Professional Documents
Culture Documents
Ann Oncol 2008 Jirillo 1817 8
Uploaded by
Mina RaghebCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ann Oncol 2008 Jirillo 1817 8
Uploaded by
Mina RaghebCopyright:
Available Formats
Annals of Oncology
Last year Bernardi et al. [1] said By 2008, anticancer drugs will
be the leading therapeutic area in term of sales. This appraisal
has been done by the Intercontinental Marketing Services
(IMS) Health, a provider of business intelligence and strategic
consulting services for the pharmaceutical and health care
industries. Oncology, considered a niche sector just a few
years ago, will reach a business volume of 41 billion dollars in
2008 compared with 24 billion dollars in 2004. The economic
aspects will increasingly restrict access to new and expensive
oncological drugs (e.g. Targeted therapy as monoclonal
antibodies and angiogenesis inhibitors) in different health care
realities.
Today the high economic cost of bevacizumab (Avastin,
Roche) is a real problem which involves also mass-media. First
of all Reuters on Thursday, 26 June 2008, announced: The
British National Institute for Clinical Health and Excellence
(NICE) said it was unable to recommend first-line use of
Avastin in lung and breast cancer after Roche failed to submit
clinical and cost effectiveness evidence. For this reason,
Roches cancer drug Avastin will not be made available for use
on Britains state health service because the Swiss drugmaker
has refused to provide enough information to assess its
cost-effectiveness.
Volume 19 | No. 10 | October 2008
Recently (6 July 2008), the USA web newspaper
International Herald Tribune wrote about Avastin: Costly
cancer drug offers hope, but also a dilemma.
Looked at one way, Avastin, made by Genentech (Roche
Partner), is a wonder drug. Approved for patients with
advanced lung, colon or breast cancer, it cuts off tumors blood
supply, an idea that has tantalized science for decades. And
despite its price, which can reach $100,000 a year, Avastin has
become one of the most popular cancer drugs in the world,
with sales last year of about $3.5 billion, $2.3 billion of that in
the United States. But there is another side to Avastin.
Studies show the drug prolongs life by only a few months, if
that. And some newer studies suggest the drug might be less
effective against cancer than the Food and Drug Administration
had understood when the agency approved its uses.
Dr Leonard Saltz, a colon cancer specialist at Memorial
Sloan-Kettering Cancer Center in New York, said of the new
data that the incremental benefit may be more modest than we
want to admit.
Then What does it mean to say an expensive drug works? Is
slowing the growth of tumors enough if life is not significantly
prolonged or improved? How much evidence must there be
before billions of dollars are spent on a drug? Who decides?
When, if ever, should cost come into the equation?
A very interesting opinion of Mr Roy Vagelos, a former chief
executive of Merck who is considered an elder statesman of
the industry, said: . in a recent speech that he was troubled by
a drug, which he would not name but which was a clear
reference to Avastin, that costs $50,000 a year and adds four
months of life. There is a shocking disparity between value and
price, and its not sustainable. Cancer drugs constitute the
second biggest category of drugs in the United States behind
cholesterol-lowering medicines, and accounted for $17.8 billion
of total prescription drug sales of $286.5 billion in 2007,
according to IMS Health, a health care information company.
Spending on drugs for cancer grew 14% last year, faster than for
all but three other diseases.
Avastin example offers an opportunity to improve the
methodological aspects: in the report [1] the three levels
macro-, meso- and microlevel include the amount of resources
that a nation devotes to health care.
What happened in UK was an example of macrolevel
decision: no supplement of data by Roche, no authorization for
drug use.
In United States, in addition to private insurance, the
patients pay 25% of the cost of the treatment, which
includes Avastin. This is an example of decision of
cooperation between macro- and microlevel to pay the
amount of cost. The last possibility (probably an unrealistic
one) is that the National health refunds the global expenses.
Since 75% of pharmaceutical expenditure is publicly
reimbursed in Europe, pharmaceuticals have been subjected to
a wide range of pricing policies. In this perspective, important
questions emerge: how to face change? Should economic
evaluation be integrated with ethical evaluation? Is this
achievable?
The problem is serious and it is the first time in the history of
Medical Oncology, in industrialized countries, that there are
different possibilities for a patient to receive treatment.
letters to the editor | 1817
Downloaded from http://annonc.oxfordjournals.org/ by guest on March 27, 2016
Bevacizumab in advanced
cancer, too much or too little?
letters to the editor
letters to the editor
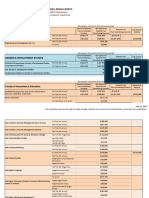
Very interesting appears the protocol between Italian
Drugs Agency (AIFA) and Roche Italia. The new agreement is
on the basis of the identification of an annual maximum cost
for patient (medium) in charge of Italian National Health
System (SSN) for all the indications independently from
Bevacizumab protocol and doses [2]:
AIFA has identified the annual maximum cost in charge of the
SSN on the base of the treatment of the colon rectal cancer
1818 | letters to the editor
with the avastin dosages (5 mg/kg every 2 weeks) for a patient
with a medium weight of 70 kg.
If the treatment exceeds the year, it will be not applied the
risk sharing for the first 6 weeks.
In Italy, at the present time, the treatment with Avastin
cannot exceed e 25,941 per year, for all approved pathologies.
All economic considerations need to balance the benefits to
be obtained with the costs to obtain the benefits.
In our opinion, this protocol AIFA/Roche Italia spa is
considered a good start for a promising future in which drug
makers and National Health cooperate for a cost reduction
but also for a better treatment in patients with low life expectancy.
A. Jirillo1*, F. Vascon1 & M. Giacobbo1
1
Department of Medical Oncology, Istituto Oncologico Veneto IOV,
IRCCS, Padova, Italy
(*E-mail: jirillo@libero.it)
references
1. Bernardi A, Jirillo A, Pegoraro R, Bonavina MG. Allocation of public sources
in oncology: which role can ethics play? Ann Oncol 2007; 18(7):
11291131.
2. www.agenziafarmaco.it (14 July 2008, date last accessed).
doi:10.1093/annonc/mdn564
Volume 19 | No. 10 | October 2008
Downloaded from http://annonc.oxfordjournals.org/ by guest on March 27, 2016
1 Identification of an annual maximum cost for patient in
charge of the SSN based on the Colon-Recto indication
(low dosage for 52 weeks).
2 Identification of the cycle number in charge of the hospital,
for year of treatment, in order to maintain the cost of the
high dosage schedules in the limits of point 1.
3 Risk sharing to 50% for the first 1.5 months (6 weeks) for all
the indications, schedules, dosages and frequency (every 2,
3 weeks).
4 Payback from the company at the end of the treatment.
5 This protocol Roche/AIFA will be in use for 24 months.
6 Otherwise for high dosages and every schedule of Avastin,
the agreement defines a cut-off on the basis of bevacizumab
dosage approved in colonrectal cancer, for this reason the
reimbursement is on the basis of 5 U/kg (lung, breast and
renal cancer)
Annals of Oncology
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Psycho Dynamic Psychotherapy For Personality DisordersDocument40 pagesPsycho Dynamic Psychotherapy For Personality DisorderslhasniaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Start and Run Sandwich and Coffee Shops PDFDocument193 pagesStart and Run Sandwich and Coffee Shops PDFsap7e88% (8)
- MCAT Practice Test 5RDocument75 pagesMCAT Practice Test 5Rhkhgkhgkhg100% (3)
- 100 Workouts Vol1 by DarebeeDocument207 pages100 Workouts Vol1 by DarebeeKoulick100% (2)
- School Threat AssessmentDocument12 pagesSchool Threat AssessmentChelsea ElizabethNo ratings yet
- Free Ukcat Questions AnswersDocument21 pagesFree Ukcat Questions AnswersMina RaghebNo ratings yet
- Psychometric Success Verbal Ability - Comprehension Practice Test 1Document8 pagesPsychometric Success Verbal Ability - Comprehension Practice Test 1Mina RaghebNo ratings yet
- Megestrol CyranDocument9 pagesMegestrol CyranMina RaghebNo ratings yet
- Sspc-Ab 2Document3 pagesSspc-Ab 2HafidzManafNo ratings yet
- FC Paed (SA) Part I Past Papers - 2011 Sept 6-4-2014Document8 pagesFC Paed (SA) Part I Past Papers - 2011 Sept 6-4-2014matenten0% (1)
- Free Gamsat Sample Questions PDFDocument27 pagesFree Gamsat Sample Questions PDFMina Ragheb100% (2)
- Health Education Plan-DiarrheaDocument10 pagesHealth Education Plan-DiarrheaMae Dacer50% (2)
- TS 0829Document79 pagesTS 0829Mina RaghebNo ratings yet
- Hepatitis C Life Cycle - Paper 1 PDFDocument13 pagesHepatitis C Life Cycle - Paper 1 PDFMina RaghebNo ratings yet
- Biology New Sample Questions PDFDocument9 pagesBiology New Sample Questions PDFMina RaghebNo ratings yet
- Megestrol Acetate PDFDocument9 pagesMegestrol Acetate PDFMina RaghebNo ratings yet
- Protein KinaseDocument1 pageProtein KinaseMina RaghebNo ratings yet
- J Biomater Appl-2011-Naderi-0885328211408946Document17 pagesJ Biomater Appl-2011-Naderi-0885328211408946Mina RaghebNo ratings yet
- CHEM426 Exam Guidance and EquationsDocument2 pagesCHEM426 Exam Guidance and EquationsMina RaghebNo ratings yet
- MarkingRubric-CHEM 426 TUTORIALS PDFDocument2 pagesMarkingRubric-CHEM 426 TUTORIALS PDFMina RaghebNo ratings yet
- Myocet Liposome Encapsulated Doxorubicin Citrate A New Approach in Breast Cancer TherapyDocument14 pagesMyocet Liposome Encapsulated Doxorubicin Citrate A New Approach in Breast Cancer TherapyMina RaghebNo ratings yet
- Nej Me 048098Document3 pagesNej Me 048098Mina RaghebNo ratings yet
- JCO 1987 Clark 55 61 PDFDocument7 pagesJCO 1987 Clark 55 61 PDFMina RaghebNo ratings yet
- Good Medical Practice - English 0914Document36 pagesGood Medical Practice - English 0914Mina RaghebNo ratings yet
- CementumDocument26 pagesCementumPrathik RaiNo ratings yet
- OGL 481 Pro-Seminar I: PCA-Ethical Communities Worksheet Erica KovarikDocument4 pagesOGL 481 Pro-Seminar I: PCA-Ethical Communities Worksheet Erica Kovarikapi-529016443No ratings yet
- 03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumDocument16 pages03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumFloba Ika SianturiNo ratings yet
- Acute k9 Pain ScaleDocument1 pageAcute k9 Pain Scaleapi-367949035No ratings yet
- Venus Technical Data Sheet of V-2400 Series RespiratorDocument7 pagesVenus Technical Data Sheet of V-2400 Series RespiratorPrabhu Mariadoss SelvarajNo ratings yet
- Breast Mass Bilateral To Consider FibroadenomaDocument5 pagesBreast Mass Bilateral To Consider FibroadenomaYum CNo ratings yet
- RecormonDocument36 pagesRecormonShamal FernandoNo ratings yet
- Guide To Referencing and Developing A BibliographyDocument26 pagesGuide To Referencing and Developing A BibliographyAHSAN JAVEDNo ratings yet
- UWI-Mona 2021-2022 Graduate Fee Schedule (July 2021)Document15 pagesUWI-Mona 2021-2022 Graduate Fee Schedule (July 2021)Akinlabi HendricksNo ratings yet
- Innovation - Edipeel Prolongs Fruit Shelf Life, Reduces SpoilageDocument5 pagesInnovation - Edipeel Prolongs Fruit Shelf Life, Reduces SpoilageahosfhaofahfouaNo ratings yet
- Theoretical Models of Nursing Practice AssignmentDocument6 pagesTheoretical Models of Nursing Practice Assignmentmunabibenard2No ratings yet
- F&F LetterDocument3 pagesF&F LetterJaskeerat Singh50% (2)
- Chronic Bacterial Prostatitis: Causes, Symptoms, and TreatmentDocument9 pagesChronic Bacterial Prostatitis: Causes, Symptoms, and TreatmentAnonymous gMLTpER9IUNo ratings yet
- Referralsystem 161202080450Document21 pagesReferralsystem 161202080450DRx Sonali Tarei100% (1)
- Semi Solids PDFDocument3 pagesSemi Solids PDFAsif Hasan NiloyNo ratings yet
- Kerry Washington. Family Secret.Document3 pagesKerry Washington. Family Secret.yulya.shevchenko110No ratings yet
- EpididymitisDocument8 pagesEpididymitisShafira WidiaNo ratings yet
- Drug in PregnancyDocument5 pagesDrug in PregnancyjokosudibyoNo ratings yet
- The Premier University in Zamboanga Del Norte: Jose Rizal Memorial State UniversityDocument1 pageThe Premier University in Zamboanga Del Norte: Jose Rizal Memorial State UniversityCHARLEES BRAVONo ratings yet
- Beddtiot ORTHO / Orthodontic Courses by Indian Dental AcademyDocument60 pagesBeddtiot ORTHO / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Physio Ex Exercise 6 Activity 4Document5 pagesPhysio Ex Exercise 6 Activity 4Roland Calipayan Jr.No ratings yet
- REAL in Nursing Journal (RNJ) : Penatalaksanaan Pasien Rheumatoid Arthritis Berbasis Evidence Based Nursing: Studi KasusDocument7 pagesREAL in Nursing Journal (RNJ) : Penatalaksanaan Pasien Rheumatoid Arthritis Berbasis Evidence Based Nursing: Studi Kasustia suhadaNo ratings yet
- Angina Pectoris: Causes, Symptoms and TreatmentsDocument17 pagesAngina Pectoris: Causes, Symptoms and TreatmentsGaming ModeNo ratings yet