Professional Documents
Culture Documents
AOSD - Rare Case
Uploaded by
Bogdan LupuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AOSD - Rare Case
Uploaded by
Bogdan LupuCopyright:
Available Formats
S H O RT C O M M U N I C AT I O N
JIACM 2004; 5(4): 327-30
A Rare Cause of Pyrexia of Unknown Origin:
Adult Onset Stills Disease
Atul Kakar*, Lalit Duggal*
Introduction
Adult onset Stills disease is a rare cause of pyrexia of
unknown origin in India. In various series adult onset Stills
disease is responsible for 5-9% patients of pyrexia of
unknown origin. Bywater first described this condition in
1971 with descriptions of 14 patients1 and since then small
series have been reported from India2-4. We report a series
of this multi-systemic inflammatory disorder which is
characterised by spiking fever, skin rash, arthralgia/
arthritis, and myalgia.
Material and methods
This study was done at Sir Ganga Ram Hospital, Delhi. All
patients who were admitted in medical wards with a
differential diagnosis of pyrexia of unknown origin were
considered for possible diagnosis of adult onset Stills
disease. The study period was July 2002 to Dec 2002.
All patients who satisfied Yamaguchi et al6 criteria were
diagnosed as adult onset Stills disease. The criteria are
tabulated in table I.
Table I : Criteria for diagnosis of adult onset Stills
disease (Yamaguchi et al6).
Major criteria
1. Fever of 39 C or higher, lasting one week or longer.
2. Arthralgias lasting two weeks or longer.
3. Typical rash.
4. Leukocytosis (10,000/mm3 or greater) including >
80% granulocytes.
Minor criteria
1. Sore throat.
2. Lymphadenopathy and /or splenomegaly.
3. Liver dysfunction.
4. Negative rheumatoid Factor and ANA.
Total of more than 5 criteria (including 2 major) were
required for diagnosis.
* The above criteria are applicable if other causes are excluded, since
this disease is relatively uncommon.
* Sensitivity 96.2%; Specificity 92.1%.
Observations
Complete blood counts, liver, and renal function test,
radiology of chest and hands was done in all patients.
Rheumatoid factor was tested by latex agglutination and
ANA by immunofluroscopy in all patients. Serum ferritin
was done in all patients. Bone marrow aspiration/biopsy
and lymph node biopsy was done if a case required so.
The onset of symptoms were acute or abrupt in all
patients. Eight patients were diagnosed as patients with
adult onset Stills disease out of 67 patients being referred
to department of Medicine for management of pyrexia
of unknown origin. The mean delay in diagnosis was 9
months (4-16 months).
The following were exclusion criteria for adult onset Stills
disease:
2. Patients less than 16 years of age.
The male to female ratio was 5:3. The age varied from 18
to 65 years with mean age of 26.2 years. All patients
presented with high grade fever. All patients had taken
course of antibiotics (> 2). Four patients were on antitubercular therapy. Two patients were being treated as
cases of rheumatic fever.
Clinical remission was defined as absence of articular or
laboratory evidence of disease activity for at least 2
consecutive months.
Three patients gave history of sore throat at onset of
illness. Rash was seen in 1 patient and was maculopapular
type seen over the neck and trunk. Lymph node
1. History of intake of steroids, hydroxychloroquine prior
to diagnosis.
* ImmnoRheumatology Clinic, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi-100 060.
enlargement was seen in 5/8 patients. Liver and spleen
enlargement was seen in 5 and 3 patients respectively.
Two patients had evidence of serositis.
Joint pains were seen in all patients. The details of joint
involvement were distal interphalangeal joint- 4/8,
proximal interphalangeal joint- 8/8, metacarpophalangeal
joint- 6/8, wrists- 4/8, elbow- 3/8, shoulder joint- 2/8, hip2/8, knee- 7/8, ankle- 5/8, feet- 4/8.
Common laboratory observations were leucocytosis,
normocytic normochromic anaemia, high ESR and ASO
and high serum ferritin levels. The findings are
enumerated in Table II. Rheumatoid factor and ANA were
negative in all patients. The X-rays of hand and feet
showed evidence of carpal/tarsal ankylosis in 1/8, no
erosions was seen in all the patients. Bone marrow
aspiration was reactive marrow in 5/8.
Table II : Shows selected laboratory test in adult onset
Stills disease.
Leucocytosis
Anaemia
High ESR
High ASO
High serum ferritin
Liver abnormalities
Lymph node biopsy
Pleural biopsy
Rheumatoid factor/ANA
Carpal/tarsal ankylosis
87.5%
87.5%
100%
50%
100%
37.5%
25%
12.5%
0%
12.5%
Seven patients required steroids due to persistent
synovitis. The break-up of the treatment was NSAIDs only
- 1/8, oral steroids with NSAIDS - 7/8, intra-muscular pulse
steroids - 2/8, DMARDS (methorexate, hydrochloroquine)
- 2/8, intra-articular steroids - 2/8, and combination of
NSAIDs, methotrexate, and steroids - 1/8.
All patients were followed-up for atleast 6 months, 3
patients required disease modifying anti-rheumatic agents.
Three patients were followed-up for a period of 11 months.
One patient shifted to alternative medication system. At 1
year he was seen again with relapse of symptoms. Serum
ferritin levels normalised in all patients by 4 weeks duration.
Discussion
Adult onset Stills disease remains a difficult clinical
diagnosis, largely because of its rarity, protean
328
manifestations, and lack of pathognomic features or
diagnostic tests. It resembles the systemic form of juvenile
rheumatoid arthritis. The adult onset syndrome is
common in age 16-35 years.
The aetiology of this disorder is not known. An increase in
frequency of HLA-35 has been found both in children and
adults with this disorder. Circadian cytokine may be
responsible for paroxysms of fever and other systemic
features. Majority of patients with systemic disease will
have self-limiting episodes of less than 1 year and fare
well once the disease is abated. Few patients have
recurrence with life threatening complications. Chronic
disease is most disabling and can lead to chronic arthritis.
Adult onset Stills disease is a mimic of tuberculosis as
patients continue to run temperature and have high ESR,
hepatosplenomegaly, lymphadenopathy in many patients.
In our series, 4 patients were on anti-tubercular treatment.
It was differentiated on the basis of leucocytosis, multiple
joint involvement, no response to anti-tubercular
treatment, and no evidence of tuberculosis on biopsy of
lymph node/pleura.
Rash was seen only in 1 patient; however, in Western
literature it is described very commonly. This could be due
to difficulty in detecting rash in Indian pigmented skin.
The involvement of DIP was seen in 4 patients and is a
notable feature of adult onset Stills disease. The
involvement of DIP is also a feature of psoriatic arthritis,
but this joint is commonly spared in inflammatory joint
diseases of young (rheumatoid arthritis, SLE, and acute
rheumatic fever).
The joint involvement was polyarticular and symmetrical
in majority of patients. The commonest joint involved in
our patient was proximal interphalangeal joints followed
by knee joint; however, knee and wrist have been reported
by others.
Hyperferritinaemia was seen in all patients of adult
onset Stills disease. Ferrtin is an acute phase reactant.
It has a diagnostic value of assessing adult onset Stills
disease and high ferritin levels are associated with high
spikes of fever. Ferritin levels show rapid response to
anti-inflammatory therapy as also seen in our series.
The cause of hyperferritinemia is thought to be
Journal, Indian Academy of Clinical Medicine
Vol. 5, No. 4
October-December, 2004
unrelated to iron metabolism and is likely to be a
consequence of cytokine-induced augmented
synthesis by reticulo-endothelial system or hepatocyte
damage resulting in increased release. Table III
compares clinical parameters in various series from
India.
Conclusions
Early diagnosis of adult onset Stills disease is possible if
treating physician is aware of the rare condition. Delay in
diagnosis is due to expensive investigations to exclude
occult infection or neoplasm. Value of hyperferritinaemia
Table III : Compares the important clinical parameters of adult onset Stills disease.
Features
Male : Female
Fever T > 39F
Rash
Arthralgia / Arthritis
Sore thorat
Lymphadenopathy
Splenomegaly
Hepatomegaly
Pleuritis / effusion
Present series (2004)
N=8
5:3
100%
12.5%
100%
37.5%
62.5%
32.5%
62.5%
12.5%
Uppal et al (1995)
N = 31
Bambery et al (1992)
N = 18
17:14
100%
36%
100%
39%
45%
58%
58%
7%
10:8
100%
50%
100%
67%
56%
56%
28%
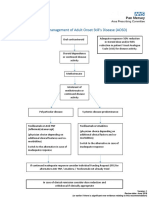
Fig. 1 : Bilateral ankle arthritis.
Journal, Indian Academy of Clinical Medicine
Vol. 5, No. 4
October-December, 2004
329
in northern India. Ann Rheum Dis 1992; 51: 529-32.
as important diagnostic tool cannot be over emphasised.
4.
Uppal SS, Pande LRA, Kumar A et al. Adult onset Still s in
northern India: comparison with juvenile onset Stills. Br J
Rheumatol 1995: 34: 429-34.
5.
Ohta A, Yamoguchti M, Kanooke H et al. Stills disease: review
of 228 cases from the literature. J Rheumatol 1987; 14: 113946.
6.
Yamaguchi M, Ohta A, Tsuenmatsu et al. Preliminary criteria
for classification of adult onset Stills disease. J Rheumatol
1992; 23: 712-9.
References
1.
Bywaters EGL. Still s disease in the adult. Ann Rheum Dis
1971; 30: 121-32.
2.
Singh VN, Adya CM, Kumar A, Malaviya AN. Adult onset
Still s in India. Br J Rheumatol 1992; 31: 417-9.
3.
Bamberry P, Thomas RS, Malhotre HS et al. Adult onset Still
s disease: clinical experience with 18 patients over 15 years
Flavedon AD
330
Journal, Indian Academy of Clinical Medicine
Vol. 5, No. 4
October-December, 2004
You might also like
- A Rare But Fascinating Disorder: Case Collection of Patients With Schnitzler SyndromeDocument5 pagesA Rare But Fascinating Disorder: Case Collection of Patients With Schnitzler SyndromeBogdan LupuNo ratings yet
- Free Job Hunt Guide v1.1 PDFDocument78 pagesFree Job Hunt Guide v1.1 PDFBogdan LupuNo ratings yet
- PUO-Clinicians Dilemma Clinical Profile of AOSDDocument3 pagesPUO-Clinicians Dilemma Clinical Profile of AOSDBogdan LupuNo ratings yet
- Ghid Instalare Decra Stratos EngDocument10 pagesGhid Instalare Decra Stratos EngBogdan LupuNo ratings yet
- Mojor 05 00192Document4 pagesMojor 05 00192Bogdan LupuNo ratings yet
- L3150 User's GuideDocument182 pagesL3150 User's GuideJitu SinghNo ratings yet
- Adult-Onset Stills Disease: Advocating For New Markers To Overcome The Diagnostic ChallengeDocument8 pagesAdult-Onset Stills Disease: Advocating For New Markers To Overcome The Diagnostic ChallengeBogdan LupuNo ratings yet
- AOSD Case ReportDocument5 pagesAOSD Case ReportBogdan LupuNo ratings yet
- AOSD Case ReportDocument4 pagesAOSD Case ReportBogdan LupuNo ratings yet
- AOSD - Juvenile Idiopathic ArthritisDocument14 pagesAOSD - Juvenile Idiopathic ArthritisBogdan LupuNo ratings yet
- Adult-Onset Stills Disease: Advocating For New Markers To Overcome The Diagnostic ChallengeDocument8 pagesAdult-Onset Stills Disease: Advocating For New Markers To Overcome The Diagnostic ChallengeBogdan LupuNo ratings yet
- 1 PBDocument5 pages1 PBBogdan LupuNo ratings yet
- AOSD - Juvenile Idiopathic ArthritisDocument14 pagesAOSD - Juvenile Idiopathic ArthritisBogdan LupuNo ratings yet
- AOSD Case ReportDocument8 pagesAOSD Case ReportBogdan LupuNo ratings yet
- The Diagnostic Challenge of Adult-Onset Still's DiseaseDocument4 pagesThe Diagnostic Challenge of Adult-Onset Still's DiseaseBogdan LupuNo ratings yet
- Adult-Onset Stills Disease: Advocating For New Markers To Overcome The Diagnostic ChallengeDocument8 pagesAdult-Onset Stills Disease: Advocating For New Markers To Overcome The Diagnostic ChallengeBogdan LupuNo ratings yet
- AOSD Case ReportDocument4 pagesAOSD Case ReportBogdan LupuNo ratings yet
- Mojor 05 00192Document4 pagesMojor 05 00192Bogdan LupuNo ratings yet
- (Journal of Cardiovascular Emergencies) Venous Thromboembolism Secondary To Adult-Onset Stills Disease A Case ReportDocument5 pages(Journal of Cardiovascular Emergencies) Venous Thromboembolism Secondary To Adult-Onset Stills Disease A Case ReportBogdan LupuNo ratings yet
- AOSD Case - International Journal of Research in DermatologyDocument6 pagesAOSD Case - International Journal of Research in DermatologyBogdan LupuNo ratings yet
- Adult Onset Still's Disease Associated With Mycoplasma Pneumoniae Infection and Hemophagocytic LymphohistiocytosisDocument5 pagesAdult Onset Still's Disease Associated With Mycoplasma Pneumoniae Infection and Hemophagocytic LymphohistiocytosisBogdan LupuNo ratings yet
- Uk Still PDFDocument5 pagesUk Still PDFBogdan LupuNo ratings yet
- Case Reports - Still A Serious HealthDocument6 pagesCase Reports - Still A Serious HealthBogdan LupuNo ratings yet
- AOSD Case ReportDocument5 pagesAOSD Case ReportBogdan LupuNo ratings yet
- The Diagnostic Challenge of Adult-Onset Still's DiseaseDocument4 pagesThe Diagnostic Challenge of Adult-Onset Still's DiseaseBogdan LupuNo ratings yet
- The Diagnostic Challenge of Adult-Onset Still's DiseaseDocument4 pagesThe Diagnostic Challenge of Adult-Onset Still's DiseaseBogdan LupuNo ratings yet
- Successful Treatment of Refractory Adult Onset Still's Disease With RituximabDocument4 pagesSuccessful Treatment of Refractory Adult Onset Still's Disease With RituximabBogdan LupuNo ratings yet
- Pathway For The Management of Adult Onset Still's DiseaseDocument1 pagePathway For The Management of Adult Onset Still's DiseaseBogdan LupuNo ratings yet
- Adult Onset Still's Disease Associated With Mycoplasma Pneumoniae Infection and Hemophagocytic LymphohistiocytosisDocument5 pagesAdult Onset Still's Disease Associated With Mycoplasma Pneumoniae Infection and Hemophagocytic LymphohistiocytosisBogdan LupuNo ratings yet
- Adult Onset Still's Disease Associated With Mycoplasma Pneumoniae Infection and Hemophagocytic LymphohistiocytosisDocument5 pagesAdult Onset Still's Disease Associated With Mycoplasma Pneumoniae Infection and Hemophagocytic LymphohistiocytosisBogdan LupuNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Chapter 7 Dopant Diffusion - IDocument32 pagesChapter 7 Dopant Diffusion - I강준호No ratings yet
- Isulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atDocument1 pageIsulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atMysterious StudentNo ratings yet
- Kinder DLL Week 8Document15 pagesKinder DLL Week 8Jainab Pula SaiyadiNo ratings yet
- Clinical Reviews: The Management of Children With Gastroenteritis and Dehydration in The Emergency DepartmentDocument13 pagesClinical Reviews: The Management of Children With Gastroenteritis and Dehydration in The Emergency DepartmentRina Dewi AnggraeniNo ratings yet
- Orbitol Motor TMTHWDocument20 pagesOrbitol Motor TMTHWRodolfo ErenoNo ratings yet
- SOPDocument16 pagesSOPjerome marquezNo ratings yet
- Comparative Study On Serial and Parallel Manipulators - ReviewDocument23 pagesComparative Study On Serial and Parallel Manipulators - ReviewShaik Himam SahebNo ratings yet
- Investigation of Skew Curved Bridges in Combination With Skewed Abutments Under Seismic ResponseDocument5 pagesInvestigation of Skew Curved Bridges in Combination With Skewed Abutments Under Seismic ResponseEditor IJTSRDNo ratings yet
- Adriano Costa Sampaio: Electrical EngineerDocument3 pagesAdriano Costa Sampaio: Electrical EngineeradrianorexNo ratings yet
- Indoor Air Quality Standard Procedures - 2014 RevDocument12 pagesIndoor Air Quality Standard Procedures - 2014 RevFioriAmeliaHathawayNo ratings yet
- PH & TemperatureDocument8 pagesPH & TemperatureNanaNo ratings yet
- Chapter 7 - Stress - TransformationsDocument21 pagesChapter 7 - Stress - TransformationsroselleNo ratings yet
- YoungMan EN131 GUIDEDocument16 pagesYoungMan EN131 GUIDErcpawar100% (1)
- FactSet London OfficeDocument1 pageFactSet London OfficeDaniyar KaliyevNo ratings yet
- 5 Contracting Activity and Technical Staff RequirementsDocument2 pages5 Contracting Activity and Technical Staff RequirementsDaniyar KussainovNo ratings yet
- Coding Decoding Sheet - 01 1678021709186Document9 pagesCoding Decoding Sheet - 01 1678021709186Sumit VermaNo ratings yet
- Pharmalytica Exhibitor List 2023Document3 pagesPharmalytica Exhibitor List 2023Suchita PoojaryNo ratings yet
- SAT Practice Test 10 - College BoardDocument34 pagesSAT Practice Test 10 - College BoardAdissaya BEAM S.No ratings yet
- Hypothesis Testing - IDocument36 pagesHypothesis Testing - Isai revanthNo ratings yet
- ECE199R-C12 Final Document OJTDocument48 pagesECE199R-C12 Final Document OJTRigel ZabateNo ratings yet
- Region 1 - Concreting Works Materials Prices - PHILCON PRICESDocument9 pagesRegion 1 - Concreting Works Materials Prices - PHILCON PRICESMark Gregory RimandoNo ratings yet
- Automatic Train OperationDocument6 pagesAutomatic Train OperationAnupam KhandelwalNo ratings yet
- Arts Class: Lesson 01Document24 pagesArts Class: Lesson 01Lianne BryNo ratings yet
- Contoh CV / Daftar Riwayat HidupDocument2 pagesContoh CV / Daftar Riwayat HiduprusmansyahNo ratings yet
- Segmentation of Blood Vessels Using Rule-Based and Machine-Learning-Based Methods: A ReviewDocument10 pagesSegmentation of Blood Vessels Using Rule-Based and Machine-Learning-Based Methods: A ReviewRainata PutraNo ratings yet
- The History of AstrologyDocument36 pagesThe History of AstrologyDharani Dharendra DasNo ratings yet
- A Study On Traditional Medicinal Herbs Used by The Ethnic People of Goalpara District of Assam, North East IndiaDocument6 pagesA Study On Traditional Medicinal Herbs Used by The Ethnic People of Goalpara District of Assam, North East IndiaDr. Krishna N. SharmaNo ratings yet
- Prevailing Torque Locknut Technical SpecificationsDocument3 pagesPrevailing Torque Locknut Technical SpecificationsLiu YangtzeNo ratings yet
- Rectifier 5G High Density Embedded Power (3U Power Rack, Three Phase Four Wire) E...Document4 pagesRectifier 5G High Density Embedded Power (3U Power Rack, Three Phase Four Wire) E...Lintas LtiNo ratings yet
- Usp Description and SolubilityDocument1 pageUsp Description and SolubilityvafaashkNo ratings yet