Professional Documents
Culture Documents
Best Evidence Statement (Best) : Definitions
Uploaded by
Fungky AnthonyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Best Evidence Statement (Best) : Definitions
Uploaded by
Fungky AnthonyCopyright:
Available Formats
Rheumatology/Juvenile Idiopathic Arthritis (JIA)/Uveitis/BESt 011
Best Evidence Statement (BESt)
Date: June 18, 2012
Title: Screening for Uveitis in Children with Juvenile Idiopathic Arthritis (JIA)
Clinical Question:
P (population/problem):
I (intervention)
O (outcome)
In pediatric patients 0 to 18 years of age with JIA
what is the optimal ophthalmologic screening schedule
to prevent and minimize uveitis-associated morbidity?
Target Population:
Included: Children (0 to 18 years of age) diagnosed with JIA
Excluded: Children with JIA who have been previously diagnosed with uveitis
Definitions:
Juvenile idiopathic arthritis is arthritis of unknown etiology that begins before the 16th birthday and persists for at least
6 weeks; other known conditions are excluded (Petty 2001 [5a]). (See table 1: International League of Associations for Rheumatology
Classification of Juvenile Idiopathic Arthritis).
Uveitis-associated morbidity includes cataracts, glaucoma, band keratopathy, phthisis bulbi and loss of vision (Cassidy 2006 [5a]).
Recommendations:
1. It is recommended that a referral for an initial screening examination for uveitis be made by the rheumatology
provider upon diagnosis of JIA, and the exam be performed within one month after diagnosis of JIA (Carvounis 2006
[1a], Grassi 2007 [4a]; Heiligenhaus 2007 [3a]; Cassidy 2006 [5a]).
Note: The onset of uveitis is often asymptomatic and/or occurs in children unable to recognize and verbalize
symptoms (Cassidy 2006 [5a]; Woreta 2006 [4b]).
2. It is recommended that after the initial screening examination, regular follow-up screenings be maintained based on risk
category and classification (see Table 2: Suggested screening intervals in patients with JIA) (Heiligenhaus 2007 [3a]).
Note: Risk category and classification include the categories of the subtype of JIA, antinuclear antibody status, age of onset of
JIA and duration of JIA (Heiligenhaus 2007 [3a]).
3. It is recommended that screening change from every six months to every twelve months in ANA positive patients
with disease onset >6 years of age who have not had uveitis within the first two years of JIA diagnosis (Heiligenhaus
2007 [3a]; Saurenmann 2010 [4a]; Woreta 2007 [4b]).
Note: The risk of developing additional complications between four years and six years of onset is minimal; this
decreased risk supports a change in the screening recommendation in these patients (Heiligenhaus 2007 [3a];
Saurenmann 2010 [4a]; Woreta 2007 [4b]).
4. It is recommended that if the patient is < 6 years of age and the provider has a strong suspicion of JIA or the patient
is known to test positive for antinuclear antibodies (ANA), the provider proactively refer the patient for a screening
examination for uveitis (Bolt 2008 [4a]; Woreta 2007 [4b]; Heiligenhaus 2007 [3a]).
Note: Given that the risk of uveitis is highest among ANA positive patients age < 2 years, it is beneficial to make
every effort to schedule an ophthalmology assessment at the earliest possible time. This could be prior or on
the day of the rheumatology assessment (Local Consensus [5]).
5. It is recommended that screenings for uveitis be performed by an optometrist or ophthalmologist experienced in
pediatric care, using a slit lamp procedure (Cassidy 2006 [5a]; Heiligenhaus 2007 [3a]).
Copyright 2012 Cincinnati Children's Hospital Medical Center; all rights reserved.
Page 1 of 6
Rheumatology/Juvenile Idiopathic Arthritis (JIA)/Uveitis/BESt 011
Table 1: International League of Associations for Rheumatology Classification of Juvenile Idiopathic Arthritis
Exclusions:
The principle of this classification is that all categories of JIA are mutually exclusive. This principle is reflected in the list of possible exclusions for
each category:
a. Psoriasis or a history of psoriasis in the patient or first degree relative.
b. Arthritis in an HLA-B27 positive male beginning after the 6th birthday.
c. Ankylosing spondylitis, enthesitis related arthritis, sacroiliitis with inflammatory bowel disease, Reiters syndrome, or acute anterior uveitis, or a
history of one of these disorders in a first-degree relative.
d. The presence of IgM rheumatoid factor on at least 2 occasions at least 3 months apart.
e. The presence of systemic JIA in the patient.
The application of exclusions is indicated under each category, and may change as new data become available.
Category
Definition
Exclusions (above)
Systemic Arthritis
Arthritis in one or more joints with or preceded by fever of at least 2 weeks duration that is
a, b, c, d.
documented to be daily (quotidian) for at least 3 days, and accompanied by one or more
of the following:
1. Evanescent (nonfixed) erythematous rash
2. Generalized lymph node enlargement
3. Hepatomegaly and/or splenomegaly
4. Serositis
Oligoarthritis
Arthritis affecting one to 4 joints during the first 6 months of disease. Two subcategories are
a, b, c, d, e
recognized:
1. Persistent oligoarthritis: Affecting not more than 4 joints throughout the disease course
2. Extended oligoarthritis: Affecting a total of more than 4 joints after the first 6 months of
disease
Polyarthritis (Rheumatoid
Arthritis affecting 5 or more joints during the first 6 months of disease; a test for RF is
a, b, c, d, e
Factor Negative)
negative.
Polyarthritis (Rheumatoid
Arthritis affecting 5 or more joints during the first 6 months of disease; 2 or more tests for RF a, b, c, e
Factor Positive)
at least 3 months apart during the first 6 months of disease are positive.
Psoriatic Arthritis
Arthritis and psoriasis, or arthritis and at least 2 of the following:
b, c, d, e
1. Dactylitis
2. Nail pitting or onycholysis
3. Psoriasis in a first-degree relative
Enthesitis Related Arthritis
Arthritis and enthesitis, or arthritis or enthesitis with at least 2 of the following:
a, d, e
1. The presence of or a history of sacroiliac joint tenderness and/or inflammatory
lumbosacral pain
2. The presence of HLA-B27 antigen
3. Onset of arthritis in a male over 6 years of age
4. Acute anterior uveitis
5. History of ankylosing spondylitis, enthesitis related arthritis, sacroiliitis with inflammatory
bowel disease, Reiters syndrome, or acute anterior uveitis in a first-degree relative
Undifferentiated Arthritis
Arthritis that fulfills criteria in no category or in 2 or more of the above categories.
(Petty 2001 [5a])
Table 2: Suggested screening intervals for uveitis in patients with JIA as classified by International League of Associations for
Rheumatology (ILAR) criteria
(Heiligenhaus 2007)[3a])- adapted
Copyright 2012 Cincinnati Children's Hospital Medical Center; all rights reserved.
Page 2 of 6
Rheumatology/Juvenile Idiopathic Arthritis (JIA)/Uveitis/BESt 011
Discussion/Summary of Evidence related to the recommendations:
A recent meta-analysis of cohort studies published 1980 through 2004 concluded that the guidelines from the American
Academy of Pediatrics are supported by the evidence, with these exceptions; younger ANA-positive, oligoarticular-onset
and polyarticular-onset patients are at the highest risk for uveitis, ANA-negative JIA patients with disease onset by age 4
years have moderate risk categories, irrespective of JIA subtype (Carvounis 2006 [1a]).
Uveitis is quite often detected at the first ophthalmologic consultation early during the course of JIA (Kotaniemi 2003 [5b]).
At presentation with JIA, ocular complications were seen in 67% of eyes affected by JIA associated uveitis (Woreta 2006
[4b]). A 2007 study found that 73% of patients exhibited uveitis before or within the first 12 months after onset of
arthritis and 77% and 90% within the first 2 and 4 years respectively (Heiligenhaus 2007 [3a]).
Given the level of scientific evidence available, it is recognized that some children may be over screened and others
under screened by 1 to 2 months (Local Consensus [5]).
Reference List
1.
Bolt, I.B.; Cannizzaro, E.; Seger, R.; and Saurenmann, K.S.: Risk factors and longterm outcome of juvenile idiopathic arthritis-associated uveitis
in switzerland. J Rheumatol, 35: 7030706, 2008, [4a].
2.
Carvounis, P. E.; Herman, D. C.; Cha, S.; and Burke, J. P.: Incidence and outcomes of uveitis in juvenile rheumatoid arthritis, a synthesis of the
literature. Graefes Archive for Clinical & Experimental Ophthalmology, 244(3): 281-90, 2006, [1a]
http://groups/p2/EBC_Files/Articles_Cited_in_EPIC_Ophth/OphthCarvounis2006.pdf .
http://www.ncbi. nlm.nih. gov/entrez/ query.fcgi?cmd= Retrieve&db= PubMe d&dopt=Citatio n&list_ uids=1 6228 217
3.
Cassidy, J.; Kivlin, J.; Lindsley, C.; and Nocton, J.: Ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics,
117(5): 1843-5, 2006, [5a]
http://groups/p2/EBC_Files/Articles_Cited_in_EPIC_Ophth/OphthCassidy2006.pdf .
http://www.ncbi.nl m.nih .gov/entrez/ query.fcgi?cmd= Retrieve&db= PubMe d&dopt=Citatio n&list_ uids= 16651 348
4.
Grassi, A.; Corona, F.; Casellato, A.; Carnelli, V.; and Bardare, M.: Prevalence and outcome of juvenile idiopathic arthritis-associated uveitis
and relation to articular disease. J Rheumatol, 34(5): 1139-45, 2007, [4a]
http://groups/p2/EBC_Files/Articles_Cited_in_EPIC_Ophth/OphthGrassi2007.pdf.
http://www.ncbi.nl m.nih. gov/entrez/q uery.fcgi?cmd=Retrieve&db=P ubMed &d opt=Citation &list_ui ds=17 3433 17
5.
Heiligenhaus, A.; Niewerth, M.; Ganser, G.; Heinz, C.; Minden, K.; and German Uveitis in Childhood Study Group: Prevalence and
complications of uveitis in juvenile idiopathic arthritis in a population-based nation-wide study in germany: suggested modification of the
current screening guidelines. Rheumatology, 46: 1015-1019, 2007, [3a].
6.
Heinz, C.; Mingels, A.; Goebel, C.; Fuchsluger, T.; and Heiligenhaus, A.: Chronic uveitis in children with and without juvenile idiopathic
arthritis: differences in patient characteristics and clinical course. J Rheumatol, 35: 1403-1407, 2008 [4a].
7.
Kotaniemi, K.; Savolainen, A.; Karma, A.; and Aho, K.: Recent advances in uveitis of juvenile idiopathic arthritis. Surv Ophthalmol, 48(5): 489502, 2003, [5b]
http://groups/p2/EBC_Files/Articles_Cited_in_EPIC_Ophth/OphthKotaniemi2003.pdf .
8.
Local Consensus: During recommendation development timeframe. [5] .
9.
Petty, R. E. et al.: International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision,
Edmonton, 2001. J Rheumatol, 31(2): 390-2, 2004, [5a]
http://groups/p2/EBC_Files/Articles_Cited_in_EPIC_Ophth/OphthPetty2004JIA.Criteria.pdf .
http://www.ncbi.nlm. nih.g ov/entrez/query. fcgi? cmd=Retrieve&d b=Pu bMed &do pt=Citation &list_uid s=144 9981 7
http://www.ncbi.nl m.nih .gov/entrez/ query.fcgi?cmd= Retrieve&db= PubMe d&dopt=Citatio n&lis t_uids=147 6081 2
10. Saurenmann, R.K.; Levin, A.V.; Feldman, B.M.; Laxer, R.M., Schneider, R.; and Silverman, E.D.: Risk factors of development of uveitis differ
between girls and boys with juvenile idiopathic arthritis. Athritis & Rheumatism, 62(6): 1824-1828, 2010, [4a].
11. Sim, K. T.; Venning, H. E.; Barrett, S.; Gregson, R. M.; and Amoaku, W. M.: Extended oligoarthritis and other risk factors for developing JIAassociated uveitis under ILAR classification and its implication for current screening guideline. Ocular Immunology & Inflammation, 14(6): 3537, 2006, [4a]
http://groups/p2/EBC_Files/Articles_Cited_in_EPIC_Ophth/OphthSim2006.pdf .
http://www.ncbi. nlm. nih.g ov/entrez/query. fcgi? cmd=Retrieve&d b=Pu bMed &do pt=Citation &list_uid s=171 6260 6
12. Woreta, F.; Thorne, J.E.; Jabs, D.A.; Kedhar, S.R.; and Dunn, J.P.: Risk factors for ocular complications and poor visual acuity at presentation
among patients with uveitis associated with juvenile idiopathic arthritis. Am J. Ophthamol, 143: 647-655, 2007, [4b].
Implementation
Applicability Issues:
Issues to consider with implementation of these recommendations include parental understanding of the complications
of uveitis and the need for prompt screening, rheumatology acceptance and follow-through with these
recommendations, and use of and follow-through of the recommendations by ophthalmologists. The ability to collect
the data may pose a challenge.
Relevant CCHMC Tools for Implementation:
Knowing Note: What you need to know about your eye exam
Copyright 2012 Cincinnati Children's Hospital Medical Center; all rights reserved.
Page 3 of 6
Rheumatology/Juvenile Idiopathic Arthritis (JIA)/Uveitis/BESt 011
Outcome or Process Measures:
Outcome Measures:
Of active patients seen by Pediatric Ophthalmology for JIA-associated screenings:
Percent who are within the recommended follow-up time period for uveitis screening
Percent whose uveitis is inactive or in remission
Percent with optimal visual acuity based on a non-verbal visual acuity exam
Percent with best corrected visual acuity of 20/20 or better
Percent whose uveitis is worsening
Process measure: Percentage of JIA patients screened for Uveitis (eye disease) at appropriate intervals
Complete operational definitions are on file.
SUPPORTING INFORMATION
Background/Purpose of BESt Development:
Juvenile idiopathic arthritis (JIA) is the most common systemic cause of pediatric uveitis in Europe and North America
(Cassidy 2006 [5a]).
Uveitis frequently associated with JIA and JIA associated uveitis, is commonly considered to have a complicated course
with frequent adverse visual outcomes (Carvounis 2006 [1a] (see Table 3 below: Number of patients with ocular complications due to
uveitis). Recent literature reports prevalence of uveitis among children with JIA in the range of 8.3% to 20.1% (Carvounis
2006 [1a], Grassi 2007 [4a], Saurenmann 2010 [4a], Sim 2006 [4a]). Although predictors for adverse visual outcome and severity in
JIA-associated uveitis have been identified there exists no model that predicts which patients will develop JIA associated
uveitis. It is reasonable and advisable to continue to subject children with JIA to frequent ophthalmological
examinations for early diagnosis of uveitis, although only a small proportion develop it (Carvounis 2006 [1a]). Visual
outcome has improved in the past 20 years; most children have a relatively good prognosis if the disorder is detected
and treated early. However, uveitis in children with JIA remains a leading cause of loss of vision and blindness in the
United States (Cassidy 2006 [5a]).
The purpose of this BESt is to provide clinicians that treat children with JIA reasonable and acceptable guidance for early
and consistent screening for uveitis. Scheduled slit-lamp examinations by an ophthalmologist at specific intervals can
detect ocular disease early, and prompt treatment can prevent vision loss (Cassidy 2006 [5a]).
Table 3: Number of patients with ocular complications due to uveitis
Posterior synechia
Cataract
Band-keratopathy
Vitreous opacities
Papille oedema
Secondary glaucoma
Macula oedema
Hypotony
Iris rubeosis
Other complications
Initial status (n=100)
n (%)
31 (31)
22 (22)
21 (21)
10 (10)
7 (7)
6 (6)
4 (4)
3 (3)
2 (2)
9 (9)
Current status (n=106)
n (%)
29 (27)
27 (26)
31 (29)
7 (7)
6 (6)
8 (8)
6 (6)
4 (4)
2 (2)
22 (21)
Heiligenhaus 2007 [3a])
Search Strategy
1. Initial Search performed 9-2011
DATABASES
- Scopus
- Pubmed
- OVID EBMR Review
- CINAHL OVID
Copyright 2012 Cincinnati Children's Hospital Medical Center; all rights reserved.
Page 4 of 6
Rheumatology/Juvenile Idiopathic Arthritis (JIA)/Uveitis/BESt 011
SEARCH TERMS & MeSH TERMS
- Scopus: Juvenile Idiopathic Arthritis and Uveitis and diagnosis
- Pubmed: Uveitis/diagnosis and Arthritis, Juvenile Rheumatoid and English and last 5 years
- OVID EMBR Review: ("Uveitis/diagnosis"[Mesh]) AND "Arthritis, Juvenile Rheumatoid"[Mesh] AND (English[lang] AND
"last 5 years"[PDat]) No results
- CINAHL: Arthritis, Juvenile Rheumatoid and Uveitis+/DI
- Children; human; English, (2006 to present)
WEBSITE SEARCH of all known ophthalmology related websites for guidelines related to JRA screening for uveitis
- National Guidelines Clearinghouse, American Academy of Pediatrics, American Academy of Ophthalmology, American
Academy of Pediatric Ophthalmology and Strabismus, American Board of Ophthalmology, Association for Research in
Vision and Ophthalmology, American Society of Retina Specialists, British Ophthalmic Anaesthesia Society, Ophthalmic
Imaging Association, Canadian Ophthalmological Society, German Ophthalmology Society, Ophthalmic Anesthesia
Society, Philippine Academy of Ophthalmology, Royal College of Ophthalmologists, Swedish Ophthalmological Society
Guidelines, Systematic Reviews, and Meta-Analyses (2006 to present)
2. Additional articles identified by clinicians
3. Additional articles identified from a search based on the strategy from the Carvounis systematic review was conducted for
publication dates subsequent to that review:
2005 to present
Ovid Medline, English, human
Search terms:
(Juvenile Arthritis OR JRA OR Juvenile Rheumatoid Arthritis OR Juvenile Chronic Arthritis OR JCA OR Juvenile Idiopathic
Arthritis OR JIA Arthritis)
AND
(Eye OR Ocular OR Eye Diseases OR Ophthalmic OR Ophthalmological OR Iritis OR Iridocyclitis OR Uveitis OR cataract OR
Glaucoma)
Group/Team Members:
Team Leader/Author: Janalee Taylor, MSN, RN-CNS, CNP, William S. Rowe, Division of Rheumatology
Team Members/Co-Authors: Hermine Brunner, MD- Professor, William S. Rowe, Division of Rheumatology; Jennifer Huggins, MD- Assistant
Professor, William S. Rowe, Division of Rheumatology; Sarah Lopper, OD- Instructor, Pediatric Ophthalmology Division
Pai-Ye Lu, MD- Clinical Fellow, William S. Rowe, Division of Rheumatology; Julie Ranz, RN- Registered Nurse II, William S. Rowe, Division of
Rheumatology; Jessica Sage, MPH- Project Specialist, William S. Rowe, Division of Rheumatology; Shweta Srivastava, BA- Clinical Research
Coordinator III, William S. Rowe, Division of Rheumatology; Patricia Vega-Fernandez, MD- Clinical Fellow, William S. Rowe, Division of
Rheumatology
Support/Consultant: Wendy Gerhardt, MSN, RN-BC- EBDM Program Administrator, Anderson Center for Health Systems Excellence
Danette Stanko-Lopp, MA, MPH, Research Associate- Anderson Center for Health Systems Excellence
Karen Vonderhaar, MS, RN - EBDM Program Administrator, Anderson Center for Health Systems Excellence
Conflicts of Interest were declared for each team member:
No financial conflicts of interest were found.
No external funding was received for development of this BESt.
Note: Full tables of evidence grading system available in separate document:
Table of Evidence Levels of Individual Studies by Domain, Study Design, & Quality (abbreviated table below)
Grading a Body of Evidence to Answer a Clinical Question
Judging the Strength of a Recommendation (abbreviated table below, dimensions table above)
Table of Evidence Levels (see note above)
Quality level Definition
1a or 1b
Systematic review, meta-analysis, or meta-synthesis of multiple studies
2a or 2b
Best study design for domain
3a or 3b
Fair study design for domain
4a or 4b
Weak study design for domain
General review, expert opinion, case report, consensus report, or
5a or 5b
guideline
5
Local Consensus
a = good quality study; b = lesser quality study
Copyright 2012 Cincinnati Children's Hospital Medical Center; all rights reserved.
Page 5 of 6
Rheumatology/Juvenile Idiopathic Arthritis (JIA)/Uveitis/BESt 011
Table of Language and Definitions for Recommendation Strength (see note above):
Language for Strength
It is strongly recommended that
It is strongly recommended that not
Definition
When the dimensions for judging the strength of the evidence are applied,
there is high support that benefits clearly outweigh risks and burdens.
(or visa-versa for negative recommendations)
It is recommended that
When the dimensions for judging the strength of the evidence are applied,
It is recommended that not
there is moderate support that benefits are closely balanced with risks and burdens.
There is insufficient evidence and a lack of consensus to make a recommendation
Given the dimensions below and that more answers to the left of the scales indicate support for a stronger recommendation, the
recommendation statement above reflects the strength of the recommendation as judged by the development group.
(Note that for negative recommendations, the left/right logic may be reversed for one or more dimensions.)
1. Grade of the Body of Evidence
High
Moderate
Low
Minimal
Moderate
Serious
Moderate
Minimal
Comments:
2. Safety/Harm (Side Effects and Risks)
Comments: Screening is of little harm as compared to the complications that can occur
3. Health benefit to patient
Significant
Comments: Minimizing complications that have life altering consequences would be of significance to patients and families
4. Burden on patient to adhere to recommendation
Low
Unable to determine
High
Comments: The frequency of ophthalmologic screening needs be weighed against risk of developing uveitis. Early identification of uveitis
allows prompt initiation of treatment (Kotaniemi 2003 [5b]).
5. Cost-effectiveness to healthcare system
Cost-effective
Inconclusive
Not cost-effective
Comments: Preventing or minimizing complications is cost effective compared to treatment of uveitis and complications
6. Directness of the evidence for this target
population
Directly relates
Some concern of
directness
Indirectly relates
High
Medium
Low
Comments:
7. Impact on morbidity/mortality or quality of life
Comments: Living without complications or prolonging the development of complications has high impact on these patients quality of life
Copies of this Best Evidence Statement (BESt) and related tools (if applicable, e.g., screening tools, algorithms, etc.) are available online and may be
distributed by any organization for the global purpose of improving child health outcomes.
Website address: http://www.cincinnatichildrens.org/svc/alpha/h/health-policy/best.htm
Examples of approved uses of the BESt include the following:
copies may be provided to anyone involved in the organizations process for developing and implementing evidence based care;
hyperlinks to the CCHMC website may be placed on the organizations website;
the BESt may be adopted or adapted for use within the organization, provided that CCHMC receives appropriate attribution on all written or
electronic documents; and
copies may be provided to patients and the clinicians who manage their care.
Notification of CCHMC at EBDMinfo@cchmc.org for any BESt adopted, adapted, implemented, or hyperlinked by the organization is appreciated.
Please cite as: Cincinnati Children's Hospital Medical Center: Best Evidence Statement: Screening for Uveitis in Children with Juvenile Idiopathic
Arthritis (JIA), http://www.cincinnatichildrens.org/svc/alpha/h/health-policy/best.htm, BESt 011, pages 1-6, June 18, 2012.
This Best Evidence Statement has been reviewed against quality criteria by 2 independent reviewers from the CCHMC Evidence Collaboration.
For more information about CCHMC Best Evidence Statements and the development process, contact the
Evidence Collaboration at EBDMinfo@cchmc.org.
Note
This Best Evidence Statement addresses only key points of care for the target population; it is not intended to be a comprehensive practice
guideline. These recommendations result from review of literature and practices current at the time of their formulation. This Best Evidence
Statement does not preclude using care modalities proven efficacious in studies published subsequent to the current revision of this document.
This document is not intended to impose standards of care preventing selective variances from the recommendations to meet the specific and
unique requirements of individual patients. Adherence to this Statement is voluntary. The clinician in light of the individual circumstances
presented by the patient must make the ultimate judgment regarding the priority of any specific procedure.
Copyright 2012 Cincinnati Children's Hospital Medical Center; all rights reserved.
Page 6 of 6
You might also like
- Clinical Updates in Rheumatoid Arthritis: New Strategies to Target Remission and Individualize Comprehensive CareFrom EverandClinical Updates in Rheumatoid Arthritis: New Strategies to Target Remission and Individualize Comprehensive CareNo ratings yet
- Juvenileidiopathicarthritis: Oligoarthritis and PolyarthritisDocument18 pagesJuvenileidiopathicarthritis: Oligoarthritis and PolyarthritiskenmitaNo ratings yet
- Juvenile Idiopathic Arthritis: An Update On PharmacotherapyDocument13 pagesJuvenile Idiopathic Arthritis: An Update On PharmacotherapyRahmi SilviyaniNo ratings yet
- Arthritis Juvenile Idiopathic ArthritisDocument6 pagesArthritis Juvenile Idiopathic ArthritismkyousufNo ratings yet
- Idiopathic Arthritis: JuvenileDocument13 pagesIdiopathic Arthritis: JuvenileHarry Rahmad S ChaniagoNo ratings yet
- The Changing Epidemiology of Acute and Subacute Haematogenous Osteomyelitis in ChildrenDocument4 pagesThe Changing Epidemiology of Acute and Subacute Haematogenous Osteomyelitis in ChildrenYudha FebrianNo ratings yet
- Subtype Patterns of Juvenile Idiopathic Arthritis Among Libyan ChildrenDocument6 pagesSubtype Patterns of Juvenile Idiopathic Arthritis Among Libyan ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Endocarditis PreventieDocument12 pagesEndocarditis PreventieLaura AmaliaNo ratings yet
- Prevention of Surgical Site Infections in Orthopaedic Surgery: A Synthesis of Current RecommendationsDocument16 pagesPrevention of Surgical Site Infections in Orthopaedic Surgery: A Synthesis of Current RecommendationsPankaj VatsaNo ratings yet
- Fitzgerald 2019Document10 pagesFitzgerald 2019senkonenNo ratings yet
- Alsubiaee Et Al 2016, The Effect of Vit D Suppl in Patients With Knee OADocument3 pagesAlsubiaee Et Al 2016, The Effect of Vit D Suppl in Patients With Knee OAedo adimastaNo ratings yet
- Geriatrics: Acute Appendicitis in The Elderly: A Literature Review On An Increasingly Frequent Surgical ProblemDocument8 pagesGeriatrics: Acute Appendicitis in The Elderly: A Literature Review On An Increasingly Frequent Surgical ProblemCRISTHIAN CASTILLO JIBAJANo ratings yet
- Gout and The Risk of Epilepsy A Population Based.44Document6 pagesGout and The Risk of Epilepsy A Population Based.44Afni Panggar BesiNo ratings yet
- 77d8 PDFDocument7 pages77d8 PDFRosyid PrasetyoNo ratings yet
- Olfu Finals BSN ReviewerDocument101 pagesOlfu Finals BSN ReviewerEdnalyn QuimboNo ratings yet
- Research Article 'S Disease: Severity of Ocular: Vision-Threatening Behcet Involvement PredictorsDocument7 pagesResearch Article 'S Disease: Severity of Ocular: Vision-Threatening Behcet Involvement PredictorsdeswitrigintaNo ratings yet
- Rhumatologie-Pediatrique FRDocument4 pagesRhumatologie-Pediatrique FRCaity YoungNo ratings yet
- Edlow 2018Document15 pagesEdlow 2018arianaNo ratings yet
- 2018 Article 2834Document11 pages2018 Article 2834mitroisergiuNo ratings yet
- Sepsis Abdominal ScoreDocument8 pagesSepsis Abdominal ScoreMaria Ocotlan Gonzalez herreraNo ratings yet
- Characterisation of Uveitis in Patients With Psoriatic ArthritisDocument4 pagesCharacterisation of Uveitis in Patients With Psoriatic ArthritisMdl WankharakorNo ratings yet
- Juvenile Idiopathic Arthritis: Jennifer E. Weiss, MD, Norman T. Ilowite, MDDocument30 pagesJuvenile Idiopathic Arthritis: Jennifer E. Weiss, MD, Norman T. Ilowite, MDAngela SmartNo ratings yet
- EBM Fara Nadya 1102018330Document11 pagesEBM Fara Nadya 1102018330Fara NadyaNo ratings yet
- Characteristics of Uveitis Presenting For The First Time in The Elderly Analysis of 91 Patients in A Tertiary CenterDocument9 pagesCharacteristics of Uveitis Presenting For The First Time in The Elderly Analysis of 91 Patients in A Tertiary CenterFrancescFranquesaNo ratings yet
- Rheumatology 2008Document3 pagesRheumatology 2008Thelma Cantillo RochaNo ratings yet
- Epsom SaltDocument48 pagesEpsom SaltSathya Palanisamy100% (1)
- Análisis Crítico de Un Artículo: Antibióticos en Otitis Media Aguda, ¿Son Necesarios?, ¿Existe Algún Subgrupo Que Se Beneficia?Document6 pagesAnálisis Crítico de Un Artículo: Antibióticos en Otitis Media Aguda, ¿Son Necesarios?, ¿Existe Algún Subgrupo Que Se Beneficia?Orlando Isaac Bayona AlvaradoNo ratings yet
- The Relationship Between Statin Use and Open-Angle GlaucomaDocument8 pagesThe Relationship Between Statin Use and Open-Angle GlaucomaFahima AlbaarNo ratings yet
- Behcet DiseaseDocument6 pagesBehcet DiseasejbahalkehNo ratings yet
- Impact of Diabetic Foot and Others Comorbidities On The Quality of Life of Diabetic Patients Monitored at A Specialized Outpatient ClinicDocument10 pagesImpact of Diabetic Foot and Others Comorbidities On The Quality of Life of Diabetic Patients Monitored at A Specialized Outpatient ClinicAyu SudiantariNo ratings yet
- Acute Osteomyelitis in Children Journal Radiology PDFDocument15 pagesAcute Osteomyelitis in Children Journal Radiology PDFRegi ShabaraNo ratings yet
- Juvenile Idiopathic ArthritisDocument6 pagesJuvenile Idiopathic ArthritissitharNo ratings yet
- Cardiovascular and Hematologic Disorders in ChildrenDocument5 pagesCardiovascular and Hematologic Disorders in ChildrenDeekayNo ratings yet
- Physical Therapy Intervention Studies On Idiopathic Scoliosis-Review With The Focus On Inclusion Criteria1Document12 pagesPhysical Therapy Intervention Studies On Idiopathic Scoliosis-Review With The Focus On Inclusion Criteria1mostafa mahmoudNo ratings yet
- Rheumatic Manifestations of Inflammatory Bowel Diseases: A Study From The Middle EastDocument11 pagesRheumatic Manifestations of Inflammatory Bowel Diseases: A Study From The Middle EastAndreiMunteanuNo ratings yet
- Preseptal and Orbital Cellulitis: A 10-Year Review of Hospitalized PatientsDocument8 pagesPreseptal and Orbital Cellulitis: A 10-Year Review of Hospitalized PatientsApril MitchellNo ratings yet
- Prospective Cohort StudyDocument6 pagesProspective Cohort StudyMãnoj MaheshwariNo ratings yet
- Anemia and Periodontitis: An Enigma?: Dr. Soumya. K. Nair, Dr. Mohamed Faizuddin, Dr. Jayanthi.D.,M.D.SDocument8 pagesAnemia and Periodontitis: An Enigma?: Dr. Soumya. K. Nair, Dr. Mohamed Faizuddin, Dr. Jayanthi.D.,M.D.SNovie ApriantiNo ratings yet
- Association Between Periodontitis and Glycosylated HaemoglobinDocument11 pagesAssociation Between Periodontitis and Glycosylated HaemoglobinAndrea MorenoNo ratings yet
- Efficacy and Safety of Subconjunctival Bevacizumab For Recurrent PterygiumDocument4 pagesEfficacy and Safety of Subconjunctival Bevacizumab For Recurrent PterygiummayangestowoNo ratings yet
- A Clinical Study of Anterior Uveitis in A Rural Hospital: DR - Anitha.S.Maiya, DR - Sundip ShenoyDocument5 pagesA Clinical Study of Anterior Uveitis in A Rural Hospital: DR - Anitha.S.Maiya, DR - Sundip ShenoyTri BasukiNo ratings yet
- Ulcera PepticaDocument8 pagesUlcera PepticaLiz Espinoza ZambranoNo ratings yet
- Access From The University of Nottingham Repository:: For More Information, Please ContactDocument12 pagesAccess From The University of Nottingham Repository:: For More Information, Please ContactDhiaul IzzahNo ratings yet
- Bacterial Etiology of Pediatric Subacute Hematogenous OsteomyelitisDocument6 pagesBacterial Etiology of Pediatric Subacute Hematogenous OsteomyelitismiNo ratings yet
- Physical Therapy For Adolescents With Idiopathic Scoliosis: Josette Bettany-Saltikov Et AlDocument39 pagesPhysical Therapy For Adolescents With Idiopathic Scoliosis: Josette Bettany-Saltikov Et AlnuyerryNo ratings yet
- ResearchDocument3 pagesResearchDr Sreeja KSNo ratings yet
- 2022 ITECritiqueDocument80 pages2022 ITECritiqueJon LetkoNo ratings yet
- Tocilizumab Employment in The Treatment of Resistant Juvenile Idiopathic Arthritis Associated UveitisDocument8 pagesTocilizumab Employment in The Treatment of Resistant Juvenile Idiopathic Arthritis Associated UveitisDavid Martínez MartínezNo ratings yet
- JURNALDocument6 pagesJURNALRemaja IslamNo ratings yet
- Foot Ulcers in The Diabetic Patient, Prevention and TreatmentDocument12 pagesFoot Ulcers in The Diabetic Patient, Prevention and TreatmentAndriawan BramNo ratings yet
- Prevalence of Statin Intolerance: A Meta-AnalysisDocument16 pagesPrevalence of Statin Intolerance: A Meta-Analysisalejandro montesNo ratings yet
- ACG Clinical Guideline: Management of Acute PancreatitisDocument8 pagesACG Clinical Guideline: Management of Acute PancreatitisNick ANo ratings yet
- Nursing VIVA FinalDocument9 pagesNursing VIVA FinalzakiatalhaNo ratings yet
- Jurnal THTDocument27 pagesJurnal THTAnonymous emqfcjJNo ratings yet
- Pi Is 0016508520300184Document12 pagesPi Is 0016508520300184ntnquynhproNo ratings yet
- Efficacy of Antiresorptive Treatment in Osteoporotic Older Adults: A Systematic Review and Meta-Analysis of Randomized Clinical TrialDocument8 pagesEfficacy of Antiresorptive Treatment in Osteoporotic Older Adults: A Systematic Review and Meta-Analysis of Randomized Clinical TrialBernardo Abel Cedeño VelozNo ratings yet
- NIH Public Access: Author ManuscriptDocument16 pagesNIH Public Access: Author Manuscriptgonzalo_acosta_6No ratings yet
- NIH Public Access: Author ManuscriptDocument22 pagesNIH Public Access: Author ManuscriptLia MirawatiNo ratings yet
- Sigmoid DiverculitisDocument7 pagesSigmoid DiverculitisArif Nurmansyah SNo ratings yet
- Risk Factors of Deep Vein Thrombosis (DVT) After Total Knee Arthroplasty (Tka) at Phramongkutklao HospitalDocument7 pagesRisk Factors of Deep Vein Thrombosis (DVT) After Total Knee Arthroplasty (Tka) at Phramongkutklao HospitalM IqbalNo ratings yet
- Formula FeedingDocument20 pagesFormula FeedingFungky AnthonyNo ratings yet
- How To Prepare Formula For: Bottle-Feeding at HomeDocument12 pagesHow To Prepare Formula For: Bottle-Feeding at HomeGloria PutrianitaNo ratings yet
- Handbook: For Clinical Management of DengueDocument124 pagesHandbook: For Clinical Management of DengueraattaiNo ratings yet
- Recommendation WHODocument176 pagesRecommendation WHODananjaya JuniorNo ratings yet
- Pediatric Eye EvaluationsDocument49 pagesPediatric Eye EvaluationsFungky AnthonyNo ratings yet
- Relapsing FeverDocument6 pagesRelapsing FeverFungky AnthonyNo ratings yet
- Pediatrics 2014 Ralston E1474 502Document32 pagesPediatrics 2014 Ralston E1474 502Juwita PratiwiNo ratings yet
- Soy Protein-Based Formulas in InfantDocument9 pagesSoy Protein-Based Formulas in InfantFungky AnthonyNo ratings yet
- 2011 ITP Pocket GuideDocument8 pages2011 ITP Pocket GuidevtNo ratings yet
- Headache in The Elderly PDFDocument6 pagesHeadache in The Elderly PDFFungky Anthony100% (1)
- CPD Article on Anxiety Disorders in Family PracticeDocument3 pagesCPD Article on Anxiety Disorders in Family PracticeFungky AnthonyNo ratings yet
- WHO Neuroscience of Psychoactive Substance Use and DependenceDocument286 pagesWHO Neuroscience of Psychoactive Substance Use and Dependencemihai corciovaNo ratings yet
- Behavsci 05 00496 v2Document22 pagesBehavsci 05 00496 v2Fungky AnthonyNo ratings yet
- Jogc PDFDocument32 pagesJogc PDFnunki aprillitaNo ratings yet
- Diabetic RetinopathyDocument65 pagesDiabetic RetinopathyFungky AnthonyNo ratings yet
- FIGO Clasificación HUA 2011Document11 pagesFIGO Clasificación HUA 2011dickenskevinNo ratings yet
- Infant Formula: NINA R. O'CONNOR, MD, Chestnut Hill Family Practice Residency, Philadelphia, PennslyvaniaDocument6 pagesInfant Formula: NINA R. O'CONNOR, MD, Chestnut Hill Family Practice Residency, Philadelphia, PennslyvaniaFungky AnthonyNo ratings yet
- Sore Throat and Tonsillitis (2007)Document7 pagesSore Throat and Tonsillitis (2007)Fungky AnthonyNo ratings yet
- Drug Safety AlertDocument92 pagesDrug Safety AlertFungky AnthonyNo ratings yet
- Diagnosis and Treatment of Otitis MediaDocument9 pagesDiagnosis and Treatment of Otitis MediaFungky AnthonyNo ratings yet
- Diah - KEBIJAKAN DAN STRATEGI NAPZA-in English PDFDocument22 pagesDiah - KEBIJAKAN DAN STRATEGI NAPZA-in English PDFFungky AnthonyNo ratings yet
- Obstructive Sleep Apnea: PrevalenceDocument4 pagesObstructive Sleep Apnea: Prevalencemurdalin100% (1)
- Pocket Guide To Antimicrobial Therapy in Otolaryngology - Head and Neck Surgery 13th EditionDocument115 pagesPocket Guide To Antimicrobial Therapy in Otolaryngology - Head and Neck Surgery 13th EditionFecky Fihayatul IchsanNo ratings yet
- Cholesteatoma (Prof. Mokhtar Bassiouny)Document15 pagesCholesteatoma (Prof. Mokhtar Bassiouny)Fungky AnthonyNo ratings yet
- Pocket Guide To Antimicrobial Therapy in Otolaryngology - Head and Neck Surgery 13th EditionDocument115 pagesPocket Guide To Antimicrobial Therapy in Otolaryngology - Head and Neck Surgery 13th EditionFecky Fihayatul IchsanNo ratings yet
- McWilliams Intracranial HemorrhageDocument49 pagesMcWilliams Intracranial HemorrhageFungky AnthonyNo ratings yet
- Diagnosis and Management of Headache in Adults PDFDocument88 pagesDiagnosis and Management of Headache in Adults PDFFungky AnthonyNo ratings yet
- AAO HNS - TinnitusDocument40 pagesAAO HNS - TinnitusFungky AnthonyNo ratings yet
- AAO HNSF Allergic Rhinitis 2015Document43 pagesAAO HNSF Allergic Rhinitis 2015Fungky AnthonyNo ratings yet
- Diagnosis and Management of SpADocument65 pagesDiagnosis and Management of SpAishaan kharbandaNo ratings yet
- Spondiloartritis Diagnosis 2017 222234456Document40 pagesSpondiloartritis Diagnosis 2017 222234456Alexandra BalanNo ratings yet
- Hla B 27 SopDocument12 pagesHla B 27 SopRajeev PareekNo ratings yet
- Spondyloarthritis ResidentDocument70 pagesSpondyloarthritis Residentviraaj pawar100% (1)
- Spine Inflammation Causes Pain and StiffnessDocument18 pagesSpine Inflammation Causes Pain and StiffnessIzni Fatihah100% (1)
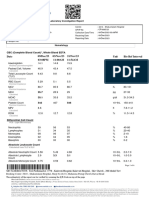
- DR Lal Pathlabs: LPL - Lpl-Rohini (National Reference Lab) Sector - 18, Block - E Rohini Delhi 110085Document2 pagesDR Lal Pathlabs: LPL - Lpl-Rohini (National Reference Lab) Sector - 18, Block - E Rohini Delhi 110085Vivek PatelNo ratings yet
- SpondyloarthritisDocument17 pagesSpondyloarthritisla_vayettezNo ratings yet
- Seminar: Joachim Sieper, Denis PoddubnyyDocument12 pagesSeminar: Joachim Sieper, Denis PoddubnyyDaniel FernandezNo ratings yet
- DR Adrian Jones - Seronegative SpondyloarthropathiesDocument38 pagesDR Adrian Jones - Seronegative SpondyloarthropathiesMaryam ShahbazNo ratings yet
- Hla B27Document5 pagesHla B27Madhu Kunchi100% (1)
- Dreams e Homoeo - 10th IssueDocument5 pagesDreams e Homoeo - 10th IssueSaurav AroraNo ratings yet
- 4ndzvyovxipmju1rfmhykayfDocument3 pages4ndzvyovxipmju1rfmhykayfKunal GuptaNo ratings yet
- Hypopyon UveitisDocument18 pagesHypopyon UveitisjochigNo ratings yet
- Radiologia in Spondilita AnchilozantaDocument18 pagesRadiologia in Spondilita AnchilozantaMarina ApostolNo ratings yet
- Max2report PrintDocument6 pagesMax2report Printdevender0yadavNo ratings yet
- 233-Article Text-355-1-10-20200213Document17 pages233-Article Text-355-1-10-20200213Kristina ParasNo ratings yet
- Poligen & MultifaktorDocument49 pagesPoligen & MultifaktorLovina Falendini AndriNo ratings yet
- Himanshu EdtedDocument6 pagesHimanshu Edteddevender0yadavNo ratings yet
- Lec 2 Seronegative Spondarthritis (Slides)Document66 pagesLec 2 Seronegative Spondarthritis (Slides)amereNo ratings yet
- Functional Medicine Resolves Rheumatoid Arthritis and Hormone IssuesDocument85 pagesFunctional Medicine Resolves Rheumatoid Arthritis and Hormone Issueslamag100% (1)
- Anesthetic Considerations in Patients Posted For Surgery With Ankylosing SpondylitisDocument43 pagesAnesthetic Considerations in Patients Posted For Surgery With Ankylosing Spondylitisanuk_1129No ratings yet
- 1998 Does Knuckle Cracking Lead To Arthritis of The Fingers PDFDocument2 pages1998 Does Knuckle Cracking Lead To Arthritis of The Fingers PDFMatías RamírezNo ratings yet
- Ankylosing SpondylitisDocument12 pagesAnkylosing SpondylitisAnnette ChavezNo ratings yet
- S94 - Harish Kumar Rao Manav Chowk Cc-Sahyogi Juneja Towers, 716, Rattangarh Road, Manav Chowk, Ambala CITY, PH-9996006678Document3 pagesS94 - Harish Kumar Rao Manav Chowk Cc-Sahyogi Juneja Towers, 716, Rattangarh Road, Manav Chowk, Ambala CITY, PH-9996006678EduNo ratings yet
- Spondyloarthritides: Key Facts about Ankylosing Spondylitis, Psoriatic Arthritis and HLA-B27Document125 pagesSpondyloarthritides: Key Facts about Ankylosing Spondylitis, Psoriatic Arthritis and HLA-B27Fazal Dalal100% (1)
- Zhong 2020Document25 pagesZhong 20202456708893No ratings yet
- SpondyloarthritisDocument77 pagesSpondyloarthritisRapid MedicineNo ratings yet
- Ankylosing SpondylitesDocument16 pagesAnkylosing SpondylitesJyotirmayeeNo ratings yet
- Chapter 65:: Psoriatic Arthritis and Reactive Arthritis:: Ana-Maria Orbai & John A. FlynnDocument12 pagesChapter 65:: Psoriatic Arthritis and Reactive Arthritis:: Ana-Maria Orbai & John A. FlynnDeb100% (1)