Professional Documents
Culture Documents
Targeting The NLRP3 Inflammasome To Reduce Diet-Induced Metabolic Abnormalities in Mice
Uploaded by
anirbanmanna88320Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Targeting The NLRP3 Inflammasome To Reduce Diet-Induced Metabolic Abnormalities in Mice
Uploaded by
anirbanmanna88320Copyright:
Available Formats
UNCORRECTED PROOF
Molecular Medicine
Targeting the NLRP3 inflammasome to reduce diet-induced metabolic
abnormalities in mice.
Fausto Chiazza1, Aurlie Couturier-Maillard2, Elisa Benetti1, Raffaella Mastrocola3, Debora Nigro3,
Juan C. Cutrin4,5, Loredana Serpe1, Manuela Aragno3, Roberto Fantozzi1, Bernard Ryffel2,
Christoph Thiemermann6*, Massimo Collino1*
1
Dipartimento di Scienza e Tecnologia del Farmaco, Universit di Torino, Turin, Italy
CNRS, UMR7355 INEM, Immunologie et Neurogntique Exprimentales et Molculaires,
University of Orlans, Orlans, France;
3
Dipartimento di Scienze Cliniche e Biologiche, Universit di Torino, Turin, Italy
Dipartimento di Biotecnologie Molecolari e Scienze per la Salute, Universit di Torino, Italy,
5
ININCA-CONICET, Buenos Aires, Argentina,
Queen Mary University of London, Centre for Translational Medicine and Therapeutics, William
Harvey Research Institute, Barts and the London School of Medicine and Dentistry, London, UK
*Both authors contributed equally to this work
Corresponding author: Massimo Collino,
Dipartimento di Scienza e Tecnologia del Farmaco, Universit di Torino,
via P. Giuria 9, 10125 Torino, Italy, Tel: +39 011 6706861 Fax: +39 011 2367955
E-mail address: massimo.collino@unito.it
Running Head: NLRP3 inflammasome as target for diabetes
Keywords: insulin resistance, metabolic disease, inflammation, interleukin-1, BAY 11-7082
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
ABSTRACT
Although the molecular links underlying the causative relationship between chronic low-grade
inflammation and insulin resistance are not completely understood, compelling evidence suggests a
pivotal role of the NLRP3 inflammasome. Here we tested the hypothesis that either a selective
pharmacological inhibition or a genetic down-regulation of the NLRP3 inflammasome results in
reduction of the diet-induced metabolic alterations. Male C57/BL6 wild-type mice and NLRP3-/littermates were fed control diet or high-fat high-fructose diet (HD). A sub-group of HD-fed wildtype mice was treated with the NLRP3 inflammasome inhibitor BAY 11-7082 (3 mg/kg, i.p.). HDfeeding increased plasma and hepatic lipids and impaired glucose homeostasis and renal function.
Renal and hepatic injury was associated with robust increases in pro-fibrogenic markers, while only
minimal fibrosis was recorded. None of these metabolic abnormalities were detected in HD-fed
NLRP3-/- mice, and they were dramatically reduced in HD-mice treated with the NLRP3
inflammasome inhibitor. BAY 11-7082 also attenuated the diet-induced increase in NLRP3
inflammasome expression, resulting in inhibition of caspase-1 activation and interleukin-(IL)-1
and IL-18 production (in liver and kidney). Interestingly, BAY 11-7082, but not gene silencing,
inhibited NF-B nuclear translocation. Overall, these results demonstrate that the selective
pharmacological modulation of the NLRP3 inflammasome attenuates the metabolic abnormalities
and the related organ injury/dysfunction caused by chronic exposure to HD, with effects similar to
those obtained by NLRP3 gene silencing.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
INTRODUCTION
Metabolically driven, chronic, low-grade inflammation has a crucial role in the pathogenesis of
obesity, metabolic syndrome and type 2 diabetes mellitus (T2DM) (1). Enhanced serum
concentrations of pro-inflammatory cytokines play a key role in the development of metabolic
derangements and new anti-inflammatory therapeutic approaches have recently been proposed for
the treatment of these conditions (2, 3). However, the identity of the specific inflammation-related
signaling pathways that are responsible for these metabolic abnormalities are still unknown..
Cytokines of the interleukin (IL)-1 family, particularly IL-1, but also IL-18, are among the most
critical, pro-inflammatory cytokines that reduce insulin formation by pancreatic -cells, thus
promoting both pathogenesis and progression of diabetes (4). IL-1 and IL-18 are produced via
cleavage of pro-IL-1 and pro-IL-18 by caspase-1, which, in turn, is activated by a multi-protein
complex called the NLRP3 inflammasome. Inflammasomes are newly identified multi-protein
platforms responsible for the activation of innate inflammatory processes and instigation of
inflammatory responses during a variety of chronic degenerative diseases (5). Among the
inflammasomes, the most studied in the area of metabolic diseases is the NOD-like receptor family,
pyrin domain containing 3 (NLRP3) inflammasome, which comprises of (a) NLRP3, (b) an
apoptosis-associated speck-like protein containing a caspase activation recruitment domain (ASC)
and (c) caspase-1. The NLRP3 inflammasome plays a substantial role in sensing obesity-associated
inducers of caspase-1 activation and, therefore, regulates the magnitude of the inflammatory
response and, hence, its downstream effects on insulin signaling in different organs, including liver
and kidney (6). The fatty acid palmitate, cholesterol crystals, low-density lipoprotein and ceramide
(generated from fatty acids), which are all increased in abundance during nutritional excess, can
each activate NLRP3, resulting in increased IL-1 production (7-9). We and others have recently
demonstrated that either a high fat diet or a high sugar diet trigger both NLRP3 inflammasome
formation and activation in target organs of metabolic inflammation (10-12). In addition, mice
genetically deficient of NLRP3 are protected against high fat diet-induced insulin resistance (9, 13).
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
Although these data suggest that the NLRP3 inflammasome is a central player in the induction of
insulin resistance, its potential role as pharmacological target for therapeutic intervention in T2DM
is ill defined and no selective NLRP3 inhibitors have been tested in preclinical models of metabolic
disease. No studies have compared the effects of pharmacological inhibition or gene silencing of the
NLRP3 inflammasome in mice chronically fed a diet enriched in both sugars and saturated fats
(high fat, high sugar diet, HD), which are the two major components of the unhealthy diet that
promotes obesity and insulin resistance. Hence, the present study was designed (i) to investigate the
effects of NLRP3 inflammasome gene ablation on the metabolic alterations caused by chronic
exposure to refined fat and fructose, the main ingredients of most processed foods, and (ii) to
determine the potential therapeutic value of the pharmacological modulation of NLRP3
inflammasome by the selective inhibitor BAY 11-7082.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
MATERIALS AND METHODS
Animals and experimental procedures.
This study was carried out in four-week-old male NLRP3/ knockout mice (KO) on C57BL/6
background (14) and NLRP3+/+ littermate control wild type mice (WT), housed in the same animal
unit under conventional housing conditions at 252 C. Both the WT and the KO were randomly
allocated into the following dietary regimens: normal diet (ND WT, n = 10 and ND KO, n = 4) and
a high-fat high sugar diet (HD WT, n = 20, and HD KO, n = 6) for 12 weeks. They were provided
with diet and water ad libitum. HD WT mice were treated with vehicle (n = 10) or BAY 11-7082
(HD WT + BAY, 3 mg/kg i.p. five days/week, n=10) for the last 7 weeks of dietary manipulation.
The BAY 11-7082 dose used in this study was previously found to improve functional and
biochemical deficits associated with experimental diabetic neuropathy (15). NLRP3 silencing was
checked in all KO mice before starting dietary manipulation (Supplementary Figure 1S). The HD
diet contained 45% kcal fat (soybean oil and lard), 20% protein (casein), 35% carbohydrate
(fructose) (D03012907 diet, from Research Diets Inc., USA). The in vivo procedures here described
were approved by the local Ethical Committee (DGSAF 0021573-P-12/11/2013) and are in keeping
with the European Directive 2010/63/EU as well as the Guide for the Care and Use of Laboratory
Animals.
Oral glucose tolerance test (OGTT).
The OGTT was performed by administration of glucose (2 g/kg) by oral gavage after a fasting
period of 6 h. The concentrations of fasting serum glucose were measured with a conventional
glucometer (GlucoMen LX kit, Menarini Diagnostics, Italy).
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
Biochemical analysis.
After 12 weeks of dietary manipulation, the mice were anesthetized using isoflurane and killed by
cardiac puncture and exsanguination. The plasma lipid profile was determined by measuring the
content of triglycerides (TGs), total cholesterol, high-density-lipoprotein (HDL), and low densitylipoprotein (LDL) by standard enzymatic procedures using reagent kits (Hospitex Diagnostics,
Florence, Italy). Plasma insulin was measured using enzyme-linked immunosorbent assay (ELISA,
R&D Systems, Abingdon, UK) kit. The albumin-to-creatinine ratio (ACR) was used to evaluate the
urinary excretion of albumin. Urine samples were collected at 18 hours in metabolic cages and urine
creatinine concentrations were determined using a creatinine kit (ArborAssays LLC, Ann Arbor,
MI, USA), and albumin concentrations were determined using a mouse albumin ELISA
quantification kit (Bethyl Labs, Montgomery, TX, USA).
Western blot analysis.
Liver, kidney and gastrocnemius extracts were prepared as previously described (12). About 60 g
of total proteins were separated by 8% sodium dodecyl sulphate-polyacrylamide gel electrophoresis
and transferred to a polyvinyldenedifluoride membrane, which was then incubated with primary and
secondary antibodies To ascertain that blots were loaded with equal amounts of proteins they were
also incubated with antibody against -actin or tubulin protein. The relative expression of the
protein bands was quantified by densitometric scanning using Gel ProAnalyzer 4.5 (Media
Cybernetics, MD, USA), and standardized for densitometric analysis to -actin levels.
Real-time RT-PCR
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
Total RNA was extracted from liver and kidney samples using the AllPrep DNA/RNA/protein Kit
(Qiagen, Hilden, Germany), according to the manufacture instructions. The total RNA
concentration (g/mL) was determined by the fluorometer Qubit and the Quant-iT RNA Assay
Kit (Invitrogen, Milano, Italy). 500 ng of total RNA were reverse-transcribed using the QuantiTect
Reverse Transcription kit (Qiagen) and the synthesized cDNA was used for real-time PCR. The
cDNA was amplified by real-time PCR using SsoFast EvaGreen (Bio-Rad, Milano, Italy) and
primers (Qiagen) specific for cytokines IL-1 (Mm_Il1b_2_SG cat. QT01048355) and IL-18
(Mm_Il18_1_SG cat. QT00171129). The PCR protocol conditions were as follows: HotStarTaq
DNA polymerase activation step at +95 C for 30 sec, followed by 40 cycles at +95 C for 5
seconds and +55 C for 10 sec. All samples were run in duplicate. At least two non-template
controls were included in all PCR runs. The transcript of the reference gene ribosomal RNA 18S
(Mm_Rn18s_3_SG cat. QT02448075) was used to normalize mRNA data and the quantification
data analyses were performed using the Bio-Rad CFX Manager Software version 1.6 (Bio-Rad,
Milano, Italy) according to the manufacturers instructions. These analyses were performed
following the MIQE guidelines (Minimum Information for Publication of Quantitative Real-time
PCR Experiments) (Bustin et al., 2009).
Histological examination of the kidney and Oil Red staining of the liver
Dewaxed 5 m sections of kidney were stained with hematoxylin and eosin and examined as
previously described (16). Neutral lipids were assessed on sections of frozen liver embedded in
OCT (10 m in thickness) by Oil Red O staining. The degree of fatty change was scored as
following: mild when lipids droplets were observed in no more of 30% of the hepatocytes;
moderate when it compromised between 31-60% of the parenchymal cells, and severe when
steatosis was observed in more of 60% of them.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
Liver TG levels
A sensitive assay kit was used to measure hepatic TGs following the provided protocol
(Triglyceride Quantification Kit, Abnova Corporation, Aachen, Germany).
Histochemistry analysis of collagen deposition in kidney and liver samples
Sirius red stain was performed in 4% formaldehyde buffered solution fixed sections from kidney
and liver to evaluate the degree of fibrosis. In the liver, portal tracts greater than 100 m in size
were not considered as they contain a large amount of collagen and therefore prevent evaluation of
collagen-associated fibrosis.
Determination of TNF-, IL-1, IL-6 and IL-18 in plasma and tissues.
Commercially available ELISA kits (R&D Systems, Abingdon, UK) were used to measure
concentrations of TNF-, IL-1, IL-6 and IL-18 in either plasma and tissue homogenates, according
to the manufacturers instructions.
Materials.
All compounds were from the Sigma-Aldrich Company Ltd. (St. Louis, Missouri, USA). Mouse
anti-IRS-1 [L3D12], rabbit anti-phospho-IRS1 [Ser 307], rabbit anti-Akt [9272], rabbit antiphospho-Akt [Ser 473 D9E], rabbit anti-GSK-3 [27C10], rabbit anti-Phospho-GSK-3 [Ser 9
D3A4], rabbit anti AS160 [2442], rabbit anti-phospho AS160 [Ser 588 D8E4], rabbit anti-NF-kB
p65
[D14E12],
rabbit
anti-Smad2/3
[D7G7],
www.molmed.org
rabbit
anti-Phospho-Smad2
UNCORRECTED PROOF
Molecular Medicine
(Ser465/467)/Smad3(Ser423/425) [D27F4], rabbit anti--actin [13E5]) were from Cell-Signaling
Technology (Beverly, MA, USA); rabbit anti-GLUT4 [ab654] and rabbit anti-TGF- [ab66043] and
(rabbit anti-NALP3 [ab109314]) were from Abcam (Cambridge, UK); rabbit anti-caspase-1 p-10
[M-20 sc-514] was from Santa Cruz (Dallas, Texas, U.S.A.).
Statistical analysis.
All values are expressed as mean S.E.M. for n observations. The results were analyzed by oneway ANOVA followed by a Bonferroni post-hoc test for multiple comparisons. A value of P<0.05
was considered significant.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
RESULTS
Chronic BAY 11-7082 administration and NLRP3 inflammasome knockdown normalized dietinduced impairment of metabolic parameters.
Wild type mice fed with the experimental high fat high sugar diet for 12 weeks (HD WT) had
greater body weights than control diet-fed littermates (ND WT) due to an increased caloric intake
(Table 1). The body weight gain was slightly, but not significantly, reduced by BAY 11-7082.
When compared to NLRP3-/- mice fed a normal diet (ND KO), NLRP3-/- mice exposed to the HD
(HD KO) showed an increased body weight gain. The levels of fasting blood glucose and fasting
serum insulin in both the ND KO and HD KO group were similar to those recorded in the ND WT
group, and significantly lower than that in the HD WT group (P<0.01, Figure 1A and 1B). The
concentrations of fasting serum glucose and insulin in WT mice treated with BAY 11-7082
(HD+BAY WT) were significantly (P<0.05) reduced when compared with that in the HD WT
group, although insulin levels remained significantly higher than that in the ND WT group. The
OGTT revealed that glycemia in the HD WT group following glucose challenge was higher than
that in the ND WT group (Figure 1C). In contrast, the dynamic changes in the levels of blood
glucose in either the HD+BAY WT and HD KO groups of mice were similar to those in the related
control groups (ND WT and ND KO, respectively).
Effects of BAY 11-7082 administration and NLRP3 inflammasome deficiency on insulin
signaling pathway in the liver and skeletal muscle.
The levels of total expression of IRS-1, Akt, and GSK-3, a downstream target of Akt, were
similar in all groups of mice (Figure 2) when measured in both liver and skeletal muscle, suggesting
that BAY 11-7082 treatment and NLRP3-/- downregulation did not alter the expression of the key
components of the insulin signaling pathway. In contrast, significant changes in the degree of
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
protein phosphorylation were recorded in the liver and skeletal muscle of WT mice exposed to HD.
These alterations in protein phosphorylation and, hence, activation status of the respective proteins
indicate that HD led to an impairment in insulin signaling. In contrast, treatment of wild-type mice
exposed to HD with BAY 11-7082 abolished all of the alterations in insulin signaling caused by HD
in vehicle-treated animals. Moreover, the degree of phosphorylation of IRS-1, Akt and GSK-3 was
similar between the ND-KO and HD-KO groups of mice. In the gastrocnemius of WT mice, the
impairment of insulin sensitivity due to dietary manipulation correlated with a slight reduction in
GLUT-4 expression, which was increased following BAY 11-7082 administration in WT mice and
not affected by diet in KO mice (Figure 3). The Thr642 phosphorylation of the Akt substrate 160
(AS160), which is needed for GLUT-4 translocation to the cell membrane, was reduced by HD in
the gastrocnemius of WT mice and it was restored to basal levels by BAY 11-7082, thus indicating
an improvement in GLUT-4 translocation to the plasma membrane when the drug was administered
to WT mice. In contrast, AS160 phosphorylation was not affected by dietary manipulation in
NLRP3 KO mice.
Chronic BAY 11-7082 administration or ablation of NLRP3 inflammasome reduced diet-induced
dyslipidemia and hepatic lipid accumulation.
Concurrent with the development of insulin resistance, HD-fed wild-type animals displayed a twofold increase in serum TG levels as well as a robust increase in total cholesterol and LDL
concentrations in comparison with ND WT mice (Table 1). The diet-induced changes in serum lipid
profile were suppressed by the pharmacological inhibition of NLRP3 inflammasome, whereas the
same experimental diet did not evoke any significant change in the serum lipid profile of NLRP3-/mice. As shown by Oil Red O staining (Figure 4A), the HD diet resulted in a significant lipid
deposition in the liver. Microscopically, the intensity of the steatosis was severe in almost all
hepatocytes containing cytoplasmic micro- or macrovacuolar lipid droplets. Chronic administration
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
of BAY 11-780 attenuated neutral fat accumulation and no difference in lipid accumulation was
recorded between ND KO and HD KO groups of mice. These effects were confirmed by
measurement of TG content (Figure 4B). Liver Oil red staining as well as assessment of hepatic TG
levels showed no effects of the HD on lipid accumulation in the liver of KO mice. As shown in
Figure 4C, the diet-induced lipid accumulation in the liver of WT mice was associated with
significant local increase in TNF- levels, which was counteracted by either pharmacological
inhibition or genetic knockdown of the NLRP3 inflammasome.
Chronic BAY 11-7082 administration or ablation of NLRP3 inflammasome limited diet-induced
renal damage.
Histological analysis of kidneys from the HD WT group revealed a marked degree of vacuolar
degeneration at level of the S1-S2 segments of the proximal convoluted tubules. Others tubular
structures of the nephrons were histologically preserved. Neither glomerular changes nor interstitial
inflammation were detected (Figure 5). Kidneys of the BAY-11-7082 treated mice, as well as those
from the NLRP3-/- mice, appeared protected against the deleterious effects of the dietary
manipulation. Although vacuolar degeneration was detectable, it was limited to less than 20 % of
the proximal convoluted tubules examined. The remaining parenchyma did not show any significant
alterations. When compared with ND WT mice, WT mice subjected to HD demonstrated a
significant increase in the albumin-to-creatinine ratio (ACR), which is an indicator of albuminuria
(401.2333.16 vs. 98.0613.16 g/mg, P<0.05; Figure 5F). Administration of BAY-11-7082
significantly attenuated the diet-induced rise in ACR (271.365.63 vs. 401.2333.16 g/mg, P
<0.05). An impaired ACR was also recorded in the kidney of NLRP3-/- mice fed the experimental
diet in comparison to control NLRP3-/- mice (263.9548.18 vs. 114.0341.94 g/mg, P <0.05).
However, the diet-induced increase in ACR in HD KO was significantly lower than that recorded in
HD WT mice (P <0.05).
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
Chronic BAY 11-7082 administration or ablation of NLRP3 inflammasome reduced diet-induced
overexpression of pro-fibrotic markers in liver and kidney.
As shown in Figure 6, Western blot analysis of the expression levels of transforming growth factor
beta (TGF-) in the liver and kidney of WT mice demonstrated a significant increase in this profibrotic marker following dietary manipulation, which led to downstream phosphorylation of
Smad2, suggestive of activation. However, these effects did not lead to a marked fibrotic process in
the liver, at least when determined at 12 weeks, as no difference among the groups was shown in
the amount of collagen detected in the portal spaces and around the terminal hepatic venules; and
the acinar structure of the liver was preserved. In contrast, kidneys of WT mice exposed to HD
showed a moderate peritubular fibrosis, with Sirius red collagen accumulation observed mainly
around the S1-S2 portion of the proximal convoluted tubule. Interestingly, chronic BAY 11-7082
administration as well as NLRP3 inflammasome deficiency blunted the diet-induced activation of
the TGF-/Smad2 pro-fibrotic signaling cascade and the renal collagen accumulation.
Diet-induced NLRP3 activation was suppressed by BAY 11-7082 administration or NLRP3 gene
silencing
HD caused a marked increase in expression of NLRP3 and activated caspase-1 in WT mice (Figure
7), which was paralleled by a robust increase in expression of IL-1 and IL-18 mRNA
(Supplementary Figure 2S) associated with upregulated local and systemic concentrations of mature
IL-1 and IL-18 (Figure 8). Chronic treatment with BAY 11-7082 reduced the expression of the
components of the NLRP3 inflammasome complex as well as the mRNA levels and active forms of
the cytokines IL-1 and IL-18. In the kidney (but not in the liver), the levels of IL-1 and IL-18 in
the HD+BAY group remained higher than those in the ND WT group. As expected, the NLRP3
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
inflammasome complex was not activated in KO mice and, hence, the HD diet did not trigger the
production of the active forms of IL-1 and IL-18 in these mice. The significant reduction in
systemic and local levels of NLRP3 inflammasome-dependent cytokines, but not IL-6
(Supplementary Figure 3S), by BAY 11-7082 administration or NLRP3-/- gene silencing confirm
that the prevention/reduction of the HD-induced metabolic alterations were secondary to the lack of
activation of the inflammasome.
BAY 11-7082 administration, but not NLRP3 silencing, inhibited diet-induced NF-kB activation.
When compared with WT mice exposed to control diet, mice that underwent the experimental diet
showed an increased phosphorylation of IB on Ser32/36 (Fig. 9A and 9C), which was associated
with an increased translocation of the p65 NF-B subunit from the cytosol to the nucleus (Fig. 9B
and 9D), in both liver and kidney. In contrast, chronic administration of BAY 11-7082 to HD WT
mice diminished of both IB phosphorylation and p65 nuclear translocation (Fig. 9B). The
experimental diet induced a robust induction of both IB phosphorylation and NF-B activation in
the livers and kidneys of NLRP3-/- mice, similar to that recorded in the HD WT group, thus
indicating that NLRP3 silencing does not affect NF-B nuclear translocation.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
DISCUSSION
In the present work, we demonstrated that NLRP3 -/- deficiency exerts protective effects against the
metabolic alterations evoked by exposure to an high-fat diet combined with an overconsumption of
the simple sugar fructose, whose use as sweetener in food processing has dramatically increased
over the last decade. Prior observations indicated that activation of the NLRP3 inflammasome plays
a role in T2DM pathogenesis, possibly by driving inflammation, obesity and insulin-resistance (7,
9, 10, 17, 18). Nevertheless, its role as specific pharmacological target for drug therapy of insulin
resistance and related metabolic diseases has been poorly investigated. There are limited
experimental data showing that pharmacological tools may ameliorate diabetic injury by regulating
NLRP3 inflammasome activity (19-22). However, none of the proposed pharmacological strategies
is based on the use of selective and specific NLRP3 inflammasome inhibitors. Thus, the described
effects could be due to interferences up- or down-stream of inflammasome activation. Only the
evaluation of small molecules that are able to selectively inhibit the NLRP3 inflammasome may
allow the future design of novel and effective therapeutics for diseases caused by excessive
activation of the NLRP3 inflammasome. However, efficacious NLRP3 inflammasome inhibitors are
still at an early stage of development. One of the few compounds which has been demonstrated to
directly target the NLRP3 inflammasome is BAY 11-7082 and selectively inhibits the ATPase
activity of NLRP3 required for its activation (23). Our study provides the first evidence that the
chronic administration of BAY11-7082 protects against the diet-induced metabolic alterations and
that the qualitative and quantitative effects of BAY11-7082 (with very minor exceptions discussed
below) are similar to those recorded in NLRP3-/- mice. The improved glucose tolerance, here
documented, was, at least in part, due to an improvement in the signaling pathway of insulin in HDfed mice. The IRS-1/Akt/GSK-3 cascade is a key regulator of glucose transportation, glycogen
synthesis and glycolysis (24). Here we demonstrated that the defects in the insulin signaling
observed in both the livers and skeletal muscles of HD-fed mice could be restored by
pharmacological inhibition of NLRP3 activity. Accordingly, the dietary manipulation did not evoke
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
any significant impairment in phosphorylation of IRS-1, Akt and GSK-3, a substrate of Akt, in
NLRP3-/- mice, thus confirming that NLRP3 suppression potentiates Akt activity. NLRP3
suppression was associated with a significant improvement in expression and membrane
translocation of GLUT-4, the most abundant glucose transporter isoform in skeletal muscle (25),
thus facilitating glucose transport. As previous findings convincingly showed that Akt regulates
translocation, targeting and fusion of GLUT-4-containing vesicles in mouse skeletal myocytes (26,
27), we speculate that GLUT-4 translocation and subsequent glucose uptake in skeletal muscle
following NLRP3 modulation is mainly due to activation of the IRS-1/Akt/GSK-3 pathway.
Overall, our data demonstrate for the first time that activation of the NLRP3 inflammasome directly
modulates the Akt pathway, thus affecting a crucial pathogenic mechanism responsible for the
development of insulin resistance. Preservation of insulin sensitivity may also account for the
improved lipid profile detected in both HD+BAY WT and HD KO groups. As previously
documented (28), the hyperinsulinemic state due to chronic exposure to HD may induce greater
lipid accumulation, thus enhancing lipotoxicity. Mice exposed to HD showed obvious lipid
accumulation and hepatic steatosis was associated with local activation of NLRP3 inflammasome.
Interestingly, NLRP3 gene silencing as well as BAY 11-7082 treatment effectively prevented lipid
accumulation as well as local and systemic inflammation by suppressing the release of TNF-, IL1 and IL-18. Similarly, inhibition of NLRP3 inflammasome activity within the mouse kidney
attenuated both renal injury (histology) and dysfunction (albuminuria) caused by HD. Consistent
with or results, a recent study showed that a high-fat diet increases NLRP3 inflammasome activity
in glomeruli, resulting in glomerular inflammation and consequent glomerular injury (29).
Moreover, we previously observed a similar activation of this inflammatory machinery in the
kidney of mice exposed to an excessive intake of fructose (12). Inflammatory microenvironments
have been previously demonstrated to promote TGF- signaling, which in turn can stimulate
Smad2/3 phosphorylation thus increasing profibrogenic responses in the liver and kidney (30, 31).
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
In this study collagen deposition in liver was not detectable and minimal in kidneys of HD WT
mice, despite of sustained significant inflammation. However, we could detect a robust increase in
TGF- levels in both liver and kidney of WT mice after HD exposure and this effect was associated
with enhanced phosphorylation of Smad2, which has an essential role in the development and
progression of obesity-related liver and kidney diseases. Very recently, the TGF-/Smad2 signaling
has also been shown to be involved in regulating insulin gene transcription and energy homeostasis
(32). Thus, based on our data it appears that HD diet induces a local inflammatory response,
resulting in activation of the TGF-/Smad2 signaling, which may potentially contribute to
development of insulin resistance and to late liver and kidney fibrosis (not yet detectable at the time
point here measured). Our observation is in concordance with previous reports indicating that local
inflammation precedes fibrosis, when the latter is determined by measuring collagen production and
accumulation (33, 34). Our data showing reduced activation of the TGF-/Smad3 signaling in KO
mice exposed to the same diet manipulation raise the possibility of an involvement of the NLRP3
inflammasome pathway in modulation of the early markers of fibrosis. The present study did not
aim to elucidate the exact mechanisms mediating the liver and kidney injury evoked by NALP3
inflammasome activation. However, we speculate that the diet-induced increased production of
inflammatory cytokines, such as IL-1 and IL-18 resulting from activation of NALP3
inflammasomes may act in an autocrine or paracrine fashion to change hepatic and renal cell
function. Moreover, we cannot rule out a contribution of the non-inflammatory effects of NALP3
inflammasome activation such as pyroptosis, cytoskeleton changes and alteration of cell
metabolism, which have also been reported to mediate the detrimental local action of
inflammasome activation (35, 36). Another unresolved question is whether the NLRP3
inflammasome activation occurs at the level of resident cells, as results so far obtained from
preclinical models of obesity and insulin resistance are quite contrasting. There is good evidence
that both haematopoietic and non-haematopoietic cells are involved in NLRP3 inflammasome
activation in both renal and hepatic tissues (37-40). The above data provide evidence in support of
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
NLRP3 inflammasome-dependent cellular and molecular events mediating the protective effects of
BAY 11-7082 against diet-induced metabolic abnormalities. It has to be stressed, however, that
BAY 11-7082 is not only an inhibitor of NLRP3 inflammasome activity, as this molecule may act
also as inhibitor of NF-B activation and other inflammatory signaling pathways (41). For this
reason, we also investigated the effects of BAY 11-7082 on NF-B nuclear translocation, as BAY
11-7082 is known to block IB phosphorylation and the subsequent NF-B activation,
independently of its inhibitory effects on NLRP3 inflammasome formation and activation (23).
Suppression of the NF-B pathway by targeted KO mice or pharmacological inhibition of this
pathway can reduce insulin resistance in mice exposed to dietary manipulation (42). Thus, both NFB nuclear translocation and activation of the NLRP3 inflammasome pathway coordinately
contribute to insulin resistance in obesity. Here we demonstrated a diet-induced activation of the
NF-B pathway in both liver and kidney and we confirmed that the administration of BAY 11-7082
inhibited phosphorylation and subsequently the degradation of IBs, which reduces nuclear
translocation of NF-B via its sequestration in an inactive state in the cytoplasm. Intriguingly, the
inhibition of NF-B activity was not seen in organs from NLRP3 KO mice. Thus, based on the
considerable qualitative and quantitative similarities between the pharmacological effects elicited
by BAY 11-7082 and the NLRP3 gene silencing in our experimental conditions, we speculate that
NLRP3 inhibition alone is sufficient to evoke a marked improvement in insulin resistance and organ
dysfunction, which is not further strengthen by the drug-induced NF-B inhibition. However, we
acknowledge that further studies with more selective NLRPL3 inflammasome inhibitors are
required to demonstrate a phencopy of data obtained from the genetic absence of the NALP3
deficient mouse. In addition, we are aware that an important limitation of the present study is that
WT and NLRP3 inflammasome KO mice were not littermates, thus involving potential differences
at epigenetic and microbiome levels. As recent findings clearly show that both NLRP3
inflammasome silencing and dietary manipulation evoke dysbiosis (43-45), it will be important to
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
perform future studies aiming at directly determining possible microbiome-dependent differences in
the role of NLRP3 inflammasome in modulating diet-induced metabolic abnormalities.
CONCLUSION
Overall, our results support the view that activation of the NLRP3 inflammasome drives the
development of T2DM and the associated end-organ injury and, most notably, highlights the use of
selective inhibitors of the NLRP3 inflammasome as novel and promising treatment options for
T2DM. In fact, while NLRP3 inflammasome silencing demonstrates that the suppression of this
pathway prevents the development of insulin resistance in response to HD feeding, the use of the
selective inflammasome inhibitor BAY11-7082, which was administered only for the last 7 weeks
of the 12 weeks-dietary manipulation, demonstrates that the deleterious effects of HD exposure may
be reversed by the pharmacological inhibition of the NLRP3 inflammasome. Interestingly, selective
inhibition of NLRP3 by a small molecule such as BAY 11-7082 might present certain advantages
over the use of biological agents targeted at IL-1 and its receptor, including fewer
immunosuppressive effects and better pharmacokinetics and cost effectiveness. Further preclinical
and clinical studies are needed to further explore this possibility and to investigate/ensure the safety
of this innovative pharmacological approach.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
Acknowledgments
This work was supported by grants from the University of Turin (Local Search ex 60%). There are
no reported potential conflicts of interest relevant to this article. M.C. designed the study, performed
the experiments, analyzed the data and wrote the manuscript. F.C. and MR performed the
experiments and contributed to the analysis and interpretation of data. E.B., A.C.M., L.S. and D.N.
researched data. R. F., M.A. and B.R. contributed to the discussion, and reviewed the manuscript.
C.T. designed the study and edited the final version of the manuscript. M.C. is the guarantor of this
work and has access to all data here reported. All authors approved the final version.
Disclosure
The authors have no competing interests, or other interests that might affect results and discussion
here reported.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
Calay ES, Hotamisligil GS. (2013) Turning off the inflammatory, but not the metabolic, flames. Nat
Med 19: 265-267.
Donath MY. (2014) Targeting inflammation in the treatment of type 2 diabetes: time to start. Nat
Rev Drug Discov 13: 465-476.
Tabas I, Glass CK. (2013) Anti-inflammatory therapy in chronic disease: challenges and
opportunities. Science 339: 166-172.
Tack CJ, Stienstra R, Joosten LA, Netea MG. (2012) Inflammation links excess fat to insulin
resistance: the role of the interleukin-1 family. Immunol Rev 249: 239-252.
Schroder K, Tschopp J. (2010) The inflammasomes. Cell 140: 821-832.
Benetti E, Chiazza F, Patel NS, Collino M. (2013) The NLRP3 Inflammasome as a novel player of the
intercellular crosstalk in metabolic disorders. Mediators Inflamm 2013: 678627.
Wen H, et al. (2011) Fatty acid-induced NLRP3-ASC inflammasome activation interferes with insulin
signaling. Nat Immunol 12: 408-415.
Duewell P, et al. (2010) NLRP3 inflammasomes are required for atherogenesis and activated by
cholesterol crystals. Nature 464: 1357-1361.
Vandanmagsar B, et al. (2011) The NLRP3 inflammasome instigates obesity-induced inflammation
and insulin resistance. Nat Med 17: 179-188.
Stienstra R, et al. (2010) The inflammasome-mediated caspase-1 activation controls adipocyte
differentiation and insulin sensitivity. Cell Metab 12: 593-605.
Reynolds CM, et al. (2012) Dietary saturated fatty acids prime the NLRP3 inflammasome via TLR4 in
dendritic cells-implications for diet-induced insulin resistance. Mol Nutr Food Res 56: 1212-1222.
Collino M, et al. (2013) Reversal of the deleterious effects of chronic dietary HFCS-55 intake by
PPAR- agonism correlates with impaired NLRP3 inflammasome activation. Biochem Pharmacol 85:
257-264.
Stienstra R, et al. (2011) Inflammasome is a central player in the induction of obesity and insulin
resistance. Proc Natl Acad Sci U S A 108: 15324-15329.
Martinon F, Ptrilli V, Mayor A, Tardivel A, Tschopp J. (2006) Gout-associated uric acid crystals
activate the NALP3 inflammasome. Nature 440: 237-241.
Kumar A, Negi G, Sharma SS. (2012) Suppression of NF-B and NF-B regulated oxidative stress and
neuroinflammation by BAY 11-7082 (IB phosphorylation inhibitor) in experimental diabetic
neuropathy. Biochimie 94: 1158-1165.
Collino M, et al. (2014) A non-erythropoietic peptide derivative of erythropoietin decreases
susceptibility to diet-induced insulin resistance in mice. Br J Pharmacol 171: 5802-5815.
Goossens GH, et al. (2012) Expression of NLRP3 inflammasome and T cell population markers in
adipose tissue are associated with insulin resistance and impaired glucose metabolism in humans.
Mol Immunol 50: 142-149.
Lee HM, et al. (2013) Upregulated NLRP3 inflammasome activation in patients with type 2 diabetes.
Diabetes 62: 194-204.
Wang C, Pan Y, Zhang QY, Wang FM, Kong LD. (2012) Quercetin and allopurinol ameliorate kidney
injury in STZ-treated rats with regulation of renal NLRP3 inflammasome activation and lipid
accumulation. PLoS One 7: e38285.
Yang SJ, Lim Y. (2014) Resveratrol ameliorates hepatic metaflammation and inhibits NLRP3
inflammasome activation. Metabolism 63: 693-701.
Honda H, et al. (2014) Isoliquiritigenin is a potent inhibitor of NLRP3 inflammasome activation and
diet-induced adipose tissue inflammation. J Leukoc Biol 96: 1087-1100.
Shan Q, et al. (2014) Purple sweet potato color ameliorates kidney damage via inhibiting oxidative
stress mediated NLRP3 inflammasome activation in high fat diet mice. Food Chem Toxicol 69: 339346.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
Juliana C, et al. (2010) Anti-inflammatory compounds parthenolide and Bay 11-7082 are direct
inhibitors of the inflammasome. J Biol Chem 285: 9792-9802.
Taniguchi CM, Emanuelli B, Kahn CR. (2006) Critical nodes in signalling pathways: insights into
insulin action. Nat Rev Mol Cell Biol 7: 85-96.
Bouzakri K, et al. (2006) siRNA-based gene silencing reveals specialized roles of IRS-1/Akt2 and IRS2/Akt1 in glucose and lipid metabolism in human skeletal muscle. Cell Metab 4: 89-96.
Leto D, Saltiel AR. (2012) Regulation of glucose transport by insulin: traffic control of GLUT4. Nat
Rev Mol Cell Biol 13: 383-396.
Zeng XQ, et al. (2012) Knockdown of NYGGF4 increases glucose transport in C2C12 mice skeletal
myocytes by activation IRS-1/PI3K/AKT insulin pathway. J Bioenerg Biomembr 44: 351-355.
Semple RK, et al. (2009) Postreceptor insulin resistance contributes to human dyslipidemia and
hepatic steatosis. J Clin Invest 119: 315-322.
Boini KM, et al. (2014) Activation of inflammasomes in podocyte injury of mice on the high fat diet:
Effects of ASC gene deletion and silencing. Biochim Biophys Acta 1843: 836-845.
Dattaroy D, et al. (2015) Micro-RNA 21 inhibition of SMAD7 enhances fibrogenesis via leptinmediated NADPH oxidase in experimental and human nonalcoholic steatohepatitis. American
journal of physiology. Gastrointestinal and liver physiology 308: G298-312.
Lan HY, Chung AC. (2012) TGF-beta/Smad signaling in kidney disease. Seminars in nephrology 32:
236-243.
Nomura M, et al. (2014) SMAD2 disruption in mouse pancreatic beta cells leads to islet hyperplasia
and impaired insulin secretion due to the attenuation of ATP-sensitive K+ channel activity.
Diabetologia 57: 157-166.
Velayudham A, et al. (2009) VSL#3 probiotic treatment attenuates fibrosis without changes in
steatohepatitis in a diet-induced nonalcoholic steatohepatitis model in mice. Hepatology 49: 989997.
Witek RP, et al. (2009) Pan-caspase inhibitor VX-166 reduces fibrosis in an animal model of
nonalcoholic steatohepatitis. Hepatology 50: 1421-1430.
Chen GY, Nuez G. (2010) Sterile inflammation: sensing and reacting to damage. Nat Rev Immunol
10: 826-837.
Lamkanfi M. (2011) Emerging inflammasome effector mechanisms. Nat Rev Immunol 11: 213-220.
Vilaysane A, et al. (2010) The NLRP3 inflammasome promotes renal inflammation and contributes
to CKD. J Am Soc Nephrol 21: 1732-1744.
Solini A, et al. (2013) The purinergic 2X7 receptor participates in renal inflammation and injury
induced by high-fat diet: possible role of NLRP3 inflammasome activation. J Pathol 231: 342-353.
Csak T, et al. (2011) Fatty acid and endotoxin activate inflammasomes in mouse hepatocytes that
release danger signals to stimulate immune cells. Hepatology 54: 133-144.
Wree A, et al. (2014) NLRP3 inflammasome activation results in hepatocyte pyroptosis, liver
inflammation, and fibrosis in mice. Hepatology 59: 898-910.
Lee J, Rhee MH, Kim E, Cho JY. (2012) BAY 11-7082 is a broad-spectrum inhibitor with antiinflammatory activity against multiple targets. Mediators Inflamm 2012: 416036.
Arkan MC, et al. (2005) IKK-beta links inflammation to obesity-induced insulin resistance. Nat Med
11: 191-198.
Dupaul-Chicoine J, et al. (2010) Control of intestinal homeostasis, colitis, and colitis-associated
colorectal cancer by the inflammatory caspases. Immunity 32: 367-378.
Hirota SA, et al. (2011) NLRP3 inflammasome plays a key role in the regulation of intestinal
homeostasis. Inflammatory bowel diseases 17: 1359-1372.
Ridaura VK, et al. (2013) Gut microbiota from twins discordant for obesity modulate metabolism in
mice. Science 341: 1241214.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
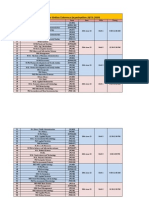
TABLE 1
Metabolic parameters at 12 weeks of dietary manipulation
ND WT
HD WT
HD+BAY WT
ND KO
HD KO
(n = 10)
(n = 10)
(n = 10)
(n = 4)
(n = 6)
8.00.4
14.90.7*
12.10.9*
7.81.2
15.90.8
Food intake, g/die
2.480.48
2.340.06
2.190.10
2.720.12
2.410.21
Caloric intake, kcal/die
9.230.24
11.320.24*
10.390.45
9.520.13
11.480.19
Serum triglyceride, mmol/L
0.390.04
0.600.06*
0.400.03
0.300.04
0.370.04
Serum total cholesterol, mmol/L
2.080.09
2.520.07*
2.200.08
2.020.06
2.200.04
Serum LDL, mmol/L
0.760.08
1.210.09*
0.870.14
0.0840.04
0.960.05
Serum HDL, mmol/L
1.050.05
1.030.07
1.010.07
1.030.06
1.040.07
Body weight gain, g
Data are meansS.E.M.
* p<
0.05 vs ND WT
p< 0.05 vs HD WT
www.molmed.org
p< 0.05 vs ND KO
UNCORRECTED PROOF
Molecular Medicine
Figure Legends
Figure 1. Effects of chronic exposure to a normal diet (ND) or a high-fat high-sugar diet (HD) on
serum insulin (Panel A), blood glucose (Panel B) and oral glucose tolerance (Panel C), evaluated in
NLRP3-/- knockout mice (KO) and wild type mice (WT) treated or not with BAY 11-7082 (BAY, 3
mg/kg, i.p.). Results are expressed as meanS.E.M of 4-5 animals per group.
Figure 2. Effects of diet manipulation and NLRP3 inflammasome inhibition or silencing on insulin
signal transduction in liver and skeletal muscle. Western blot analysis of total IRS-1 and Ser307
phosphorylation (Panel A), total Akt and Ser473 phosphorylation (Panel B), and total GSK-3 and
Ser9 phosphorylation (Panel C) were performed in the liver and gastrocnemius of NLRP3-/knockout mice (KO) and wild type mice (WT) treated or not with BAY 11-7082 (BAY, 3 mg/kg,
i.p.). The relative expression of the protein bands was expressed as relative optical density (O.D.)
and standardized to the corresponding -actin contents. The data are means S.E.M. of pooled data
from three separate experiments (n = 4-6 mice per group). P < 0.05 versus ND WT.
Figure 3. Effects of diet manipulation and NLRP3 inflammasome inhibition or silencing on GLUT4 expression in the skeletal muscle. Western blot analysis of GLUT-4 (Panel A) and AS160 total
protein expression and Thr642 phosphorylation (Panel B). were performed in the liver and
gastrocnemius of NLRP3-/- knockout mice (KO) and wild type mice (WT) treated or not with BAY
11-7082 (BAY, 3 mg/kg, i.p.). The relative expression of the protein bands was expressed as
relative optical density (O.D.) and standardized to the corresponding -actin contents. The data are
means S.E.M. of pooled data from three separate experiments (n = 4-6 mice per group). P <
0.05 versus ND WT.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
Figure 4. Effects of diet manipulation and NLRP3 inflammasome inhibition or silencing on liver
lipid accumulation and inflammation. Panel A: representative photomicrographs (40
magnification) of Oil Red O staining on liver sections from either NLRP3-/- knockout mice (KO) or
wild type mice (WT) treated or not with BAY 11-7082 (BAY, 3 mg/kg, i.p.) and maintained on a
normal diet (ND) or a high-fat high-sugar diet (HD). Panel B: triglyceride (TG) content in mouse
liver. Panel C: TNF- concentrations in mouse liver. Data are meanS.E.M of 4-6 animals per
group. P < 0.05 vs ND WT.
Figure 5. Effects of diet manipulation and NLRP3 inflammasome inhibition or silencing on kidney
structure and function. Panels A-E: histological appearance of kidneys from either NLRP3-/knockout mice (KO) or wild type mice (WT) treated or not with BAY 11-7082 (BAY, 3 mg/kg,
i.p.) and maintained on a normal diet (ND) or a high-fat high-sugar diet (HD). Panel F: urinary
albumin-to-creatinine (ACR) levels in the absence or presence of diet manipulation and BAY 117082 treatment. Values are mean SEM of 4-6 animals per group. P < 0.05 versus ND WT; P
< 0.05 versus HD WT; P < 0.05 versus HD KO.
Figure 6. Effects of diet manipulation and NLRP3 inflammasome inhibition or silencing on hepatic
and renal fibrotic response. Western blot analysis of TGF- (Panels A and D) and Smad2 (Panels B
and E) proteins in the liver and kidney of NLRP3-/- knockout mice (KO) or wild type mice (WT)
exposed or not to diet manipulation in the absence or presence of BAY 11-7082 (BAY, 3 mg/kg,
i.p.).
Representative Sirus red staining of liver and kidney sections from WT or KO mice fed a control
diet, HD diet in the absence or presence of BAY 11-7082 (BAY, 3 mg/kg, i.p.) are reported in
Panels C and F, respectively. The autoradiograms here reported are representative of three
independent experiments. The relative expression of the protein bands was expressed as relative
optical density (O.D.) and standardized to the corresponding -actin contents. The data are means
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
S.E.M. of pooled data from three separate experiments (n = 4-6 mice per group). P < 0.05 versus
ND WT.
Figure 7 Western blot analysis of NLRP3, procaspase-1 and activated caspase-1 proteins in the
liver and kidney of NLRP3-/- knockout mice (KO) or wild type mice (WT) exposed or not to diet
manipulation in the absence or presence of BAY 11-7082 (BAY, 3 mg/kg, i.p.). The
autoradiograms here reported are representative of three independent experiments.
Figure 8. Effects of diet manipulation and NLRP3 inflammasome inhibition or silencing on local
and systemic levels of IL-1 and IL-18. IL-1 and IL-18 concentrations were analyzed by enzymelinked immunosorbent assay (ELISA) in liver (Panels A and B), kidney (Panels C and D) and serum
(Panels E and F) of NLRP3-/- knockout mice (KO) or wild type mice (WT) maintained on a normal
diet (ND) or a high-fat high-sugar diet (HD), in the absence or presence of BAY 11-7082 (BAY, 3
mg/kg, i.p.). Data are means S.E.M. of 4-6 animals/group. P < 0.05 versus ND WT.
Figure 9. Effects of diet manipulation and NLRP3 inflammasome inhibition or silencing on NF-kB
signaling pathway. Signaling events were assessed in liver (Panels A and B) and kidney (Panels C
and D) tissues from NLRP3-/- knockout mice (KO) or wild type mice (WT) maintained on a normal
diet (ND) or a high-fat high-sugar diet (HD), in the absence or presence of BAY 11-7082 (BAY, 3
mg/kg, i.p.). The relative expression of the protein bands was expressed as relative optical density
(O.D.) and standardized to the corresponding -actin contents. NFB p65 subunit translocation was
evaluated expressing p65 subunit levels as a nucleus:cytosol ratio corrected for the -actin contents
and normalized using the ND WT band. The data are means S.E.M. of pooled data from three
separate experiments (n = 4-6 mice per group). P < 0.05 versus ND WT; P < 0.05 vs HD WT;
P < 0.05 vs ND KO.
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
UNCORRECTED PROOF
Molecular Medicine
www.molmed.org
You might also like
- Leptin: Regulation and Clinical ApplicationsFrom EverandLeptin: Regulation and Clinical ApplicationsSam Dagogo-Jack, MDNo ratings yet
- Grupo 3 Obesity InflammationDocument9 pagesGrupo 3 Obesity InflammationJeisonAlejandroÁlvarezVergaraNo ratings yet
- Ijo 201493 ADocument9 pagesIjo 201493 AKurtisNo ratings yet
- Jurnal InternationalDocument9 pagesJurnal InternationalAngelNo ratings yet
- 1diet-Induced Obesity Increases NF-JB Signaling in Reporter MiceDocument8 pages1diet-Induced Obesity Increases NF-JB Signaling in Reporter MicepopopioNo ratings yet
- Berberine Moderates Glucose and Lipid Metabolism TDocument10 pagesBerberine Moderates Glucose and Lipid Metabolism THitesh VermaNo ratings yet
- Flaxseed OilDocument36 pagesFlaxseed OilKamal UddinNo ratings yet
- Research ArticleDocument12 pagesResearch ArticleKarthiNo ratings yet
- Pnpla2 rs693Document7 pagesPnpla2 rs693Vishnu Sai MokshagnaNo ratings yet
- Diabetes PDFDocument12 pagesDiabetes PDFDANIELA MALAGÓN MONTAÑONo ratings yet
- Microrna 375 Mediates Palmitate-Induced Enteric Neuronal Damage and High-Fat Diet-Induced Delayed Intestinal Transit in MiceDocument14 pagesMicrorna 375 Mediates Palmitate-Induced Enteric Neuronal Damage and High-Fat Diet-Induced Delayed Intestinal Transit in MicekasabeNo ratings yet
- Clinical Nutrition ESPEN: Hiroshige Itakura, Michie Kobayashi, Seiji NakamuraDocument7 pagesClinical Nutrition ESPEN: Hiroshige Itakura, Michie Kobayashi, Seiji NakamuraPáblo EugênioNo ratings yet
- Diabetes 2Document9 pagesDiabetes 2Adán LópezNo ratings yet
- 2090 FullDocument9 pages2090 FullChloe WongNo ratings yet
- Moderate Weight Loss Attenuates Chronic Endoplasmic Reticulum Stress and Mitochondrial Dysfunction in Human ObesityDocument10 pagesModerate Weight Loss Attenuates Chronic Endoplasmic Reticulum Stress and Mitochondrial Dysfunction in Human ObesityJulia SCNo ratings yet
- Diabetes in Mice With Selective Impairment of Insulin Action in Glut4-Expressing TissuesDocument10 pagesDiabetes in Mice With Selective Impairment of Insulin Action in Glut4-Expressing TissuesDraGollarzaNo ratings yet
- Alterations in Peripheral Purinergic and Muscarinic Signaling of Rat Bladder After Long-Term Fructose-Induced Metabolic SyndromeDocument13 pagesAlterations in Peripheral Purinergic and Muscarinic Signaling of Rat Bladder After Long-Term Fructose-Induced Metabolic SyndromeThalia KarampasiNo ratings yet
- Zhou 2019Document11 pagesZhou 2019Andreea Claudia NegrilaNo ratings yet
- MD 1 Section E2 Group 3 Biochem REVISEDDocument10 pagesMD 1 Section E2 Group 3 Biochem REVISEDParadoxistNo ratings yet
- Chronic Inflammation in Fat Plays A Crucial Role in The Development of Obesity-Related Insulin ResistanceDocument10 pagesChronic Inflammation in Fat Plays A Crucial Role in The Development of Obesity-Related Insulin ResistanceRachel Lalaine Marie SialanaNo ratings yet
- Neonatal Hyperbilirubinemia and Elevated Liver Enzymes Associated With Thyroid Hormone Deficiency in NeonatesDocument4 pagesNeonatal Hyperbilirubinemia and Elevated Liver Enzymes Associated With Thyroid Hormone Deficiency in NeonatesOlfiany Laurenzia PongohNo ratings yet
- High-Fat Diet Induces Endothelial Dysfunction Through A Down-Regulation of The Endothelial AMPK-PI3K-Akt-eNOS PathwayDocument13 pagesHigh-Fat Diet Induces Endothelial Dysfunction Through A Down-Regulation of The Endothelial AMPK-PI3K-Akt-eNOS PathwayJorge CamargoNo ratings yet
- Fitoterapia: Jianfeng Xue, Wenjun Ding, Yan LiuDocument5 pagesFitoterapia: Jianfeng Xue, Wenjun Ding, Yan LiuAamir SohailNo ratings yet
- Fitoterapia: Jianfeng Xue, Wenjun Ding, Yan LiuDocument5 pagesFitoterapia: Jianfeng Xue, Wenjun Ding, Yan LiuAamir SohailNo ratings yet
- 2014 Article 9408Document10 pages2014 Article 9408kasabeNo ratings yet
- Nesca2013 Article IdentificationOfParticularGrou PDFDocument10 pagesNesca2013 Article IdentificationOfParticularGrou PDFBelen GaleraNo ratings yet
- Onion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsDocument8 pagesOnion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsRizky Agustian HadiNo ratings yet
- Effect of Wakame On Non Alcoholic Fatty LiverDocument14 pagesEffect of Wakame On Non Alcoholic Fatty LiverCătălina RădulescuNo ratings yet
- The Central Sirtuin 1/p53 Pathway Is Essential For The Orexigenic Action of GhrelinDocument9 pagesThe Central Sirtuin 1/p53 Pathway Is Essential For The Orexigenic Action of GhrelinJulia SCNo ratings yet
- Vaccines v11 I03 - 20230622Document98 pagesVaccines v11 I03 - 20230622Editor IJDMNo ratings yet
- Am J Clin Nutr 2012 Theytaz 1008 16Document9 pagesAm J Clin Nutr 2012 Theytaz 1008 16evaNo ratings yet
- Liraglutide Improves Non-Alcoholic Fatty Liver Disease in Diabetic Mice by Modulating in Ammatory Signaling PathwaysDocument10 pagesLiraglutide Improves Non-Alcoholic Fatty Liver Disease in Diabetic Mice by Modulating in Ammatory Signaling PathwaysAndreea Claudia NegrilaNo ratings yet
- Patel 2020Document31 pagesPatel 2020larissa brandaliseNo ratings yet
- Improvement in Glycemia After Glucose or Insulin Overload in Leptin-Infused Rats Is Associated With Insulin-Related Activation of Hepatic Glucose MetabolismDocument6 pagesImprovement in Glycemia After Glucose or Insulin Overload in Leptin-Infused Rats Is Associated With Insulin-Related Activation of Hepatic Glucose MetabolismDaniel Gomez GalindoNo ratings yet
- Hepatology - 2018 - Li - mTOR Signaling in X A Like Cells Contributes To Lipid Homeostasis in MiceDocument16 pagesHepatology - 2018 - Li - mTOR Signaling in X A Like Cells Contributes To Lipid Homeostasis in MiceTiange FengNo ratings yet
- Waterman Et Al-2015-Molecular Nutrition & Food ResearchDocument12 pagesWaterman Et Al-2015-Molecular Nutrition & Food ResearchIqra RubabNo ratings yet
- DownloadDocument11 pagesDownloadadri90No ratings yet
- Sugary Kefir Strain Lactobacillus Mali APS1 Ameliorated Hepatic Steatosis by Regulation of SIRT-1 NR-2 and Gut Microbiota in RatsDocument24 pagesSugary Kefir Strain Lactobacillus Mali APS1 Ameliorated Hepatic Steatosis by Regulation of SIRT-1 NR-2 and Gut Microbiota in RatsCristina OliveiraNo ratings yet
- Delgado Et Al 2009Document8 pagesDelgado Et Al 2009tcardosodelgadoNo ratings yet
- Dietary L-Arginine Supplementation Reduces Methotrexate Induced Intestinal Mucosal Injury in RatDocument9 pagesDietary L-Arginine Supplementation Reduces Methotrexate Induced Intestinal Mucosal Injury in RatMohamed IsmailNo ratings yet
- Artificially Cultivated Ophiocordyceps Sinensis AlleviatesDocument17 pagesArtificially Cultivated Ophiocordyceps Sinensis AlleviatesHoang IceNo ratings yet
- s12010 023 04399 9 PDFDocument14 pagess12010 023 04399 9 PDFVengateshwaran TDNo ratings yet
- Dr. Blanco ArticleDocument11 pagesDr. Blanco ArticleCarlosNo ratings yet
- Efecto Hipotalamico Lira2016-ObesityDocument8 pagesEfecto Hipotalamico Lira2016-ObesitylucilaNo ratings yet
- Boss Ola 2009Document8 pagesBoss Ola 2009nettoxsNo ratings yet
- Glikogen 6Document12 pagesGlikogen 6DZoel FAcHMyNo ratings yet
- Research Article: The Extract of Herbal Medicines Activates AMP-Activated Protein Kinase in Diet-Induced Obese RatsDocument9 pagesResearch Article: The Extract of Herbal Medicines Activates AMP-Activated Protein Kinase in Diet-Induced Obese RatsJoshNo ratings yet
- Julia Nur Faridha SDocument9 pagesJulia Nur Faridha SJulia Nur Faridha SeptyaniNo ratings yet
- J. Nutr.-2004-Wang-1032-8Document7 pagesJ. Nutr.-2004-Wang-1032-8Daniel Lee Eisenberg JacobsNo ratings yet
- Hyperlipidemic Effects of Dietary Saturated Fats Mediated Through PGC-1Document13 pagesHyperlipidemic Effects of Dietary Saturated Fats Mediated Through PGC-1Ilya BerahaNo ratings yet
- 2-Heremans-Schmid Glycoprotein: Fetuin-A Is Associated With Insulin Resistance and Fat Accumulation in The Liver in HumansDocument5 pages2-Heremans-Schmid Glycoprotein: Fetuin-A Is Associated With Insulin Resistance and Fat Accumulation in The Liver in HumansOcto IndradjajaNo ratings yet
- Transcriptomic and Proteomic Analysis of Potential Therapeutic Target Genes in The Liver of Metformin Treated Sprague Dawley Rats With Type 2 Diabetes Mellitusijmm-41!06!3327Document15 pagesTranscriptomic and Proteomic Analysis of Potential Therapeutic Target Genes in The Liver of Metformin Treated Sprague Dawley Rats With Type 2 Diabetes Mellitusijmm-41!06!3327ErickNo ratings yet
- Sirtori2012 Efectos de La Proteína de Altramuz y Arveja en Individuos Con Hipertensión LeveDocument8 pagesSirtori2012 Efectos de La Proteína de Altramuz y Arveja en Individuos Con Hipertensión Leveconsuelo aguilarNo ratings yet
- 1 s2.0 S2212877821001113 MainDocument7 pages1 s2.0 S2212877821001113 MainMonaNo ratings yet
- Retinoid X Receptor Agonists Have Anti-Obesity Effects and Improve Insulin Sensitivity in Zucker Fa Fa RatsDocument8 pagesRetinoid X Receptor Agonists Have Anti-Obesity Effects and Improve Insulin Sensitivity in Zucker Fa Fa RatsKurnia Fitri AprillianaNo ratings yet
- Lept in 012Document7 pagesLept in 012Carolina De Lima FerreiraNo ratings yet
- Karatsoreos Et Al 2010Document11 pagesKaratsoreos Et Al 2010zacharymweil100% (1)
- (03241750 - Acta Medica Bulgarica) The Heparanase Inhibitor (Sulodexide) Decreases Urine Glycosaminoglycan Excretion and Mitigates Functional and Histological Renal Damages in Diabetic RatsDocument6 pages(03241750 - Acta Medica Bulgarica) The Heparanase Inhibitor (Sulodexide) Decreases Urine Glycosaminoglycan Excretion and Mitigates Functional and Histological Renal Damages in Diabetic RatsTeodorNo ratings yet
- Metabolic Changes in Serum Metabolome in Response To A MealDocument11 pagesMetabolic Changes in Serum Metabolome in Response To A MealmarcusmattosantosNo ratings yet
- Obesity Is Associated With Macrophage Accumulation in Adipose TissueDocument13 pagesObesity Is Associated With Macrophage Accumulation in Adipose TissueRachel Lalaine Marie SialanaNo ratings yet
- Adherens and Tight Junctions: Structure, Function and Connections To The Actin CytoskeletonDocument10 pagesAdherens and Tight Junctions: Structure, Function and Connections To The Actin Cytoskeletonanirbanmanna88320No ratings yet
- Janeway's Immunobiology: Seventh EditionDocument12 pagesJaneway's Immunobiology: Seventh Editionanirbanmanna88320No ratings yet
- Journal of Investigative Dermatology (2007) 127, 2525-2532: Doi:10.1038/sj - Jid.5700865Document1 pageJournal of Investigative Dermatology (2007) 127, 2525-2532: Doi:10.1038/sj - Jid.5700865anirbanmanna88320No ratings yet
- Result of Online Entrance Examination 2015 of M.Sc. Life ScienceDocument2 pagesResult of Online Entrance Examination 2015 of M.Sc. Life Scienceanirbanmanna88320No ratings yet
- Acid Dissociation ConstantDocument15 pagesAcid Dissociation Constantanirbanmanna88320No ratings yet
- Course: MSC BT Semester: Iii Subject Code: MBT 305 Subject Name: Computational Biology Unit Number: 1 Unit Title: Introduction To BioinformaticsDocument19 pagesCourse: MSC BT Semester: Iii Subject Code: MBT 305 Subject Name: Computational Biology Unit Number: 1 Unit Title: Introduction To Bioinformaticsanirbanmanna88320No ratings yet
- South Asian University: Admission FormDocument3 pagesSouth Asian University: Admission Formanirbanmanna88320No ratings yet
- BiopsyDocument4 pagesBiopsyanirbanmanna88320No ratings yet
- 3 Clinical significance: Interleukin-1 beta (IL-1β) also known as catabolin, isDocument4 pages3 Clinical significance: Interleukin-1 beta (IL-1β) also known as catabolin, isanirbanmanna88320No ratings yet
- CRISPRDocument15 pagesCRISPRanirbanmanna88320No ratings yet
- 1 Types: 2.3 Diagnostic RelevanceDocument3 pages1 Types: 2.3 Diagnostic Relevanceanirbanmanna88320No ratings yet
- Babasaheb Bhimrao Ambedkar University: (A Central University) LucknowDocument16 pagesBabasaheb Bhimrao Ambedkar University: (A Central University) Lucknowanirbanmanna88320No ratings yet
- Schedule For Online Entrence Examination-2015-2016: S.No. Course Code Date Shift TimingDocument3 pagesSchedule For Online Entrence Examination-2015-2016: S.No. Course Code Date Shift Timinganirbanmanna88320No ratings yet
- Structure, Activation and Biology of CalpainDocument7 pagesStructure, Activation and Biology of Calpainanirbanmanna88320No ratings yet
- Soal Review B. Inggris - XIIDocument11 pagesSoal Review B. Inggris - XIIKhairul IkhwanNo ratings yet
- Narrative Paragraphs Part 2Document14 pagesNarrative Paragraphs Part 2hyfsh hdgdysgNo ratings yet
- Sir Thomas WyattDocument6 pagesSir Thomas WyattAAMIR FAROOQNo ratings yet
- Penguin Kids TextsDocument4 pagesPenguin Kids TextsAwanabellaNo ratings yet
- RDO No. 80 - Mandaue City, CebuDocument1,113 pagesRDO No. 80 - Mandaue City, CebuArnold DrilonNo ratings yet
- Solved Paper 2020Document13 pagesSolved Paper 2020anuragak2346No ratings yet
- Hungarian SelftaughtDocument136 pagesHungarian Selftaughtbearinghu100% (11)
- Chapter 1-7Document45 pagesChapter 1-7caironsalamNo ratings yet
- Terlaris Shopee Desember 2021Document1,084 pagesTerlaris Shopee Desember 2021Soni ChanNo ratings yet
- Halen Dinata Atmaja - 10511910000003 - Quiz NotetakingDocument8 pagesHalen Dinata Atmaja - 10511910000003 - Quiz NotetakingAndika Surya HadiwinataNo ratings yet
- Chemistry Project CBSEDocument23 pagesChemistry Project CBSEH0% (2)
- A Sample Indian Grocery Store Business Plan TemplateDocument17 pagesA Sample Indian Grocery Store Business Plan Templatekinley dorjee0% (1)
- White Fang PRL2Document9 pagesWhite Fang PRL2Mercedes ManavellaNo ratings yet
- The Noun Plural: 1. Substantive NUMARABILEDocument4 pagesThe Noun Plural: 1. Substantive NUMARABILEDia DiduNo ratings yet
- Slides Curso de Inglés Básico A1 Fechas, Horas y Expresiones SimplesDocument95 pagesSlides Curso de Inglés Básico A1 Fechas, Horas y Expresiones SimplesAndres CordobaNo ratings yet
- Saikumar Lingam ResumeDocument4 pagesSaikumar Lingam ResumesaikumarNo ratings yet
- Dil Sinifi Ingilizce Sinav Kelime Calisma ListesiDocument42 pagesDil Sinifi Ingilizce Sinav Kelime Calisma ListesimnazNo ratings yet
- UntitledDocument42 pagesUntitledaufcheNo ratings yet
- How To Prevent Poop From Sticking To The Toilet Bowl?: Why Does My Poop Stick So Bad?Document3 pagesHow To Prevent Poop From Sticking To The Toilet Bowl?: Why Does My Poop Stick So Bad?Jerry GZavaletaNo ratings yet
- Gourmand Awards General Presentation 2014Document14 pagesGourmand Awards General Presentation 2014SA BooksNo ratings yet
- Jayden Cano - Analogies-1Document14 pagesJayden Cano - Analogies-1JAYDEN CANONo ratings yet
- Commissioning and Qualification ASTM ApproachDocument0 pagesCommissioning and Qualification ASTM Approachvenki_beeNo ratings yet
- Drug ExpiryDocument3 pagesDrug Expiryhap hazardNo ratings yet
- The Apex Predator DietDocument73 pagesThe Apex Predator Dietdeclanku100% (2)
- Ohi Case Study Powerpoint Presentation 220a - Savanna BeddoesDocument18 pagesOhi Case Study Powerpoint Presentation 220a - Savanna Beddoesapi-307780636No ratings yet
- PART 1 - SET 9. Describe A Cultural Event That You Are Interested inDocument2 pagesPART 1 - SET 9. Describe A Cultural Event That You Are Interested inboy cuteNo ratings yet
- RFD 2011 12 Crop Science DivisionDocument12 pagesRFD 2011 12 Crop Science DivisionXeenNo ratings yet
- Environmental Science and Engineering Course File and Lesson Plan by GopinathDocument64 pagesEnvironmental Science and Engineering Course File and Lesson Plan by Gopinathbajjugopi166575% (4)
- Bulletin 12 16 11Document3 pagesBulletin 12 16 11Michael AllenNo ratings yet
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainFrom EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainRating: 3.5 out of 5 stars3.5/5 (38)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 4.5 out of 5 stars4.5/5 (4)
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarFrom EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarRating: 5 out of 5 stars5/5 (352)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsFrom EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsRating: 4 out of 5 stars4/5 (49)
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingFrom EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingRating: 4 out of 5 stars4/5 (3)
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthFrom EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthRating: 4 out of 5 stars4/5 (6)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomFrom EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomRating: 4 out of 5 stars4/5 (1)
- The End of Craving: Recovering the Lost Wisdom of Eating WellFrom EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellRating: 4.5 out of 5 stars4.5/5 (82)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyFrom EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyNo ratings yet
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthFrom EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNo ratings yet
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- Hungry for Change: Ditch the Diets, Conquer the Cravings, and Eat Your Way to Lifelong HealthFrom EverandHungry for Change: Ditch the Diets, Conquer the Cravings, and Eat Your Way to Lifelong HealthRating: 4 out of 5 stars4/5 (7)
- Rapid Weight Loss Hypnosis: Deep Sleep Your Way to Rapid Weight Loss, Healing Your Body and Self Esteem with Guided Meditations and Positive AffirmationsFrom EverandRapid Weight Loss Hypnosis: Deep Sleep Your Way to Rapid Weight Loss, Healing Your Body and Self Esteem with Guided Meditations and Positive AffirmationsRating: 5 out of 5 stars5/5 (7)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeFrom EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeRating: 5 out of 5 stars5/5 (1)
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingFrom EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingRating: 5 out of 5 stars5/5 (61)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouFrom EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNo ratings yet
- The Whole Body Reset: Your Weight-Loss Plan for a Flat Belly, Optimum Health & a Body You'll Love at Midlife and BeyondFrom EverandThe Whole Body Reset: Your Weight-Loss Plan for a Flat Belly, Optimum Health & a Body You'll Love at Midlife and BeyondRating: 4.5 out of 5 stars4.5/5 (28)
- Keto Friendly Recipes: Easy Keto For Busy PeopleFrom EverandKeto Friendly Recipes: Easy Keto For Busy PeopleRating: 3.5 out of 5 stars3.5/5 (2)
- Good Sugar Bad Sugar: Eat yourself free from sugar and carb addictionFrom EverandGood Sugar Bad Sugar: Eat yourself free from sugar and carb addictionRating: 4.5 out of 5 stars4.5/5 (29)
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (2)