Professional Documents
Culture Documents
Anatomy of the Peritoneum and Peritoneal Cavity
Uploaded by
wardahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anatomy of the Peritoneum and Peritoneal Cavity
Uploaded by
wardahCopyright:
Available Formats
Peritoneum & Peritoneal Cavity
- Peritoneum continuous, glistening, slippery transparent serous membrane, lines abdominopelvic cavity
and invests the viscera.
- Consists of continuous layers: the parietal peritoneum (lines the internal surface of the abdominopelvic
wall) and the visceral peritoneum (invests viscera such as the stomach and intestines). Both consist of
mesothelium
- Parietal peritoneum served by the same blood and lymphatic vasculature and the same somatic nerve
supply as is the region of the wall it lines. It is sensitive to pressure, pain, heat and cold, and laceration.
Pain here is well localized, except on the inferior surface of the central part of the diaphragm, where
innervation is provided by the phrenic nerves; irritation is often referred to the C3C5 dermatomes over
the shoulder.
- Visceral peritoneum and the organs it covers are served by the same blood and lymphatic vasculature
and visceral nerve supply. It is insensitive to touch, heat and cold, and laceration; it is stimulated
primarily by stretching and chemical irritation. Pain produced is poorly localized, referred to the
dermatomes of the spinal ganglia providing the sensory fibers, particularly to midline portions of these
dermatomes. Pain from foregut derivatives epigastric region, midgut derivatives umbilical region,
hindgut derivatives pubic region.
- Peritoneum and viscera are in the abdominopelvic cavity. The relationship of the viscera to the peritoneum
is as follows:
Intraperitoneal organs : almost completely covered with visceral peritoneum (stomach, spleen).
Intraperitoneal organs have conceptually, if not literally, invaginated into the closed sac, like pressing
fist into inflated balloon.
Extraperitoneal, retroperitoneal, and subperitoneal organs : outside the peritoneal cavityexternal to
the parietal peritoneumand only partially covered with peritoneum (usually on just one surface).
Kidneys (retroperitoneal) are between the parietal peritoneum and the posterior abdominal wall and
have parietal peritoneum only on anterior surfaces (with variable amount of intervening fat).
Subperitoneal urinary bladder has parietal peritoneum only on superior surface.
- Peritoneal cavity : within abdominal cavity, continues inferiorly into the pelvic cavity. A potential space of
capillary thinness between the parietal and visceral layers of peritoneum. Contains no organs, but a thin
film of peritoneal fluid, composed of water, electrolytes, etc derived from interstitial fluid in adjacent
tissues.
- It lubricates the peritoneal surfaces, enabling viscera to move without friction, allowing movements of
digestion. Contains leukocytes and antibodies to resist infection. Lymphatic vessels, particularly on
inferior surface of diaphragm, absorb the peritoneal fluid.
- Peritoneal cavity is completely closed in males, but there is a communication pathway in females.
Peritoneal Formations
Various terms are used to describe the parts of the peritoneum that connect organs with other organs or to
the abdominal wall, and the compartments and recesses that are formed as a consequence.
-
Mesentery double layer of peritoneum, occurs as a result of the invagination of the peritoneum by
an organ and constitutes a continuity of the visceral and parietal peritoneum. It provides neurovascular
communications between organ and body wall.
Mesentery connects an intraperitoneal organ to the body wallusually the posterior abdominal wall.
Mesenteries related to other specific parts are named accordinglythe transverse and sigmoid
mesocolons, mesoesophagus, mesogastrium, and mesoappendix.
Mesenteries have a core of CT containing blood and lymphatic vessels, nerves, lymph nodes, and fat.
Omentum double-layered extension or fold of peritoneum that passes from the stomach and
proximal part of the duodenum to adjacent organs in the abdominal cavity.
Greater omentum prominent, 4-layered peritoneal fold, hangs down from the greater curvature
of the stomach and the proximal part of the duodenum. After descending, it folds back and attaches to
the anterior surface of the transverse colon and its mesentery.
Lesser omentum much smaller, double-layered peritoneal fold, connects lesser curvature of the
stomach and the proximal part of the duodenum to the liver. It also connects the stomach to a triad of
structures that run between the duodenum and liver in the free edge of the lesser omentum.
Peritoneal ligament double layer of peritoneum, connects an organ with another organ or to the
abdominal wall.
The liver is connected to the:
Anterior abdominal wall by the falciform ligament.
Stomach by the hepatogastric ligament, the membranous portion of the lesser omentum.
Duodenum by the hepatoduodenal ligament, the thickened free edge of the lesser omentum,
which conducts the portal triad: portal vein, hepatic artery, and bile duct. The hepatogastric and
hepatoduodenal ligaments are continuous parts of the lesser omentum and are separated only for
descriptive convenience.
The stomach is connected to the:
Inferior surface of the diaphragm by the gastrophrenic ligament.
Spleen by the gastrosplenic ligament, which reflects to the hilum of the spleen.
Transverse colon by the gastrocolic ligament, the apronlike part of the greater omentum, descends
from greater curvature, turns under, then ascends to the transverse colon. All these structures are part
of the greater omentum, separated only for descriptive purposes.
Bare areas area that is not covered to allow the entrance or exit of neurovascular structures.
Formed in relation to the attachments of the peritoneal formations to the organs, including
mesenteries, omenta, and ligaments that convey the neurovascular structures.
Peritoneal fold reflection of peritoneum that is raised from the body wall by underlying blood
vessels, ducts, and ligaments formed by obliterated fetal vessels (e.g., the umbilical folds on the
internal surface of the anterolateral abdominal wall).
Peritoneal recess, or fossa, pouch of peritoneum formed by a peritoneal fold (e.g., inferior recess
of the omental bursa between greater omentum, and the supravesical and umbilical fossae between
the umbilical folds).
Subdivisions of Peritoneal Cavity
-
Peritoneal cavity is divided into the greater and lesser peritoneal sacs.
Greater sac is the main and larger part of the peritoneal cavity. The omenta bursa (lesser sac) lies
posterior to the stomach and lesser omentum.
The transverse mesocolon (mesentery of the transverse colon) divides the abdominal cavity into a
supracolic compartment, containing the stomach, liver, and spleen, and an infracolic
compartment, containing the small intestine and ascending and descending colon.
The infracolic compartment lies posterior to the greater omentum and is divided into right and left
infracolic spaces by the mesentery of the small intestine.
Free communication occurs between the supracolic and the infracolic compartments through the
paracolic gutters, the grooves between the lateral aspect of the ascending or descending colon and
the posterolateral abdominal wall.
Omental bursa extensive sac-like cavity that lies posterior to the stomach, lesser omentum, and
adjacent structures. Has a superior recess, limited superiorly by the diaphragm and the posterior
layers of the coronary ligament of the liver, and an inferior recess between the superior parts of the
layers of the greater omentum.
Omental bursa permits free movement of the stomach because the anterior and posterior walls of the
omental bursa slide smoothly over each other.
Omental bursa communicates with the greater sac through the omental foramen (epiploic foramen),
an opening posterior to the free edge of lesser omentum (hepatoduodenal ligament).
The boundaries of the omental foramen are
Anteriorly: the hepatoduodenal ligament, containing the hepatic portal vein, hepatic artery, and bile
duct
Posteriorly: the IVC and a muscular band, the right crus of the diaphragm, covered anteriorly with
parietal peritoneum.
Superiorly: the liver, covered with visceral peritoneum.
Inferiorly: the superior or first part of the duodenum.
Physiology of Peritoneum
-
Helps protect the organs in the abdomen and keeps them in place.
Makes a lubricating fluid (peritoneal fluid) that helps organs move smoothly against each other inside
the abdomen as we move around and allowing movements of digestion. It also contains leukocytes and
antibodies to resist infection.
The peritoneum is a semipermeable membrane with an extensive surface area, much of which overlies
blood and lymphatic capillary beds. Water & solutes may diffuse through peritoneal membrane.
Therefore, fluid injected into the peritoneal cavity is absorbed rapidly. Anesthetic agents, may be
injected into the peritoneal cavity by intraperitoneal (I.P.) injection. In renal failure, waste products
accumulate in the blood and tissues and ultimately reach fatal levels. Peritoneal dialysis may be
performed in which soluble substances and excess water are removed from the system by transfer
across the peritoneum.
The greater omentum, prevents visceral peritoneum from adhering to the parietal peritoneum. The
greater omentum also cushions the abdominal organs against injury and forms insulation against loss
of body heat.
You might also like
- DIGESTIVE Lecture Notes PDFDocument20 pagesDIGESTIVE Lecture Notes PDFAaliya Minar100% (4)
- Dr. Reynaldo V. Lopez Senior Lecturer Department of AnatomyDocument55 pagesDr. Reynaldo V. Lopez Senior Lecturer Department of AnatomyMohammad AliNo ratings yet
- Round Rock Independent School District: Human ResourcesDocument6 pagesRound Rock Independent School District: Human Resourcessho76er100% (1)
- Peritoneum: General FeaturesDocument92 pagesPeritoneum: General FeaturestuhinsinghNo ratings yet
- (Evolutionary Psychology) Virgil Zeigler-Hill, Lisa L. M. Welling, Todd K. Shackelford - Evolutionary Perspectives On Social Psychology (2015, Springer) PDFDocument488 pages(Evolutionary Psychology) Virgil Zeigler-Hill, Lisa L. M. Welling, Todd K. Shackelford - Evolutionary Perspectives On Social Psychology (2015, Springer) PDFVinicius Francisco ApolinarioNo ratings yet
- SHS Track and Strand - FinalDocument36 pagesSHS Track and Strand - FinalYuki BombitaNo ratings yet
- Peritoneal Anatomy Lecture NotesDocument4 pagesPeritoneal Anatomy Lecture Noteschc300No ratings yet
- Felomino Urbano vs. IAC, G.R. No. 72964, January 7, 1988 ( (157 SCRA 7)Document1 pageFelomino Urbano vs. IAC, G.R. No. 72964, January 7, 1988 ( (157 SCRA 7)Dwight LoNo ratings yet
- Peritoneum and Peritoneal CavityDocument26 pagesPeritoneum and Peritoneal CavitytuhinsinghNo ratings yet
- Gastrointestinal AnatomyDocument70 pagesGastrointestinal AnatomyNatasya Ryani PurbaNo ratings yet
- The Free Little Book of Tea and CoffeeDocument83 pagesThe Free Little Book of Tea and CoffeeNgopi YukNo ratings yet
- English: Quarter 1 - Module 1Document16 pagesEnglish: Quarter 1 - Module 1Ryze100% (1)
- Peritoneum and Gastro-Intestinal TractDocument108 pagesPeritoneum and Gastro-Intestinal TractKAYISIRE EMERYNo ratings yet
- A. 2019. 07. Peritoneum DPTDocument39 pagesA. 2019. 07. Peritoneum DPTAzhar Ahmed SoomroNo ratings yet
- Peritoneum 2022Document86 pagesPeritoneum 2022Tayyib KhanNo ratings yet
- Peritoneum & Peritoneal Cavity PresentationDocument59 pagesPeritoneum & Peritoneal Cavity Presentationsaint thuggerNo ratings yet
- PeritoneumDocument53 pagesPeritoneumtuhinsinghNo ratings yet
- By: Ameer Ali Abbas Hassan First Stage (A4)Document7 pagesBy: Ameer Ali Abbas Hassan First Stage (A4)Ahmed AliNo ratings yet
- 4 Peritoneum PDFDocument64 pages4 Peritoneum PDFN ANo ratings yet
- The Peritoneum and Abdominal OrgansDocument34 pagesThe Peritoneum and Abdominal Organsandrea titusNo ratings yet
- Peritoneum, Peritoneal Cavity, and Diaphragm 11-6-15-1Document67 pagesPeritoneum, Peritoneal Cavity, and Diaphragm 11-6-15-1Deny ShajiniNo ratings yet
- PERITONITISDocument45 pagesPERITONITISMariam KajaiaNo ratings yet
- Prak 1 AbdomenDocument19 pagesPrak 1 Abdomen22712055No ratings yet
- PeritoneumDocument39 pagesPeritoneumtuhinsinghNo ratings yet
- Ac 2Document104 pagesAc 2saide limNo ratings yet
- Peritoneum. Development of The Digestive System: Department of Human Anatomy Lecturer Dr. Globa LilianDocument24 pagesPeritoneum. Development of The Digestive System: Department of Human Anatomy Lecturer Dr. Globa LilianCristina GrajdeanNo ratings yet
- Peritoneum Ab CavityDocument6 pagesPeritoneum Ab CavityrohitNo ratings yet
- Abdomen AnatomyDocument9 pagesAbdomen AnatomyPhan Hoàng SơnNo ratings yet
- Introduction To The Abdominal Cavity and Viscera Study ObjectivesDocument16 pagesIntroduction To The Abdominal Cavity and Viscera Study Objectivesacoolz90No ratings yet
- Organ IntraperiotnealDocument13 pagesOrgan Intraperiotnealfera novisarlitaNo ratings yet
- 1 Abdominal VisceraDocument45 pages1 Abdominal VisceraMero HamedNo ratings yet
- 3.digestive SystemDocument103 pages3.digestive Systemokoti.omutanyi22No ratings yet
- UNIT 9 (Digestive System)Document8 pagesUNIT 9 (Digestive System)Workinesh Kaynabo KambaloNo ratings yet
- Peritoneal CavityDocument1 pagePeritoneal CavityRizki Adi SantosaNo ratings yet
- Anatomy of the PeritoneumDocument11 pagesAnatomy of the PeritoneumLeona Tinotenda ManjeruNo ratings yet
- The Peritoneum. The Peritoneal Cavity. The Development of The Peritoneum. The Histology of Tonsils PDFDocument9 pagesThe Peritoneum. The Peritoneal Cavity. The Development of The Peritoneum. The Histology of Tonsils PDFredderdatNo ratings yet
- Peritoneum Vertical Disposition 2Document112 pagesPeritoneum Vertical Disposition 2Noor KhanNo ratings yet
- Peritoneum 1Document47 pagesPeritoneum 1Mohd FardeenNo ratings yet
- Med II GIT 2 Peritoneum Aug 23Document24 pagesMed II GIT 2 Peritoneum Aug 23Suhayb CumarNo ratings yet
- AbdomenDocument26 pagesAbdomenOlivia Chandra DeviNo ratings yet
- Body Cavities and MembranesDocument31 pagesBody Cavities and MembranesMary AkellaNo ratings yet
- The AbdomenDocument3 pagesThe AbdomenotaNo ratings yet
- Abdominal CavityDocument78 pagesAbdominal Cavitytanishapatel1005No ratings yet
- Lecture 4Document14 pagesLecture 4X RamboNo ratings yet
- Abdominal WallDocument6 pagesAbdominal WallIfeanyichukwu OgbonnayaNo ratings yet
- Peritoneum & Peritoneal CavityDocument1 pagePeritoneum & Peritoneal CavityHugh SmithNo ratings yet
- Amboss - GITDocument16 pagesAmboss - GITAllysahNo ratings yet
- Nec BC2 Ut5Document9 pagesNec BC2 Ut5miriam garrido blancoNo ratings yet
- 2 Anatomy of The Abdominal VisceraDocument9 pages2 Anatomy of The Abdominal VisceraLinh PhanNo ratings yet
- 4rd Lecture - AbdomenDocument26 pages4rd Lecture - AbdomenZainab Jamal SiddiquiNo ratings yet
- Abdominal Wall Lec 1Document17 pagesAbdominal Wall Lec 1Gul Rukh MohmandNo ratings yet
- Referat PeritonitisDocument18 pagesReferat PeritonitisWilliam Grandinata Soeseno100% (2)
- Abdominal Cavity Anatomy ReviewDocument15 pagesAbdominal Cavity Anatomy ReviewCaperlac MarjorieNo ratings yet
- 7) Anatomy of OMENTUMDocument22 pages7) Anatomy of OMENTUMGoodone OneNo ratings yet
- 5.2 AbdomenDocument4 pages5.2 Abdomensaxman011No ratings yet
- 8.-ANATOMY and Physiology GIDocument12 pages8.-ANATOMY and Physiology GIAngelica Cassandra VillenaNo ratings yet
- Anatomy of The Abdomen (1) : - IntroductionDocument21 pagesAnatomy of The Abdomen (1) : - IntroductionMunachande KanondoNo ratings yet
- Course Code: Ran 1206 Course Title: Radiography Anatomy IiDocument9 pagesCourse Code: Ran 1206 Course Title: Radiography Anatomy IisamuelNo ratings yet
- Abdominal Wall Lec 1Document17 pagesAbdominal Wall Lec 1Mohmand KhanNo ratings yet
- Anatomy and Physiology of Colon of Case StudyDocument4 pagesAnatomy and Physiology of Colon of Case StudySimran JosanNo ratings yet
- Anatomy: Know Your Abdomen: GlossaryDocument5 pagesAnatomy: Know Your Abdomen: GlossaryNaida KapetanovicNo ratings yet
- Chapter 6 Alimentry System PDFDocument51 pagesChapter 6 Alimentry System PDFNasir MunirNo ratings yet
- Peritoneal Cavity Anatomy in CT PeritoneographyDocument24 pagesPeritoneal Cavity Anatomy in CT PeritoneographyHugo Alberto C FNo ratings yet
- The Abdomen: Stuart M BuntDocument36 pagesThe Abdomen: Stuart M BuntEmmy BankzNo ratings yet
- The Small Intestine-1Document38 pagesThe Small Intestine-1ChiderahNo ratings yet
- Transportation ProblemDocument12 pagesTransportation ProblemSourav SahaNo ratings yet
- SyllabusDocument8 pagesSyllabusrickyangnwNo ratings yet
- Critiquing a Short Story About an Aged MotherDocument2 pagesCritiquing a Short Story About an Aged MotherJohn Rey PacubasNo ratings yet
- Study Habits Guide for Busy StudentsDocument18 pagesStudy Habits Guide for Busy StudentsJoel Alejandro Castro CasaresNo ratings yet
- Reduce Home Energy Use and Recycling TipsDocument4 pagesReduce Home Energy Use and Recycling Tipsmin95No ratings yet
- WAS Argumentative EssayDocument4 pagesWAS Argumentative EssayJandresNo ratings yet
- Cover Letter IkhwanDocument2 pagesCover Letter IkhwanIkhwan MazlanNo ratings yet
- Dr. Xavier - MIDocument6 pagesDr. Xavier - MIKannamundayil BakesNo ratings yet
- Syllabus Sibos CLTDocument5 pagesSyllabus Sibos CLTgopimicroNo ratings yet
- Does social media improve or impede communicationDocument3 pagesDoes social media improve or impede communicationUmar SaleemNo ratings yet
- Konsep SRA (Sekolah Ramah Anak) Dalam Membentuk Budaya Islami Di Sekolah DasarDocument10 pagesKonsep SRA (Sekolah Ramah Anak) Dalam Membentuk Budaya Islami Di Sekolah Dasarsupriyono hasanNo ratings yet
- Understanding Abdominal TraumaDocument10 pagesUnderstanding Abdominal TraumaArmin NiebresNo ratings yet
- Adorno - Questions On Intellectual EmigrationDocument6 pagesAdorno - Questions On Intellectual EmigrationjimmyroseNo ratings yet
- Part 4: Implementing The Solution in PythonDocument5 pagesPart 4: Implementing The Solution in PythonHuỳnh Đỗ Tấn ThànhNo ratings yet
- Chapter 1Document11 pagesChapter 1Albert BugasNo ratings yet
- DODAR Analyse DiagramDocument2 pagesDODAR Analyse DiagramDavidNo ratings yet
- Final DSL Under Wire - FinalDocument44 pagesFinal DSL Under Wire - Finalelect trsNo ratings yet
- 2-Library - IJLSR - Information - SumanDocument10 pages2-Library - IJLSR - Information - SumanTJPRC PublicationsNo ratings yet
- Das MarterkapitalDocument22 pagesDas MarterkapitalMatthew Shen GoodmanNo ratings yet
- Lcolegario Chapter 5Document15 pagesLcolegario Chapter 5Leezl Campoamor OlegarioNo ratings yet
- Intel It Aligning It With Business Goals PaperDocument12 pagesIntel It Aligning It With Business Goals PaperwlewisfNo ratings yet
- Entrepreneurship and Small Business ManagementDocument29 pagesEntrepreneurship and Small Business Managementji min100% (1)
- Compund and Complex Sentences ExerciseDocument3 pagesCompund and Complex Sentences ExerciseTimothyNo ratings yet
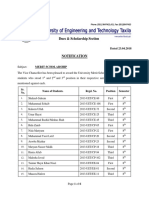
- Dues & Scholarship Section: NotificationDocument6 pagesDues & Scholarship Section: NotificationMUNEEB WAHEEDNo ratings yet