Professional Documents
Culture Documents
Laryngopharyngeal Reflux: A Review of New Diagnostic Methods
Uploaded by
Eve MacíasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Laryngopharyngeal Reflux: A Review of New Diagnostic Methods
Uploaded by
Eve MacíasCopyright:
Available Formats
REVIEW ARTICLE
Rev. Otorrinolaringol. Cir. Head Neck 2015; 75: 61-66
PHARYNGOLARYNGEAL REFLUX:
REVIEW OF NEW DIAGNOSTIC METHODS
Laryngopharyngeal reflux: A review of new diagnostic methods
Christian Olavarria L1, Pedro Cortez v1.
SUMMARY
The pharyngo laryngeal reflux (RFL) is a common cause of morbidity upper
aerodigestive tract. Despite its high prevalence, there is still controversy
regarding the diagnostic accuracy of this disease and its pathophysiology and
management. Current diagnostic tests still have significant limitations, hence
arises the interest in finding fast and efficient methods that will improve their
research. This paper aims to review the current literature regarding the methods
available for diagnosis.
Keywords: Laryngitis, pharyngolaryngeal reflux, pH-metry, pepsin in saliva.
ABSTRACT
The laryngopharyngeal reflux is a common cause of morbidity of the upper
aero- gestive tract. DESPITE ITS high prevalence, there is still controversy
Regarding the accuracy of diag- Nostitz esta disease and Its pathophysiology and
management. The current diagnostic test Still Have significant Limitations,
HENCE the interest Arises to find fast and efficient methods to Improve Their
research. This paper AIMS to review the current litera- ture available methods for
diagnosis Regarding.
Key words: Laryngitis, laryngopharyngeal reflux, pH monitoring, Salivary
pepsin test.
INTRODUCTION
The RFL, corresponding to a variant of
gastroesophageal reflux disease (GERD) is
a condition most commonly diagnosed in
practice otorrinolarin-
gologa. It is estimated that the prevalence of
RFL 10% -30% of the population occidental1.
In 2006, the Montreal Consensus defined the
existence of established extraesophageal
syndromes that manifest with coughing,
laryngitis, asthma and erosionsdentales2.
Department of Otolaryngology, University of Chile Clinical Hospital.
Received August 17, 2014. Accepted October 12, 2014.
EBB FARINGEOLARNGEO: REVIEW OF NEW DIAGNOSTIC TESTS - Ch Olavarria, P Cortez
Interest has grown substantially RFL in the
last two decades. Despite the large
number of existing studies on the subject,
controversy still exists regarding the
diagnostic accuracy of the disease, its
pathophysiology and treatment efficacy.
Current diagnostic tests still have
significant limitations, hence arises the
interest in finding fast and efficient
methods to improve the diagnostic
approach.
The
role
of
upper
gastrointestinal endoscopy (EDA) in
GERD is very limited, because the
prevalence of endoscopic findings in
patients with symptoms of GERD does not
exceed 30% 3. Reflux measurement using
the quite acceptable ambulatory pH
monitoring and / or monitoring the
impedance as a diagnostic test for GERD
Ticos have sensitivity (77% -100%) and
specificity (85% -100%) in patients with
signs of esophagitis endoscpica4 .
However the sensitivity is much lower in
normal cases EDA. Then both the EDA as
ambulatory monitoring test are suboptimal
reflux for diagnosis of GERD besides
being costly and invasive. This is
magnified in the diagnosis of reflux
disease
extraesophageal,
the
low
sensitivity of the EDA, monitoring of pH
and
unspecific
findings
nasofibrolaryngoscopy (NFL).
In recent years he has appeared in the
market place a device for rapid detection of
pepsin in saliva, which is proposed as an
objective method to diagnose reflux
(PEPTESTTM).
The reason of this article is to review
the current evidence on new diagnostic
methods in the RFL.
PHYSIOPATHOLOGY
It is believed that the RFL is caused by the
backflow of gastric contents (particularly
acid and pepsin) affecting the pharyngeal
mucosa and laryngeal by direct contact or
by a secondary mechanism. The latter
could be given by acid irritation of the
distal esophagus, causing chronic cough
and hoarseness mediated by the vagus
nerve and thus act as a factor of larngeo5
mechanical damage. Furthermore, it has
shown that the reflux of bile salts can also
cause irritation of the mucosa larngea6,7.
In 2010,
Habesoglu8 et al demonstrated in an
animal model that exposure of the
laryngeal mucosa to acid and pepsin
causes edema of the lamina propria,
submucosal glands hyperplasia and
muscle wasting. Erickson and cols9
reported that less than three episodes per
week acid reflux over the laryngeal
mucosa are sufficient to cause histological
changes in the vocal cords, unlike the
mucosa of distal esophagus that is able to
tolerate up to 50 reflux episodes per day
and It is considered physiological in this
area.
It is likely that patients with poor
response to acid suppression may have
involvement of other components of gastric
reflux, such as pepsin and bile acids.
Pepsin is the main proteolytic enzyme produced in the stomach. It has been shown
that pepsin is present in the laryngeal
epithelium of patients with laryngeal
disease attributed to reflujo10. Even it has
been determined significant association
between the presence of pepsin in
laryngeal epithelium in patients with RFL
and depletion two proteins which provide
protection to the mucosa of the larynx. One
is the carbonic anhydrase isoenzyme III
(CAIII) and the other is the stress protein
epithelial squamous tissue (Sep70) 11. It is
known that the maximum activity of
pepsinis achieved in an acidic (pH
medium <2) and it is quenched with pH>
6.5, average normal pH being in
pharyngolaryngeal 6.8. Using an animal
model in vitro it was determined that the
pepsin which is isolated in the laryngeal
mucosa after an event reflux can be kept
inactive until at least 24 hours (at a pH
not more than 8 at 37 C temperature) ,
being capable of reactivating up to 80%
of its enzymatic capacity when the pH in
its surroundings reacidifica12.
Revista from ORtORRinOlaRingOlOga
CURGERY from Cabeza Y Cuello
DIAGNOSIS
therapeutic
trial
Whereas RGE / RFL is a phenomenon that
occurs in 65% -75% of people sanas13,
and
despite the many published studies, there
is still no test to be considered a true gold
standard for detecting RFL patolgico13fifteen. Until now, the diagnosi
of reflux extraesophageal is based on clinical
suspicion added either to the response to
inhibitors
proton
pump
(PPIs)
or
supraesofgico positivos16 pH studies.
Proponents of the "therapeutic trial" with
PPIs are based on the absence of welldefined criteria and methods for detecting
the presence of supraesofgico reflux and
the low correlation between reflux events
and response to IBPs17,18. The answer to
this "therapeutic trial" with PPIs, still lacks
serious well-controlled studies to allow
razonables15 draw conclusions.
pH
monito
ring
The group cols19 Ayazi and pose a new
paradigm for diagnosing based RFL loss
alkalinization in the cervical esophagus.
They observed in patients with RFL, an
inability to maintain a neutral pH in this
area, based on a higher exposure at pH
<4 and less exposure to pH 7 compared
to healthy patients. These authors
suggest that sensitivity to detect abnormal
reflux and its causal relationship to
faringolarngeos symptoms increases
when considering both the highest
percentage of time pH <4 is recorded as
the lowest percentage of time with pH 7.
They I consider that the loss of an alkaline
medium (pH 7) in the cervical
esophagus is an indicator of decreased
ability to protect tissue from damage, in
contrast to the time pH <4, which until
now has been accepted to cause
pathological changes associated with
RFL19 symptomatology. At the moment,
the pH-metry 24 hrs is the most relevant
to quantify esophageal reflux in patients
with symptoms of RGE20 examination.
Originally, a catheter with a single sensor
located 5 cm above the lower esophageal
sphincter (LES) was used. Subsequently,
a second sensor to this level probe was
added hypopharynx, becoming long
regarded as the gold standard for
diagnosis of RFL. However there is still no
consensus on the location of the sensors,
the number of required sensors and
interpretation of results. In 2009 the
company Restech developed a test that
measures both pH "I aerosolized" as the
liquid environment of the oropharynx, one
test less
invasive and more tolerable for the patient
with good clnico21 result. This company
and group study raise even the
traditional criterion of pH <4 as an
indicator of RFL is not usable in the
oropharynx. They suggest that a
significant event would be one that
exceeds the 3.5 "standard deviations"
base22 pH.
Sato and cols23 described their
experience by using a monitoring system
pH-metry 24 hrs using 4 sensors. The
proximal located in hypopharynx, the
second in the middle third that- phage,
the third a few cm on IAS (5 cm not like
the other) and the distal located in the
stomach. Have the advantage of being
able to record simultaneously the pH in
all these localities tions can compare the
relationship between them. The problem
is that it is not possible to assimilate its
results with other tests that have
esophageal sensor 5 cm from the ISS. In
his studies they conclude that both the
values of pH less than 4 and less than 5
are significant and indicators of RFL.
intraluminal impedance
The multichannel intraluminal impedance
monitoring associated with pH (IIM / ph)
is a relatively new technique that is
EBB FARINGEOLARNGEO: REVIEW OF NEW DIAGNOSTIC TESTS - Ch Olavarria, P Cortez
considered the gold standard in current
detection RFL20. This test can detect
reflux episodes in its liquid form, or in the
form of gas or mixed. Even detects both
acid reflux as acid. MII is based on
changes in electrical resistance to flow of
an electric current between two
electrodes placed on a probe, when a
liquid, semisolid or gaseous bolus
passes between ellos24. In general,
several "suitable for age" for studies of
impedance
catheters
are
used.
Impedance sensors 7 are placed along
each catheter, resulting 6 channels
corresponding impedance. The pH
electrode is placed in the center of the
space (infant and pediatric catheters)
more distant sensor impedance or
impedance sensor space that is
immediately next to it (catheters for
adults). There are also catheters with 2
pH measurement points. Areflux episode
impedance is defined as a drop in
intraluminal impedance 50% from
baseline retrograde mode progresses
through two or more of the more distant
channels. Acid is considered an episode
when the esophageal pH decreases and
remains in <4 for at least 5 seconds. An
episode is considered non acid when the
This new questionnaire is that it is able to
discriminate between patients with RFL of
those who do not have.
Detection of pepsin
As discussed above, pepsin plays an important
role in the pathophysiology of reflux-related
disorders. So that detection has been considered
as a diagnostic marker in the RFL30 and may
pesquisarla in airway secretions when gastric
and well below the concentration of pepsin in gastric
juice is 269 ng / ml.
pH increases, remains unchanged or
decreases by 1 pH unit while remaining
4.
Lee et al25 documented a substantial
increase in the diagnosis of reflux using
this test Classic respect pH monitoring.
Loots and cols26 reported an increase in
diagnostic performance by combining the
IIM with esophageal pH monitoring in
children and infants with confirmed reflux.
Questionnaire and indexes
The rate of reflux symptoms (RSI - Reflux
Symptom Index) 27 [Table 1] was
designed to measure the severity of
laryngeal symptoms, and the score of
endoscopic findings of reflux (RFS Reflux Finding Score) 28 [Table 2], is
used to grade the laryngeal findings
fibroscopy. Both tools have been used for
more than a decade, helping in the
clinical approach to the diagnosis of RFL.
In recent years, Anderson and cols29,
developed a questionnaire pharyngeal
reflux
symptoms,
self-administered,
which has a strong correlation with the
RSI. The main advantage
reflux has occurred for a period of time. In 2010,
Wang and cols31 correlated concentrations of
pepsin secretion in oral> 0,108 ng / ml detected
by ELISA with RSI> 10, RFS> 8 and in groups of
patients with obstructive sleep apnea syndrome
moderate to severe sleep. They concluded that
there are significant differences in the levels of
pepsin in oral secretions of patients with RFL and
healthy patients (p = 0.000). The concentration of
pepsin average EOL group was 199 ng / ml,
consistent with that reported by Knight and cols31
A few years ago appeared on the market a device for detecting pepsin in saliva (PepTest - RT
Biomed, www.rdbiomed.com) is available in recent months in our country. It is a simple, inexpensive,
non-invasive, which allows detecting pepsin in saliva through two monoclonal antibodies against
pepsin-3, to detect and to capture another pepsin if present in the sample. This test has the ability to
detect pepsin saliva around a concentration of 16 ng / ml up and can be performed a
semiquantitative interpretation of its concentration according to the signal intensity of positivity
Revista from ORtORRinOlaRingOlOga
CURGERY from Cabeza Y Cuello
regarding control. There are still many studies to demonstrate real utility, but performance test
according Saritas and cols33 show a sensitivity = 50%, specificity = 92%, VPP
= 85% and NPV = 68% in the group of patients with esophagitis and GERD defined by pH-metry
altered. This was the first study with an "n" substantial, prospective and blind mentions the
characteristics of this test both in vitro and in patients with RGE. One of the benefits of this test
would be the possibility of dispensing with an upper endoscopy and / or pH-metry in cases of
positive PepTest.
CONCLUSION
The RFL is an extremely prevalent condition, despite the substantial increase in research in the last
decade, remains a matter of discussion, both in its pathophysiology and diagnostic criteria. The
diagnostic technology has improved considerably in recent years but still its diagnosis remains
controversial. It is important to keep up with advances in the study of the pathophysiology and new
diagnostic methods, as well as a critical evaluation of them, provided irlos gradually adding to daily
clinical practice.
BIBLIOGRAPHY
1. gRoome M. Prevalence of Laryngopharyngeal Reflux in a Population With Gastroesophageal
Reflux. Laryngoscope 2007; 117: 1424-8.
2. vakil n, v ton zbeforen s, k aHRilas P, andt to the. T h e Montreal definition and Classification of
GERD: a global evience-based consensus. Am J Gastroenterol 2006; 101: 1900-1920.
3. POH CH, Ga-R. Upper GI tract finsdigs in Patients With hearthburn in Whom proton pump inhibitor
treatment failed antireflux vs Those not receiving treatment. Gastrointest Endosc 2010; 71: 28-34.
4. lACY b, wEiser k, CHeRtOff J, et to the. The diagnosis of GERD. Am J Med 2010; 123: 583-92.
5. kOllaRik M, Ror F, orNDEM b, et to the. Acid-sensitive vagal sensory pathways and cough. Pulm
Pharmacol Ther 2007; 20: 402-11.
6. galli J, C to theOR l, t o GostinOR s, andt to the. B i l and R e flux as possible risk factor in
laryngopharyngeal inflammatory and neoplastic lesions. Ital Otorhinolaryngol Act 2003; 23:
377-82.
7. M aHMOud to, sHruti P, andt to the. Bile Acids in Laryngopharyngeal refluxate: Will They or
Attenuate Enhance the Action of Pepsin? Laryngoscope 2013; 123: 434-9.
8. HabesOglor t, HabesOglor M, surmeli M, andt to the. histological Changes With soft palate of rat
experimental expopsure to laryngopharyngeal reflux. Auris nasus Larynx 2010; 37: 730-6.
E mail:christian.olavarria@gmail.com
You might also like
- Reflux Laryngitis: An Update, 2009-2012: Philadelphia, Pennsylvania, and Ylancaster, CaliforniaDocument9 pagesReflux Laryngitis: An Update, 2009-2012: Philadelphia, Pennsylvania, and Ylancaster, CaliforniaJaime Crisosto AlarcónNo ratings yet
- Is Pepsin Detected in The Saliva of Patients Who Experience Pharyngeal Reflux?Document5 pagesIs Pepsin Detected in The Saliva of Patients Who Experience Pharyngeal Reflux?anon_740277752No ratings yet
- Sensitive Pepsin Immunoassay...Document6 pagesSensitive Pepsin Immunoassay...Peter SalimNo ratings yet
- Laryngopharyngeal Reflux Diagnosis, Treatment, and Latest ResearchDocument8 pagesLaryngopharyngeal Reflux Diagnosis, Treatment, and Latest ResearchfrizkapfNo ratings yet
- The Laryngoscope - 2019 - Weitzendorfer - Pepsin and Oropharyngeal PH Monitoring To Diagnose Patients WithDocument7 pagesThe Laryngoscope - 2019 - Weitzendorfer - Pepsin and Oropharyngeal PH Monitoring To Diagnose Patients WithfelitaNo ratings yet
- Saliva Pepsin Detection and Proton Pump Inhibitor Response in Suspected Laryngopharyngeal Re UxDocument6 pagesSaliva Pepsin Detection and Proton Pump Inhibitor Response in Suspected Laryngopharyngeal Re UxFuyumi RiaNo ratings yet
- 1678 4219 Ag s0004280320200000028 PDFDocument4 pages1678 4219 Ag s0004280320200000028 PDFTOMOKO TERUYANo ratings yet
- Upper GI Surgery for Laryngopharyngeal RefluxDocument4 pagesUpper GI Surgery for Laryngopharyngeal Refluxaulia sufarnapNo ratings yet
- Vaezi LPR More Questions Than Answers CC 2010Document8 pagesVaezi LPR More Questions Than Answers CC 2010Phoespha MayangSarieNo ratings yet
- Gerd in Subglottic StenosisDocument5 pagesGerd in Subglottic StenosisPantelis ChouridisNo ratings yet
- Wang 2012Document7 pagesWang 2012priskaNo ratings yet
- LPR vs GERD: Understanding the DifferenceDocument3 pagesLPR vs GERD: Understanding the DifferenceWilhelm HeinleinNo ratings yet
- PPI Role Laryngopharyngeal RefluxDocument5 pagesPPI Role Laryngopharyngeal RefluxROBINSON ELIOTT GONZ�LEZ P�EZNo ratings yet
- Aliment Pharmacol Ther - 2001 - Fackler - Ambulatory Gastric PH Monitoring Proper Probe Placement and Normal ValuesDocument8 pagesAliment Pharmacol Ther - 2001 - Fackler - Ambulatory Gastric PH Monitoring Proper Probe Placement and Normal ValuesSofia CorreaNo ratings yet
- Corpus GastritisDocument5 pagesCorpus Gastritisameer143No ratings yet
- Reflux LaryngitisDocument6 pagesReflux LaryngitisfahmimiraNo ratings yet
- PediatricsDocument7 pagesPediatricsbravoirvingNo ratings yet
- Lechien Saussez Karkos Curr Opin 2018Document12 pagesLechien Saussez Karkos Curr Opin 2018alivanabilafarinisaNo ratings yet
- Reflux and LaryngitisDocument7 pagesReflux and LaryngitisyannecaNo ratings yet
- 571 FullDocument7 pages571 FullMilav AliNo ratings yet
- Del Gaudio 2005Document12 pagesDel Gaudio 2005Rodrigo Felipe Toro MellaNo ratings yet
- Veterinary Internal Medicne - 2022 - Appelgrein - Quantification of Gastroesophageal Regurgitation in Brachycephalic DogsDocument8 pagesVeterinary Internal Medicne - 2022 - Appelgrein - Quantification of Gastroesophageal Regurgitation in Brachycephalic DogsRenato HortaNo ratings yet
- Monitoreo de Reflujo Ambulatorio para El Diagnóstico de La Enfermedad Por Reflujo Gastroesofágico Actualización Del Consenso de Oporto y Recomendaciones de Un Grupo de Consenso InternacionalDocument15 pagesMonitoreo de Reflujo Ambulatorio para El Diagnóstico de La Enfermedad Por Reflujo Gastroesofágico Actualización Del Consenso de Oporto y Recomendaciones de Un Grupo de Consenso Internacionalcaresq1340No ratings yet
- 1 s2.0 S0196070920301198 MainDocument5 pages1 s2.0 S0196070920301198 MainMeutia LaksaniNo ratings yet
- Clinical Manifestations and Role of Proton Pump Inhibitors in The Management of Laryngopharyngeal RefluxDocument12 pagesClinical Manifestations and Role of Proton Pump Inhibitors in The Management of Laryngopharyngeal RefluxElisa Vina JayantiNo ratings yet
- Globus Pharyngeus: A Review of Etiology, Diagnostics, and TreatmentDocument10 pagesGlobus Pharyngeus: A Review of Etiology, Diagnostics, and TreatmentMiguel QNo ratings yet
- Novel scintigraphic study finds asymptomatic volunteers experience upright gastroesophageal refluxDocument7 pagesNovel scintigraphic study finds asymptomatic volunteers experience upright gastroesophageal refluxMarylin Acuña HernándezNo ratings yet
- Saliva Transit and GERDDocument6 pagesSaliva Transit and GERDjmccoyNo ratings yet
- PH SalivaDocument5 pagesPH SalivaBia KneippNo ratings yet
- Esophageal Baseline Impedance Levels Diagnose NERDDocument8 pagesEsophageal Baseline Impedance Levels Diagnose NERDFhienovdhieyHa ThreuvHyNo ratings yet
- Background: Reflux LaryngitisDocument5 pagesBackground: Reflux LaryngitisElisa Vina JayantiNo ratings yet
- 38.park2006 Diagnosis of Laryngopharyngeal Reflux AmongDocument5 pages38.park2006 Diagnosis of Laryngopharyngeal Reflux AmongWahyu JuliandaNo ratings yet
- 4) bilis y acidoDocument7 pages4) bilis y acidopbchantaNo ratings yet
- Changing Trends of Color of Different Laryngeal Regions in Laryngopharyngeal Reflux DiseaseDocument5 pagesChanging Trends of Color of Different Laryngeal Regions in Laryngopharyngeal Reflux DiseaseNoviTrianaNo ratings yet
- 17 Ambulatory-pH-and-Impedance-Monitoring CLC Mortensen 2019Document3 pages17 Ambulatory-pH-and-Impedance-Monitoring CLC Mortensen 2019Judy AncyNo ratings yet
- Aga: Clinical Practice UpdateDocument12 pagesAga: Clinical Practice UpdatextineNo ratings yet
- GERD SchwartzDocument10 pagesGERD SchwartzMina Tharwat AzerNo ratings yet
- Laryngopharyngeal Reflux and Atypical GERD 2019Document16 pagesLaryngopharyngeal Reflux and Atypical GERD 2019Thespian VentrueNo ratings yet
- Final-clean-Revised Version Respiratory Manifestations GERDocument11 pagesFinal-clean-Revised Version Respiratory Manifestations GERDewiNo ratings yet
- Clinical Medicine Insights: Ear, Nose, ThroatDocument5 pagesClinical Medicine Insights: Ear, Nose, ThroatagustinadianasariaguNo ratings yet
- Pendekatan Diagnostik Refluks Laring Faring: Karin I. Rompas, Steward K. Mengko, Ora Et Labora I. PalandengDocument9 pagesPendekatan Diagnostik Refluks Laring Faring: Karin I. Rompas, Steward K. Mengko, Ora Et Labora I. PalandengFannyNo ratings yet
- Stricture EsofagealDocument11 pagesStricture EsofagealInes Camilla PutriNo ratings yet
- Original Articles: Proton Pump Inhibitor Therapy For Chronic Laryngo-Pharyngitis: A Randomized Placebo-Control TrialDocument9 pagesOriginal Articles: Proton Pump Inhibitor Therapy For Chronic Laryngo-Pharyngitis: A Randomized Placebo-Control TrialAnonymous iM2totBrNo ratings yet
- Laparoscopic and Open Nissen Fundoplication: Preoperative EvaluationDocument11 pagesLaparoscopic and Open Nissen Fundoplication: Preoperative EvaluationLuis FelipeNo ratings yet
- 55.wilson1989pharyngoesophageal DysmotilityDocument5 pages55.wilson1989pharyngoesophageal DysmotilityWahyu JuliandaNo ratings yet
- LkjkusteiDocument8 pagesLkjkusteiPeriyasami GovindasamyNo ratings yet
- LPRDocument6 pagesLPRGoranJankovicNo ratings yet
- Hubungan Nilai PH Cairan Pleura Dengan Hasil Pleur PDFDocument6 pagesHubungan Nilai PH Cairan Pleura Dengan Hasil Pleur PDFHerliNo ratings yet
- Alimentary Pharmacology & TherapeuticsDocument7 pagesAlimentary Pharmacology & TherapeuticsArchie TobiasNo ratings yet
- Laryngeal Manifestations of Gastroesophageal Reflux DiseaseDocument7 pagesLaryngeal Manifestations of Gastroesophageal Reflux DiseaseAna BrankovićNo ratings yet
- Effect of An Antireflux Bed Wedge On Gastro Esophageal Reflux Symptoms and Acid Reflux 1467Document5 pagesEffect of An Antireflux Bed Wedge On Gastro Esophageal Reflux Symptoms and Acid Reflux 1467abel assefaNo ratings yet
- Literatur - Rohs, Et - Al. Esomeprazole Compared To Other PPIsDocument9 pagesLiteratur - Rohs, Et - Al. Esomeprazole Compared To Other PPIsChristine LilyanaNo ratings yet
- Joevence - Journal ArticleDocument15 pagesJoevence - Journal ArticleJoevence CuaresmaNo ratings yet
- Role of Gastroesophageal Reflux Disease in Asthmatic PatientsDocument10 pagesRole of Gastroesophageal Reflux Disease in Asthmatic PatientsWindy Gigiers SeptianiNo ratings yet
- Anticholinergic Medication Use Is Associated With Globus Pharyngeus (HAFT 2016)Document5 pagesAnticholinergic Medication Use Is Associated With Globus Pharyngeus (HAFT 2016)DANDYNo ratings yet
- Laryng Reflux 090825Document12 pagesLaryng Reflux 090825Putri SilviaNo ratings yet
- Diagnosis and Management of Functional HeartburnDocument9 pagesDiagnosis and Management of Functional Heartburnal ghiffari muhammad rayhanNo ratings yet
- Laryngopharyngeal and Gastroesophageal Reflux: A Comprehensive Guide to Diagnosis, Treatment, and Diet-Based ApproachesFrom EverandLaryngopharyngeal and Gastroesophageal Reflux: A Comprehensive Guide to Diagnosis, Treatment, and Diet-Based ApproachesCraig H. ZalvanNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- MS Prelim Exam ReviewerDocument9 pagesMS Prelim Exam ReviewerSheril100% (2)
- Gastrointestinal Tract Disorders Upper Lower Organ: Stomatitis (Dietcd) Gastritis GerdDocument125 pagesGastrointestinal Tract Disorders Upper Lower Organ: Stomatitis (Dietcd) Gastritis GerdAnonymous rzPX6lUNo ratings yet
- Dyspepsia Hypertension 1Document32 pagesDyspepsia Hypertension 1Jeno Luis AcubNo ratings yet
- Is It Ethical to Brand This ConditionDocument4 pagesIs It Ethical to Brand This Conditionfabian dionNo ratings yet
- GERD and Hiatal Hernia GuideDocument4 pagesGERD and Hiatal Hernia GuideAmoroso, Marian Corneth D.No ratings yet
- Bmj-2021-069211.full Reduce Unnecessary Use of Proton Pump InhibitorsDocument7 pagesBmj-2021-069211.full Reduce Unnecessary Use of Proton Pump InhibitorsYo MeNo ratings yet
- DRUGSDocument5 pagesDRUGSDanica EspejoNo ratings yet
- 1 Week Gastritis Diet Plan (My Personal Experience)Document8 pages1 Week Gastritis Diet Plan (My Personal Experience)ps piasNo ratings yet
- 7 Low Acid FoodsDocument7 pages7 Low Acid FoodsIce BibovskiNo ratings yet
- Pediatrics 2010 Thakkar E925 30Document8 pagesPediatrics 2010 Thakkar E925 30ivanhariachandraNo ratings yet
- Barralvisceral Bi Study Guide SamplerDocument47 pagesBarralvisceral Bi Study Guide SamplerLuulaa Minguin Garcia100% (8)
- The Effect of Thickened-Feed Interventions On Gastroesophageal RefluxDocument13 pagesThe Effect of Thickened-Feed Interventions On Gastroesophageal Refluxminerva_stanciuNo ratings yet
- GIDocument47 pagesGIJuliaNo ratings yet
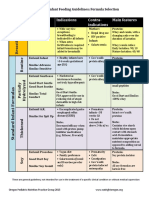
- Formula Selection OPNPGDocument2 pagesFormula Selection OPNPGRina PratiwiNo ratings yet
- Haad 3 Questions GiDocument16 pagesHaad 3 Questions GiPatpat De Guzman67% (3)
- HIATAL HERNIA PPT Final PDFDocument49 pagesHIATAL HERNIA PPT Final PDFregysujit60% (5)
- SMK 01Document12 pagesSMK 01FathiyaNo ratings yet
- Modified Inspiratory Muscle Training (m-IMT) As Promising Treatment For Gastro-Oesophageal Reflux Disease (GERD)Document5 pagesModified Inspiratory Muscle Training (m-IMT) As Promising Treatment For Gastro-Oesophageal Reflux Disease (GERD)B RGNo ratings yet
- Laryngomalaci 2016 Ajoshua Bedwell, MD, GeorgeZalzal, MDNDocument4 pagesLaryngomalaci 2016 Ajoshua Bedwell, MD, GeorgeZalzal, MDNwawa chenNo ratings yet
- Test Bank For Medical Physiology 3rd Edition Walter Boron Emile BoulpaepDocument3 pagesTest Bank For Medical Physiology 3rd Edition Walter Boron Emile BoulpaepMisti Keane100% (25)
- Drug Study (MS)Document9 pagesDrug Study (MS)Kristine GallardoNo ratings yet
- Letters Combined (11 Referral, 2 Discharge, 1 Transfer)Document49 pagesLetters Combined (11 Referral, 2 Discharge, 1 Transfer)Faisal ImtiazNo ratings yet
- Candida EsofagitisDocument5 pagesCandida EsofagitisVina IsmawatiNo ratings yet
- Videofluoroscopic Swallowing StudiesDocument25 pagesVideofluoroscopic Swallowing StudiesPriisciilla Vicencio100% (1)
- Gastroesophageal Reflux in Children and AdolescentsDocument20 pagesGastroesophageal Reflux in Children and AdolescentsruthmindosiahaanNo ratings yet
- MS Lec Gi and Icp Reviewer - Limon, Adine Jeminah DDocument8 pagesMS Lec Gi and Icp Reviewer - Limon, Adine Jeminah DShawn TejanoNo ratings yet
- Surgical Patient Body Composition Changes and Post-Operative RecoveryDocument52 pagesSurgical Patient Body Composition Changes and Post-Operative RecoveryDr-Shadi Meteir100% (1)
- Nursing Plan of Care - FinalDocument3 pagesNursing Plan of Care - Finalapi-642989736No ratings yet
- Peptic UlcerDocument6 pagesPeptic UlcerNader Smadi100% (1)
- Pediatric Feeding DisorderDocument74 pagesPediatric Feeding Disorderkklaudia.pszichoNo ratings yet