 1977.
I 1. Pardee, A. B. Principles of cancer biology: biochemistry and
cell biology. In: DeVita, V. T. Jr.; Hellman, S.; Rosenberg,
S. A., eds. Cancer--Principles and practice ofoneology. Philadelphia: J. B. Lippincott Company; 1985:3-22.
12. Mottram, J. C. A developing factor in experimental blastogenesis. J. Pathol. Bacteriol. 56:181-187; 1944.
13. Berenblum, 1.; Shubik, P. The role of croton oil applications,
associated with a single painting of a carcinogen, in turnout
induction of the mouse's skin. Br. J. Cancer 1:379-382; 1947.
14. Boutwell, R. K. Some biological aspects of skin carcinogenesis. Progr. Exp. Tumor Res. 4:207-250; 1964.
15. Boutwell, R. K. The function and mechanism of promoters of
carcinogenesis. CRC Crit. Rev. Toxicol. 2:419-443; 1974.
16. Bader. G. M.; Cook, J. W.; Hewett, C. L.; Kennaway, E. L.;
Kennaway, N. M.; Martin, R. H. The production of cancer
by pure hydrocarbons. VI. Proc. R. Soc. Lond. (Biol.) 131:
170-182; 1942.
17. Hecker, E. Isolation and characterization of the cocarcinogenic
principles from croton oil. In: Busch, H., ed. Methods in cancer research. Vol. 6. New York: Academic Press; 1971:439484.
18. Van Duuren, B. L.; Orris, L. The tumor enhancing principles
of croton tiglium L. Cancer Res. 25:1871-1875; 1965.
19. DiGiovanni, J.; Slaga, T. J.; Boutwell, R. K. Comparison of
the tumor initiating activity of 7,12-dimethylbenz[a]anthracene
and benzo[a]pyrene in female SENCAR and CD-1 mice. Carcinogenesis 1:381-389; 1980.
20. Verma, A. K.; Boutwell, R. K. Effects of dose and duration
of treatment with the tumor-promoting agent, 12-0-tetradecanoylphorbol-13-acetate on mouse skin carcinogenesis. Carcinogenesis 1:271-276; 1980.
21. Terracini, B.; Shubik, P.; Della Porta, G. A study of skin
carcinogenesis in the mouse with single applications of 9,10dimethyl-l,2-benzanthracene at different dosages. Cancer
Res. 20:1538-1542; 1960.
22. Turusov, V.; Day, N.; Andrianov, L.; Jain, D. Influence of
dose on skin tumors induced in mice by single application of
7,12-dimethylbenz-[a]anthracene. J. Natl. Cancer Inst. 47:
105-111; 1971.
23. Miller, J. A.; Miller, E. C. Ultimate chemical carcinogens as
reactive mutagenic electrophiles. In: Hiatt, H. H.; Watson, J.
D.; Winsten, J. A., eds. Origin of human cancer, Book B.
New York: Cold Spring Harbor Laboratory; 1977:605-627.
24. Farber, E. Chemical carcinogenesis. A biologic perspective.
Am. J. Pathol. 106:269-296; 1982.
399
25. Brown, K.; Quintanilla, M.; Ramsden, M.; Kerr, I. B.; Young,
S.; Balmain, A. v-ras Genes from Harvey and BALB murine
sarcoma viruses can act as initiators of two-stage mouse skin
carcinogenesis. Cell 46:447-456; 1986.
26. Quintanilla, M.; Brown, K.; Ramsden, M.; Balmain, A. Carcinogen-specific mutation and amplification of Ha-ras during
mouse skin carcinogenesis. Nature 322:78-80; 1986.
27. Roop, D. R.; Lowy, D. R.; Tambourin, P. E.; Strickland, J.;
Harper, J. R.; Balaschak, M.; Spangler, E. F.; Yuspa S. H.
An activated Harvey ras oncogene produces benign tumours
on mouse epidermal tissue. Nature 323:822-824; 1986.
28. Strickland, J. E.; Greenhalgh, D. A.; Koceva-Chyla, A.; Hennings, H.; Restrepo, C.; Balaschak, M.; Yuspa, S. H. Development of murine epidermal cell lines which contain an
activated ras H" oncogene and form papillomas in skin grafts
on athymic nude mouse hosts. Cancer Res. 48:165-169; 1988.
29. Quintinilla, M.; Brown, K.; Fee, F.; Young, S.; Balmain, A.
Oncogene mutation and amplification during initiation and progression stages of mouse skin carcinogenesis. In: Colburn, N.
H.: Moses, H. L.; Stanbridge, E. J., eds. Growth factors,
tumor promoters, and cancer genes. New York: Alan R. Liss;
1988:257-266.
30. Bowden, G. T. A National Institute of Health workshop report.
Chemical carcinogenesis and the oncogenes--A Chemical Pathology Study Section workshop. Cancer Res. 45:914-918;
1985.
31. Pelling, J. C.; Ernst, S.; Strawhecker, J. M.; Johnson, J. A.;
Nairn, R. S.; Slaga, T. J. Elevated expression of Ha-ras is an
early event in two-stage skin carcinogenesis in SENCAR mice.
Carcinogenesis 7:1599-1602; 1986.
32. Colburn, N. H.; Farber, E.; Weinstein, I. B.; Diamond, L.;
Slaga, T. J. American Cancer Society workshop conference
on tumor promotion and antipromotion. Cancer Res. 47:55095513; 1987.
33. Boutwell, R. K.; Verma, A. K.; Ashendel, C. L.; Astrup, E.
Mouse skin: a useful model system for studying the mechanism
of chemical carcinogenesis. In: Hecker, E.; Kuntz, W.; Fusenig, N. E.; Marks, F.; Thielmann, H. W., eds. Carcinogenesis, Vol. 7, Cocarcinogenesis and biological effects of tumor
promoter. New York: Raven Press; 1982:1-12.
34. Berenblum, I.; Shubik, P. The persistence of latent tumor cells
induced in the mouse's skin by a single application of 9,10dimethyl-1,2-benzanthracene. Br. J. Cancer3:384-386; 1949.
35. Van Duuren, B. L.; Sivak, A.; Katz, C.; Seidman, 1.; Melchionne, S. The effect of aging and interval between primary
and secondary treatment in two-stage carcinogenesis on mouse
skin. Cancer Res. 35:502-505; 1975.
36. Yuspa, S. H.; Morgan D. L. Mouse skin cells resistant to
terminal differentiation associated with initiation of carcinogenesis. Nature 293:72-74; 1981.
37. Kawamura, H.; Strickland, J. E.; Yuspa, S. H. Association
of resistance to terminal differentiation with initiation of carcinogenesis in adult mouse epidermal cells. Cancer Res.
45:2748-2752; 1985.
38. Kilkenny, A. E.; Morgan, D.; Spangler, E. F.; Yuspa, S. H.
Correlation of initiating potency of skin carcinogens with potency to induce resistance to terminal oifferentiation in cultured
mouse keratinocytes. Cancer Res, 45:2219-2225; 1985.
39. Boutwell, R. K. Biochemical mechanism of tumor promotion.
In: Slaga, T. J.; Sivak, A.; Boutwell, R. K., editors. Carcinogenesis, Vol. 2, Mechanisms of tumor promotion and cocarcinogenesis. New York: Raven Press; 1978:~o-58.
40. Yuspa, S. H.; Hennings, H.; Saffiotti, U. Cutaneous chemical
carcinogenesis: past, present, and future. J. Invest. Dermatol.
67:199-208; 1976.
41. Weinstein, I. B.; Lee, L.-S.; Fisher, P. B.; Mufson, A.; Yamasaki, H. Action of phorbol esters in cell culture: mimicry
of transformation, altered differentiation, and effects on cell
membrane. J. Supramol. Struct. 12:195-208; 1979.
42. Blumberg, P. In vitro studies on the mode of action of the
phorbol esters, potent tumor promoters. CRC Crit. Rev. Toxicol. 8:153-197; 1980.
400
J.-P. PERCHELLETand E. M. PERCHELLET
43. Slaga, T. J. Mechanisms involved in two-stage carcinogenesis
in mouse skin. In: Slaga, T. J., ed. Mechanisms of tumor
promotion, Vol. 2, Tumor promotion and skin carcinogenesis.
Boca Raton, FL: CRC Press; 1984:1-16.
44. Yuspa, S, H. Tumor promotion in epidermal cells in culture.
In: Slaga, T. J., ed. Mechanisms of tumor promotion, Vol. 3,
Tumor promotion and carcinogenesis in vitro. Boca Raton,
FL: CRC Press; 1984:1-11.
45. Ashendel, C. L. The phorbol ester receptor: a phospholipidregulated protein kinase. Biochim. Biophys. Acta 822:219242; 1985.
46. Blumberg, P. M. protein kinase C as the receptor for the phorbol ester tumor promoters: sixth Rhoads memorial award lecture. Cancer Res. 48:1-8; 1988.
47. Mufson, R. A. The relationship of alterations in phospholipid
metabolism to the mechanism of action of phorbol ester tumor
promoters. In: Slaga, T. J., ed. Mechanisms of tumor promotion, Vol. 4, Cellular responses to tumor promoters. Boca
Raton, FL: CRC Press; 1984:109-117.
48. Fischer, S. M. The role of prostaglandins in tumor promotion.
In: Slaga, T. J., ed. Mechanisms of tumor promotion, Vol. 2,
Tumor promotion and skin carcinogenesis. Boca Raton, FL:
CRC Press; 1984:113-126.
49. Raineri, R.; Simsiman, R. C.; Boutwell, R. K. Stimulation of
the synthesis of mouse epidermal histones by tumor-promoting
agents. Cancer Res. 37:4584-4589; 1977.
50. Troll, W.; Meyn, M. S.; Rossman, T. G. Mechanisms of protease action in carcinogenesis. In: Slaga, T. J.; Sivak, A.;
Boutwell, R. K., eds. Carcinogenesis, Vol. 2, Mechanisms of
tumor promotion and cocarcinogenesis. New York: Raven
Press; 1978:301-312.
51. Troll, W. ; Wiesner, R. The role of oxygen radicals as a possible
mechanism of tumor promotion. Ann. Rev. Pharmacol. Toxicol. 25:509-529; 1985.
52. Weinstein, I. B. Growth factors, oncogenes, and multistage
carcinogenesis. J. Cell. Biochem. 33:213-224; 1987.
53. Colburn, N. H.; Smith, B. M. Genes that cooperate with tumor
promoters in transformation. J. Cell. Biochem. 34:129-142;
1987.
54. Boutwell, R. K.; O'Brien, T. G.: Verma, A. K.; Weekcs, R.
G.; DeYoung, L. M.; Ashendel, C. L.; Astrup, E. G. The
induction of ornithine decarboxylase activity and its control in
mouse skin epidermis. In: Weber, G., ed. Advances in enzyme
regulation. Vol. 17. Elmsford, NY: Pergamon Press; 1979:89112.
55. Baird, W. M.; Sedgwick, J. A.; Boutwell, R. K. Effects of
phorbol and four diesters of phorbot on the incorporation of
tritiated precursors into DNA, RNA, and protein in mouse
epidermis, Cancer Res. 31:1434-1439; 1971.
56. Klein-Szanto, A. J. P. Morphological evaluation of tumor promoter effects on mammalian skin. In: Slaga, T. J., ed. Mechanisms of tumor promotion, Vol. 2, Tumor promotion and skin
carcinogenesis. Boca Raton, FL: CRC Press; 1984:41-72.
57. Trosko, J. E.; Chang, C.-C. Role of intercellular communication in tumor promotion. In: Slaga, T. J., ed. Mechanisms
of tumor promotion, Vol. 4, Cellular responses to tumor promoters. Boca Raton, FL: CRC Press; 1984:119-145.
58. Yamasaki, H. Modulation of cell differentiation by tumor promoters. In: Slaga, T. J., ed. Mechanisms of tumor promotion,
Vol. 4, Cellular responses to tumor promoters. Boca Raton,
FL: CRC Press; 1984:1-26.
59. Slaga, T. J. Multistage skin tumor promotion and specificity
of inhibition. In: Slaga, T. J., ed. Mechanisms of tumor promotion, Vol. 2, Tumor promotion and skin carcinogenesis.
Boca Raton, FL: CRC Press; 1984:189-196.
60. Fiirstenberger, G.; Berry, D. L.; Sorg, B.; Marks, F. Skin
tumor promotion by phorbol esters is a two-stage process.
Proc. Natl. Acad. Sci. USA 78:7722-7726; 1981.
61. Slaga, T. J.; Fischer, S. M.; Nelson, K.,; Gleason, G. L.
Studies on the mechanism of skin tumor promotion: evidence
for several stages in promotion. Proc. Natl. Acad. Sci. USA
77:3659-3663; 1980.
62. Rose-John, S.; Fi.irstenberger, G.; Krieg, P.; Besemfelder, E.;
Rincke, G. ; Marks, F. Differential effects of phorbol esters on
c-fos and c-myc and ornithine decarboxylase gene expression
in mouse skin in vivo. Carcinogenesis 9:831-835; 1988.
63. Fiirstenberger, G.; Sorg, B.; Marks, F. Tumor promotion by
phorbol esters in skin: evidence for a memory effect. Science
220:89-91: 1983.
64. Kinzel, V.; Loehrke, H.; Goerttler, K.; FiJrstenberger, G.;
Marks, F. suppression of the first stage of phorbol 12-tetradecanoate 13-acetate-effected tumor promotion in mouse skin
by nontoxic inhibition of DNA synthesis. Proc. Natl. Acad.
Sci. USA 81:5858-5862; 1984.
65. Aldaz, C. M.; Conti, C. J.; Gimenez, 1. B.; Slaga, T. J.; KlcinSzanto, A. J. P. Cutaneous changes during prolonged application of 12-0-tetradecanoylphorbol-13-acetate on mouse skin
and residual effects after cessation of treatment. Cancer Res.
45:2753-2759; 1985.
66. FiJrstenberger, G.; Kinzel, V.; Schwarz, M.; Marks, F. Partial
inversion of the initiation-promotion sequence of multistage
tumorigenesis in the skin of NMRI mice. Science 230:76-78;
1985.
67. Ordman, A. B.; Cleaveland, J. S.; Boutwell, R. K. 12-0Tetradecanoylphorbol-13-acetate promotes tumors prior to initiation in two-stage promotion. Cancer Lett. 29:79-84; 1985.
1985.
68. Kinzel, V.; Fiirstenberger, G.; Loehrke, H.; Marks, F. Threestage tumorigenesis in mouse skin: DNA synthesis as a prerequisite for the conversion stage induced by TPA prior to
initiation. Carcinogenesis 7:779-782: 1986.
69. Dzarlieva-Petrusevska, R. T.; Fusenig, E. Induction of chromosomal alterations in primary mouse keratinocyte cultures
by TPA but not RPA and inhibition of the clastogenic effects
by ETYA and antipain. Cancer Len. 30(Suppl.):S62; 1986.
70. Parry, J. M.; Parry, E. M.; Barrett, J. E. tumor promoters
induce mitotic aneuploid in yeast. Nature 294:263-265; 1981.
71. Conti, C. J., Aldaz, C. M.; O'Connell, J.; Klein-Szanto, A.
J. P.: Slaga, T. J. Aneuploidy, an early event in mouse skin
tumor development. Carcinogenesis 7:1845-1848; 1986.
72. Emerit, 1. E.; Cerutti, P. A. Tumor promoter phorbol-12-myristate- 13-acetate induced chromosomal damage via indirect action. Nature 293:144-146; 1981.
73. Dzarlieva, R. T.: Fusenig, N. E. Tumor promoter 12-0-tetradecanoylphorbol-13-acetate enhances sister chromatid exchanges and numerical and structural chromosome aberrations
in primary mouse epidermal cell cultures. Cancer Len. 16:7
17; 1982.
74. Fusenig, N. E.; Dzarlieva, R. Phenotypic and chromosomal
alterations in cell cultures as indicators of tumor promoting
activity. In: Hecker, E.; Fusenig, N. E.; Kunz, W.: Marks, F.;
Thielmann, H. W., eds. Carcinogenesis, Vol. 7, Cocarcinogenesis and biological effects of tumor promoters. New York:
Raven Press; 1982:325-329.
75. Cerutti, P. A.; Armstad, P.; Emerit, B. Tumor promoter phorbol myristate acetate induces membrane-mediated chromosomal damage. In: Nygaard, O. F.: Simic, M. G., eds.
Radioprotectors and anticarcinogens. New York: Academic
Press; 1983:527-537.
76. Kinsella, A. R.; Radman, M. Tumor promoter induces sister
chromatid exchanges: relevance to the mechanisms of carcinogenesis. Proc. Natl. Acad. Sci. USA 75:6149-6153: 1978.
77. Nagasawa, H.; Little, J. B. Effect of tumor promoters, protease
inhibitors, and repair processes on X-ray-induced sister chromatid exchanges in mouse cells. Proc. Natl. Acad. Sei. USA
76:1943-1947; 1979.
78. Gentil, A.; Renault, G.; Margot, A. The effect of the tumour
promoter 12-O-tetradecanoylphorbol- 13-acetate (TPA) on UVand MNNG-induced sister chromatid exchanges in mammalian
cells. Int. J. Cancer 26:517-521; 1980.
79. Nagasawa, H.; Little, J. B. Factors influencing the induction
of sister chromatid exchanges in mammalian cells by 12-0tetradecanoylphorbol-13-acetate. Carcinogenesis 2:601 607,
1981.
Antioxidants and skin carcinogenesis
80. Schwartz, J. L.; Banda, M. J.; Wolff, S. 12-0-Tetradecanoylphorbol-13-acetate (TPA) induces sister-chromatid exchanges and delays in cell progression in Chinese hamster
ovary and human cell lines. Mutat. Res. 92:393-409; 1982.
81. Birnboim, H. C. DNA Strand breakage in human leukocytes
exposed to a tumor promoter, phorbol myristate acetate. Science 215:1247-1249; 1982.
82. Hsiao, W.-L. W.; Gattoni-Celli, S.; Weinstein, I. B. Oncogene-induced transformation of C3H 10T 1/2 cells is enhanced
by tumor promoters. Science 226:552-555; 1984.
83. Hennings, H.; Yuspa, S. H. Two-stage tumor promotion in
mouse skin: an alternative interpretation. J. Natl. Cancer Inst.
74:735-740; 1985.
84. Kruszewski, F. H.; Conti, C. J.; DiGiovanni, J. Characterization of skin tumor promotion and progression by chrysarobin
in SENCAR mice. Cancer Res. 47:3783-3790; 1987.
85. Miller, D. R.; Viaje, A.; Aldaz, C. M.; Conti. C. J.; Slaga,
T. J. Terminal differentiation-resistant epidermal cells in mice
undergoing two-stage carcinogenesis. Cancer Res. 47:19351940; 1987.
86. Gueur, M. C.; Maskens, A.; Maes, P. Experimental skin carcinogenesis: a critical review. Cancer Lett. 30(Suppl):S64:
1986.
87. Pelling, J. C., Fischer, S. M.; Neades, R.; Strawhecker, J.
Schweickert, L. Elevated expression and point mutation of the
Ha-ras proto-oncogene in mouse skin tumors promoted by benzoyl peroxide and other promoting agents. Carcinogenesis
8:1481-1484; 1987.
88. Burns, F. J.; Albert, R. E.; Altshuler, B. Cancer progression
in mouse skin. In: Slaga, T. J., ed. Mechanisms of tumor
promotion, Vol. 2, Tumor promotion and skin carcinogenesis.
Boca Raton, FL: CRC Press; 1984:17-39.
89. Hennings, H.; Shores, R.; Wenk, M. L.; Spangler, E. F.:
Tarone, R.; Yuspa, S. H. Malignant conversion of mouse skin
tumors is increased by tumour initiators and unaffected by
tumour promoters. Nature 304:67-69; 1983.
90. Hennings, H.; Shores, R.; Mitchell, P.; Spangler, E. F.; Yuspa,
S. H. Induction of papillomas with a high probability of conversion to malignancy. Carcinogenesis 6:1607-1610; 1985.
91. Roe, F. J.; Carter, R. L.: Mitchley, B. C.; Peto, R.; Hecker,
E. On the persistence of tumor initiation and the acceleration
of tumor progression in mouse skin tumorigenesis. Int. J. Cancer 9:264-273; 1972.
92. O'Connell, J. F.; Klein-Szanto, A. J. P.: DiGiovanni, D. M.;
Fries. J. W.; Slaga, T. J. Malignant progression of mouse skin
papillomas treated with ethylnitrosourea, N-methyl-N'-nitroN-nitrosoguanidine, or 12-0-tetradecanoylphorbol-13-acetate.
Cancer Lett. 30:269-274; 1986.
93. Rotstein, J.; O'Connell, J.; Slaga, T. J. The enhanced progression of papillomas to carcinomas by peroxides in the 2stage mouse skin model. Proc. Am. Assoc. Cancer Res. 27:
143; 1986.
94. O'Connell, J. F.; Klein-Szanto, A. J. P.; DiGiovanni, D. M.;
Fries, J. W.; Slaga, T. J. Enhanced malignant progression of
mouse skin tumors by the free-radical generator benzoyl peroxide. Cancer Res. 46:2863-2865; 1986.
95. Reddy, A. L.; Fialkow, P. J. Influences of dose of initiator on
two-stage skin carcinogenesis in BALB/c mice with cellular
mosaicism. Carcinogenesis 9:751-754; 1988.
96. Cerutti, P. A. Response modification creates promotability in
multistage carcinogenesis. Carcinogenesis 9:519-526; 1988.
97. Slaga, T. J.; Klein-Szanto, A. J. P.; Triplett, L. L.; Yotti, L.
P.; Trosko, J. E. Skin tumor-promoting activity of benzoyl
peroxide, a widely used free radical-generating compound.
Science 213:1023-1025; 1981.
98. Verma, A. K. Biochemical mechanism of modulation of skin
carcinogenesis by retinoids. In: Orfanos, C. E.; Braun-Falco,
O.; Farber, E. M.; Grupper, C.; Polano, M. K.; Schuppli, R.,
eds. Retinoids. Berlin: Springer-Verlag; 1981 : 117-131.
99. Egner, P. A.; Kensler, T. W. Effects of a biomimetic superoxide dismutase on complete and multistage carcinogenesis in
mouse skin. Carcinogenesis 6:1167-1172; 1985.
401
100. Perchellet, J. P.; Abney, N. L.; Thomas, R. M.; Guislain, Y.
L.; Perchellet, E. M. Effects of combined treatments with
selenium, glutathione, and vitamin E on glutathione peroxidase
activity, ornithine decarboxylase induction, and complete and
multistage carcinogenesis in mouse skin. Cancer Res. 47:477
485; 1987.
101. DiGiovanni, J.; Decina, P. C.; Prichett, W. P.; Cantor, J.;
Aalfs, K. K.; Coombs. M. M. Mechanism of mouse skin tumor promotion by chrysarobin. Cancer Res. 45:2584-2589;
1985.
102. Kruszewski, F. H.; Chenicek, C. J.; DiGiovanni, J. Effect of
application frequency on epidermal ornithine decarboxylase
induction by chrysarobin in SENCAR mice. Cancer Lett.
32:263-269; 1986.
103. Scribner, N. K.; Scribner, J. D. Separation of initiating and
promoting effects of the skin carcinogen 7-bromomethylbenz/a)anthracene. Carcinogenesis 1:97- 100; 1980.
104. Copeland, E. S. A National Institute of Health Workshop report: free radicals in promotion--a Chemical Pathology Study
Section Workshop. Cancer Res. 43:5631 5637; 1983.
105. Cerutti, P. A. Prooxidant states and tumor promotion. Science
227:375- 381 ; 1985.
106. Cerutti, P. A. Oxidant tumor promoters. In: Colburn, N. H.;
Moses, H. L.; Stanbridge, E. J. eds. Growth.factors, tumor
promoters, and cancer genes. New York: Alan R. Liss;
1988:239-247.
107. Kensler, T. W., Trush, M. A. Oxygen free radicals in chemical
carcinogenesis. In: Oberley, L. W., ed. Superoxide dismutase,
Vol. 3, Pathological states. Boca Raton, FL: CRC Press;
1985:191-236.
108. Kensler, T. W.: Taffe B. G. Free radicals in tumor promotion.
Adv. Free Radical Biol. Med. 2:347-387; 1986.
109. Nishimura, S.: Ames, B. N. U.S.-Japan Meeting on "Oxygen
radicals in cancer". Jpn. J. Cancer Res. (Gann)77:843-848;
1986.
110. Fischer, S. M.; Floyd R. A.; Copeland, E. S. Workshop report
from the Division of Research Grants, National Institute of
Health. Oxy radicals in carcinogenesis--a Chemical Pathology
Study Section workshop. Caneer Res. 48:3882-3887: 1988.
111. Halliwell, B.; Gutteridge, J. M. C. Oxygen free radicals
and iron in relation to biology and medicine: some problems
and concepts. Arch. Biochem. Biophys. 246:501-514; 1986.
112. Haliiwell, B.; Gutteridge, J. M. C. Oxygen toxicity, oxygen
radicals, transition metals and disease. Biochem. J. 219:1 14;
1984.
113. lmlay, J. A.; Chin, S. M.; Linn, S. Toxic DNA damage by
hydrogen peroxide through the Fenton reaction in vivo and in
vitro. Science 240:640-642; 1988.
114. Marnett, L. J. Peroxyl free radicals: potential mediators of
tumor initiation and promotion. Carcinogenesis 8:1365-1373;
1987.
115. Halliwell, B. Oxidants and human disease: some new concepts.
FASEB J. 1:358-364; 1987.
116. McLennan, G.; Oberley, L. W.; Autor, A. P. The role of
oxygen-derived free radicals in radiation-induced damage and
death of nondividing, eucaryotic cells. Radiation Res. 84:122132; 1980.
117. Biaglow, J. E. The effects of ionizing radiation on mammalian
cells. J. Chem. Educ. 58:144-156; 1981.
118. Cross, C. E.; Halliwell, B.; Borish, E. T.; Pryor, W. A.: Ames,
B. N.; Saul, R. L.; McCord, J. M.; Harmon, D. Oxygen
radicals and human disease. Ann. Intern. Med. 107:526-545;
1987.
119. Imlay, J. A., Linn, S. DNA damage and oxygen radical toxicity. Science 240:1302-1309; 1988.
120. Halliwell, B.; Gutteridge, J. M. C. Free radicals in biology
and medicine. New York: Oxford University Press; 1985.
121. Liebler, D. C.; Kling, D. S.; Reed, D. J. Antioxidant protection of phospholipid bilayers by a-tocopherol. J. Biol. Chem.
261:12114-12119; 1986.
122. Meister, A.; Anderson, M. E. Glutathione. Ann. Rev. Biochem. 52:711-760; 1983.
402
J.-R PERCHELLE'rand E. M. PERCHELt.E'r
123. Lawrence, R. A.; Burk, R. F. Glutathione peroxidase activity
in selenium-deficient rat liver. Biochem. Biophys. Res. Commun. 71:952-958; 1976.
124. Prohaska, J. R.; Ganther, H. E. Glutathione peroxidase activity of glutathione S-transferases purified from rat liver.
Biochem. Biophys. Res. Commun. 76:437-445: 1977.
125. Pierce, S.; Tappel, A. L. Glutathione peroxidase activities
from rat liver. Biochim. Biophys. Acta 523:27-36; 1978.
126. Jakoby, W. B.; Habig, W. H. Glutathione transferases. In:
Jakoby, W. B., ed. Enzymatic basis ofdetoxification. Vol. 2.
New York: Academic Press; 1980:63-94.
127. Chasseaud, L. F. The role of glutathione and glutathione Stransferases in the metabolism of chemical carcinogens and
other electrophilic agents. Adv. Cancer Res. 29:175 274;
1979.
128. Saneto, R. P.; Awasthi, Y. C.; Srivastava, S. K. Glutathione
S-transferases of the bovine retina. Biochem. J. 205:213-217;
1982.
129. Perchellet, J. P.; Perchellet, E. M.; Orten, D. K.; Schneider,
B. A. Inhibition of the effects of 12-0-tetradecanoylphorbol13-acetate on mouse epidermal glutathione peroxidase and ornithine decarboxylase activities by glutathione level-raising
agents and selenium-containing compounds. Cancer Lett.
26:283-293; 1985.
130. Klein-Szanto, A. J. P.; Slaga, T. J. Effects of peroxides on
rodent skin: epidermal hyperptasia and tumor promotion. J.
Invest. Dermatol. 79:30-34; 1982.
131. loannides, C.; Parke, D. V. The cytochromes P-448--a unique
family of enzymes involved in chemical toxicity and carcinogenesis. Biochem. Pharmacol. 36:4197-4207; 1987.
132. Bowden, G. T.;Slaga, T. J.;Shapas, B.G.:BoutwelI, R. K.
The role of aryl-hydrocarbon hydroxylase in skin tumor initiation by 7,12-dimethylbenz(a)anthracene and 1,2,5,6-dibenzanthracene using DNA binding and thymidine-~H incorporation into DNA as criteria. Cancer Res. 34:2634-2642:
1974.
133. Pyerin, W. G.; Hecker, E. On the biochemical mechanism of
tumorigenesis in mouse skin, IX. Interrelation between tumor
initiation by 7,12-dimethylbenz(a)anthracene and the activities
of epidermal arylhydrocarbon monooxygenase and epoxide hydratase. J. Cancer Res. Clin. Oncol. 93:7 30: 1979.
134. Miller, E. C. Some current perspectives on chemical carcinogenesis in humans and experimental animals: presidential address. Cancer Res. 38:1479-1496; 1978.
135. Conney, A. H. Induction of microsomal enzymes by foreign
chemicals and carcinogenesis by polycyclic aromatic hydrocarbons. G. H. A. Clowes Memorial Lecture. Cancer Res.
42:4875-4917; 1982.
136. Chouroulinkov, I.; Gentil, A.; Tierney, B.; Grover, P. L.;
Sims, P. The initiation of tumours on mouse skin by dihydrodiols derived from 7,12-dimethylbenz(a)anthracene and 3methylcholanthrene. Int. J. Cancer 24:455-460: 1979.
137. Gelboin, H. V.; Wiebel, F.; Diamond, L. Dimethylbenzanthracene tumorigenesis and aryl hydrocarbon hydroxylase in
mouse skin: inhibition by 7,8-benzoflavone. Science 170:169171; 1970.
138. Gelboin, H. V.; Kinoshita, N.; Wiebel, F. J. Microsomal hydroxylases: induction and role in polycyclic hydrocarbon carcinogenesis and toxicity. Fed. Proc. 31:1298-1309; 1972.
139. Slaga, T. J.; Thompson, S.; Berry, D. L.; DiGiovanni, J.;
Juchau, M. R.; Viaje, A. The effects of benzoflavones on
polycyclic hydrocarbon metabolism and skin tumor initiation.
Chem.-Biol. Interact. 17:297-312; 1977.
140. Pyerin, W. G.; Hecker, E. Tumor initiation in mouse skin by
7,12-dimethylbenz[aJanthracene: irrelevance of systemic activation. Cancer Lett. 8:317- 321 ; 1980.
141. Lesca, P.; Mansuy, D. 9-Hydroxyellipticine: inhibitory effect
on skin carcinogenesis induced in Swiss mice by 7,12-dimethylbenz[a]anthracene. Chem.-Biol. Interact. 30:181-187;
1980.
142. Camus, A. M.; Pyerin, W. G.; Grover, P. L.; Sims, P.; Malaveille, C.; Bartsch, H. Mutagenicity of benzo[a]pyrene 7,8-
143.
144.
145.
146.
147.
148.
149.
150.
151.
152.
153.
154.
155.
diyhydrodiol and 7,12-dimethylbenz[a]anthracene 3,4-dihydrodiol in S. typhimurium mediated by microsomes from rat
liver and mouse skin. Chem.-Biol. Interact. 32:257-265;
1980.
Nebert, D. W.; Benedict, W. T.; Kouri, R. E. Aromatic hydrocarbon-produced tumorigenesis and the genetic differences
in aryl hydrocarbon hydroxylase. In: Ts'o, P. O. P.; DiPaolo,
J. A., eds. Chemical carcinogenesis, Part A. New York: Marcel Dekker; 1974:277-288.
Cavalieri, E.; Auerbach, R. Reactions between activated
benzo[a]pyrene and nucleophilic compounds, with possible
implications on the mechanism of tumor initiation. J. Natl.
Cancer Inst. 53:393-397; 1974.
Cavalieri, E.; Rogan, E.; Roth, R. Multiple mechanisms of
activation in aromatic hydrocarbon carcinogenesis. In: Floyd,
R. A., ed. Free radicals and cancer. New York: Marcel Dekker; 1982:117-158.
Nagata, C.; Kodama, M.; Ioki, Y.: Kimura, T. Free radicals
produced from chemical carcinogens and their significance in
carcinogenesis. In: Floyd, R. A., ed. Free radicals and cancer.
New York: Marcel Dekker; 1982:1 62.
Lesko, S. A.; Ts'o, P. O.; Yang, S. U.; Cheng, R.
Benzo(a)pyrene radicals and oxygen radical involvement in
DNA damage, cellular toxicity and carcinogenesis. In: McBrien, D. C.: Slater, T. F., eds. Free radicals, lipid peroxidation and cancer. New York: Academic Press; 1982:401
420.
Slater, T. F.; Cheeseman, K. H.; Proudfoot, K. Free radicals,
lipid peroxidation, and cancer. In: Armstrong, D.; Sohal, R.
S.: Cutler. R. G.: Slater, T. F., eds. Free radicals in molecular
biology, aging and disease. New York: Raven Press: 1984:
293-305.
Lesko, S.; Caspary, W.; Lorentzen, R.: Ts'o, P. O. P. Enzymic
formation of 6-oxobenzo[a]pyrene radical in rat liver homogcnatcs from carcinogenic benzo[a]pyrene. Biochem. 14:39783984; 1975.
Lorentzen, R. J.; Lesko, S. A.; McDonald, K.; Ts'o, P. O. P.
Toxicity of metabolic benzo[a]pyrenediones to cultured cells
and the dependence upon molecular oxygen. Cancer Res.
39:3194-3198; 1979.
Jaffe, D.; Bowden, G. T. Ionizing radiation as an initiator:
effects of proliferation and promotion time on tumor incidence
in mice. Cancer Res. 47:6692-6696; 1987.
Trush, M. A.; Seed, J. L,; Kensler, T. W. Oxidant-dependent
metabolic activation of polycyclic aromatic hydrocarbons by
phorbol ester-stimulated human polymorphonuclear leukocytes: possible link between inflammation and cancer. Proc.
Natl. Acad. Sci. USA 82:5194-5198; 1985.
Kensler, T. W.: Egner, P. A.; Moore. K. G.; Taffe, B. G.:
Twerdok, L. E.; Trush, M. A. Role of inflammatory cells in
the metabolic activation of polycyclic aromatic hydrocarbons
in mouse skin. Toxicol. Appl. Pharmacol. 90:337-346; 1987.
Marnett, L. J. Polycyclic hydrocarbon oxidation during prostaglandin biosynthesis. Life Sci. 29:531-546; 1981.
Marnett, L. J.: Dix, T. A.: Sachs, R. J.; Siedlik, P. H. Oxidations by fatty acid hydroperoxides and prostaglandin synthetase. In: Samuelsson, B.; Ramwetl, P.; Paoletti, R., eds.
Advances in prostaglandin and thromboxane research. Vol.
11. New York: Raven Press, 1983:79-86.
156. Ohki, S.; Ogino, N.; Yamamoto, S.; Hayashi, O. Prostaglandin hydroperoxidase, an integral part of prostaglandin endoperoxide synthetase from bovine vesicular gland microsomes.
J. Biol. Chem. 254:829-836: 1979.
157. Eling, T. E.: Krauss, R. S. Arachidonic acid-dependent metabolism of chemical carcinogens and toxicants. In: Marnett,
L. J., ed. Arachidonic acid metabolism and tumor initiation.
New York: Martinus Nijhoff; 1985:83-124.
158. Eling, T.; Curtis, J.; Battista, J.; Marnett, L. J. Oxidation of
( + )-7,8-dihydroxy-7,8-dihydrobenzo[a]pyrene by mouse keratinocytes: evidence for peroxyl radical- and monooxygenasedependent metabolism. Carcinogenesis 7:1957-1963; 1986.
159. Dix, T. A.; Marnbett, L. J. Metabolism of polycyclic aromatic
Antioxidants and skin carcinogenesis
160.
161.
162.
163.
164.
165.
166.
167.
168.
169.
170.
171.
172.
173.
174.
175.
176.
177.
178.
hydrocarbon derivatives to ultimate carcinogens during lipid
peroxidation. Science 221:77-79; 1983.
Troll, W.; Witz, G.: Goldstein, B.; Stone, D.; Sugimura, T.
The role of free oxygen radicals in tumor promotion and carcinogenesis. In: Hecker, E., Fusenig, N. W. ; Kunz, W. ; Marks,
F.; Thielmann, H. W., eds. Carcinogenesis, Vol. 7, Carcinogenesis and biological effects of tumor promoters. New York:
Raven Press; 1982:593-597.
Slaga, T. J.: Solanki, V.; Logani, M. Studies on the mechanism
of action of antipromoting agents: suggestive evidence for the
involvement of free radicals in promotion. In: Nygaard, O. F.;
Simic, M. G., eds. Radioprotectors and anticarcinogens. New
York: Academic Press; 1983:471-485.
Perrella, F. W.; O'Leary, P.; Boutwell, R. K. Effects of 120-tetradecanoylphorbol-13-acetate and mezerein on gamma radiation-induced DNA repair in resting bovine lymphocytes.
Cancer Lett. 15:87-93; 1982.
Birnboim, H. C.: Morrison, D. P.: Joyce, T. L. Measurement
of enzyme activities in mouse epidermis following phorbol
ester treatment: a potential artifact. Carcinogenesis 7:495497; 1986.
Solanki, V.; Rana, R. S.; Slaga, T. J. Diminution of mouse
epidermal superoxide dismutase and catalase activities by tumor promoters. Carcinogenesis 2:1141-1146; 1981.
Kinsella, A. R.; Gainer, H. S. C.; Butler, J. Investigation of
a possible role for superoxide anion production in tumor promotion. Carcinogenesis 4:717-719; 1983.
Emerit, 1. ; Levy, A. ; Cerutti, P. Suppression of tumor promoter
phorbol-myristate acetate-induced chromosome breakage by
antioxidants and inhibitors of arachidonic acid metabolism.
Murat. Res. 110:327-335: 1983.
Friedman, J.; Cerutti, P. The induction of ornithine decarboxylase by phorbol 12-myristate 13-acetate or by serum is inhibited by antioxidants. Carcinogenesis 4:1425-1427; 1983.
Kensler, T. W.; Bush D. M.; Kozumbo, W. J. Inhibition of
tumor promotion by a biomimetic superoxide dismutase. Science 221:75-77; 1983.
Schwarz, M.; Peres, G.; Kunz, W.; Ftistenberger, G.; Kittstein, W.: Marks, F. On the role of superoxide anion radicals
in skin tumor promotion. Carcinogenesis 5:1663-1670:1984.
Perchellet, J. P.: Perchellet, E. M.; Abney, N. L. Enzymic
and nonenzymic generation of peroxides in mouse epidermal
cell and cell-free systems treated with tumor promoters. Proc.
Am. Assoc. Cancer Res. 29:161; 1988.
Perchellet, E. M.; Abney, N. L.; Perchellet, J. P. Stimulation
of hydroperoxide generation in mouse skins treated with tumorpromoting or carcinogenic agents in vivo and in vitro. Cancer
Lett. 42:169 177; 1988.
Perchellet, J. P.: Boutwell, R. K. Enhancement by 3-isobutyll-methylxanthine and cholera toxin of 12-0-tetradecanoylphorbol- 13-acetate-stimulated cyclic nucleotide levels and ornithine decarboxylase activity in isolated epidermal cells.
Cancer Res. 40:2653-2660; 1980.
Speier, C.; Baker, S. S.; Newburger, P. E. Relationships between in vitro selenium supply, glutathione peroxidase activity, and phagocytic function in the HL-60 human myeloid cell
line. J. Biol. Chem. 260:8951-8955; 1985.
Thurman, R. G.; Ley, H. G.; Scholz, R. Hepatic microsomal
ethanol oxidation. Hydrogene peroxide formation and the role
of catalase. Eur. J. Biochem. 25:420-430; 1972.
Barham, D.; Trinder, P. An improved colour reagent for the
determination of blood glucose by the oxidase system. Analyst
97:142-145; 1972.
Frew, J. A.; Jones, P.; Scholes, G. Spectrophotometric determination of hydrogen peroxide and organic hydroperoxides at
low concentration in aqueous solution. Analyt. Chim. Acta
155:139-150; 1983.
Green, M. J.; Hill, H. A. O. Chemistry of dioxygen. Methods
in Enzymol. 105:3-22; 1984.
Robertson, F. M.; Laskin, D. L.; Laskin, J. D. Production of
reactive oxygen intermediates in mouse skin following topical
application of the tumor promoter, 12-0-tetradecanoylphorbol-
179.
180.
181.
182.
183.
184.
185.
186.
187.
188.
189.
190.
191.
192.
193.
194.
403
13-acetate (PMA). Proc. Am. Assoc. Cancer Res. 29:155;
1988.
Perchellet, J. P.; Kishore, G. S.; Perchellet, E. M. Enhancement by adriamycin of the effects of 12-0-tetradecanoylphorbol-13-acetate on mouse epidermal glutathione peroxidase
activity, ornithine decarboxylase induction and skin tumor promotion. Cancer Lett. 29:127-137; 1985.
Perchellet, J. P.; Perchellet, E. M.; Orten, D. K.; Schneider,
B. A. Decreased ratio of reduced/oxidized glutathione in
mouse epidermal cells treated with tumor promoters. Carcinogenesis 7:503-506: 1986.
Perchellet, J. P.; Perchellet, E. M.; Abney, N. L.; Zirnstein,
J. A. : Belman, S. Effects of garlic and onion oils on glutathione
peroxidase activity, the ratio of reduced/oxidized glutathione
and ornithine decarboxylase induction in isolated mouse epidermal cells treated with tumor promoters. Cancer Biochem.
Biophvs. 8:299-312; 1986.
Perchellet, E. M.: Maatta, E. A.: Abney, N. L.; Perchellet,
J. P. Effects of diverse intracellular thiol delivery agents on
glutathione peroxidase activity, the ratio of reduced/oxidized
glutathione, and ornithine decarboxylase induction in isolated
mouse epidermal cells treated with 12-0-tetradecanoylphorbol13-acetate. J. Cell. Phvsiol. 131:64-73; 1987.
Perchellet, J. P.; Abney, N. L.; Thomas, R. M.; Perchellet,
E. M. ; Maatta, E. A. Inhibition of multistage tumor promotion
in mouse skin by diethyldithiocarbamate. Cancer Res. 47:
6302-6309; 1987.
Hildebrandt. A. G.; Roots, I. Reduced nicotinamide adenine
dinucleotide phosphate (NADPH)-dependent formation and
breakdown of hydrogen peroxide during mixed function oxidation reactions in liver microsomes. Arch. Biochem. Biophys.
171:385-397: 1975.
Oberley, L. W. Superoxide dismutase and cancer. In: Oberley,
L. W., editor. Superoxide dismutase, Vol. 2. Boca Raton: CRC
Press; 1982:127-165.
DeChatelet, L. R.; Shirley, P. S.; Johnston, R. B. Effects of
phorbol myristate acetate on the oxidative metabolism of human polymorphonuclear leukocytes. Blood 47:545-554: 1976.
Nathan, C. F.: Brukner, L. H.; Silverstein, S. C.; Cohn, Z.
A. Extracellular cytolysis by activated macrophages and
granulocytes. I. Pharmacologic triggering of effector cells and
the release of hydrogen peroxide. J. Exp. Med. 149:84-99:
1979.
Keisari, Y.; Flescher, E.; Geva, 1. Macrophage oxidative burst
and related cytotoxicity. 1. Differential activation by tumorpromoting and non-tumor-promoting phorbol esters. Int. J.
Cancer 34:845-848: 1984.
Goldstein, B.: Witz, G.; Zimmerman, J.; Gee. C. Free radicals
and reactive oxygen species in tumor promotion. In: Greenwald, R. A. : Cohen, G., eds. Oxy radicals and their scavenger
systems, Vol. 2, Cellular and medical aspects. New York:
Elsevier; 1983:321- 325.
Reiners, J. J.; Pence, B. C.; Barcus, M. C. S.: Cantu, A. R.
12-0-Tetradecanoylphorbol- 13-acetate-dependent induction of
xanthine dehydro-genase and conversion to xanthine oxidase
in murine epidermis. Cancer Res. 47:1775-1779; 1987.
Fischer, S. M.; Reiners, J. J.: Pence, B. C.; Aldaz, C. M.;
Conti, C. J.; Morris, R. J.; O'Connell, J. F.: Rotstein, J. B.;
Slaga, T. J. Mechanisms of carcinogenesis using mouse skin:
the multistage assay revisited. In: Langenbach, R.; Elmore,
E.; Barrett, J. C.; eds. Tumor promoters: biological approaches for mechanistic studies and assay systems. New
York: Raven Press; 1988:11-30.
Zimmerman, R.; Cerutti, P. Active oxygen acts as a promoter
of transformation in mouse embryo C3H/10T~/CI8 fibroblasts. Proc. Natl. Acad. Sci. USA 81:2085-2087; 1984.
Lillehaug, J. R.; Berge, R. K. The tumour promoter 12-0tetradecanoylphorbol-13-acetate increases the activities of
some peroxisome-associated enzymes in in vitro cell culture.
Br. J. Cancer 53:121-127; 1986.
Lillehaug, J. R.; Aarsaether, N.: Berge, R. K.; Male, R. Peroxisome proliferators show tumor-promoting but no direct
404
J.-P. PERCItELLETand E. M. PERCHELLET
transforming activity in vitro. Int. J. Cancer 37:97-100; 1986.
195. Fukami, M. H.; Eikhom, T. S.; Ekanger, R.; Flatmark, T.;
Nillson, A. Relationship between induction of ornithine decarboxylase and specific gene expression in rat liver in response to the tumor promoter agent clofibrate. Carcinogenesis
7:1441-1446; 1986.
196. Goel, S. K.; Lalwani, N. D.; Reddy, J. K. Peroxisome proliferation and lipid peroxidation in rat liver. Cancer Res.
46:1324-1330; 1986.
197. Logani, M. K.; Solanki, V.; Slaga, T. J. Effect of tumor promoters on lipid peroxidation in mouse skin. Carcinogenesis
3:1303-1306; 1982.
198. Tomaszewski, K. E.; Agarwal, D. K.; Melnick, R. L. In vitro
steady-state levels of hydrogen peroxide after exposure of male
F344 rats and female B6C3F~ mice to hepatic peroxisome proliferators. Carcinogenesis 7:1871-1876; 1986.
199. Capel, I. D.; Thornley, A. C. Lipoperoxide levels, glutathione
status and glutathione peroxidase activity in liver and tumors
of mice bearing the Lewis lung carcinoma. Cancer Biochem.
Biophys. 6:167-172; 1983.
200. Lewis, J. G.; Adams, D. O. Enhanced release of hydrogen
peroxide and metabolites of arachidonic acid by macrophages
from SENCAR mice following stimulation with phorbol esters.
Cancer Res. 46:5696-5700; 1986.
201. Dixit, R.; Mukhtar, H.; Bickers, D. R. Studies on the role of
reactive oxygen species in mediating lipid peroxide formation
in epidermal microsomes of rat skin. J. Invest. Dermatol.
81:369-375; 1983.
202. Black, H. S.; Lenger, W. A.; Gerguis, J.; Thornby, J. I. Relation of antioxidants and level of dietary lipid to epidermal
lipid peroxidation and ultraviolet carcinogenesis. Cancer Res.
45:6254-6259; 1985.
203. Yuspa, S. H.; Lichti, U.: Ben, T.; Patterson, E.; Her, lings,
H.; Slaga, T. J.; Colburn, N.; Kelsey, W. Phorbol ester~ stimulate DNA synthesis and ornithine decarboxylase activity in
mouse epidermal cell cultures. Nature 262:402-404; 1976.
204. Verma, A. K.; Boutwell, R. K. An organ culture of adult
mouse skin: an in vitro model for studying the molecular mechanism of skin tumor promotion. Biochem. Biophys. Res. Commun. 96: 854-862; 1980.
205. Fischer, S. M.; Baldwin, J. K.; Jasheway, D. W.; Patrick, K.
E,; Cameron, G. S. Phorbol ester induction of 8-1ipoxygenase
in inbred SENCAR (SSIN) but not C57BL/6J mice correlated
with hyperplasia, edema, and oxidant generation but not ornithine decarboxylase induction. Cancer Res. 48:658 664:
1988.
206. Nishizuka, Y. Perspectives on the role of protein kinase C in
stimulus-response coupling. J. Natl. Cancerlnst. 76:363 370;
1986.
207. Serhan, C. N.; Broekman, M. J., Korchak, H. M.; Smolen,
J. E.; Marcus, A. J.; Weissmann, G. Changes in phosphatidylinositol and phosphatidic acid in stimulated human neutrophils, relationship to calcium mobilization, aggregation and
superoxide radical generation. Biochim. Biophys. Acta
762:420-428; 1983.
208. Fujita, I.: Irita, K.; Takeshige, K.: Minakami, S. Diacylglycerol, 1-oleoyl-2-acetyl-glycerol, stimulates superoxidegeneration from human neutrophils. Bioehem. Biophys. Res.
Commun. 120:318-324; 1984.
209. Robinson, J. M.; Badwey, J. A.; Karnovsky, M. L.: Karnovsky, M. J. Superoxide release by neutrophils: synergistic effects of a phorbol ester and a calcium ionophore. Biochem.
Biophys. Res. Commun. 122:734-739; 1984.
210. Penfield, A.; Dale, M. M. Synergism between A23187 and Ioleoyl-2-acetyl-glycerol in superoxide production by human
neutrophils. Biochem. Biophys. Res. Commun. 125:332-336:
1984.
211. Dewald, B.; Payne, T. G.; Baggiolini, M. Activation of
NADPH oxidase of human neutrophils, potentiation of chemotactic peptide by a diacylglycerol. Biochem. Biophys. Res.
Commun. 125:367-373; 1984.
212. Di Virgilio, F.; Lew, D. P.: Pozzan, T. Protein kinase C ac-
213.
214.
215.
216.
217.
218.
219.
22(I.
221.
222.
223.
224.
225.
226.
227.
228.
229.
230.
tivation of physiological processes in human neutrophils at
vanishingly small cytosolic Ca 2+ levels. Nature 310: 691-693:
1984.
Pontremoli, S.; Melloni, E.; Michetti, M.; Sacco, O.; Salamino, F.; Sparatore, B.; Horecker, B. L. Biochemical responses in activated human neutrophils mediated by protein
kinase C and a Ca-'+-requiring proteinase. J. Biol. Chem.
261:8309-8313; 1986.
Dale, M, M.; Penfield, A. Synergism between phorbol ester
and A23187 in superoxide production by neutrophils. FEBS
Len. 175:170-172, 1984.
Wilson, E.; Olcott, M. C.; Bell, R. M.; Merrill, A. H.: Lambeth, J. D. Inhibition of the oxidative burst in human neutrophils by sphingoid long-chain bases. Role of protein kinase C
in activation of the burst. J. Biol. Chem. 261:12616 12623:
1986.
lrita, K.; Fujita, I.: Takeshige, K.: Minakami, S.; Yoshitake,
J. Calcium channel antagonist induced inhibition of superoxide
production in human neutrophils. Mechanisms independent of
antagonizing calcium influx. Biochem. Pharmacol. 35:3465
3471: 1986.
Fujita, 1.: Takeshige, K.: Minakami, S. Inhibition of superoxide formation by l-(5-isoquinolinesulfonyl)-2-methylpiperazine (H-7), an inhibitor of protein kinase C. Biochem.
Pharmacol. 35:4555 4562; 1986.
Rider, L. G.; Niedel, J. E. Diacytglycerol accumulation and
superoxide anion production in stimulated human neutrophils.
J. Biol. Chem. 262:5603-5608; 1987.
Kano, S.; lisuka, T.; Ishimura, Y.; Fujiki, H.; Sugimura, T.
Stimulation of superoxide anion formation by the non-TPA
type tumor promoters palytoxin and thapsigargin in porcine
and human neutrophils. Biochem. Biophys. Res. Commun.
143:672-677: 1987.
Miyachi, Y.: Yoshioka, A.: Imamura, S.: Niwa. Y. Effect of
antibiotics on the generation of reactive species. J. Invest.
Dermatol. 86:449-453; 1986.
Pence, B. C.: Reiners, J. J. Murine epidermal xanthine oxidase
activity: correlation with degree of hyperplasia induced by
tumor promoters. Cancer Res. 47:6388 6392; 1987.
Donnelly, T. E.: Pelling, J. C.; Anderson, C. L.: Dalbey, D.
Benzoyl peroxide activation of protein kinase C activity in
epidermal cell membranes. Carcinogenesis 8:1871-1874',
1987.
Gindhart. T. D.; Srinivas, L.: Colburn, N. H. Benzoyl peroxide promotion of transformation of JB6 mouse epidermal
cells: inhibition by ganglioside G1 but not retinoic acid. Carcinogenesis 6:309-31 I: 1985.
Hartley, J. A.: Gibson, N. W.; Zwelling, L. A.; Yuspa, S. H.
The association of DNA strand breaks with accelerated terminal differentiation in mouse epidermal cells exposed to tumor promoters. Cancer Res. 45:4864-4870; 1985.
Frenkel, K.: Chrzan, K. Hydrogen peroxide formation and
DNA base modification by tumor promoter-activated polymorphonuclear leukocytes. Carcinogenesis 8:455-460; 1987.
Fischer, S. M.; Klein-Szanto, A. J. P.; Adams, L. M.; Slaga,
T. J. The first stage and complete promoting activity of
retinoic acid but not the analog RO-10-9359. Carcinogenesis
6:575-578; 1985.
Birnboim, H. C. Factors which affect DNA strand breakage
in human leukocytes exposed to a tumor promoter, phorbol
myristate acetate. Can. J. Physiol. Pharmacol. 60:1359-1366:
1982.
Frenkel, K.; Chrzan, K.; Troll, W.; Teebor, G. W.: Steinberg,
J. J. Radiation-like modification of bases in DNA exposed to
tumor promoter-activated polymorphonuclear leukocytes.
Cancer Res. 46:5533-5540; 1986.
Birnboim, H. C. Importance of DNA strand-break damage in
tumor promotion. In: Nygaard, O. F.; Simic, M. G., eds.
Radioprotectors and anticarcinogens. New York: Academic
Press; 1983:539-556.
Birnboim, H. C. DNA strand breaks in human leukocytes induced by superoxide anion, hydrogen peroxide and tumor pro-
Antioxidants and skin carcinogenesis
231,
232,
233.
234.
235.
236.
237.
238.
239.
240.
241.
242.
243.
244.
245.
246.
247.
248.
249.
moters are repaired slowly compared to breaks induced by
ionizing radiation. Carcinogenesis 7:1511-1517; 1986.
Oya, Y.; Yamamoto, K.; Tonomura, A. The biological activity
of hydrogen peroxide. I. Induction of chromosome-type aberrations susceptible to inhibition by scavengers of hydroxyl
radicals in human embryonic fibroblasts. Mutat. Res. 172:
245-253; 1986.
Verma, A. K.; Carcia, C. T.; Ashendel, C. L.; Boutwell, R.
K. Inhibition of 7-bromomethylbenz[a]anthracene-promoted
mouse skin tumor formation by retinoic acid and dexamethasone. Cancer Res. 43:3045-3049; 1983.
Hartley, J. A.; Gibson, N. W.; Kilkenny, A.; Yuspa, S. H.
Mouse keratinocytes derived from initiated skin or papillomas
are resistant to DNA strand breakage by benzoyl peroxide: a
possible mechanism for tumor promotion mediated by benzoyl
peroxide. Carcinogenesis 8:1827-1830; 1987.
Wattenberg, L. W. Inhibition of chemical carcinogenesis by
antioxidants. In: Slaga, T. J., ed. Carcinogenesis, Vol. 5,
Modifiers of chemical carcinogenesis. New York: Raven Press:
1980:85-98.
Wattenberg, L. W. Chemoprevention of cancer. Cancer Res.
45:1-8; 1985.
Ito, N.; Hirose, M. The role of antioxidants in chemical carcinogenesis. Jpn. J. Cancer Res. (Gann) 78:1011-1026; 1987.
Hocman, G. Chemoprevention of cancer: phenolic antioxidants
(BHT, BHA). Int. J. Biochem. 20:639-651; 1988.
Shamberger, R. J. Relationship of selenium to cancer. I. Inhibitory effect of selenium on carcinogenesis. J. Natl. Cancer
Inst. 44:931-936; 1970.
Slaga, T. J.; Bracken, W. M. The effects of antioxidants on
skin tumor initiation and aryl hydrocarbon hydroxylase. Cancer Res. 37:1631-1635; 1977.
Shamberger, R. J. Increase of peroxidation in carcinogenesis.
J. Natl. Cancer Inst. 48:1491 1497; 1972.
Shamberger~ R. J.; Rudolph, G. Protection against carcinogenesis by antioxidants. Experientia 22:116; 1966.
Perchellet, J. P.; Owen, M. D.: Posey, T. D.; Often, D. K.;
Schneider, B. A. Inhibitory effects of glutathione level-raising
agents and D-a-tocopherol on ornithine decarboxylase induction and mouse skin tumor promotion by 12-0-tetradecanoy[phorbol- 13-acetate. Carcinogenesis 6:567-573; 1985.
Smart, R. C.; Huang, M.-T.; Han, Z. T.; Kaplan, M. C.;
Focella, A.; Conney, A. H. Inhibition of 12-0-tetradecanoy[phorbol- 13-acetate induction of ornithine decarboxylase activity, DNA synthesis, and tumor promotion in mouse skin by
ascorbic acid and ascorbyl palmitate. Cancer Res. 47:66336638; 1987.
Chan, J. T.; Black, H. S. The mitigating effect of dietary
antioxidants on chemically-induced carcinogenesis. Experientia 34:110-111; 1978.
Wilt, S.; Pereira, M.; Couri, D. Selenium effect on initiation
and promotion of tumors by benzo(a)pyrene and 12-0-tetradecanoylphorbol-13-acetate. Proc. Am. Assoc. Cancer Res.
20:21: 1979.
Watson, R. R.; Moriguchi, S.; Gensler, H. L. Effects of dietary
retinyl palmitate and selenium on tumoricidal capacity of macrophages in mice undergoing tumor promotion. Cancer Lett.
36:181-187; 1987.
Solanki, V.; Yotti, L.; Logani, M. K.; Slaga, T. J. The
reduction of tumor initiating activity and cell mediated
mutagenicity of dimethylbenz[a]anthracene by a copper coordination compound. Carcinogenesis 5:129-131 ; 1984.
Chang, R. L.; Huang, M.-T.; Wood, A. W.; Wong, C.-Q.;
Newmark, H. L.; Yagi, H.; Sayer, J. M.; Jerina, D. M.; Conhey, A. H. Effect of ellagic acid and hydroxylated flavonoids
on the tumorigenicity of benzo[a]pyrene and (+-)-7[3,8o~-dihydroxy-9a, 10s-epoxy, 7,8,9,10-tetrahydrobenzo[a]pyrene
on mouse skin and in the newborn mouse. Carcinogenesis
6:1127-1133; 1985.
Kato, R.; Nakadate, T.; Yamamoto, S.; Sugimura, T. Inhibition of 12-0-tetradecanoylphorbol- 13-acetate-induced tumor
promotion and ornithine decarboxylase activity by quercetin:
250.
251.
252.
253.
254.
255.
256.
257.
258.
259.
260.
261.
262.
263.
264.
265.
266.
267.
268.
405
possible involvement of lipoxygenase inhibition. Carcinogenesis 4:1301-1305; 1983.
Sadhana, A. S.; Rao, A. R.; Kucheria, K.; Bijani, V. Inhibitory action of garlic oil on the initiation of benzo[a]pyreneinduced skin carcinogenesis in mice. Cancer Lett. 40:193197; 1988.
Belman, S. Onion and garlic oils inhibit tumor promotion.
Carcinogenesis 4:1063-1065; 1983.
Belman, S.; Block, E.; Perchellet, J. P.; Perchellet, E. M.;
Fischer, S. M. Onion and garlic oils inhibit promotion whereas
the oils enhance the conversion of papillomas to carcinomas.
These agents inhibit lipoxygenase and ornithine decarboxylase.
Proc. Am. Assoc. Cancer Res. 28:166; 1987.
Fischer, S. M.; FiJrstenberger, G.; Marks, F.; Slaga, T. J.
Events associated with mouse skin tumor promotion with respect to arachidonic acid metabolism: a comparison between
SENCAR mice and NMRI mice. Cancer Res. 47:3174-3179;
1987.
Verma, A. K.; Ashendel, C. L.; Boutwell, R. K. Inhibition
by prostaglandin synthesis inhibitors of the induction of epidermal ornithine decarboxylase activity, the accumulation of
prostaglandins, and tumor promotion caused by 12-0-tetradecanoylphorbol- 13-acetate. Cancer Res. 40:308- 315: 1980.
Fischer, S. M.; Gleason, G. L.; Mills, G. D.; Slaga, T. J.
lndomethacin enhancement of TPA tumor promotion in mice.
Cancer Lett. 10:343-350: 1980.
Aizu, E.; Nakadate, T.; Yamamoto, S.; Kato, R. Inhibition of
12-0-tetradecanoylphorbol-13-acetate-mediated epidermal ornithine decarboxylase induction and skin tumor promotion by
new lipoxygenase inhibitors lacking protein kinase C inhibitory
effects. Carcinogenesis 7:1809-1812; 1986.
Dawson, M. l.; Chao, W.-R. Comparison of the inhibitory
effects of retinoids on 12-0-tetradecanoylphorbol-13-acetate
promoted tumor formation in CD-I and SENCAR mice. Cancer Lett. 40:7-12; 1988.
Bo[lag, W. Prophylaxis of chemically induced benign and malignant epithelial tumors by vitamin A acid (retinoic acid).
Europ. J. Cancer 8:689-693; 1972.
Dawson, M. 1.; Chao, W.-R.: Helmes, C. T. Inhibition by
retinoids of anthralin-induced mouse epidermal ornithine decarboxylase activity and anthralin-promoted skin tumor formation. Cancer Res. 47:6210-6215; 1987.
Bollag, W. Therapeutic effects of an aromatic retinoic acid
analog on chemically induced skin papillomas and carcinomas
of mice. Europ. J. Cancer 10:731-737; 1974.
Jacoby W. T.: Weiss, H. S. Inhibition and enhancement of
skin tumors in mice by dimethyl sulfoxide depending on
method of application. J. Natl. Cancer Inst. 77:983-987;
1986.
Verma, A. K. Inhibition of both stage I and stage II mouse
skin tumor promotion by retinoic acid and the dependence of
inhibition of tumor promotion on the duration of retinoic acid
treatment. Cancer Res. 47:5097- 5101 ; 1987.
Gensler, H. L.; Sim, D. A.; Bowden, G. T. Influence of the
duration of topical 13-cis-retinoic acid treatment on inhibition
of mouse skin tumor promotion. Cancer Res. 46:2767-2770;
1986.
Weerapradist, W.; Shklar, G. Vitamin E inhibition of hamster
buccal pouch carcinogenesis. Oral Surg. 54:304-312; 1982.
Shklar, G. Oral mucosal carcinogenesis in hamster: inhibition
by vitamin E. J. Natl. Cancer Inst. 68:791 797; 1982.
Trickier, D.; Shklar, G. Prevention by vitamin E of experimental oral carcinogenesis. J. Natl. Cancer Inst. 78:165-169;
1987.
Dunham, W. B.; Zuckerkandl, E.; Reynolds, R.; Willoughby,
R.; Marcuson, R.; Barth, R.; Pauling, L. Effects of intake of
L-ascorbic acid on the incidence of dermal neoplasms induced
by ultraviolet light. Proc. Natl. Acad. Sci. USA 79:7532-7536;
1982.
Black, H. S. Effects of dietary antioxidants on active tumor
induction. Res. Commun. Chem. Pathol. Pharmacol. 7:783786; 1974.
406
J.-P. PERCHELLETand E. M. PERCHELLET
269. Overvad, K.; Thorling, E. B.; Bjerring, P.; Ebbesen, P. Selenium inhibits UV-light-induced skin carcinogenesis in hairless mice. Cancer Lett. 27:163-170; 1985.
270. Mukhtar, H.; Das, M.: Del Tito, B. J.; Bickers, D. R. Protection against 3-methylcholanthrene-induced skin tumorigenesis in BALB/c mice by ellagic acid. Biochem. Bioph3s.
Res. Commun. 119:751-757; 1984.
271. Mukhtar, H.; Das, M.; Bickers, D. R. Inhibition of 3-methylcholanthrene-induced skin tumorigenicity in BALB/c mice
by chronic oral feeding of trace amounts of ellagic acid in
drinking water. Cancer Res. 46:2262-2265; 1986.
272. Niukina, K.: Schwartz, J.; Shklar, G. Effects of onion extract
on the development of hamster buccal pouch carcinomas as
expressed in tumor burden. Nutr. Cancer 9:171-176: 1987.
273. Shklar, G.; Marefat, R; Kornhauser, A.; Trickier, D. P.; Wallace, K. D. Retinoid inhibition of lingual carcinogenesis. Oral
Surg. 49:325-332; 1980.
274. Shklar, G.; Schwartz, J.; Grau, D.; Trickier, D. P.: Wallace,
K. D. Inhibition of hamster buccal pouch carcinogenesis by
13-cis-retinoic acid. Oral Surg. 50:45-52; 1980.
275. DeLong, M. J.; Prochaska, H. J.; Talalay, P. Substituted phenols as inducers of enzymes that inactivate electrophilic compounds. In: McBrien, D. C.; Slater, T. F., eds. Protective
agents in human and experimental cancer. London: Academic
Press: 1983:175-196.
276. Woolley, P. V.; Kumar, S.; Fitzgerald, P.: Simpson, R. T.
Ascorbate potentiates DNA damage by l-methyl-I-nitrosourea
in vivo and generates DNA strand breaks in vitro. Carcinogenesis 8:1657-1662; 1987.
277. Mimnaugh, E. G.; Trush, M. A.; Bhamagar, M.; Gram, T.
E. Enhancement of reactive oxygen-dependent mitochondrial
membrane lipid peroxidation by the anticancer drug adriamycin. Biochem. Pharmacol. 34:847-856; 1985.
278. Mikuni, T.; Tatsuta, M.; Kamachi, M. Scavenging effect of
butylated hydroxytoluene on the production of free radicals by
the reaction of hydrogen peroxide wtih N-methyl-N'-nitro-Nnitrosoguanidine, J. Natl. Cancer Inst. 79:281-283; 1987.
279. Kensler, T. W.; Egner, P. A.; Dolan, P. M.; Groopman, J. D.:
Roebuck, B. D. Mechanism of protection against aflatoxin
tumorigenicity in rats fed 5-(2-pyrazinyl)-4-methyl-l,2-dithiol-3-thione (Oltipraz) and related 1,2-dithiol-3-thiones and
1,2-dithiol-3-ones. Cancer Res. 47:4271-4277:1987.
280. Benson, A. M.; Batzinger, R. P.; Ou, S,-Y. L.; Bueding, E.:
Cha, Y.-N.: Talalay, P. Elevation of hepatic glutathione Stransferase activities and protection against mutagenic metabolites of benzo[a]pyrene by dietary antioxidants. Cancer Res.
38:4486-4495; 1978.
281. Reiners, J. J.; Brott, E.; Sorenson, J. R. J. Inhibition of
benzo[a]pyrene-dependent mutagenesis and cytochrome P-450
reductase activity by copper complexes. Carcinogenesis
7:1729-1732; 1986.
282. Rosin, M. P.; Stich, H. F. The inhibitory effect of cysteine on
the mutagenic activities of several carcinogens. Mutat. Res.
54:73-81; 1978.
283. Hesse, S.: Hernstr6m, B.; Martinez, M.: Moldeus, P.: Christodoulides, L.; Ketterer, B. Inactivation of DNA-binding
metabolites of benzo[a]pyrene and benzo[a]pyrene-7,8-dihydrodiol by glutathione and glutathione S-transferases. Carcinogenesis 3:757-760: 1982.
284. Recio, L.; Hsie, A. W. Modulation of the cytotoxicity and
mutagenicity of benzo[a]pyrene and benzo[a]pyrene 7,8-diol
by glutathione and glutathione S-transferases in mammalian
cells (CHO/HGPRT assay). Mutat. Res. 178:257 269; 1987.
285. Wargovich, M. J. Diallyl sulfide, a flavor component of garlic
(Allium sativum), inhibits dimethylhydrazine-induced colon
cancer. Carcinogenesis 8:487-489; 1987.
286. Schallreuter, K. U.; Wood, J. M. The role of thioredoxin
reductase in the reduction of free radicals at the surface of the
epidermis. Biochem. Biophys. Res. Commun. 136:630-637;
1986.
287. Chan, J. Y. H.; Ruchirawat, M.; Lapeyre, J.-N.: Becker, F.
F. The protective role of thiol reducing agents in the in vitro
288.
289.
290.
291.
292.
293.
294.
295.
296.
297.
298.
299.
300.
301.
302.
303.
304.
305.
306.
307.
inhibition of rat liver DNA methylase by direct acting carcinogens. Carcinogenesis 4:1097-1100; 1983.
Bartoli, G. M.; Mfiller, A.; Cadenas. E.; Sies, H. Antioxidant
effect of diethyldithiocarbamate on microsomal lipid peroxidation assessed by low-level chemiluminescence and alkane
production. FEBS Lett. 164:371-374: 1983.
Heikkila, R. D.; Cabbat, F. S.; Cohen, G. In vivo inhibition
of superoxide dismutase in mice by diethyldithiocarbamate. J.
Biol. Chem. 251:2182 2185: 1976.
Mansour, H.: Levacher, M.; Gougerot-Pocidalo, M. A.; Rouveix, B.; Pocidalo, J. J. Diethyldithiocarbamate provides partial protection against pulmonary and lymphoid oxygen
toxicity. J. Pharmacol. Exp. 236:476-480; 1986.
Kumar, K. S.: Sancho, A. M.: Weiss, J. F. A novel interaction
of diethyldithiocarbamate with the glutathione/glutathione
peroxidase system. Int. J. Radiat. OncoL Phys. 12:14631467: 1986.
Novi, A. M. Regression of aflatoxin B~-induced hepatocellular
carcinomas by reduced glutathione. Science 212:541 542:
1981.
Glatt, H : Protid-Sablji~, M.; Oesch, F. Mutagenicity o1" glutathione and cysteine in the Ames test. Science 220:961-963:
1983.
Cook, J. R.: Huang, D. P.: Burkhardt, A. L.; Goldman, M.
E.; Carroll, M.; Bresnick, E.; Chiu, J. F. assessment of the
anti-tumor potential of glutathione. Cancer Lett. 21:277-283:
1984.
Stark, A.-A.; Zeiger, E.; Pagano, D. A. Glutathione nmtagenesis in Salmonella typhimurium is a 5'-glutamyltranspeptidase-enhanced process involving active oxygen species.
Carcinogenesis 9:771-777: 1988.
Vernie, L. N. Selenium in carcinogenesis. Biochim. Biophys.
Acta 738:203-217: 1984.
Ip. C. Selenium inhibition of chemical carcinogenesis. Fed.
Proe. 44:2573-2578; 1985.
Horvath, P. M.; lp, C. Synergistic effect of vitamin E and
selenium in the chemoprevention of mammary carcinogenesis
in rats. Cancer Res. 43:5335-5341: 1983.
Hoekstra, W. G. Biochemical function of selenium and its
relation to vitamin E. Fed. Proc. 34:2083 2089: 1975.
Zee-Cheng, R. K. Y.: Cheng, C. C. Ellagic acid. Drugs Of the
Future 11:1029-1033: 1986.
Del Tito, B. J.; Mukhtar, H.: Bickers, D. R. Inhibition of
epidermal metabolism and DNA-binding of benzo(a)pyrene by
ellagic acid. Biochem. Biophys. Res. Commun. 114:388-394:
1984.
Mukhtar, H.:DelTito, B.J.:Marcelo, C. L.;Das. M.:Bickers, D. Etlagic acid: a potent naturally occurring inhibitor of
benzo(a)pyrene metabolism and its subsequent glucuronidation, sulfation and covalent binding to DNA in cultured BALB/
c mouse keratinocytes. Carcinogenesis 5:1565 1572; 1984.
Teel, R. W.; Martin, R. M.: Allahyari, R. Ellagic acid metabolism and binding to DNA in organ explant cultures of the
rat. Cancer Lett. 36:203-211: 1987.
Wood, A. W.; Huang, M. T.; Chang, R. L.: Newmark, H. L.:
Lehr, R. E.: Yagi, H.; Sayer, J. M.; Jerina, D. M.; Conney,
A. H. Inhibition of the mutagenicity of bay-region diol epoxides of polycyclic aromatic hydrocarbons by naturally occurring plant phenols: exceptional activity of ellagic acid. Proc.
Natl. Acad. Sci. USA 79:5513 5517: 1982.
Verma, A. K.; Rice, H. M.: Shapas, B. G.; Boutwell, R. K.
Inhibition of 12-0-tetradecanoylphorbol-13-acetate-induced
ornithine decarboxylase activity in mouse epidermis by vitamin
A analogs (retinoids). Cancer Res. 38:793- 801 : 1978.
Dennert, G.; Lotan, R. Effects of retinoic acid on the immune
system: stimulation of T killer cell induction. Europ. J. Immunol. 8:23-29; 1978.
Slaga, T. J.; Klein-Szanto, A. J. P.; Fischer, S. M.: Weeks.
C. E.: Nelson, K.; Mayor, S. Studies on mechanism of action
of antitumor-promoting agents: their specificity in two-stage
tumor promotion. Proc. Natl. Acad. Sci. USA 77:2251-2254:
1980.
Antioxidants and skin carcinogenesis
308. Goldstein, B. D.; Witz, G.; Amoruso, M.; Troll, W. Protease
inhibitors antagonize the activation of polymorphonuclear leukocyte oxygen consumption. Biochem. Biophys. Res. Commun. 88:854-860; 1979.
309. Yavelow, J.; Gidlund, M.; Troll, W. Protease inhibitors from
processed legumes effectively inhibit superoxide generation
response to TPA. Carcinogenesis 3:135-138; 1982.
310. Fischer, S. M.; Baldwin, J. K.; Adams, L. M. Effects of antipromoters and strain of mouse on tumor promoter-induced
oxidants in murine epidermal cells. Carcinogenesis 7:915918; 1986.
311. Frenkel, K.; Chrzan, K.; Ryan, C. A.; Wiesner, R.; Troll, W.
Chymotrypsin-specific protease inhibitors decrease H_,O, formation by activated human polymorphonuclear leukocytes.
Carcinogenesis 8:1207 1212; 1987.
312. Abramovitz, A. S.; Yavelow, J.; Randolph, V.; Troll, W. Inhibition of superoxide production in human neutrophils by
purified soybean polypeptides. J. Biol. Chem. 258:1515315157; 1983.
313. Fischer, S. M. ; Adams, L. M. Suppression of tumor promoterinduced chemiluminescence in mouse epidermal cells by several inhibitors of arachidonic acid metabolism. Cancer. Res.
45:3130-3136; 1985.
314. Gescher, A.: Brodie, A. E.; Reed. D. J. Oxidative properties
of 12-0-tetradecanoylphorbol-13-acetate-stimulated human
blood monomorphonuclear leukocytes and their toxicity
against a human lung carcinoma cell line. Cancer Res.
45:1638-1643; 1985.
315. Kozumbo, W. J.; Trush, M. A.: Kensler, T. W. Are free radicals involved in tumor promotion? Chem.-Biol. Interact.
54:199-207; 1985.
316. Witz, G.; Goldstein, B. D.; Amoruso, M.; Stone, D. S.; Troll,
W. Retinoid inhibition of superoxide anion radical production
by human polymorphonuclear leukocytes stimulated with tumor promoters. Biochem. Biophys. Res. Commun. 97:883888; 1980.
317. Kensler, T. W.; Trush, M. A. Inhibition of phorbol esterstimulated chemiluminescence in human polymorphonuclear
leukocytes by retinoic acid and 5,6-epoxyretinoic acid. Cancer
Res. 41:216-222; 1981.
318. Whitcomb, J. M.; Schwartz, A. G. Dehydroepiandrosterone
and 16c~-Br-epiandrosterone inhibit 12-0-tetradecanoylphorbol-13-acetate stimulation of superoxide radical production by
human polymorphonuclear leukocytes. Carcinogenesis 6:333335; 1985.
319. Pascale, R.; Garcea, R.; Ruggiu, M. E.; Daino, L.; Frassetto,
S.; Vannini, M. G.; Cozzolino, P.; Lenzerini, L." Feo, F.;
Schwartz, A. G. Decreased stimulation by 12-0-tetradecanoylphorbol-13-acetate of superoxide radical production by
polymorphonuclear leukocytes carrying the Mediterranean
variant of glucose-6-phosphate dehydrogenase. Carcinogenesis 8:1567-1570; 1987.
320. Machlin, L. J.; Bendich, A. Free radical tissue damage: protective role of antioxidant nutrients. FASEB J. 1:441-445;
1987.
321. Armato, U.; Andreis, P. G.; Romano, F. Exogenous Cu, Znsuperoxide dismutase suppresses the stimulation of neonatal
rat hepatocytes' growth by tumor promoters. Carcinogenesis
5:1547-1555; 1984.
322. Borek, C.; Troll, W. Modifiers of free radicals inhibit in vitro
the oncogenic actions of X-rays, bleomycin, and the tumor
promoter 12-0-tetradecanoylphorbol-13-acetate. Proc. Natl.
Acad. Sci. USA 80:1304-1307; 1983.
323. Nakamura, Y.; Colburn, N. H.; Gindhart, T. D. Role of reactive oxygen in tumor promotion: implication of superoxide
anion in promotion of neoplastic transformation in JB-6 cells
by TPA. Carcinogenesis 6:229-235; 1985.
324. Saito, M.; Tanaka, N.; Ohkawa, Y.; Inui, N. Inhibition of 120-tetradecanoylphorbol- 13-acetate-enhanced transformation in
vitro by radical scavengers. Cancer Lett. 35:167-171 ; 1987.
325. Novogrodsky, A.; Patya, M.; Rubin, A. L.; Stenzel, K. H.
Inhibition of 13-adrenergic stimulation of lymphocyte adenylate
326.
327.
328.
329.
330.
331.
332.
333.
334.
335.
336.
337.
407
cyclase by phorbol myristate acetate is mediated by activated
macrophages. Biochem. Biophys. Res. Commun. 104:389393; 1982.
Saito, M.; Ohkawa, Y.; Inui, N. Retinoic acid and butylated
hydroxyanisole inhibit promoter-enhanced transformation in
vitro. Cancer Lett. 33:161-165; 1986.
Kozumbo, W. J.; Seed, J. L.; Kensler, T. W. Inhibition by
2(3)-tert-butyl-4-hydroxyanisole and other antioxidants of epidermal ornithine decarboxylase activity induced by 12-0-tetradecanoylphorbol-13-acetate. Cancer Res. 43:2555-2559;
1983.
Birt, D. F.; Walker, B.; Tibbels, M. G.; Bresnick, E. Antimutagenesis and anti-promotion by apigenin, robinetin and
indole-3-carbinol. Carcinogenesis 7:959-963; 1986.
Baxter, C. S.; Lawrence, A. T. Specific inhibition of phorbol
diester-induced granulocyte-macrophage progenitor cell (GMCFU) differentiation by lipoxygenase inhibitors. Cancer Lett.
37:251-256; 1987.
Ohuchi, K.; Levine, L. a-Tocopherol inhibits 12-0-tetradecanoylphorbol-13-acetate-stimulated deacylation of cellular
lipids, prostaglandin production, and changes in cell morphology of Madin-Darby canine kidney cells. Biochim. Binphys. Acta 619:11-19; 1980.
Nakadate, T.; Yamamoto, S.; Ishii, M.; Kato, R. Inhibition
of 12-0-tetradecanoylphorbol-13-acetate-induced epidermal
ornithine decarboxylase activity by lipoxygenase inhibitors:
possible role of product(s) of lipoxygenase pathway. Carcinogenesis 3:1411-1414; 1982.
Uzumaki, H.; Yamamoto, S.; Kato, R. Effects of lipoxygenase
and cyclooxygenase inhibitors on the induction of ornithine
decarboxylase by 12-0-tetradecanoylphorbol-13-acetate and isoproterenol in mouse tissues in vivo. Carcinogenesis 7:289294; 1986.
Kumar, S.; Antony, M.; Mehrotra, N. K. Oxidized glutathione
reductase activity in mouse epidermis: TPA-induced change
and its modulation by vitamin A. Biochem. Biophys. Res.
Commun. 125:967-973; 1984.
Belman, S. Inhibition of soybean lipoxygenase by onion and
garlic oil constituents. Proc. Am. Assoc. Cancer Res. 26:231 ;
1985.
Logani, M. K.; Sambuco, C. P.; Forbes, P. D.; Davies, R. E.
Skin-tumor promoting activity of methyl ethyl ketone peroxide--a potent lipid-peroxidizing agent. Food Chem. Toxicol.
22:879-882; 1984.
Rotstein, J.B.; Slaga, T. J. Effect of exogenous glutathione
on tumor progression in the murine skin multistage carcinogenesis model. Carcinogenesis 9:1547-1551 ; 1988.
Ruch, R. J.; Klaunig, J. E. Antioxidant prevention of tumor
promoter induced inhibition of mouse hepatocyte intercellular
communication. Cancer Lett. 33:137-150; 1986.
ABBREVIATIONS
ROS--Reactive
Pa--Papilloma
Ca--Carcinoma
oxygen species
PAH--Polycyclic aromatic hydrocarbon
DMBA--7,12-Dimethylbenz[a]anthracene
TPA-- 12-0-Tetradecanoylphorbol- ! 3-acetate
MEZ--Mezerein
PKC--Protein kinase C
BPx--Benzoyi peroxide
PG--Prostaglandin
ODC--Ornithine
decarboxylase
EPP--Ethyl phenylpropiolate
408
J.-P. PERCHELLETand E. M. PERCHELLET
MNNG--Methyl-3-nitro- 1-nitrosoguanidine
ENU--Ethylnitrosourea
GSH--Reduced glutathione
GSSG--Oxidized glutathione
GSSG-R--Glutathione reductase
RA--Retinoic acid (vitamin A)
BrMBA--7-Bromomethylbenz[a]anthracene
SOD--Superoxide dismutase
CAT--Catalase
oLTH--c~-Tocopherol (vitamin E)
CuDIPS--Cu(II)-(3,5-diisopropylsalicylate)2
AHH--Aryl hydrocarbon hydroxylase
PMN--Polymorphonuclear
BP--Benzo[a]pyrene
MC--Methylcholanthrene
DMSO--Dimethyl sulfoxide
DEM--Diethyl maleate
CL--Chemiluminescence
CDNB--1-Chloro-2,4-dinitrobenzene
G/GO/Glucose/glucose oxidase
X / XO--Xanthine / xanthine oxidase
ASC--Ascorbic acid (vitamin C)
XD--Xanthine dehydrogenase
BHA--Butylated hydroxyanisole
BHT--Butylated hydroxytoluene
Cys--L-cysteine
DDTC--Diethyldithiocarbamate
HPETE/HETE--Hydroperoxy- / hydroxy -eicosatetraenoic acid
ADR--Adriamycin (doxorubicin)
You might also like
- First Tier Icp Agreement: BetweenDocument2 pagesFirst Tier Icp Agreement: BetweenaribniminnakNo ratings yet
- Chap 07 ControlDocument6 pagesChap 07 ControlaribniminnakNo ratings yet
- Topic3 Periodic TableDocument66 pagesTopic3 Periodic TableNana SazanaNo ratings yet
- NDU Referee Report FormDocument2 pagesNDU Referee Report FormaribniminnakNo ratings yet
- SBP 3114-Salivary SecretionDocument3 pagesSBP 3114-Salivary SecretionaribniminnakNo ratings yet
- Journal Free With Good IntegrityDocument2 pagesJournal Free With Good IntegrityaribniminnakNo ratings yet
- 1way ANOVA of Data 1Document1 page1way ANOVA of Data 1aribniminnakNo ratings yet
- Salt 2Document3 pagesSalt 2Sulaiman MohamadNo ratings yet
- Formula KimiaDocument1 pageFormula KimiaShamshul DidarellyNo ratings yet
- Periodic TableDocument8 pagesPeriodic TableKhairiyah AbdullahNo ratings yet
- QPCR Optimization 2011.unlockedDocument22 pagesQPCR Optimization 2011.unlockedaribniminnakNo ratings yet
- Teaching Plan SBP3112 Semester 1 2013-2014Document4 pagesTeaching Plan SBP3112 Semester 1 2013-2014aribniminnakNo ratings yet
- 25 ChemopreventionDocument19 pages25 ChemopreventionaribniminnakNo ratings yet
- 29 Identifying The Cellular Origin of Squamous Skin TumorsDocument6 pages29 Identifying The Cellular Origin of Squamous Skin TumorsaribniminnakNo ratings yet
- 76 Antitumor-Promoting Effects of Cyclic Diarylheptanoids On Epstein Barr Virus Activation and Two Stage Mouse Skin CarcinogenesisDocument6 pages76 Antitumor-Promoting Effects of Cyclic Diarylheptanoids On Epstein Barr Virus Activation and Two Stage Mouse Skin CarcinogenesisaribniminnakNo ratings yet
- Year 2 Pupil Conversation Topics and InstructionsDocument9 pagesYear 2 Pupil Conversation Topics and InstructionsaribniminnakNo ratings yet
- Ace To Genin As Natural EsDocument31 pagesAce To Genin As Natural EsNathaly Jiménez DíazNo ratings yet
- 38 Bullatacin, A Potent Antitumor Annonaceous Acetogenin, Induces Apoptosis Through A Reduction of Intracellular CAMP and CGMP Levels in Human Hepatoma 2.2.15 CellsDocument9 pages38 Bullatacin, A Potent Antitumor Annonaceous Acetogenin, Induces Apoptosis Through A Reduction of Intracellular CAMP and CGMP Levels in Human Hepatoma 2.2.15 CellsaribniminnakNo ratings yet
- Tox 26 293Document7 pagesTox 26 293aribniminnakNo ratings yet
- 26 Mechanisms of Inhibitors of Mutagenesis and CarcinogenesisDocument8 pages26 Mechanisms of Inhibitors of Mutagenesis and CarcinogenesisaribniminnakNo ratings yet
- 23 A Collaborative Methodology For Developing A Semantic Model For Interlinking Cancer Chemoprevention Linked Data SourcesDocument18 pages23 A Collaborative Methodology For Developing A Semantic Model For Interlinking Cancer Chemoprevention Linked Data SourcesaribniminnakNo ratings yet
- 30 The Malignant Conversion Step of Mouse Skin CarcinogenesisDocument3 pages30 The Malignant Conversion Step of Mouse Skin CarcinogenesisaribniminnakNo ratings yet
- 29 Identifying The Cellular Origin of Squamous Skin TumorsDocument6 pages29 Identifying The Cellular Origin of Squamous Skin TumorsaribniminnakNo ratings yet
- Group Band Four Picnic OutingDocument6 pagesGroup Band Four Picnic OutingaribniminnakNo ratings yet
- 37 Bullatacin SintesisDocument4 pages37 Bullatacin SintesisaribniminnakNo ratings yet
- Teacher's Classroom Activities to Improve Students' Communication SkillsDocument7 pagesTeacher's Classroom Activities to Improve Students' Communication SkillsaribniminnakNo ratings yet
- Adjuvant PeDocument1 pageAdjuvant PeAlexandru IacobanNo ratings yet
- Hello, Hello My Dear Friend, My Dear Friend, My Dear Friend, Hello, Hello My Dear FriendDocument14 pagesHello, Hello My Dear Friend, My Dear Friend, My Dear Friend, Hello, Hello My Dear FriendaribniminnakNo ratings yet
- Cover Manual - Sbp3105Document1 pageCover Manual - Sbp3105aribniminnakNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Chicken LiverDocument10 pagesChicken LiverZoran MiladinovićNo ratings yet
- Factors Determining Lion Mane Growth & ColourDocument8 pagesFactors Determining Lion Mane Growth & ColourDonné KrugerNo ratings yet
- Jim LaValle - Atlanta PresentationDocument222 pagesJim LaValle - Atlanta Presentationtquint23100% (1)
- Oxidative Stress and AntioxidantsDocument34 pagesOxidative Stress and AntioxidantsTauseefNo ratings yet
- RawTruth FinalDocument109 pagesRawTruth Finalsk_1000100% (1)
- Effects of food preservative sodium benzoate on memory and oxidative stressDocument8 pagesEffects of food preservative sodium benzoate on memory and oxidative stressBenson Ha.No ratings yet
- Antiox FullDocument456 pagesAntiox FullRida FaragNo ratings yet
- Topical and Oral Melatonin for Melasma ManagementDocument15 pagesTopical and Oral Melatonin for Melasma ManagementdeswitrigintaNo ratings yet
- Calendula Officinalis Scientific PaperDocument15 pagesCalendula Officinalis Scientific PaperBekaNo ratings yet
- Biological Activities of Curcuminoids, Other Biomolecules From Turmeric and Their Derivatives e A ReviewDocument29 pagesBiological Activities of Curcuminoids, Other Biomolecules From Turmeric and Their Derivatives e A ReviewRigotti BrNo ratings yet
- Metabolism of XenobioticsDocument5 pagesMetabolism of XenobioticsJanelle Bondad100% (2)
- Aktivitas Antioksidan SeldriDocument6 pagesAktivitas Antioksidan SeldriAbeiasaNo ratings yet
- Appendices FinalDocument44 pagesAppendices FinalSurya PrakashNo ratings yet
- 39 Austrian Chemistry OlympiadDocument27 pages39 Austrian Chemistry OlympiadsyavinaNo ratings yet
- Studies On The Metabolism of A Triptolide Derivative (5R) - 5-Hydroxytriptolide in VitroDocument9 pagesStudies On The Metabolism of A Triptolide Derivative (5R) - 5-Hydroxytriptolide in Vitroxiaoming wangNo ratings yet
- J. Biol. Chem.-1988-Meister-17205-8Document4 pagesJ. Biol. Chem.-1988-Meister-17205-8Pepé DubNo ratings yet
- Science of The Total EnvironmentDocument16 pagesScience of The Total Environmentadelia rajagukgukNo ratings yet
- Mechanisms of Drug-Induced HepatotoxicityDocument20 pagesMechanisms of Drug-Induced Hepatotoxicityfebri kusuma arfiskaNo ratings yet
- Toxicophores: Groups and Metabolic Routes Associated With Increased Safety RiskDocument13 pagesToxicophores: Groups and Metabolic Routes Associated With Increased Safety RiskMercedes ArmijosNo ratings yet
- Review Article Pharmacological Actions and Potential Uses of TrigonellaDocument10 pagesReview Article Pharmacological Actions and Potential Uses of Trigonellavinayguru82No ratings yet
- Synthesis and Antifilarial Evaluation of N, N - Xylofuranosylated DiaminoalkanesDocument12 pagesSynthesis and Antifilarial Evaluation of N, N - Xylofuranosylated DiaminoalkanesRumana AhmadNo ratings yet
- Xenobiotic MetabolismDocument64 pagesXenobiotic MetabolismBelajar dan berdoaNo ratings yet
- Intracellular AccumulationDocument38 pagesIntracellular AccumulationElena PoriazovaNo ratings yet
- Hepatoprotective Activity A Review PharmatutorDocument11 pagesHepatoprotective Activity A Review PharmatutorAbhipsa SinhaNo ratings yet
- Jurnal Bentuk Dan Dampak Senyawa Partikel Dalam Batu Bara PDFDocument10 pagesJurnal Bentuk Dan Dampak Senyawa Partikel Dalam Batu Bara PDFsinarNo ratings yet
- Detoxification Therapeutics For Heavy Metals, Toxic Chemicals and Other NeurotoxinsDocument175 pagesDetoxification Therapeutics For Heavy Metals, Toxic Chemicals and Other Neurotoxins300r100% (9)
- Tips For Detoxing MercuryDocument11 pagesTips For Detoxing Mercurya100% (1)
- Ascorbic Acid in Plant Growth, Development and Stress Tolerance PDFDocument514 pagesAscorbic Acid in Plant Growth, Development and Stress Tolerance PDFmalin.oloier100% (1)
- To Optimize Mitochondria: 22 Natural WaysDocument26 pagesTo Optimize Mitochondria: 22 Natural Waysreyshme100% (11)
- Pro-Oxidant Strategies - Cancer Treatments ResearchDocument71 pagesPro-Oxidant Strategies - Cancer Treatments ResearchSpore FluxNo ratings yet