Professional Documents
Culture Documents
AMOEBIASIS
Uploaded by
Wendy EscalanteCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AMOEBIASIS
Uploaded by
Wendy EscalanteCopyright:
Available Formats
1 (Amoebiasis, Red Tide, Candidiasis, DHF, Leptospirosis, Malaria, Filariasis, SARS)
Escalante-Saac
AMOEBIASIS (amoebic dystentery)
Amoebiasis
Acute or chronic protozoal infection of human beings initially involves the colon, but may be
spread to soft tissues, most commonly the liver and lungs, by contiguity or hematogenous or
lymphatic dissemination
Entamoeba histolytica
ETIOLOGIC AGENT:
Prevalent in unsanitary areas, common in warm climates, acquired by swallowing, Cyst can
survive a few days outside the body, cyst passes to the large intestine and hatches into
trophozoites. It passes into the mesenteric veins, the portal vein, and finally to the liver,
where it causes amoebic liver abscess.
Entamoeba histolytica has 2 developmental stages:
1. Trophozoites/ Vegetative form
-these are facultative parasites that may invade the tissue or may be found in the
parasitized tissue and liquid colonic contents.
2. Cysts
a. the cyst is passed out with formed or semi-formed stools and is resistant to environmental
conditions.
b. the cyst is considered as the infective stage in the life cycle of E. histolytica
PATHOLOGY:
When the cyst is swallowed, it passes through the stomach unharmed and shows no activity while in an acidic environment. When
it reaches thee alkaline medium of the intestine, the metacyst begins to move within the cyst wall, which rapidly weakens and
tears. The quadrinucleate amoeba emerges and divides into amoebulas that are swept down into the cecum. This is the first
opportunity of the organism to colonize and its success depends on one or more metacystic trophozoites making contact with the
mucosa. The mature cyst in the large intestine leaves the host in the great numbers. The cyst can remain visible and infective in a
moist and cool environment for about 12 days, and in water 30 days. The cyst are resistant to levels of chlorine normally used for
water purification. They are rapidly killed by putrefaction, desiccation, and temperature below 5 and above 40 degrees centigrade.
Human excreta
SOURCE:
INCUBATION PERIOD:
3 days, several months
In severe infection, in sub-acute and chronic form is_
Entire duration of the illness
PERIOD OF COMMUNICABILITY:
1.Fecal-oral transmission
MODE OF TRANSMISSION:
2. direct contact through sexual
contact
3. indirect contact by ingestion of
food especially uncooked leafy
vegies or contaminated with fecal
material
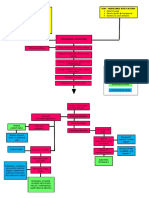
PATHOGENESIS
Ingestion of bacteriamultiplication of bacteriaendotoxin production affecting the lining of the small intestine ,colon and
capilliariesnecrosis of the mucosal layerulcerationgangrenetoxemia
1. The metacystic trophozoites or their progenies reach the cecum and those that come in contact with the mucosa penetrate or
invade the epithelium by lytic digestion
2. The trophozoites burrow deeper , with tendency to spread laterally or continue the lysis of cells until they reach the submucosa ,
forming flask-shape ulcers. There may be several points of pentration.
3. From the primary sites of invasion, secondary lesions may be produced at the lower level of the large intestine.
4. Progenies of the original colony are squeezed out to the lower portion of the bowel and thus have the opportunity to invade and
produce additional ulcers.
5. E. histolytica has been demonstrated in practically every soft organ of the body.
6. Trophozoites which reach the mascularis mucosa frequently erode the lymphatic of the wall of the mesenteric venules on the
floor of the ulcer and are carried to the intrahepatic portal vein.
7.if thrombi occurs in the small branches of the portal veins causes lytic necrosis on the walls of the vesssels and digest a pathway
into the lobules
8. The colony increases in size and develops into the abscess. A typical liver abscess develops and consist of: a. a central zone
necrosis, b. median zone of stroma only, c. outer zone of normal tissue newly invaded by amoeba
9. next to the liver, the organ which is the most frequent site if extra-intestinal amoebiasis is the lung.
CLINICAL MANIFESTATION:
1. Acute amoebic dysentery
a. slight attack of diarrhea, altered with periods of constipation and often accompanied by
tenesmus
b. diarrhea, watery, and foul-smelling stools often containing blood streaked mucus
c. colic and gaseous distention of the lower abdomen
2. Chronic amoebic dysentery
d. nausea, flatulence, abdominal distention, and tenderness in the right iliac region over the
colon
a. attack of dysentery lasts for several days usually by constipation
b. tenesmus accompanied by desire to defecate
c. anorexia, weight loss, and weakness
d. liver may be enlarged
e. stools at first are semifluid, but soon become watery, bloody and mucoid
f. vague abdominal distress, flatulence, constipation or irregularity of bowel movement
g. mild toxemia, constant fatigue, and lassitude
h. the abdomen loses its elasticity when picked up between the fingers.
i. on sigmoidoscopy ,scattered ulceration, with yellowish and erythematous borders
3. Extraintestinal forms
j. gangrenous type(fatal) characterized by appearance of large sloughs of intestinal tissues in
the stools, accompanied by hemorrhage
a. pain in the RUQ with tenderness of the liver
b. jaundice
c. intermittent fever
d. loss of weight or anorexia
e. abscess may break through the lungs, patient coughs anchovy sauce sputum
CLINICAL FEATURE:
Gradual
1. onset is_
Bloody and mucoid
2. diarrhea increases and stools becomes_
3. in untreated cases:
Fluid stoolssevere bloody-mucoid stoolhemorrhageintestinal perforationperitonitis-death
1. stool exam
DIAGNOSTIC EXAM
2. blood exam
3. proctoscopy/sigmoidoscopy
2 (Amoebiasis, Red Tide, Candidiasis, DHF, Leptospirosis, Malaria, Filariasis, SARS)
Escalante-Saac
1. Metronidazole (Flagyl) 800 mg
TID x5 days
2. Tetracycline 250 mg q 6 hours
3. ampicillin, quinolone,
sulfadiazine
4. streptomycin S04,
chloramphenicol
5. lost fluids and electrolytes
should be replaced
Isolation and enteric
Altered nutrition: less than body
requirement
Alteration in bowel elimination
High risk for infection
Anxiety
Altered body temp
Health education
Sanitary disposal of feces
Chlorinate water
Observe cleanliness in food
preparation
Fly control
RED TIDE
RED TIDE
TREATMENT MODALITIES:
NURSING MANAGEMENT:
1. observe_precaution
2. provide health education and instruct patient to: boil water for drinking, avoid washing
food with water from drums, cover leftover food, wash hands after defecation, avoid eating
ground food (cabbage, lettuce, carrots etc.)
3. proper collection of stool specimen: never give paraffin or any oil preparation 48 hours
prior to collectionof specimen, instruct patient to avoid mixture of stool and urine, select
large portion containing blood and mucus . send specimen to lab immediately, label properly
4. skin care
5. mouth care
6. provide optimum comfort
7. diet
COMMON NURSING DIAGNOSIS
METHODS OF PREVENTION
Caused by population explosion of toxic, naturally occurring microscopic phytoplanktons
,specifically a subgroup known as dinoflagellates
ETIOLOGIC AGENT:
The marine red tide organism used to be referred to as Gonyaulaz, protogonyaulax, and
gesnerium. Presently ,they are known by the aaccepted name Alexandrium sp.
-Found along the atlantic coast
-found along the pacific west coast
-present in the gulf of mexico along the west florida coast
FACTORS WHICH ARE FAVORABLE FOR GROWTH OF BLOOMS:
1. alexandrium tamarense
2. alexandrium catenella
3. ptychodiscus brevis
1. warm surface temperature
2. high nutrient content
3. low salinity and calm seas
4. rainy days followed by sunny
weather
DOES IT REALLY COLOR THE WATER?
Yes. Water in coastal areas can be colored red by algae, thus, the term red tide. The toxic blooms often turn the water reddish
brown, although there algae that are not poisonous.
SEAFOODS THAT ARE UNSAFE TO EAT FROM INFECTED WATERS
Shellfish are particularly prone to contamination as they feed by filtering microsocopic food out of the water.
Such shellfish include: quahogs, soft shellfish, oysters, mussels, scallops, moon smails
1. Paralytic shellfish poisoning
FOUR SYNDROMES OF SHELLFISH POISONING:
2. Diarrheal shellfish poisoning
3. Amnestic shellfish poisoning
4. Neurologic shellfish poisoning
Mussels, clams, oysters, and
All four syndrome share some common features and are primarily associated with bivalve
scallops
mollusk such as_
dinoflagellates and diatoms
These shellfish are filter feeders and, therefore, accumulate toxins produced by microscopic
algae in the form of _
Lobster,crabs, shrimps and fish
_ do not accumulate toxins and are safe to eat even if they are from affected waters.
PATHPHYSIOLOGY
Eating toxic shellfish can cause paralytic shellfish poisoning(PSP) in humans. PSP is caused by saxitoxin, which is produced by A
catenella and is one of the most potent toxins known. Saxitoxin acts by blocking sodium movement in muscle tissue. Conduction
block primarily occurs in the neurons and muscle. The toxins responsible for shellfish poisoning are water soluble, heat and acid
stable, and are not inactivated by ordinary cooking. Afer ingestion, the toxin immediately affects the nervous systemwith
symptoms usually appearing within 30 minutes. Severity depends on the amount of toxin consumed. Toxic shellfish taste appear
no different from non toxic shellfish and cooking does not destroy the organism.
CLINICAL MANIFESTATION
lips and tongue
1. the initial sign is the tingling of the _which spreads to the face, neck, fingertips and toes
headache, dizziness and nausea
2. _follow, symptoms which may be mistaken as being due to drunken condition
alcohol consumption
3. such symptoms are aggrevated by _
muscular paralysis and breathing
4. in severe cases, _may occur in 5 to 12 hours due to paralysis of the diaphragm, the victim
difficulty
can survive with the aid of respirator
5. fatalities from _have been reported
respiratory arrest
MODALITIES OF TREATMENT
vomit
1. The patient is induced to _
Charcoal hemoperfusion
2. _is a process done by pumping the arterial blood through the activated charcoal filter to
sodium bicarbonate
remove the toxin
Artificial respiration
3. Alkaline fluids, such as_, are thought to be helpful because the toxin is unstable in alkaline
condition
4._ is required if the patient exhibits respiratory stress
3 (Amoebiasis, Red Tide, Candidiasis, DHF, Leptospirosis, Malaria, Filariasis, SARS)
Escalante-Saac
PREVENTION AND CONTROL
1. all shellfish producing areas should have a monitoring program to test water, sediments and shellfish for contamination
2. the department of environmental quality engineering(DEQE) is responsible for year rounf testing of shellfish
3. if accidental ingestion, seek medical attention immediately
CANDIDIASIS (MONILIASIS/CANDDIDOSIS)
CANDIDIASIS
An infection that ranges from mild superficial fungal infection to systemic and potentially life
threatening disease.
nails(onychomycosis), the
Most often, candidiasis infects the _
ski(diaper rash), and mucous
membranes, particularly those
of the oropharynx(thrush),
vagina(monillasis), esophagus,
and GIT.
INFECTIOUS AGENT:
Candida albicans
1. these organism are part of the norma flora of the GIT, mouth, Vagina, and skin.
2. they cause infection when: there is rise in blood glucose, persons resistance is lowered,
taking immunosuppressive drugs, level of estrogen rises, broad-spectrum antibiotics are
used ,these depress normal flora and allow candida to proliferate
SIGNS AND SYMPROMS
scaly, erythematous and popular
1. The skin is _is present, sometimes covered with exudates appearing below the brest,
rash
between the fingers, and the axilla, groin and umbilicus
2. Nails are red and swollen, the nailbeds are darkened. There is occasional purulent
discharge and the separation of pruritic nails from nailbeds is evident
3. Oropharyngeal mucosa (thrush)- _exude on the tongue ,mouth, or pharynx, and reveal
cream colored or bluish white
bloody engorgement when scraped.
patches
4. The patient _
5. Vaginal mucosa- _with pruritus and local excoriation, white gray raised patches on vaginal
feels retrosternal pain and
walls with local inflammation
regurgitation
6. Renal system- _
white or yellow discharge
7. Pulmonary- _
8. Brain- _
fever, flank pain, dysuria,
9. Endocardium- _
hematuria, pyuria
hemoptysis, fever, cough
10. Eyes- _
headache, nucha rigidity, seizures
systolic or diastolic murmur,
fever,chest pain
blurred vision, orbital or periorbital
pain
DIAGNOSIS:
Stool culture
Gram staining of skin, vaginal
discharge, or scraping
1. Avoid sharing utensils
NURSING MANAGEMENT:
2. Meticulous mouth care
3. Proper disposal of oral
secretions
1. Nystatin, for oral thrush
TREATMENT:
2. Clitrimazole, fluconaxole,
ketoconazole, for mucous
membrane and vaginal infection
3. Fluconazole or amphotericin for
systemic infection
1. Check high-risk patient daily for
PREVENTION:
patchy areas for irritation , sore
throat, and gum bleeding.
2. Check vaginal discharge and
note the color, odor and treatment
DENGUE FEVER (BREAKBONE FEVER/HEMORRHAGIC FEVER/DANDY FEVER/INFECTIOUS THROMBOCYTOPENIC
PURPURA)
DENGUE FEVER
It is an acute febrile disease caused by infection with one of the serotypes of dengue virus,
which is transmitted by mosquito genus Aedes.
DENGUE FEVER
It refers to a benign form of a disease with systematic symptoms, fever, and often rash
associated with pain and in the joints, bones, and behind the eyes.
Dengue hemorrhagic fever
It is a severe, sometimes fatal manifestation of the dengue virus infection characterized by
bleeding diathesis and hypovolemic shock.
1. Flavivirus 1,2,3,4 a family of
ETIOLOGIC AGENT
togoviridae, are small virus that
contain single stranded RNA
2. Arbovirus group B
MODE OF TRANSMISSION
1. Bite of an infected mosquito,
a. AEDES AEGYPTI is a day biting mosquito (they appear 2 hours after sunrise and 2 hours
AEDES AEGYPTI
before sunset)
b. It breeds in areas of stagnant water
c. It has limited . low flying movement
2. AEDES ALBOPTICUS may
d. It has fine white dots at the base of the wings and white bands on the legs
contribute to the transmission of
the dengue virus in rural ares
3. AEDES POLYNENSIS AND
AEDES SCUTELLARIS SIMPLEX
INCUBATION PERIOD
the day before the febrile period to 1. Patients are usually infective to the mosquito from_.
the end of it.
8 to 12
2. The mosquito becomes infective from day _after the blood meal and remains infective
throughout his life.
4 (Amoebiasis, Red Tide, Candidiasis, DHF, Leptospirosis, Malaria, Filariasis, SARS)
Escalante-Saac
SOURCES OF INFECTION
The virus is present in the blood of patient during the acute phase of the disease and will
become reservoir of the virus, sucked by mosquito, which may transmit the disease.
2. Standing water
Any stagnant water in the household and its premise are usual breeding places of these
mosquito
INCIDENCE
1. Age
Common in children and peaks between four to nine years old
2. Sex
Both sexes
3. Season
Rainy season
4. Location
Prevalent in urban communities
PATHOGENESIS AND PATHOLOGY
1. the infectious agent is deposited in the skin by the vector and initial replication occurs at the
site of infection and in local lymphatic tissues
2. within few days, viremia occurs, lasting until the 4th to 5th day after the onset of symptoms
3. evidence indicates the macrophage are the principal site of replication
4. At the site of petechial rash , non-specific changes are noted, which include endothelial
swelling, perivascular edema, and extravasation of blood
5. There is marked increase in vascular permeability, hypotension, hemoconcentration,
thrombocytopenia, with increased platelet agglutinability and or moderate disseminated
intravascular coagulation
6. The most serious pathophysiological abnormality is hypovolemic shock resulting from
increased permeability of the vascular endothelium and loss of plasma from the
intravascular space.
CLINICAL MANIFESTATION:
A. DENGUE FEVER
1. Prodromal symptoms:
a) Malaise and anorexia up to 12 hours
b) Fever and chills accompanied by severe frontal headache, ocular pain, myalgia with
severe backache, and arthralgia
2. Nausea and vomiting
3. Fever is non remitting and persists for 3 to 7 days
4. Rash is more prominent on the extremities and the trunk. It may involve the face in some
isolated cases
5. Petechiae usually appears near the end of the febrile period and most commonly on the
B. DENGUE HEMORRHAGIC
lower extremities
FEVER(DHF)
This severe form of dengue virus infection is manifested by fever , hemorrhagic diathesis
hepatomegaly and hypovolemic shock
PHASES OF ILLNESS:
1. initial febrile phase lasting from
>fever(39-40)and headache, febrile convulsion may appear, palms and sole are usually
2-3 days
flushed, positive tourniquet test, anorexia, vomiting , myalgia, maculopapular or petechial
rash may be present and starts at the distal portion of the extremities, and skin appears
purple, with blanched areas (Hermans sign- pathognomonic sign)
2. Circulatory Phase
>there is fall of temperature accompanied by profound circulatory changes, usually on the
3rd to 5th day, becomes restless with cool clammy skin, cyanosis is present, profound
thrombocytopenia, bleeding diathesis, pulse is rapid and weak, untreated shock may result
in coma, metabolic acidosis, with effective therapy, recovery may follow in 2-3 days
CLASSIFICATION ACCORDING TO SEVERITY ( HALSTEAD AND NIMMANITYA)
Grade I
>there is fever accompanied with non-specific constitutional symptoms and the only
hemorrhagic manifestation is positive in tourniquet test
Grade II
>all signs of grade I, plus spontaneous bleeding from the nose, gums, and GIT, are present.
Grade III
>there is presence of circulatory failure, as manifested by weak pulse, narrow pulse
pressure, hypotension, cold, clammy skin, and restless
Grade IV
>there is profound shock , and undetectable blood pressure and pulse
COMPLICATION
1.Dengue fever
>epistaxis, menorrhagia, GI bleeding, concomitant GI disorder
2. DHF
>metabolic acidosis, hyperkalemia, tissue anoxia, urine bleeding, myocarditis
3. Severe manifestation
>dengue encephalopathy is manifested by increasing restlessness, apprehension, anxiety,
disturbd sensorium, conculsion, spacity, hyporeflexia
DIAGNOSTIC TEST:
1. tourniquet test
>screening test, done by occluding the arm veins for 5 minutes to detect capillary fragility
2. platelet count
3. hemoconcentration
4. occult blood
5. hemoglobin determination
TREATMENT MODALITIES:
There is no effective antiviral therapy for dengue. Treatment is entirely symptomatic
1. analgesic drugs
relief from headache ocular pain, and myalgia
2. IV infusion
to prevent dehydration
3. Blood transfusion
with bleeding
4. O2 therapy
for shock
5. sedatives
to alley anxiety and apprehension
NURSING MANAGEMENT:
1. patient should be kept in a mosquito free environment to avoid further transmission of infection
2. keep patient at rest during bleeding episodes
3. monitor vital signs
4. in cases of bleeding, keep patients trunk elevated, apply ice bag to bridge of nose and to forehead
5. observe signs of shock such as slow pulse, cold clammy skin, prostration, and fall BP
6. restore blood volume by putting the patient In Trendelenburgs position to provide greater blood volume to the head part
7. patient with dengue is not infectious, therefore isolation is not required
1. Altered body temperature
NURSING DIAGNOSIS:
2. Fear
3. Anxiety
4. Knowledge deficit
5. Activity intolerance
PREVENTION AND CONTROL:
1. Infected person
5 (Amoebiasis, Red Tide, Candidiasis, DHF, Leptospirosis, Malaria, Filariasis, SARS)
Escalante-Saac
1. health education
2. early detection and treatment of cases will not worsen the victims condition
3. treat mosquito nets with insecticides
4. house spraying is advised
5. eliminate vector by changing water and scrubbing sides of the vases, destroying breeding places, keeping the water contained
covered
6. avoid hanging too many clothes inside the house
LEPTOSPIROSIS (WEILS DISEASE.CANICOLA FECER/ HEMORRHAGIC JAUNDICE/ MUD FEVER/ SWINE HARD DISEASE
LEPTOSPIROSIS
It is a zoonotic infectious bacterial disease carried by animals, both domestic and wild.
Infected urine contaminates water or food, which causes disease when ingested or
inoculated through the skin.
Leptospira (Leptospira
>these are chiefly saphrophytic aquatic organism which are found in river and lake waters,
Interrogans)
sewage and in the sea, there are 150 serotypes
Serovar icterohaemorrhagiae
Weils disease is specifically causesd by_
6-15 days
INCUBATION PERIOD
10-20 days
PERIOD OF COMMUNICABILITY
1. Rats (L. icterohaemorrhagiae)
ETIOLOGIC AGENTS:
and L. batviae
Contaminated food and water and infected wildlife and domestic animals, especially rodents
2. Dogs (L. canicola)
Infection among breeders and vets
3. Mice (L. gripotyphossa)
Affects workers and flax workers
MODE OF TRANSMISSION
1. leptospirosis is transmitted through ingestion/contact with the skin mucous membrane of infected urine or carcasses of wild
/domestic animals
2. the disease can be transmitted through the mucous membrane of the eyes, nose, and mouth and breaks though the skin
3. Leptospira enters the blood to cause damage , and thereafter, in the kidneys the liver meninges febrile and conjunctiva
4. it can be transmitted by the semen of infected animals
5. human to human transmission is rare.
CLINICAL MANIFESTATION
1. the symptoms range in severity from asymptomatic to fatal
2. clinical course is generally biphasic and the majority of the cases are unicertic
3. three stages can be recognized:
a. septic stage
>febrile lasting from4 days to 7 days. Abrupt onset of remittent fever, chills, headache,
b. immune or toxic stage
anorexia, abdominal pain
>this can be with or without jaundice and last for 4-30 days. Iritis, headache, meningeal
manifestation like disorientation, and convulsion, with CSF finding of aseptic meninges,
c. convalescence
oliguria and anuria with progressive renal failure, shock coma, and CHF
>relapse may occur during the 4th to 5th weeks
1. BUN ,CREATININE
LABORATORY DIAGNOSIS
2. ELISA
3, AST,ALT, GGT
ORGANS OF THE BODY INVADED BY ORGANISM
1. after the organism gains entrance in the body, it multiplies in the bloodstream and invade
the liver, resulting in jaundice
2. in the kidneys, the presence of the organism of the nephrons and tubulae necrosis,
resulting in renal failure
3. Leptospira may affect the muscles, resulting in pain and edema
4. the organism may invade the eyes, resulting in conjunctivitis
Meningitis, respiratory distress,
COMPLICATIONS:
cardiovascular problems
MANAGEMENT:
(MEDICAL)
a. suppressing the causative agent
b. fighting possible complication.
doxycycline 100 mg p.o every
>Aetiotropic drugs- peniciliin doxycycline, ampciliin, amoxicillin, for prophylaxis _
12 hours
> peritoneal dialyisis
>administration of fluid and electrolytes and blood as indicated
(NURSING)
a. Isolate the patient
b. darken the patient room
c. observe meticulous skin care to ease pruritus
d. eradicate rats and rodents
e. encourage oral fluid intake
Body image disturbance, high risk
COMMON NURSING DIAGNOSIS
for injury, anxiety, altered
nutrition: less than body
requirement, impaired physical
mobility, impaired skin integrity,
knowledge deficit
Sanitation in homes, proper
PREVENTION AND CONTROL
drainage system, animals must be
vaccinated, infected humans and
pets must be treated, information
dissemination
MALARIA (AGUE)
MALARIA
It is an acute and chronic parasitic disease transmitted by the bite of infected mosquitos and
is confined mainly to tropical and subtropical areas. This disease causes more disability and
heavier economic burden than any other parasitic disease
Protozoa of genus plasmodia
ETIOLOGIC AGENT
(type)
>considered most serous malarial infection because of the development of high parasitic
a. plasmodium falciparum
densities in the RBC, causes agglutination, resulting to micro embolus formation, type is
(malignant tertian)
most common in the Philippines
b. plasmodium vivax (benign
>non-life threatening, except for very young age, and very old, manifested by chills every 48
tertian)
hours on 3rd day
c. plasmodium malariae (quartan)
>less frequently seen than 2 types, nonlife threatening, fever and chills usually occurs every
6 (Amoebiasis, Red Tide, Candidiasis, DHF, Leptospirosis, Malaria, Filariasis, SARS)
Escalante-Saac
d. plasmodium ovale
Breeds in clear, flowing, and
shaded streams, it is bigger in size
than ordinary mosquito, it is brown
in color, a night biting mosquito,
does not bite person in motion,
assumes 36 degree position
12 days
14 days
30 days
Not more than 1 year
1-2 years
3 years
blood transfusion
contaminated needles
72 hours,on the 4th day
> this is the rare type , rarely seen in the Philippines
the primary vector of the malaria is the female anopheles mosquito which has the following
characteristics:
INCUBATION PERION
a. plasmodium falciparum (malignant tertian)
b. plasmodium vivax and ovale(benign tertian)
c. plasmodium malariae (quartan)
PERIOD OF COMMUNICABILITY
a. plasmodium falciparum (malignant tertian)
b. plasmodium vivax and ovale(benign tertian)
c. plasmodium malariae (quartan)
MODE OF TRANSMISSION
1. the disease is transmitted mechanically through the bite of an infected female Anopheles
mosquito
2. It can be transmitted parenterally through _
3. it can be transmitted from shared _
CLINICAL MANIFESTATION
>paroxysms with shaking chills, rapidly rising fever with severe headache, profuse sweating, myalgia, splenomegaly,
PATHOGENESIS
1. the parasite enters the mosquitos stomach through infected human blood obtained during blood meal
2. within the stomach of the female mosquito, they undergo sexual conjugation and form a zygote
3. the zygote matures into a motile form called ookinete
4. after a number of days, young parasites are released and work their way into the salivary glands of the mosquito the life cycle
last 8-35 days
5. the organism is transmitted from the saliva into the victim when the mosquito bites
6. the female alone plays the role of vector and definitive host
7. in humans, the organism, invaded the RBC, where they grow and undergo asexual schizogony
8. erythrocytic merozoites are produced ,leading to rupture of RBC
9. Young merozoites invade a new batch of RBCs to start another cycle.
DIAGNOSTIC PROCEDURE:
1. Malarial Smear
>in the procedure , a film of blood is placed on a slide, stained and examined
2. Rapid diagnostic test
>this is a blood test for malaria that can be conducted outside the labs and in the field
MANAGEMENT:
(MEDICAL)
a. anti-malarial drugs- chloroquine, quinine, sulfadoxine p. falciparum, primaquine p. vivax and ovale
b. erythrocyte exchange transfusion for rapid production of high levels of parasite in blood
Nursing management:
a. must be closely monitored
b. monitor intake and output to prevent pulmo edema, daily monitoring to BUN, creatinine
c. provide comfort, encourage fluid intake, evaluate degree of anemia
Altered body temp, activity
COMMON NURSING DIAGNOSIS:
intolerance, knowledge deficit,
altered nutrition : less than body
requirement
PREVENTION AND CONTROL:
1. malarial cases should be reported, screening of all infected persons, destroy breeding places of mosquito, nets should be used,
blood donors should be screened, insect repellant should be used
FILARIASIS (ELEPHANTIASIS)
FILARIASIS
It is a parasitic disease caused by microscopic, threadlike African eye worm. The adult worms
can live only in the lymphatic system. It affects the woman, men and children, affects the
poor in both rural and urban areas, it is rarely fatal, it causes extensive disability, gross
disfigurement, and untold suffering in millions of people
CAUSATIVE ORGANISM:
1. Wuchereria bancrofti
>is the causative agent of filariasis, it is a threadworm four to five cm long and affects the
lymph nodes and lymph vessels of the legs, arms, vulva, and breast
>shows manifestation resembling that of a Bancroftian, but swelling of the extremities is
2. Brugia malayi
confined to the ares below the knee and below the elbow
>rarely affects the genitals
3. Brugia timori
>transmitted by deer fly
4. Loa loa
>person-person by mosquito bites
MODE OF TRANSMISSION
PATHOGENESIS
1. when a mosquito bites a person with lymphatic filariasis, microscopic worms circulating in the persons blood enter and infect
the mosquito
2. pass from the mosquito through the human skin through human skin and travel to the lymph vessel where they grow into adults
3. Adult worm lives for 7 years in the lymph vessels. They mate and release into the bloodstream known as microfilaria
4. once the person has the worm in his/her blood, these are picked up by the mosquito when it feeds and transmitted to other
person via larvae
5. larvae migrates to the lymph nodes , reach sexual maturity and cycle is complete
6. the person need to get many mosquito bites over several months to years to get filariasis
7. this disease damaged the kidney and lymph system
8. a person with this disease tends to have more bacterial infection in the skin thus, skin hardens and thickens called
elephantiasis
On and off chills, headache, fever
SYMPTOMS:
that last for 3 months and 1 year
after the insect bite, swelling
redness, and pain in the arms, legs
and scrotum, areas of abscess
may be present
7 (Amoebiasis, Red Tide, Candidiasis, DHF, Leptospirosis, Malaria, Filariasis, SARS)
Escalante-Saac
DIAGNOSTIC PROCEDURE:
Circulating filarial antigen
Performed on a finger prick blood droplet taken any time of day
test(CFA)
Ivermectin, albendazole,
MODALITIES OF TREATMENT:
diethylcarbamezine(DEC)
Impaired physical mobility,
COMMON NURSING DIAGNOSIS:
knowledge deficit, impaired skin
integrity, activity intolerance
Mosquito net, repellant, medicine
PREVENTION
yearly to kill worms
SEVERE ACUTE RESPIRATORY SYNDROME (SARS)
SEVERE ACUTE RESPIRATORY
Scientist confirms that a novel coronavirus is the primary cause of the disease
SYNDROME (SARS)
1. asymptomatic or mild
CLINICAL CRITERIA:
respiratory illness with temp of
>100.4 F />38 C
2. respiratory illnesses(cough,
SOB, DOB,hypoxia
>direcrt
MODE OF TRANSMISSION:
>contact with infectious
respiratory droplet or exposure to
fomite
>contamination of inanimate
materials
HOW LONG WILL THE SARS EXIST ON SURFACE?
>the virus is stable in urine or feces at room temperature for at least 1-2 days
> its survives on paper , after 36 hours on a plastic surface or stainless steel for 72 hours and on glass for 96 hours
>heat at 56 C rapidly kills the virus
Onset of high grade fever,
SIGNS AND SYMPTOMS:
headache, mild respiratory
symptoms
No specific treatment
TREATMENT:
recommendation. Empiric therapy
CLINICAL COURSE AND MANAGEMENT:
>it is difficult to decide on the appropriate time to discharge a SARS patient.
>build good body immunity
PREVENTIVE MEASURE:
>personal hygiene
>wear a mask
>wash hands properly
You might also like
- Course of Automation in IndustrialDocument3 pagesCourse of Automation in IndustrialWendy EscalanteNo ratings yet
- Nurs1117 AlphaDocument118 pagesNurs1117 AlphaRappler0% (1)
- Cardiac 1.09 Blood Pressure Normal ValuesDocument1 pageCardiac 1.09 Blood Pressure Normal ValuesRandy Mar TagudarNo ratings yet
- Birth Rates and Death Rates Etc Formulas PDFDocument2 pagesBirth Rates and Death Rates Etc Formulas PDFHafiz Zahid MahmoodNo ratings yet
- PATHODocument2 pagesPATHOWendy EscalanteNo ratings yet
- NCPDocument3 pagesNCPWendy EscalanteNo ratings yet
- Classification LFDocument34 pagesClassification LFAnonymous 4tzR698No ratings yet
- Drug StudyDocument14 pagesDrug StudyWendy EscalanteNo ratings yet
- Laboratory Exams and ResultsDocument15 pagesLaboratory Exams and ResultsWendy EscalanteNo ratings yet
- NCP 2 MiDocument16 pagesNCP 2 MiWendy EscalanteNo ratings yet
- Assessment of Kidneys PDFDocument1 pageAssessment of Kidneys PDFWendy EscalanteNo ratings yet
- Nasogastric Tube Management and CareDocument21 pagesNasogastric Tube Management and CareWendy EscalanteNo ratings yet
- Drug StudyDocument14 pagesDrug StudyWendy EscalanteNo ratings yet
- NCP 2 MiDocument16 pagesNCP 2 MiWendy EscalanteNo ratings yet
- 02 Orig Art 02 PDFDocument3 pages02 Orig Art 02 PDFWendy EscalanteNo ratings yet
- Integrated Management of Childhood Illness3 1 PDFDocument78 pagesIntegrated Management of Childhood Illness3 1 PDFWendy EscalanteNo ratings yet
- Caring For The Bedridden PatientDocument1 pageCaring For The Bedridden PatientWendy EscalanteNo ratings yet
- PATHODocument2 pagesPATHOWendy EscalanteNo ratings yet
- Modifiable Risk Factors Non - Modifiable Risk Factors: LegendDocument2 pagesModifiable Risk Factors Non - Modifiable Risk Factors: LegendWendy Escalante100% (1)
- Nasogastric Tube Management and CareDocument21 pagesNasogastric Tube Management and CareWendy EscalanteNo ratings yet
- Concept Map of Carotid Artery DiseaseDocument2 pagesConcept Map of Carotid Artery DiseaseWendy EscalanteNo ratings yet
- Lift CarryDocument7 pagesLift CarryBianca ThereseNo ratings yet
- Assessment of KidneysDocument1 pageAssessment of KidneysWendy EscalanteNo ratings yet
- Acid-Ash DietDocument10 pagesAcid-Ash DietWendy Escalante0% (1)
- Brat DietDocument8 pagesBrat DietWendy EscalanteNo ratings yet
- Concept Map in Head and Neck CancerDocument3 pagesConcept Map in Head and Neck CancerWendy EscalanteNo ratings yet
- Clear Liquid DietDocument6 pagesClear Liquid DietWendy EscalanteNo ratings yet
- At DietDocument8 pagesAt DietWendy EscalanteNo ratings yet
- Concept Map of CKD Gastrointestinal SymptomsDocument4 pagesConcept Map of CKD Gastrointestinal SymptomsWendy Escalante0% (1)
- Example of Invitation CardDocument2 pagesExample of Invitation CardWendy EscalanteNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Liver AbscessDocument23 pagesLiver AbscessAdeWahyuniNo ratings yet
- Clinical Parasitology Module 1 Merged 1Document174 pagesClinical Parasitology Module 1 Merged 1Hanan Ali BacarNo ratings yet
- PARASITOLOGY (Quizlet)Document9 pagesPARASITOLOGY (Quizlet)Allyssa AniNo ratings yet
- Post-Lecture Exam - Parasitology Answer KeyDocument87 pagesPost-Lecture Exam - Parasitology Answer KeylenvycahpdelusaNo ratings yet
- Lab Activity1 - LoboseaDocument21 pagesLab Activity1 - LoboseaJosh Buenafe MacapallagNo ratings yet
- Protozoa 1Document46 pagesProtozoa 1Muhammad Abu HurairaNo ratings yet
- Stool AnalysisDocument8 pagesStool AnalysisAbed AbusalemNo ratings yet
- Typhoid Fever and AmoebiasisDocument37 pagesTyphoid Fever and Amoebiasisibnbasheer100% (4)
- CHAPTER 2 ProjectDocument15 pagesCHAPTER 2 ProjectbonfaceNo ratings yet
- Arasitology: Intestinal AmoebaeDocument5 pagesArasitology: Intestinal AmoebaeMa. Mil Adrianne PamaNo ratings yet
- AmebiasisDocument14 pagesAmebiasisxxxchi chaxxxNo ratings yet
- AMEBIASISDocument19 pagesAMEBIASISDika Herza Pratama100% (1)
- ClinPara AmoebaDocument8 pagesClinPara AmoebaStephen YorNo ratings yet
- PARA20 3rd Long ExamDocument4 pagesPARA20 3rd Long ExamEricNo ratings yet
- (CGPT) B11M4.1Document12 pages(CGPT) B11M4.1adriennemartha.barrientosNo ratings yet
- Me7 o Lab Quiz QuestionsDocument25 pagesMe7 o Lab Quiz QuestionsJen CANo ratings yet
- Case Presentation DysenteryDocument11 pagesCase Presentation Dysenteryjoanne0550% (2)
- 5 30990 1207 PDFDocument2 pages5 30990 1207 PDFWasilla MahdaNo ratings yet
- Parasitology: - IntroductionDocument62 pagesParasitology: - IntroductionHana AliNo ratings yet
- AmebiasisDocument40 pagesAmebiasisAhlam AliNo ratings yet
- Amoebiasis in Wild Mammals: Ayesha Ahmed M Phil. Parasitology 1 Semester 2013-Ag-2712Document25 pagesAmoebiasis in Wild Mammals: Ayesha Ahmed M Phil. Parasitology 1 Semester 2013-Ag-2712Abdullah AzeemNo ratings yet
- AMOEBIASISDocument31 pagesAMOEBIASISpriyagerard100% (1)
- Para Sample QuestionsDocument5 pagesPara Sample QuestionsMaria Christina LagartejaNo ratings yet
- AmoebaDocument5 pagesAmoebasarguss14No ratings yet
- Entamoeba Histolytica: Causes: Amoebiasis. Geog - Distribution: Habitat: Infective Stage: Mode of InfectionDocument46 pagesEntamoeba Histolytica: Causes: Amoebiasis. Geog - Distribution: Habitat: Infective Stage: Mode of InfectionAlfia Nikmah100% (3)
- Parasite and Communicable Disease PDFDocument58 pagesParasite and Communicable Disease PDFDr Dhruva PrasadNo ratings yet
- Amoeba, Flagellates, Ciliates and SporozoansDocument7 pagesAmoeba, Flagellates, Ciliates and SporozoansHani HairullaNo ratings yet
- Report On AmoebiasisDocument36 pagesReport On Amoebiasisrhimineecat71No ratings yet
- Evolutionary Genomics and Population Structure of Entamoeba HistolyticaDocument8 pagesEvolutionary Genomics and Population Structure of Entamoeba HistolyticaMerlina WijayawatiNo ratings yet
- Abses Hepar AmoebaDocument18 pagesAbses Hepar Amoebaaswad 0008No ratings yet