Professional Documents
Culture Documents
Atropine Sulfate
Uploaded by
Manelle SingzonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Atropine Sulfate
Uploaded by
Manelle SingzonCopyright:
Available Formats
atropine sulfate
(a troe peen)
Parenteral and oral preparations:
AtroPen, Minims (CAN), Sal-Tropine
Ophthalmic solution:
Atropine Sulfate S.O.P., Isopto Atropine Ophthalmic
Pregnancy Category C
Drug classes of Atrophine Sulfate
Anticholinergic
Antimuscarinic
Parasympatholytic
Antiparkinsonian
Antidote
Diagnostic agent (ophthalmic preparations)
Belladonna alkaloid
Therapeutic actions of Atrophine Sulfate
Competitively blocks the effects of acetylcholine at muscarinic cholinergic
receptors that mediate the effects of parasympathetic postganglionic
impulses, depressing salivary and bronchial secretions, dilating the bronchi,
inhibiting vagal influences on the heart, relaxing the GI and GU tracts,
inhibiting gastric acid secretion (high doses), relaxing the pupil of the eye
(mydriatic effect), and preventing accommodation for near vision (cycloplegic
effect); also blocks the effects of acetylcholine in the CNS.
Dosage & Route
ADULTS
Systemic administration
0.40.6 mg PO, IM, IV, or subcutaneously.
Hypotonic radiography: 1 mg IM.
Surgery: 0.5 mg (0.40.6 mg) IM (or subcutaneously or IV) prior to induction
of anesthesia; during surgery, give IV; reduce dose to < 0.4 mg with
cyclopropane anesthesia.
Bradyarrhythmias: 0.41 mg (up to 2 mg) IV every 12 hr as needed.
Antidote: For poisoning due to cholinesterase inhibitor insecticides, give large
doses of at least 23 mg parenterally, and repeat until signs of atropine
intoxication appear; for rapid type of mushroom poisoning, give in doses
sufficient to control parasympathetic signs before coma and CV collapse
intervene. Auto-injector provides rapid administration.
Ophthalmic solution
For refraction: Instill 12 drops into eye 1 hr before refracting.
For uveitis: Instill 12 drops into eye qid.
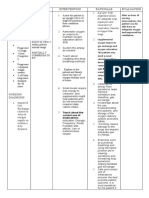
PEDIATRIC PATIENTS
Systemic administration
Refer to the following table:
Weight
Dose (mg)
716 lb (3.27.3 kg)
0.1
1624 lb (7.310.9 kg)
0.15
2440 lb (10.918.1 kg)
0.2
4065 lb (18.129.5 kg)
0.3
6590 lb (29.540.8 kg)
0.4
> 90 lb (> 40.8 kg)
0.40.6
Surgery: 0.1 mg (newborn) to 0.6 mg (12 yr) injected subcutaneously 30 min
before surgery.
Antidote:
> 90 lb: 2 mg auto-injector.
4090 lb: 1-mg auto-injector.
1540 lb: 0.5 mg auto-injector.
< 15 lb: 0.25 mg auto-injector.
GERIATRIC PATIENTS
More likely to cause serious adverse reactions, especially CNS reactions, in
elderly patients; use with
Indications of Atrophine
Systemic administration
Antisialagogue for preanesthetic medication to prevent or reduce respiratory
tract secretions
Treatment of parkinsonism; relieves tremor and rigidity
Restoration of cardiac rate and arterial pressure during anesthesia when
vagal stimulation produced by intra-abdominal traction causes a decrease in
pulse rate, lessening the degree of AV block when increased vagal tone is a
factor (eg, some cases due to digitalis)
Relief of bradycardia and syncope due to hyperactive carotid sinus reflex
Relief of pylorospasm, hypertonicity of the small intestine, and hypermotility
of the colon
Relaxation of the spasm of biliary and ureteral colic and bronchospasm
Relaxation of the tone of the detrusor muscle of the urinary bladder in the
treatment of urinary tract disorders
Control of crying and laughing episodes in patients with brain lesions
Treatment of closed head injuries that cause acetylcholine release into CSF,
EEG abnormalities, stupor, neurologic signs
Relaxation of uterine hypertonicity
Management of peptic ulcer
Control of rhinorrhea of acute rhinitis or hay fever
Antidote (with external cardiac massage) for CV collapse from overdose of
parasympathomimetic (cholinergic) drugs (choline esters, pilocarpine), or
cholinesterase inhibitors (eg, physostigmine, isoflurophate,
organophosphorus insecticides)
Antidote for poisoning by certain species of mushroom (eg, Amanita
muscaria)
Ophthalmic preparations
Diagnostically to produce mydriasis and cycloplegia-pupillary dilation in acute
inflammatory conditions of the iris and uveal tract
Adverse effects of Atrophine
Systemic administration
CNS: Blurred vision, mydriasis, cycloplegia, photophobia, increased IOP,
headache, flushing, nervousness, weakness, dizziness, insomnia, mental
confusion or excitement (after even small doses in the elderly), nasal
congestion
CV: Palpitations, bradycardia (low doses), tachycardia (higher doses)
GI: Dry mouth, altered taste perception, nausea, vomiting, dysphagia,
heartburn, constipation, bloated feeling, paralytic ileus, gastroesophageal
reflux
GU: Urinary hesitancy and retention; impotence
Other: Decreased sweating and predisposition to heat prostration,
suppression of lactation
Ophthalmic preparations
Local: Transient stinging
Systemic: Systemic adverse effects, depending on amount absorbed
Contraindications of Atrophine
Contraindicated with hypersensitivity to anticholinergic drugs.
Systemic administration
Contraindicated with glaucoma; adhesions between iris and lens; stenosing
peptic ulcer; pyloroduodenal obstruction; paralytic ileus; intestinal atony;
severe ulcerative colitis; toxic megacolon; symptomatic prostatic
hypertrophy; bladder neck obstruction; bronchial asthma; COPD; cardiac
arrhythmias; tachycardia; myocardial ischemia; impaired metabolic, hepatic,
or renal function; myasthenia gravis.
Use cautiously with Down syndrome, brain damage, spasticity, hypertension,
hyperthyroidism, lactation.
Ophthalmic solution
Contraindicated with glaucoma or tendency to glaucoma.
Nursing considerations of Atrophine
Assessment
History: Hypersensitivity to anticholinergics; glaucoma; adhesions between
iris and lens; stenosing peptic ulcer; pyloroduodenal obstruction; paralytic
ileus; intestinal atony; severe ulcerative colitis; toxic megacolon;
symptomatic prostatic hypertrophy; bladder neck obstruction; bronchial
asthma; COPD; cardiac arrhythmias; myocardial ischemia; impaired
metabolic, liver, or renal function; myasthenia gravis; Down syndrome; brain
damage; spasticity; hypertension; hyperthyroidism; lactation
Physical: Skin color, lesions, texture; T; orientation, reflexes, bilateral grip
strength; affect; ophthalmic examination; P, BP; R, adventitious sounds;
bowel sounds, normal GI output; normal urinary output, prostate palpation;
LFTs, renal function tests, ECG
Interventions
Ensure adequate hydration; provide environmental control (temperature) to
prevent hyperpyrexia.
Have patient void before taking medication if urinary retention is a problem.
Teaching points
When used preoperatively or in other acute situations, incorporate teaching about
the drug with teaching about the procedure; the ophthalmic solution is mainly used
acutely and will not be self-administered by the patient; the following apply to oral
medication for outpatients:
Take as prescribed, 30 minutes before meals; avoid excessive dosage.
Avoid hot environments; you will be heat intolerant, and dangerous reactions
may occur.
You may experience these side effects: Dizziness, confusion (use caution
driving or performing hazardous tasks); constipation (ensure adequate fluid
intake, proper diet); dry mouth (sugarless lozenges, frequent mouth care may
help; may be transient); blurred vision, sensitivity to light (reversible; avoid
tasks that require acute vision; wear sunglasses in bright light); impotence
(reversible); difficulty in urination (empty the bladder prior to taking drug).
Report rash; flushing; eye pain; difficulty breathing; tremors, loss of
coordination; irregular heartbeat, palpitations; headache; abdominal
distention; hallucinations; severe or persistent dry mouth; difficulty
swallowing; difficulty in urination; constipation; sensitivity to light.
You might also like
- Flores Mary Jane Generic Drug ChartDocument23 pagesFlores Mary Jane Generic Drug ChartKristine Dela CruzNo ratings yet
- Atropine Sulfate for Bradycardia and PoisoningDocument4 pagesAtropine Sulfate for Bradycardia and PoisoningSuraya_Mohamed_3281No ratings yet
- Tuberculosis Power PointDocument20 pagesTuberculosis Power PointLeena LapenaNo ratings yet
- Pharma - Drugs Affecting Git MotilityDocument6 pagesPharma - Drugs Affecting Git MotilityBobet ReñaNo ratings yet
- Peptic UlcerDocument5 pagesPeptic UlcermerobabuNo ratings yet
- BSN ANGELICA NASOGASTRIC FEEDING TUBE CAREDocument3 pagesBSN ANGELICA NASOGASTRIC FEEDING TUBE CAREMarius Clifford Billedo50% (2)
- Ortho NCLEX Questions 1 PDFDocument39 pagesOrtho NCLEX Questions 1 PDFElizabella Henrietta TanaquilNo ratings yet
- Naloxone in AdultsDocument8 pagesNaloxone in AdultsRoboschi StefaniaNo ratings yet
- ASSESSMENT PLANNING INTERVENTION RATIONALE EVALUATIONDocument2 pagesASSESSMENT PLANNING INTERVENTION RATIONALE EVALUATIONIrish Jane GalloNo ratings yet
- GitDocument302 pagesGitjgcriste100% (7)
- Gastrointestinal SystemDocument17 pagesGastrointestinal SystempreetNo ratings yet
- VerA Ok-Prelim Ncm104 (Autosaved) VeraDocument30 pagesVerA Ok-Prelim Ncm104 (Autosaved) Verajesperdomincilbayaua100% (1)
- The Musculoskeletal HandoutsDocument3 pagesThe Musculoskeletal Handouts_Advernice_No ratings yet
- Hand Hygiene: Alcohol Based Hand RubDocument2 pagesHand Hygiene: Alcohol Based Hand RubKIERSTINE MARIE BARCELONo ratings yet
- #2-NCM 109 - TransesDocument19 pages#2-NCM 109 - TransesJaimie BanaagNo ratings yet
- Vaccination or ImmunizationDocument4 pagesVaccination or ImmunizationPrincessNo ratings yet
- Medical Surgical Nursing Understanding HemophiliaDocument2 pagesMedical Surgical Nursing Understanding HemophiliaChieChay DubNo ratings yet
- Oxytocin and Methylergonovine Nursing StudyDocument16 pagesOxytocin and Methylergonovine Nursing StudyDinarkram Rabreca EculNo ratings yet
- Medical Surgical: SNS (Anti-Cholinergic/adrenergic)Document12 pagesMedical Surgical: SNS (Anti-Cholinergic/adrenergic)Pedro SorianoNo ratings yet
- Final NCM 116 PDFDocument20 pagesFinal NCM 116 PDFJoshua MendezNo ratings yet
- Chapter 067 Sirs ModsDocument25 pagesChapter 067 Sirs Modsapi-232466940No ratings yet
- Ulcerative ColitisDocument9 pagesUlcerative Colitiskint manlangitNo ratings yet
- Drugs Used in AnesthesiaDocument33 pagesDrugs Used in AnesthesiaDelvine AderoNo ratings yet
- The Child With Hematologic DisordersDocument149 pagesThe Child With Hematologic DisordersNics FranciscoNo ratings yet
- DRUG STUDY: NCM 106 PHARMACOLOGYDocument6 pagesDRUG STUDY: NCM 106 PHARMACOLOGYKevin RosalesNo ratings yet
- Infectious and Inflammatory Disorders of The Urinary SystemDocument16 pagesInfectious and Inflammatory Disorders of The Urinary SystemBibi Renu100% (1)
- Chapter 54 Drugs Acting On The Upper Respiratory TractDocument42 pagesChapter 54 Drugs Acting On The Upper Respiratory TractVillanueva, Alwyn Shem T.No ratings yet
- Drug StudyDocument9 pagesDrug StudyMäc LäntinNo ratings yet
- EENT Disorders StudentsDocument26 pagesEENT Disorders StudentsPye Antwan DelvaNo ratings yet
- First Stage: Stages of Labor Start End Duration Nullipara MultiparaDocument4 pagesFirst Stage: Stages of Labor Start End Duration Nullipara MultiparaElleNo ratings yet
- 4 Measurement and ComputationDocument6 pages4 Measurement and ComputationBernardMarkMateoNo ratings yet
- A. A Sudden Change in How Brain Cells Send Electrical Signals To One AnotherDocument70 pagesA. A Sudden Change in How Brain Cells Send Electrical Signals To One AnotherMwansaay Twain HolyNo ratings yet
- Pharma Cards.Document19 pagesPharma Cards.Brent NicholsNo ratings yet
- 3 Post Test PediaDocument4 pages3 Post Test PediaJanine BaticbaticNo ratings yet
- Ob Nursing BulletsDocument22 pagesOb Nursing BulletsDick Morgan FerrerNo ratings yet
- Hypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumDocument5 pagesHypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumMelodia Turqueza GandezaNo ratings yet
- FundaDocument101 pagesFundaMelanieTriezlVillaseñorJosonNo ratings yet
- A. The Sum of All Chemical Reactions in The Organisms, That Produce Energy or Synthesize Organic MatterDocument5 pagesA. The Sum of All Chemical Reactions in The Organisms, That Produce Energy or Synthesize Organic MatterShane Aileen AngelesNo ratings yet
- Meningitis Pathophysiology PDFDocument59 pagesMeningitis Pathophysiology PDFpaswordnyalupa100% (1)
- Short Term Goal: After 1 Hour of Short Term Goal: After 1Document2 pagesShort Term Goal: After 1 Hour of Short Term Goal: After 1Jordz PlaciNo ratings yet
- MicrocephalyDocument4 pagesMicrocephalykurei_bluflamedNo ratings yet
- Types of ShocksDocument33 pagesTypes of Shocksmark OrpillaNo ratings yet
- Cardiogenic Shock NclexDocument81 pagesCardiogenic Shock NclexKrishna SapkotaNo ratings yet
- Drugs Used in TuberculosisDocument27 pagesDrugs Used in Tuberculosisapi-3705123No ratings yet
- Geria ReviewerDocument7 pagesGeria ReviewerCarl John ManaloNo ratings yet
- See Full Prescribing Information For Complete Boxed WarningDocument43 pagesSee Full Prescribing Information For Complete Boxed WarningParishan SaeedNo ratings yet
- Presentation Dengue FeverDocument21 pagesPresentation Dengue Feverpolarbear12121250% (2)
- Cushing's SyndromeDocument5 pagesCushing's SyndromesummerduskNo ratings yet
- Practice Drill For Partograph Case ScenarioDocument2 pagesPractice Drill For Partograph Case ScenarioBethrice MelegritoNo ratings yet
- Pathophysiology of ArrhythmiasDocument15 pagesPathophysiology of ArrhythmiasJonathan MontecilloNo ratings yet
- Drug StudyDocument11 pagesDrug StudyJay VillasotoNo ratings yet
- Midterm Exam Antiinfective, Biotic, ViralDocument5 pagesMidterm Exam Antiinfective, Biotic, ViralJojo Justo100% (2)
- Kabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDocument24 pagesKabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDivine Mercy De JulianNo ratings yet
- MS HemaDocument6 pagesMS HemaFrechel Ann Landingin PedrozoNo ratings yet
- Anti-Cholinergic Drugs and Cholinesterase InhibitorsDocument24 pagesAnti-Cholinergic Drugs and Cholinesterase InhibitorsKhalid I. Abdullah100% (1)
- Important Estimates in Pregnancy & Danger Signs in Pregnancy PDFDocument3 pagesImportant Estimates in Pregnancy & Danger Signs in Pregnancy PDFTandingco, Olivia Mari H.No ratings yet
- ValvularDocument2 pagesValvularJulia Rae Delos SantosNo ratings yet
- Ob FinalDocument43 pagesOb FinalPrincess LotusNo ratings yet
- HANDOUT Chapter 11 Promoting Fetal and Maternal HealthDocument7 pagesHANDOUT Chapter 11 Promoting Fetal and Maternal HealthClouiseNo ratings yet
- BIRTHMONTH SALE UpdatedDocument114 pagesBIRTHMONTH SALE UpdatedManelle SingzonNo ratings yet
- BIRTHMONTH SALE UpdatedDocument114 pagesBIRTHMONTH SALE UpdatedManelle SingzonNo ratings yet
- Isosorbide DinitrateDocument4 pagesIsosorbide DinitrateManelle Singzon100% (1)
- Radiofrequency AblationDocument4 pagesRadiofrequency AblationManelle SingzonNo ratings yet
- HNBBDocument3 pagesHNBBManelle SingzonNo ratings yet
- Abs WorkoutDocument2 pagesAbs WorkoutManelle SingzonNo ratings yet
- Sal But AmolDocument6 pagesSal But AmolManelle SingzonNo ratings yet
- Managerial Control FunctionsDocument27 pagesManagerial Control FunctionsKaustubh TiwaryNo ratings yet
- Toradol Drugs Nsaids Pain Ibuprofen Motrin Naproxen Naprosyn Aleve Pain Immune System FeverDocument1 pageToradol Drugs Nsaids Pain Ibuprofen Motrin Naproxen Naprosyn Aleve Pain Immune System FeverManelle SingzonNo ratings yet
- NursingDocument2 pagesNursingManelle SingzonNo ratings yet
- CPR 2005 & 2010 Comparison2003Document11 pagesCPR 2005 & 2010 Comparison2003Manelle SingzonNo ratings yet
- NursingDocument2 pagesNursingManelle SingzonNo ratings yet
- Neurological Exam ComponentsDocument10 pagesNeurological Exam ComponentsManelle SingzonNo ratings yet
- Glasgow Coma Scale HandoutDocument2 pagesGlasgow Coma Scale HandoutFajar Ahmad PrasetyaNo ratings yet
- Necrotizing Faciitis and Burn2003Document10 pagesNecrotizing Faciitis and Burn2003Manelle SingzonNo ratings yet
- Somalia HCDocument7 pagesSomalia HCManelle SingzonNo ratings yet
- Carcinoma (SCLC), Also Called Oat Cell Cancer, and Non-Small Cell Lung Carcinoma (NSCLC) - The MostDocument17 pagesCarcinoma (SCLC), Also Called Oat Cell Cancer, and Non-Small Cell Lung Carcinoma (NSCLC) - The MostManelle SingzonNo ratings yet
- Renal Failure: Manelle R. Singzon BSN 4A1-1Document30 pagesRenal Failure: Manelle R. Singzon BSN 4A1-1Manelle SingzonNo ratings yet
- One Armed Blind Deaf MuteDocument9 pagesOne Armed Blind Deaf MuteManelle SingzonNo ratings yet
- Related LiteratureDocument1 pageRelated LiteratureManelle SingzonNo ratings yet
- Inflammation Is A Secret KillerDocument7 pagesInflammation Is A Secret KillerManelle SingzonNo ratings yet
- Types of LearningDocument2 pagesTypes of LearningManelle SingzonNo ratings yet
- HealthDocument10 pagesHealthManelle SingzonNo ratings yet
- Nursing Care Plan HypertensionDocument2 pagesNursing Care Plan Hypertensionderic98% (124)
- CancerDocument37 pagesCancerManelle SingzonNo ratings yet
- Dystocia - Case ReportDocument51 pagesDystocia - Case ReportPaijo SusenoNo ratings yet
- Principles and Practice of Single Implant and Restoration - Saunders 1 Edition (March 26, 2013)Document204 pagesPrinciples and Practice of Single Implant and Restoration - Saunders 1 Edition (March 26, 2013)Sergiu Pinte100% (1)
- Elevated LDL Triglycerides and Atherosclerotic Risk: BackgroundDocument17 pagesElevated LDL Triglycerides and Atherosclerotic Risk: BackgroundRoxana MariaNo ratings yet
- Diseccion Aortica Acguda CronicaDocument10 pagesDiseccion Aortica Acguda Cronicaarturo garciaNo ratings yet
- AllergiesDocument11 pagesAllergiesAficionadoNo ratings yet
- Yellow Fever Vaccination Requirements From India - Chalo AfricaDocument148 pagesYellow Fever Vaccination Requirements From India - Chalo AfricaAbishek ChandranNo ratings yet
- Teriparatide, Vitamin D, Cinacalcet, SevelamerDocument2 pagesTeriparatide, Vitamin D, Cinacalcet, SevelamerJosh KalishNo ratings yet
- Family Case Study For HydrocephalusDocument9 pagesFamily Case Study For HydrocephalusjaegergranNo ratings yet
- Wound Care InstructionsDocument3 pagesWound Care InstructionsKat TaasinNo ratings yet
- The Neurological History Taking: Osheik Seidi Sunderland Royal Hospital UKDocument38 pagesThe Neurological History Taking: Osheik Seidi Sunderland Royal Hospital UKHassen Kavi Isse100% (3)
- Govorno Jezicki Poremecaji Razvojnog Doba Speech and Language Disorders at Developmental AgeDocument259 pagesGovorno Jezicki Poremecaji Razvojnog Doba Speech and Language Disorders at Developmental AgeVeljko BorovinaNo ratings yet
- MCQs blood & cell physiology blogDocument8 pagesMCQs blood & cell physiology bloglubna malikNo ratings yet
- Nur 097 Sas 1 3Document9 pagesNur 097 Sas 1 3gekkonoojiNo ratings yet
- Chapter 2 Herbs That Clear HeatDocument159 pagesChapter 2 Herbs That Clear HeatCarleta Stan100% (1)
- CHAPTER II Open BurningDocument6 pagesCHAPTER II Open Burningjedric_14100% (1)
- Food For The BrainDocument34 pagesFood For The BrainKristine Mae AbrasaldoNo ratings yet
- Research Proposal First Draft (Adamu Moti)Document25 pagesResearch Proposal First Draft (Adamu Moti)ODAA TUBENo ratings yet
- NASAL SEPTUM DEVIATION: CAUSES, SYMPTOMS AND SURGICAL CORRECTIONDocument105 pagesNASAL SEPTUM DEVIATION: CAUSES, SYMPTOMS AND SURGICAL CORRECTIONNguyễn ThànhNo ratings yet
- Ophthalmic Drops 101Document9 pagesOphthalmic Drops 101David NgNo ratings yet
- Parasitology study table overviewDocument10 pagesParasitology study table overviewBashaer GellehNo ratings yet
- Turkish Angora CatDocument6 pagesTurkish Angora CatprosvetiteljNo ratings yet
- Renal Vegetarian NutritionDocument2 pagesRenal Vegetarian NutritionSg Balaji100% (1)
- Information Bulletin A FMC Mbbs 2021Document27 pagesInformation Bulletin A FMC Mbbs 2021Bidyut Bikash BaruahNo ratings yet
- Imaging of Nasopharyngeal CarcinomaDocument9 pagesImaging of Nasopharyngeal CarcinomayohanasmjtNo ratings yet
- RT MapehDocument2 pagesRT MapehRowan ImperialNo ratings yet
- Pain Scales and Assessment UnhasDocument93 pagesPain Scales and Assessment Unhashaphahap0% (1)
- Discussion Topics: Seafood Red ListDocument3 pagesDiscussion Topics: Seafood Red ListНадія ЛупійNo ratings yet
- Dimension Exl 200 Tech SpecsDocument2 pagesDimension Exl 200 Tech SpecsOo Kenx OoNo ratings yet
- Auxiliary VerbsDocument12 pagesAuxiliary VerbsNoe Lia CastroNo ratings yet
- Mitochondrial Cytopathies in Children and AdultsDocument28 pagesMitochondrial Cytopathies in Children and AdultsmmaitehmdNo ratings yet