Professional Documents
Culture Documents
Cases Journal: Endogenous Endophthalmitis Caused by Pseudomonas Aeruginosa in A Preterm Infant: A Case Report
Uploaded by
Surendar KesavanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cases Journal: Endogenous Endophthalmitis Caused by Pseudomonas Aeruginosa in A Preterm Infant: A Case Report
Uploaded by
Surendar KesavanCopyright:
Available Formats
Cases Journal
BioMed Central
Open Access
Case Report
Endogenous endophthalmitis caused by Pseudomonas aeruginosa in
a preterm infant: a case report
Sofia Figueiredo*1, Anabela Joo1, Manuela Mateus1, Rosrio Varandas2 and
Leonor Ferraz1
Address: 1Department of Pediatrics - Neonatal Unit, Centro Hospitalar Vila Nova de Gaia/Espinho, EPE, Rua Conceio Fernandes, 4434-502 Vila
Nova de Gaia, Portugal and 2Department of Ofthalmology, Centro Hospitalar Vila Nova de Gaia/Espinho, EPE, Rua Conceio Fernandes, 4434502 Vila Nova de Gaia, Portugal
Email: Sofia Figueiredo* - coxicori@gmail.com; Anabela Joo - joao.anabela@gmail.com; Manuela Mateus - mmateus19@gmail.com;
Rosrio Varandas - rosariovarandas@gmail.com; Leonor Ferraz - leonorferraz@zapp.pt
* Corresponding author
Published: 10 December 2009
Cases Journal 2009, 2:9304
doi:10.1186/1757-1626-2-9304
Received: 5 November 2009
Accepted: 10 December 2009
This article is available from: http://www.casesjournal.com/content/2/1/9304
2009 Figueiredo et al; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Endophthalmitis is an infection of the vitreous or aqueous humor of the eye. Although it rarely
occurs in the neonatal period it has been previously diagnosed in preterm infants.
Endogenous endophthalmitis is when eye infection is secondary to septicemia and represent 20%
of the cases of endophthalmitis. Pseudomonas aeruginosa is responsible for more than 75% of
invasive neonatal eye infections. The course of pseudomonal endophthalmitis is typically fulminant,
developing over hours even in early diagnosis. For survivors, the usual result is blindness of the
affected eye.
We report the case of a preterm infant who developed septicemia and was later diagnosed as
having a pseudomonas endophthalmitis.
Introduction
Endophthalmitis is results from a bacterial or fungal infection of the vitreous or aqueous humor of the eye. It is rare
in the neonatal period only occurring in susceptible individuals such as preterm infants [1,2].
We report the case of a preterm infant who developed septicemia and was later diagnosed as having a pseudomonas
endophthalmitis
Case presentation
Endogenous endophthalmitis represents 20% of the cases
of endophthalmitis and occurs when eye infection is secondary to septicemia [3]. Pseudomonas aeruginosa is an
aggressive gram-negative bacillus and is responsible for
more than 75% of invasive neonatal eye infections
[1,2,4].
A female infant was born at 32 weeks' gestational age by
caesarean delivery. The caesarean was performed after
detection of signs of fetal distress by cardiotocography.
The mother was initially admitted with premature labor
and subsequently treated with two doses of antenatal steroids. The baby weighted 1660 g and had Apgar scores of
7, 7 and 7 at 1, 5 and 10 minutes, respectively.
Acute bacterial endophthalmitis is a vision-threatening
condition and must be managed as an emergency.
On admission the newborn presented moderate respiratory distress syndrome. No other relevant physical signs
Page 1 of 3
(page number not for citation purposes)
Cases Journal 2009, 2:9304
were observed. Chest radiography revealed diffused reticulogranular pattern of the lung. She started on Infant Flow
Driver nasal continuous positive airway pressure (nCPAP)
and received one dose of surfactant. An evaluation for sepsis was performed. In view of the history of premature
labor, she was treated with intravenous (i.v.) ampicillin
and gentamicin and completed a nine day course despite
negative blood cultures.
The newborn was maintained on nCPAP until day 3
(FiO2 max: 32%). Afterwards, she required O2 supplementation (0,5-1 L/min) until the fifth day of hospital
stay.
On the third day a 3/6 systolic murmur was noted after
which an echocardiogram revealed patent ductus arteriosus (PDA) and patent foramen ovale (PFO). She received
a 3 days treatment with i.v. administration of a prostaglandin inhibitor (indomethacin). Closed ductus diagnosis was further confirmed by control echocardiography.
http://www.casesjournal.com/content/2/1/9304
Blood culture revealed Pseudomonas aeruginosa. Antibiotherapy was changed to amicacin and ceftazidime and carried out for 21 days. Cerebrospinal fluid culture was
negative. The sample from mother's caesarean wound also
grew Pseudomonas aeruginosa.
The baby showed progressive clinical improvements.
However the intensive systemic and topical antibiotic
therapy did not prevent intraocular infection deterioration. Indeed proptosis and spontaneous corneal perforation with a purulent discharge occurred. There was no
visual potential. On day 25 an evisceration was performed
and a silicon ocular prosthesis was set. Histological examination of the removed eye showed a supurative inflammatory infiltrate of choroid and retina. This is consistent
with an endophthalmitis's lesion.
Observation of the right eye did not show signs of development of Retinopathy of Prematurity.
Discussion
On day 9 of admission the baby's condition deteriorated
acutely: she was lethargic, with a subicteric tint appearance
and presented important gastric aspirates. A full infection
screen followed by an initial treatment with i.v. amicacin
and vancomycin were performed. Hematologic data
revealed anemia and thrombocytopenia (Hemoglobin 105 g/L; Leucocytes counts - 15.9*109/L with 60% neutrophilis and 36% lynfocytes, platelet count - 102*109/L).
The value of C-reactive protein was 174 mg/L. The analysis of cerebrospinal fluid was normal. On the same day
her mother reported a post-cesarean wound infection and
a wound swab was taken.
Endophthalmitis can be classified as either endogenous or
exogenous, depending on the route of infection. Exogenous endophthalmitis contributes to 80% of the cases of
endophthalmitis and occurs when the eye infection develops as a result of corneal infection, perforating injury or
intraocular surgery [3-5]. Endogenous endophthalmitis
results from hematogenous spread to the eye secondary to
septicemia [4]. We report a case of a newborn that showed
signs of sepsis before ocular's manifestations of endophthalmitis and presented an intact corneal surface at an initial stage. These observations were consistent with a
diagnostic of endogenous endophthalmitis [3,5]. Conjunctival swabs were negative for the presence of pseudomonas whereas blood cultures were positive. These
results also suggested an endogenous source of infection.
In unilateral cases of endogenous endophthalmitis, the
right eye is twice as likely to become infected as the left
eye, probably because of its greater proximity to direct
arterial blood flow [6,7]. In our case the affected eye was
the left one.
On day 10 of admission conjunctival erythema associated
with purulent discharge was observed on the left eye of
the newborn. At this stage it was not possible to visualize
the iris and the pupil due to the development of corneal
clouding. Conjunctival swabs were sent for microbiological investigations and the result was negative for the presence
of
microorganisms.
After
an
urgent
ophthalmological consultation an endophthalmitis with
hypopyon was diagnosed. The patient underwent hourly
topical treatment with tobramicine. Ocular echography
revealed alterations that were suggestive of vitreitis and
retinal detachment.
Organisms previously reported as pathogenic agents of
endophtalmitis include Pseudomonas aeruginosa, group B
streptococci, Haemophilus influenzae type b, Staphylococcus
aureus, Salmonella enteritis, Streptococcus pneumoniae, Neisseria meningitis and Candida species [3]. Pseudomonas is a
virulent organism that produces proteoglycanolytic
enzymes that are able to break down tissue barriers as the
corneal stroma and conjunctival blood vessels [1,3].
Although our patient started at an early stage intensive
intravenous topic antibiotherapy, deterioration of the
intraocular infection was observed. This could be justified
by the high virulence of Pseudomonas.
Due to the fact that the newborn developed physiological
jaundice phototherapy treatment was performed from
day 3 to day 5.
Oral feeds were introduced on day 3 and established by
day 20. From day 2 to day 21 she was on parenteral nutrition through a peripheral catheter.
Page 2 of 3
(page number not for citation purposes)
Cases Journal 2009, 2:9304
Premature infants are particularly vulnerable to Pseudomonas infections [1]. They are immunocompromised
and they often have multiple systemic problems related to
prematurity [3]. Moreover they are depended on a range
of different equipments (humidifiers, incubators, respirators and suction apparatus) that are required to keep them
alive but that can also be a source of nosocomial infection
(when contaminated) [1,3]. In our case the source for the
eye infection could have been the mother's post-caesarean
wound infection caused by Pseudomonas aeruginosa. Furthermore, neonates are unable to complain of eye pain or
of decreasing vision, making early diagnosis more difficult
[3,5,8]. An eye examination is vital in the septic neonate
and should be included by neonatologists as part of the
systemic work-up [2].
Physical findings are correlated with the structures
involved and with the degree of infection. These include:
eyelid swelling and erythema, corneal edema and infection, injected conjunctiva and sclera, purulent discharge,
hypopyon (layering of inflammatory cells and exudate in
the anterior chamber), vitreitis, vitreal mass and debris,
reduced or absent red reflex, limited view of the fundus,
proptosis (a late finding in panophthalmitis) [7,9]. Additionally an ultrasonography could be necessary to establish the diagnosis.
Although organisms can be occasionally cultured from
aspirated vitreous fluid, the diagnosis is established most
frequently from blood cultures [7,9]. In our case aspiration of vitreous fluid was not performed. Culture of the
purulent discharge can be useful but is less reliable for the
identification of the causative organism [4]. Nevertheless,
growth of P. aeruginosa on discharge from an eye of a sick
child should alert the clinician to the risk of life threatening infections [4].
The most appropriate treatment for endogenous endophthalmitis is a combination of intravenous vancomycin
and third-generation cephalosporin or aminoglycoside.
As intraocular accumulation of intravenous antibiotics is
poor, the use of intravitreal antibiotics is indicated [4].
However some case series had shown a poor visual outcome despite treatment with intravitreal antibiotics
[7,10]. In our case the ocular echography that was performed when diagnosis was made revealed retinal detachment, which contraindicate the use of intravitreal
antibiotics. Topical treatment may be also used, but not as
sole treatment [2,4]. Evisceration may be necessary in lifethreatening sepsis or in cases of endphthalmitis unresponsive to antibiotics (as happened with our newborn)
[1].
http://www.casesjournal.com/content/2/1/9304
ity in pseudomonal endophthalmitis are high, even in
early diagnosis [4]. For survivors, the usual result is blindness of the affected eye [2,4].
Consent
Written informed consent was obtained from the patient's
parents for publication of this case report. A copy of the
written consent is available for review by the Editor-inChief of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SF did the literature search and wrote the manuscript. AJ
has been involved in critical revision of manuscript. RV
made the diagnostic and ophthalmologic follow-up, and
performed the evisceration. MM and LF had been involved
in drafting of the manuscript. LF obtained written consent.
All authors read and approved the final manuscript.
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
O'Keefe M, Nolan L, Lanigan B, Murphy J: Pseudomonas Aeruginosa
Endophthalmitis in a Preterm Infant. J AAPOS 2005, 9(3):288-289.
Matasova K, Hudecova J, Zibolen M: Bilateral endogenous endophthalmitis as a complication of late-onset sepsis in premature infant. Eur J Pediatr 2003, 162:346-347.
Wasserman BN, Sondhi N, Carr BL: Pseudomonas-induced bilateral endophthalmitis with corneal perforation in a neonate.
J AAPOS 1999, 3(3):183-184.
Boyle EM, Ainsworth JR, Levin AV, Campbell AN, Watkinson M:
Ophthalmic Pseudomonas infection in infancy. Arch Dis Child
Fetal Neonatal 2001, 85:139-140.
Gaili H, Woodruff GHA: Exogenous Pseudomonas endophthalmitis: a cause of lens enucleation. Arch Dis Child Fetal Neonatal 2002, 86:204-206.
Betrosian AP, Kolomtsas E, Balla M, Papanikolaou M, Labroulis G,
Georgiadis G: Endogenous endophthalmitis. Intensive Cara Med
2000, 26:1714.
Jackson TL, Eykyn SJ, Graham EM, Stanford MR: Endogenous Bacterial Endophthalmitis: A 17-year Prospective Series and
Review of 267 Reported Cases. Surv Opthalmol 2003, 48:403-423.
Tovilla-Canales JL, Nava A, Tovilla y Pomar JL: Orbital and periorbital infections. Curr Opin Ophthalmol 2001, 12:335-341.
Sparks JR, Recchia FM, Weitkamp JH: Endogenous group B streptococcal endophthalmitis in a preterm infant. Journal of Perinatology 2007, 27:392-394.
Eifrig CWG, Scott IU, Flynn HW, Miller D: Endophthalmitis
Caused by Pseudomonas aeruginosa. Ophthalmology 2003,
110(9):1714-1717.
Publish with Bio Med Central and every
scientist can read your work free of charge
"BioMed Central will be the most significant development for
disseminating the results of biomedical researc h in our lifetime."
Sir Paul Nurse, Cancer Research UK
Your research papers will be:
available free of charge to the entire biomedical community
peer reviewed and published immediately upon acceptance
cited in PubMed and archived on PubMed Central
The course of pseudomonal endophthalmitis is typically
fulminant developing over hours. Morbidity and mortal-
yours you keep the copyright
BioMedcentral
Submit your manuscript here:
http://www.biomedcentral.com/info/publishing_adv.asp
Page 3 of 3
(page number not for citation purposes)
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hora Makarand by GunagarDocument143 pagesHora Makarand by GunagarSurendar KesavanNo ratings yet
- Sterilisation of Medical DevicesDocument49 pagesSterilisation of Medical DevicesYogesh BorkarNo ratings yet
- 14 Chapter 8Document28 pages14 Chapter 8Surendar KesavanNo ratings yet
- Aided Prospectus 2018Document16 pagesAided Prospectus 2018Surendar KesavanNo ratings yet
- Bioburden:The Burden On Our Biological OperationsDocument48 pagesBioburden:The Burden On Our Biological OperationsSurendar Kesavan100% (1)
- Continuous Quality Verification: G.K.Raju, PH.DDocument56 pagesContinuous Quality Verification: G.K.Raju, PH.DSurendar KesavanNo ratings yet
- PAT For Biologics: Ensuring Quality of Biologically Produced DrugsDocument19 pagesPAT For Biologics: Ensuring Quality of Biologically Produced DrugsSurendar KesavanNo ratings yet
- Astrology Easy Way of PredictionDocument108 pagesAstrology Easy Way of PredictionSurendar KesavanNo ratings yet
- Validating Sterilization of Medical DevicesDocument16 pagesValidating Sterilization of Medical DevicesSurendar KesavanNo ratings yet
- 2-1 2-2 AsepticProcessingDocument47 pages2-1 2-2 AsepticProcessingKyle Alexander HillegassNo ratings yet
- Comparison of Plate Count Agar and R2A Medium For Enumeration of Heterotrophic Bacteria in Natural Mineral WaterDocument4 pagesComparison of Plate Count Agar and R2A Medium For Enumeration of Heterotrophic Bacteria in Natural Mineral WaterSurendar KesavanNo ratings yet
- Microbial Limit Testing Technology Overview: Advisory Committee For Pharmaceutical ScienceDocument8 pagesMicrobial Limit Testing Technology Overview: Advisory Committee For Pharmaceutical ScienceSurendar KesavanNo ratings yet
- Microbial Control Physical Methods GuideDocument13 pagesMicrobial Control Physical Methods GuideSurendar KesavanNo ratings yet
- 2-5a MediaFillDocument37 pages2-5a MediaFillbeobua100% (1)
- Microbial Limit TestDocument33 pagesMicrobial Limit TestSurendar KesavanNo ratings yet
- Cleaning ValidationDocument38 pagesCleaning ValidationSurendar KesavanNo ratings yet
- 0901001Document7 pages0901001Surendar KesavanNo ratings yet
- Understand and Control Bioburden to Ensure Medical Device SafetyDocument13 pagesUnderstand and Control Bioburden to Ensure Medical Device SafetySurendar KesavanNo ratings yet
- Clean Room BasicsDocument26 pagesClean Room BasicsSurendar KesavanNo ratings yet
- CS January17 2014Document31 pagesCS January17 2014Surendar KesavanNo ratings yet
- Trend Data: Jul 2013 - Dec 2013 Action Limit: 20 Cfu Per PlateDocument3 pagesTrend Data: Jul 2013 - Dec 2013 Action Limit: 20 Cfu Per PlateSurendar KesavanNo ratings yet
- Raw DataDocument1 pageRaw DataSurendar KesavanNo ratings yet
- Review of Cleanroom MicrofloraDocument8 pagesReview of Cleanroom MicrofloraSurendar KesavanNo ratings yet
- The Environmental Monitoring Program in a GMP EnvironmentDocument9 pagesThe Environmental Monitoring Program in a GMP EnvironmentFaisal AbbasNo ratings yet
- Manual On Antimicrobial Susceptibility Testing Dr. M.K. LalithaDocument47 pagesManual On Antimicrobial Susceptibility Testing Dr. M.K. LalithaAntoniuz Liem100% (2)
- J. Bacteriol.-2004-Beck-2766-73Document8 pagesJ. Bacteriol.-2004-Beck-2766-73Surendar KesavanNo ratings yet
- Impact Analysis ReportDocument28 pagesImpact Analysis ReportprasikumarNo ratings yet
- Arai Et Al-1970-Microbiology and ImmunologyDocument6 pagesArai Et Al-1970-Microbiology and ImmunologySurendar KesavanNo ratings yet
- AGM (QC) RecruitmentDocument7 pagesAGM (QC) RecruitmentSurendar KesavanNo ratings yet
- 33513Document24 pages33513Surendar KesavanNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Anorexia NervosaDocument2 pagesAnorexia NervosaDhea Mae MadisNo ratings yet
- Alternator NotesDocument24 pagesAlternator Notesarunima arunimaNo ratings yet
- Smart Asthma ConsoleDocument35 pagesSmart Asthma ConsoleMohamad Mosallam AyoubNo ratings yet
- Basicline BL 21t9stDocument28 pagesBasicline BL 21t9stgabriel6276No ratings yet
- Mercy PlansDocument126 pagesMercy Plansdharry8108No ratings yet
- Conflict and Factional Disputes - Siegel & BealsDocument12 pagesConflict and Factional Disputes - Siegel & BealsDanielNo ratings yet
- Study Plan NCEPU PDFDocument2 pagesStudy Plan NCEPU PDFAhsan100% (1)
- BS 7941-1-2006Document20 pagesBS 7941-1-2006Willy AryansahNo ratings yet
- Plug & Socket TypesDocument49 pagesPlug & Socket TypeskerissaktiemasNo ratings yet
- Management of Septic Shock in An Intermediate Care UnitDocument20 pagesManagement of Septic Shock in An Intermediate Care UnitJHNo ratings yet
- Đánh giá chế độ ăn kiêng: Nhịn ăn gián đoạn để giảm cân- wed HarvardDocument14 pagesĐánh giá chế độ ăn kiêng: Nhịn ăn gián đoạn để giảm cân- wed HarvardNam NguyenHoangNo ratings yet
- Radiesse Pálpebras Gox-8-E2633Document7 pagesRadiesse Pálpebras Gox-8-E2633Camila CrosaraNo ratings yet
- The Focus Shooting Method CourseDocument48 pagesThe Focus Shooting Method CourseKobiXDNo ratings yet
- 3-Ph Induction MotorDocument246 pages3-Ph Induction MotorAn00pgadzillaNo ratings yet
- Hart Transmitter Calibration: Application NoteDocument8 pagesHart Transmitter Calibration: Application NoteThulasi Raman KowsiganNo ratings yet
- Steel 17-4PH MmpdsDocument18 pagesSteel 17-4PH MmpdsManoj ManoharanNo ratings yet
- Ratana Outdoor FurnitureDocument107 pagesRatana Outdoor FurnitureNova TechieNo ratings yet
- HYKDDocument15 pagesHYKDAri RamadhanNo ratings yet
- Tenofovir Disoproxil Fumarate: Riefing - Nfrared BsorptionDocument4 pagesTenofovir Disoproxil Fumarate: Riefing - Nfrared BsorptionMostofa RubalNo ratings yet
- Etabloc Technical DataDocument108 pagesEtabloc Technical Dataedward ksbNo ratings yet
- Avh p6050dvd EngDocument119 pagesAvh p6050dvd EngcaimanaterNo ratings yet
- SEFT Islamic care effect on hypertension patients' blood pressureDocument12 pagesSEFT Islamic care effect on hypertension patients' blood pressureSopian HadiNo ratings yet
- Welding Defects and AcceptanceDocument76 pagesWelding Defects and Acceptancearavindan100% (1)
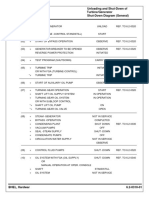
- Steam Turbine Unloading and Shut-Down of Operation Turbine/Generator Shut-Down Diagram (General)Document1 pageSteam Turbine Unloading and Shut-Down of Operation Turbine/Generator Shut-Down Diagram (General)parthibanemails5779No ratings yet
- Présentation Transportation ManagementDocument14 pagesPrésentation Transportation ManagementHiba Hmito100% (1)
- Design and Development of Manually Operated ReaperDocument8 pagesDesign and Development of Manually Operated ReaperIOSRjournalNo ratings yet
- Elimination - Nursing Test QuestionsDocument68 pagesElimination - Nursing Test QuestionsRNStudent1100% (1)
- 5-in-1 Document Provides Lessons on Trees and Environmental ConservationDocument45 pages5-in-1 Document Provides Lessons on Trees and Environmental ConservationPriya DharshiniNo ratings yet
- Ben Wilkins PRISON MADNESS and LOVE LETTERS: THE LOST ARTDocument5 pagesBen Wilkins PRISON MADNESS and LOVE LETTERS: THE LOST ARTBarbara BergmannNo ratings yet
- Wire Rope: - Bright - 6 X 19 - Fibre CoreDocument8 pagesWire Rope: - Bright - 6 X 19 - Fibre CoreQuynh NguyenNo ratings yet