Professional Documents
Culture Documents
Brain Death Testing Protocol (Rev220605) PDF
Uploaded by
Rei IrincoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Brain Death Testing Protocol (Rev220605) PDF
Uploaded by
Rei IrincoCopyright:
Available Formats
TTSH Brain Death Testing Guide
We understand that you do not perform brain death certification on a regular basis and may not recall the details of each test
offhand. We have therefore compiled these concise guidelines to the 7 tests you will need to perform. On the reverse side are
additional explanatory notes on each test that you may refer to should you require additional information.
First, ensure that these pre-conditions have been met before performing the 7 brainstem tests:
a) Have an identifiable, irreversible structural cause for brain death present (CT or MRI evidence)
b) Exclude other reversible causes of CNS depression
i)
Drugs (narcotics, barbiturates, benzodiazepines, tricyclic antidepressants, phenothiazines, lithium, ethanol)
ii) Hypotension (SBP <90 mmHg); Hypoxia (PaO2 <60 mmHg)
iii) Hypothermia (>35C); endocrine causes (e.g. hypothyroidism)
iv) Severe electrolyte and/or acid base disorders; hypoglycemia
c) Ensure absence or reversal of neuromuscular blockade
1.
Absent pain response
Apply firm pressure with thumb over the supraorbital notch and observe for response in face or extremities.
Apply sternal rub or pressure to the nail beds of all 4 extremities.
There should be no limb movements or facial grimaces elicited
2.
Absent pupillary response to light stimulation
Check that no anti-cholinergic drugs or eyedrops have been administered recently.
Shine a bright light into each eye and observe for a pupillary light response
There should be no constrictive pupillary response in both eyes.
3.
Absent corneal reflex
Elevate the eyelid and touch the cornea with a wisp of cotton wool.
If no response is elicited, repeat test by applying firm pressure with a moistened cotton bud, taking care to
avoid traumatizing the cornea.
There should be no muscle contractions elicited around the eyes (from the orbicularis oculi).
4.
Absent oculo-cephalic reflex (Dolls eye reflex)
This test is contra-indicated if the cervical spine has not been cleared.
Stand at the head end and grasp the sides of patients head firmly with both hands and hold the eyelids
open with both thumbs. Turn the head quickly 90 degrees to the left and to the right and observe for
movements of the eyes
The eye should not move with head turning but remain fixed in the midline, turning with the head.
5.
Absent gag and cough reflex
Using one spatula to depress the tongue, apply firm pressure to the posterior pharyngeal wall with a
second wooden spatula.
Insert a suction catheter all the way down the endotracheal tube to stimulate the trachea
There should be no gagging or coughing elicited.
6.
Absent oculo-vestibular reflex (caloric test)
Inspect both external ear canals with an otoscope to ensure intact tympanic membranes and rule out
obstruction with blood or other debris. Perforation of the TM is not a contraindication to caloric testing.
Elevate the head of bed to 30. Have an assistant elevate both eyelids. Using a black suction catheter and
50 ml syringe, inject 50 ml of ice-cold water slowly (over 15-30s) into the ear. Look for tonic deviation of the
pupil towards the ear being irrigated. Observe for at least 1 minute.
Wait 5 min and repeat test on the other ear.
There should be no eye movements noted.
7.
Apnoea test
Pre-oxygenate the patient with 100% oxygen for 10-20 minutes before commencing the test.
Check an arterial blood gas (ABG) to determine the baseline PaCO2 (should be around 35-40 mmHg).
Monitor ECG, BP, and SpO2 and ensure that systolic BP >90 mmHg and SpO2 >90% throughout the test. If
SBP <90 mmHg or SpO2 <90% or severe arrhythmias develop, take an ABG and reconnect to ventilator.
Insufflate oxygen at 6 L/min via white or green suction catheter after disconnecting from the ventilator.
Take care to avoid passing the catheter too far in (endobronchial position).
Disconnect from the ventilator and observe for respiratory efforts from the patient. Observe for 5-8 min and
check an ABG before reconnecting the patient to the ventilator.
There should be no respiratory movements seen at a PaCO2 > 50 mmHg or a rise of >20 mmHg
over the baseline) .
If the target PaCO2 has not been reached, repeat the test (after pre-oxygenation and restoration of
normocapnia) and lengthen the apnoeic interval to 10 minutes.
If any of the 7 brainstem tests cannot be completed and those completed are consistent with brain death,
supplementary tests (cerebral angiogram or radionuclide scan) may be performed to confirm brain death.
Compiled by Dr Chin Ki Jinn, Registrar, Dept of Anaesthesiology
Dr Kwek Tong Kiat, Director, Neurosurgical ICU and
Dr Chua Hoe Chin, Senior Consultant, Dept of Neurology, NNI
Version: 220605
TTSH Brain Death Testing Guide
Explanatory notes on brain death testing
Pain response
Pain should be applied to a number of sites, including supraorbital nerve, sternum and fingers . It is important to apply pain
to and look for responses in the cranial nerve distribution.
Spontaneous movements of the limbs from spinal mechanisms (spinal reflexes) can occasionally occur, especially in
younger patients. These often occur during apnoea testing, in response to hypoxia, respiratory acidosis, or hypotension,
rather than during application of painful stimuli. These reflexes include; rapid flexion in arms, raising of all limbs off the bed,
grasping movements, spontaneous jerking of one leg, walking-like movements, and movements of the arms up to the point
2
of reaching the ETT .
Pupillary response
Oculo-cephalic (Dolls eye) reflex
Testing is done only when no fracture or instability of the cervical spine is present .
The normal response is eye deviation to the side opposite to that of head turning.
Gag and cough reflex
It is not necessary for pupils to be fully dilated; however they should not be constricted . In brain dead patients, they are
2
usually moderately dilated (4-6mm) .
2
Round, oval or irregularly shaped pupils are compatible with brain death .
2
Pre-existing anatomic abnormalities of the iris or effects of previous surgery should be excluded .
Both reflexes must be tested. The gag reflex may be difficult to interpret in orally intubated patients .
Tugging on the ETT or tracheostomy tube is not an adequate stimulus for testing the cough reflex.
Oculo-vestibular reflex (caloric test)
The purpose of otoscopy is to look for obstruction of the ear canal by clotted blood or earwax, and presence of acute injury or
disease in the middle ear, which may render the test unreliable. Gentle attempts to irrigate or clear the canal of debris may
be attempted; referral to an ENT specialist may be required.
4
In chronic perforations of the tympanic membrane, cold air has been suggested as an alternative stimulus to water .
4
Base of skull fractures resulting in blood, CSF or brain tissue in the external auditory canal is a contraindication to the test .
Supplementary testing is indicated in this case.
4
Elevation of the head to 30 ensures that the lateral semi-circular canals are vertical, maximizing the response .
1
Local guidelines suggest that the eyes be observed for up to 3 minutes after injection ; AAN and other guidelines
2,4
recommend 1 minute and waiting at least 5 minutes before testing the other side .
Apnoea testing
AAN guidelines suggest the following pre-requisites to minimize the risk of deterioration in vital signs (hypoxia, hypotension,
arrhythmias) during testing. These are a) core temperature 36.5; b) systolic BP 90 mmHg; c) euvolemia or positive
balance in previous 6 hours; d) normocapnia or PaCO2 40 mmHg; e) normoxemia or PaO2 200 mmHg.
Insufflation of oxygenation and preoxygenation help to prevent hypoxemia during the apnoeic period. Preoxygenation with
4
100% O2 for 10-30 minutes has been suggested . Using flow rates in excess of 6 L/min during the test may result in partial
4
clearance of CO2 and hence invalidate the test .
The catheter should be secured at the appropriate depth to avoid endobronchial placement. It should also be narrow enough
to allow expiratory flow around it, or else air trapping may occur leaking to hypotension and pneumothorax.
2
Respiration is defined as abdominal or chest excursions that produce adequate tidal volumes .
Respiratory-like movements can occur (agonal breathing patterns), characterized by shoulder elevation and adduction, back
arching, and intercostals expansion without generating significant tidal lung volumes. Spinal reflexes may also be seen.
2
These movements are compatible with the presence of brain death .
There is no firm evidence on the upper limit of PaCO2 required for maximal stimulation of the respiratory centre. Local and
1,3
2,4
UK guidelines target a PaCO2 of >50 mmHg . Most other guidelines adopt a higher threshold of 60 mmHg . Others have
2
4
suggested using an increase of 20 mmHg over baseline PaCO2 or an arterial pH of < 7.30 .
1
Local guidelines recommend an apnoeic interval of 5 minutes. PaCO2 rises by 2.5 mmHg/minute on average. AAN
2
guidelines recommend an apnoeic interval of 8-10 minutes.
If the test has to be aborted prematurely because of cardiovascular instability or desaturation, and the PaCO2 has not
reached the target level, this is an indeterminate result, and supplementary testing is indicated to confirm the diagnosis of
brain death.
References
1. Manual on Organ Donation and Transplantation. Ministry of Health, Singapore. Feb 2005.
2. Determining brain death in adults. EFM Wijdicks. Neurology 1995;45:1003-1011. (expanded version of the American
Academy of Neurologys practice parameters for determining brain death in adults)
3. A code of practice for the diagnosis of brain death. Working Party of the Royal Colleges, UK. March 1998.
4. Clinical confirmation of brain death. Dobb GJ, Weekes JW. Anaesthesia and Intensive Care 1995;23:37-43. (represents the
Australian and New Zealand Intensive Care Societys guidelines on certification of brain death)
Compiled by Dr Chin Ki Jinn, Registrar, Dept of Anaesthesiology
Dr Kwek Tong Kiat, Director, Neurosurgical ICU and
Dr Chua Hoe Chin, Senior Consultant, Dept of Neurology, NNI
Version: 220605
You might also like
- Ataxia 10Document19 pagesAtaxia 10Cristina GhizdavetNo ratings yet
- Major Haemorrhage ProtocolsDocument3 pagesMajor Haemorrhage ProtocolsleicesterbugNo ratings yet
- IsometricsDocument3 pagesIsometricsgtlaau100% (1)
- Cerebrovascular AccidentDocument62 pagesCerebrovascular AccidentJaydee DalayNo ratings yet
- Management of Status Asthmatic Us in ChildrenDocument7 pagesManagement of Status Asthmatic Us in Childrenjshq1971No ratings yet
- The Nurses and Midwives Act No. 10 of 2019. PMDDocument43 pagesThe Nurses and Midwives Act No. 10 of 2019. PMDhfcvbNo ratings yet
- Acute Severe AsthmaDocument5 pagesAcute Severe AsthmaRizsa Aulia DanestyNo ratings yet
- ACLS Suspected Stroke AlgorithmDocument8 pagesACLS Suspected Stroke AlgorithmBirhane GebreegziabiherNo ratings yet
- Valvular Heart DiseaseDocument27 pagesValvular Heart DiseaseOwen J. WieseNo ratings yet
- ICU TriageDocument27 pagesICU TriageAkmal FahrezzyNo ratings yet
- Management of Emergencies in ChildrenDocument39 pagesManagement of Emergencies in ChildrensastroboyzNo ratings yet
- ABC Acute Renal FailureDocument5 pagesABC Acute Renal FailureAngela CristinoNo ratings yet
- Neonatal Seizure 1Document5 pagesNeonatal Seizure 1Rayhanun MardhatillahNo ratings yet
- Critical Care Nurses Association of The PhilippinesDocument2 pagesCritical Care Nurses Association of The Philippinesnurseharebee100% (2)
- Posterior Cranial Fossa Anesthetic ManagementDocument48 pagesPosterior Cranial Fossa Anesthetic ManagementDivya Rekha KolliNo ratings yet
- 2022 Mart YÖKDİL YÖKDİL - Fen BilimleriDocument17 pages2022 Mart YÖKDİL YÖKDİL - Fen BilimleriErdal Bozkurt100% (2)
- Cerebrovascular Accident (CVA)Document71 pagesCerebrovascular Accident (CVA)nur muizzah afifah hussinNo ratings yet
- PharmacyDocument27 pagesPharmacyJenilNo ratings yet
- Cerebrovascular Accident (Stroke)Document15 pagesCerebrovascular Accident (Stroke)mesdejen100% (1)
- ECHMODocument52 pagesECHMOanupama varghese100% (1)
- Top 10 Care Essentials in Ventilated PtsDocument3 pagesTop 10 Care Essentials in Ventilated PtsAdel HamadaNo ratings yet
- BiotechnologyDocument39 pagesBiotechnologyChrystal Kyla SalengaNo ratings yet
- Fundamentals of Nursing Test IIIDocument15 pagesFundamentals of Nursing Test IIIRose AnnNo ratings yet
- Cerebrovascular Disorders: PathophysiologyDocument4 pagesCerebrovascular Disorders: PathophysiologyMhae De GuzmanNo ratings yet
- Main Stroke Protocol - Use For All Suspected Stroke-TIA PatientsDocument2 pagesMain Stroke Protocol - Use For All Suspected Stroke-TIA PatientsRivulet1No ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Hydrocephalus: Mr. Fadi J. Zaben RN MSN IMET2000, Ramallah February, 2013Document30 pagesHydrocephalus: Mr. Fadi J. Zaben RN MSN IMET2000, Ramallah February, 2013WisnuBaskoro100% (1)
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Case Presentation 1Document70 pagesCase Presentation 1shadow gonzalezNo ratings yet
- Assessment of bleeding Shock in a Politraumatized PatientFrom EverandAssessment of bleeding Shock in a Politraumatized PatientNo ratings yet
- Cerebrovascular AccidentDocument79 pagesCerebrovascular AccidentKathy B. AbuanNo ratings yet
- Hygienic Design Food IndustryDocument19 pagesHygienic Design Food IndustryLinaArev H100% (1)
- Selective, Differential, & Enriched Media Lab ChartDocument2 pagesSelective, Differential, & Enriched Media Lab ChartFrankiesgirl6yr100% (6)
- Spinal TuberculosisDocument46 pagesSpinal TuberculosisAbby Austero100% (1)
- Management of Cerebral Edema, Brain Compression,.4Document29 pagesManagement of Cerebral Edema, Brain Compression,.4Jorge MontenegroNo ratings yet
- Field Visit PresentationDocument33 pagesField Visit PresentationNib IndranilNo ratings yet
- Brain Death Role of Intensivist in Diagnosis and Preparation For Organ RetrievalDocument86 pagesBrain Death Role of Intensivist in Diagnosis and Preparation For Organ Retrievalharsha mummaka100% (1)
- Subarachnoid Hemorrhage in The Emergency DepartmentDocument8 pagesSubarachnoid Hemorrhage in The Emergency DepartmentLuis octavio carranzaNo ratings yet
- Subarachnoid HemorrhageDocument3 pagesSubarachnoid Hemorrhagetenaj_purpleNo ratings yet
- Status AsthmaticusDocument29 pagesStatus AsthmaticusDavid OlsonNo ratings yet
- Seizures in The Preterm NeonateDocument10 pagesSeizures in The Preterm NeonateRoosevelt Santibañez Dla TorreNo ratings yet
- 01-Guidelines For Use of Hypertonic SalineDocument13 pages01-Guidelines For Use of Hypertonic SalineSatish VeerlaNo ratings yet
- Critical Care Nephrology Core Curriculum 2019Document34 pagesCritical Care Nephrology Core Curriculum 2019Edmilson R. LimaNo ratings yet
- A Neonate With Acute Kidney Injury: Case PresentationDocument4 pagesA Neonate With Acute Kidney Injury: Case PresentationSahil DhamijaNo ratings yet
- Aneurysmal Subarachnoid Hemorrhage.6Document19 pagesAneurysmal Subarachnoid Hemorrhage.6Aldy Setiawan PutraNo ratings yet
- Stable and Unstable AnginaDocument19 pagesStable and Unstable AnginaAli B. SafadiNo ratings yet
- How Stroke Affects Speech and LanguageDocument5 pagesHow Stroke Affects Speech and Languagemino songNo ratings yet
- Status Asthmaticus!!!!!! PDFDocument13 pagesStatus Asthmaticus!!!!!! PDFKassandra Mildred GutierrezNo ratings yet
- Cardiogenic ShockDocument18 pagesCardiogenic ShockBagus Andi PramonoNo ratings yet
- Head Trauma: Yoon Seung-Hwan, M.DDocument53 pagesHead Trauma: Yoon Seung-Hwan, M.DAhmed ZahranNo ratings yet
- Critical Care - Improving OutcomesDocument81 pagesCritical Care - Improving OutcomeshimanshuNo ratings yet
- Treatment of Acute Ischemic StrokeDocument22 pagesTreatment of Acute Ischemic StrokeByron Coello ViñánNo ratings yet
- Acute Ischemic Stroke UpdateDocument38 pagesAcute Ischemic Stroke Updatenarendra wahyuNo ratings yet
- Status EpilepticusDocument70 pagesStatus Epilepticusfloppyfishh100% (1)
- Use of Vasopressors and InotropesDocument14 pagesUse of Vasopressors and InotropesEdwin VargasNo ratings yet
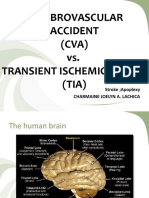
- Cerebrovascular Accident (CVA) vs. Transient Ischemic Attack (TIA)Document37 pagesCerebrovascular Accident (CVA) vs. Transient Ischemic Attack (TIA)Grace IgnacoNo ratings yet
- Postoperative Cognitive Dysfunction Preoperative Risk Assessment and Perioperative Risk Minimization A Pragmatic Review of The LitDocument5 pagesPostoperative Cognitive Dysfunction Preoperative Risk Assessment and Perioperative Risk Minimization A Pragmatic Review of The Litade_liaNo ratings yet
- Hemorrhagic StrokeDocument57 pagesHemorrhagic StrokeAnonymous oEbVOENo ratings yet
- Overview of The Management of Acute Kidney Injury in Adults - UpToDateDocument13 pagesOverview of The Management of Acute Kidney Injury in Adults - UpToDateDaniely FreitasNo ratings yet
- ICU Triage (Edit)Document22 pagesICU Triage (Edit)FatyahNo ratings yet
- Hypertonic Saline and Mannitol Therapy in Critical Care NeurologyDocument9 pagesHypertonic Saline and Mannitol Therapy in Critical Care NeurologyRonAlNo ratings yet
- Spinal Cord Injuries: Gabriel C. Tender, MDDocument49 pagesSpinal Cord Injuries: Gabriel C. Tender, MDCathyCarltonNo ratings yet
- Anesthesia For GeriatricDocument21 pagesAnesthesia For GeriatricintanNo ratings yet
- JCI Booklet Final EditedDocument40 pagesJCI Booklet Final EditedRei IrincoNo ratings yet
- Schengen Visa Application: Photo StampDocument3 pagesSchengen Visa Application: Photo StampRei IrincoNo ratings yet
- BibliographyDocument1 pageBibliographyRei IrincoNo ratings yet
- Test I.Parts of Speech: Capitals Early Early Lively Lively SHE Them Those WHO This Whose YOU That WhichDocument5 pagesTest I.Parts of Speech: Capitals Early Early Lively Lively SHE Them Those WHO This Whose YOU That WhichRei IrincoNo ratings yet
- Arterial LinesDocument9 pagesArterial LinesRei IrincoNo ratings yet
- Top 10 Ranking Universities in West Africa 2022Document1 pageTop 10 Ranking Universities in West Africa 2022Bright OtchereNo ratings yet
- HRMDocument20 pagesHRMSyeda AleenaNo ratings yet
- Ufgs 01 57 19.01 20Document63 pagesUfgs 01 57 19.01 20jackcan501No ratings yet
- Matter For PGDIPC Course PromotionDocument1 pageMatter For PGDIPC Course PromotionAnkur VasudevaNo ratings yet
- RA-100722 CRIMINOLOGIST Palawan 12-2021Document55 pagesRA-100722 CRIMINOLOGIST Palawan 12-2021Robert V. AbrasaldoNo ratings yet
- LPV Fault Detection of Glucose-Insulin System: Cite This PaperDocument6 pagesLPV Fault Detection of Glucose-Insulin System: Cite This PaperfatihaNo ratings yet
- Free End SaddleDocument5 pagesFree End SaddleAdry AnnaNo ratings yet
- Philhealth Circular 013-2015Document12 pagesPhilhealth Circular 013-2015Kim Patrick DayosNo ratings yet
- NT90004212Document58 pagesNT90004212Jelena ĆukNo ratings yet
- Baby Led-WeaningDocument7 pagesBaby Led-WeaningsophieNo ratings yet
- 2011 Urine Therapy J of NephrolDocument3 pages2011 Urine Therapy J of NephrolCentaur ArcherNo ratings yet
- Nursing Process Patients With DiabetesDocument14 pagesNursing Process Patients With DiabetesJelly Jia100% (2)
- BrochureDocument6 pagesBrochureRahul ShettyNo ratings yet
- Osteoarthritis of The Hip and Knee Flowchart PDFDocument2 pagesOsteoarthritis of The Hip and Knee Flowchart PDFsilkofosNo ratings yet
- Project ProposalDocument3 pagesProject ProposalSkrrtt SkrrttNo ratings yet
- Darrells ResumeDocument5 pagesDarrells Resumeapi-273253154No ratings yet
- Project Proposal CFW Lean MonthsDocument2 pagesProject Proposal CFW Lean MonthskapeatbutasNo ratings yet
- Guide State Local Emergency Operations Plans (Cpg1 8 1)Document21 pagesGuide State Local Emergency Operations Plans (Cpg1 8 1)ebjlNo ratings yet
- 2018 Overview Digestive System HandoutDocument11 pages2018 Overview Digestive System HandoutdraganNo ratings yet
- Periodontal AbscessDocument27 pagesPeriodontal AbscessAhmed Tawfig GamalNo ratings yet
- Diastasis Recti Ebook DownloadDocument19 pagesDiastasis Recti Ebook DownloadMertcan DamatNo ratings yet
- Material Safety Data Sheet: AES-A-350-RBDocument7 pagesMaterial Safety Data Sheet: AES-A-350-RBSajidawan. OlineNo ratings yet
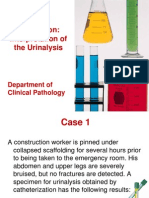
- Urine Case 2010-2Document9 pagesUrine Case 2010-2hendra_darmawan_4No ratings yet