Professional Documents
Culture Documents
584348
Uploaded by
Vicra AdhityaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
584348
Uploaded by
Vicra AdhityaCopyright:
Available Formats
TEVA UK Ref:
231-30-62606-Z LEA GLIBENCLAMIDE 2.5MG AND 5MG TAB TUK
Version:
26 March 2015
PAGE 1: FRONT FACE (INSIDE OF REEL)
PACKAGE LEAFLET: INFORMATION
FOR THE USER
Read all of this leaflet carefully before you
start taking this medicine because it contains
important information for you.
Keep this leaflet. You may need to read it
again.
If you have any further questions, ask your
doctor or pharmacist.
This medicine has been prescribed for you.
Do not pass it on to others. It may harm
them, even if their symptoms are the same
as yours.
If you get any side effects, talk to your doctor
or pharmacist. This includes any possible
side effects not listed in this leaflet. See
section 4.
IN THIS LEAFLET:
Pharma code 154
1. What Glibenclamide is and what it is used for
2. What you need to know before you take
Glibenclamide
3. How to take Glibenclamide
4. Possible side effects
5. How to store Glibenclamide
6. Contents of pack and other information
WHAT GLIBENCLAMIDE IS AND WHAT
IT IS USED FOR
Glibenclamide is an anti-diabetic drug.
Glibenclamide tablets are used in the
management of non-insulin dependent
diabetes to lower the level of sugar in the
blood. They are used in cases where diet alone
does not provide sufficient control.
BEFORE YOU TAKE GLIBENCLAMIDE
Do NOT take Glibenclamide if you:
are allergic (hypersensitive) to Glibenclamide
or any of the other ingredients of this medicine
have a serious problems with your kidneys,
liver, adrenal glands or pituitary gland
are about to undergo any form of surgery
have a severe infection
have porphyria (Symptoms you may feel are
like abdominal pain, mental confusion,
anxiety, fits, muscle pain etc.)
have juvenile or insulin-dependent diabetes
are in trauma or suffering from stress.
suffering from a history of diabetic
ketoacidosis (presence of ketones in the
urine) or diabetic coma or pre-coma.
are elderly (Age over 70 years).
These tablets should not be used in patients
suffering from or with a history of diabetic
ketoacidosis (presence of ketones in the urine)
or diabetic coma.
Warnings and precautions
Talk to your doctor before you start to take this
medicine if you:
are weak or feeble as you are more likely to
suffer from a hypo (low blood-sugar attack)
have a controlled diet or you take less
calorie food or glucose
have irregular meal time or you miss your
meals often
are doing excessive exercise
If you have G6PD- deficiency (G6PD is an
enzyme which protects red blood cells in
blood). Please speak to your doctor if you
are not sure about it.
are debilitated.
have lapp lactose deficiency (you are unable
to digest milk or milk product)
have mild to moderate kidney problems.
Other medicines and Glibenclamide
Talk to your doctor if you are taking any of the
following:
laxatives (used for loosening stools)
chloramphenicol, isoniazid (used for the
treatment of bacterial infection)
tetracycline antibiotics e.g. doxycycline
quinolone antibacterials e.g. ciprofloxacin
sulphonamides e.g. co-trimoxazole
miconazole, fluconazole (an anti-fungal drug)
phenylbutazone, azapropazone (a
non-steroidal anti-inflammatory drug)
treatment for psychological disorders, e.g.
chlorpromazine, lithium
antidepressants e.g. fluoxetine or a
monoamine oxidase inhibitor e.g. phenelzine
fenfluramine (an appetite suppressant)
anti-ulcer medicine e.g. ranitidine or cimetidine
diuretics (water tablets) e.g. furosemide or
amiloride
anabolic steroids e.g. nandrolone or
stanozolol
corticosteroids e.g. cortisone or prednisolone
oral contraceptives (the Pill)
sex hormone for the treatment purpose e.g.
testosterone, oestrogens, progesterones
regular doses of aspirin
phenylbutazone (used to treat pain, fever
and inflammation of the body)
ACE inhibitors (used to treat high blood
pressure and heart failure) e.g. captopril or
enalapril
anti-coagulants e.g. warfarin or heparin
disopyramide (used to treat irregular heart
rhythms)
clofibrate, nicotinic acid and bezafibrate (all
used to lower fat levels in the blood)
sulfinpyrazone, allopurinol, probenecid
(used to treat gout)
phenytoin (an anti-convulsant)
rifampicin (an anti-tuberculosis drug)
cyclophosphamide (an anti-cancer drug)
bronchodilators (for asthma treatment) e.g.
salbutamol
thyroid hormone treatment
diazoxide or glucagon (used to treat
hypoglycaemia).
bosentan (used to treat high blood pressure)
crisantaspase (used to treat cancer)
alcohol
quinine, quinidine (used to treat malaria)
clofibrate (used to treat blood cholesterol)
cyclosporin (used to suppress immune
system).
If you are taking clonidine or guanethidine
(used to reduce high blood pressure), or a
beta-blocker, e.g. propranolol, you should be
aware that these drugs may affect the warning
signs of a hypo (low blood sugar attack).
Please tell your doctor or pharmacist if you are
taking or have recently taken any other
medicines, including medicines obtained
without a prescription.
Important information about some of the
ingredients of Glibenclamide
Patients who are intolerant to lactose should
note that Glibenclamide tablets contain a
small amount of lactose. If your doctor has
told you that you have an intolerance to
some sugars, contact your doctor before
taking this medicine.
Pregnancy and breast-feeding
Do NOT use Glibenclamide if you are pregnant
or planning to become pregnant. Speak to
your doctor before taking any medicine.
You should let your doctor know as soon as
possible if you are breast feeding or you want
to start breast-feeding whilst taking these
tablets.
Driving and using machines
If you have jaundice (yellowing of skin and
whites of the eyes) then please discontinue this Glibenclamide is not known to affect your
ability to drive or operate machinery unless
medicine. Speak to your doctor in this case.
you have very low blood sugar which makes
you feel very sick.
Top of page cut-off to middle of registration mark: 44 mm.
GLIBENCLAMIDE
2.5 mg OR 5 mg TABLETS
TEVA UK Ref:
231-30-62606-Z LEA GLIBENCLAMIDE 2.5MG AND 5MG TAB TUK
Version:
PAGE 2: REAR FACE (OUTSIDE OF REEL)
loss of appetite, diarrhoea, feeling sick,
vomiting, burning chest pain that is caused
by stomach acidity, eating disorder
Always take Glibenclamide exactly as your
jaundice (yellowing of skin and whites of the
doctor has told you. You should check with
eyes)
your doctor or pharmacist if you are not sure.
allergic skin reactions, rash, itching or skin
The tablets should be swallowed preferably
sensitivity after light exposure
with a drink of water. The usual dose is:
skin cell death
fever
Adults
The starting dose is 5 mg a day, taken during metallic taste in the mouth
weight gain
or straight after breakfast (or the first main
meal of the day). This may then be adjusted by increased appetite
swelling of limbs due to accumulation of
your doctor, to a maximum of 15 mg a day.
water
Elderly and very frail patients
low sodium concentration in the blood (this
The normal adult starting dose should be
can be detected from a blood test).
reduced to 2.5 mg a day.
You may occasionally suffer from a hypo (low
Changing from another anti-diabetic medicine blood-sugar attack) relating to your dosage, diet
The starting dose is 5 mg to 10 mg a day,
and exercise, during which you may feel faint,
depending on your previous dosage. This
sick and have cold sweats or palpitations. Your
may then be increased by your doctor, to a
doctor will advise you what to do when you
maximum of 15 mg a day.
first start your treatment with Glibenclamide.
If you are changing from metformin to
You may become allergic to other
Glibenclamide, your starting dose will be
sulphonamide drugs, such as co-trimoxazole.
2.5 mg a day and then adjusted as the
metformin treatment stops, to a maximum Rarely, blood disorders may occur, which may
of 15 mg a day. You may occasionally be
be characterised by pallor, fever or chills, sore
required to take both types of medication throat, ulcers in your mouth or throat, unusual
at the same time, but your doctor will
bleeding or unexplained bruising.
advise you of this.
Similarly, if you are changing from insulin Reporting of side effects
treatment to Glibenclamide, your starting If you get any side effects, talk to your doctor
dose will be 5 mg a day and then adjusted or pharmacist. This includes any possible side
effects not listed in this leaflet. You can also
as the insulin treatment stops, to a
report side effects directly via the Yellow Card
maximum of 15 mg daily.
Scheme at: www.mhra.gov.uk/yellowcard
Children
By reporting side effects you can help provide
Glibenclamide is not recommended for use
more information on the safety of this medicine.
in children.
HOW TO TAKE GLIBENCLAMIDE
If you take more Glibenclamide than you
should
If you (or someone else) swallow a lot of the
tablets all together, or if you think a child has
swallowed any of the tablets, contact your
nearest hospital casualty department or your
doctor immediately.
An overdose is likely to cause low blood sugar
characterised by faintness, feeling sick, cold
sweats, and/or palpitations.
Please take this leaflet, any remaining tablets,
and the container with you to the hospital or
doctor so that they know which tablets were
consumed.
If you forget to take Glibenclamide
If you forget to take a tablet, take one as soon
as you remember, unless it is nearly time to
take the next one. Do NOT take a double dose
to make up for a forgotten dose. Take the
remaining doses at the correct time.
If you stop taking Glibenclamide
Do NOT stop taking your medicine without
talking to your doctor first even if you feel
better.
HOW TO STORE GLIBENCLAMIDE
Keep out of the reach and sight of children.
Do not store above 25C. Keep in the original
package or container supplied. Do not transfer
them to another container.
Do not use Glibenclamide after the expiry date
that is stated on the outer packaging. The
expiry date refers to the last day of that month.
Medicines should not be disposed of via
wastewater or household waste. Ask your
pharmacist how to dispose of medicines no
longer required. These measures will help to
protect the environment.
CONTENTS OF THE PACK AND OTHER
INFORMATION
What Glibenclamide tablets contain:
The active ingredient is Glibenclamide.
The other ingredients are lactose anhydrous,
croscarmellose sodium and magnesium
stearate (E572).
What Glibenclamide tablets look like and
contents of the pack:
If you have any further questions on the use of The Glibenclamide 2.5 mg tablets are white,
biconvex tablets. They are engraved 2.5 over
this product, ask your doctor or pharmacist.
3103 on one side and plain on the reverse.
The Glibenclamide 5 mg tablets are white,
4 POSSIBLE SIDE EFFECTS
oval, biconvex tablets. They are engraved 5
breakline 3104 on one side and plain on the
Like all medicines, Glibenclamide can cause
reverse.
side effects, although not everybody gets them.
The product is available in pack sizes of 7, 10,
If the following happens, stop taking the tablets
14, 21, 28, 30, 56, 60, 84, 90, 100, 110, 112, 120,
and tell your doctor immediately or go to the
150, 160, 168, 250, 500, and 1000 tablets.
casualty department at your nearest hospital:
Not all pack sizes may be marketed.
an allergic reaction (swelling of the lips, face
Marketing Authorisation Holder and
or neck leading to severe difficulty in
Manufacturer
breathing; skin rash or hives).
The Marketing Authorisation holder and
This is a very serious but rare side effect. You
company responsible for manufacture is
may need urgent medical attention or
TEVA UK Limited, Eastbourne, BN22 9AG.
hospitalisation.
Rare:
Decrease in blood cells which places
individuals at increased risk of infection.
Unknown:
problems with your vision (at the beginning
of your treatment only)
This leaflet was last revised: March 2015
PL 00289/0047-0048
62606-Z
160 x 323
26 March 2015
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Math Practice For Paramedic StudentsDocument8 pagesMath Practice For Paramedic StudentsGreg Zeitlin50% (2)
- Pharmacology Drug ClassificationDocument4 pagesPharmacology Drug ClassificationRPh Krishna Chandra Jagrit100% (4)
- Clinical Review: Tablet Splitting: A Review of Weight and Content UniformityDocument12 pagesClinical Review: Tablet Splitting: A Review of Weight and Content Uniformitymukesh choudharyNo ratings yet
- Analgesics: Pharmacist Marwan QasimDocument20 pagesAnalgesics: Pharmacist Marwan QasimWaliNo ratings yet
- Ma - Loai Gia Loai - CP DVT Idloait DMT - BytDocument9 pagesMa - Loai Gia Loai - CP DVT Idloait DMT - BytCường PhạmNo ratings yet
- Formulasi Tablet Salut Teofilin Menggunakan Eksipien Koproses Pregelatinisasi Pati Singkong - Metilselulosa Sebagai Bahan PenyalutDocument14 pagesFormulasi Tablet Salut Teofilin Menggunakan Eksipien Koproses Pregelatinisasi Pati Singkong - Metilselulosa Sebagai Bahan PenyalutWira AdjieNo ratings yet
- Current and Future Pharmacological Agents For The Treatment of Back PainDocument6 pagesCurrent and Future Pharmacological Agents For The Treatment of Back Painskola onlajnNo ratings yet
- Company Detail Uttarakhand PDFDocument61 pagesCompany Detail Uttarakhand PDFRahul Chauhan67% (3)
- Paclitaxel Monograph-1 PDFDocument10 pagesPaclitaxel Monograph-1 PDFClaudia TiffanyNo ratings yet
- Antidepressants UpdateDocument24 pagesAntidepressants Updatedrsayis2No ratings yet
- Rational Use of Drugs-IDocument38 pagesRational Use of Drugs-IUmair Mazhar100% (1)
- MyasteniaDocument7 pagesMyastenialmcarmonaNo ratings yet
- Nasal Drug Delivery SystemDocument46 pagesNasal Drug Delivery Systemrat001100% (1)
- Vigorin CapsuleDocument3 pagesVigorin Capsulehk_scribdNo ratings yet
- BAB V FixDocument4 pagesBAB V FixPUSKESMAS CIPATATNo ratings yet
- Regulatory Requirements For Clinical TrialDocument8 pagesRegulatory Requirements For Clinical TrialGyana SahooNo ratings yet
- Opioid Rotation Conversion Learning PackageDocument18 pagesOpioid Rotation Conversion Learning Packagepaul casillasNo ratings yet
- Medication AdministrationDocument3 pagesMedication Administrationqueenzk100% (4)
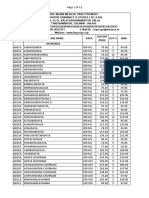
- Impcops Price List 01.09.2018Document33 pagesImpcops Price List 01.09.2018Dawood Batcha0% (1)
- 2011 - Practical Guide Insulin TherapyDocument6 pages2011 - Practical Guide Insulin Therapytheva_thy100% (1)
- Description: Clonidine: Drug Mechanism of Action Indication Contraindication Adverse Effects Nursing ImplicationsDocument2 pagesDescription: Clonidine: Drug Mechanism of Action Indication Contraindication Adverse Effects Nursing ImplicationsThimiNo ratings yet
- Prescription - 1780912 - 12 11 2021 - Dr. Anindya Dutt - Apollo 2471636716100978Document2 pagesPrescription - 1780912 - 12 11 2021 - Dr. Anindya Dutt - Apollo 2471636716100978Debjit GangulyNo ratings yet
- (Escitalopram) : NC CH O N CH C H ODocument2 pages(Escitalopram) : NC CH O N CH C H OKhurram AzizNo ratings yet
- Antifungal Drugs: Anti-Infectives and Anti-Inflammatory: Ncm106 - Pharmacology 2 Semester, AY 2020-2021Document34 pagesAntifungal Drugs: Anti-Infectives and Anti-Inflammatory: Ncm106 - Pharmacology 2 Semester, AY 2020-2021imnas100% (1)
- 7861 - 131060 - 0 - 43116 - Formularium Obat PT - PGM RSPG Group 2018Document149 pages7861 - 131060 - 0 - 43116 - Formularium Obat PT - PGM RSPG Group 2018Miss AmyNo ratings yet
- Part 1 Pharm ModuleDocument49 pagesPart 1 Pharm ModuleJojo JustoNo ratings yet
- LevodopaDocument3 pagesLevodopaderic50% (2)
- InflammatoryDocument20 pagesInflammatoryAS RifathNo ratings yet
- Rationaldruguse 150519185142 Lva1 App6892Document12 pagesRationaldruguse 150519185142 Lva1 App6892nikki_bamsNo ratings yet
- General and Systemic Veterinary PharmacologyDocument97 pagesGeneral and Systemic Veterinary PharmacologyDEV3LLS100% (4)