Professional Documents
Culture Documents
Art:10.1186/1745 6215 15 418
Uploaded by
Ana BarbaraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Art:10.1186/1745 6215 15 418
Uploaded by
Ana BarbaraCopyright:
Available Formats
Yang et al.
Trials 2014, 15:418
http://www.trialsjournal.com/content/15/1/418
STUDY PROTOCOL
TRIALS
Open Access
Effectiveness of Chinese massage therapy (Tui Na)
for chronic low back pain: study protocol for a
randomized controlled trial
Mingxiao Yang1, Yue Feng1, Hong Pei2, Shufang Deng1, Minyu Wang1, Xianjun Xiao1, Hui Zheng1,
Zhenhong Lai1, Jiao Chen1, Xiang Li1, Xiaoguo He2* and Fanrong Liang1*
Abstract
Background: Low back pain is a common, disabling musculoskeletal disorder in both developing and developed
countries. Although often recommended, the potential efficacy of massage therapy in general, and Chinese
massage (tuina) in particular, for relief of chronic low back pain (CLBP) has not been fully established due to
inadequate sample sizes, low methodological quality, and subclinical dosing regimens of trials to date. Thus, the
purpose of this randomized controlled trial (RCT) is to evaluate the comparative effectiveness of tuina massage
therapy versus conventional analgesics for CLBP.
Methods/Design: The present study is a single center, two-arm, open-label RCT. A total of 150 eligible CLBP patients
will be randomly assigned to either a tuina treatment group or a conventional drug control group in a 1:1 ratio. Patients
in the tuina group receive a 20 minutes, 4-step treatment protocol which includes both structural and relaxation
massage, administered in 20 sessions over a period of 4 weeks. Patients in the conventional drug control group are
instructed to take a specific daily dose of ibuprofen. The primary outcome measure is the change from baseline back
pain and function, measured by Roland-Morris Disability Questionnaire, at two months. Secondary outcome measures
include the visual analogue scale, Japanese orthopedic association score (JOAS), and McGill pain questionnaire.
Discussion: The design and methodological rigor of this trial will allow for collection of valuable data to evaluate the
efficacy of a specific tuina protocol for treating CLBP. This trial will therefore contribute to providing a solid foundation
for clinical treatment of CLBP, as well as future research in massage therapy.
Trial registration: This trial was registered with ClinicalTrials.gov of the National Institute of Health on 22 October 2013
(NCT01973010).
Keywords: Chronic low back pain, Effectiveness, Randomized controlled trial, Tuina, Chinese massage therapy
Background
Low back pain is a common, disabling musculoskeletal
disorder in both developing and developed countries [1],
with chronic low back pain (CLBP) being the leading
cause of disability and absenteeism, worldwide [2]. The
lifetime prevalence of low back pain in the general population is estimated to be between 70 and 85%, with an
annual incidence rate ranging from 6.3 to 15.4% [1,3].
* Correspondence: 315363573@qq.com; acuresearch@126.com
Equal contributors
2
Tuina Massage Department, The Fifth Hospital of Sichuan Province, No. 66,
Shangye District, Chengdu, Sichuan 610031, China
1
Chengdu University of Traditional Chinese Medicine, No.37, Shierqiao Road,
Jinniu District, Chengdu, Sichuan 610072, China
According to the 2000 UK guidelines, 90% of episodes of
acute low back pain resolve spontaneously, with patients
returning to work within a month [4,5]. However, several
studies claim that low back pain and related loss of function persist for 3 to 12 months [6,7] with more than 25%
of patients experiencing recurrence of low back pain
within a year [8]. Up to 7% of patients develop CLBP
[9]. Because CLBP is not life-threatening, its enormous
social and economic cost is often underestimated. As of
2010, the global burden of CLBP was reported to be
comparable to that of cardiovascular disease, infectious
disease, and cancer [10-12].
2014 Yang et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,
unless otherwise stated.
Yang et al. Trials 2014, 15:418
http://www.trialsjournal.com/content/15/1/418
The pathophysiology of CLBP is poorly understood
due to difficulties in localizing the source of the pain
[13]. Potential causes of low back pain include, but are
not limited to, changes in the spinal disc structure with
aging and degeneration, as well as changes in local concentrations of cytokines such as matrix metalloproteinases, phospholipase A2, nitric oxide, and tumor necrosis
factor- [14]. Based on data from the Low Back Pain
Group of the Bone and Joint Health Strategies for
Europe Project, most cases of low back pain are
non-specific, with a specific cause being identified in
only 10% of cases; non-specific low back pain is, by its
definition, a symptom of unknown cause [15]. Specific
conditions contributing to low back pain include degeneration, inflammation, infective and neoplastic causes, metabolic bone diseases, referred pain, psychogenic pain,
trauma, and congenital disorders [16].
In clinical practice, a focused medical history and
comprehensive physical examination are required for
doctors to make appropriate treatment recommendations. Diagnostic tests, including imaging studies such as
X-ray, magnetic resonance imaging (MRI), and computed tomography (CT) are not routinely recommended
for uncomplicated low back pain, except when severe or
progressive deficits are present or when serious potential
factors are suspected [17]. Conventional medications in
several classes have been shown to have moderate shortterm benefits for patients with low back pain. For most
patients, first-line medication options include analgesics
like acetaminophen or nonsteroidal anti-inflammatory
drugs (NSAIDs) [18,19]. These medications have limited
effectiveness and are frequently associated with undesirable side-effects on gastrointestinal, renovascular, and
other systems [20-22]. The heavy economic burden of
low back pain has a huge impact on individuals, families,
communities, governments, and businesses throughout
the world. Thus, alternative back pain treatments are
needed that minimize cost and maximize health benefit
[23]. Although non-pharmacological treatments such as
bed rest, exercise, acupuncture, massage, spinal manipulation, yoga, and cognitive behavioral therapy are commonly prescribed in addition to pharmacologic therapy,
the evidence supporting their efficacy is inconclusive.
Chinese massage therapy (referred to as tuina) is
commonly defined as the ancient healing art of fingers
and strength [24]. Tuina has been practiced in China for
over 5000 years [25]. It is a well-respected treatment
modality known to be helpful and safe for a wide range
of conditions. For these reasons, it is rapidly gaining
international favor [26]. Tuina involves a wide range of
technical manipulations conducted by a practitioners
finger, hand, elbow, knee, or foot applied to muscle or
soft tissue at specific body locations. It incorporates
many of the principles of acupuncture including the use
Page 2 of 7
of acupoints. For instance, tuina often uses manual
techniques such as pushing, rubbing, kneading, or
high-intensity, high-frequency patting to clear energy
blocks along specific meridians associated with particular conditions [24].
At present, Chinese massage therapy is widely accepted
as a complementary and alternative medicine modality
[27]. Its efficacy has been demonstrated for the management of many medical and psychiatric conditions. These
include, but are not limited to, failure to thrive in preterm
infants, major depressive disorder, substance abuse
and dependence, pain syndromes, and immune and
autoimmune conditions [28-31]. Massage therapy has
been shown to be particularly effective for disorders of
musculoskeletal origin [32]. However, due to a paucity of
high-quality studies, there remains controversy about the
efficacy and effectiveness of massage. Many clinical trials
suffer from inadequate sample size, low methodological
quality, and/or sub-therapeutic massage dosing [33]. As a
result, the findings of recent systematic reviews about
massage therapy for low back pain are consistently inconclusive, due to the methodology flaws in the primary studies they reference. Therefore, studies without these flaws
are important to confirm the efficacy and effectiveness of
tuina for low back pain [32,34]. This trial will therefore
contribute to providing a solid foundation for clinical
treatment of CLBP, as well as future research in massage
therapy.
Methods/Design
Ethics approval
All trial procedures place the participants benefit as the
highest priority. The present study protocol has already
been ethically reviewed and approved by the Sichuan
Regional Ethics Review Committee on Traditional
Chinese Medicine (TCM) with the ethical approval
identifier 2013KL-002.
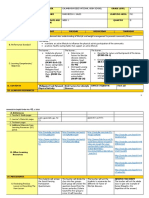
Study design
The present study is a single center, two-arm, open-label
randomized controlled trial. All trial procedures will be
conducted in the Fifth Hospital of Sichuan Province,
Chengdu, China. A total of 150 eligible CLBP patients
will be randomly assigned to either a tuina treatment
group or a conventional drug control group in a 1:1 ratio
(Figure 1).
Participants
Eligible participants include patients diagnosed with
CLBP according to the clinical guideline for traditional
Chinese medicine (the Criteria of Diagnosis and Therapeutic Effect of Diseases and Syndromes in Traditional
Chinese Medicine, ZY/T001.1-94) [35]. Patients presenting for the first time to either the Neurology Department
Yang et al. Trials 2014, 15:418
http://www.trialsjournal.com/content/15/1/418
Page 3 of 7
Eligible Chronic Low Back Pain patients
Assessed by Clinical Center
Ineligible
Excluded
Screening
Randomization
Tuina massage group (N=75)
Conventional drug group (N=75)
Baseline assessment
Dropout
Treatment: 20 sessions in 4 weeks
ITT analysis
Post-treatment assessment and follow ups
Data collection and statistical analysis
Effectiveness
Safety
Health economics
Figure 1 Trial flow chart. The present study is a single center, randomized, conventional drug controlled, open-labeled trial. A total of 150
eligible CLBP patients are anticipated to be included and randomly allocated to either tuina massage treatment group or conventional drug
control group, in a 1:1 ratio. Patients in the tuina group receive a four-step massage treatment consisting both structural and relaxation massage.
Tuina massage treatment consists of 20 sessions of approximately 20 minutes duration, each administered over a period of four weeks. Patients
in the conventional drug control group are instructed to administer ibuprofen. The effectiveness, safety, and health economics of tuina massage
versus conventional drugs is analyzed after data collection. The full analysis set including the dropout will be analyzed by the intention-to-treat
(ITT) population analysis.
or the Tuina Department in the hospital for low back pain
for over three months (without relief for over two weeks)
will be informed of this trial. If the patient expresses interest, a clinical trial communicator will contact them to
provide a brief introduction about the trial. Detailed information regarding patients low back pain will be acquired
for further assessment of inclusion eligibility according to
the following criteria.
of the central lumbar intervertebral disc, ankylosing
spondylitis, spinal stenosis, intraspinal tumor, and tuberculosis; (v) free from any kind of hormonal or antirheumatic drugs for the two months prior to inclusion;
(vi) free from allergies to hormones or analgesics; and
(vii) able to understand and accept all trial procedures
and cooperate with clinical physicians practices.
Exclusion criteria
Inclusion criteria
In order to be included in this trial, participants have to
be: (i) diagnosed with CLBP according to the aforementioned diagnostic methods; (ii) between 20 to 55-yearold; (iii) free of immune dysfunction, genetic disorders,
or severe cardiovascular diseases; (iv) free from prolapse
Participants with any one of the following conditions
will be excluded from this trial: (i) pregnancy; (ii) severe
heart, liver, or renal dysfunction; (iii) tumor; (iv) any
hematological, respiratory, or cardiovascular disease; (v)
any psychiatric disorder; (vi) severe nervous dysfunction
resulting from vertebral pulp prolapse, (vii) cauda equina
Yang et al. Trials 2014, 15:418
http://www.trialsjournal.com/content/15/1/418
compression or other indications for spinal surgery; (viii)
sciatica, (ix) lumbar surgery within the past three years;
(x) any disorders that may confound the assessment of
tuina efficacy, such as severe fibromyalgia or rheumatic
arthritis; (xi) ongoing corticosteroid or NSAID use, (xii)
history of allergy to NSAIDs; and (xiii) have received
tuina therapy for CLBP in the past three months.
Benefits and risks are clearly explained to eligible patients before inclusion. Prior to trial inclusion, all eligible
patients will provide their written consent.
Randomization
In this trial, participants will be randomly assigned to
either the tuina group or the ibuprofen group in a 1:1
ratio using a random number generator (SPSS 16.0, SPSS
Inc, Chicago, IL, USA).
Blinding
As an open-label clinical trial, both patients and clinicians know which treatment approach they will receive,
and they are required to cooperate with their physicians
or therapists prior to treatment. The assessment of clinical efficacy will be performed over the telephone by a
clinical assessor who will be masked to the treatment assignment. During the data collection and analysis stages,
the clinical researcher, assessor, and statistician do not
share study information with each other.
Interventions
The tuina protocol used in this trial is the same as those
used in our previous studies [36,37]. It includes both relaxation methods and structural methods such as rolling,
pressing, jostling, friction, pulling, and tapping.
Tuina treatment group
The CLBP patient will receive tuina massage therapy for
20 minutes, five times a week for a total of four weeks.
Lumbar function will be assessed at baseline as well as at
four, six, and eight weeks after the baseline assessment.
In this arm of the study, the tuina therapist will
administer a four-step protocol intended to ease low
back pain and improve lumbar function by promoting Qi
movement (which according to traditional Chinese medicine theory activates blood circulation), or by inducing a
state of general relaxation sensation while addressing
specific structural issues determined by the clinician to be
likely to contribute to the patients CLBP. The specific
protocol used is described below.
Step one: relaxation manipulation Patients are
instructed by the tuina therapist to lie in the prone
position and to relax their mind and body. Low back
pain conditions can be carefully examined by postural
and palpatory assessment prior to treatment. Tender
Page 4 of 7
tissues, trigger points, contracted muscle tissue (knots),
and nodules are identified for further treatment. The therapist will use his forearm to gently roll on the low back
area from the bilateral erector spinae muscles to both
thighs, and then continuously from the low back to the
gastrocnemius muscle through to the buttocks, for a total
of five minutes. During this time, the force and pressure
are gradually increased with the intention of smoothing
the Qi pathways to promote Qi movement in different
physiological layers. Then, the therapist will apply mild
force and pressure with overlapped palms to the lumbosacral area and lower limbs for five minutes, moving inferiorly and concluding with the gastrocnemius muscle. This
technique will be performed to resolve adhesions and
increase general circulation.
Step two: local pressing pain point manipulation The
pressing pain point, or namely A-Shi point in acupuncture theory, is the tender local dermal or muscular area.
It is generally recognized as reflecting the underlying
condition and is frequently manipulated to stop pain. In
this step, the therapist will apply muscle pressing, stripping, and deep tissue kneading to the pressing pain
point in the lumbar region in a direction perpendicular
to the erector spinae. The pressure and amplitude shall
be gradually intensified and enlarged throughout the
five-minute manipulation, which is intended to unblock
Qi stagnation, remove blood stasis by separating adherent fascicles, and resolve contracted nodules of muscle.
The amount of force used is determined by the patients
Deqi sensation, often described as a dull pain, heaviness,
numbness, or soreness, and commonly regarded as an
indicator of manipulation effectiveness in acupuncture
and tuina [38-40].
Step three: lumbar structural rectification Lumbar
structural rectification is performed after the above two
procedures have relieved the tensions of muscles and
soft tissues. The patient will be instructed to lie on his
or her side (with the affected side up). The affected leg
is slightly flexed at the hip and knee in a relaxed position, while the other leg is naturally extended on the
massage table. The therapist stands facing the patient
with two hands joined and elbows bent. One of the
therapists elbows will be fixed on the anterior aspect of
the patients shoulder, while the other will be placed in
the posterior-lateral aspect of the patients iliac bone, in
the gluteal area of the external hip rotators.
First, the therapist can exert a gentle torque to align
the patients lower back and perform a slight shake to
relax the area. Second, the therapist will push down
(toward the table) and stretch the patients shoulder
anteriorly while stretching the hips posteriorly, rotating
the lumbar vertebra along the spinal axis to release the
Yang et al. Trials 2014, 15:418
http://www.trialsjournal.com/content/15/1/418
Page 5 of 7
fixing points instantly. After the lumbar muscles are sufficiently relaxed by gentle tractions and twisting forces,
the therapist can twist the lumbar muscles slightly further to remove any remaining slack in them. The therapist shall hold this position for a moment and then made
an abrupt pulling motion to advance the stretch by 5 to
10 degrees.
Step four: tapping manipulation The therapist use his
or her palm to tap the lumbosacral area for two minutes
to generate a warm sensation in deep tissue, and then
rub the area superficial to the back pain, as well as the
bilateral lines of the urinary bladder meridian.
Conventional control group
Patients in the control group will receive a conventional
pharmacological treatment regimen of one 0.3 g capsule
of sustained-release ibuprofen, taken three times each day
(Ibuprofen Sustained Release Capsules, 0.3 g per capsule,
Sino-GlaxoSmithKline, Tianjin, China).
Study therapists
All practitioners in this trial are licensed TCM tuina
therapists with at least five years clinical experience in
the hospitals Tuina Department. Before taking part in
this trial, they will be required to complete a 40-hour
training course to master the study protocol. When
completed, clinicians will be required to pass an examination during which they are asked to recite the protocol
verbally and provide a demonstration of each technique.
Outcome measurements
The efficacy of massage therapy for the treatment of
CLBP is assessed by the primary outcome measure:
change in back pain and function from baseline as measured by the Roland-Morris Disability Questionnaire at
four time points (baseline, four, six, and eight weeks).
Secondary outcome measures also measured at these
four time points included the (i) 100-point visual analog
scale (VAS), (ii) Japanese Orthopedic Association Score
to assess the improvement of back function, and (iii)
McGill pain questionnaire to assess the alleviation of
pain. Table 1 demonstrates all measurements and measuring time points.
Safety
Therapeutic safety will be monitored by assessment of
patient symptoms as well as blood, urine, and stool tests
conducted pre- and post-treatment. Adverse events such
as changes in pain, syncope, vertigo, and lumbar function degradation, will be carefully recorded in the case
report form.
Table 1 Trial process chart
Period
Inclusion
Treatment
Follow-up
Assessment
Baseline
First
Second
Third
Measure point
0 weeks after inclusion
4 weeks after inclusion
6 weeks after inclusion
8 weeks after inclusion
Diagnosis and treatment
Inclusion confirmed
Informed consent
Body sign
Disease history
Treatment history
Comorbidity
Current treatment
Pain condition and lumbar function assessment
Visual Analogue Scale
Roland-Morris Disability Questionnaire
McGill pain questionnaire
Japanese Orthopedic Association Score
Data collection and statistical analysis
Adverse event
Causes of dropout
Safety analysis
Compliance analysis
Health economics
Yang et al. Trials 2014, 15:418
http://www.trialsjournal.com/content/15/1/418
Health economics
All costs associated with this trial will be recorded. They
primarily include the medical costs for direct treatment
of the CLBP, such as inpatient bed fees, medication fees,
massage treatment fees, usual care, and testing fees.
Additionally, any cost of treatment for adverse events
will be recorded and included in the health economics
evaluation.
Sample size calculation
Sample size was calculated by G*Power 3 software, developed by the Institute for Experimental Psychology
(Heinrich-Heine University, Germany). For this trial, it
was determined prospectively that =0.05 and 1- =0.90.
Consistent with a previous trial on massage for lumbar
disc herniation [41], a total of 150 participants will be included in this trial (75 in each group) to compensate for
an anticipated dropout rate of 15%.
Data analysis
Demographic and baseline data will be analyzed with
standard, descriptive statistics. Between-group differences will be tested using repeated measure analyses of
variance. The accepted level of significance for all analyses was P <0.05. The whole data analysis process will
be performed by statisticians who are independent from
the research team and blinded to the group settings.
SPSS software (SPSS 12.0 KO for Microsoft Windows
SPSS, Inc., Chicago, IL, USA ) was used to perform the
data analysis.
Discussion
The present trial is a comparative effectiveness study of
TCM tuina massage and conventional analgesics for
pain relief and function recovery in patients with CLBP.
The massage techniques used in this trial combine relaxation and structural massage methods applied in a manner which is consistent with TCM theory and is based
on recognition of the same energetic meridians and acupoints used in acupuncture.
According to TCM, a state of health reflects an underlying state of balance in the Qi and blood of the human
body. Pain is usually caused by obstruction of Qi and
consequently of blood circulation in the affected body
region. Pathogenic factors such as blood stasis, Qi stagnation, phlegm, dampness, and others can be identified
as causative factors in the blockage. Thus, the central
therapeutic goal of tuina is to remove energetic blocks
which lead to Qi stagnation. This leads to increased circulation and reduction of localized edema, which helps
to reduce associated pain.
The A-Shi point in TCM is the site on the body surface which reproduces the specific pain being treated
when it is gently pressed. Its location indicates the
Page 6 of 7
precise place where Qi and blood are blocked. Manipulation at the A-Shi point is done with the intention of removing the energetic block there to promote the free
movement of Qi and improve blood circulation in the
region. Studies have demonstrated that one mechanism
by which massage therapy appears to be clinically
beneficial is by reducing inflammation and promoting
mitochondrial biogenesis for repair of damaged skeletal
muscle [42].
A recent trial reported no clinically meaningful difference in the effectiveness of structural and relaxation
massage [43]. In contrast, this trial compares the efficacy
of a specific form of massage based on the principles of
TCM (tuina) with conventional analgesics (ibuprofen)
for pain relief and functional recovery in patients with
CLBP. Each of these types of massage is done with very
different intentions underlying theoretical frameworks.
Therefore, it is important to develop a degree of specificity in referring to a type of massage, both in research
and in prescribing clinical massage for a particular condition. There is no placebo control in this trial because
of the difficulties in designing a proper placebo for massage therapy which have been described by others [44].
A possible limitation of this study is that it may possibly
be difficult to maintain high compliance in follow-up,
due to the long interval since the completion of trial.
Proper actions, such as frequent telephone interview,
will be taken to improve compliance.
The design and methodological rigor of this trial will
allow for collection of valuable, high-quality data to
evaluate the efficacy of a specific tuina protocol for
treating CLBP, and so will contribute to providing a solid
foundation for the clinical treatment of CLBP, as well as
future research in massage therapy.
Trial status
This trial is recruiting patients now. Participant recruitment started in June 2013, and is expected to end in
December 2014.
Abbreviations
CLBP: Chronic Low Back Pain; CT: Computed tomography; JOAS: Japanese
Orthopedic Association Score; MRI: Magnetic resonance imaging;
NSAIDs: Nonsteroidal anti-inflammatory drugs; TCM: Traditional Chinese
Medicine; VAS: Visual Analogue Scale; ITT: Intention-to-Treat.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
FRL conceived of the study, and participated in its design. MXY participated
in the design of the study and coordination and drafted the manuscript.
XGH carried out the massage treatments for patients. YF participated in the
design of the study. HP recruited patients from inpatient department and
performed massage treatment. SFD interviewed patients before and after
treatment and collected clinical data. MYW recruited and screened eligible
participants from outpatient department. XJX assigned patients to either
massage group or control group. HZ participated in the design of the study
and performed the statistical analysis. ZHL participated in trial design and
Yang et al. Trials 2014, 15:418
http://www.trialsjournal.com/content/15/1/418
helped to prepare the manuscript. JC assessed treatment effectiveness and
collected clinical data. XL recruited patients from outpatient department. All
authors read and approved the final manuscript.
Acknowledgments
We thank Dr Kristin Jerger from Duke Integrative Medicine (Duke University,
Durham, North Carolina, United States) for her constructive suggestions and
tremendous help in manuscript revision. We also thank Dr Jie Yang from
Chengdu University of Traditional Chinese Medicine for her suggestions in
trial design and guidance in trial implementation.
This trial was financially supported by funds from the Science and
Technology Department of Sichuan province (grant number 2011SZ0302),
and funds from the National Scientific Foundation Committee (grant number
81102662).
Received: 20 June 2014 Accepted: 15 October 2014
Published: 29 October 2014
References
1. Hoy D, Brooks P, Blyth F, Buchbinder R: The epidemiology of low back
pain. Best Pract Res Clin Rheumatol 2010, 24:769781.
2. Lidgren L: The bone and joint decade 20002010. Bull World Health Organ
2003, 81:629629.
3. Andersson GB: Epidemiological features of chronic low-back pain. Lancet
1999, 354:581585.
4. Koes BW, van Tulder MW, Ostelo R, Burton AK, Waddell G: Clinical
guidelines for the management of low back pain in primary care: an
international comparison. Spine 2001, 26:25042513.
5. Waddell G, Burton AK: Occupational health guidelines for the
management of low back pain at work: evidence review. Occup Med
2001, 51:124135.
6. Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ: Outcome
of low back pain in general practice: a prospective study. BMJ 1998,
316:1356.
7. Pengel LH, Herbert RD, Maher CG, Refshauge KM: Acute low back pain:
systematic review of its prognosis. BMJ 2003, 327:323.
8. Stanton TR, Henschke N, Maher CG, Refshauge KM, Latimer J, McAuley JH:
After an episode of acute low back pain, recurrence is unpredictable
and not as common as previously thought. Spine 2008, 33:29232928.
9. Speed C: Low back pain. BMJ 2004, 328:11191121.
10. Dionne CE, Dunn KM, Croft PR: Does back pain prevalence really decrease
with increasing age? A systematic review. Age Ageing 2006, 35:229234.
11. Hoy D, March L, Brooks P, Woolf A, Blyth F, Vos T, Buchbinder R: Measuring
the global burden of low back pain. Best Pract Res Clin Rheumatol 2010,
24:155165.
12. Maetzel A, Li L: The economic burden of low back pain: a review of
studies published between 1996 and 2001. Best Pract Res Clin Rheumatol
2002, 16:2330.
13. Jenner J, Barry M: ABC of rheumatology: low back pain. BMJ 1995,
310:929.
14. Biyani A, Andersson GB: Low back pain: pathophysiology and
management. J Am Acad Orthop Surg 2004, 12:106115.
15. Balagu F, Mannion AF, Pellis F, Cedraschi C: Non-specific low back pain.
Lancet 2012, 379:482491.
16. Krismer M, Van Tulder M: Low back pain (non-specific). Best Pract Res Clin Rheumatol
2007, 21:7791.
17. Goodman DM, Burke AE, Livingston EH: JAMA patient page: low back
pain. JAMA 2013, 309:1738.
18. Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, Owens DK:
Diagnosis and treatment of low back pain: a joint clinical practice
guideline from the American College of Physicians and the American
Pain Society. Ann Intern Med 2007, 147:478491.
19. Mens J: The use of medication in low back pain. Best Pract Res Clin Rheumatol
2005, 19:609621.
20. Hernandez-Diaz S, Rodriguez LAG: Association between nonsteroidal
anti-inflammatory drugs and upper gastrointestinal tract bleeding/
perforation: an overview of epidemiologic studies published in the
1990s. Arch Intern Med 2000, 160:2093.
21. van Tulder MW, Scholten RJ, Koes BW, Deyo RA: Nonsteroidal anti-inflammatory
drugs for low back pain: a systematic review within the framework of the
Cochrane Collaboration Back Review Group. Spine 2000, 25:25012513.
Page 7 of 7
22. Watkins PB, Kaplowitz N, Slattery JT, Colonese CR, Colucci SV, Stewart PW,
Harris SC: Aminotransferase elevations in healthy adults receiving 4
grams of acetaminophen daily. JAMA 2006, 296:8793.
23. Maniadakis N, Gray A: The economic burden of back pain in the UK.
Pain 2000, 84:95103.
24. Goats GC: Massagethe scientific basis of an ancient art: Part 1:
the techniques. Br J Sports Med 1994, 28:149152.
25. Goats GC: Massagethe scientific basis of an ancient art: Part 2:
physiological and therapeutic effects. Br J Sports Med 1994, 28:153156.
26. Ernst E: The safety of massage therapy. Rheumatology 2003, 42:11011106.
27. Moyer CA, Rounds J, Hannum JW: A meta-analysis of massage therapy
research. Psychol Bull 2004, 130:3.
28. Field T: Massage therapy. Med Clin North Am 2002, 86:163.
29. Weinrich SP, Weinrich MC: The effect of massage on pain in cancer
patients. Appl Nurs Res 1990, 3:140145.
30. Field T, Hemandez-Reif M, Taylor S, Quintino O, Burman I: Labor pain is reduced
by massage therapy. J Psychosom Obstet Gynaecol 1997, 18:286291.
31. Field TM: Massage therapy effects. Am Psychol 1998, 53:1270.
32. Kumar S, Beaton K, Hughes T: The effectiveness of massage therapy for
the treatment of nonspecific low back pain: a systematic review of
systematic reviews. Int J General Med 2013, 6:733.
33. Lewis M, Johnson MI: The clinical effectiveness of therapeutic massage
for musculoskeletal pain: a systematic review. Physiotherapy 2006,
92:146158.
34. Furlan AD, Imamura M, Dryden T, Irvin E: Massage for low-back pain.
Cochrane Database Syst Rev 2008, CD001929: 1-104.
35. Xue CC, English R, Zhang JJ, Da Costa C, Li CG: Effect of acupuncture in
the treatment of seasonal allergic rhinitis: a randomized controlled
clinical trial. Am J Chinese Med 2002, 30:111.
36. Luo C, Wang F: Chinese Tuina Therapeutics. Beijing: Peoples Medical
Publishing House; 2003.
37. Luo C, Lv Z: A clinical resport of the effectiveness of massage therapy for 40
cases of chronic low back pain. Chin Manipulation Qi Gong Ther 1995, 6:78.
38. Hui KK, Nixon EE, Vangel MG, Liu J, Marina O, Napadow V, Hodge SM, Rosen
BR, Makris N, Kennedy DN: Characterization of the deqi response in
acupuncture. BMC Complement Altern Med 2007, 7:33.
39. Kong J, Gollub R, Huang T, Polich G, Napadow V, Hui K, Vangel M, Rosen B,
Kaptchuk TJ: Acupuncture de qi, from qualitative history to quantitative
measurement. J Altern Complement Med 2007, 13:10591070.
40. Shi G-X, Yang X-M, Liu C-Z, Wang L-P: Factors contributing to therapeutic
effects evaluated in acupuncture clinical trials. Trials 2012, 13:15.
41. Huang K-Y, Xia H-M: Massage for treatment of lumbar disc herniation in
371 cases of efficacy. J Clin Acupunct Moxibustion 2010, 3:019.
42. Crane JD, Ogborn DI, Cupido C, Melov S, Hubbard A, Bourgeois JM,
Tarnopolsky MA: Massage therapy attenuates inflammatory signaling
after exercise-induced muscle damage. Sci Transl Med 2012, 4:3002882.
43. Cherkin DC, Sherman KJ, Kahn J, Wellman R, Cook AJ, Johnson E, Erro J,
Delaney K, Deyo RA: A comparison of the effects of 2 types of massage
and usual care on chronic low back pain: a randomized, controlled trial.
Ann Intern Med 2011, 155:19.
44. Machado L, Kamper S, Herbert R, Maher C, McAuley J: Analgesic effects
of treatments for non-specific low back pain: a meta-analysis of
placebo-controlled randomized trials. Rheumatology 2009, 48:520527.
doi:10.1186/1745-6215-15-418
Cite this article as: Yang et al.: Effectiveness of Chinese massage
therapy (Tui Na) for chronic low back pain: study protocol for a
randomized controlled trial. Trials 2014 15:418.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Handbook of Pediatric Anesthesia (2015)Document363 pagesHandbook of Pediatric Anesthesia (2015)Sanna Huhtamaki100% (5)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- q2 Grade 9 Pe DLL Week 1Document11 pagesq2 Grade 9 Pe DLL Week 1Airaa A. Baylan88% (8)
- Mount Sinai Obstetrics and Ginecology 2020Document414 pagesMount Sinai Obstetrics and Ginecology 2020David Bonnett100% (1)
- Humanization and Work in NursingDocument5 pagesHumanization and Work in NursingAna BarbaraNo ratings yet
- Indivíduo e Pessoa Na Experiência Da SaúdeDocument11 pagesIndivíduo e Pessoa Na Experiência Da SaúdeCleber Rangel ZanettiNo ratings yet
- Systematic Review 2011 Full ReportDocument233 pagesSystematic Review 2011 Full ReportAna BarbaraNo ratings yet
- Šijacu I Bol U VratuDocument20 pagesŠijacu I Bol U VratuLjubica SaranNo ratings yet
- Shiatsu and M EDocument9 pagesShiatsu and M EAna BarbaraNo ratings yet
- A Review of The EvidenceDocument130 pagesA Review of The Evidenceapi-26008400No ratings yet
- Shiatsu Final ReportDocument291 pagesShiatsu Final ReportAna BarbaraNo ratings yet
- Šijacu I Bol U VratuDocument20 pagesŠijacu I Bol U VratuLjubica SaranNo ratings yet
- Oriental MassageDocument8 pagesOriental MassageAna BarbaraNo ratings yet
- Shiatsu and ME Chronic Fatigue SyndromeDocument11 pagesShiatsu and ME Chronic Fatigue SyndromeAna BarbaraNo ratings yet
- PeteItni Trauma EDocument9 pagesPeteItni Trauma EAna BarbaraNo ratings yet
- PT - 1806 0013 Rdor 16 01 0053Document7 pagesPT - 1806 0013 Rdor 16 01 0053Ana BarbaraNo ratings yet
- NIH Public Access: Author ManuscriptDocument14 pagesNIH Public Access: Author ManuscriptAna BarbaraNo ratings yet
- HEALING BEGINS IN THE HARADocument4 pagesHEALING BEGINS IN THE HARAAna BarbaraNo ratings yet
- Et Al-2007-Journal of Gastroenterology and HepatologyDocument19 pagesEt Al-2007-Journal of Gastroenterology and HepatologyAna BarbaraNo ratings yet
- Et Al-2007-Journal of Gastroenterology and HepatologyDocument19 pagesEt Al-2007-Journal of Gastroenterology and HepatologyAna BarbaraNo ratings yet
- PT - 1806 0013 Rdor 16 01 0053Document7 pagesPT - 1806 0013 Rdor 16 01 0053Ana BarbaraNo ratings yet
- Syllabus Form: Southern California University School of Oriental Medicine and AcupunctureDocument2 pagesSyllabus Form: Southern California University School of Oriental Medicine and AcupunctureAna BarbaraNo ratings yet
- Merged PDF 2021 11 16T12 - 01 - 01Document15 pagesMerged PDF 2021 11 16T12 - 01 - 01Ericsson CarabbacanNo ratings yet
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDocument2 pagesNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDeanne Carla DalilisNo ratings yet
- Autopsy PDFDocument3 pagesAutopsy PDFstprepsNo ratings yet
- Referensi Nomor 5Document4 pagesReferensi Nomor 5audreynatalia777No ratings yet
- Acute Stroke TreatmentDocument77 pagesAcute Stroke TreatmentRohitUpadhyayNo ratings yet
- Cutaneous Leishmania: Dr. Vijayakumar Unki Asst Professor VCGDocument16 pagesCutaneous Leishmania: Dr. Vijayakumar Unki Asst Professor VCGLohith MCNo ratings yet
- Wa0008.Document2 pagesWa0008.Mmangaliso KhumaloNo ratings yet
- Etiology of Eating DisorderDocument5 pagesEtiology of Eating DisorderCecillia Primawaty100% (1)
- Current Liberty Healthcare ContractDocument46 pagesCurrent Liberty Healthcare ContractABC10No ratings yet
- Ajab SinghDocument2 pagesAjab SinghapNo ratings yet
- 02-09 2022 Pharm Pediatrics 2022 R4Document44 pages02-09 2022 Pharm Pediatrics 2022 R4Amira HelayelNo ratings yet
- Treating pediatric patients with fever, weakness and respiratory distressDocument1 pageTreating pediatric patients with fever, weakness and respiratory distresshandykavebigNo ratings yet
- Verorab Drug StudyDocument2 pagesVerorab Drug StudyHanna SeNo ratings yet
- Vas 1Document10 pagesVas 1Abdul Latiful KhabirNo ratings yet
- Volunteer Report FinalDocument11 pagesVolunteer Report FinalBeenish JehangirNo ratings yet
- AnalgesicDocument56 pagesAnalgesicMuhammad hilmiNo ratings yet
- Rajiv Gandhi College of Nursing BSC Nursing 1St Year 2020 Fundamental of Nursing Pathology SetbDocument3 pagesRajiv Gandhi College of Nursing BSC Nursing 1St Year 2020 Fundamental of Nursing Pathology SetbNeenu RajputNo ratings yet
- The Blood Circulatory SystemDocument3 pagesThe Blood Circulatory SystemListiyani IsmailNo ratings yet
- RETDEMDocument2 pagesRETDEMDoneva Lyn MedinaNo ratings yet
- Surgery and Post OpDocument96 pagesSurgery and Post OpNguyễn Nhật HoàngNo ratings yet
- Mata Merah Visus TurunDocument27 pagesMata Merah Visus TurunErinNo ratings yet
- RCOG - Management of Suspected Ovarian Masses in Premenopausal WomenDocument14 pagesRCOG - Management of Suspected Ovarian Masses in Premenopausal WomenGabriela Andrade AriasNo ratings yet
- CNS Drug StudyDocument4 pagesCNS Drug StudyMAHUSAY JOYCE CARINANo ratings yet
- Guidelines For The Surgical Treatment of Esophageal Achalasia PDFDocument24 pagesGuidelines For The Surgical Treatment of Esophageal Achalasia PDFInomy ClaudiaNo ratings yet
- Surgical Audit and Peer Review Guide 2014Document54 pagesSurgical Audit and Peer Review Guide 2014juweriyNo ratings yet
- Arthritis Fact SheetDocument2 pagesArthritis Fact SheetClaire MachicaNo ratings yet
- Asepsis and Aseptic Practices in The Operating RoomDocument6 pagesAsepsis and Aseptic Practices in The Operating RoomMichelle ViduyaNo ratings yet