Professional Documents
Culture Documents
Case4 BreastCancer Handout
Uploaded by
Jeremiah HiiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case4 BreastCancer Handout
Uploaded by
Jeremiah HiiCopyright:
Available Formats
Approach to all cases
Solid Organ Malignancy
Breast cancer
What is the diagnosis
Why did it happen
What complications are present (disease / treatment)
Dr Graham Dark
Senior Lecturer in Medical Oncology
graham.dark@ncl.ac.uk
Introduction
UK Cancer incidence and mortality
Breast cancer is the most frequent cancer in women after nonmelanotic skin tumours (32% of female malignancies)
Causes approximately 13,000 deaths per year in the UK
(2002)
The lifetime risk of breast cancer is 1 in 9 women
In England (2001) 80% of patients are alive and disease-free
at 5 years from diagnosis
With improved awareness on the part of both women and
health-care providers, more breast cancers are being
diagnosed while still in-situ
Breast cancer: Rising incidence
Epidemiology of breast cancer
In the UK, the incidence of breast cancer is approximately
42,000 cases per year
It is the commonest cause of death in women aged 3554
years in England
Follows an unpredictable course with metastases presenting
up to 20 years after the initial diagnosis
In England and Wales the 5-year age-standardized survival
rate in 1990 was 62% compared to over 70% in France, Italy
and Switzerland. This has improved recently with earlier
detection by screening and improved treatment
Female to male ratio is approximately 100:1
2014 Centre for Cancer Education
Epidemiology of breast cancer
Reasons for fewer breast cancer deaths
Race
Earlier diagnosis
White women have a higher overall rate of breast cancer than AfricanAmerican women; however, this is not apparent until age 40 and is
marked only after menopause
Breast cancer risk is extremely low in Native American women
Geography
5-fold variation in incidence among different countries, being lower in
Japan, Thailand, Nigeria, and India than in Denmark, the Netherlands,
New Zealand, Switzerland, UK & US
Socioeconomic status
incidence of breast cancer is greater in women of higher socioeconomic
background
Disease site
left breast is more common than the right
One stop clinics
Screening
Better treatment
More women are cured
More cure saves money on subsequent treatments
Those who arent cured are living for longer
More treatments available
Sequential benefits
most common locations of the disease are the upper outer quadrant and
retroareolar region
Breast cancer: Risk factors
Risk of developing breast cancer
Age
By age 30...1 out of 2,525
Family history / personal history
By age 40...1 out of 217
Previous benign breast disease
Reproductive and menstrual history
Early menarche / Late menopause
Nulliparous / late first pregnancy (>35 years)
Oestrogen therapy
By age 50...1 out of 50
By age 60...1 out of 24
By age 70...1 out of 14
By age 80...1 out of 8
OCP
HRT (relative risk 1.66 in long term users)
Radiation
Obesity
Alcohol
Familial breast cancer
Family history of breast cancer
Hereditary predisposition is implicated in around 10% of
breast cancer cases
The overall relative risk of breast cancer in a woman with
a positive family history in a first-degree relative (mother,
daughter, or sister) is 1.7
Multiple affected relatives
Young age at diagnosis
Multiple primary cancers
Male breast cancers
Ovarian cancer
Autosomal dominant pattern of inheritance
Premenopausal onset of the disease in a first-degree
relative is associated with a three-fold increase in risk
Postmenopausal diagnosis increases relative risk by only
1.5
If first-degree relative has bilateral disease: 5-fold risk
increase
If first-degree relative has bilateral disease prior to
menopause: 9-fold risk increase
2014 Centre for Cancer Education
Breast cancer genes
Characteristics of BRCA associated cancer
BRCA1
Younger age of onset
BRCA2
Frequent bilateral occurrence
p53 (Li-Fraumeni syndrone)
Worse histological features:
more aneuploidy
Others
Cowden syndrome (breast & GI cancers, thyroid disease)
higher grade
Ataxia telangiectasia
higher proliferation indices
Peutz-Jeghers syndrome
higher proportion hormone receptor negative
Presenting symptoms
Clinical signs
Mammographic findings: discovered in asymptomatic patients
through the use of screening mammography
Neck and axilla: lymphadenopathy
Breast lump: the most common presenting complaint. The
incidence can range from 65-76% of patients
Pagets disease: associated with intraductal carcinoma
involving the terminal ducts of the breast and may have an
associated invasive component. Presents as an eczematoid
change in the nipple, a breast mass, or bloody nipple
discharge
Other local symptoms
Nipple: discharge or retraction
Breast: discolouration, oedema, peau dorange,
erythema, nodules, ulceration, lack of symmetry, skin
thickening
Chest: signs of consolidation, nodules in skin
Abdomen: hepatomegaly
Breast pain 5%
MS: focal tenderness in axial and peripheral skeleton
Breast enlargement 1%
Distant metastases:
Skin or nipple retraction 5%
Nipple discharge 2%, nipple crusting or erosion 1%
bone 70%, lung 60%, liver 55%, pleura 40%, adrenals 35%, skin
30%, brain 1020%
Pagets disease of the breast
Erythematous keratotic patches
over the areola area
Extramammary Pagets is
associated with internal
malignancy in 50% cases
2014 Centre for Cancer Education
Breast self-examination
Evaluation of a cystic mass
Recommendation to begin monthly breast self-examination at
the age of 20
Fine-needle aspiration (FNA)
If the mass is a cyst it can simply be aspirated with a fine
needle, which should yield non-bloody fluid and result in
complete resolution of the lesion
Ultrasonography
Used to determine whether a lesion is solid or cystic, and
whether a cyst is simple or complex
Biopsy
A biopsy is indicated if the cyst fluid is bloody, the lesion does
not resolve completely after aspiration, or the cyst recurs after
repeated aspirations
Meta-analysis of 12 studies involving a total of 8,118 patients
with breast cancer correlated the performance of breast selfexamination with tumour size and regional lymph node status
Women who performed breast self-examination were more
likely to have smaller tumours and less likely to have axillary
node metastases than those who did not
A major problem with breast self-examination as a screening
technique is that it is rarely performed well. Only 2-3% of
women do an ideal examination a year after instruction has
been provided
Cystic carcinoma accounts for < 1% of all breast cancers
An intraluminal solid mass is a concerning sign suggesting
(intra) cystic carcinoma, and should be biopsied
Evaluation of a solid mass
Evaluation of a non-palpable mass
The decision to observe a patient with a breast mass that
appears to be benign should be made only after careful
clinical, radiological, and cytological examinations
Mammography
To assess radiological characteristics of the mass and
evaluation of the remainder of the ipsilateral breast as well as
the contralateral breast
FNA
Simple method for obtaining material for cytological
examination. False-positive results from 0%-2.5% and falsenegatives varies from 3-27%
Biopsy
A core biopsy (18 gauge or larger needle biopsy) can be
advantageous since architectural as well as cellular
characteristics can be evaluated. An excisional biopsy, in
which the entire breast mass is removed, definitively
establishes the diagnosis
Wire excision biopsy
Tumour marker: CA 15.3
Pathology
Elevated serum levels found in 12.5% of women with benign breast
disease, preoperatively in 11% of women with operable breast
cancer, and in 64% of women with metastatic breast cancer
Invasive ductal carcinoma
Has no value in screening because of low sensitivity for the early
stages of disease
Invasive lobular carcinoma
False positive: Elevated in gynaecological cancers
CA 15.3 elevation increases with increasing stage of disease and
highest levels are seen in patients with liver or bone metastases
It is not accurate enough to be used alone to define response
Several trials have shown that a rising CA 15.3 level during follow-up
can detect relapse 2-9 months before clinical signs or symptoms
develop
Rising levels indicated recurrence in 73% of those with a recurrence
and in 6% of those without a recurrence
2014 Centre for Cancer Education
Stereotactic-guided core biopsies
Ultrasound-guided core biopsies
Breast MRI
With or without ductal carcinoma in situ is the commonest
histology accounting for 70%
Accounts for most of the remaining cases
Ductal carcinoma in situ (DCIS)
20% of screen-detected breast cancers. It is multifocal in onethird of women and has a high risk of becoming invasive (10%
at 5 years following excision only). Pure DCIS does not cause
lymph node metastases, although these are found in 2% of
cases where nodes are examined, owing to undetected
invasive cancer
Lobular carcinoma in situ (LCIS)
A predisposing risk factor for developing cancer in either breast
(7% at 10 years)
Breast cancer: Triple assessment
Clinical examination
Breast imaging
Mammography
Ultrasound
MRI
Fine needle aspiration
Needle core biopsy
Mammotome (vacuum assisted biopsy)
Cytological assessment
Reported as
C1-5
1: no cells
2: insufficient
3: normal
4: suspicious
5: malignant
Predictive value of investigations
Modality Imaging
Cytology Risk of
Cancer %
Disposable cutting needle
5
7.3
22.5
69.3
95.1
13.6
2.3
8.0
40.3
85.2
5.3
0.8
3.0
19.4
67.3
11.6
1.9
6.8
36.0
82.8
83.5
43.2
73.6
95.6
99.5
99.2
94.8
98.5
99.8
100
0 or 1
2014 Centre for Cancer Education
HercepTest staining guide
O
Negative
No staining is observed or
membrane staining is observed in
less than 10% of the tumour cells
1+
Negative
Faint membrane staining is detected
in more than 10% of tumour cells.
The cells are only stained in part of
their membrane
2+
Weak
Positive
Weak to moderate complete
membrane staining is observed in
more than 10% of the tumour cells
3+
Strong
Positive
Moderate to strong complete
membrane staining is observed in
more than 10% of the tumour cells
Radioisotope bone scan
FISH for HER-2
Normal gene copy
number
Amplified gene copy
number
Bone metastasis
Most of the people who die of cancer each year have
tumour metastasis
Bone is the third most common organ involved by
metastasis, behind lung and liver
In breast cancer, bone is the second most common site of
metastatic spread, and 90% of patients dying of breast
cancer have bone metastasis
Breast and prostate cancers metastasise to bone most
frequently, which reflects the high incidence of both of
these tumours, as well as their prolonged clinical courses
Other tumours that commonly cause symptomatic bone
metastases include kidney and thyroid cancer, and
multiple myeloma
Bone metastasis
Bone metastasis
Patients with bone metastasis from breast cancer have
an average 2-year survival from the time of presentation
with their first bone lesion
There are four main goals in managing patients with
metastatic disease to the skeleton:
More patients are living with bone metastases, and thus
the challenge is to improve their quality of life
Early detection and aggressive management of
metastases is the goal
Maintain and maximize patients' quality of life and
functional level
Currently, care is optimised in only a fraction of patients
with bone metastases
2014 Centre for Cancer Education
pain relief
preservation and restoration of function
skeletal stabilization
local tumour control (e.g., relief of tumour impingement on
normal structures, prevention of release of chemical
mediators that have local and systemic effects)
Spinal cord compression
Spinal cord compression
Diagnosis is clinical
The finding of bilateral UMN signs should be considered
spinal cord compression until proved otherwise
confirmation can only be
made radiologically
SCC from metastatic cancer remains an important source
of morbidity despite the fact that with early diagnosis,
treatment is effective in 90% of patients
MRI is investigation of choice :
Thoracic 70%
Malignant spinal cord compression is defined as the
compressive indentation, displacement, or encasement of
the spinal cord's thecal sac by metastatic or locally
advanced cancer
Lumbar 15%
Cervical 10%
Sacral 5%
Any neoplasm capable of metastasis or local invasion can
produce malignant spinal cord compression
Spinal cord compression
Spinal cord compression
Response to nonsurgical therapy and the duration of
survival following treatment can vary considerably among
different histological tumour types
Tumour type
Frequency %
The degree of pretreatment neurological dysfunction is
the strongest predictor of treatment outcome
Breast cancer
29
Lung cancer
17
Ambulation can be preserved in greater than 80% of
patients who are ambulatory at presentation
Prostate
14
Myeloma
Key to successful management is a heightened
awareness of signs and symptoms, specifically newly
developed back pain or motor dysfunction, leading to
early diagnosis and treatment.
Renal
Lymphoma
Leptomeningeal metastasis
Sarcoma
Other
23
TNM Staging
T
CSF
Primary tumours
T0
T1
No palpable tumour
Tumour <=2cm
T2
T3
Tumour > 2cm but < 5cm
Tumour > 5cm in greatest dimension
T4
Tumour of any size fixed with direct extension to chest wall, skin, rib
intercostal muscles, serratus anterior muscle (not pectoral muscle)
N Regional lymph nodes
N0
No palpable homolateral lymph nodes
N1a Palpable nodes, not felt to contain tumour
N1b Palpable nodes thought to contain tumour
N2
Nodes > 2cm or fixed to one another or other structures
N3
Supraclavicular or infraclavicular nodes involved
M Distant metastases
M0
M1
2014 Centre for Cancer Education
No evidence of distant metastases
Distant metastases present including skin involvement beyond the breast area
Survival by number of involved axillary nodes
Number of
positive nodes
Percent Surviving
100
0
1
2-3
4-5
80
60
6-10
11-15
16-20
40
21 or more
20
0
1
2
3
Years after diagnosis
Lymph node surgery
Progression through lymph nodes
Sentinel
98.7% - orderly progression
Radioisotope/Blue dye directed sample
Sample
4-6 nodes from the lower axilla sampled
Level 1
Lateral to pectoralis minor
54% - level 1 only
23% - levels 1 & 2
21% - levels 1, 2 & 3
1.2% - level 2 skipping level 1
0.1% - level 3 skipping levels 1 & 2
Level 2
Posterior to pectoralis minor
Level 3
Medial to pectoralis minor
Who to stage for early breast cancer
Staging results
1076 patients, Early Breast Cancer Trial
30 (2.8%) patients found to have distant metastases
All were asymptomatic
130 (12.0%) suspected but not confirmed on CT, MRI or
PET
All staged with CXR, US, bone scan
All suspicious findings explored further with CT, MRI or
PET
7 of these 130 confirmed to have metastases within 6
months
916 (85.2%) metastases excluded
2014 Centre for Cancer Education
Risk factors for distant metastasis
Recommendation for staging
> 3 involved lymph nodes (p=0.06)
Tumour > 5 cm
> 10 involved nodes (p=0.002)
> 3 Nodes (clinically palpable nodes)
T3/4 tumour (p=0.08)
Clinical suspicion
36/37 patients with metastatic disease had one of these
risks
All should have CXR, US, bone scan
36/269 (13.4%) with risk factors had metastasis
1/807 (0.12%) without risk factors had metastasis
1 in 7.5 will have metastases
1 in 800 will be missed
Recommendation for staging
Breast cancer treatment
CT or MRI are used if there is a clinical suspicion of
metastasis
Surgery
Tumour markers? (not as part of staging )
Radiotherapy
Hormone therapy
Chemotherapy
Biological therapy
Everything else
Breast cancer: Radiotherapy
NCN Guidelines for radiotherapy
Mandatory for the conserved breast
Breast conserving surgery
May be used as an alternative to surgery to the axilla
Radiotherapy to the chest wall and/or axilla reduces the
local recurrence rate in patients who have heavy lymph
node infiltration
Radiotherapy to lymph node areas improves cause
specific survival
2014 Centre for Cancer Education
All patients
Post mastectomy
All tumours > 5cm
Tumours deep in the breast where surgical clearance is
3mm or less
All patients with 4 or more lymph node metastases
Use of tamoxifen: Oxford overview 1995
Aromatase inhibitors
Some advantages compared to tamoxifen for diseasefree survival
% Reduction in mortality
% Reduction in recurrence
Only of value in POSTMENOPAUSAL women
No clear advantage in survival except in extended
adjuvant setting
Trial data for aromatase inhibitors ab initio or after 2/3 or
5 years of tamoxifen
Incidence of contralateral breast cancer
Adjuvant chemotherapy
Use of cytotoxic drugs to reduce the risk of recurrence
and death
Number 60
of
50
cases
40
HR
95% CI
p-value
HR+
0.47
(0.290.75)
0.001
ITT
0.58
(0.38-0.88)
0.01
53
5 DCIS
Newer drugs
CMF > Surgery alone
Anthracyclines > CMF
30
26
20
5 DCIS
21
Invasive*
10
0
Trials have shown incremental advantages with the
addition of:
48
Invasive*
Taxanes > Anthracyclines
Different combination strategies
Increase in dose density
Anastrozole
(n=2618)
Tamoxifen
(n=2598)
Block sequential regimens
*p=0.001 for invasive cancers
Effect of polychemotherapy vs. control
Anthracycline vs. CMF: Overall survival
100
80.2%
80
68.0%
76.7%
3.6% (SE 0.8)
60
63.4%
4.6% (SE 1.2)
40
Actuarial estimate and SE:
allocated A/E+
allocated CMF
0
Annual death rates
A/E+
CMF
5
Years 0-4
10
Years 5-9
4.40% (SE 0.12) 3.63% (SE 0.17)
5.07% (SE 0.15) 3.81% (SE 0.20)
years
Years 10+
2.87% (SE 0.36)
4.16% (SE 0.59)
Deaths/woman-years
A/E+
CMF
2014 Centre for Cancer Education
1246/28305
1219/24067
470/12940
372/9758
64/2233
49/1177
10
Addition of taxanes: Overall survival
Breast cancer prevention
Mastectomy
100
92%
90
Ovarian ablation
TAC
Drugs
% Alive
87%
Surveillance
FAC
80
70
# Events
TAC
60
57
FAC
76
Total
133
RR
p-value
0.76
0.11
50
0
Number at Risk
TAC 745
FAC 746
12
18
24
Months
30
36
42
48
741
738
732
728
718
713
393
375
171
171
24
33
1
1
700
678
Risk reducing mastectomy
Surgical oophorectomy in BRCA1 carriers
Reduces risk of breast cancer because it reduces volume
of breast tissue
In patients with BRCA mutations, risk is reduced to 1%
Tamoxifen: NSABP P1 Trial
Tamoxifen: NSABP P1 Trial
13388 women at increased risk of breast cancer
Tamoxifen 20 mg/day
x 5 years
(6681)
2014 Centre for Cancer Education
Placebo daily
x 5 years
(6707)
11
NSABP P1 Trial: endometrial cancer
NSABP P1 Trial: Results
Tamoxifen advantages
49% less invasive cancer (p<0.00001)
50% less DCIS (p<0.002)
Only prevented ER+ tumours
Tamoxifen disadvantages
2.53 x more endometrial cancer
Increased DVT and PE risk
No clear cut impact on SURVIVAL
Aromatase inhibitors in prevention
Breast surveillance in young women
Secondary prevention has been an endpoint in adjuvant
studies of aromatase inhibitors
Increasing evidence that the combination of
mammography and MRI is superior to either modality
alone
Aromatase inhibitors reduce contralateral cancer
incidence
Ultrasound has little or no value as a screening tool
Now being used in prevention trials in postmenopausal
women
Breast cancer: Summary
Timely and accurate diagnosis
Appropriate staging investigations
Meticulous surgery
Appropriate post surgical therapy
Radiotherapy
Hormones
Chemotherapy
Targeted therapies
Treatment should be tailored to the patient and to cancer
biology
2014 Centre for Cancer Education
12
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- NRP Guidelines Flyer English FINALDocument2 pagesNRP Guidelines Flyer English FINALJeremiah HiiNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- CPG Management of Acute ST Segment Elevation Myocardial Infarction STEMI 3rd Edition 2014 PDFDocument106 pagesCPG Management of Acute ST Segment Elevation Myocardial Infarction STEMI 3rd Edition 2014 PDFNeesha SundraNo ratings yet
- Resident Ortho RotationDocument18 pagesResident Ortho RotationRuth PoeryNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 7 How To Write A Report and Presentation v3Document7 pages7 How To Write A Report and Presentation v3Jeremiah HiiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- CSIM ACS LectureDocument60 pagesCSIM ACS LectureJeremiah HiiNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- MC GlothinDocument27 pagesMC GlothinJeremiah HiiNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Asia Chart IscosDocument2 pagesAsia Chart IscosJeremiah HiiNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Unusual DiabetesDocument32 pagesUnusual DiabetesJeremiah HiiNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- ConstipationDocument4 pagesConstipationJeremiah HiiNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
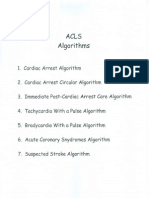
- Acls AlgorithmsDocument8 pagesAcls Algorithmsdydy_7193No ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Acute Spinal InjuryDocument8 pagesAcute Spinal InjuryJeremiah HiiNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- F4 EverDocument1 pageF4 EverJeremiah HiiNo ratings yet
- Common Surgical PresentationsDocument49 pagesCommon Surgical PresentationsJeremiah HiiNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Femoral Neck FractureDocument6 pagesFemoral Neck FractureJeremiah HiiNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- MuetDocument8 pagesMuetJeremiah HiiNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Critical AppraisalDocument13 pagesCritical AppraisalSigit Harya Hutama100% (2)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- 1985 2000 Al Chem EssayDocument62 pages1985 2000 Al Chem EssayEunice_Chong_2134No ratings yet
- ESUR Quick Guide: To Female Pelvis ImagingDocument80 pagesESUR Quick Guide: To Female Pelvis ImagingGallicoAulioNo ratings yet
- Association of Intratumoral Microbiota With Prognosis in Patients With Nasopharyngeal Carcinoma From 2 Hospitals in ChinaJAMA OncologyDocument9 pagesAssociation of Intratumoral Microbiota With Prognosis in Patients With Nasopharyngeal Carcinoma From 2 Hospitals in ChinaJAMA OncologyAiden LiangNo ratings yet
- Ohtas 15 1Document39 pagesOhtas 15 1indahNo ratings yet
- Efektifitas Latihan Progressive Muscle Relaxation (PMR) Terhadap Mual Muntah Kemoterapi Pasien Kanker OvariumDocument8 pagesEfektifitas Latihan Progressive Muscle Relaxation (PMR) Terhadap Mual Muntah Kemoterapi Pasien Kanker OvariumMutmin AnsariNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Papers For Students - Candidates List 4 - 19-4Document1 pagePapers For Students - Candidates List 4 - 19-4Thiago Negrão ChubaNo ratings yet
- A Radiologist's Guide To The 2021 WHO Central Nervous System Tumor ClassificationDocument15 pagesA Radiologist's Guide To The 2021 WHO Central Nervous System Tumor ClassificationMANGNo ratings yet
- Don Interstitial BrachytherapyDocument53 pagesDon Interstitial BrachytherapyRajalakshmi RadhakrishnanNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Chemo Practice ProblemsDocument12 pagesChemo Practice ProblemsSamNo ratings yet
- Phytotherapy On CancerDocument21 pagesPhytotherapy On CancerSiddhendu Bhattacharjee100% (1)
- Daftar Pustaka: Universitas Kristen MaranathaDocument9 pagesDaftar Pustaka: Universitas Kristen MaranathaErica ValenciaNo ratings yet
- Hyperthermic Intraperitoneal Chemotherapy - Hipec-: Rusie Daniel, Medic Rezident Chirurgie GeneralaDocument23 pagesHyperthermic Intraperitoneal Chemotherapy - Hipec-: Rusie Daniel, Medic Rezident Chirurgie GeneralaDaniel RusieNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Best Practice & Research Clinical Obstetrics and GynaecologyDocument5 pagesBest Practice & Research Clinical Obstetrics and GynaecologyGeorge CarpNo ratings yet
- GI Polyps DR OdzeDocument30 pagesGI Polyps DR OdzeJuliana Do CoutoNo ratings yet
- Breast - DCIS.Bx 1.0.1.0.REL CAPCPDocument6 pagesBreast - DCIS.Bx 1.0.1.0.REL CAPCPkarimahihdaNo ratings yet
- Onco, TSG & CancerDocument8 pagesOnco, TSG & Cancersumera120488No ratings yet
- Histological Classifi Cation of Breast CancerDocument12 pagesHistological Classifi Cation of Breast Cancersilviailie100% (1)
- Journal Club: Dr. Preethi.S DNB Resident Ent 31/03/23Document27 pagesJournal Club: Dr. Preethi.S DNB Resident Ent 31/03/23PreethiNo ratings yet
- Pre-Invasive Lesions of The Cervix 2020Document58 pagesPre-Invasive Lesions of The Cervix 2020Jeno Luis J. ACUBNo ratings yet
- Uterine Neoplasms: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document112 pagesUterine Neoplasms: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Bianca IoanaNo ratings yet
- SOX17 Enables Immune Evasion of Early Colorectal Adenomas and CancersDocument33 pagesSOX17 Enables Immune Evasion of Early Colorectal Adenomas and Cancersannaba85No ratings yet
- PathologyDocument4 pagesPathologyVISHAKHANo ratings yet
- Targeted Percutaneous Microwave Ablation at The Pulmonary Lesion Combined With Mediastinal Radiotherapy With or Without Concurrent Chemotherapy inDocument8 pagesTargeted Percutaneous Microwave Ablation at The Pulmonary Lesion Combined With Mediastinal Radiotherapy With or Without Concurrent Chemotherapy inMalekseuofi مالك السيوفيNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- (Medical Radiology) Jack F. Fowler (Auth.), Seymour H. Levitt, James a. Purdy, Carlos a. Perez, Philip Poortmans (Eds.) - Technical Basis of Radiation Therapy_ Practical Clinical Applications-SpringerDocument1,145 pages(Medical Radiology) Jack F. Fowler (Auth.), Seymour H. Levitt, James a. Purdy, Carlos a. Perez, Philip Poortmans (Eds.) - Technical Basis of Radiation Therapy_ Practical Clinical Applications-SpringerPiotr JankowskiNo ratings yet
- Oral Patho For DR ARA Khan Soft Form PDFDocument43 pagesOral Patho For DR ARA Khan Soft Form PDFreema aslamNo ratings yet
- Clinical Breast Problems and Unusual Breast Conditions - Radiology Key PDFDocument16 pagesClinical Breast Problems and Unusual Breast Conditions - Radiology Key PDFdivyanshu kumarNo ratings yet
- Radiation Therapy For Sarcomas and Skin CancersDocument376 pagesRadiation Therapy For Sarcomas and Skin CancersAr-pardo RogerNo ratings yet
- TOC Prof Chintamanis Comprehensive Book On SurgeryDocument4 pagesTOC Prof Chintamanis Comprehensive Book On SurgeryKoustav ChakrabortyNo ratings yet
- Dermoscopy of Facial LesionsDocument55 pagesDermoscopy of Facial LesionssajithaNo ratings yet
- LeiomiosarcomaDocument8 pagesLeiomiosarcomaYosset Emilet Rodrìguez CalderònNo ratings yet
- Biopsy Report LakshmananDocument1 pageBiopsy Report LakshmananRJIO NAGPURNo ratings yet