Professional Documents
Culture Documents
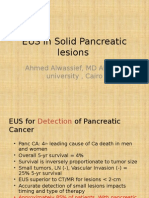
Endoscopic Ultrasound and Early Diagnosis of Pancreatic Cancer
Uploaded by
Achmad Dzulfikar AziziOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endoscopic Ultrasound and Early Diagnosis of Pancreatic Cancer
Uploaded by
Achmad Dzulfikar AziziCopyright:
Available Formats
The American Journal of Surgery 194 (Suppl to October 2007) S87S90
Endoscopic ultrasound and early diagnosis of pancreatic cancer
Lars Helmstaedter, M.D., Juergen Ferdinand Riemann, M.D.*
Department of Medicine C, Klinikum Ludwigshafen, Academic Hospital of the Johannes Gutenberg-University of Mainz, Medical Department C,
Klinikum Ludwigshafen gGmbH, Bremserstrasse 79, D-67063 Ludwigshafen, Germany
Abstract
Incidence of pancreatic cancer has increased, but prognosis remains poor. Curative treatment is
dependent on early diagnosis. Endoscopic ultrasound (EUS) has been described as highly sensitive and
accurate in staging, superior to other imaging modalities in early publications. With rapid advances in
technology, other imaging techniques have reached better results. EUS still has the highest accuracy in
assessing tumor size and lymph node involvement. For assessment of tumor respectability, a combination
of a computed tomography (CT) scan and EUS seems to be the procedure with the highest accuracy.
Promising new techniques might improve the diagnostic yield of EUS. But there are several reasons for
failure, and EUS shows a high interobserver variety. Nevertheless, EUS proved to have a high negative
predictive value. Screening for pancreatic cancer and its precursor lesions in the general population is not
feasible, but high-risk subpopulations could be suitable targets for screening, preferably with an EUS- and
CT-based protocol. 2007 Excerpta Medica Inc. All rights reserved.
Keywords: Pancreatic cancer; Early detection; Endoscopic ultrasound
The incidence of pancreatic cancer has increased continuously over the last decades. Despite rapid improvements in
imaging technologies and therapeutic modalities, the prognosis remains poor. The overall 5-year relative survival rate
for 1996 to 2002 is estimated at 5.0% [1]. If data are
critically reviewed, it seems to be even less. CarpelanHolmstrm et al [2] found a 5-year survival rate for pancreatic ductal adenocarcinoma of 0.2%. At the time of
diagnosis, only 7% of pancreatic cancers are found to be
localized to the organ without locoregional spreading or
distant metastases (American Joint Committee on Cancer
stage I) and therefore resectable in a curative intention.
Even if they are found to be in stage I, the prognosis remains
poor with a 5-year survival rate of 19.6% [1]. These data
underline the importance of early diagnosis of pancreatic
cancer, but pain, jaundice, weight loss, and obstruction
usually are late symptoms.
Endoscopic Ultrasound
One of the most promising imaging techniques to detect
early pancreatic cancers is endoscopic ultrasound (EUS).
This method is able to detect focal lesions as small as 2 to
3 mm with the possibility to get tissue samples by fineneedle aspiration (FNA) or true-cut needle biopsy for his* Corresponding author. Tel.: 49-0621-503-4100; fax: 49-0621503-4114.
E-mail address: ToddMc@baylorhealth.edu
topathological examination. At present, there are 3 fundamental different techniques of EUS available: (1)
electronic or mechanical radial scanning scopes, in which
the electronic scanning scopes seem to produce better
B-mode image quality with no apparent difference in
maneuverability, endurance, and endoscopic images [3];
(2) linear scanning scopes; and (3) radial or linear scanning probes for use with standard scopes or alone. Frequencies range from 5 to 20 MHz for scopes up to 30
MHz for probes. The accuracy in staging of pancreatic
cancer is equivalent for radial and linear scanners [4], in
which radial scanners offer a better overview of surrounding structures (Fig. 1), whereas linear scanners allow the safe execution of tissue sampling. In relation to
pancreatic cancer, indications for EUS are persistent epigastric and/or back pain, acute onset of diabetes in the
elderly, unclarified weight loss, and suspect results in
ultrasonography, especially in individuals over 45 years
of age and in high-risk individuals (eg, persons with a
strong family history of pancreatic cancers, with PeutzJeghers syndrome, or multiple endocrine neoplasia). EUS
is a highly sensitive method, but results for accuracy
differ. Whereas initial studies showed excellent accuracy,
results in later publications declined (Table 1 [511]). If
tissue diagnosis is necessary before therapy, EUS-guided
FNA should be the method of choice. EUS-FNA is highly
sensitive (84%), specific (97%), and accurate (84%) and
has a high positive predictive value (99%) with rare
0002-9610/00/$ see front matter 2007 Excerpta Medica Inc. All rights reserved.
doi:10.1016/j.amjsurg.2007.05.009
S88
L. Helmstaedter and J.F. Riemann / The American Journal of Surgery 194 (Suppl to October 2007) S87S90
single technique. With regard to cost minimization, the
combination of CT and EUS seems to increase the price
compared with each single method. However, if the cost of
unnecessary explorative laparotomies were taken into account, the cost minimization analysis favored a sequential
strategy in which EUS was used as a confirmatory technique
in those patients in whom helical CT suggested resectability
of the tumor [11].
Fig. 1. Endoscopic ultrasound of an adenocarcinoma in the pancreatic head
with a maximum diameter of 4.2 cm.
Table 1
Results for accuracy of EUS in literature
Accuracy (%)
Legmann et al [6], AJR Am J Roentgenol 1998
Akahoshi et al [7], Br J Radiol 1998
Cannon et al [8], Gastrointest Endosc 1999
Ahmad et al [9], Gastrointest Endosc 2000
Meining et al [10], Gut 2002
Soriano et al [11], Am J Gastroenterol 2004
93
94
78
69
72
63
major complications but with a low negative predictive
value of only 64% [12]. If pancreatic cancer is suspected
and if EUS-FNA is negative, cancer cannot be excluded
and operation will be the next step despite positive or
negative FNA.
Comparing EUS
As mentioned earlier, early studies showed high sensitivity and accuracy for EUS. In most studies, EUS was
superior or at least equal to other imaging modalities regarding sensitivity, determining tumor size and extent,
lymph node involvement and vascular infiltration [6,13].
With rapid advances in technology, first of all, computed
tomography (CT) and magnetic resonance imaging (MRI)
have reached better results. Compared with helical CT, MRI
(Fig. 2), and angiography in a prospective study with histopathological or surgical confirmation of results, helical
CT had the highest accuracy in assessing extend of primary
tumor, locoregional extension, vascular invasion, distant
metastasis, tumor TNM stage and tumor resectability,
whereas EUS reached the highest accuracy in assessing
tumor size and lymph node involvement. To predict tumor
resectability, the combination of CT and EUS proved to be
the method with the highest accuracy compared with each
Improving EUS
One of the major problems in diagnosing pancreatic
cancer is the discrimination between focal pancreatitis and
pancreatic cancer. A promising technique seems to be the
contrast-enhanced EUS using perfusion characteristics to
differentiate between focal inflammation and pancreatic
carcinoma. The sensitivity and specificity of conventional EUS were 73.2% and 83.3% for pancreatic carcinoma, increasing to 91.1% and 93.3% with the contrastenhanced power mode [14].
Another major problem for EUS is the assessment of
vascular invasion. Sensitivity and specificity of EUS are
63% and 64% for vascular adherence and 50% and 58% for
vascular invasion [15]. In a pilot study of 22 patients, the
additional 3-dimensional reconstructions appeared to improve the evaluation of vesseltumor relationships, but the
acquisition system needs to be improved [16]. These promising new techniques to improve EUS may enrich the armamentarium for staging pancreatic cancer correctly, but
they need to be evaluated in further studies.
Reasons for failure
EUS is not a foolproof method for detecting pancreatic
neoplasm. It has a high interobserver variety even among
experienced endosonographers [17,18]. In addition, accuracy of EUS seems to be dependent on further clinical and
imaging information [10]. Chronic pancreatitis, diffusely
infiltrating carcinoma, a prominent ventral/ dorsal split, and
a recent episode of acute pancreatitis are also possible
associated factors that may increase the likelihood of a
false-negative EUS examination [19].
Negative predictive value
Normal EUS examination findings seem to have a high
negative predictive value (NPV). In 2 studies with 76 and
135 patients and a mean follow-up period of 23.9 and 25
months, respectively, none of the patients with clinically
indeterminate suspicion of pancreatic cancer and a normal
EUS developed pancreatic cancer [20,21], which means an
NPV of 100%. In contrast, Soriano et al [11] found an NPV
for locoregional extension, lymph node involvement, and
vascular invasion of merely 44%, 65%, and 74% confirmed
by intraoperative or histopathological findings.
Screening for pancreatic cancer
Pancreatic cancer is a disease with a poor overall 5-year
survival rate of 5% [1]. There are reports of a 4-year survival rate of 78% in resected stage 1 ductal adenocarcinomas of the pancreas 2 cm in size, in which 42% were not
associated with symptoms [22]. These data suggest that
screening and early detection of pancreatic neoplasia might
L. Helmstaedter and J.F. Riemann / The American Journal of Surgery 194 (Suppl to October 2007) S87S90
S89
improve the dismal outcome of pancreatic cancer. There are
morphologically well-defined noninvasive precursor lesions
for invasive pancreatic cancer, including pancreatic intraductal neoplasia and intraductal papillary mucinous neoplasms (IPMNs). The treatment of these precursor lesions
might prevent their progression to invasive cancer, as it is
well experienced in other organs. Because of the low incidence of pancreatic cancer and the lack of accurate, inexpensive, and noninvasive diagnostic tests for early disease,
screening for pancreatic cancer and its precursor lesions in
the entire population is not reasonable. But there are some
known high-risk subpopulations, such as members of families with a strong history of pancreatic cancer or with
hereditary pancreatitis and with distinct hereditary cancer
syndromes, such as Peutz-Jeghers syndrome, hereditary
breast or ovarian cancer syndrome, familial atypical multiple mole melanoma syndrome, and hereditary nonpolyposis
colorectal cancer. Canto et al [23] screened for early pancreatic neoplasia with an EUS-based and an EUS- and
CT-based [24] protocol. In the latter, pancreatic abnormalities were compared in high-risk individuals and control
subjects. The EUS- and CT-based approach found 8 patients
among 78 high-risk individuals with pancreatic neoplasms
confirmed by surgery or FNA (6 patients with 8 benign
IPMNs, 1 patient with an IPMN with progression to invasive ductal adenocarcinoma, and 1 patient with pancreatic
intraepithelial neoplasia) and no pancreatic neoplasia
among 149 control subjects. Abnormalities suggestive of
chronic pancreatitis were more common in high-risk individuals.
Conclusions
The incidence of pancreatic cancer has increased over the
last decades. Despite rapid improvements in imaging techniques and therapeutic modalities, prognosis remains poor.
One of the most promising techniques for early diagnosis
seemed to be endoscopic ultrasound. EUS with or without
fine-needle aspiration has a high sensitivity, whereas accuracy in TNM staging differs. Optimistic results in early
studies yielded to a more critical view. Compared with CT
scan, MRI, and angiography, EUS showed the highest accuracy in assessing tumor size and lymph node involvement, whereas helical CT had the highest accuracy in assessing extend of primary tumor, locoregional extension,
vascular invasion, distant metastasis, tumor TNM stage, and
tumor resectability. The evaluation of tumor resectability
should be done by a minimum of 2 imaging techniques, in
which the combination of CT scan and EUS proved to be
the method with highest accuracy at lowest cost or if needed
intraoperatively. A detection of distand metastases with
EUS is not possible. A normal EUS examination excludes a
pancreatic tumor with a high probability. The quality of
EUS shows a high interobserver variance; additional reasons for failure are a chronic or recent episode of acute
pancreatitis, diffusely infiltrating carcinoma, and a prominent ventral/ dorsal split. New techniques such as contrastenhanced EUS or additional 3-dimensional reconstructions
look promising for improving EUS. Screening for pancreatic cancer or its noninvasive precursor lesions in the general population is not feasible because of its low incidence,
Fig. 2. (A) Endoscopic ultrasound of a carcinoma in the pancreatic head
and (B) corresponding MRI.
but high-risk subpopulations, such as families with a strong
history of pancreatic cancer, hereditary cancer syndromes,
or pancreatitis, seem to be suitable targets for screening
programs.
References
[1] Ries LAG, Harkins D, Krapcho M, et al. SEER Cancer Statistics
Review, 19752003. National Cancer Institute, Bethesda, MD.
[2] Carpelan-Holmstrm M, Nordling S, Pukkala E, et al. Does anyone
survive pancreatic ductal adenocarcinoma? A nationwide study reevaluating the data of the Finnish Cancer Registry. Gut 2005;54:
3857.
[3] Niwa K, Hirooka Y, Niwa Y, et al. Comparison of image quality
between electronic and mechanical radial scanning echoendoscopes
in pancreatic diseases. J Gastroenterol Hepatol 2004;19:454 9.
[4] Gress F, Savides T, Cummings O, et al. Radial scanning and linear
array endosonography for staging pancreatic cancer: a prospective
randomized comparison. Gastrointest Endosc 1997;45:24350.
[5] Rsch T. Endoscopic ultrasonography: state of the art 1995, part 2.
Gastrointest Endosc Clin N Am 1995;5:699 849.
[6] Legmann P, Vignaux O, Dousset B, et al. Pancreatic tumors: comparison of dual-phase helical CT and endoscopic sonography. AJR
Am J Roentgenol 1998;170:131522.
S90
L. Helmstaedter and J.F. Riemann / The American Journal of Surgery 194 (Suppl to October 2007) S87S90
[7] Akahoshi K, Chijiiwa Y, Nakano I, et al. Diagnosis and staging of
pancreatic cancer by endoscopic ultrasound. Br J Radiol 1998;71:492 6.
[8] Cannon ME, Carpenter SL, Elta GH, et al. EUS compared with CT,
magnetic resonance imaging, and angiography and the influence of
biliary stenting on staging accuracy of ampullary neoplasms. Gastrointest Endosc 1999;50:2733.
[9] Ahmad NA, Lewis JD, Ginsberg GG, et al. Endoscopic ultrasound in
preoperative staging of pancreatic cancer. Gastrointest Endosc 2000;
52:463 8.
[10] Meining A, Dittler HJ, Wolf A, et al. You get what you expect? A
critical appraisal of imaging methodology in endosonographic cancer
staging. Gut 2002;50:599 603.
[11] Soriano A, Castells A, Ayuso C, et al. Preoperative staging and tumor
resectability assessment of pancreatic cancer: prospective study comparing endoscopic ultrasonography, helical computed tomography,
magnetic resonance imaging, and angiography. Am J Gastroenterol
2004;99:492501.
[12] Eloubeidi MA, Chen VK, Eltoum IA, et al. Endoscopic ultrasoundguided fine needle aspiration biopsy of patients with suspected pancreatic cancer: diagnostic accuracy and acute and 30-day complications. Am J Gastroenterol 2003;98:2663 8.
[13] Rsch T, Braig C, Gain T, et al. Staging of pancreatic and ampullary
carcinoma by endoscopic ultrasonography: comparison with conventional sonography, computed tomography, and angiography. Gastroenterology 1992;102:188 99.
[14] Hocke M, Schulze E, Gottschalk P, et al. Contrast-enhanced endoscopic ultrasound in discrimination between focal pancreatitis and
pancreatic cancer. World J Gastroenterol 2006;12:246 50.
[15] Aslanian H, Salem R, Lee J, et al. EUS diagnosis of vascular invasion
in pancreatic cancer: surgical and histologic correlates. Am J Gastroenterol 2005;100:13815.
[16] Fritscher-Ravens A, Knoefel WT, Krause C, et al. Three-dimensional
linear endoscopic ultrasoundFeasibility of a novel technique applied for the detection of vessel involvement of pancreatic masses.
Am J Gastroenterol 2005;100:1296 302.
[17] Ahmad NA, Kochman ML, Brensinger C, et al. Interobserver agreement among endosonographers for the diagnosis of neoplastic versus
non-neoplastic pancreatic cystic lesions. Gastrointest Endosc 2003;
58:59 64.
[18] Meining A, Rosch T, Wolf A, et al. High interobserver variability in
endosonographic staging of upper gastrointestinal cancers. Z Gastroenterol 2003;41:391 4.
[19] Bhutani MS, Gress FG, Giovannini M, et al. The No Endosonographic
Detection of Tumor (NEST) Study: a case series of pancreatic cancers
missed on endoscopic ultrasonography. Endoscopy 2004;36:3859.
[20] Catanzaro A, Richardson S, Veloso H, et al. Long-term follow-up of
patients with clinically indeterminate suspicion of pancreatic cancer
and normal EUS. Gastrointest Endosc 2003;58:836 40.
[21] Klapman JB, Chang KJ, Lee JG, et al. Negative predictive value of
endoscopic ultrasound in a large series of patients with a clinical
suspicion of pancreatic cancer. Am J Gastroenterol 2005;100:
2658 61.
[22] Furukawa H, Okada S, Saisho H, et al. Clinicopathologic features of
small pancreatic adenocarcinoma: a collective study. Cancer 1996;
78:986 90.
[23] Canto MI, Goggins M, Yeo CJ, et al. Screening for pancreatic
neoplasia in high-risk individuals: an EUS-based approach. Clin Gastroenterol Hepatol 2004;2:606 21.
[24] Canto MI, Goggins M, Hruban RH, et al. Screening for early pancreatic neoplasia in high-risk individuals: a prospective controlled
study. Clin Gastroenterol Hepatol 2006;4:766 81.
You might also like
- Upper Tract Urothelial CarcinomaFrom EverandUpper Tract Urothelial CarcinomaShahrokh F. ShariatNo ratings yet
- Role of Cpre en Tumores Pancreas 2016Document18 pagesRole of Cpre en Tumores Pancreas 2016bagnerd2@hotmail.comNo ratings yet
- Characterization of Adrenal Metastatic Cancer Using FDG PET CTDocument8 pagesCharacterization of Adrenal Metastatic Cancer Using FDG PET CTEngky ChristianNo ratings yet
- EUS and Management of Pancreatic CancerDocument11 pagesEUS and Management of Pancreatic CancerKonstantinos IliakopoulosNo ratings yet
- Ardengh Et Al - 2013 - Accuracy of Endoscopic Ultrasound-Guided Fine-Needle Aspiration in TheDocument7 pagesArdengh Et Al - 2013 - Accuracy of Endoscopic Ultrasound-Guided Fine-Needle Aspiration in TheMaria ChenNo ratings yet
- Managment Biliary ObstructionDocument6 pagesManagment Biliary ObstructionhanissyazaniNo ratings yet
- Updates in Management of Ampullary Carcinomas: Highlight ArticleDocument4 pagesUpdates in Management of Ampullary Carcinomas: Highlight Articlecorinna291No ratings yet
- Imaging of HCC: Carmen Ayuso, Jordi Rimola, A Ngeles Garcı A-CriadoDocument16 pagesImaging of HCC: Carmen Ayuso, Jordi Rimola, A Ngeles Garcı A-CriadoMahmoud AbouelsoudNo ratings yet
- The Diagnostic Accuracy of Abdominal Ultrasound Imaging For Detection of Ovarian MassesDocument5 pagesThe Diagnostic Accuracy of Abdominal Ultrasound Imaging For Detection of Ovarian MassesHanny TanzilNo ratings yet
- Pancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyDocument4 pagesPancreatic Head Mass: What Can Be Done ? Diagnosis: Ultrasonographynarsing59No ratings yet
- Lessismore:Minimally Invasiveandquality Surgicalmanagementof GynecologiccancerDocument12 pagesLessismore:Minimally Invasiveandquality Surgicalmanagementof GynecologiccancerNita AgarwalNo ratings yet
- 03 JGLD PDFDocument2 pages03 JGLD PDFWiguna Fuuzzy WuuzzyNo ratings yet
- Ultrazvuk AbdomenaDocument10 pagesUltrazvuk AbdomenaLejlaNo ratings yet
- Minimally Invasive AdrenalectomyDocument14 pagesMinimally Invasive AdrenalectomyTJ LapuzNo ratings yet
- Editorial Surveillance in Testicular Cancer: Who, When, What and How?Document3 pagesEditorial Surveillance in Testicular Cancer: Who, When, What and How?Jocho NeavesNo ratings yet
- 009 - The-Perioperative-and-Operative-Management-of - 2023 - Surgical-Oncology-ClinicsDocument17 pages009 - The-Perioperative-and-Operative-Management-of - 2023 - Surgical-Oncology-ClinicsDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- 368-Manuscript Word File (STEP 1) - 1722-1-10-20210720Document6 pages368-Manuscript Word File (STEP 1) - 1722-1-10-20210720Muhammad Babar KhanNo ratings yet
- Hepatic Nodules CEUSDocument8 pagesHepatic Nodules CEUScalustre2016No ratings yet
- Managementofgastric Adenocarcinomaforgeneral Surgeons: Hisakazu HoshiDocument12 pagesManagementofgastric Adenocarcinomaforgeneral Surgeons: Hisakazu HoshiNelson William UsnayoNo ratings yet
- EUS Solid Pancreatic LesionsDocument42 pagesEUS Solid Pancreatic LesionsAhmed ElwassiefNo ratings yet
- Abdominoperineal Resection For Squamous Cell Anal Carcinoma: Survival and Risk Factors For RecurrenceDocument8 pagesAbdominoperineal Resection For Squamous Cell Anal Carcinoma: Survival and Risk Factors For RecurrenceWitrisyah PutriNo ratings yet
- Review Article: Malignant Pleural Effusion: Diagnosis and ManagementDocument11 pagesReview Article: Malignant Pleural Effusion: Diagnosis and ManagementRuth WibowoNo ratings yet
- Diagnostic Parameters To Differentiate Benign From Malignant Ovarian Masses With Contrast-Enhanced Transvaginal SonographyDocument8 pagesDiagnostic Parameters To Differentiate Benign From Malignant Ovarian Masses With Contrast-Enhanced Transvaginal SonographyRush32No ratings yet
- Format For Manuscript Submission: ReviewDocument26 pagesFormat For Manuscript Submission: ReviewMariaNo ratings yet
- Pancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyDocument4 pagesPancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyMolla WariNo ratings yet
- Sarcopenia Predicts Reduced Survival in Patients With Hepatocellular Carcinoma at First DiagnosisDocument8 pagesSarcopenia Predicts Reduced Survival in Patients With Hepatocellular Carcinoma at First DiagnosisHendra KoncoroNo ratings yet
- 0100 3984 RB 51 06 0VII PDFDocument2 pages0100 3984 RB 51 06 0VII PDFMarcelitaTaliaDuwiriNo ratings yet
- The OncologistDocument7 pagesThe OncologistManunart FeungpeanNo ratings yet
- Rosendahl 2017Document7 pagesRosendahl 2017Prince VallejosNo ratings yet
- Venous Thromboembolism (VTE) in Patients With Advanced Gastric CancerDocument9 pagesVenous Thromboembolism (VTE) in Patients With Advanced Gastric CancerMaria PerezNo ratings yet
- IkjjjkjDocument7 pagesIkjjjkjMohammad AjiNo ratings yet
- Medicina: Diagnostic Performance of Contrast-Enhanced Ultrasound (CEUS) in The Evaluation of Solid Renal MassesDocument8 pagesMedicina: Diagnostic Performance of Contrast-Enhanced Ultrasound (CEUS) in The Evaluation of Solid Renal MassesAgamNo ratings yet
- Appendicitis Imaging: Practice EssentialsDocument6 pagesAppendicitis Imaging: Practice EssentialsAjp Ryuzaki CaesarNo ratings yet
- Diagnostic Values of Ultrasound and The Modified Alvarado Scoring System in Acute AppendicitisDocument5 pagesDiagnostic Values of Ultrasound and The Modified Alvarado Scoring System in Acute Appendicitissela_hasibuanNo ratings yet
- Bladder 8Document9 pagesBladder 8Duddy Ari HardiantoNo ratings yet
- Accepted Manuscript: European Journal of RadiologyDocument46 pagesAccepted Manuscript: European Journal of Radiologykashika 75No ratings yet
- JURNAL RadiologiDocument16 pagesJURNAL RadiologiBintang Saputra PilliangNo ratings yet
- Knut Tel 2014Document6 pagesKnut Tel 2014IridaeNo ratings yet
- A Comparison Between The Reference Values of MRI and EUS and Their Usefulness To Surgeons in Rectal CancerDocument9 pagesA Comparison Between The Reference Values of MRI and EUS and Their Usefulness To Surgeons in Rectal CancerСергей СадовниковNo ratings yet
- Del Beke 2004Document7 pagesDel Beke 2004nitsuga oneNo ratings yet
- Usg Acute AppendicitisDocument10 pagesUsg Acute AppendicitisAtika RahmahNo ratings yet
- Role of spp1 in Breast CancerDocument8 pagesRole of spp1 in Breast Cancerpadma maliniNo ratings yet
- Down-Staging of Early Stage Prostate Can PDFDocument9 pagesDown-Staging of Early Stage Prostate Can PDFNelma TuiranNo ratings yet
- Neuroendocrine Tumors Dr. WarsinggihDocument20 pagesNeuroendocrine Tumors Dr. WarsinggihAndi Eka Putra PerdanaNo ratings yet
- Glucocorticoid Excess As Well As COVID19 Diseasetedhk PDFDocument1 pageGlucocorticoid Excess As Well As COVID19 Diseasetedhk PDFedgerdaniel6No ratings yet
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDocument6 pagesSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedNo ratings yet
- DX Ca PancreasDocument4 pagesDX Ca PancreasGustavo UriondoNo ratings yet
- Clinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypeDocument12 pagesClinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypesilviailieNo ratings yet
- AbstractsDocument1 pageAbstractsArely Villa RodriguezNo ratings yet
- Cancer Pulmonar EstadiajeDocument8 pagesCancer Pulmonar EstadiajeCarlos MichasNo ratings yet
- Imagerie DG CHCDocument16 pagesImagerie DG CHCnessimNo ratings yet
- Arc PSA PDFDocument17 pagesArc PSA PDFBharat KumarNo ratings yet
- 3.MRI of HCCDocument13 pages3.MRI of HCCOana AndreeaNo ratings yet
- Jurnal ApendisitisDocument6 pagesJurnal ApendisitisHilda MarsellaNo ratings yet
- PSA Level and Gleason Score in Predicting The Stage of Newly Diagnosed Prostat CancerDocument6 pagesPSA Level and Gleason Score in Predicting The Stage of Newly Diagnosed Prostat CancergumNo ratings yet
- Gallbladder CancerDocument5 pagesGallbladder CancerandyjayaNo ratings yet
- Esophageal Cancer Recurrence Patterns and Implicati 2013 Journal of ThoracicDocument5 pagesEsophageal Cancer Recurrence Patterns and Implicati 2013 Journal of ThoracicFlorin AchimNo ratings yet
- Update Imagenes ApendicitisDocument14 pagesUpdate Imagenes ApendicitisAlejandra MuglisaNo ratings yet
- PublishedDocument5 pagesPublishedMudassar SaeedNo ratings yet
- CA MammaeDocument6 pagesCA MammaeRiaNo ratings yet
- BPJS e-SIMULASI KODING&TARIF BEDAH UMUM RS TYPE D (inaCBG)Document1 pageBPJS e-SIMULASI KODING&TARIF BEDAH UMUM RS TYPE D (inaCBG)Achmad Dzulfikar AziziNo ratings yet
- Simulasi Koding&Tarif Bedah Umum Rs Type D (Inacbg)Document1 pageSimulasi Koding&Tarif Bedah Umum Rs Type D (Inacbg)Achmad Dzulfikar AziziNo ratings yet
- Sensus Plastik 26 Maret 2015Document10 pagesSensus Plastik 26 Maret 2015Achmad Dzulfikar AziziNo ratings yet
- Flea Market Outdoors 2015 PDFDocument148 pagesFlea Market Outdoors 2015 PDFAchmad Dzulfikar Azizi100% (3)
- Internal Medicine Residency BrochureDocument23 pagesInternal Medicine Residency Brochuredanskip1025No ratings yet
- FOI Response From Barnsley HospitalDocument3 pagesFOI Response From Barnsley HospitalnhswatchukNo ratings yet
- Assessment of Learning NeedsDocument4 pagesAssessment of Learning NeedsRhonaJoyNo ratings yet
- Anterolateral ThoracotomyDocument6 pagesAnterolateral Thoracotomyfluid_man_brazilNo ratings yet
- Bladder IrrigationDocument3 pagesBladder IrrigationRuth GunjalNo ratings yet
- How I Do CMR Scanning Safely: Elisabeth Burman Research Sister Royal Brompton Hospital, London UKDocument41 pagesHow I Do CMR Scanning Safely: Elisabeth Burman Research Sister Royal Brompton Hospital, London UKYuda FhunkshyangNo ratings yet
- H. Pylori Stool Antigen TestDocument30 pagesH. Pylori Stool Antigen TestcafemedNo ratings yet
- #3 Beydler-2017-AORN - JournalDocument7 pages#3 Beydler-2017-AORN - JournalMarina ENo ratings yet
- Premalignant LesionsDocument76 pagesPremalignant LesionsPrima D Andri100% (1)
- Pro DrugDocument4 pagesPro DrugIbnu SinaNo ratings yet
- Peer Support Workers Theory and PracticeDocument16 pagesPeer Support Workers Theory and PracticeSimple FaceNo ratings yet
- Huntleigh BD4000 Fetal Monitor - User ManualDocument48 pagesHuntleigh BD4000 Fetal Monitor - User ManualAtiqurrehman UmairNo ratings yet
- Coherencia HemodinamicaDocument9 pagesCoherencia HemodinamicaMaritza Alejandra Baeza EricesNo ratings yet
- AbstractDocument23 pagesAbstractaashish21081986No ratings yet
- Congenital Diaphragmatic HerniaDocument21 pagesCongenital Diaphragmatic HerniaJennifer Dixon100% (1)
- Pulmonary TuberculosisDocument17 pagesPulmonary TuberculosisRobert Dominic GonzalesNo ratings yet
- Postpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiDocument4 pagesPostpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiAstrit GashiNo ratings yet
- Amniotic Fluid Embolism ArticleDocument3 pagesAmniotic Fluid Embolism ArticleShailesh JainNo ratings yet
- Evidence Based Medicine & GuidelinesDocument32 pagesEvidence Based Medicine & GuidelinesCarmel Joy DifuntorumNo ratings yet
- In Service Exam For Breast DR Paul BalisiDocument11 pagesIn Service Exam For Breast DR Paul BalisiAmiel Francisco ReyesNo ratings yet
- Nurse Anesthesia 6Th Edition Edition John J Nagelhout Full ChapterDocument63 pagesNurse Anesthesia 6Th Edition Edition John J Nagelhout Full Chapterjay.hart148100% (6)
- Journal Reading: Chronic Kidney Disease Related To Renal Tuberculosis: A Case ReportDocument15 pagesJournal Reading: Chronic Kidney Disease Related To Renal Tuberculosis: A Case ReportnikoapredoNo ratings yet
- Approach To Spontaneous PneumothoraxDocument25 pagesApproach To Spontaneous PneumothoraxMohdGhazaliAcoyNo ratings yet
- Effects of Implementation of Focus-Pdca Model To Decrease Patients' Length of Stay in Emergency DepartmentDocument5 pagesEffects of Implementation of Focus-Pdca Model To Decrease Patients' Length of Stay in Emergency DepartmentMuhammad RamadhanNo ratings yet
- FluticasoneDocument4 pagesFluticasoneCiera YoungNo ratings yet
- T1/2 DiazepamDocument9 pagesT1/2 DiazepamanisfauziaNo ratings yet
- Myopic MaculopathyDocument17 pagesMyopic MaculopathyjochigNo ratings yet
- Iv PushDocument21 pagesIv PushChaseNo ratings yet
- 1-Medical Gases Systems. The First Lecture.Document18 pages1-Medical Gases Systems. The First Lecture.Fireproof Sistemas Electromecánicos100% (1)
- Arteri LineDocument13 pagesArteri Linemuthia octavianaNo ratings yet
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (254)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (60)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)