Professional Documents
Culture Documents
HSG Vs Sonohysterography
Uploaded by
#15Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HSG Vs Sonohysterography
Uploaded by
#15Copyright:
Available Formats
SCIENTIFIC PAPER
Hysterosalpingography Versus Sonohysterography
for Intrauterine Abnormalities
Uchenna C. Acholonu, Jr., MD, James Silberzweig, MD, Daniel E. Stein, MD, Martin Keltz, MD
ABSTRACT
Objective: The hysterosalpingogram is commonly used
to evaluate the uterine cavity and the fallopian tubes in the
workup of infertile couples. The sonohysterogram is gaining popularity as part of this evaluation. This study compares hysterosalpingography to sonohysterography for
the detection of polyps, cavitary fibroids, adhesions, and
septae in infertile patients.
Methods: We conducted a retrospective chart review of
149 infertility patients seen at a University Hospital Center,
divisions of Reproductive Endocrinology and Interventional Radiology. Patients underwent hysterosalpingography and sonohysterography as part of their infertility evaluation. The reports were reviewed and findings like
polyps, fibroids, adhesions, and septae were compared to
the findings obtained at the time of hysteroscopy. Sensitivity, specificity, and accuracy of radiologic tests were the
main outcome measures.
Results: The sensitivity of hysterosalpingography and
sonohysterography was 58.2% and 81.8%, respectively.
The specificity for hysterosalpingography and sonohysterography was 25.6% and 93.8%. The differences in sensitivity and specificity were both statistically significant.
Hysterosalpingography had a general accuracy of 50.3%,
while sonohysterography had a significantly higher accuracy of 75.5%.
Ob/Gyn Department, St. Lukes-Roosevelt Hospital, New York, New York, USA
(Dr. Acholonu).
Interventional Radiology, Columbus Circle Imaging, New York, New York, USA
(Dr. Silberzweig).
Division of Reproductive Endocrinology and Infertility, Department of Obstetrics
and Gynecology, St. Lukes-Roosevelt Hospital, New York, New York, USA (Dr.
Stein).
Division of Reproductive Endocrinology and Infertility, Department of Obstetrics
and Gynecology, St. Lukes-Roosevelt Hospital Center, Columbia College of Physicians and Surgeons, New York, New York, USA (Dr. Keltz).
Address correspondence to: Uchenna C. Acholonu, Jr., MD, Ob/Gyn Department,
St. Lukes-Roosevelt Hospital, 1000 Tenth Avenue, New York, New York 10019,
USA. E-mail: uacholon@cphnet.org. Telephone: (212) 636-1130, Fax: (212) 6361130.
DOI: 10.4293/108680811X13176785203923
2011 by JSLS, Journal of the Society of Laparoendoscopic Surgeons. Published by
the Society of Laparoendoscopic Surgeons, Inc.
Conclusion: Although hysterosalpingography is the standard screening test for the diagnosis of tubal infertility and
can provide useful information about the uterine cavity,
sonohysterography is more sensitive, specific, and accurate in the evaluation of the uterine cavity.
Key Words: Hysterosalpingogram, Sonohysterogram, Imaging in infertility, Intrauterine defects.
INTRODUCTION
The hysterosalpingogram (HSG) is a contrast enhanced
fluoroscopic and flat plate study used to evaluate the
endometrial cavity and fallopian tubes. It has been a
standard test in the workup of infertile couples as a minimally invasive method of evaluating tubal patency. In
addition to crucial information about tubal patency and
contour, HSG reports include information about uterine
size and filling defects. HSG reports often present findings
suggestive of fibroids, polyps, adhesions, and septa. The
sonohysterogram (SHG) is a more recent addition for
intrauterine evaluation. A number of studies have shown
a benefit of SHG over HSG in evaluating uterine defects in
patients with recurrent pregnancy loss as well as for uterine screening prior to IVF.15 Other studies have suggested
that the sensitivity and specificity of SHG are comparable
to that of hysteroscopy for evaluating patients with abnormal uterine bleeding and postmenopausal bleeding.6 Our
study compares HSG to SHG in the evaluation of the
endometrial cavity in infertile patients.
METHODS
IRB approval was obtained for this retrospective study.
Over a 2-year period, 140 patients seen at our center
underwent hysteroscopy as part of the evaluation or treatment of infertility. All were included in this study. All 149
patients had a prior HSG and 93 underwent SHG. In our
practice, HSG is performed as part of the evaluation of
women seeking assistance with conception. SHG is performed on infertile patients with suspicious uterine findings on transvaginal ultrasound performed during the initial evaluation.
JSLS (2011)15:471 474
471
Hysterosalpingography Versus Sonohysterography for Intrauterine Abnormalities, Acholonu UC et al.
The HSG was performed by members of the Interventional Radiology division. The procedure was performed
under fluoroscopy in an outpatient office setting typically
between days 5 and 11 of the menstrual cycle at least 24
hours after menses had ceased. Prophylactic antibiotics
were prescribed. The patients were routinely premedicated with oral ibuprofen 600mg prior to the procedure.
A urine pregnancy test (QuickVue One-Step hCG Urine
Test, Quidel, San Diego, CA) was performed immediately
before the HSG procedure. HSG was performed in a
standard fashion using a sterile technique. The patient was
placed in a lithotomy position, and a vaginal speculum
was inserted. After cleansing the external os with povidone-iodine solution, the cervical os was cannulated with
a balloon catheter. A cervical tenaculum was not used.
The balloon catheter was inflated within the endocervical
canal or lower uterine cavity and contrast injection was
performed with fluoroscopic control (OEC 9800, General
Electric Company, Fairfield, CT). The balloon catheter was
not routinely placed in the uterine cavity, because it may
prevent or obscure opacification of underlying pathology
in the lower uterine segment. A combination of pulse
fluoroscopy (8 frames per second) and continuous fluoroscopy were used with automated exposure control.
Static image capture was achieved by use of the fluoroscopic last image hold feature. Images of early and maximal opacification of the uterine cavity, fallopian tubes,
and peritoneal contrast spillage were obtained. A completion image was obtained after removal of the balloon
catheter to assess for abnormalities in the lower uterine
segment and endocervical canal that may have been obscured by the presence of the balloon catheter. Selected
static images were transferred to a picture archive and
communications system (PACS).
SHG was performed during the follicular phase of the
cycle by 1 of 2 examiners. An H-S catheter (Ackrad Labs,
Cranford, NJ) was placed during a speculum examination,
with the balloon distended intracervically. In some cases,
the balloon distended with 1mL of saline would not remain in the cervix and either a tenaculum was placed
occluding the exocervix or the balloon was placed in the
lower uterine segment. After transvaginal sonographic
evaluation of the adnexae, uterus, endometrium, and culde-sac, saline in a 10-mL syringe was instilled through the
catheter during concomitant transvaginal sonography of
the endometrium with sagittal and coronal views recorded.
A study was considered normal when serial sagittal and
coronal views of the distended endometrial cavity failed
472
to reveal any distortion, cavitary defect, or undistended
regions. Incomplete separation of the anterior and posterior endometrium during saline instillation suggested
intrauterine synechiae. A midline avascular extension
into the uterine cavity in the absence of other evidence
of intrauterine synechiae, and the presence of a normal
serosal border of the fundus suggested a septum. While
vascular myometrium found between 2 uterine horns
combined with a midline dimpling of the serosal fundal
border suggested a bicornuate uterus. Other intracavitary defects were described and a likely diagnosis was
suggested.
Hysteroscopy was performed by 1 of 2 examiners in the
operating room with the patient under general anesthesia.
The cervix was grasped with a tenaculum and dilated to
accommodate the 7-mm hysteroscope. The scope was
advanced under direct visualization. Saline was instilled to
gravity. Positive and pertinent negative findings were recorded, and any required therapeutic procedures were
completed. When a myoma was anticipated or encountered, a 9-mm resectoscope was used.
The written reports from HSG, SHG, and hysteroscopy
were reviewed. Data collected included presence of fibroids, polyps, adhesions, or a septum. In the absence of
these findings, the cavity was described as normal.
Sensitivity, specificity, and accuracy were computed using
findings at hysteroscopy as the confirmatory result.7 Data
are expressed as number of patients and percentage. Chisquare analysis was performed with SYSTAT 10.2. We use
a P-value of .01 as statistically significant.
RESULTS
Of the 149 patients who underwent HSG and hysteroscopy, 110 had hysteroscopic abnormalities. HSG detected
abnormalities in 64 of these patients for a sensitivity of
58.2%. Of the 39 normal cavities on hysteroscopy, 29 were
described as having an abnormality on HSG for a specificity of 25.6% (Table 1).
Table 1.
Comparison of General Results for Sonohysterogram (SHG)
and Hysterosalpingogram (HSG)
SHG (%)
HSG (%)
p-value
Sensitivity
81.8
58.2
0.001
Specificity
93.8
25.6
0.001
Accuracy
75.5
50.3
0.001
JSLS (2011)15:471 474
Of the 93 patients who underwent SHG and hysteroscopy,
77 had hysteroscopic abnormalities. SHG described an
abnormality in 63 of these patients for a sensitivity of
81.8%. Of the 16 normal cavities on hysteroscopy, 1 was
described as abnormal on SHG for a specificity of 93.8%.
tile; as such, they entered with a high index of suspicion
for intracavitary abnormalities. This is compounded by the
fact that patients who had a normal HSG and SHG rarely
underwent the hysteroscopy, which may have confirmed
the negative findings.
The positive predictive value of HSG and SHG are 68.8%
and 98.4%, respectively. The negative predictive values
are 17.9% and 51.7%, respectively.
The sensitivity and specificity of SHG in our study are
comparable to those found in prior studies. Krample et al4
describe a sensitivity of 94% and specificity of 84%, Bonnamy et al11 quote 95% and 77%, and Ragni et al12 quote
98% and 94%.
For our study, we describe overall accuracy as:
The number of cavities with confirmed lesions the
number of confirmed normal cavities
Total number of uterine cavities evaluated
This is also described as:
________True Positive True Negative________
True Positive False Positive True Negative False
Negative
HSG had an overall accuracy of 50.3%, while SHG had an
accuracy of 75.5%. In addition to overall accuracy, we
looked at the accuracy of each modality in detecting
specific lesions (polyp, fibroid, adhesion, or septum) or a
normal cavity (Table 2).
DISCUSSION
HSG identified defects in 64 of the 110 abnormal cavities,
missing almost 42%. SHG identified 63 of the 77 defects
missing 20%. In addition, HSG described abnormalities
in 29 of 39 normal cavities for a false-positive rate of
74.4%. In a similar study, Goldberg et al8 found a false
positive rate of 20%. This is consistent with other reports
comparing HSG with hysteroscopy, which describe falsepositive rates in the range of 10% to 30%.9,10 The falsepositive rate in our study may be higher than that in others
due to a selection bias and the absence of blinding for
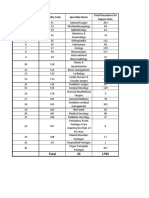
clinicians. The patients selected for this study were inferTable 2.
Accuracy Results of Sonohysterogram (SHG) and
Hysterosalpingogram (HSG) for Specific Lesions
Our secondary evaluation showed that SHG is more accurate than HSG in identifying the specific lesion distorting the endometrial cavity. This is similar to findings in a
previous study of recurrent pregnancy loss13 and an earlier study in infertile patients.14 Accurately identifying the
intracavitary lesion is important in preparing for operative
management. For example, if an adhesion is expected, a
hysteroscopic lysis procedure may be planned. However
if a myoma is encountered, a resecting instrument may be
required instead of a standard diagnostic hysteroscope.
This study was limited by its retrospective design and lack
of blinding for the physicians. In addition, patients with
normal-appearing cavities on SHG and HSG generally did
not go on to hysteroscopy. This resulted in a lower specificity and negative predictive values for both HSG and
SHG. Another limitation is that interpretation of the images of HSG and SHG depends on the experience and
ability of the clinicians involved.15 Finally, adhesions that
may have been accurately diagnosed on HSG or SHG may
have been lysed by a cervical dilator, uterine sound, or
uterine manipulator prior to the introduction of the hysteroscope for confirmation.
CONCLUSION
SHG has greater sensitivity, positive predictive value, and
accuracy than HSG has for detecting intrauterine lesions.
Although HSG will continue to be an important screening
tool in infertility for its proven ability to evaluate the
architecture and patency of the fallopian tubes, SHG is a
more reliable diagnostic tool for the evaluation of intrauterine defects.
SHG (%)
HSG (%)
p-value
Fibroids
75
52.6
0.405
References:
Polyps
69.4
38.8
0.008
Septum
52.9
40
0.517
Scaring
63.2
26.9
0.031
1. van Roessel J, Wamsteker K, Exalto N. Sonographic investigation of the uterus during artificial uterine distention. J Clin
Ultrasound. 1987;15:439 450.
Normal
94.4
79.5
0.247
2. Bonilla-Musoles F, Simon C, Serra V, et al. An assessment of
hysterosalpingosonography (HSSG) as a diagnostic tool for uter-
JSLS (2011)15:471 474
473
Hysterosalpingography Versus Sonohysterography for Intrauterine Abnormalities, Acholonu UC et al.
ine cavity defects and tubal patency. J Clin Ultrasound. 1992;20:
175181.
gography in evaluation of female infertility. Fert Steril. 1984;41:
709 713.
3. Syrop CH, Sahakian V. Transvaginal sonographic detection
of endometrial polyps with fluid contrast augmentation. Obstet
Gynecol. 1992;79:10411043.
10. Fayez JA, Mutie G, Schneider PJ. The diagnostic value of
hysterosalpingography and hysteroscopy in infertility investigation. Am J Obstet Gynecol. 1987;156:558 560.
4. Kim AH, McKay H, Keltz MD, Nelson HP, Adamson GD.
Sonohysterographic screening before in vitro fertilization. Fert
Steril. 1998;69:841 844.
11. Bonnamy L, Marret H, Perrotin F, Body G, Berger C, Lansac
J. Sonohysterography: a prospective survery of results and complications in 81 patients. Eur J Obstet Gynecol Reprod Bio. 2002;
102:42 47.
5. Tur-Kaspa I, Gal M, Hartman M, Hartman J, Hartman A. A
prospective evaluation of uterine abnormalities by saline infusion sonohysterography in 1,009 women with infertility or abnormal uterine bleeding. Fert Steril. 2006;86:17311735.
6. Krampl E, Bourne T, Hurlen-Solbakken H, Istre O. Transvaginal ultrasonography sonohysterography and operative hysteroscopy for the evaluation of abnormal uterine bleeding. Acta
Obstet Gynecol Scand. 2001;80:616 622.
7. Lindheim SR, Adsuar N, Kushner DM, Pritts E, Olive D.
Sonohysterography: A valuable tool in evaluating the female
pelvis. Ob Gynecol Survey. 2003;58:770 784.
8. Goldberg JM, Falcone T, Attaran M. Sonohysterographic
evaluation of uterine abnormalities noted on hysterosalpingography. Hum Reproduction. 1997;12:21512153.
9. Snowden EU, Jarret JC, Dawood YM. Comparison of diagnostic accuracy of laparoscopy, hysteroscopy and hysterosalpin-
474
12. Ragni G, Diaferia D, Vegetti W, Colombo M, Arnoldi M,
Crosignani PG. Effectiveness of sonohysterography in infertile
patient work-up: a comparison with transvaginal ultrasonography and hysteroscopy. Gynecol Obstet Invest. 2005;59:184 188.
13. Keltz MD, Olive DL, Kim AH et al. Sonohysterography for
screening in recurrent pregnancy loss. Fertil Steril. 1997;67:670674.
14. Soares SR, Barbosa dos Reis MM, Camargos AF. Diagnostic
accuracy of sonohysterography, transvaginal sonography, and
hysterosalpingography in patients with uterine cavity diseases.
Fertil Steril. 2000;73:406 411.
15. Grimbizis GF, Tsolakidis D, Mikos T, et al. A prospective
comparison of transvaginal ultrasound, saline infusion sonohysterography, and diagnostic hysteroscopy in the evaluation of
endometrial pathology. Fertil Steril. 2010;94:2720 2725.
JSLS (2011)15:471 474
You might also like
- How to Perform Ultrasonography in EndometriosisFrom EverandHow to Perform Ultrasonography in EndometriosisStefano GuerrieroNo ratings yet
- Transabdominal Sonography Before Uterine Exploration As A Predictor of Retained Placental FragmentsDocument5 pagesTransabdominal Sonography Before Uterine Exploration As A Predictor of Retained Placental FragmentsDownloadNo ratings yet
- Lower Genital Tract Precancer: Colposcopy, Pathology and TreatmentFrom EverandLower Genital Tract Precancer: Colposcopy, Pathology and TreatmentNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Techniques of Robotic Urinary Tract Reconstruction: A Complete ApproachFrom EverandTechniques of Robotic Urinary Tract Reconstruction: A Complete ApproachMichael D. StifelmanNo ratings yet
- Evaluation of Transvaginal Sonography in Detecting Endometrial Polyps and The Pregnancy Outcome Following Hysteroscopic Polypectomy in Infertile WomenDocument5 pagesEvaluation of Transvaginal Sonography in Detecting Endometrial Polyps and The Pregnancy Outcome Following Hysteroscopic Polypectomy in Infertile WomenMoe AboamNo ratings yet
- Der Chi 2001Document19 pagesDer Chi 20013bood.3raqNo ratings yet
- Transvaginal Saline Sonosalpingography For The Assessment of Tubal PatencyDocument7 pagesTransvaginal Saline Sonosalpingography For The Assessment of Tubal PatencyConsita VictoriaNo ratings yet
- Performance of A ColposcopicDocument27 pagesPerformance of A ColposcopicAnt GuzmanNo ratings yet
- Accuracy of Tubal Patency Assessment in Diagnostic Hysteroscopy Compared With Laparoscopy in Infertile WomenDocument20 pagesAccuracy of Tubal Patency Assessment in Diagnostic Hysteroscopy Compared With Laparoscopy in Infertile Womenria.janitaNo ratings yet
- Lateral ColposuspentionDocument24 pagesLateral ColposuspentionMohammad QuayyumNo ratings yet
- Nursing and Midwifery StudiesDocument5 pagesNursing and Midwifery StudiesYohanes Hadi PutrantoNo ratings yet
- 0068KJR - KJR 5 39Document8 pages0068KJR - KJR 5 39Louis HadiyantoNo ratings yet
- Jurnal Kista Ovarium2Document5 pagesJurnal Kista Ovarium2Isara Nur LatifahNo ratings yet
- Management of AUB in A Bicornuate Uterus - Endometrial Ablation in A CompDocument1 pageManagement of AUB in A Bicornuate Uterus - Endometrial Ablation in A Comptipu42No ratings yet
- Art 20177509Document4 pagesArt 20177509Jashashree SaikiaNo ratings yet
- Diagnostic Tools in ObgynDocument27 pagesDiagnostic Tools in ObgynHenok Y KebedeNo ratings yet
- Transvaginal Sonography Versus Hysteroscopy in Evaluation of Abnormal Uterine BleedingDocument6 pagesTransvaginal Sonography Versus Hysteroscopy in Evaluation of Abnormal Uterine BleedingKoko AgungNo ratings yet
- Core TanDocument6 pagesCore TanNita WidjayaNo ratings yet
- Hysterosalpingography 2009Document7 pagesHysterosalpingography 2009Niko MontgomeryNo ratings yet
- Testicular BloodDocument6 pagesTesticular Bloodsalcor00No ratings yet
- Radiology RadiologyDocument6 pagesRadiology RadiologyJonathan ReinaldoNo ratings yet
- HydrotubationDocument4 pagesHydrotubationAna Di Jaya100% (1)
- Ultrasonographic Usg Evaluation of Acute AppendiciDocument8 pagesUltrasonographic Usg Evaluation of Acute AppendiciKurnia HandayaniNo ratings yet
- Comparative Study of The Diagnostic Accuracy of Transvaginal Sonography Versus Hysteroscopy in Abnormal Uterine BleedingDocument11 pagesComparative Study of The Diagnostic Accuracy of Transvaginal Sonography Versus Hysteroscopy in Abnormal Uterine BleedingvenkayammaNo ratings yet
- Three-Dimensional Sonographic Findings of A Cervical PregnancyDocument4 pagesThree-Dimensional Sonographic Findings of A Cervical PregnancyEdwin AtencioNo ratings yet
- Urn NBN Si Doc Dk0qwtapDocument6 pagesUrn NBN Si Doc Dk0qwtapRaga ManduaruNo ratings yet
- The Effects of A Shoulder Roll During LaryngosDocument11 pagesThe Effects of A Shoulder Roll During LaryngospaulaNo ratings yet
- 1 s2.0 S1028455909601686 MainDocument5 pages1 s2.0 S1028455909601686 MainAgudisarfNo ratings yet
- Endometriomas: Their Ultrasound CharacteristicsDocument11 pagesEndometriomas: Their Ultrasound CharacteristicseunikesondangNo ratings yet
- 08 Trans Perineal UltrasoundDocument4 pages08 Trans Perineal UltrasoundArif BudimanNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document2 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)shelly_shellyNo ratings yet
- Atresia Ani DR - BaoDocument12 pagesAtresia Ani DR - BaoAnonymous turPUJtErNo ratings yet
- PIIS0749073923000184Document14 pagesPIIS0749073923000184Allende Tellechea CarrilloNo ratings yet
- Recurrence Rate of Endometriomas Following A Laparoscopic CystectomyDocument5 pagesRecurrence Rate of Endometriomas Following A Laparoscopic CystectomyPutri Tamara DasantosNo ratings yet
- Angle of Progression Measurements of Fetal Head at TermDocument5 pagesAngle of Progression Measurements of Fetal Head at TermcherryaaNo ratings yet
- Comparison of Laparoscopy and Laparotomy in The Surgical Management of Ectopic PregnancyDocument5 pagesComparison of Laparoscopy and Laparotomy in The Surgical Management of Ectopic PregnancyFitri Maya AnggrainiNo ratings yet
- Single-Port Laparoscopic Salpingectomy For Surgical Treatment of Tubal Pregnancy - Comparison With Multi-Port Laparoscopic Salpingectomy - PMCDocument11 pagesSingle-Port Laparoscopic Salpingectomy For Surgical Treatment of Tubal Pregnancy - Comparison With Multi-Port Laparoscopic Salpingectomy - PMCria.janitaNo ratings yet
- Ajceu 0072410Document5 pagesAjceu 0072410Azad AhmedNo ratings yet
- Histeroctomy PDFDocument6 pagesHisteroctomy PDFsanta_pangaribuan_1No ratings yet
- US en EndometritisDocument7 pagesUS en EndometritisRubí FuerteNo ratings yet
- Original ArticleDocument5 pagesOriginal ArticlehengkyNo ratings yet
- Usmle QuestionnarieDocument85 pagesUsmle QuestionnariegwapingMDNo ratings yet
- 3-Original ArticleDocument6 pages3-Original ArticleabhishekkuduguntiNo ratings yet
- Person's Correlation Coeffkient (I) WithDocument1 pagePerson's Correlation Coeffkient (I) WithMika OikuNo ratings yet
- Best of Best in ENTDocument34 pagesBest of Best in ENTNagaraj ShettyNo ratings yet
- Menopausal Symptoms and Surgical Complications After Opportunistic Bilateral Salpingectomy, A Register-Based Cohort StudyDocument10 pagesMenopausal Symptoms and Surgical Complications After Opportunistic Bilateral Salpingectomy, A Register-Based Cohort StudytriNo ratings yet
- Learning Curve in Determining Fetal Sex by First Trimester Ultrasound ScanDocument6 pagesLearning Curve in Determining Fetal Sex by First Trimester Ultrasound ScanAisahNo ratings yet
- Oligohydramnion PDFDocument6 pagesOligohydramnion PDFhusain abdul halimNo ratings yet
- Zhao2015 PDFDocument9 pagesZhao2015 PDFmavarthavaNo ratings yet
- Hysteroscopic Fallopian Tube Recanalization Using A Exible Guide Cannula and Hydrophilic Guide WireDocument5 pagesHysteroscopic Fallopian Tube Recanalization Using A Exible Guide Cannula and Hydrophilic Guide WireAswathy KumaranNo ratings yet
- Peritonela TumorDocument6 pagesPeritonela TumorEuis Maya SaviraNo ratings yet
- Accuracy of Prenatal Sonography For Detecting Circumvallate PlacentaDocument6 pagesAccuracy of Prenatal Sonography For Detecting Circumvallate PlacentaTeNri MaulaniNo ratings yet
- 3 PBDocument6 pages3 PBAulia Rizqi MulyaniNo ratings yet
- Hum. Reprod.-2013-Romosan-1569-79Document11 pagesHum. Reprod.-2013-Romosan-1569-79Ahmad Arbi AninditoNo ratings yet
- Transvaginal Removal of Ectopic Pregnancy Tissue and Repair of Uterine Defect For Caesarean Scar PregnancyDocument4 pagesTransvaginal Removal of Ectopic Pregnancy Tissue and Repair of Uterine Defect For Caesarean Scar PregnancyGladstone AsadNo ratings yet
- USMLE - VirusesDocument120 pagesUSMLE - Viruseszeal7777100% (1)
- Mobicare BrochureDocument4 pagesMobicare Brochuremicrobotica126No ratings yet
- Welcome To The Celestial Biolabs LimitedDocument8 pagesWelcome To The Celestial Biolabs LimitedsaahilsinghiNo ratings yet
- Teknik SAB Ideal-1Document31 pagesTeknik SAB Ideal-1Buatlogin DoangNo ratings yet
- The Secrets To Gaining Muscle Mass Fast by Anthony Ellis PDFDocument125 pagesThe Secrets To Gaining Muscle Mass Fast by Anthony Ellis PDFVishal DokaniaNo ratings yet
- Angelie ADocument4 pagesAngelie AMaja TusonNo ratings yet
- Medical Decision MakingDocument14 pagesMedical Decision MakingwbothaNo ratings yet
- LP + Askep CKD ON HDDocument51 pagesLP + Askep CKD ON HDArista BaruNo ratings yet
- Quality Management in The Imaging Sciences 5th Edition Papp Test BankDocument35 pagesQuality Management in The Imaging Sciences 5th Edition Papp Test Bankmisdateholinessaubzt6100% (22)
- Lab Policies Differential Counting and Morphology Lab 5074Document14 pagesLab Policies Differential Counting and Morphology Lab 5074Egil SantosNo ratings yet
- An Introduction To NutritionDocument17 pagesAn Introduction To NutritionAlejandra Diaz RojasNo ratings yet
- Ileus ObstructionDocument22 pagesIleus ObstructionfitrahNo ratings yet
- Iaso Tea IngredientDocument7 pagesIaso Tea Ingredientsizzla7No ratings yet
- RetailerPriceList OHDocument1 pageRetailerPriceList OHMuhammad Samiur RahmanNo ratings yet
- AnthropometricDocument11 pagesAnthropometricdrrebaNo ratings yet
- Intern Annual16Document7 pagesIntern Annual16Akash PanwarNo ratings yet
- Post-Cardiac Arrest Therapeutic Hypothermia Targeted Temperature Manangement (TTM) Quick SheetDocument3 pagesPost-Cardiac Arrest Therapeutic Hypothermia Targeted Temperature Manangement (TTM) Quick SheetkimberlyNo ratings yet
- ARI Company Catalogue PDFDocument29 pagesARI Company Catalogue PDFEd Gar YundaNo ratings yet
- 2018 Article 242 PDFDocument57 pages2018 Article 242 PDFOscar NgNo ratings yet
- Drug Study SitagliptinDocument3 pagesDrug Study SitagliptinEzron Kendrick Duran50% (2)
- Biofeedback 2000x-Pert Hardware ManualDocument45 pagesBiofeedback 2000x-Pert Hardware ManualNery BorgesNo ratings yet
- Homeopathy Cases by KadwaDocument179 pagesHomeopathy Cases by Kadwaabckadwa100% (3)
- Marine-Derived Pharmaceuticals - Challenges and OpportunitiesDocument11 pagesMarine-Derived Pharmaceuticals - Challenges and OpportunitiesElda ErnawatiNo ratings yet
- TRIKATUDocument5 pagesTRIKATUAngshuman DuttaNo ratings yet
- Fracture of Shoulder and Upper Arm S42Document9 pagesFracture of Shoulder and Upper Arm S42yunitaNo ratings yet
- Sanjeevini Combination Sheet For SSC 8 Blood Pressure HighDocument1 pageSanjeevini Combination Sheet For SSC 8 Blood Pressure HighEduardoNo ratings yet
- 9000 One Liner GK PDF in Hindi (For More Book - WWW - Gktrickhindi.com)Document25 pages9000 One Liner GK PDF in Hindi (For More Book - WWW - Gktrickhindi.com)Ashish gautam100% (1)
- Acknowledgement32564178993.Doc Final1Document6 pagesAcknowledgement32564178993.Doc Final1Rashid AzmiNo ratings yet
- Interpretation of Peripheral SmearDocument34 pagesInterpretation of Peripheral Smearswathi bs100% (1)
- All PackageRates (ABPMJAY) PDFDocument300 pagesAll PackageRates (ABPMJAY) PDFSumit Soni0% (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (34)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (4)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (2)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Hearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIFrom EverandHearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIRating: 4 out of 5 stars4/5 (20)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4.5 out of 5 stars4.5/5 (6)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)