Professional Documents
Culture Documents
"J 1432-2277 2011 01339 X
Uploaded by
Vher SisonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
"J 1432-2277 2011 01339 X
Uploaded by
Vher SisonCopyright:
Available Formats
Transplant International ISSN 0934-0874
ORIGINAL ARTICLE
Removable intraductal stenting in duct-to-duct biliary
reconstruction in liver transplantation
Hadrien Tranchart,1,2 Stephane Zalinski,1,2 Ailton Sepulveda,1,2 Mircea Chirica,1,2 Frederic Prat,3,4
Olivier Soubrane1,4 and Olivier Scatton1,2
1 Department of Hepatobiliary Surgery and Liver Transplantation, Saint-Antoine Hospital, Assistance Publique Hopitaux de Paris, Paris Cedex,
France
2 Universite Pierre et Marie Curie, Paris, France
3 Department of Gastroenterology and Endoscopy, Cochin Hospital, Paris, France
4 Universite Paris Descartes, Paris, France
Keywords
biliary reconstruction, intraductal stent, liver
transplantation.
Correspondence
Olivier Scatton MD, PhD, Department of
Hepatobiliary Surgery and Liver
Transplantation, Hopital Saint-Antoine, 184
rue du Faubourg Saint-Antoine, 75571 Paris
Cedex 12, France. Tel.: +33 (0) 1 71 97
01 81; fax: +33 (0) 1 71 97 01 57; e-mail:
olivier.scatton@sat.aphp.fr
Conflicts of interest
The authors have declared no conflicts of
interest.
Received: 16 June 2011
Revision requested: 13 July 2011
Accepted: 22 August 2011
Published online: 29 September 2011
doi:10.1111/j.1432-2277.2011.01339.x
Summary
Biliary reconstruction during liver transplantation (LT) is most oftenly performed by duct-to-duct biliary anastomosis. We hypothesized that the internal
stenting might diminish the incidence and severity of biliary complications in
patients receiving small duct size donor grafts. The purpose of this study was
to report a technique of biliary reconstruction, including intraductal stent tube
(IST) placement followed by postoperative endoscopic removal. A custommade segment of a T-tube was placed into the bile in 20 patients in whom the
diameter of the graft bile duct was smaller than 5 mm. The tube was removed
endoscopically 48 months after LT, or in case of IST-related adverse events.
After a median follow-up of 15.2 (range 2.527.5) months, endoscopic removal
of the IST was performed in 17 patients. No technical failure and no procedure-related complications were recorded during drain removal. Biliary complications occurred in four patients, including one cholangitis, one hemobilia,
one asymptomatic biliary leakage, and one anastomotic stricture. No biliary
complication occurred in the group of patients who underwent deceased donor
whole graft LT. IST is technically feasible and safe, and may help to prevent
severe biliary complication when duct-to-duct biliary anastomosis is performed
on small size bile ducts.
Introduction
In liver transplantation (LT), biliary tract reconstruction is
the final step of the surgical procedure and requires good
technical skills. It can be performed either by an end-toend [1] or a side-to-side [2] ductal anastomosis. When a
duct-to-duct anastomosis is not feasible for anatomical
reasons or because of an underlying biliary disease, the biliary reconstruction is performed by hepaticojejunostomy
[3]. At the end of a difficult procedure, the biliary anastomosis is inappropriately viewed as the easy step of the
operation; however, biliary complications are severe events
which may eventually compromise outcomes of LT.
Despite technical progress in the field of LT, incidence of
biliary complications remains high, ranging from 10% to
50% in large clinical series [1,48].
Biliary complications are significant causes of posttransplantation morbidity and graft loss. Early complications are mostly represented by bile leaks whereas
strictures and their consequences are described as late
complications [9]. Technically, the end-to-end choledococholedocostomy is the most widely accepted technique
for biliary reconstruction. The usefulness of a T-tube
placement in whole graft deceased LT has been debated
in the literature [1,10].
Our group has published the first randomized
study demonstrating that biliary reconstruction may preferentially be performed without a T-tube [1]. In this
2011 The Authors
Transplant International 2011 European Society for Organ Transplantation 25 (2012) 1924
19
Biliary stents in liver transplantation
Tranchart et al.
multicentric randomized trial, 60% of the overall biliary
complications tube following LT were related to the use
of the T-tube itself and included mostly bile leaks around
the T-tube and cholangitis. Finally, the use of a T-tube
had no impact on the rate of biliary strictures but T-tubes
were usually removed early, within 3 months following
LT. Based on these results, we do not use external biliary
drain in LT.
On the other end, endoscopic series have highlighted
the efficiency of a prolonged stenting to treat for the
treatment of biliary stenosis [11,12]. Given the potential
benefit of a prolonged stenting and the reported side
effects of an external biliary drainage, we sought to
develop a new technique of intraoperative intraductal
stent tube (IST) placement followed by its endoscopic
stent removal in the postoperative period. We hypothesized that a prolonged and exclusive internal stenting of
the duct-to-duct biliary anastomosis may decrease the
incidence and severity of both early and late biliary complications while avoiding the drawbacks of a T-tube
placement in patients who receive small duct liver grafts.
The primary goal of the study was to evaluate the feasibility and safety of this new IST technique. The second endpoint was to assess the ability of the IST technique to
prevent the occurrence of biliary complications, especially
in the case of small bile ducts reconstruction, which carry
a high risk of stenosis.
Methods
Study population
From February 2007 to May 2009, 119 adult LT were performed in our department. Among this population, 20
patients underwent an elective deceased donor LT with
the IST technique and were followed prospectively.
Demographic characteristics and indications for LT are
depicted in Table 1.
Surgical technique and outcomes monitoring
Patients
Gender (M/F)
Age (year), mean SD (range)
Body mass index (kg/m2),
mean SD (range)
Previous abdominal surgery, n (%)
Indication for liver transplantation
HCC, n (%)
Posthepatitis C cirrhosis, n (%)
Posthepatitis B cirrhosis, n (%)
Alcoholic cirrhosis, n (%)
Polycystic liver disease, n (%)
Cystic fibrosis, n (%)
Overlap syndrome, n (%)
Cirrhosis, n (%)
Child (A/B/C)
MELD score, mean SD (range)
20
15/5
49.2 13 (1565)
23.5 4.3 (16.435.9)
10 (50)
7 (35)
4 (20)
1 (5)
3 (15)
2 (10)
2 (10)
1 (5)
17 (85)
5/5/7
15.5 6.4 (626)
HCC, hepatocellular carcinoma; SD, standard deviation.
were created. The stent was inserted in the biliary duct
without suture fixation. The endoscopic procedure for
IST removal was scheduled 48 months following LT.
Immediate removal was performed in case of IST-related
adverse events, such as: abnormal liver function tests
(cholestasis or transient hepatocellular dysfunction), fever
or intrahepatic bile duct dilatation of more than 2 mm
on ultrasound, computed tomography scan or magnetic
resonance cholangiography (MRC). IST extraction was
performed using a Dormia basket or an endoscopic staple
extractor (Fig. 2). The endoscopic IST removal procedure
was performed by the same endoscopist (FP), highly
experienced with endobiliary maneuvers [13,14].
Operative mortality and morbidity were recorded prospectively for both the LT and endoscopic retrograde cholangiopancreatography (ERCP) procedures. For ERCP,
(a)
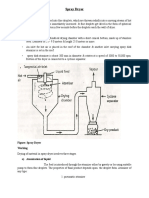
Liver recovery was performed using standard techniques,
and University of Wisconsin solution was used for organ
preservation. Bile ducts were systematically washed with
preservation fluid during organ procurement. Indication
for an IST placement at the time of LT was a diameter of
the donor bile duct of 5 mm or less. Duct-to-duct biliary
reconstruction was always performed via a hepaticocholedocostomy using interrupted polydioxanone .00000
sutures. The connective tissue surrounding bile ducts of
the donor and the recipient bile ducts were systematically
preserved to ensure a good periductal vascularization. A
custom-made segment (2 cm) of a 8 French T-tube was
used for the confection of the IST (Fig. 1). No side holes
20
Table 1. Demographic characteristics and surgical indications of
patients undergoing transplantation.
(b)
Figure 1 The biliary duct-to-duct anastomosis is performed (a, black
arrow) with interrupted sutures, using a custom-made IST (b).
2011 The Authors
Transplant International 2011 European Society for Organ Transplantation 25 (2012) 1924
Tranchart et al.
Biliary stents in liver transplantation
(a)
(b)
Figure 2 Endoscopic removal of the stent (a) and post-ERCP cholangiography (b).
the rate of pancreatitis, bleeding, duodenal perforations,
and failure to remove the IST were specifically monitored.
Evaluation of postoperative biliary complications was the
second endpoint of the study. All deaths, operative complications [before postoperative day (POD) 90], and late
complications (>POD 90) were recorded; complication
severity was stratified according to the modified Clavien
classification [15].
Statistical analysis
Categorical data were analyzed after setting up multiple
2 2 contingency tables using the chi-squared test or
Fisher exact test when appropriate. Because of the small
sample size, continuous data were analyzed using the
MannWhitney U-test and expressed as mean standard
deviation and (range), or median and (range). Cumulative overall survival was computed according to the
KaplanMeier method. Statistical analysis was made using
spss 16.0 (Chicago, IL, USA) for Windows software.
Results
Among the 20 patients who underwent IST, 16 patients
received a whole liver graft (including one domino), three
patients received a split graft (full right graft: segments
V-VI-VII-VIII), and one patient received a reduced graft
(full left graft: segments II-III-IV). The donor common
bile duct was always conserved in partial grafts; thus,
hepaticocholedocostomy could be undertaken in these
patients as previously described. A combined liver and
kidney transplantation was performed in two patients.
Intraoperative data of patients who underwent LT and
IST are depicted in Table 2. No patient died postoperatively. Postoperative morbidity was 50%. One-year overall
survival was 95% (Fig. 3). After a median follow-up of
12.7 (range 3.528.5) months, one patient died from a
hepatitis C virus recurrence 16 months after LT and
another one died from a pulmonary embolism 1 year
after LT.
Feasibility and safety of IST
The IST was successfully inserted in all the patients during LT. Eighteen patients underwent a pre-ERCP imaging
prior to stent removal: 12 MRC and six ultrasounds after
a median of 15 (range 7180) days following LT. After a
median follow-up of 12.7 (range 3.528.5) months, endoscopic removal of the IST was successfully performed in
17 patients (85%). One patient died from a pulmonary
embolism and two others were lost to follow-up before
stent ablation. The median delay between LT and IST
Table 2. Intraoperative data of patients undergoing transplantation.
Type of graft
Whole deceased donor, n (%)
Split (full right graft: V-VI-VII-VIII), n (%)
Reduced (full left graft: II-III-IV), n (%)
Domino, n (%)
Graft weight (g), mean SD (range)
Graft steatosis (>10%/101%/<1%)
Donor age (year), mean SD (range)
Cold ischemia time (hour), mean SD
(range)
Warm ischemia time (min), mean SD
(range)
Piggyback implantation of the liver graft
Vena cava replacement
Intraoperative transfusion, n (%)
Packed red cell units SD
Donor bile duct size (3 mm/4 mm/5 mm)
15 (75)
3 (15)
1 (5)
1 (5)
1234 311 (5801700)
1/2/17
48 11.2 (6025)
9.7 2.4 (3.513)
64 20.9 (40120)
16
4
5 (25)
4.6 3.9
4/6/10
SD, standard deviation.
2011 The Authors
Transplant International 2011 European Society for Organ Transplantation 25 (2012) 1924
21
Biliary stents in liver transplantation
Tranchart et al.
Percent survival
110
100
90
80
70
10
20
30
Follow-up (months)
Figure 3 Overall survival.
removal was 26.5 (range 472) weeks. During ERCP, a
limited sphincterotomy (infundibulotomy) was necessary
for IST removals in 15 (88.2%) patients. IST extraction
was performed using a Dormia basket in five patients
(29.4%) or using an endoscopic staple extractor in 11
patients (64.7%). No technical failure was recorded during drain removal. In one patient, imaging showed
5 months after LT that the drain had spontaneously
migrated into the duodenum. It was confirmed during
ERCP. A minor and transient elevation of serum amylase
level with no clinical symptoms was the only event
recorded in one patient after drain removal (Table 3).
The stent removal procedure and post-ERCP cholangiography are illustrated in Fig. 2.
Impact of IST placement on biliary complications
Biliary complications occurred in four patients during follow-up. One cholangitis (Clavien II) was successfully treated with antibiotics and drain removal. However, the
stent culture did not demonstrated infection. This event
Table 3. Data of patients undergoing intraductal stent tube ablation.
Ablation, n (%)
ERCP
Surgery*
Delay between LT and IST removal
(weeks), median (range)
Endoscopic infundibulotomy, n (%)
IST extraction, n (%)
Dormia basket
Endoscopic staple extractor
Spontaneous migration
Technical failure, n
Procedure-related complication rate, n
18 (90)
17 (94.4)
1 (5.6)
12.7 (3.528.5)
15 (88.2)
5 (29.4)
11 (64.7)
1 (5.9)
0
0
ERCP, endoscopic retrograde cholangiopancreatography; IST, intraductal stent tube.
*One patient who underwent combined liverkidney transplantation
developed bilioportal fistula requiring reoperation on POD 30 and
stent removal.
22
was suspected to be related to the migration of the distal
part of the drain through the sphincter of Oddi, causing
a reflux of digestive contents along the drain into the
common bile duct. One patient who underwent combined liverkidney transplantation developed a hemobilia
(Clavien IVa) related to a bilioportal fistula, and was
reoperated on POD 30. The IST was removed at the time
of reoperation; external T-tube biliary drainage and
suture of the portal vein were undertaken in this patient.
Eventually, his postoperative course was uneventful. In
another patient, asymptomatic biliary leakage (Clavien
IIIb) was diagnosed at the time of endoscopic IST
removal and was treated successfully by immediate positioning of a covered stent. An anastomotic stricture
(Clavien IIIb) occurred 12 months after LT in one patient
and was successfully treated by an endoscopic dilatation
and stenting. No biliary complication was recorded in the
group of patients who underwent a whole graft LT with
IST placement. During the same period, biliary strictures
occurred in 15 patients (15.1%) among the group of
patients who underwent LT without IST placement.
Discussion
Decreasing the rates of biliary complications following LT
remains a crucial goal for transplant surgeons and technical refinements are sought actively. To allow tissue healing and to prevent biliary complications, external
diversion of the bile flow has been repeatedly advocated
in the past. Eventually, reports from several transplant
groups worldwide have shown that T-tube diversion of
the biliary flow during LT did not prevent from bile leaks
or ductal stenosis. Moreover, T-tube insertion itself was
associated with an increased morbidity, mainly related to
bile leaks at the site of drain insertion. Although others
have recently reported opposite results for side-to-side
anastomosis [10], we believe that an external biliary
drainage in LT is not a valuable option and we do not
use T-tubes anymore because of an increased morbidity
related the drain placement itself [1,16].
Moreover, T-tubes have been hypothesized to prevent
from late complications [17]. However, such assumptions
are not supported by clinical reports as T-tubes are often
removed early, within the initial three postoperative
months, and this delay is probably too short to prevent
from the development of biliary stricture. With the present study, we sought to develop a new technique to palliate these shortcomings of external biliary T-tube
diversion. In patients with small size biliary duct-to-duct
anastomosis, who are at high risk of biliary complication,
the IST technique has two potential benefits: (i) protect
the biliary anastomosis during tissue healing and (ii) prevent late stricture formation as a result of longer duration
2011 The Authors
Transplant International 2011 European Society for Organ Transplantation 25 (2012) 1924
Tranchart et al.
of stenting. These assumptions are supported by the fact
that endoscopic maneuvers, to treat biliary complications,
have been widely used and the efficacy of endobiliary
stents in treatment and prevention purpose is commonly
accepted in the transplant community [11,12]. To our
knowledge, internal stenting of the biliary anastomosis
followed by delayed endoscopic stent removal with the
aim to reduce the incidence and the severity of biliary
complications after LT has not been previously reported.
The present results show that IST placement in patients
with high risk biliary reconstruction (duct size 5 mm)
followed by endoscopic removal is technically feasible,
safe, and seems to ameliorate early and late biliary outcomes after LT. No biliary complication occurred in the
group of patients who underwent deceased donor whole
graft transplantation with small bile ducts. Overall, most
complications that occurred in our cohort of patients
were successfully treated with a conservative treatment.
The first main finding of our study was that no technical failures were recorded during stent removal. The only
procedure-related complication was a minor (<3N) and
transitory elevation of serum amylase level without clinical consequences following stent ablation. A single expert
operator performed all the ERCPs. The IST was removed
using a Dormia basket or an endoscopic staple extractor.
In one case, a spontaneous migration was diagnosed
during endoscopy. The tube was evacuated through the
natural way without incident. A short endoscopic sphincterotomy (infundibulotomy) was most of the time
required but none were associated with complications.
Interestingly enough, although the median delay between
LT and IST removal was 26.5 (range 472) weeks, no difficulties were recorded during IST ablation because of
stent incrustation. This may be explained by the fact that
no side holes were created when the custom-made segment of a 8 French T-tube was used for the confection of
the IST. The technical skills of the endoscopist and the
limited sphincterotomy may highly contribute to the very
low rate of post-ERCP morbidity, which fully support
our strategy of intraoperative endobiliary stenting in
selected patients with high risk biliary anastomosis.
The second finding of this study was a very low biliary
morbidity rate, especially in the group of patients who
received a whole graft. There was no complication
directly associated with the use of the IST in this group,
even if the IST was removed after a median delay of 26.5
(472) weeks. We have previously reported overall biliary
complications rate among whole graft transplanted
patients who underwent a biliary reconstruction with or
without a T-tube of 33.3% and 15.5%, respectively [1].
Although not significantly relevant, it was interesting to
note that the majority of complications occurred in the
group of patient who received reduced size grafts. This
Biliary stents in liver transplantation
finding is in accordance with data in the literature showing higher rates of biliary complications after living donor
or split LT [18]. A multicentric prospective comparative
study would be required to determine whether IST could
improve biliary outcomes in this subset of patients.
The rate of complications after endoscopic ERCP
reaches 4% [19]. Despite the low rate of endoscopic complication during IST removal in the present study, it is
obvious that introduction of this technique in the current
practice would lead to a nonzero, ERCP-related morbidity. Surgical placement of a biodegradable stent might
palliate this shortcoming by avoiding further endobiliary
maneuvers. Synthetic bioabsorbable stents have been successfully used in animal models for treatment of cystic
duct leakage, hepaticojejunal anastomosis, and duct-toduct biliary reconstruction [2024]. Although use of biodegradable stents has not yet been reported in clinical LT,
this might represent an interesting perspective and a
rewarding field of research.
In conclusion, IST is technically feasible and safe, and
seems to prevent from severe biliary complication in
transplantation of whole liver grafts and small size bile
duct. A large prospective study should be performed to
confirm the results of this preliminary study.
Authorship
HT: collected data, analyzed data and wrote the paper.
SZ: wrote the paper. AS: collected data. MC: performed
study. FP: performed study. OS: designed study and performed study, OS: designed study, performed study and
analyzed data.
Funding
No grants and no financial supports to disclose.
References
1. Scatton O, Meunier B, Cherqui D, et al. Randomized trial
of choledochocholedochostomy with or without a T tube
in orthotopic liver transplantation. Ann Surg 2001; 233:
432.
2. Neuhaus P, Blumhardt G, Bechstein WO, Steffen R, Platz
KP, Keck H. Technique and results of biliary reconstruction using side-to-side choledochocholedochostomy in 300
orthotopic liver transplants. Ann Surg 1994; 219: 426.
3. Welsh FK, Wigmore SJ. Roux-en-Y choledochojejunostomy is the method of choice for biliary reconstruction in
liver transplantation for primary sclerosing cholangitis.
Transplantation 2004; 77: 602.
4. Stratta RJ, Wood RP, Langnas AN, et al. Diagnosis and
treatment of biliary tract complications after orthotopic
2011 The Authors
Transplant International 2011 European Society for Organ Transplantation 25 (2012) 1924
23
Biliary stents in liver transplantation
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
24
Tranchart et al.
liver transplantation. Surgery 1989; 106: 675. discussion
83-4.
Vallera RA, Cotton PB, Clavien PA. Biliary reconstruction
for liver transplantation and management of biliary complications: overview and survey of current practices in the
United States. Liver Transpl Surg 1995; 1: 143.
Fleck A, Zanotelli ML, Meine M, et al. Biliary tract complications after orthotopic liver transplantation in adult
patients. Transplant Proc 2002; 34: 519.
Krawczyk M, Nyckowski P, Zieniewicz K, et al. Biliary
complications following liver transplantation. Transplant
Proc 2000; 32: 1429.
Hernandez Q, Ramirez P, Munitiz V, et al. Incidence and
management of biliary tract complications following 300
consecutive orthotopic liver transplants. Transplant Proc
1999; 31: 2407.
Greif F, Bronsther OL, Van Thiel DH, et al. The incidence,
timing, and management of biliary tract complications after
orthotopic liver transplantation. Ann Surg 1994; 219: 40.
Weiss S, Schmidt SC, Ulrich F, et al. Biliary reconstruction
using a side-to-side choledochocholedochostomy with or
without T-tube in deceased donor liver transplantation: a
prospective randomized trial. Ann Surg 2009; 250: 766.
Ostroff JW. Post-transplant biliary problems. Gastrointest
Endosc Clin N Am 2001; 11: 163.
Vandenbroucke F, Plasse M, Dagenais M, Lapointe R,
Letourneau R, Roy A. Treatment of post liver transplantation bile duct stricture with self-expandable metallic stent.
HPB (Oxford) 2006; 8: 202.
Chaput U, Scatton O, Bichard P, et al. Temporary placement of partially covered self-expandable metal stents for
anastomotic biliary strictures after liver transplantation: a
prospective, multicenter study. Gastrointest Endosc 2010;
72: 1167.
Farhat S, Bourrier A, Gaudric M, et al. Endoscopic treatment of biliary fistulas after complex liver resection. Ann
Surg 2011; 253: 88.
15. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a
cohort of 6336 patients and results of a survey. Ann Surg
2004; 240: 205.
16. Zalinski S, Soubrane O, Scatton O. Reducing biliary morbidity in full graft deceased donor liver transplantation: is
it really a matter of T-tube? Ann Surg 2010; 252: 570.
author reply 1-2.
17. Shaked A. Use of T tube in liver transplantation. Liver
Transpl Surg 1997; 3: S22.
18. Duailibi DF, Ribeiro MA Jr. Biliary complications following deceased and living donor liver transplantation: a
review. Transplant Proc 2010; 42: 517.
19. Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk
factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc
2009; 70: 80.
20. Tashiro H, Ogawa T, Itamoto T, et al. Synthetic bioabsorbable stent material for duct-to-duct biliary reconstruction. J Surg Res 2009; 151: 85.
21. Meng B, Wang J, Zhu N, Meng QY, Cui FZ, Xu YX. Study
of biodegradable and self-expandable PLLA helical biliary
stent in vivo and in vitro. J Mater Sci Mater Med 2006; 17:
611.
22. Laukkarinen J, Nordback I, Mikkonen J, Karkkainen P,
Sand J. A novel biodegradable biliary stent in the endoscopic treatment of cystic-duct leakage after cholecystectomy. Gastrointest Endosc 2007; 65: 1063.
23. Laukkarinen JM, Sand JA, Chow P, et al. A novel biodegradable biliary stent in the normal duct hepaticojejunal
anastomosis: an 18-month follow-up in a large animal
model. J Gastrointest Surg 2007; 11: 750.
24. Heistermann HP, Palmes D, Stratmann U, et al. A new
technique for reconstruction of the common bile duct by
an autologous vein graft and a biodegradable endoluminal
stent. J Invest Surg 2006; 19: 57.
2011 The Authors
Transplant International 2011 European Society for Organ Transplantation 25 (2012) 1924
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Questionnaire - RichelleDocument2 pagesQuestionnaire - RichelleVher SisonNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elmd TCPDocument3 pagesElmd TCPPrince QueenoNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Schedule of Stay in JapanDocument5 pagesSchedule of Stay in JapanVher SisonNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- RCN Bulletin Jobs Fair 2013 Management and Leadership in Community NursingDocument20 pagesRCN Bulletin Jobs Fair 2013 Management and Leadership in Community NursingVher SisonNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- HIV AIDS Determinants EnglishDocument9 pagesHIV AIDS Determinants EnglishVher SisonNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Definition of Terms Sison ADocument1 pageDefinition of Terms Sison AVher SisonNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Rizal Was Implicated in The Activities of The Emerging Rebellion and in July 1892Document3 pagesRizal Was Implicated in The Activities of The Emerging Rebellion and in July 1892Vher SisonNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- DiIorio SSBQ ExhibitDocument2 pagesDiIorio SSBQ ExhibitVher SisonNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Definition of TermsDocument1 pageDefinition of TermsVher SisonNo ratings yet
- Statement of The ProblemDocument1 pageStatement of The ProblemVher SisonNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- MS Word 2013 Exercise 1 MAEdDocument3 pagesMS Word 2013 Exercise 1 MAEdVher SisonNo ratings yet
- A Beautiful Mind (A Reaction Paper)Document4 pagesA Beautiful Mind (A Reaction Paper)Reisha FungoNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Ms Word 2013 Exercise 3 Output MaedDocument1 pageMs Word 2013 Exercise 3 Output MaedVher SisonNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- What Is A Simple MachineDocument3 pagesWhat Is A Simple MachineVher SisonNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Literature Review SampleDocument13 pagesLiterature Review SampleArjay Alvaran Sanchez100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- ContraDocument41 pagesContraVher SisonNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Illegal MiningDocument10 pagesIllegal MiningVher SisonNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Cues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationDocument3 pagesCues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationVher SisonNo ratings yet
- Statement of The ProblemDocument1 pageStatement of The ProblemVher SisonNo ratings yet
- Vher's Sample Title, BoS & RPDocument3 pagesVher's Sample Title, BoS & RPVher SisonNo ratings yet
- Inflam L7 2012Document29 pagesInflam L7 2012Vher SisonNo ratings yet
- QuestionnaireDocument2 pagesQuestionnaireVher SisonNo ratings yet
- Parental ApprovalDocument1 pageParental ApprovalVher SisonNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Continuity of CareDocument16 pagesContinuity of CareVher SisonNo ratings yet
- GamesDocument1 pageGamesVher SisonNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanVher SisonNo ratings yet
- History LyricsDocument2 pagesHistory LyricsVher SisonNo ratings yet
- Europe - June 1, 2015Document1 pageEurope - June 1, 2015Vher SisonNo ratings yet
- Periodic Table PtableDocument1 pagePeriodic Table Ptableapi-239694539No ratings yet
- Security Testing MatDocument9 pagesSecurity Testing MatLias JassiNo ratings yet
- SPSS-TEST Survey QuestionnaireDocument2 pagesSPSS-TEST Survey QuestionnaireAkshay PatelNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- BBRC4103 - Research MethodologyDocument14 pagesBBRC4103 - Research MethodologySimon RajNo ratings yet
- 1651 EE-ES-2019-1015-R0 Load Flow PQ Capability (ENG)Document62 pages1651 EE-ES-2019-1015-R0 Load Flow PQ Capability (ENG)Alfonso GonzálezNo ratings yet
- What Are Universities ForDocument19 pagesWhat Are Universities ForBikash Ranjan MishraNo ratings yet
- L P 10Document13 pagesL P 10Bình Minh HoàngNo ratings yet
- Jharkhand Steel Casting CompaniesDocument6 pagesJharkhand Steel Casting CompaniesCatherine Jovita50% (2)
- Symbolic InteractionismDocument8 pagesSymbolic InteractionismNice tuazonNo ratings yet
- Business Ethics Concepts & Cases: Manuel G. VelasquezDocument19 pagesBusiness Ethics Concepts & Cases: Manuel G. VelasquezRaffi MouradianNo ratings yet
- Vonovia 9M2021 Presentation 20211118Document76 pagesVonovia 9M2021 Presentation 20211118LorenzoNo ratings yet
- HCCM System Technical Specification v1Document12 pagesHCCM System Technical Specification v1Ankita ChowdhuryNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Neural Network For PLC PDFDocument7 pagesNeural Network For PLC PDFMarcelo Moya CajasNo ratings yet
- Dryers in Word FileDocument5 pagesDryers in Word FileHaroon RahimNo ratings yet
- MMADDocument2 pagesMMADHariharan SNo ratings yet
- 03 Seatwork 1 ProjectManagement SenisRachelDocument2 pages03 Seatwork 1 ProjectManagement SenisRachelRachel SenisNo ratings yet
- GSMA Moile Money Philippines Case Study V X21 21Document23 pagesGSMA Moile Money Philippines Case Study V X21 21davidcloud99No ratings yet
- Health Information SystemDocument11 pagesHealth Information SystemVineeta Jose100% (1)
- Food Science, Technology & Nutitions - Woodhead - FoodDocument64 pagesFood Science, Technology & Nutitions - Woodhead - FoodEduardo EstradaNo ratings yet
- Tendernotice 2Document20 pagesTendernotice 2VIVEK SAININo ratings yet
- Nataraja Stotram - A Hymn Without 'CharaNa' and 'ShRi~NgaDocument8 pagesNataraja Stotram - A Hymn Without 'CharaNa' and 'ShRi~NgaSiva Krishna100% (1)
- Electronics HubDocument9 pagesElectronics HubKumaran SgNo ratings yet
- CE ProblemDocument5 pagesCE ProblemJho FNo ratings yet
- Anatomy 090819Document30 pagesAnatomy 090819Vaishnavi GourabathiniNo ratings yet
- Sample Interview Questions for Motivation, Communication, TeamsDocument6 pagesSample Interview Questions for Motivation, Communication, TeamsSahibzada Muhammad MubeenNo ratings yet
- Measures of CentralityDocument13 pagesMeasures of CentralityPRAGASM PROGNo ratings yet
- Product Manual 82434 (Revision C) : Generator Loading ControlDocument26 pagesProduct Manual 82434 (Revision C) : Generator Loading ControlAUGUSTA WIBI ARDIKTANo ratings yet
- Health Optimizing Physical Education: Learning Activity Sheet (LAS) Quarter 4Document7 pagesHealth Optimizing Physical Education: Learning Activity Sheet (LAS) Quarter 4John Wilfred PegranNo ratings yet
- Andrew Linklater - The Transformation of Political Community - E H Carr, Critical Theory and International RelationsDocument19 pagesAndrew Linklater - The Transformation of Political Community - E H Carr, Critical Theory and International Relationsmaria luizaNo ratings yet
- EDIBLE VACCINES: A COST-EFFECTIVE SOLUTIONDocument21 pagesEDIBLE VACCINES: A COST-EFFECTIVE SOLUTIONPritish SareenNo ratings yet
- Short Answers Class 9thDocument14 pagesShort Answers Class 9thRizwan AliNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet