Professional Documents
Culture Documents
Case Study (OSD)
Uploaded by
Elza ZherebchukOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Study (OSD)
Uploaded by
Elza ZherebchukCopyright:
Available Formats
Running head: CASE STUDY
Case Study
Name:
Course:
Tutor:
Date:
Running head: CASE STUDY
2
1. Client map
Diagnosis: Obsessive Compulsive Disorder, 300.3 (F42)
Objectives of treatment: bring symptoms of disorder under control, so that they do not rule
patients daily life.
Clinicians characteristics viewed as Therapeutic:
Therapist's personal attributes like, for
example, being friendly and motivating are necessary. Moreover, he should be persistent to
that patient would deal with the object of obsession.
Location of Treatment: patients everyday circumstances and therapists office.
Interventions to be used: hypnosis, yoga, exposure and response prevention (ERP),
medications, cognitive behavioral therapy.
Emphasis of Treatment: emphasis on keeping a job and developing of interpersonal skills
Nature of treatment: individual and group sessions. Pharmaceutical treatment is also to be
provided.
Timing: 3 months once or a few times a week.
Medications needed: Serotonin Reuptake Inhibitor (SRI) or another antidepressants
Adjunct services: N/A
Prognosis: The treatment is going to be effective, but our patient has spent much time on this
obsession, that is why it can take a time. (Mayoclinic.org, 2016)
Diagnosis: Obsessive Compulsive Disorder, 300.3 (F42)
Provisional diagnosis: Social Anxiety disorder 300.23 (F40.10)
Rule out: Obsessive Compulsive Disorder, 300.3 (F42) is to be treated in different ways. Two of
them is psychotherapy and medications. The first step should be a doctor to try to determine
whether the patient is faking his symptoms, or because he has something to gain as to avoid
responsibility. The next step is to determine drug or substance related causes. And after all, it is
very important to understand the real nature of the disorder and to determine the precise
diagnosis of this syndrome.
2. Diagnosis
Diagnostic and Statistical Manual -5 defines obsessive-compulsive personal disorder (OCD)
(300.3 (F42)) by at least four of the following signs:
The person is concerned in lists, rules, procedures and organizational aspects, which
can even lead to loss of the main essence of the problem.
Running head: CASE STUDY
3
Detects perfectionism that interferes in the execution of a task
Excessively works, can even sacrifice vacation and friendly or family relations.
Not flexible and has strong views on issues of morality, ethics values.
Unable to get rid of unneeded items, even when they have significant value.
Reluctantly cooperates with others, because, in his opinion, they are doing things and
tasks wrong.
Detects excessive firmness and perseverance.
Compulsions are repetitive behaviors or mental acts that an individual feels driven to
perform in response to an obsession or according to rules that must be strongly applied. (DSM-V,
2013)
3. Provisional diagnosis
The extensive and abnormal work regime must lead to Social disorders, that are
misunderstanding of the requirements of the society.
In social anxiety disorder (social phobia) 300.23 (F40.10) , the individual is
anxious about or scared of or avoidant of social interactions and situations that involve
the possibility of being analyzed. This includes social interactions such as meeting
unknown people. There is a fear of being evaluated by others in a negative way, by being
humiliated, or ignored, or offending others. In panic disorder, the individual experiences
recurrent unexpected panic attacks. This is a provisional diagnosis. Nevertheless, our
patient is likely to develop this kind of disorders through his lifestyle and habits.
4. Rule out.
There are some certain steps in ruling out the right disorder to provide a necessary
medication and treatment.
Determine malingering and factitious disorder
Check drug-related causes
Determine any general medical conditions
Understand the precise primary disorder
Differentiate adjustment disorders from unspecified categories
Running head: CASE STUDY
4
Determine boundaries with no mental disorder ( Schimelpfening, N. 2016)
Our diagnosis is likely not to be drug-related. This disorder is very broad and of high
quantity all around the world.
5. Discussion
Our patient, John, during last years, became more and more aware that he spends much
time on his studying and working. When he graduated, he got a job in a big company, so that he
tried to do his best. Within weeks, firm had second thoughts on John, because he was doing his
commitments for a long period and with excessive persistence. He knew that it took for him too
long for his job, but he felt compelled to continue checking the lists. After the probation period,
the organization let him go.
This history is a perfect example of the Obsessive Compulsive Disorder. In this
case, there are different groups of disorders: some of them are with compulsions, some of
them are with obsessions. This disorder is likely to be genetic and inherited, but there are
several scientific studies, that prove, that OCD is to be changed in the circumstances of
society.
This disorder is guided by compulsions or obsessions. Our patient is likely to be
compulsive, because he spends much time doing the same work. Our mind is using
psychological defense mechanism get rid of accumulating tension, stress, that is why patients
are guided by the compulsions.
There are several ways to get rid of it. One of them is exposure and response
prevention (ERP), which is the therapy of confronting with your fears. Our patient should try,
Running head: CASE STUDY
5
by the help of the doctor, to avoid his compulsion and to make his consciousness understand,
that there is no use in these repeatable actions.
The next way is the use of medications, which can help to create new habits and
help to confront with the patients fears. These medications are most of all antidepressants or
the one of the hormone nature.
Conclusion
The obsessive-compulsive disorder is vast spread all around the world. This
disorder is more common among the men. Even if such a problem weighs years and decades,
it is possible to cope with. That is why there is no use in fears of failure of medications. The
first thing for patient is to believe in the strength of this procedure and in the strength of his
mind, because the best factor of treatment is our brain.
There are several ways to help our mind to meet the requirements of the
specialists. Some of them are hypnosis and yoga. Moreover, these skills are not only
important in treatment, but also in everyday life. It happens that regular meetings with the
therapist in a patient with OCD are stretched for several months, but it takes time fruitfully.
Negative comments and criticism may worsen OCD and calm, supportive
environment are likely to help improve treatment outcomes. It makes no sense to swear or
scold person with OCD to stop the execution of rituals. He can not do it, and the pressure will
make it worse. The best way to help cope with OCD loved to be with him kind and patient.
Praise each successful attempt to resist OCD, and focus on the positive things in life
Running head: CASE STUDY
6
Running head: CASE STUDY
7
References
Diagnostic And Statistical Manual Of Mental Disorders, Dsm - 5. (2013).
.Available at: http://psy-gradaran.narod.ru/lib/clinical/DSM5.pdf
Schimelpfening, N. (2016). What Is a Provisional Diagnosis Vs. a Differential
Diagnosis?. [online] About.com Health. Available at:
http://depression.about.com/od/majordepressivedisorder/fl/What-Is-a-ProvisionalDiagnosis-Vs-a-Differential-Diagnosis.htm [Accessed 28 Jan. 2016].
Mayoclinic.org, (2016). Obsessive-compulsive disorder (OCD) Treatments and
drugs - Mayo Clinic. [online] Available at: http://www.mayoclinic.org/diseasesconditions/ocd/basics/treatment/con-20027827 [Accessed 28 Jan. 2016].
You might also like
- Rakocevic-Medojevic, D. - Rani Stilovi Afektivne Vezanosti Kao Prediktori Kvaliteta Partnerskih Veza I Razvoda BrakaDocument11 pagesRakocevic-Medojevic, D. - Rani Stilovi Afektivne Vezanosti Kao Prediktori Kvaliteta Partnerskih Veza I Razvoda BrakaSvetlana RadovanovicNo ratings yet
- Cognition, Brain, and Consciousness: Introduction to Cognitive NeuroscienceFrom EverandCognition, Brain, and Consciousness: Introduction to Cognitive NeuroscienceRating: 4 out of 5 stars4/5 (4)
- Psychoanalytic Theories of PersonalityDocument29 pagesPsychoanalytic Theories of PersonalityAdriana Bogdanovska ToskicNo ratings yet
- Ljubav I TraumaDocument12 pagesLjubav I TraumaZoran IlicNo ratings yet
- Knjiga Rezimea EIP 2012Document197 pagesKnjiga Rezimea EIP 2012MilicaMilijicNo ratings yet
- Sadisticke Seksualne Serijske UbiceDocument14 pagesSadisticke Seksualne Serijske UbiceKatarina Felbab50% (2)
- Gestalt Therapy Approach To Depressive ExperiencesDocument7 pagesGestalt Therapy Approach To Depressive Experiencesv_azygosNo ratings yet
- Dramski Trougao ENGLnoviDocument7 pagesDramski Trougao ENGLnovinikola-avramov-8934No ratings yet
- Shizofrenija: Psihički Poremećaj Ili Stanje Uma?: Univerzitet U Sarajevu Filozofski Fakultet Odsjek Za PsihologijuDocument38 pagesShizofrenija: Psihički Poremećaj Ili Stanje Uma?: Univerzitet U Sarajevu Filozofski Fakultet Odsjek Za PsihologijuAyakkkNo ratings yet
- Gestalt Contact StylesDocument7 pagesGestalt Contact StylesNina S MoraNo ratings yet
- Drama DjetinjstvaDocument10 pagesDrama DjetinjstvaInes IdekNo ratings yet
- Zbornik - Iksi - 1 - 2 - 2006 - Strana 41Document220 pagesZbornik - Iksi - 1 - 2 - 2006 - Strana 41Jasmina HrvattNo ratings yet
- Psihijatrijski I Pravni Aspekti Prisilne Psihijatrijske HospitalizacijeDocument4 pagesPsihijatrijski I Pravni Aspekti Prisilne Psihijatrijske HospitalizacijeRade Grbić100% (1)
- Pathology of LoveDocument17 pagesPathology of Loveindocilidadreflexiva100% (1)
- OCD and Related Disorders 1Document67 pagesOCD and Related Disorders 1Catherine Faith100% (1)
- Provjera Metrijskih Karakteristika I Faktorska Analiza Skale Procjene Socijalne Podrške Ss-ADocument8 pagesProvjera Metrijskih Karakteristika I Faktorska Analiza Skale Procjene Socijalne Podrške Ss-AAnela HasanagicNo ratings yet
- Obsessive Compulsive DisorderDocument12 pagesObsessive Compulsive DisorderGERSON RYANTONo ratings yet
- Am I My GenesDocument10 pagesAm I My GenesLívia ReisNo ratings yet
- Roditeljska Percepcija O Vrijednosti Školovanja Kao Faktor Motivacije Za Školsko Postignuće Učenika"Document13 pagesRoditeljska Percepcija O Vrijednosti Školovanja Kao Faktor Motivacije Za Školsko Postignuće Učenika"Anonymous 1nsMHrNo ratings yet
- Srodna Dusa Vs Zivotni PartnerDocument2 pagesSrodna Dusa Vs Zivotni PartnerMarina KolesarNo ratings yet
- Schizophrenia DiagnosisDocument2 pagesSchizophrenia DiagnosisShervin AslaniNo ratings yet
- Abnormal Psychology Module 11 Schizophrenia Spectrum and Other Psychotic DisordersDocument23 pagesAbnormal Psychology Module 11 Schizophrenia Spectrum and Other Psychotic DisordersSumriddhi SrivastavaNo ratings yet
- Parkinsonova BolestDocument8 pagesParkinsonova BolestSami DayekhNo ratings yet
- Cicchetti 2002Document15 pagesCicchetti 2002Kiara JohanaNo ratings yet
- Fear of SuccessDocument11 pagesFear of SuccessabelardbonaventuraNo ratings yet
- Dijagnoza Kroz Ciklus Konatakta II GrupaDocument43 pagesDijagnoza Kroz Ciklus Konatakta II Grupabojana413No ratings yet
- Leahy2019 Article IntroductionEmotionalSchemasAnDocument4 pagesLeahy2019 Article IntroductionEmotionalSchemasAnsharahoNo ratings yet
- Mediating Role of Cognitive Emotion Regulation Strategies On The Relanshionship Between Attachment Styles and AlexithymiaDocument12 pagesMediating Role of Cognitive Emotion Regulation Strategies On The Relanshionship Between Attachment Styles and AlexithymiaGabriela AlinaNo ratings yet
- Wk. 3 - Brain N Endocrine SystemDocument47 pagesWk. 3 - Brain N Endocrine SystemShayyy JacksonNo ratings yet
- Dream Work Peter PhillpsonDocument4 pagesDream Work Peter Phillpsonfrancis qatoyireetiNo ratings yet
- KORIŠĆENJE TEHNIKE DIREKTNOG OBRAĆANJA - Emocionalni Metod - Google GroupsDocument4 pagesKORIŠĆENJE TEHNIKE DIREKTNOG OBRAĆANJA - Emocionalni Metod - Google Groupstigerlo75No ratings yet
- Popis LiteratureDocument3 pagesPopis LiteraturesuyijaaNo ratings yet
- Artmetodebi Tanamedrove Fsiqoterapiasa Da Treningsi: Rusudan MircxulavaDocument28 pagesArtmetodebi Tanamedrove Fsiqoterapiasa Da Treningsi: Rusudan Mircxulavaთამუ სურმანიძეNo ratings yet
- Biography BanduraDocument1 pageBiography BanduraEdrianne J.No ratings yet
- Affective Temperaments and SH in Adolescents - PortugalDocument8 pagesAffective Temperaments and SH in Adolescents - Portugalsoliveira_149796No ratings yet
- Fear Axiety and PhobiaDocument11 pagesFear Axiety and PhobiasimonzosiNo ratings yet
- Personality and Social Psychology ResearchDocument5 pagesPersonality and Social Psychology ResearchWalter Cerna QuevedoNo ratings yet
- Basic Neurobiological and Preclinical ResearchDocument6 pagesBasic Neurobiological and Preclinical ResearchOlivera VukovicNo ratings yet
- A Case Study of A Mental DisorderDocument7 pagesA Case Study of A Mental DisorderMaurine TuitoekNo ratings yet
- In On It: What Adoptive Parents Would Like You To Know About AdoptionDocument14 pagesIn On It: What Adoptive Parents Would Like You To Know About AdoptionemotooleNo ratings yet
- RTG Atlas Za Studente PDFDocument43 pagesRTG Atlas Za Studente PDFGabrijela PejkićNo ratings yet
- Perls Layers and Empty Chair Reconsideration Norman FriedmanDocument14 pagesPerls Layers and Empty Chair Reconsideration Norman FriedmanIvana0% (1)
- Monster Study (Edit)Document2 pagesMonster Study (Edit)faizal1978No ratings yet
- Oppositional Defiant DisorderDocument4 pagesOppositional Defiant Disordernigo100% (1)
- The Power Tactics of Jesus Christ and Other EssaysDocument169 pagesThe Power Tactics of Jesus Christ and Other EssaysMEG GrunwaldtNo ratings yet
- Biological Bases of BehaviorDocument87 pagesBiological Bases of BehaviorJirahNo ratings yet
- Transakcijska AnalizaDocument29 pagesTransakcijska AnalizaAkuna RaNo ratings yet
- Ciccarelli3e Full Study GuideDocument215 pagesCiccarelli3e Full Study GuideMikaela Victoria LopezNo ratings yet
- EnactmentDocument20 pagesEnactmentCamelia Dracsineanu GheorghiuNo ratings yet
- Paradoksalna Teorija Promene EngleskiDocument12 pagesParadoksalna Teorija Promene EngleskiIvanaNo ratings yet
- Obsessive Compulsive DisorderDocument26 pagesObsessive Compulsive DisorderMhaane Desepeda VillanuevaNo ratings yet
- Alexander Lowen Ljubav I OrgazamDocument78 pagesAlexander Lowen Ljubav I OrgazamJob KirNo ratings yet
- Emotions and Emotional IntelligenceDocument116 pagesEmotions and Emotional IntelligenceSreepati Das100% (1)
- Popis Upitnika U ZbirkamaDocument4 pagesPopis Upitnika U ZbirkamaErik Augustin MamićNo ratings yet
- Antidpresivi U Lecenju DepresijeDocument10 pagesAntidpresivi U Lecenju DepresijeStefan95No ratings yet
- Norman H. Hadley (Auth.) Elective Mutism - A Handbook For Educators, Counsellors and Health Care Professionals 1994Document268 pagesNorman H. Hadley (Auth.) Elective Mutism - A Handbook For Educators, Counsellors and Health Care Professionals 1994ancadianaNo ratings yet
- Borderline Personality DisorderDocument9 pagesBorderline Personality DisorderElton BaranaskasNo ratings yet
- Management and Social MediaDocument5 pagesManagement and Social MediaElza ZherebchukNo ratings yet
- How Politics Should Be ConductedDocument6 pagesHow Politics Should Be ConductedElza ZherebchukNo ratings yet
- Affordable Care ActDocument5 pagesAffordable Care ActElza ZherebchukNo ratings yet
- DepressionDocument8 pagesDepressionElza ZherebchukNo ratings yet
- Increase in Drug Use: Who Is To Blame?: Last Name: 1Document3 pagesIncrease in Drug Use: Who Is To Blame?: Last Name: 1Elza ZherebchukNo ratings yet
- Last Name: 1: Is A Two-State Solution To The Arab-Israeli Conflict Still Viable?Document10 pagesLast Name: 1: Is A Two-State Solution To The Arab-Israeli Conflict Still Viable?Elza ZherebchukNo ratings yet
- ERP Test BankDocument29 pagesERP Test BankAsma 12No ratings yet
- Simple Past Story 1Document7 pagesSimple Past Story 1Ummi Umarah50% (2)
- Spoken KashmiriDocument120 pagesSpoken KashmiriGourav AroraNo ratings yet
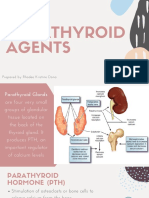
- Parathyroid Agents PDFDocument32 pagesParathyroid Agents PDFRhodee Kristine DoñaNo ratings yet
- A Social Movement, Based On Evidence, To Reduce Inequalities in Health Michael Marmot, Jessica Allen, Peter GoldblattDocument5 pagesA Social Movement, Based On Evidence, To Reduce Inequalities in Health Michael Marmot, Jessica Allen, Peter GoldblattAmory JimenezNo ratings yet
- Ipsoot Rating ClarificationsDocument9 pagesIpsoot Rating ClarificationsJerry PanNo ratings yet
- Reflection IntouchablesDocument2 pagesReflection IntouchablesVictoria ElazarNo ratings yet
- Audi A4 Quattro 3.0 Liter 6-Cyl. 5V Fuel Injection & IgnitionDocument259 pagesAudi A4 Quattro 3.0 Liter 6-Cyl. 5V Fuel Injection & IgnitionNPNo ratings yet
- 1820 Celestial EventDocument8 pages1820 Celestial EventDoor Of ElNo ratings yet
- BTS WORLD-Crafting GuideDocument4 pagesBTS WORLD-Crafting GuideAn ARMYNo ratings yet
- Project Procurement Management: 1 WWW - Cahyo.web - Id IT Project Management, Third Edition Chapter 12Document28 pagesProject Procurement Management: 1 WWW - Cahyo.web - Id IT Project Management, Third Edition Chapter 12cahyodNo ratings yet
- Glgq1g10 Sci Las Set 4 ColoredDocument4 pagesGlgq1g10 Sci Las Set 4 ColoredPogi AkoNo ratings yet
- S.I.M. InnovaDocument51 pagesS.I.M. InnovaPauline Karen ConcepcionNo ratings yet
- 3a Ela Day 3Document5 pages3a Ela Day 3api-373496210No ratings yet
- Walmart Assignment1Document13 pagesWalmart Assignment1kingkammyNo ratings yet
- Karaf-Usermanual-2 2 2Document147 pagesKaraf-Usermanual-2 2 2aaaeeeiiioooNo ratings yet
- Inheritance : Trung Tâm Anh NG Nhung PH M 27N7A KĐT Trung Hòa Nhân Chính - 0946 530 486 - 0964 177 322Document3 pagesInheritance : Trung Tâm Anh NG Nhung PH M 27N7A KĐT Trung Hòa Nhân Chính - 0946 530 486 - 0964 177 322Trung PhamNo ratings yet
- Government of Kerala: Minority CertificateDocument1 pageGovernment of Kerala: Minority CertificateBI185824125 Personal AccountingNo ratings yet
- Possessive Adjectives 3Document1 pagePossessive Adjectives 3RAMIRO GARCIA CANCELANo ratings yet
- SOCI 223 Traditional Ghanaian Social Institutions: Session 1 - Overview of The CourseDocument11 pagesSOCI 223 Traditional Ghanaian Social Institutions: Session 1 - Overview of The CourseMonicaNo ratings yet
- Commercial LawDocument61 pagesCommercial LawthebfilesNo ratings yet
- Dictums of Famous ArchitectsDocument3 pagesDictums of Famous ArchitectsErwin Ariola100% (2)
- Book - IMO Model Course 7.04 - IMO - 2012Document228 pagesBook - IMO Model Course 7.04 - IMO - 2012Singgih Satrio Wibowo100% (4)
- Soal Ujian Tengah Semester Genap Sma Islam Diponegoro Surakarta TAHUN PELAJARAN 2020/2021Document5 pagesSoal Ujian Tengah Semester Genap Sma Islam Diponegoro Surakarta TAHUN PELAJARAN 2020/2021Dian OctavianiNo ratings yet
- Self-Learning Home Task (SLHT) : Key Drawings and Animation BreakdownsDocument6 pagesSelf-Learning Home Task (SLHT) : Key Drawings and Animation BreakdownsRUFINO MEDICONo ratings yet
- Basic Statistics For Business AnalyticsDocument15 pagesBasic Statistics For Business AnalyticsNeil Churchill AniñonNo ratings yet
- House of Wisdom - Bayt Al Hikma (For Recording) - ArDocument83 pagesHouse of Wisdom - Bayt Al Hikma (For Recording) - ArMaeda KNo ratings yet
- Business Information Systems 2021: Cardiff Metropolitan UniversityDocument30 pagesBusiness Information Systems 2021: Cardiff Metropolitan UniversityMichelle FernandoNo ratings yet
- Test Bank For Davis Advantage For Medical-Surgical Nursing: Making Connections To Practice, 2nd Edition, Janice J. Hoffman Nancy J. SullivanDocument36 pagesTest Bank For Davis Advantage For Medical-Surgical Nursing: Making Connections To Practice, 2nd Edition, Janice J. Hoffman Nancy J. Sullivannombril.skelp15v4100% (15)
- Message To St. MatthewDocument3 pagesMessage To St. MatthewAlvin MotillaNo ratings yet