Professional Documents
Culture Documents
Van Os 2016 BMJ 'Schizophrenia' Does Not Exist
Uploaded by
hselageaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Van Os 2016 BMJ 'Schizophrenia' Does Not Exist
Uploaded by
hselageaCopyright:
Available Formats
BMJ 2016;352:i375 doi: 10.1136/bmj.
i375 (Published 2 February 2016)
Page 1 of 2
Views & Reviews
VIEWS & REVIEWS
PERSONAL VIEW
Schizophrenia does not exist
Disease classifications should drop this unhelpful description of symptoms
Jim van Os full professor and chair, Department of Psychiatry and Psychology, Maastricht University
Medical Centre, PO Box 616, 6200 MD Maastricht, Netherlands
In March 2015 a group of academics, patients, and relatives
published an opinion piece in a national newspaper in the
Netherlands, proposing that we drop the essentially contested1
term schizophrenia, with its connotation of hopeless chronic
brain disease, and replace it with something like psychosis
spectrum syndrome.2
We launched two websites (www.schizofreniebestaatniet.nl/
english/ and www.psychosenet.nl) aimed at informing the public
about the nature of psychotic illness and helping patients deal
with pervasive, unscientifically pessimistic, organic views of
their symptoms. The timing was no coincidence.
Several recent papers by different authors have called for
modernised psychiatric nomenclature, particularly regarding
the term schizophrenia.3-6 Japan and South Korea have already
abandoned this term.
Current classifications
The classification of mental disorders, as laid down in ICD-10
(International Classification of Diseases, 10th revision) and
DSM-5 (Diagnostic and Statistical Manual of Mental Disorders,
fifth edition), is complicated, particularly psychotic illness.
Currently, psychotic illness is classified among myriad
categories, including schizophrenia, schizophreniform disorder,
schizoaffective disorder, delusional disorder, brief psychotic
disorder, depression/bipolar disorder with psychotic features,
substance induced psychotic disorder, and psychotic disorder
not otherwise classified. Categories such as these do not
represent diagnoses of discrete diseases, because these remain
unknown; rather, they describe how symptoms can cluster, to
allow grouping of patients.
This elegant solution allows clinicians to say, for example, You
have symptoms of psychosis and mania, and we classify that
as schizoaffective disorder. If your psychotic symptoms
disappear we may reclassify it as bipolar disorder. If, on the
other hand, your mania symptoms disappear and your psychosis
becomes chronic, we may re-diagnose it as schizophrenia.
That is how our classification system works. We dont know
enough to diagnose real diseases, so we use a system of
symptom based classification. The DSM-5 does this differently
than ICD-10but that does not matter, because its only a
classification.
If everybody agreed to use the terminology in ICD-10 and
DSM-5 in this fashion, there would be no problem. However,
this is not what is generally communicated, particularly
regarding the most important category of psychotic illness:
schizophrenia.
The American Psychiatric Association, which publishes the
DSM, on its website describes schizophrenia as a chronic brain
disorder, and academic journals describe it as a debilitating
neurological disorder,7 a devastating, highly heritable brain
disorder,8 or a brain disorder with predominantly genetic risk
factors.9
Current language suggests discrete
disease
This language is highly suggestive of a distinct, genetic brain
disease. Strangely, no such language is used for other categories
of psychotic illness (schizophreniform disorder, schizoaffective
disorder, delusional disorder, brief psychotic disorder, and so
on). In fact, even though they constitute 70% of psychotic illness
morbidity (only 30% of people with psychotic illness have
symptoms that meet the criteria for schizophrenia),10 these other
categories tend be ignored in the academic literature (see box)
and on websites of professional bodies. They are certainly not
referred to as brain disorders or similar. Its as if they dont
exist.
What remains is the paradox that 30% of psychotic illness
morbidity is portrayed as a discrete brain disease; the other 70%
of the morbidity is communicated only in classification manuals.
Psychosis susceptibility syndrome
Scientific evidence indicates that the different psychotic
categories can be viewed as part of the same spectrum syndrome,
with a lifetime prevalence of 3.5%,10 of which schizophrenia
represents the minority (less than a third) with the poorest
outcome, on average. However, people with this psychosis
spectrum syndromeor, as patients have recently suggested,
vanosj@gmail.com
For personal use only: See rights and reprints http://www.bmj.com/permissions
Subscribe: http://www.bmj.com/subscribe
BMJ 2016;352:i375 doi: 10.1136/bmj.i375 (Published 2 February 2016)
Page 2 of 2
VIEWS & REVIEWS
psychosis susceptibility syndrome6display extreme
heterogeneity, both between and within people, in
psychopathology, treatment response, and outcome.
The best way to inform the public and provide patients with
diagnoses, therefore, is to forget about devastating
schizophrenia as the only category that matters and start doing
justice to the broad and heterogeneous psychosis spectrum
syndrome that really exists.
ICD-11 should remove the term schizophrenia.
Competing interests: I have read and understood the BMJ policy on
declaration of interests and declare the following interests: in the past
five years, the Maastricht University psychiatric research fund that I
manage has received unrestricted investigator led research grants or
recompense for presenting research from Servier, Janssen-Cilag, and
Lundbeck, companies that have an interest in the treatment of psychosis.
Provenance and peer review: Not commissioned; externally peer
reviewed.
For personal use only: See rights and reprints http://www.bmj.com/permissions
1
2
3
4
5
6
7
8
9
10
Geekie J, Read J. Making sense of madness: contesting the meaning of schizophrenia.
Routledge, 2009.
Van Os J, Boevink W, Van der Gaag RJ, et al. Laten we de diagnose schizofrenie vergeten
[Lets forget about the diagnosis of schizophrenia]. NRC Handelsblad 2015 Mar 7. www.
chapeau-woonkringen.nl/documenten/artikelen/150307_NRC_Jim_van_Os.pdf. (In Dutch.)
Henderson S, Malhi GS. Swan song for schizophrenia? Aust N Z J Psychiatry
2014;48:302-5.
Lasalvia A, Penta E, Sartorius N, Henderson S. Should the label schizophrenia be
abandoned? Schizophr Res 2015;162:276-84.
Moncrieff J, Middleton H. Schizophrenia: a critical psychiatry perspective. Curr Opin
Psychiatry 2015;28:264-8.
George B, Klijn A. A modern name for schizophrenia (PSS) would diminish self-stigma.
Psychol Med 2013;43:1555-7.
Brennand KJ, Simone A, Jou J, et al. Modelling schizophrenia using human induced
pluripotent stem cells. Nature 2011;473:221-5.
Esslinger C, Walter H, Kirsch P, et al. Neural mechanisms of a genome-wide supported
psychosis variant. Science 2009;324:605.
Goldman AL, Pezawas L, Mattay VS, et al. Widespread reductions of cortical thickness
in schizophrenia and spectrum disorders and evidence of heritability. Arch Gen Psychiatry
2009;66:467-77.
Perala J, Suvisaari J, Saarni SI, et al. Lifetime prevalence of psychotic and bipolar I
disorders in a general population. Arch Gen Psychiatry 2007;64:19-28.
Cite this as: BMJ 2016;352:i375
BMJ Publishing Group Ltd 2016
Subscribe: http://www.bmj.com/subscribe
BMJ 2016;352:i375 doi: 10.1136/bmj.i375 (Published 2 February 2016)
Page 3 of 2
VIEWS & REVIEWS
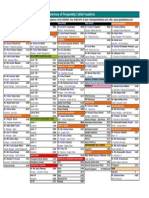
Number of PubMed hits with specific diagnostic categories in the title (November 2015)
Schizophrenia: 51 675
Schizoaffective disorder: 1170
Schizophreniform disorder: 216
Delusional disorder: 212
Brief psychotic disorder: 17
Psychotic disorder (not otherwise specified): 5
Bipolar disorder with psychotic features: 1201
Depression with psychotic features: 409
Substance induced psychotic disorder: 28
For personal use only: See rights and reprints http://www.bmj.com/permissions
Subscribe: http://www.bmj.com/subscribe
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Life Overseas 7 ThesisDocument20 pagesLife Overseas 7 ThesisRene Jr MalangNo ratings yet
- Quiz EmbryologyDocument41 pagesQuiz EmbryologyMedShare90% (67)
- fLOW CHART FOR WORKER'S ENTRYDocument2 pagesfLOW CHART FOR WORKER'S ENTRYshamshad ahamedNo ratings yet
- Farid Jafarov ENG Project FinanceDocument27 pagesFarid Jafarov ENG Project FinanceSky walkingNo ratings yet
- Nicenstripy Gardening Risk AssessmentDocument38 pagesNicenstripy Gardening Risk AssessmentVirta Nisa100% (1)
- Laboratorio 1Document6 pagesLaboratorio 1Marlon DiazNo ratings yet
- FinalsDocument8 pagesFinalsDumpNo ratings yet
- UNICESS KR Consmetics Maeteria Nunssupjara 01apr23Document44 pagesUNICESS KR Consmetics Maeteria Nunssupjara 01apr23ZB ChuaNo ratings yet
- Tutorial 7: Electromagnetic Induction MARCH 2015: Phy 150 (Electricity and Magnetism)Document3 pagesTutorial 7: Electromagnetic Induction MARCH 2015: Phy 150 (Electricity and Magnetism)NOR SYAZLIANA ROS AZAHARNo ratings yet
- Impact of Energy Consumption On The EnvironmentDocument9 pagesImpact of Energy Consumption On The Environmentadawiyah sofiNo ratings yet
- Apc 8x Install Config Guide - rn0 - LT - enDocument162 pagesApc 8x Install Config Guide - rn0 - LT - enOney Enrique Mendez MercadoNo ratings yet
- How To Practice Self Care - WikiHowDocument7 pagesHow To Practice Self Care - WikiHowВасе АнѓелескиNo ratings yet
- Maximizing Oredrive Development at Khoemacau MineDocument54 pagesMaximizing Oredrive Development at Khoemacau MineModisa SibungaNo ratings yet
- Introduction To Animal Science For Plant ScienceDocument63 pagesIntroduction To Animal Science For Plant ScienceJack OlanoNo ratings yet
- Schneider Electric PowerPact H-, J-, and L-Frame Circuit Breakers PDFDocument3 pagesSchneider Electric PowerPact H-, J-, and L-Frame Circuit Breakers PDFAnonymous dH3DIEtzNo ratings yet
- Ucg200 12Document3 pagesUcg200 12ArielNo ratings yet
- Cap 716 PDFDocument150 pagesCap 716 PDFjanhaviNo ratings yet
- Insurance Principles, Types and Industry in IndiaDocument10 pagesInsurance Principles, Types and Industry in IndiaAroop PalNo ratings yet
- Iso 28000Document11 pagesIso 28000Aida FatmawatiNo ratings yet
- MEDICO-LEGAL ASPECTS OF ASPHYXIADocument76 pagesMEDICO-LEGAL ASPECTS OF ASPHYXIAAl Giorgio SyNo ratings yet
- RHS NCRPO COVID FormDocument1 pageRHS NCRPO COVID Formspd pgsNo ratings yet
- Q1 Tle 4 (Ict)Document34 pagesQ1 Tle 4 (Ict)Jake Role GusiNo ratings yet
- 2020-11 HBG Digital EditionDocument116 pages2020-11 HBG Digital EditionHawaii Beverage GuideNo ratings yet
- A&P 2 - Digestive System Flashcards - QuizletDocument1 pageA&P 2 - Digestive System Flashcards - QuizletMunachande KanondoNo ratings yet
- Funds Flow Statement ExplainedDocument76 pagesFunds Flow Statement Explainedthella deva prasad0% (1)
- Model Fs CatalogDocument4 pagesModel Fs CatalogThomas StempienNo ratings yet
- WSAWLD002Document29 pagesWSAWLD002Nc BeanNo ratings yet
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocument1 pageDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoNo ratings yet
- M-LVDT: Microminiature Displacement SensorDocument2 pagesM-LVDT: Microminiature Displacement Sensormahdi mohammadiNo ratings yet
- Dip Obst (SA) Past Papers - 2020 1st Semester 1-6-2023Document1 pageDip Obst (SA) Past Papers - 2020 1st Semester 1-6-2023Neo Latoya MadunaNo ratings yet