Professional Documents
Culture Documents
Trauma As A Neglected Etiological PDF
Uploaded by
SašaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Trauma As A Neglected Etiological PDF
Uploaded by
SašaCopyright:
Available Formats
Aleksandar Dimitrijevic, PhD1
Originalni nauni rad
Assistant Professor, Department of Psychology, UDK: 159.944.4: 616.89-008.1
Faculty of Philosophy, University of Belgrade
Primljeno: 11.5.2015.
Substitute Professor,
DOI: 10.2298/SOC1502286D
International Psychoanalytic University, Berlin
TRAUMA AS A NEGLECTED ETIOLOGICAL
FACTOR OF MENTAL DISORDERS
ABSTRACT Throughout the history of mental health care field, trauma was
prescribed different and frequently opposing roles. In psychoanalysis, the attitude
toward trauma was ambiguous: it was considered a crucial factor, but at the same
time its role could happen to be minimized. In biological psychiatry, it is seen as a
dominant cause of some disorders and completely irrelevant for the others.
In this paper, two issues are discussed: frequency of traumatic events in general
population and among persons with mental disorders; and hypothesized intrapsychic
mechanisms that lead to detrimental consequences of trauma on mental health.
It is advocated that prevention of early, especially attachment, trauma should be
the focus of our work in dealing with mental disorders.
KEYWORDS: trauma, mental disorder, attachment, mentalization
SAETAK Tokom razvoja zatite mentalnog zdravlja, trauma je esto dobijala
razliite, pa ak i suprotstavljene uloge. U psihoanalizi je smatrana kljunim
faktorom nastanka mentalnih poremeaja, ali je u isto vreme mogla biti i
zanemarena, dok je u biolokoj psihijatriji prihvaena za glavni uzrok nekih
poremeaja ali i kao potpuno nevana za druge.
U ovom tekstu u diskutovati dva pitanja: uestalost traumatskih dogaaja u
optoj populaciji i meu osobama s mentalnim poremeajima, te pretpostavljene
intrapsihike mehanizme koji vode do nepoeljnih posledica traume po mentalno
zdravlje.
Na osnovu svih podataka moe se zakljuiti da bi prevencija ranih trauma, a
posebno trauma u odnosima vezanosti, trebalo da bude fokus u naem radu s
osobama koje pate od mentalnih poremeaja.
KLJUNE REI trauma, mentalni poremeaj, vezanost, mentalizacija
adimitri@f.bg.ac.rs, a.dimitrijevic@ipu-berlin.de
Aleksandar Dimitrijevic: Trauma as a neglected etiological factor of mental disorders
287
History of trauma in the mental health care field
A long debate about the role of trauma started with French psychiatrists of
the XIX century and Freud (e.g.: Ellenberger, 1970; Hacking, 1998; Makari, 2008).
While Freud believed that actual trauma is a necessary trigger for neurosis, his
opinion about the infantile trauma changed. Initially, he found infantile trauma
to be of utmost importance, because it would define the fixation point and thus
the symptoms of the disorder (e.g., Bonomi, 2015). In a letter to Wilhelm Fliess,
however, on October 15, 1897, Freud introduced the conception of what will
come to be known the Oedipus complex: it was childrens fantasy that defined
the root of the disorder and not the actual traumatic events (Masson, 1985, p.
272). The shift was so dramatic that it was labeled the assault on truth about
the molestation of children in the conservative Vienna (Masson, 1992).
It had not been until the second half of the 1920s that this view was
challenged. In two of his last papers, Sandor Ferenczi tried to bring trauma
back to the centre of attention. He described developmental and clinical details
related to problems faced by the unwanted children, who are traumatized
by simply not being welcomed with enough love and care (1929), as well as
reactions of children to adult experiences they cannot represent in their
immature minds (1933). These ideas were rejected by Freud, to the level that
Ferenczi was declared psychotic and his papers forgotten/forbidden for about
half a century (Bonomi, 2004).
It seems that the concept of trauma has been polarizing psychoanalysts
during the entire century, constantly considered as opposite to the concept
of inner fantasy. On one side were Melanie Klein and her followers, who
thought that what mattered were mental drives, representations, anxieties, and
defense mechanisms, while social objects (like actual parents) were outside
the field of their interest. Opposite to them, the Independents, most explicitly
Donald Winnicott and John Bowlby, studied the importance of interpersonal
relationships and consequences of trauma (Dimitrijevic, 2011a). They started
with a joint paper that recommended the evacuation of whole families from
1939 London, so that children are not separated from their parents (Bowlby et
al., 1939), and kept studying trauma, albeit in different ways: Winnicott worked
as pediatrician and psychoanalyst, while Bowlby founded attachment theory
as a special form of object-relations theory, closer to natural sciences than to
psychoanalytic hermeneutics (Issroff, 2005).
Out of this grew many hypothesized types of trauma, several proposed
underlying mechanisms, many forms of treatment. By 1967, Anna Freud claimed
that the concept of trauma has become empty due to overuse. Although that was
still the time when psychodynamic model dominated psychiatry, especially in
the US, the situation there was much different. It now looks curious that the
widely used Kaplans Synopsis of Psychiatry has up to the 1980 edition relied
on a 1955 study that had claimed incest occurred in just one out of one million
American families (after Ross, 1996, pp. 67). And although current estimates are
more realistic, the division in approaches resembles that inside psychoanalysis.
288
SOCIOLOGIJA, Vol. LVII (2015), N 2
Namely, since the third revision, published in 1980, the Diagnostic and
Statistical Manual does not include discussions about possible causes of mental
disorders and this principle is included even in the generic definition offered
at the Manuals beginning. Without going into details of the possible critique
of this, it should be emphasized that there is one clear exemption to this rule.
The same DSM-III included (in the new category Anxiety Disorders) PostTraumatic Stress Disorders (PTSD), explicitly defined by their cause, and that
cause was trauma. One can reason that behind this is the now omnipresent
biological model of mental disorders (in all cases but PTSD, the causes is in the
dis-balance of neurotransmitters), which suits the pharmacological industry, and
that the role of trauma, and thus of more psychological models, is limited to just
one disorder (Lewis, 2006).
The best, and possibly the only, way to tell who is right and who is wrong
would be to see what research tells us about the incidence of trauma in general
population and in samples of persons with mental disorders. Luckily, we have
more and more solid data about this.
Incidence of trauma
So, is trauma very rare, as we used to believe, or could it be that it is
everywhere around us? And: is it more frequent in the lives and growing up of
the persons with mental disorders?
We can decide on these issues now based on several large-scale
epidemiological studies, mostly done in the United States. In general, it seems
that high incidence of early individual trauma seems not to be disputed in
contemporary scientific literature. In contrast to the 1955 study quoted above,
for instance, more recent estimates claim that there are approximately one
million cases of child abuse and neglect substantiated in the US each year (US
Department of Health, 2005, www.acf.hhs.gov). And we have even more precise
data, showing the incidence of various types of trauma in percentage:
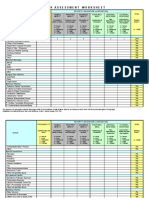
Table 1. Incidence of different types of trauma
in general population (adapted after: Putnam et al., 2015)
Sample size
Type of abuse
Physical abuse
Sexual abuse
Emotional abuse
Women
N=9367
Men
N=7970
Total
N=17337
27
24.7
13.1
29.9
16
7.6
28.3
20.7
10.6
The table shows that the incidence rate changes for different types of trauma,
but is constantly alarmingly high. This impressively large sample shows that in
some cases one quarter or even a third of the subjects were exposed to trauma,
with strong gender differences (e.g., there are more physically abused men, but
more sexually abused women). From this, we cannot make conclusions about
the difference between general and clinical populations, but we will return to
289
Aleksandar Dimitrijevic: Trauma as a neglected etiological factor of mental disorders
that shortly. It seems, however, that we have learned that trauma occurs very
frequently in contemporary Western society.
How about cumulative trauma? Is it frequent that the same child gets
molested or exposed to witnessing trauma2 more than once? Here is data from
the same sample:
Table 2. Cumulative incidence of trauma
in general population (after: Putnam et al., 2015)
Sample size
0
1
2
3
4 or more
Women
N=9367
34.5
24.5
15.5
10.3
15.2
Men
N=7970
38
27.9
16.4
8.6
9.2
Total
N=17337
36.1
26
15.9
9.5
12.5
We can be relieved about the almost two fifths of the population who have
grown up without serious trauma. The problem may be, however, important for
the majority, at 63.9%, have been traumatized. Worse still, among them as many
as 37.9% were traumatized more than once, and every eighth subject had adverse
experiences repeatedly (four or more times). This study would, thus, suggest that
there are almost twice more traumatized than non-traumatized individuals and
that almost two fifths of the general population (or, in real numbers, millions
and millions of adults) suffered repeatedly.
To make the matters more worrisome, empirical evidence shows that most
maltreatment happens in the earliest childhood, when it has greater negative
effects on developing mind and brain. The troubling 5.7% children of ages 03
experience trauma or neglect, which is, happily, followed by a steady decline, to
reach 1.9% at the age 1617 (US Department of Health and Human Services,
2014).
Another important question may well be where all this takes place. How
frequent is family trauma?
Table 3. Incidence of family dysfunctions
in general population (after: Putnam et al., 2015)
Sample size
Type of household dysfunction
Substance abuse
Parental separation or divorce
Mental illness
Mother treated violently
Incarcerated member
Women
N=9367
Men
N=7970
Total
N=17337
29.5
24.5
23.3
13.7
5.2
23.8
21.8
14.8
11.5
4.7
26.9
23.3
19.4
12.7
5.1
Data in this table report adverse childhood experiences (ACES)
family dysfunction.
trauma, neglect and
290
SOCIOLOGIJA, Vol. LVII (2015), N 2
We see, again, that the incidence is disturbingly high, and especially for
women. Every fifth subject has experienced at least one type of household
dysfunction, sometimes the rate is higher, and for some it must have been more
than one. It is also significant that four out of five types of the listed family
disfunctions actually make parents emotionally unavailable: substance abuse,
divorce, mental illness and incarceration (this one does not have to involve the
parent, though).3
Based on all this evidence, which comes from recent studies on large samples,
we can conclude that trauma is a widespread phenomenon and that it frequently
happens to infants and preschool children, inside their homes. But, what are the
consequences of trauma? Does this evidence bear clinical importance?
Consequences of childhood trauma
Many clinical psychologists have, in studies of various types, found that
consequences of childhood trauma include and are not limited to the following
(see Lieberman & Van Horn, 2011; Osofsky, 2011):
more frequent adoptions, child fatalities, developmental delays;
poor attachment and socialization, low self-esteem;
distortions in sensory perception and meaning, constrictions in action,
deficits in readiness to learn, attention, abstract reasoning and executive
function;
HPA/cortisol dysregulation, smaller frontal lobe volume, asymmetry of
left and right brain centers included in the cognitive processes of language
production.
It is also found that prevalence of many serious somatic conditions correlates
positively with the number of traumatic events, like Ischemic Heart Disease,
Stroke, Diabetes, and especially Chronic Obstructive Pulmonary Disease and
Sexually Transmitted Diseases (Felitti et al., 1998).
Besides developmental and health issues, trauma is especially important for
the field of mental health care. Strong positive correlations were found between
the number of traumatic events and several types of mental disorders:
If we consider tables 1&3 together, we may come to the conclusion that many adults report
being traumatized as well as many report coming from dysfunctional families. We do not
know whether these are the same individuals, but it is quite probable that they are. In case
this really is true, it would mean that children cannot get support from their parents when
they need it most.
Aleksandar Dimitrijevic: Trauma as a neglected etiological factor of mental disorders
291
Figure 1 Correlation between number
of traumatic events and mental disorders
(Adapted after: Putnam et al., 2013; Wang et al., 2005)
Colleagues gathered in the International Society for Psychological and Social
Approaches to Psychosis (www.isps.org) have prepared reviews of more than
40 research studies about trauma and psychotic disorders conducted between
1984 and 2003 (Read et al., 2004). Clinical samples included in the meta-analysis
ranged between 7 and 321 and included: persons with schizophrenia; persons
with other psychoses; outpatient samples in which at least 50% of subjects were
persons with psychotic disorders; child and adolescent inpatients. I have used
their work to draw a simple table that compares frequencies of trauma in general
population and among psychiatry patients.
Table 4. Frequency of childhood trauma among adults
with mental disorders (after: Read et al., 2004)
Physical abuse
Sexual molestation
Incest
Parental loss
General population
3% of men
5% of women
Psychiatry patients
30% of men
3442% of women
3% of men
12% of women
7% of men
1317% of women
18% of men
51% of women
62% of men
62% of women
38% of patients with SCH
17% of patients with BAD
I believe that the table clearly illustrates that certain forms of early individual
trauma are 410 times more frequent among our patients than in general
populations (although values for the latter are much lower than in the studies
performed in the US). This is further underlined by comparison studies that
established differences between psychotic patients with the history of childhood
292
SOCIOLOGIJA, Vol. LVII (2015), N 2
trauma and those without it (Read et al., 2004, p. 223), which resulted in the
finding that the consequences of childhood trauma are associated with:
more self-mutilation, higher symptom severity, more suicide attempts;
earlier first admissions;
more medication;
longer and more frequent hospitalizations and seclusions.
We can, thus, plausibly conclude, based on many international studies and
meta-analyses, that trauma is far more frequent among persons who experience
somatic or mental health problems. We still have to wonder, however, whether
these correlations indicate causal relationships or not.
Attachment trauma
One type of trauma has in recent studies been emphasized as specially
important and that is attachment trauma.4 Consequences seem to be most
disturbing when trauma is inflicted in closest relationships, those from which
children expect safety and encouragement for exploration. Children exposed to
attachment trauma frequently develop the so-called disorganized attachment
pattern, characterized by complete lack of strategy in close relationships, freezing
out of movement and expression, and/or incomprehensible behavior. About 15%
of children in non-clinical samples are classified as disorganised (Van Ijzendoorn
& Bakermans-Kranenburg, 1997, p. 136), but this number raises to astonishing
82% of maltreated children (Lyons-Ruth & Jacobvitz, 1999, p. 526).
There is obvious connection between the disorganized attachment in
children and their parents mental health status. Most mothers suffering from
depression and schizophrenia, and about 80% of mothers with anxious disorders,
have insecurely attached children (Greenberg, 1999, p. 478). More than a half of
D-children have parents who had suffered significant loss(es) two years before
the childrens birth that are still unresolved (Lyons-Ruth & Jacobvitz, 1999, pp.
5289, 540; Van Ijzendoorn & Bakermans-Kranenburg, 1997, p. 136).
Disorganized attachment pattern at the age of 12 months, based very
frequently on attachment trauma, is predictive of the following set of variables
(based on Greenberg, 1999, p. 479; Solomon & George, 1999, p. 294):
controlling, pseudo-parental behavior in preschool years;
aggressive behavior in 83% of 7-year-olds;
problems with adaptation to school in majority of these children;5
delinquency, addictions, and personality disorders in majority of these
adolescents;
Another form that is attracting more attention is social or genocidal trauma, but it cannot
be discussed properly here for the lack of space. For detailed review see Delic et al., 2014;
Hamburger, in press.
Recent empirical data about the relationship between attachment and cognition can be found
in Banjac et al., 2013; Dimitrijevic et al., 2013.
Aleksandar Dimitrijevic: Trauma as a neglected etiological factor of mental disorders
293
mental health problems in about 80% of these adults, and especially dissociative
phenomena and disorders.
One additional benefit from attachment research is that we now have
empirical evidence substantiating and nuancing our understanding of the
mechanisms that lead from trauma to disorganized attachment to deviant
behavior and mental disorder.
Attachment theory predicted that trauma would inhibit investigation and
heighten the need for comfort coming from the secure attachment base (Bowlby,
1988), and this was indeed corroborated. Furthermore, it was found that
traumatized children move toward parents and at the same time away from them
and are forced to create multiple models of caregivers (Fonagy & Target, 2008).
Faced with the situation in which, for instance, the father, supposed or until
recently actual source of comfort and love, starts abusing him or her, the child
may unconsciously decide to sacrifice his or her own mind in order to save the
representation of the father. Such is the importance of the parent for the highly
dependent preschooler that it is easier to lose ones own inner world, because
children survive without introspective capacity, but vanish without adults. These
children may split in their minds two types of experiences with parents: loving
father from abusive father. There is, then, one part of themselves they do not dare
admit even to themselves, one part to horrible to face. The traumatized child
first defensively inhibits her capacity to mentalize, trying to avoid the insight
that the parent may wish to hurt her (Fonagy et al., 1997, p. 253). Consequently,
trauma impedes deeper procession of emotional experiences, and interferes with
the (further) development of mentalizing capacity or can even destroy it (Fonagy
et al., 2002).6 This experience may generalize and the child then feels that
looking inside is dangerous under any circumstances. Being unaware of inner
psychological processes means, of course, that you cannot control or regulate
them. Exactly this is considered to lead not only to the disorganized attachment,
which is not a pathological condition per se, but to the later dissociative disorders
(Liotti, 2004) as well as Borderline Personality Disorder (Allen & Fonagy, 2006).
It is even more beneficial that we can use this research evidence to propose
prevention and psychotherapy interventions for disorders caused by trauma.
Treatment of (attachment) trauma
This evidence cannot but motivate us to look for ways to prevent trauma
or treat its consequences. Sceptics, if they exist, are often reminded about the
costs: The US spend about $1.8 Million per victim of early trauma in order to
deal with the consequences of child abuse, teen pregnancy, high school dropout,
illegal drug and alcohol abuse (Pew Issue Brief, 2011); estimated lifetime costs
for all those who in 2014 were victimized for the first time will be $5.9 Trillion
(The Perryman Group, 2014).
6
Attachment trauma can also interfere with ethical development and development of empathy.
For a detailed review see Milojevi & Dimitrijevi, 2012, and for empirical data see Milojevi
& Dimitrijevi, 2014.
294
SOCIOLOGIJA, Vol. LVII (2015), N 2
Luckily, effective prevention and treatment programs exist.7 Meta-analysis
of 70 studies with 88 different interventions, 7,636 parents and 1,503 children
revealed that there was a small but significant improvement ONLY when
programs were focused on improving parental capacity to accurately perceive
and translate social signals contained in the infants and childrens non-verbal
signals (Bakermans-Kranenburg, van Ijzendoorn, & Juffer, 2003). Frame-byframe analysis shows that maternal reactions of smiling, surprise, withdrawal
or looking away to the signs of four-months-old infants distress are predictive
of disorganized attachment, or even that differences between facial and vocal
emotional expressions are predictive of adults dissociation (Beebe et al., 2010).
On the basis of this, several programs were developed that use video-taping
of parent-infant interaction and subsequent discussion with parents aimed at
improving their sensitivity.
It seems, however, that improvement may come even from far less
sophisticated issues. For instance, successful public advocacy of positive parental
skills should be effective, as we have evidence showing that while cumulative
trauma and resilience are negatively correlated, positive childhood experiences
can counteract negative ones (Lieberman et al., 2005). These might include such
broad categories as parental devotion, emotional availability8 and behavioral
predictability (see Winnicott, 1960), but also more specific ones like the positive
influence of coherence and mentalizing nature of general discourse at home
(Fonagy & Bateman, 2008, p. 145). It turns out that children who grow up in
families where emotions are a topic the parents frequently talk and think together
develop faster and better in terms of theory of mind and mentalization; the
same goes for situations in which mothers ascribe psychological features to their
six-months-old babies (Fonagy & Bateman, 2008, p. 145). And where there is
mentalization, effects of trauma cannot be too bad.
Several studies conducted at the University of Leiden, Holland, confirmed
that most disorganized children have mothers with severe trauma and/or loss
they were unable to overcome, so they behave frighteningly or frightfully, and
are both the source of and the solution for the childrens anxiety, found also who
are the most helpful parents. The results showed that securely attached childrens
mothers do not suffer from unintegrated trauma, but are not particularly helpful
in extreme situations, possibly because they lack personal experience of this
kind. On the other hand, autonomously attached women who had experienced
significant loss(es) that they managed to overcome (labeled Earned Secure, as
opposed to Continuous Secure) were able to show the lowest frequency and
intensity of frightening or frightful behavior, and proved to be most helpful to
their children. Due to their experiences of both traumatization and overcoming
it, these mothers, more or less unconsciously, know what their children need and
how to provide that (after Coates, 1998, pp. 299300).
7
8
The always pragmatic Americans have counted that child abuse prevention programs return
$3, and Parent Child Interaction Therapy $3.64 to every $1 invested (Lieb et al., 2004).
On detrimental effects of parental emotional non-involvement see Fonagy & Bateman, 2008,
p, 145.
Aleksandar Dimitrijevic: Trauma as a neglected etiological factor of mental disorders
295
This lead many authors to come up with a very specific etiological hypothesis.
It is now believed that the cause of many mental disorders is a combination of:
a) severe and/or repeated childhood trauma, and b) lack of a person who could
provide the intersubjective foundation for mentalizing. Trauma, thus, does not
have to lead to a mental disorder and will not do so in cases when there are
adults ready to face and recognize childs traumatic experience and offer help in
thinking about and overcoming it (Fonagy, 2000; Levine, 2014).
For many children, unfortunately, benevolent, emotionally available and
mentalizing adults are not present in their social world, and preventive programs
have not reached many others. It is highly likely, as we have seen above, that they
will develop one or several forms of somatic illnesses, deviant behaviors and/
or mental disorders. And it is for them that we need to come up with treatment
procedures. While noumerous psychotherapy variations are considered applicable
for work with victims of trauma, at least one is developed especially for them.
The so called Mentalization Based Treatment is being formulated over the last
decade or so, with all the above mentioned principles in mind (e.g., Bateman &
Fonagy, 2006; for a review see Dimitrijevi, 2011b). Initially aimed at persons
with Borderline Personality Disorder, it is a manualized, short-term treatment,
that should help clients acquire capacity and skill of mentalization. They are first
faced with many questions that should help them realize how much of the inner
and social world they are or have been taking for granted. Subsequently, they
should hopefully start understanding their own and other persons behaviors in
terms of intentional mental states. A randomized control trial has shown that
MBT is highly effective in the follow up after 42 months (Fonagy & Bateman,
2008): patients needed less medication and fewer and shorter hospitalizations,
referred less self-harming and suicidal behavior, and improved educationally and
professionally.
Conclusion
In the last half century, the biological model of mental disorders, and
especially the psychotic ones, has gained such prevalence that discussing anything
but genes, dopamine, and cerebral ventricles is considered obsolete and nonscientific. There were various forms of resistance to admitting the importance of
trauma, including tendency that the best-selling textbooks report about trauma
in a misconceived and one-sided way (Brand & McEwan, 2015). It was only in
recent times that enough evidence was gathered to make it even more obvious
that trauma plays an important role in both development and clinically relevant
conditions of a huge number of children and adults.
The most troubling aspect of this situation, however, is not denial of the
importance of trauma, but the ensuing impossibility for persons with mental
disorders to get what they need at the institutions that are meant to provide help.
Traumatized persons are more often hospitalized than non-traumatized persons
with mental disorders (Read et al., 2004), yet many of them get nothing but
disappointment and conviction that help cannot be found, looking for the fault
296
SOCIOLOGIJA, Vol. LVII (2015), N 2
in themselves or allegedly incurable diseases instead of at the re-traumatizing
nature of depersonalized institutions (see Dimitrijevic, in press).
For all these reasons, the frequency and the role of trauma in the onset of
various somatic and mental disorders have to be advocated and substantiated, and
prevention and therapy of its consequences further developed. Otherwise, the world
will remain full of unheard, unrecognized and wrongly treated victims of peace.
Acknowledgements:
The preparation of this paper was supported by Ministry of Education and
Science of the Republic of Serbia, Grant No. 179018, and by Trauma, Trust, and
Memory Project funded by German Academic Exchange Service [DAAD],
Grant No. 57173352.
References:
Allen, J. G., & Fonagy, P. (Eds.). (2006). The handbook of mentalization-based
treatment. John Wiley & Sons.
Bakermans-Kranenburg, M. J., Van Ijzendoorn, M. H., & Juffer, F. (2003). Less
is more: meta-analyses of sensitivity and attachment interventions in early
childhood. Psychological Bulletin, 129(2), 195.
Banjac, S., Altaras Dimitrijevi, A., & Dimitrijevi, A. (2013). Odnos vezanosti,
mentalizacije i inteligencije u uzorku srednjokolaca. Psiholoka istraivanja,
16(2), 175190.
Bateman, A. & P. Fonagy (2008): 8-Year Follow-Up of Patients Treated for
Borderline Personality Disorder: Mentalization-Based Treatment Versus
Treatment as Usual. American Journal of Psychiatry, 165, 5, 631638.
Bateman, A. W., & Fonagy, P. (Eds.). (2012). Handbook of mentalizing in mental
health practice. American Psychiatric Publishers.
Beebe, B., Jaffe, J., Markese, S., Buck, K., Chen, H., Cohen, P., & Feldstein, S.
(2010). The origins of 12-month attachment: A microanalysis of 4-month
motherinfant interaction. Attachment & Human Development, 12(12),
3141.
Bonomi, C. (2004). Trauma and the symbolic function of the mind. International
Forum of Psychoanalysis, 13, 12, 4550.
Bonomi, C. (2015). The Cut and the Building of Psychoanalysis, Volume I:
Sigmund Freud and Emma Eckstein. Routledge.
Bowlby, J. (1988). A secure base: Clinical applications of attachment theory. Taylor
& Francis.
Bowlby, J., Miller, E., & Winnicott, D. W. (1939). Evacuation of small children.
British Medical Journal, 2(4119), 1202.
Brand, B. L. & McEwan, L. E. (2014). Coverage of CHILD Maltreatment and
Its Effects in Three Introductory Psychology Textbooks. Trauma Psychology
News, 9(3).
Aleksandar Dimitrijevic: Trauma as a neglected etiological factor of mental disorders
297
Coates, S. (1998): Having a Mind of Ones Own and Holding the other in
Mind: Commentary on Paper by Peter Fonagy and Mary Target (1998).
Psychoanalytic Dialogues, 8, str. 115148.
Deli, A., Hasanovi, M., Avdibegovi, E., Dimitrijevi, A., Hancheva, C., Scher,
C., Stefanovic-Stanojevic, T., Streeck-Fischer, A., & Hamburger, A. (2014).
Academic model of trauma healing in post-war societies. Acta medica
academica, 43(1), 7680.
Dimitrijevic, A. (2011a). Bindung und Phantasie in einer psychoanalytischen
Behandlung. Journal fuer Psychoanalyse, 31, 52, 84100.
Dimitrijevi, A. (2011b). Pregled naela tretmana zasnovanog na
mentalizovanju. Psihijatrija danas, 43, 1, 520.
Dimitrijevic, A. (in press). Psychiatric Treatment as a Form of Social Trauma. In
A. Hamburger (ed.), Trauma, Trust, Memory. Psychoanalytic Approaches to
Social Trauma. Karnac Books.
Dimitrijevi, A., Altaras Dimitrijevi, A., & Joli Marjanovi, Z. (2013). An
examination of the relationship between intelligence and attachment in
adulthood. In C. Pracana & L. Silva (Eds.), InPACT 2013 International
Psychological Applications Conference and Trends. Book of proceedings (pp.
2125). Lisbon: World Institute for Advanced Research and Science.
Ellenberger, H. F. (2008). The discovery of the unconscious: The history and
evolution of dynamic psychiatry. Basic Books.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M.,
Edwards, V., & Marks, J. S. (1998). Relationship of childhood abuse and
household dysfunction to many of the leading causes of death in adults: The
Adverse Childhood Experiences (ACE) Study. American Journal of Preventive
Medicine, 14(4), 245258.
Ferenczi, S. (1929). The unwelcome child and his death-instinct. International
Journal of Psycho-Analysis, 10, 125129.
Ferenczi, S. (1933/1949): Confusion of Tongues between the Adult and the Child.
International Journal of Psycho-Analysis, 30, 225230. Originally published in
1933.
Fonagy, P. (2000): Attachment and Borderline Personality Disorder. Journal of
the American Psychoanalytic Association, 48, 4, 11291146.
Fonagy, P., G. Gergely, E. L. Jurist & M. Target (2002): Affect Regulation,
Mentalization and the Development of the Self. New York, NY: Other Press.
Fonagy, P. & M. Target (2008). Attachment, Trauma, and Psychoanalysis. Where
Psychoanalysis Meets Neuroscience. In E. L. Jurist, A. Slade & S. Bergner
(eds) Mind to Mind. Infant Research, Neuroscience, and Psychoanalysis (pp.
1549). New York: Other Press.
Fonagy, P., M. Target, M. Steele, H. Steele, T. Leigh, A. Levinson & R. Kennedy
(1997): Morality, disruptive behavior, borderline personality disorder, crime,
and their relationship to security of attachment. In L. Atkinson & K. J. Zucker
(eds.) Attachment and psychopatology (pp. 223274). New York: Guilford.
298
SOCIOLOGIJA, Vol. LVII (2015), N 2
Freud, A. (1967). Comments on trauma. In S. Furst (ed.), Psychic Trauma (pp.
235246). New York: Basic Books.
Greenberg, M. T. (1999): Attachment and Psychopathology in Childhood. U: J.
Cassidy & P. R. Shaver (ur.) Handbook of Attachment. Theory, Research and
Clinical Applications (pp. 469496). New York & London: The Guilford Press.
Hacking, I. (1998). Rewriting the soul: Multiple personality and the sciences of
memory. Princeton University Press.
Hamburger, A. (in press): Genocidal Trauma. Individual and Social Consequences
of the Assault on the Mental and Physical Life of a Group. In: A. Hamburger
& D. Laub (eds.), Psychoanalytic Approaches to Social Trauma and Testimony:
Unwanted Memory and Holocaust survivors. London: Routledge.
Hesse, E. (1999): Adult Attachment Interview: Historical and Current
Perspectives. In J. Cassidy & P. R. Shaver (eds.) Handbook of Attachment.
Theory, Research and Clinical Applications (pp. 395433). New York &
London: The Guilford Press.
Issroff, J. (2005). Donald Winnicott and John Bowlby: Personal and Professional
Perspectives. London: Karnac Books.
Levine, H. (2014). Psychoanalysis and trauma. Psychoanalytic Inquiry, 34:214224.
Lewis, B. (2006): Moving Beyond Prozak, DSM, and the New Psychiatry. The Birth
of Postpsychiatry. Ann Arbor, MI: The University of Michigan Press.
Lieb, R., Mayfield, J., Miller, M., & Pennucci, A. (2004). Benefits and costs of
prevention and early intervention programs for youth (No. 0407, p. 3901).
Olympia, WA: Washington State Institute for Public Policy.
Lieberman, A. F., Padrn, E., Van Horn, P., & Harris, W. W. (2005). Angels in
the nursery: The intergenerational transmission of benevolent parental
influences. Infant mental health journal, 26(6), 504520.
Lieberman, A. F., & Van Horn, P. (2011). Psychotherapy with infants and young
children: Repairing the effects of stress and trauma on early attachment.
Guilford Press.
Liotti, G. (2004). Trauma, dissociation, and disorganized attachment: Three
strands of a single braid. Psychotherapy: Theory, research, practice, training,
41(4), 472.
Lyons-Ruth, K. & Jacobvitz, D. (1999). Attachment Disorganization: Unresolved
Loss, Relational Violence, and Lapses in Behavioral and Attentional Strategies.
In J. Cassidy & P. R. Shaver (eds.) Handbook of Attachment. Theory, Research
and Clinical Applications (pp. 520554). New York & London: The Guilford
Press.
Makari, G. (2008). Revolution in mind: The creation of psychoanalysis. New York:
HarperCollins.
Masson, J. (ed.) (1985). The Complete Letters of Sigmund Freud to Wilhelm Fliess,
18871904. Cambridge, Mass.: Harvard University Press.
Masson, J. (1992). The assault on truth: Freud and child sexual abuse. London:
Fontana.
Aleksandar Dimitrijevic: Trauma as a neglected etiological factor of mental disorders
299
Milojevi, S. & Dimitrijevi, A. (2012). Socioemocionalni model maloletnike
delinkvencije. Engrami, 34 (4), 7185.
Milojevi, S. & Dimitrijevi, A. (2014). Empathic capacity in convicted delinquent
minors. Psihologija, 47(1), 6579. DOI: 10.2298/PSI1401065M.
Osofsky, J. D. (Ed.). (2011). Clinical work with traumatized young children.
Guilford Press.
Paying later: High cost of failing to invest in young children. 2011. Pew Issue
Brief.
Putnam, K. T., Harris, W. W., & Putnam, F. W. (2013). Synergistic childhood
adversities and complex adult psychopathology. Journal of traumatic stress,
26(4), 435442.
Putnam, K. T., Harris, W. W., & Putnam, F. W., Lieberman, A., & Amaya-Jackson,
L. (2015). Oportunities to change the outcomes of traumatized children.
Downloaded from CANarratives.org.
Read, J., Mosher, L. R., & Bentall, R. P. (Eds.) (2004). Models of madness:
Psychological, social and biological approaches to schizophrenia. Psychology
Press.
Ross, C. A. (1996). History, Phenomenology, and Epidemiology of Dissociation.
In L. K. Michelson & W. J. Ray (eds.) Handbook of Dissociation. Theoretical,
Empirical, and Clinical Perspectives (pp. 324). New York London: Plenum
Press.
Solomon J. & C. George (1999). The Measurement of Attachment Security in
Infancy. In J. Cassidy & P. R. Shaver (eds.) Handbook of Attachment. Theory,
Research and Clinical Applications (pp. 287316). New York & London: The
Guilford Press.
The Perryman Group. (2014). Suffer the Little Children: An Assessment of the
Economic costs of Child Maltreatment. http://perrymangroup.com/specialreports/child-abuse-study/
US Department of Health and Human Services. (2014). Child Maltreatment
2012. Washington, DC: US Department of Health and Human Services.
Van Ijzendoorn, M. H. & M. J. Bakermans-Kranenburg (1997). Intergenerational
Transmission of Attachment: A Move to the Contextual Level. In L. Atkinson
& K. J. Zucker (eds.) Attachment and Psychopathology (pp. 135170). New
York & London: The Guilford Press.
Wang, P. S., Lane, M., Olfson, M., Pincus, H. A., Wells, K. B., & Kessler, R. C.
(2005). Twelve-month use of mental health services in the United States:
results from the National Comorbidity Survey Replication. Archives of general
psychiatry, 62(6), 629640.
Winnicott, D. W. (1975). Primary Maternal Preocupation. In Through Paediatrics
to Psycho-Analysis (pp. 300305). London: Hogarth Press & Institute of
Psychoanalysis.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 1 Forthyron Pi 200 400 en PDFDocument1 page1 Forthyron Pi 200 400 en PDFjohnybarNo ratings yet
- NCPDocument14 pagesNCPclaidelynNo ratings yet
- Lab Exercise 5Document3 pagesLab Exercise 5Yeong-Ja KwonNo ratings yet
- Subjective: Diarrhea Related To Watery Short Term: IndependentDocument4 pagesSubjective: Diarrhea Related To Watery Short Term: IndependentEmma Lyn SantosNo ratings yet
- Geria NCPDocument4 pagesGeria NCPBrylle CapiliNo ratings yet
- Menstrual Blood Derived Stem Cells and Their Scope in Regenerative Medicine A Review ArticleDocument6 pagesMenstrual Blood Derived Stem Cells and Their Scope in Regenerative Medicine A Review ArticleInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- What Is Malnutrition?: WastingDocument6 pagesWhat Is Malnutrition?: WastingĐoan VõNo ratings yet
- Mapeh: Music - Arts - Physical Education - HealthDocument23 pagesMapeh: Music - Arts - Physical Education - HealthExtremelydarkness100% (1)
- Malawi Clinical HIV Guidelines 2019 Addendumversion 8.1Document28 pagesMalawi Clinical HIV Guidelines 2019 Addendumversion 8.1INNOCENT KHULIWANo ratings yet
- ZFN, TALEN, and CRISPR-Cas-based Methods For Genome EngineeringDocument9 pagesZFN, TALEN, and CRISPR-Cas-based Methods For Genome EngineeringRomina Tamara Gil RamirezNo ratings yet
- Kelseys ResumeDocument1 pageKelseys Resumeapi-401573835No ratings yet
- 2018 Surgical Rescue in Medical PatientsDocument11 pages2018 Surgical Rescue in Medical PatientsgiseladlrNo ratings yet
- National Geographic USA - January 2016Document148 pagesNational Geographic USA - January 2016stamenkovskib100% (4)
- The Nadi Vigyan by DR - Sharda Mishra MD (Proff. in Jabalpur Ayurved College)Document5 pagesThe Nadi Vigyan by DR - Sharda Mishra MD (Proff. in Jabalpur Ayurved College)Vivek PandeyNo ratings yet
- Lesson 5 Core Elements Evidenced Based Gerontological Nursing PracticeDocument38 pagesLesson 5 Core Elements Evidenced Based Gerontological Nursing PracticeSam GarciaNo ratings yet
- Liver Meeting Brochure 2016 PDFDocument4 pagesLiver Meeting Brochure 2016 PDFManas GhoshNo ratings yet
- Nursing Care of The Client With High-Risk Labor & DeliveryDocument10 pagesNursing Care of The Client With High-Risk Labor & DeliveryWilbert CabanbanNo ratings yet
- SNB Exam Sample Question Paper 2Document19 pagesSNB Exam Sample Question Paper 2Ketheesaran LingamNo ratings yet
- IC Risk Assessment Worksheet - Kangas-V2.1-Aug.2010 1Document4 pagesIC Risk Assessment Worksheet - Kangas-V2.1-Aug.2010 1Juon Vairzya AnggraeniNo ratings yet
- Orthobullets Foot and AnkleDocument88 pagesOrthobullets Foot and AnkleStevent Richardo100% (1)
- Sample Chapter of Assessment Made Incredibly Easy! 1st UK EditionDocument28 pagesSample Chapter of Assessment Made Incredibly Easy! 1st UK EditionLippincott Williams and Wilkins- Europe100% (1)
- Angina PectorisDocument17 pagesAngina PectorisRakesh Reddy100% (1)
- Gut Health Guidebook 9 22Document313 pagesGut Health Guidebook 9 2219760227No ratings yet
- Pathophysiology of Ischemic Stroke FinalDocument3 pagesPathophysiology of Ischemic Stroke FinalAcohCChao67% (3)
- Anatomi & Fisiologi Sistem RespirasiDocument57 pagesAnatomi & Fisiologi Sistem RespirasijuliandiNo ratings yet
- Páginas de Rockwood Fraturas em Adultos, 8ed3Document51 pagesPáginas de Rockwood Fraturas em Adultos, 8ed3Estevão CananNo ratings yet
- Fertilization Reflection PaperDocument2 pagesFertilization Reflection PaperCrisandro Allen Lazo100% (2)
- PowersDocument14 pagesPowersIvan SokolovNo ratings yet
- Resveratrol and Its Effects On Human Health and LongevityDocument367 pagesResveratrol and Its Effects On Human Health and LongevityArnulfo Yu LanibaNo ratings yet
- Complications and Failures of ImplantsDocument35 pagesComplications and Failures of ImplantssavNo ratings yet