Professional Documents
Culture Documents
Circulation 1973 ALONSO 588 96
Uploaded by
Jessica AROriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Circulation 1973 ALONSO 588 96
Uploaded by
Jessica ARCopyright:
Available Formats
Pathophysiology of Cardiogenic Shock
Quantification of Myocardial Necrosis, Clinical, Pathologic
and Electrocardiographic Correlations
By DANIEL R. ALONSO, M.D., STEPHEN SCHEIDT, M.D., MARTIN POST, M.D.,
AND
THOMAS KILLIP, M.D.
SUMMARY
Clinical and pathologic data were correlated in 22 patients with cardiogenic shock and 10 "control" patients who died suddenly after infarction without shock. A pathologic technique of ventricular mapping allowed quantification of recent as well as old infarction. Total left ventricular
(LV) damage averaged 51% (range 35-68%) in the shock patients and 23% (range 14-31%) in
the control group. Shock was associated with recent infarction (all 22 patients), old infarction
(21 patients) and extension of infarction (18 patients). Extension, often in a subepicardial manner, averaged 6% of LV mass (range 3-10%) in 18 patients with shock; it preceded shock in
four, coincided with the onset of shock in six, and followed shock in seven patients with shock.
In contrast, small extensions averaging 2% of LV mass were found in three, and multiple recent
infarctions in two control patients. Although progressive myocardial damage was a common
pathologic finding, it was infrequently recognized clinically. The electrocardiogram reflected evidence of recent infarction in 56%, old infarction in 31%, and extension in only 30% of patients.
These data suggest that appropriate early therapeutic intervention might limit myocardial damage by preventing extension or reinfarction. Since shock was best correlated with total LV damage, such limitation of infarction might reduce the incidence and mortality of cardiogenic shock.
Additional Indexing Words:
Quantification of infarct size
Myocardial infarction
Extension of infarction
therapy directed at limiting the amount of myocardial damage during the episode of acute infarction
might reduce the incidence and mortality of
cardiogenic shock.
CARDIOGENIC shock remains the major cause
of death among patients hospitalized with
acute myocardial infarction.' Mortality is high in
spite of pharmacologic agents, mechanical circulatory assistance and surgery. Development of
optimal therapy requires better understanding of
the pathophysiology of the cardiogenic shock
syndrome.
We present herein a detailed clinical-pathologic
study of patients who died with cardiogenic shock.
The data demonstrate that shock is associated with
massive myocardial damage and that myocardial
injury frequently occurs in a stepwise or progressive
fashion. Interruption of the cycle of clinical
deterioration and progressive damage through
Methods
Clinical, physiologic and postmortem studies have
been obtained in 32 patients over a two-year period.
Twenty-two patients died with cardiogenic shock
complicating acute myocardial infarction. All had intraarterial systolic pressure less than 90 mm Hg and
abnormal renal or cerebral perfusion manifested by
hourly urine flow less than 20 ml or abnormalities of
mental status. Hypovolemia was excluded either by
measurement of left ventricular filling pressure, which
exceeded 12 mm Hg whenever obtained, or by trial
expansion of intravascular volume. Severe pain, significant arrhythmias, disorders of electrolyte or acid base
balance, and abnormalities of ventilation or oxygenation
were corrected whenever possible.
The findings in the patients with shock were
compared to those of a control group, composed of ten
patients who died suddenly and unexpectedly during
convalescence in the hospital following acute myocardial infarction.
Table 1 lists characteristics of the shock and control
groups. Differences in age, time of admission to the
Cardiac Care Unit and total duration of illness between
From the Departments of Pathology and Medicine, the
New York Hospital-Cornell Medical Center, New York, New
York.
Supported by USPHS Contract PH 43-67-1439.
Address for reprints: Daniel R. Alonso, M.D., Department
of Pathology, The New York Hospital-Cornell Medical
Center, 525 East 68th Street, New York, New York 10021.
Received February 26, 1973; revision accepted for
publication April 25, 1973.
588
Circulation, Volume XLVIII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
PATHOPHYSIOLOGY OF CARDIOGENIC SHOCK
Table 1
Comparison of Patient Groups
Cardiogenic
shock
Sudden
death after
myocardial
infarction
22
N
10
Male
14
6
Female
8
4
Age, mean (range)
66 (50-85) 70 (57-89)
Median time from
clinical "moment of infarction"
to CCU admission, hr
6
13
Median survival after infarction,
hr
100
172
Number of patients with
complications at CCU admission
none
9
4
mild or moderate CHF
6
6
2
pulmonary edema
0
4
cardiogenic shock
0
Median time from infarction to
onset of shock, hr, (range)
66 (0-331)
Median survival after onset of
42
shock, hr
Abbreviations: CCU = Cardiac Care Unit, CHF = congestive heart failure.
the two groups are not statistically significant. Patients
who developed shock did so at varying times after
admission. Only seven of the 22 patients developed
shock within 24 hr of the acute myocardial infarct.
In the group who died suddenly two patients had
ventricular rupture and eight had unexpected cardiac
arrest.
589
accomplished by sectioning the heart in a
standardized manner, determining the degree of
necrosis in each standard segment and calculating total
damage through comparison with data obtained from
was
normal hearts. The method employed is a modification
of one originally devised by Dr. Donald B. Hackel of
Duke University Medical Center.
The method is as follows: After completion of
arteriography the crux of the heart was identified. A cut
was made 2 cm below the crux parallel to the
atrioventricular groove (fig. 1). Thus, the heart was
divided into a basal and a ventricular portion. The
latter was then cut into six equal and parallel coronal
slices. These coronal slices were labelled A through F,
from the apex to the base. The ventricular myocardium
of the basal portion was separated by sharp dissection
from the atria along the atrioventricular groove and
labelled G.
Each of the seven coronal slices (A through G) was
then cut into six radial segments in a standard manner.
The interventricular septum was divided into equal
anterior and posterior halves (segments 5 and 1
respectively). The perimeter of the epicardial aspect of
the remaining free wall of the left ventricle was
measured with a flexible plastic ruler and divided into
three equal segments. The segments were labelled 4
(anterior), 3 (lateral) and 2 (diaphragmatic). The
entire free wall of the right ventricle was separated and
assigned number 6, but was not included in the
calculation to follow. Thus a total of 35 segments (5
Pathologic Studies
The heart was removed intact from the chest. A
radiograph was obtained in various projections, and the
coronary arteries were then perfused with a mixture of
barium sulfate and gelatin through polyethylene
catheters placed in each coronary ostium and secured
by a ligature around the origin of the vessel. A
nonpulsatile perfusion pressure of 100 mm Hg was
applied until all visible epicardial branches were filled.
At the completion of the perfusion, the heart was fixed
by immersion in a solution of 20% formalin for 48 hr.
Care was taken to fill the cardiac chambers with
formalin to complete fixation. The heart was weighed
before and after fixation; no significant difference in the
weights was found.
After 48 hr of fixation radiographs of the heart were
obtained in four projections. The coronary arteries were
then dissected free from the epicardial surface. The
entire length of major vessels was resected. The arteries
were decalcified in 7% nitric acid for 24-48 hr,
according to the amount of calcium present in each
vessel. Radiographs were taken of isolated coronary
arteries by placing them directly on mammography Xray film.
Quantification of infarcted ventricular myocardium
sulcus
Figure 1
(Top) Method of sectioning the heart for quantification ot
ventricular myocardial damage. (Bottom) Method of dividing each coronal slice of myocardium into radial segments.
Five radial segments (1-5) in each of 7 coronal slices (A-G)
provide 35 standard segments comprising the entire mass of
the left ventricular myocardium.
Circulation, Volume XLVIII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
590
ALONSO ET AL.
radial segments in each of 7 coronal slices) of
myocardium of left ventricular wall and interventricular
septum was obtained.
In the hearts from patients with shock or sudden
death, areas of myocardial infarction and fibrosis were
identified grossly and mapped in each coronal section.
Microscopic sections were then obtained from areas of
obvious infarction as well as from grossly normal
myocardium. A minimum of 20 large blocks of left
ventricular myocardium were studied microscopically in
each heart.
The technique of sectioning the heart in a standard
manner was performed in 25 normal adult hearts
obtained at autopsy from patients who died from
noncardiac causes. The percent contribution of each
standard segment to the total left ventricular weight of
the normal heart is shown in figure 2.
In hearts with infarction, viable myocardium in each
standard segment was estimated by gross and microscopic observations. If viable myocardium was totally
absent, either due to recognizable recent necrosis or as
a result of old infarction with subsequent fibrosis and
loss of mass, the percent of left ventricular mass
represented by that standard segment (as determined
from the expected percent in the 25 normal hearts)
was subtracted from 100%. If, for example, the anterior
septal segment in section G (fig. 2) was totally
infarcted, the necrosis represented 5.5% of ventricular
mass. Loss of myocardium in part of a standard
A nterior
segment was subtracted in proportion to the amount of
damage or loss of tissue in the segment. Thus this
method accounts for not only recognizable recent
damage, but also old necrosis which has resulted in loss
of ventricular mass.
The age of infarcts was estimated by conventional
histopathologic criteria.2-4 Three categories were established: recent infarct (less than 2 weeks old),
intermediate infarct (2 weeks to 3 months old) and old
infarct (more than 3 months old). While this separation
according to age was both workable and useful, it is
recognized that aging of a myocardial infarct is not a
precise process.
Results
The hearts of patients who died with cardiogenic
shock showed massive left ventricular destruction
and the extent of infarction was significantly greater
than in the patients who died without shock. Thus
the total mass of left ventricular infarction averaged
51% (range 35-68%) in the 22 patients with shock
and 23% (range 14-31%) in the ten patients with
sudden death (fig. 3). The mass of old or
intermediate infarction was not different in the
shock and sudden death groups; the highly
significant difference in total infarction between the
two groups was explained by the difference in mass
of recent infarction which averaged 31% in the
DEATH DUE TO ACUTE MYOCARDIAL INFARCT:
SUMMARY OF LEFT VENTRICULAR DAMAGE
HISTOLOGIC
AGE OF INFARCT
60
w
LU
RECENT
INTERMEDIATE
. 2
- 50
WEEKS TO 3 MONTHS)
OLD
U-1
'
Z 40
p<.001
U 30
p< 001
z
lit
20
LLJ
-:
K')
-,
ns
10
CARDIOGENIC
SHOCK n=22
Figure 2
Mean percent of left ventricular myocardial mass contained
in each of the 35 standard segments as determined from
25 normal hearts.
DIED SUDDENLY
(NON-SHOCK) n 10
=
Figure 3
Mass of left ventricular infarction in 22 patients who died
from cardiogenic shock compared to 10 with sudden death.
There is no significant difference in mass of old (clear portion
of bar) or intermediate (lightly stippled) infarction. The
highly significant difference in mass of total infarction is
explained by the much larger recent infarction (dark stippling) in the shock patients.
Circulation, Volume XLVlII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
PATHOPHYSIOLOGY OF CARDIOGENIC SHOCK
shock group but only 12% in the sudden death
group.
Figure 4 depicts the distribution of damage by
age of infarct in each of the patients with shock and
sudden death. The relative proportions of old,
intermediate and recent damage are highly variable. In 16 of the 32 patients most of the myocardial
damage was due to recent necrosis. Six patients,
only two of whom died from shock, had relatively
small recent infarcts combined with larger old or
intermediate infarets. In general, the appearance of
shock seems best correlated with total left ventricular damage.
Duration of Shock
The 22 patients with shock were divided into two
groups according to the clinical duration of shock.
Group 1 consisted of patients in shock longer than
24 hr. Group 2 was comprised of patients who died
within 24 hr of the onset of shock. The mean
duration of shock was 88 hr for Group 1 and 12 hr
for Group 2. The two groups do not differ
70
significantly with respect to the total or recent mass
of left ventricular infarction, the frequency or mass
of extension, or the extent of coronary artery
thrombosis (table 2). Figure 5 demonstrates that
there is no relationship between the mass of left
ventricular infarct and the duration of shock. Thus
length of survival following the onset of shock does
not appear to influence the pathologic findings.
Extension of Infarction
An infarct was considered to have extended when
myocardial necrosis of a more recent vintage was
demonstrated at the edges of an established infarct.
This was distinguished from "multiple recent
infarction" (hereafter "reinfarction"), where several
discrete infarcts in scattered locations were apparent.
Two patterns of extension, type A and type B,
were observed. Type A extension occurred at the
edges of a subendocardial infarct, usually involving
the subepicardial aspect of the ventricular wall.
Type B extension developed at the lateral margins
DEATH DUE TO ACUTE M)(OCARDIAL INFARCT:
LEFT VENTRICULAR DAMAGE
AGE OF INFARCT
60
LU
RECENT
INTERMEDIATE
CLi
591
(2 WEEKS TO 3 MONTHS)
50
OLD
U-
z 40
U30-
z
LUJ
> 20U-
LU
~10
CARDIOGENIC SHOCK
n =22
DIED SUDDENLY
(NON -SHOCK) n = 10
Figure 4
Mass of left ventricular infarction in individual patients.
Circulation, Volume XLViII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
592
ALONSO ET AL.
Table 2
of Duration of Sih~ock on Pathologic Findings
Influence
Grouip 1
shock
(duiration
2
Groulp
Rapid
demise
(dturation
12
88
12
<.001
54t
47
32
NS
NS
Prolonged
>24 hrs)
N
Mlean duration of shock,
onset to death, hr
Mass of LV inifarct,
%7C of LV
\lass of recent LV infarct.,
% of LV
Extension of infarction,
patients
Mass of extension,
%c of LV
Recent coronary artery
thrombosis, patients
Abbreviations: LV
<24
36
1.
(89%0/)
5.4
hrs)
10 (83%) NS
NS
4. 7
6 (67%)
left, ventricle, NS
10 (83%c) NS
=
sudden death group, comprising 2, 2 and 3% of left
ventricular mass, respectively.
Seven of the patients in the shock group and one
in the sudden death group had two or more
anatomically distinct reinfarctions.
The pathologic determination of the infarets
recognized at autopsy was correlated with clinical
events as described in the medical record. Chronologic relationships for the 22 patients are depicted
in figure 7 and table 3. Extension or reinfarction
followed the onset of shock in seven patients. In six
patients an extension or reinfarction clearly preceded and perhaps precipitated shock. In six
instances the onset of shock and extension or
reinfarction occurred at about the same time, so
that the pathophysiologic sequence could not be
determined.
not significant
of transmural infarcts since no viable subepicardial
myocardium remained (fig. 6).
Extension of infarction was observed in 18 of the
22 shock patients but in only 3 of the 10 sudden
death patients (P < .005). Type A extension
occurred in 9 and type B extension in 9 of the 18
patients with shock in whom extension was
documented. The mass of left ventricle involved by
extension averaged 6% (range 3-10%) in the shock
group. There were three small extensions in the
RELATIONSHIP BETWEEN MASS OF LEFT VENTRICULAR
INFARCT AND DURATION OF CARDIOGENIC SHOCK
70r-
60
.0
00
z
U 50
ui
00
*
0
40
z
> 30
0
e 20
10
I1
0
20
40
60
80
100
120
140
160
DURATION OF SHOCK, HOURS
Figure 5
Figure 6
Mass of left ventricular infarct plotted against the duration
of cardiogenic shock. Apparent lack of any relationship suggests that shock itself is not responsible for the pathologic
findings.
Schematic representation of two types of extension of myocardial infarction. Type A (top) was observed at the edges
of an infarct, usually subepicardially. Type B (bottom)
occurred at the lateral margins.
Circulation, Volume XLVIII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
PATHOPHYSIOLOGY OF CARDIOGENIC SHOCK
200
180
160
140
100
120
593
80
60
40
20
HOURS BEFORE DEATH
Figure 7
Chronologic relationships between clinical and pathologic events in the
22 patients dying from cardiogenic shock. The age of infarction, extension or reinfarction was estimated by standard pathologic techniques and is shown as a range of minimum to maximum estimated age. Original infarcts have been
omitted where they occurred long before the clinical onset of shock. Table 3 s-ummarizes the relationships shown here.
Arranging the data in another way, the onset of
shock was related to the original infarct in 9
episodes of shock, followed extension or reinfarction
in 6, occurred simultaneously with extension or
reinfaretion in 6, and was not closely related to an
obvious pathologic event in 3 instances.
Coronary Artery Pathology
Thrombosis was common. in both groups of
patients. Recent occlusive thrombosis of major
coronary arteries was found in 16 of the 22 (72%)
patients with shock and 6 of the 10 (60%) patients
with sudden death. The thrombi averaged 18.4 mm
Table 3
Chronologic Relationships between Infarction, Extension, Reinfarction and Shock
Clinical onset of shock:
(episodes of shock)
Extension or reinfarction
(patients)
Followed shock
Preceded shock
Occurred simultaneously with the
onset of shock
No extension or reinfarction
6
6
3
22
Related to original infarct
Followed extension or reinfarction
Occurred simultaneously with extension
or reinfarction
No obvious pathologic event
Circulation, Volume XLVIII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
6
6
3
24
594
ALONSO ET AL.
(range 2.0 to 52.0 mm) in length in the shock
and 28.6 mm (range 13.0 to 47.0 mm) in the
sudden death group. The presence and size of
recent thrombi could not be correlated with the
duration of shock, survival after the onset of acute
myocardial infarction or the presence, type or mass
of extension.
Table 4 compares the distribution of major
coronary artery stenoses ( >75% of luminal area) in
the shock and sudden death patients. Extensive
three-vessel disease was the dominant finding in
patients who died with cardiogenic shock, but 3
patients had involvement of one vessel only (left
anterior descending coronary artery in two, right
coronary artery in one).
ELECTROCARDIOGRAPHIC DIAGNOSIS
AND EXTENT OF INFARCTION
group,
o TRANSMURAL INFARCT
A CENTRAL
1 NON-TRANSMURAL
O SUBENDOCARDIAL J INFARCT
70r
RECENT INFARCTION
LUJ
U
W
60k
0
50k
LL
Electrocardiographic Correlations
Scalar electrocardiograms were evaluated for
evidence of old and new myocardial infarction
using standard criteria.5 Forty discrete old infarcts
were identified pathologically in the 32 patients.
Electrocardiographic diagnosis was not possible in
six instances because of left bundle branch block,
acute infarction in the same location as old
infarction (thus obscuring any old changes) or
inadequate electrocardiograms. Of the remaining 34
old infarctions, only 12 (35%) could be diagnosed
from the scalar electrocardiogram (fig. 8).
Of the 38 discrete recent infarcts identified
pathologically, chronologically suitable electrocardiograms were available in 33 instances. Nineteen
of the 33 acute infarctions (58%) could be
diagnosed from the electrocardiogram.
In 19 instances of acute transmural infarction, an
average of 32% of left ventricular mass was
destroyed. Of these transmural infarcts, only three
could not be diagnosed from the electrocardiogram,
for a diagnostic accuracy of 84%. In contrast, 19
acute nontransmural infarcts were small, averaging
12.5% of left ventricular mass. Only four nontransmural infarcts were apparent from the electrocardiogram, for a diagnostic accuracy of 21% (fig. 8).
OLD INFARCTION
40H
0
0
:D
0
0
z 30k
LU
U-
LUJ
-J
20h
0:
00
0
0
a
a
10
0
00
00
*:
0
000
00
I .
v
00
ECG DIAGNOSTIC
ECG DIAGNOSTIC
NON- DiAGNOSTIC
NON- DIAGNOSTIC
Figure
Diagnostic utility of the standard scalar electrocardiogram
according to mass and type (transmural, central or subendocardial) of infarction. Transmural infarctions were larger and
usually produced diagnostic electrocardiographic changes.
In ten instances an electrocardiogram was
available after the presumed chronologic time of
extension of infarction. In only three of these
instances could acute injury (new ST-segment
elevation or Q wave) be recognized electrocardio-
graphically.
Discussion
Table 4
Coronary Artery Pathology in Patients with Shock and
Sudden Death
Shock
Major coronary vessels
wxith > 75 c, c stenosis
1 vessel
2 vessels
3 vessels
Abbreviation. pts
pts
Co
3
7
12
14
32
54
patients.
Sudden death
pts
%
2
6
2
20
60
20
This study demonstrates that when cardiogenic
shock complicates acute myocardial infaretion,
massive left ventricular infarction is to be expected.
Furthermore, the extent of myocardial damage is
much greater in patients who die from shock than
in those who die unexpectedly while convalescing
in the hospital from acute infarction. Our observations are in agreement with recent clinical-pathologic studies in which the mass of left ventricular
Circulation, Volume XLVIII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
PATHOPHYSIOLOGY OF CARDIOGENIC SHOCK
infarction was established by other pathologic
techniques.6' 7, 8 The difference in mass of infarcted
left ventricle between the cardiogenic shock and
sudden death groups is highly significant and is not
related to the duration of shock, the use of drugs or
of mechanical circulatory assistance with the intraaortic counterpulsating balloon.
On the average, more than half of the left
ventricular mass is destroyed in patients who die
from cardiogenic shock. Stated another way, in the
patients with cardiogenic shock less than half of the
left ventricular myocardium remains to maintain
ventricular function. The theoretical consequences
of such loss of myocardium are considered with
reference to a conceptual model by Swan et al.9
Under certain circumstances, loss of half of the left
ventricular myocardium is sufficient to explain the
hemodynamic and clinical consequences of shock,
and contractility of the remaining viable tissue need
not be impaired. One implication of this analysis is
that preservation of functioning myocardium is of
paramount importance. Current and past experience have amply demonstrated that therapy directed at the remaining viable tissue (which is
already functioning at normal or perhaps abovenormal levels of contractility) does little to improve
salvage.
We have further shown that patients dying
during hospitalization from myocardial infarction
often have a stepwise increase or progression of
myocardial necrosis, usually from marginal extension of infarction. Thus, extension was found in 18
of 22 patients with shock but in only three of ten
with sudden death. Multiple recent infarctions were
found in seven patients with shock and two with
sudden death. Page et al. observed extension to be
present only in patients with shock and suggested
that extension was a consequence of the shock
state.8 In our patients, although extension followed
the onset of shock in some, it clearly preceded (and
perhaps caused) shock in others. These observations indicate that extension is an important
mechanism resulting in progressive myocardial
necrosis following acute myocardial infarction.
Extension of infarction is often a process which
goes unrecognized clinically. None of the three
extensions recognized pathologically in the patients
with sudden death were suspected despite close
observation in a cardiac care unit. In the patients
with shock, only three of ten electrocardiograms
available after the presumed time of extension
demonstrated an acute injury pattern. Only three of
the 18 extensions were suspected clinically because
595
of renewed or protracted chest pain. Although
diagnosis of extension is infrequent, the process
may not be silent. Perhaps more frequent recording
of electrocardiograms, serial precordial ST-segment
maps or assay of serum enzymes several times daily
would improve diagnostic accuracy.
The limitations of the standard scalar electrocardiogram in the diagnosis of myocardial infarction
have been previously recognized.10' 11 In our study,
after excluding patients with left bundle branch
block and intraventricular block, old infarction
could be diagnosed in only 31% and acute infarction
in only 59% of hearts with pathologically confirmed
areas of myocardial necrosis. Our findings closely
parallel those of Levine and Phillips.12 Infarcts that
are nontransmural, diaphragmatic and posterior, or
those that comprise less than 10% of left ventricular
mass are often not apparent electrocardiographically. At least part of the difficulty is due to the fact
that a significant Q wave, evidence of a transmural
scar, is generally necessary for diagnostic certainty.
Others have noted the inadequacies of the electrocardiogram in the diagnosis of purely subendocardial infarction.10' 13 It must be recognized therefore,
that although cardiogenic shock is usually temporally related to acute infarction or recent extension,
the electrocardiogram will be of diagnostic value
only about half of the time.
There was a preponderance of patients with
disease of all three major coronary arteries in the
shock group, although three patients developed
shock with a single major coronary artery occlusion.
The frequency of coronary thrombosis encountered
in our patients with shock is comparable to that
reported by Page.8 The incidence of thrombi in the
sudden death group, higher than that reported in
other studies of sudden death,'4 is probably
explained by the fact that our group comprised
hospitalized patients who died suddenly during
convalescence, often many days following acute
infarction. Other studies of sudden death generally
deal with patients dying within a short time of the
onset of symptoms. Our inability to determine the
age of thrombus precludes any attempt to establish
a causal relationship between thrombosis and
infarction or extension of the original injury.
The apparent temporal association between
extension of infarction and the clinical onset of
shock suggests that progression of myocardial
damage plays an important role in the pathogenesis
of shock. Extension probably represents loss of
viability of an ischemic zone which surrounds the
initial infarct.'5-17 Infarction of this zone of
Circulation, Volume XLVIII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
596
ALONSO ET AL.
marginal viability could be precipitated by any
factor that unfavorably influences its metabolic
milieu. The balance of factors which regulate
metabolic demands and the supply of nutrients to
the myocardium becomes crucial in controlling the
progressive necrosis which may follow the initial
insult. Perhaps treatment designed to improve
oxygenation and substrate utilization or to reduce
myocardial oxygen needs can enhance the viability
of the marginal ischemic zone. The hypothesis that
progressive loss of functioning myocardium following acute infarction is preventable requires further
investigation as specific therapeutic interventions
are critically evaluated. Limitation of myocardial
damage, rather than intensive therapy after cardiogenic shock is manifest, may succeed in reducing
both the incidence and mortality of progressive
power failure complicating acute myocardial infarction.
References
1. SCHEIDT S, ASCHEIM R, KILLIP T: Shock after acute
myocardial infarction. Amer J Cardiol 26: 556,
1971
2. MALLORY GK, WHITE PD, SALCEDO-SALGAR J: The
speed of healing of myocardial infarction: A study of
the pathologic anatomy in seventy-two cases. Amer
Heart J 18: 647, 1939
3. LODGE-PATCH I: The ageing of cardiac infarcts and its
influence on cardiac rupture. Brit Heart J 13: 37,
1951
4. WHO SCIENTIFIC GROUP: The pathologic diagnosis of
acute ischemic heart disease. WHO Technical Report
Series No. 441. Geneva, World Health Organization,
1970
5. BLACKBURN H, KEYS A, SIMONSON E, RAUTAHARJU P,
PUSAR S: The electrocardiogram in population
studies: A classification system. Circulation 21: 1160,
1960
6. BOOLOOKI H, LEMBERG L, GHAHRAMANI A,
ECONOMIDES C, CALDWELL T, JUDE JR: The clinical,
surgical and pathologic correlations in patients with
acute myocardial infarction and pump failure.
Circulation 44: 1034, 1971
7. HARNARAYAN C, BENNETT MA, PE-NTECOST BL, BREWER
DB: Quantitative study of infarcted myocardium in
cardiogenic shock. Brit Heart J 32: 728, 1970
8. PAGE DL, CAULFIELD JB, KASTOR JA, DESANCTIS RW,
SANDERS CA: Myocardial changes associated with
cardiogenic shock. New Eng J Med 285: 133,
1971
9. SWAN HJC, FORRESTER JS, DIAMOND G, CHATTERJEE
K, PARMILEY WW: Hemodynamic spectrum of
myocardial infarction and cardiogenic shock. A
conceptual model. Circulation 45: 197, 1972
10. PRUITT RD, DENNIS EW, KINARD SA: The difficult
electrocardiographic diagnosis of myocardial infarction. Progr Cardiovasc Dis 6: 85, 1963
11. ANDERSSEN N, SKJAEGGSTAD 0: The electrocardiogram
in patients with previous myocardial infarction. Acta
Med Scand 176: 123, 1964
12. LEVINE H, PHILLIPS E: An appraisal of the new
electrocardiography in one hundred and fifty consecutive autopsied cases. New Eng J Med 245: 833,
1951
13. GEORAS CS, DAHLQUIST E, CUTTS FB: Subendocardial
infarction. Arch Intern Med 111: 488, 1963
14. ROBERTS WC, BUJA LM: The frequency and significance of coronary arterial thrombi and other
observations in fatal acute myocardial infarction. A
study of 107 patients. Amer J Med 52: 425, 1972
15. MAROKO PR, LIBBY P, COVELL JW, SOBEL BE, Ross J,
BRAUNWALD E: Precordial ST segment elevation
mapping: An atraumatic method for assessing
alterations in the extent of myocardial ischemic
injury. Amer J Cardiol 29: 223, 1972
16. MAROKO PR, KJEKSHUS JK, SOBEL BE, WATANABE T,
COVELL JW, Ross J, BRAUNWALD E: Factors
influencing infarct size following experimental coronary artery occlusion. Circulation 43: 67, 1971
17. HOOD WB JR: Salvage of myocardium in acute
ischemia. Circulation 43: 11, 1971
Circulation, Volume XLVIII, September 1973
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
Pathophysiology of Cardiogenic Shock: Quantification of Myocardial Necrosis, Clinical,
Pathologic and Electrocardiographic Correlations
DANIEL R. ALONSO, STEPHEN SCHEIDT, MARTIN POST and THOMAS KILLIP
Circulation. 1973;48:588-596
doi: 10.1161/01.CIR.48.3.588
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright 1973 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on the World
Wide Web at:
http://circ.ahajournals.org/content/48/3/588
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click Request
Permissions in the middle column of the Web page under Services. Further information about this process is available
in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/
Downloaded from http://circ.ahajournals.org/ by guest on April 12, 2016
You might also like
- BR Heart J 1985 Hartnell 392 5Document5 pagesBR Heart J 1985 Hartnell 392 5phng77No ratings yet
- Anterior Acute Myocardial Infarction Complicated With Ventricular Septal Rupture: Case Reports and Literature ReviewDocument5 pagesAnterior Acute Myocardial Infarction Complicated With Ventricular Septal Rupture: Case Reports and Literature ReviewIJAR JOURNALNo ratings yet
- JurnalDocument35 pagesJurnalsakinaNo ratings yet
- Coronary Angiographic Morphology in Myocardial Infarction: A Link Between The Pathogenesis of Unstable Angina and Myocardial InfarctionDocument6 pagesCoronary Angiographic Morphology in Myocardial Infarction: A Link Between The Pathogenesis of Unstable Angina and Myocardial InfarctionSabila RosyidaNo ratings yet
- Eriksen Et Al-2002-Clinical Cardiology PDFDocument5 pagesEriksen Et Al-2002-Clinical Cardiology PDFmedskyqqNo ratings yet
- Cardiac Autotransplantation: Cooley Society 15th International SymposiumDocument5 pagesCardiac Autotransplantation: Cooley Society 15th International SymposiumPeter Paul PascualNo ratings yet
- Fmar 2016033110082864Document6 pagesFmar 2016033110082864Karina Mega WNo ratings yet
- Cardiac Resynchronisation Therapy For Patients With Heart FailureDocument5 pagesCardiac Resynchronisation Therapy For Patients With Heart FailureIpar DayNo ratings yet
- The Fate of The Distal Aorta After Repair of Acute Type A Aortic DissectionDocument10 pagesThe Fate of The Distal Aorta After Repair of Acute Type A Aortic Dissectionapi-160333876No ratings yet
- Jama Samsky 2021 RV 210015 1636669111.74911Document11 pagesJama Samsky 2021 RV 210015 1636669111.74911Yo MeNo ratings yet
- Jama 2021 326 1840Document11 pagesJama 2021 326 1840silviaNo ratings yet
- Cardiogenic Shock After Acute Myocardial InfarctionDocument11 pagesCardiogenic Shock After Acute Myocardial InfarctionMauricio Martinez HernandezNo ratings yet
- Cardiogenic Shock Workup (Medscape)Document8 pagesCardiogenic Shock Workup (Medscape)Tia WasrilNo ratings yet
- CabgDocument12 pagesCabgShreeja Sajit100% (1)
- Shock Cardiogenico - IamDocument19 pagesShock Cardiogenico - IamYESSICA CARENALGANo ratings yet
- Clinical Experience With A Novel Multielectrode Basket Catheter in Right Atrial Tachycardias (Schmitt Et Al., 1999)Document10 pagesClinical Experience With A Novel Multielectrode Basket Catheter in Right Atrial Tachycardias (Schmitt Et Al., 1999)Ioan AlexandreNo ratings yet
- Detection of Myocardial Infraction Monisha C M - 17bei0092: Select, Vit VelloreDocument8 pagesDetection of Myocardial Infraction Monisha C M - 17bei0092: Select, Vit VelloresubramanianNo ratings yet
- Paracardiac Masses Caused A Right Coronary Artery Aneurysm and A Saphenous Vein Graft AneurysmDocument3 pagesParacardiac Masses Caused A Right Coronary Artery Aneurysm and A Saphenous Vein Graft AneurysmSheikh Mizanur RahmanNo ratings yet
- Ect AsiaDocument4 pagesEct Asiajessik zavalaNo ratings yet
- Left Hemothorax: Unusual Manifestation of Aortic DissectionDocument5 pagesLeft Hemothorax: Unusual Manifestation of Aortic DissectionIJAR JOURNALNo ratings yet
- Acute Aortic Dissection Type A Extended, Complicated Extensive Stroke About A Case, and Literature ReviewDocument31 pagesAcute Aortic Dissection Type A Extended, Complicated Extensive Stroke About A Case, and Literature ReviewIJAR JOURNALNo ratings yet
- Acute Aortic Dissection Type A Extended, Complicated Extensive Stroke About A Case, and Literature ReviewDocument31 pagesAcute Aortic Dissection Type A Extended, Complicated Extensive Stroke About A Case, and Literature ReviewIJAR JOURNALNo ratings yet
- Evaluation of A Scoring System For Extracranial Carotid Atherosclerosis Extent With B-Mode Ultrasound, 1986Document7 pagesEvaluation of A Scoring System For Extracranial Carotid Atherosclerosis Extent With B-Mode Ultrasound, 1986CAMILO ARMANDO BENAVIDES BURBANONo ratings yet
- Atrial Hemangioma A Case Report and Review of The LiteratureDocument11 pagesAtrial Hemangioma A Case Report and Review of The LiteratureSaya MenarikNo ratings yet
- Pathophysiology and Investigation of Coronary Artery DiseaseDocument4 pagesPathophysiology and Investigation of Coronary Artery DiseasekartikaparamitaNo ratings yet
- Madit CRTNEJMseot 09Document10 pagesMadit CRTNEJMseot 09binh doNo ratings yet
- 182 FullDocument3 pages182 FullViona ApriliaNo ratings yet
- AR Yang Komplikasi Menjadi Gagal Jantung PDFDocument5 pagesAR Yang Komplikasi Menjadi Gagal Jantung PDFFitriani AlawiyahNo ratings yet
- End Arte Rec To MyDocument7 pagesEnd Arte Rec To MyLuming LiNo ratings yet
- Hypovolemic Shock Complex in The Trauma Setting: A Pictorial ReviewDocument8 pagesHypovolemic Shock Complex in The Trauma Setting: A Pictorial ReviewSafitryNo ratings yet
- Dishivam9876mbimph, Elsaka512021AJOAIR1499Document16 pagesDishivam9876mbimph, Elsaka512021AJOAIR1499morena19932308No ratings yet
- 99591Document7 pages99591jimejuanfeNo ratings yet
- 2 Casos Clinicos de Tratamiento Homeopatico de Cardiopatia CoronariaDocument5 pages2 Casos Clinicos de Tratamiento Homeopatico de Cardiopatia Coronariaalbertompg100% (1)
- Isolated Right Ventricle Myocardial Infarction - Is The Right Ventricle Still The Forgotten Ventricle?Document4 pagesIsolated Right Ventricle Myocardial Infarction - Is The Right Ventricle Still The Forgotten Ventricle?Nadyaindriati96No ratings yet
- Reverse Tria24 MolDocument12 pagesReverse Tria24 Molbinh doNo ratings yet
- 1 s2.0 S0735109700006902 MainDocument6 pages1 s2.0 S0735109700006902 MainEyal RobinsonNo ratings yet
- s0735 1097 (85) 80117 0Document8 pagess0735 1097 (85) 80117 0John DoeNo ratings yet
- European Heart Journal (2003) 24, 787-788Document2 pagesEuropean Heart Journal (2003) 24, 787-788api-26263700No ratings yet
- Management of Cardiogenic Shock After Acute - 2023Document10 pagesManagement of Cardiogenic Shock After Acute - 2023Angy KarakostaNo ratings yet
- 49 54 PDFDocument6 pages49 54 PDFray m deraniaNo ratings yet
- Fisiopatologia Del Shock Cardiogenico Por Iam PDFDocument12 pagesFisiopatologia Del Shock Cardiogenico Por Iam PDFYESSICA CARENALGANo ratings yet
- 10.1007@s00296 008 0601 0Document3 pages10.1007@s00296 008 0601 0Kuber RawaNo ratings yet
- Articulo 2Document8 pagesArticulo 2Andrea OrtizNo ratings yet
- Stroke 1982 Myers 838 42Document6 pagesStroke 1982 Myers 838 42Widyawan SyahputraNo ratings yet
- JLM 03 26Document8 pagesJLM 03 26Roberto DianNo ratings yet
- Mitral Valve Endocarditis in Hypertrophic Cardiomyopathy: Case Report and Literature ReviewDocument3 pagesMitral Valve Endocarditis in Hypertrophic Cardiomyopathy: Case Report and Literature ReviewChristabella Natalia WijayaNo ratings yet
- Echocardiography Dissertation IdeasDocument8 pagesEchocardiography Dissertation IdeasWhoCanWriteMyPaperForMeCanada100% (1)
- ContentServer AspDocument9 pagesContentServer Aspganda gandaNo ratings yet
- Pereira Et Al-2016-Jornal Vascular Brasileiro - Sup-1Document5 pagesPereira Et Al-2016-Jornal Vascular Brasileiro - Sup-1carmenNo ratings yet
- AtherosclerosisDocument8 pagesAtherosclerosisLeidy LambertinezNo ratings yet
- Modified Batista Procedure For Idiopathic Dilated Cardiomyopathy: Report of A CaseDocument10 pagesModified Batista Procedure For Idiopathic Dilated Cardiomyopathy: Report of A CasepatramaleNo ratings yet
- HHS Public Access: Myocardial Bridging: An Up-to-Date ReviewDocument16 pagesHHS Public Access: Myocardial Bridging: An Up-to-Date ReviewDavid J. SaavedraNo ratings yet
- Bradicardy ManagementDocument7 pagesBradicardy ManagementMarshall ThompsonNo ratings yet
- Cryptogenic Stroke: Clinical PracticeDocument10 pagesCryptogenic Stroke: Clinical PracticenellieauthorNo ratings yet
- Handbook of Contrast Echocardiography: Left Ventricular Function and Myocardial PerfusionDocument0 pagesHandbook of Contrast Echocardiography: Left Ventricular Function and Myocardial PerfusionelenaresmeritaNo ratings yet
- Review Trombosis CerebrovascularDocument10 pagesReview Trombosis CerebrovascularDiego Velásquez HerreraNo ratings yet
- Application of Strain and Other Echocardiographic Parameters in The Evaluation of Early and Long-Term Clinical Outcomes After Cardiac Surgery RevascularizationDocument8 pagesApplication of Strain and Other Echocardiographic Parameters in The Evaluation of Early and Long-Term Clinical Outcomes After Cardiac Surgery RevascularizationSondang JasmineNo ratings yet
- Clinical Handbook of Cardiac ElectrophysiologyFrom EverandClinical Handbook of Cardiac ElectrophysiologyBenedict M. GloverNo ratings yet
- Acute Stroke Management in the Era of ThrombectomyFrom EverandAcute Stroke Management in the Era of ThrombectomyEdgar A. SamaniegoNo ratings yet
- Unstable AnginaDocument11 pagesUnstable AnginaAdrian BoboceaNo ratings yet
- 03 IjnhDocument4 pages03 Ijnhalev palantökenNo ratings yet
- Class 7 Holiday Homework-MergedDocument29 pagesClass 7 Holiday Homework-MergedidkNo ratings yet
- 12-Lead EKG InterpretationDocument47 pages12-Lead EKG InterpretationAlice ChoiNo ratings yet
- Pericardial Diseases 3rd Yr BMTDocument38 pagesPericardial Diseases 3rd Yr BMT211941103014100% (1)
- 2018 ESC-ESH Guidelines For The Management of Arterial HypertensionDocument98 pages2018 ESC-ESH Guidelines For The Management of Arterial HypertensionjulzcatNo ratings yet
- Valvular Esc Book ChapterDocument96 pagesValvular Esc Book ChapterkikiwulandariNo ratings yet
- SDL DL BrochureDocument2 pagesSDL DL BrochureNanda Nabilah UbayNo ratings yet
- Grand Case CHF Final Na Final Na Final Na TrueDocument40 pagesGrand Case CHF Final Na Final Na Final Na Truelyndzy100% (2)
- AcceptedDocument28 pagesAcceptedChistian LassoNo ratings yet
- Cardiac Condition NCM 112Document10 pagesCardiac Condition NCM 112Irish Eunice FelixNo ratings yet
- Deep Venous Thrombosis: Practice EssentialsDocument27 pagesDeep Venous Thrombosis: Practice Essentialsphoechoex100% (1)
- Rabbit Anatomy - Atlas and Dissection Guide - Part 2 - Cardiovascular System - Second EditionDocument35 pagesRabbit Anatomy - Atlas and Dissection Guide - Part 2 - Cardiovascular System - Second EditionFrancis Mary RosaNo ratings yet
- Pregnancy Hypertension: Llinos Roberts, Piya Chaemsaithong, Daljit S. Sahota, Kypros H. Nicolaides, Liona C.Y. PoonDocument6 pagesPregnancy Hypertension: Llinos Roberts, Piya Chaemsaithong, Daljit S. Sahota, Kypros H. Nicolaides, Liona C.Y. PoonalexandraNo ratings yet
- Fibrous Skeleton of Heart PDFDocument2 pagesFibrous Skeleton of Heart PDFMeghan0% (1)
- NicardDocument2 pagesNicardElyNo ratings yet
- CHF Preparation QuestionsDocument6 pagesCHF Preparation Questionsgenium0689% (9)
- Constrictive Pericarditis - Clinical Features and Causes - UpToDateDocument20 pagesConstrictive Pericarditis - Clinical Features and Causes - UpToDatemayteveronica1000No ratings yet
- Unit 4 - Checking Vital SignsDocument29 pagesUnit 4 - Checking Vital SignsoktikaNo ratings yet
- ACLS Rhythms Practice Test 2020 Recognition Rhythm Strips (PDF)Document11 pagesACLS Rhythms Practice Test 2020 Recognition Rhythm Strips (PDF)김민길100% (2)
- Anxiety Nitroglycerin: Myocardial InfarctionDocument135 pagesAnxiety Nitroglycerin: Myocardial InfarctionDefensor Pison Gringgo0% (1)
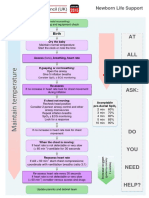
- Neonatal Life Support UK Ressusstation Council G2015 - NLSDocument1 pageNeonatal Life Support UK Ressusstation Council G2015 - NLSBharat Kumar SharmaNo ratings yet
- Thermal Hydrotherapy Improves Quality of Life and Hemodynamic Function in Patients With Chronic Heart FailureDocument6 pagesThermal Hydrotherapy Improves Quality of Life and Hemodynamic Function in Patients With Chronic Heart FailurearitabrunoNo ratings yet
- Antiarrhythmic Drugs Classification (Vaughan Williams)Document8 pagesAntiarrhythmic Drugs Classification (Vaughan Williams)ana100% (1)
- PPP v3Document771 pagesPPP v3Steven Lam100% (1)
- Research Poster PresentationDocument1 pageResearch Poster Presentationapi-328441669No ratings yet
- POCUS IVC-shock PDFDocument55 pagesPOCUS IVC-shock PDFKorkrit MeekaewNo ratings yet
- Generic Name Brand Name Drug Class Mechanism of Action StructureDocument4 pagesGeneric Name Brand Name Drug Class Mechanism of Action StructurenoelkiddoNo ratings yet
- BonitaDocument257 pagesBonitaCardio Family of July 2018 Universitas Indonesia100% (1)
- ECG UworldDocument4 pagesECG UworldBaebee LouNo ratings yet