Professional Documents
Culture Documents
Respiratory Distress Syndrome
Uploaded by
Vicky NeshCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Respiratory Distress Syndrome
Uploaded by
Vicky NeshCopyright:
Available Formats
1
CHAPTER 1
INTRODUCTION
1.1 Background
1.1.1. Premature Baby
A premature baby is one who is born too early, before 37 weeks. Premature
babies may have more health problems and may need to stay in the hospital
longer than babies born later. They also may have long-term health problems that
can affect their whole lives. About 1 in 10 babies is born prematurely each year in
the United States.
The earlier in pregnancy a baby is born, the more likely he is to have health
problems. Some premature babies have to spend time in a hospitals neonatal
intensive care unit (also called NICU). This is the part of a hospital that takes care
of sick newborns. But thanks to advances in medical care, even babies born very
prematurely are more likely to survive today than ever before.
Premature babies can have some health problems after birth. Health problems
that may affect premature babies include apnea, respiratory distress
syndrome(RDS), Intraventricular hemorrhage (IVH), Patent ductus arteriosus
(PDA), Necrotizing enterocolitis (NEC) and many more. But the most common
breathing problem in babies born before 34 weeks of pregnancy is the respiratory
distress syndrome. Babies with RDS dont have a protein called surfactant that
keeps small air sacs in the lungs from collapsing.
Babies with RDS have some condition to go home from the hospital, like:
Weighs at least 4 pounds.
Can keep warm on his own, without the help of an incubator. An incubator is
an enclosed unit that helps premature babies stay warm.
Can breastfeed or bottle-feed
Gains weight steadily ( to 1 ounce each day)
Can breathe on his own.
1.1.2. Respiratory Distress Syndrome
Neonatal respiratory distress syndrome (RDS) is a condition of pulmonary
insufficiency that in its natural course commences at or shortly after birth and
increases in severity over the first 2 days of life. Clinically, RDS presents with
early respiratory distress comprising cyanosis, grunting, retractions and
tachypnea. Respiratory failure may develop, indicated by blood gas analysis, and
the diagnosis can be confirmed on chest X-ray with a classical ground glass
appearance and air bronchograms.If left untreated death may occur from
progressive hypoxia and respiratory failure.
In survivors resolution begins between 2 and 4 days. RDS is due to a
deficiency of alveolar surfactant along with structural immaturity of the lung and
it is mainly, but not exclusively, a disease of preterm babies. However, defining
RDS is difficult when prophylactic surfactant and very early continuous positive
airway pressure (CPAP) are used. The Vermont Oxford Neonatal Network
definition requires that babies have a PaO 2 <50 mm Hg (<6.6kPa) in room air,
central cyanosis in room air or need for supplemental oxygen to maintain PaO 2
>50 mm Hg(>6.6 kPa), as well as the classical chest X-ray appearances.
The pathophysiology of this disorder has been clearly elucidated. Briefly, the
structurally immature and surfactant-deficient lung has a tendency to collapse.
The presence of relatively well perfused but poorly ventilated areas of the lung
results in ventilation/perfusion mismatch, with hypoxemia and hypercarbia. In
some patients, pulmonary vasoconstriction leads to persistence of pulmonary
hypertension and right-to-left shunts (via the patent ductus arteriosus and/or the
foramen ovale), resulting in more severe hypoxemia. This phenomenon, once
thought to be patrimony of the full term infant, is frequently observed in preterm
babies with RDS and has led some clinicians to consider the use of inhaled nitric
oxide in preterm infants when hypoxemia is unresponsive to adequate support
with mechanical ventilation.
Fortunately, the natural course of the disease in many low-birth weight
infants has been altered by the introduction of exogenous surfactant. The
management of these infants is complex and requires a multidisciplinary team
approach to obtain best outcomes. The application of the basic principles of
neonatal care, such as thermoregulation, cardiovascular and nutritional support,
treatment of early neonatal infection, and prevention of nosocomial infection, is
crucial to achieve the therapeutic goals. Clearly, surfactant replacement therapy,
continuous positive airway pressure (CPAP), and mechanical ventilation in its
different modalities are the main stay for the respiratory support of these patients.
CHAPTER 2
LITERATURE REVIEW
2.1. Prematurity
2.1.1. Definition prematurity
Prematurity is a term for the broad category of neonates born at less than 37
weeks' gestation. Preterm birth is the leading cause of neonatal mortality and the
most common reason for antenatal hospitalization.For premature infants born
with a weight of less than 1000 g, the 3 primary causes of mortality are
respiratory failure, infection, and congenital malformation.
2.1.2 Sign and symptoms
Confirmation of gestational age is based on physical and neurologic
characteristics. The Ballard Scoring System remains the main tool clinicians use
after delivery to confirm gestational age by means of physical examination. The
major parts of the anatomy used in determining gestational age include the
following:
Ear cartilage (eg, a preterm infant at 28 weeks gestation has a small
amount of ear cartilage and/or a flattened pinna)
Sole (eg, a preterm infant at 33 weeks gestation has only an anterior
crease on the sole of the foot)
Breast tissue (eg, a preterm infant at 28 weeks gestation has no breast
tissue, and the areolae are barely visible)
Genitalia
At birth, the premature infant may show these signs:
Trouble breathing
Low weight
Inability to maintain a constant body temperature
Lanugo (body hair)
Low body fat
Less activity than normal
Underdeveloped muscles
Problems
feeding
due
to
underdeveloped
sucking/swallowing
coordination
Transparent skin
Yellow skin (jaundice)
2.1.3 Patophysiology
Infection and premature delivery
The action of micro-organisms results in the development of fetal and/or
maternal inflammatory response chorionamnioitis, funisitis
and
particularly Fetal Inflammatory Response Syndrome FIRS. These
symptoms are recognized as intraamnial inflammation. There is no exact
Czech equivalent to the term FIRS so far, the common term is fetal
inflammation with an analogous term for adults SIRS (Systemic
Inflammatory Response Syndrome). Fetuses with fetal inflammatory
response have higher perinatal morbidity, particularly due to severe stage
(III.
and
IV.)
leukomalacia,
intraventricular
necrous
haemorrhage
enterocolitis,
(IVH),
periventricular
bronchopulmonary
dysplasia,
myocardial dysfunction and neonatal sepsis with more frequent incidence of
premature delivery, compared with fetuses without inflammatory response.
The elevation of interleukin-6 in umbilical blood is post partum followed by
significantly higher incidence of funisitis (umbilical inflammation); the
inflammation is considered as a histological symptom of FIRS. At present,
the basic criteria include the elevation of cytokine levels (particularly
interleukin-6), elevated levels of immature forms of neutrophilic
granulocytes, elevated CRP in umbilical blood sampled after the delivery
and histological, (funisitis, chorionamnioitis) and clinical correlates
mentioned above. In an experiment, a diagnostic criterion is the elevation of
interleukin-6 in umbilical blood sampled during cordocentesis.
Uteroplacental ischaemia
The problem of the involvement of uteroplacental ischaemia in the
ethiopathogenesis of premature delivery represents a relatively newly
studied area. Again, the first work dealing with this problem was published
by Professor Romeros team. Concerning other studies, there is a rising
trend in the number of evidence of the relationship between thrombophilias
and premature delivery. In congenital (thrombophilic mutations) or acquired
(anti-phospholipid syndrome) thrombophilic conditions, we assume an
excessive coagulation activity with a potential effect on placental microcirculation; the related endothelial dysfunction initiates a cascade of
biochemical processes resulting in premature delivery. As mentioned above,
PRR activation is assumed. The detailed mechanism has not been described
yet. The most significant thrombophilias include Leiden Mutation, mutation
of coagulation factor II prothrombin, and anti-phospholipid syndrome.
These coagulation disorders play a role in other pathological conditions in
pregnancy, such as thromboembolism, intrauterine fetal death, intrauterine
growth restriction (IUGR), placental abruption, severe pre-eclampsia and
multiple spontaneous abortions (the role of thromboembolism to be found
in literature). MTHFR mutation has not been considered significant until
recently. Present works show that even this folic acid metabolism disorder
might be, probably in combination with other factors, related to premature
delivery. The metabolic transformation of folic acid results in the formation
of an active vitamin 4-THF-metafoline. One of the enzymes involved in
its metabolism is methyltetrahydrofolate reductase (MTHFR). MTHFR
gene polymorphism is connected with the reduction of their enzymatic
activity, particularly in homozygote constitution, resulting in reduced
formation of active folic acid metabolite, 4-THF. 4-THF represents a
catalyst of the remethylation of methionine into homocysteine. Its lack
(MTHFR mutation) causes insufficient homocysteine transformation,
followed by its accumulation in the body. The homocysteine elevation is
connected with endothelial impairment. Hyperhomocysteinaemia is a
significant risk factor for arteriosclerosis. In MTHFR mutation carriers, it is
assumed that the above mentioned mechanism might be related to placental
micro-circulation impairment and to all other consequences (abortion,
premature delivery, IUGR, sudden death syndrome). This area has now
been studied intensively; however, there is no bigger study so far. There is
evidence of the relationship between absolute (insufficient intake) or
relative (MTHFR) lack of folic acid and congenital fetal disorders. The
elevated concentration of toxic homocysteine in the body is considered as
one of the main causes of the development of congenital disorders of the
neural tube and heart
The role of gestagens
The uterus belongs to the organs formed by smooth muscles; its
physiology includes the same processes as those of other human organs of
the same structure. However, some biochemical processes running in this
organ have specific features. To understand the pathophysiological
processes, it is necessary to remind the basic features of its physiology. The
principle of its function is contraction, resulting from the interaction between
actin and myosin proteins of muscle cells myocytes. Particular myocytes
are connected with gap and tight junctions, involved in co-ordination and
synchronisation of the contractions in the whole uterus. The key process of
the interaction between actin and myosin is myosin phosphorylation
mediated by myosin kinase. The activation of myosin kinase requires the
complex calmodulin and calcium ions. Calcium ion homeostasis plays a key
role in the activity of myocytes. Intracellular calcium levels are regulated by
two mechanisms: cell membrane influx and release from depots in myocytes
(the sarcoplasmatic reticulum). Calcium ions enter the cells by at least two
pathways: currentdependent involving cell membrane depolarisation and
non-current-dependent involving the stimulation of the receptors with proper
agonists or by the blockage with antagonists. The membrane receptors are
formed by the action of ovarial and placental steroids. The action of
progesterone results in the formation of type 2 receptors = beta-adrenergic
receptors. The action of estradiol causes the formation of type 1 receptors =
alpha-adrenergic, muscarinergic, cholinergic, oxytocin and prostaglandin
ones. The calcium influx into the cells is stimulated by type 1 receptor
agonists. The contraction is followed by the return of calcium ions into
previous deposits against the concentration gradient by means of ATP-pump.
The return of calcium is stimulated by type 2 receptor agonists betamimetics and magnesium. In addition, an important process is the regulation
of myosin kinase by cAMP (cyclic adenosine monophosphate), which
inhibits its function. The cAMP levels are elevated by the stimulation of type
1 beta-adrenergic receptors, e.g. beta-mimetics. The transport of calcium
ions into the cytoplasm and thus the activation and relaxation of the
contractile system depends on the amount of the receptors and
concentrations of proper agonists and antagonists.
2.1.4.Diagnosis
Laboratory studies
Initial laboratory studies in cases of prematurity are performed to identify issues
that, if corrected, improve the patient's outcome. Such tests include the following:
Complete blood count (CBC): May reveal anemia or polycythemia that is
not clinically apparent
White blood cell (WBC) count: A high or low WBC count and numerous
immature neutrophil types may be found; an abnormal WBC count may
suggest subtle infection
Blood type and antibody testing (Coombs test): These studies are
performed to detect blood-group incompatibilities between the mother and
infant and to identify antibodies against fetal red blood cells (RBCs); such
incompatibilities increase the risk for jaundice and kernicterus
Serum electrolyte levels: Frequent determination of serum sodium,
potassium, and glucose concentrations, in conjunction with monitoring of
daily weight and urine output in extremely low birth weight (ELBW)
infants, assist the practitioner in determining fluid requirements
Imaging studies
Imaging studies are specific to the organ system affected. Chest radiography is
performed to assess lung parenchyma in newborns with respiratory distress.
Cranial ultrasonography is performed to detect occult intracranial hemorrhage in
ELBW newborns. Prematurity itself is not an indication for an imaging study.
Lumbar puncture
Lumbar puncture is performed in infants with positive blood cultures and in those
who have clinical signs of infection (presumed sepsis) and for whom a full course
of antibiotic coverage is planned.
2.1.5 Treatment
Management
Stabilization in the delivery room with prompt respiratory and thermal
management is crucial to the immediate and long-term outcome of premature
infants, particularly extremely premature infants.
Respiratory management
Recruitment and maintenance of adequate or optimal lung volume; in
infants with respiratory distress, this step may be accomplished with early
continuous positive airway pressure (CPAP) given nasally, by mask
(Neopuff), or by using an endotracheal tube when ventilation and/or
surfactant is administered
Avoidance of hyperoxia and hypoxia by immediately attaching a pulse
oximeter and, using an oxygen blender, keeping the oxygen saturation
(SaO2) between 86% and 93%
Prevention of barotrauma or volutrauma by using a ventilator that permits
measurement of the expired tidal volume and by keeping it at 4-7 mL/kg
Administration of surfactant early (< 2 hr of age) when indicated and
prophylactically in all extremely premature neonates (< 29 wk)
Thermoregulation
In the intensive care nursery, radiant warmers may be used to compensate for heat
loss in the premature infant. Incubators are more efficient than radiant warmers
10
because the heated environment decreases heat loss due to conduction,
convection, and radiation. In all nurseries, the environmental temperature should
be maintained at more than 70F (>21C).
Fluid and electrolyte management
Preterm infants need intense monitoring of their fluid and electrolytes because of
increased transdermal water loss and immature renal function in these infants, as
well as various environmental issues (eg, radiant warming, phototherapy,
mechanical ventilation). The degree of prematurity and the infant's specific
medication problems dictate initial fluid therapy. However, the following general
principles apply to all preterm infants:
Initial fluid should be a solution of glucose and water
Electrolytes should not be added until the infant is 24 hours of age, when
urine output is adequate
Infants who develop acute tubular necrosis (ATN) should be treated with
fluid restriction that equals insensible water loss plus urine output
Hyponatremia and weight gain should be treated with decreasing fluid
administration
The patient's weight should be followed up every 24 hours. Results of laboratory
monitoring and change in weight dictate changes in fluid and electrolyte support.
2.2 Respiratory Distress Syndrome
2.2.1 Definition RDS
Neonatal respiratory distress syndrome (RDS) is acondition of pulmonary
insufficiency that in its naturalcourse commences at or shortly after birth and
increasesin severity over the first 2 days of life. Clinically, RDS presents with
early respiratory distress
comprising
cyanosis,grunting,
retractions
and
tachypnea. Respiratoryfailure may develop, indicated by blood gas analysis,
andthe diagnosis can be confirmed on chest X-ray with aclassical ground glass
appearance and air bronchograms.If left untreated death may occur from
progressivehypoxia and respiratory failure. In survivors resolutionbegins between
2 and 4 days. RDS is due to a deficiencyof alveolar surfactant along with
11
structuralimmaturity of the lung and it is mainly, but not exclusively,a disease of
preterm babies. However, definingRDS is difficult when prophylactic surfactant
and veryearly continuous positive airway pressure (CPAP) areused.
2.2.2. Epidiemology RDS
About 12 percent of babies born in the United States are preterm, which is
higher thanin other developed countries. About 10 percent of premature babies in
theUnited
States
develop
RDS
each
year. The risk of RDS
rises
withincreasingprematurity. In 2003, the total number of live births in the United
States for all raceswas 4,089,950; about 0.6 percent of newborns had RDS (about
24,000 or 6 per1,000 live births). In 2005, there were 4,138,000 live births in the
UnitedStates, and a slightly larger number of babies were affected with RDS
becausethe rate of premature births had increased from 11.6 percent to 12.7
percent,mainly due to a rise in late preterm births (34 to 36 weeks of gestation).
Even though the number of RDS cases in the United States is growing,
theinfant mortality ratefrom RDS has dramatically declined from about 25,000
deathsper year in the 1960s to 860 deaths in 2005 because of surfactant
replacementtherapy. Infant deaths from RDS were 2.6 times greater in African
Americanbabies than in Caucasian babies, although Caucasian babies are at a
higherrisk to develop the condition. In Indonesia, out of 950.000 newborn with
low-weight, approximately 150.000 newborn suffers from RDS and most of the
case is hyalin membrane disease.
2.2.3. Pathogenesis
1. Transient tachypnea of the newborn
TTN is a parenchymal lung disorder characterized bypulmonary edema
thatresults from delayed resorption andclearance of fetal alveolar fluid in term
infants). Theexcess fluid in the lungs in TTN results in decreasedpulmonary
compliance and increased airway resistanceThe mechanism causing changes in
pulmonary function areprimarily associated with the extrinsic compression
ofsmall airways by fluid in the extra-alveolar interstitium.Tachypnea develops
12
tocompensate for the increased workof breathing associated with reduced
compliance and increasedairway resistance. (Avery ME, 2004)
2. Respiratory distress syndrome
RDS is also known as hyaline membrane disease; it is themajor cause of
neonatal respiratory distress, especially inpreterm infants. RDS is caused by a
deficiency of surfactant.Surfactant is a phospholipid mixture that is
responsiblefor stabilizing distal alveoli, at low end-expiratory lungvolumes, by
reducing surface tension). When surfactant isdeficient, the infant may not be able
to generate the increasedinspiratory pressure required to inflate alveolarunits,
resulting in the development of progressive atelectasis.Diffuse atelectasis results
in low compliance, highresistance in small airways, and low functional
residualcapacity. Hypoxemia results primarily from mismatching ofventilation
and perfusion as blood bypasses the atelectaticair spaces. Right-to-left shunting
then occurs through theductus arteriosus and foramen ovale because of
increasedpulmonary vascular resistance (PVR) and contributes to thedecreased
oxygenation.
3. Persistent pulmonary hypertension
PPHN is caused by persistently elevated PVR that leadsto right-to-left
shuntingthrough the foramen ovale and theductus arteriosus, resulting in
hypoxemia). PPHN occursprimarily in term or late preterm infants (34 weeks
gestation).The high pulmonary resistance is secondary to anumber of factors,
including: low arteriolar and alveolaroxygen levels; hypercarbia; acidosis;
alveolar fluid pressure;lack of mechanical, rhythmic distention of the lung;and
the net vasoconstricting action of a number of humoralagents. Catecholamines,
histamine,
bradykinin,
angiotensin,adenosine,
serotonin,
prostaglandins,
thromboxane, atrialnatriuretic peptide, endothelin, and nitric oxide (NO)
areinvolved in the regulation of pulmonary vascular tone in thefetus). Newborns
with PPHN are at risk of severe asphyxiaand its complications including death,
neurologic injuryand other problems. Studies over the past two decadeshave
clearly shown the critical role of NO-cGMP signalingin the regulation of the fetal
13
and neonatal pulmonary circulation,and that disruption of the NO-cGMP cascade
duringthe perinatal period leads to PPHN.
2.2.4. Pathofisiology
The primary cause of RDS is inadequate pulmonarysurfactant. The
structurally immature and surfactant-deficient lung has compliance anda
tendency to atelectasis; other factors in preterm infants that the risk of
atelectasis aredecreased alveolar radius and weak chest wall. With atelectasis,
well perfused but poorlyventilated areas of lung lead to V/Q mismatch (with
intra-pulmonary shunting) andalveolar hypoventilation with resultant hypoxemia
and hypercarbia. Severe hypoxemiaand systemic hypoperfusion result in
decreased O2 delivery, anaerobic metabolism and subsequent lactic acidosis.
Hypoxemia and acidosis may further impair oxygenatiob by causing pulmonary
vasoconstriction, resulting in right-to-left shunting at the levels of the foramen
ovale and ductus arteriosus. (Hermencan C,2007)
Other factors, such as baro/volutrauma and high FiO2, may initiate release of
inflammatory cytokines abd chemokines causing more endothelial and epithelial
cell injury. The injury results in reduced surfactant synthesis and function as well
as increased endothelial permeability leading to pulmonary edema. Leakage of
proteins into thealveolar space further exacerbatessurfactant deficiency by
causingsurfactant inactivation.Macroscopically, the lungs appearcongested,
atelectatic and solid.Microscopically, diffuse alveolaratelectasis and pulmonary
edema areseen. An eosinophilic membranecomposed of a fibrinous matrix
ofmaterials from the blood and cellulardebris (the hyaline membrane) lines the
visible airspaces that usually constitute dilatedterminal bronchioles and alveolar
ducts.
14
Diagram 1 Pathophysiology of RDS
2.2.5. Risk Factors
Prematurity
Male gender
Familial predisposition
Cesarean section without labor
Perinatal asphasia
Cancasian race
Infant of diabetic mother
Chorioamnonitis
Non-Immune hydrops fetalis
15
2.2.6. Clinical Manifestation
Signs of RDS appear immediately after birth or within 4 h.RDS is
characterized
by
tachypnea
(>60
breaths/min),
intercostal
and
subcostalretractions, nasal flaring, grunting, and cyanosis in room air. Tachypnea
is due to anattempt to increase minute ventilation to compensate for a decreased
tidal volume andincreased dead space. Retractions occur as the infant is forced to
generate a highintrathoracic pressure to expand the poorly compliant lungs.
Grunting resultsfrom thepartial closure of the glottis during forced expiration in
an effort to maintain FRC. Afteran initial improvement with resuscitation and
stabilization, an uncomplicated course isoften characterized by a progressive
worsening for 48 to 72 h. Recovery usuallycoincides with a diuresis after an
initial period of oliguria. Other clinical features mayinclude hypotension, acidosis
and hyperkalemia. The typical chest radiograph shows lowlung volumes and a
bilateral, reticular granular pattern (ground glass appearance) withsuperimposed
air bronchograms. In more severe cases, there is complete white out ofthe lung
fields. Application of positive airway pressure may minimize or even
eliminatethese radiographic findings. Acute complications include air leaks and
intracranialhemorrhage. Long-term, RDS has been associated with an increased
incidence of chroniclung disease, ROP, and neurologic impairment.
2.2.7. Diagnosis
RDS diagnosis can be enforced through clinical manisfestation and can be
confirmed with gas blood analysis. Clinical manisfestation that happen to
neonatal baby is:
Cyanosis
Apnea
Decreased urine output
Nasal flaring
Puffy or swollen arms and legs
Rapid breathing
Shallow breathing
16
Shortness of breath and grunting sounds while breathing
Increased oxygen requirement
Paradoxical chest wall movement with breathing
Breath sounds that include rales
Poor lung aeration
Accessory muscle usage
Chest x-ray showing atelectasis, air bronchograms, and granular
infiltrates
Blood gas analysis is a defenite indicator from exchange of gas to measure
acute respiratory failure. Eventhough the clinical manifestation need intubation
action and use of mechanical ventilation, the sampling of atrial blood is needed to
analys blood gas pressure ( PaO2, PaCO2 and pH) while monitoring with pulse
oxymetry. Heavy hypocxemia is marked with PaO2 < 50-60 mmHg with FiO2
60% or PaO2 <60 mmHg with FiO2 > 40% for babies < 1250 g, heavy
hipercapnea with PaCO2 > 55-60 mmHg with pH < 7,2 -7,25. Severity level of
respiratory distress can be evaluated through Silverman-Anderson score or
Downes score.
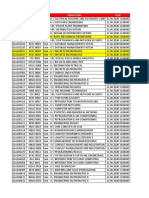
Table 1 : Downs Score
2.2.8 Management
The goals of management of an infant with RDS are to (Halliday, 2010)
17
Avoid hypoxemia and acidosis
Optimize fluid management which is avoid fluid overload and resultant
body and pulmonaryedema while averting hypovolemia and hypotension
Reduce metabolic demands and maximize nutrition
Minimize lung injury secondary due to volutrauma and oxygen toxicity
The three most important advances in prevention and treatment of RDS have
been:
a) antenatal glucocorticoids
b) continuous positive airway pressure (CPAP) and positiveendexpiratory pressure (PEEP)
c) surfactant replacement therapy. These havedramatically decreased
morbidity and mortality from RDS.
1. Antenatal glucocorticoids
Antenatal administration of corticosteroids that pass through the placenta to
the foetus (betamethasone 24 mg; or dexamethasone 24 mg; or 2 g.
hydrocortisone) has been shown to decrease the incidence of RDS. Best results
are obtained if more than 24 hours and less than 7 days have elapsed between
commencement of treatment and delivery.
2. Exogenous surfactant
It has been shown in multiple randomized controlled trials that the use of
exogenous surfactant in preterm infants improves oxygenation, decreases air
leaks, reduces mortality due to RDS, and decreases overall mortality.
A. Timing of surfactant administration:
Two approaches have been used for surfactant delivery which is prophylactic
and rescue treatment.
Prophylactic administration
Involves giving surfactant soon after birth, as soon as the infant has been
stabilized. The theoretical benefit of this approach is that replacement of
surfactant before RDS develops will avoid or ameliorate lung injury. Animal
studies have shown that the lung epithelium of very premature subjects can be
18
damaged within minutes of onset of ventilation. The damage can result in protein
leak which subsequently interferes with surfactant function.
Rescue administration
Involves giving surfactant to infants who have established RDS and require
mechanical ventilation and supplemental O2. The advantage of this approach is
that patients are not treated unnecessarily. Because surfactant currently can only
be given via an endotrachealtube, this would prevent intubation and mechanical
ventilation of infants who would do well without surfactant and avoid
unnecessary baro/volutrauma, adverse physiological effects of laryngoscopy, and
possible inadvertent hyperventilation. Past studies have shown greater reduction
in neonatal mortality with prophylactic administration versus rescue, especially in
infants greatest at risk for RDS (i.e., <27weeks GA). However, with the use of
nasal CPAP in VLBW infants and higher rates of antenatal steroid administration,
there exists controversy on the optimal timing of surfactant administration,
balancing the benefits of early surfactant administration with the advantages of
avoiding mechanical ventilation and volutrauma. The current approach to the
timing of surfactant therapy at UCSF is summarized in Table 1.
19
Table 2: Guidelines for intubation and timing of surfactant administration
inpreterm infants.
B. Administration and dose of surfactant
For prophylactic administration, the position of the endotracheal (ET) tube should
be verified by two people before surfactant is given. Attach the surfactant syringe
to the side port of the ET tube, occlude end of ET tube, and administer surfactant
as a single aliquot over 5 sec. For rescue therapy, obtain chest radiograph to
confirm tube position. Administer surfactant through a feeding tube inserted to
(but not past) the end of the ET tube. Administer in same manner as with
prophylactic treatment. Slower administration may interfere with its efficacy.
After administration, the infant should be hand ventilated and may transiently
require higher ventilatory support. Several studies have shown that two doses, 12
h apart, may be more effective than single dose therapy. More than 2 doses is
rarely required and is rarely effective. The dose of surfactant is:
Infasurf 3mL/kg
Survanta 4 mL/kg
C. Criteria for rescue treatment
Rescue treatment with surfactant should be given to preterm infants who have:
Respiratory distress, necessitating intubation and assisted ventilation,
No radiological evidence of another disease process, and require either
FIO2 > 0.3 or a mean airway pressure 7 cmH2O
D. Complications
Although surfactant administration is relatively safe, complications include
obstruction of the endotracheal tube, transient increases in O2 requirement and
20
ventilatory settings, and pulmonary hemorrhage, an infrequent adverse effect
reported in 2-6% of infants given surfactant.
3. Oxygen
Oxygen should be administered to preterm infants in concentrations sufficient
to maintain PaO2 between 50-70 mmHg or saturation (by pulse oximetry)
between 85-92%.Higher O2 concentrations may exacerbate lung injury and will
increase the risk of retinopathy of prematurity.
4. Respiratory Management
The initial decision in respiratory management of an infant with RDS is
whether the infant can be adequately managed with nasal CPAP (i.e., no treatment
with surfactant) or should receive endotracheal intubation, surfactant therapy and
mechanical ventilation. Endotraheal intubation should be performed in infants
that require prophylactic surfactant administration or who meet the criteria.
Table 3: Indications for intubation of preterm infant during resuscitation.
The goals of ventilatory management in the intubated infant are to maintain
adequate oxygenation and ventilation while minimizing ventilator induced lung
injury. To achieve these aims, utilize a strategy of permissive hypercarbia,
maintaining PaCO2 between 45-55 mmHg, theoretically reducing volutrauma
and preventing deleterious effects of hypocarbia. To reduce further the risk of
volutrauma, adjust ventilatory pressures to maintain tidal volume between 4-5
mL/kg. Administration of surfactant improves lung mechanics ( lung
compliance) and increases oxygenation by reducing atelectasis and increasing
21
FRC. It is extremely important to recognize the time frame of these changes.
After surfactant administration, there may be very rapid improvements in
pulmonary function that necessitate rapid weaning of ventilator settings.
Close attention must be paid to tidal volume, blood gas tensions,
transcutaneous CO2 and pulse oximetry values in order to avoid inadvertent
hyperventilation, hyperoxia and over distension of the lung, all of which can
result in lung injury. Although it may be necessary to wean FIO2, inspiratory
pressure and ventilator rate, one should decrease PEEP with extreme caution.
Infants in the early phases of RDS will rarely maintain adequate lung inflation if
PEEP is <5 cmH2O, even after administration of surfactant. Recently, much
effort has been directed towards other, less invasive modalities of respiratory
support to prevent lung injury, specifically nasal CPAP. CPAP, as treatment for
RDS, was first described in 1971 by George Gregory at UCSF. Modifications in
the nasal CPAP delivery system have generated renewed interest in nasal CPAP
for the ventilatory management of RDS. Randomized controlled trials have
shown a decreased need for mechanical ventilation in VLBW infants treated with
nasal CPAP, although the impact on mortality and chronic lung disease have not
been defined.
Furthermore, recent reports indicate that approximately 70% of infants with birth
weight <1,000 g will not be adequately managed with nasal CPAP and will
require intubation and mechanical ventilation. Nevertheless, in order to minimize
ventilator-induced lung injury, early extubation to nasal CPAP is a reasonable
strategy. Criteria for extubation to nasal CPAP in the first week of life are:
Adequate respiratory drive, and
Mean airway pressure 7 cmH2O, and
FIO2 0.35
Nasal CPAP is delivered via a specialized nasal mask or prongs, utilizing a
patient demand flow system. CPAP is administered between 4 and 6
cmH2O.Lower pressures do not maintain lung inflation and higher pressures
often cause gastric distension. Limitations to the use of nasal CPAP include
22
hypercarbia, frequent episodes of apnea, gastric distension and breakdown of
nasal skin and mucosa from the mask/prongs. The method and timing of further
weaning, from nasal CPAP to supplemental O2 via nasal cannula, varies with
gestational age, post-natal age, weight and stability of the individual patient.
Some infants require a gradual transition to nasal cannula through sprinting, a
process in which infants are trialed on nasal cannula for a portion of the day and
then returned to nasal CPAP. As the infant demonstrates increased tolerance of
these trials, the length of these trials is slowly extended. The time of these trials
often coincides with feeds, in order to minimize handling of VLBW infants (e.g.,
if feedings are q3 hours, trials of nasal cannula are usually increased in 3 hour
intervals).
3. Antibiotic therapy
The clinical and radiographic features of pneumonia may be indistinguishable
from RDS at birth. As a result, all infants with RDS should have blood cultures
and CBC drawn, and should receive empiric antibiotic therapy (Ampicillin and
Gentamicin). Generally, antibiotics may be discontinued if the blood culture has
no growth after 48 hours, unless prenatal history or clinical scenario warrants
extended treatment.
4. Thermoregulation
Careful temperature control is imperative in all VLBW infants and is especially
important in infants with RDS to minimize metabolic demands and oxygen
consumption. RDS can limit oxygen uptake leading to hypoxia which limits the
ability of an infant to increase their metabolic rate when cold stressed, resulting in
a falling body temperature. An incubator or radiant warmer must be utilized to
maintain a neutral thermal environment for the infant.
23
CHAPTER III
CASE REPORT
3.1 Objective
The objective of this paper is to report a case of a 1 hour old boy with a diagnosis
of premature birth and respiratory distress.
3.2 Case
Baby AD, a 1 hour old boy, with 1.33 kg of birth weight and 38 cm of body
height, was admitted in Perinatology Division on 20 th July at 6.30 AM with chief
complaint of premature birth.
24
3.3 History of disease:
Baby AD, a boy, 1 hour old, with 1.33 kg of BW and 38 cm of BH, was
admitted in Perinatology Division on 20th July at 6.30AM with premature birth as
chief complaint. SP was given birth an hour ago (5.30AM) at RSUP Haji Adam
Malik Medan. It was a normal premature delivery with the indication of severe
oligohydromnion,. Patient cried spontaneously after delivery, weak muscle tone
and less active movement.
History of medication
:-
History of family
:-
History of parents medication
:-
History of pregnancy
: The age of the patients mother was 25
during pregnancy. The gestational age was
28 weeks.
History of birth
: Birth was assisted by SpOG in RSUP HAM.
The patient was born paravaginal and cry
immediately after birth. Body weight at
birth was 1330 gram, body length at birth
was 38 cm and head circumference was 26
cm. Cyanosis (+), Jaundice (-). Patient was
placed in preheated infant warmer and
suctioned through mouth and nasal. Patient
was given oxygen litre per minute via
nasal canule. Patient was dried with cloth
and the baby cried louder, gained good
muscle tone, skin appears reddish and active
movement. Umbilical was wrapped with
strerile gauze.
History of feeding
Physical Examination:
: Breast feeding was given 7 days after birth.
25
Present status:
Sensorium : compos mentis
Body temperature: 36.0C
HR: 150 bpm
RR: 56 bpm
BW: 1.33 kg
BL: 38 cm
Chest circumference (CC): 24.5cm
Head circumference (HC) : 26cm
APGAR score: 6/9
anemic (-), icteric (+), dyspnea (+), cyanosis (+), edema (-).
Localized status:
Head
:
Head : frontal within normal limit
Face : edema (-), icteric (+)
Eye : light reflex (+/+), isochoric pupil, palpebral
conjunctiva pale (-/-), icteric (-)
Ears
: both ear lobes in normal morphologic, less
cartilage
Nose : septum deviation (-), nasal canule (+), NGT (-)
Mouth : normal
Neck
:
Lymph node enlargement (-), neck stiffness (-)
Thorax
:
Symmetrical fusiform, retraction (+) epigastrial,
icteric (-), areola barely visible, no breast tissue
HR: 150 bpm, regular, murmur (-/-)
RR: 56 bpm, regular, ronchi (-/-)
Abdomen :
Soepel, normal peristaltic, liver and spleen
unpalpable, icteric (-)
Extremities
:
adequate p/v, felt warm, CRT < 3, pitting oedema
(-/-), icteric (-)
Anogenital
: Male, within normal limits
26
Differential diagnosis : 1) Premature
2) Respiratory Distress ec DD/ - Neonatal Pneumonia
- Hyalin Membrane
Disease
3) Low Birth Weight (LBW)
4) Suspect of sepsis
Working diagnosis
: 1) Premature
2) Respiratory Distress ec DD/ - Neonatal Pneumonia
- Hyalin Membrane
Disease
3) Low Birth Weight (LBW)
4) Suspect of sepsis
Laboratory finding:
Complete blood analysis (July 20th 2016 / 0932WIB)
Test
Hemoglobin
Erythrocyte
Leucocyte
Thrombocyte
Hematocrite
Eosinophil
Basophil
Neutrophil
Lymphocyte
Monocyte
Neutrophil absolute
Lymphocyte absolute
Monocyte absolute
Eosinophil absolute
Basophil absolute
MCV
MCH
Result
17.2
4.73
23.3
391
50
0.30
0.70
72.80
13.70
12.50
16.97
3.19
2.92
0.07
0.16
106
36.4
Unit
g/dL
106/L
103/L
103/L
%
%
%
%
%
%
103/L
103/L
103/L
103/L
103/L
fL
Pg
References
17 22
4.50 6.50
10 30
150 450
31 59
13
0.00-1.00
50 70
20 40
28
5.5-18.3
2.8-9.3
0.5-1.7
0.02-0.70
0.1-0.2
80-97
26.5-33.5
27
MCHC
Procalcitonin
34.4
g/dL
31.5 -36
0.43
ng/ml
< 0.05
Therapy :
Recommended: Infant Radiant Warmer Therapy with target skin
temperature 36,5-37,5.
Total fluid requirement: 80cc/kgBW/day = 106.4cc/ day
o Parenteral 80cc/kgBW/day = 106.4cc/day
- IVFD D10% NaCl 0,225% (500cc) + D40% (50cc) + KCl
10 mEq + Ca Gluconas 10cc
-
4cc/ 5hour
GIR: 7,3
kg/kgBW/minute (D8%)
Aminosteril 6% 2gr/kgBW/day = 2,8 gr/day = 47cc/day =
1,9cc/hour/iv
o Enteral: Fasting (24 hours)
Ceftazidine injection 65mg/12 hour/iv (Day 1)
Gentamicin injection 6,5mg/36 hour/iv (Day 1)
28
FOLLOW UP
21st July 2016
S
Less active movement, cyanosis (-)
CNS: stable
Sensorium: CM Temp: 36.9C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 145 bpm, regular without murmur
Pulse: 145 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
Nasal CPAP with FiO2 21% PEEP 6,
Flow 8 litre per minute, regular without ronchi
Metabolic system: unstable
Blood glucose (20/7): 65mg/dL
Infectious : unstable
Fever (-) Temp: 36.9 C
Leucocyte (20/7) : 23 310 PCT: 0.43
Hematologic : unstable
Hb/Ht/T: 17.2/50/391 000
IT Ratio: 0.16 CRP: <0.7
Musculoskeletel: stable
1. Respiratory distress ec dd Hyaline membrane disease
Neonatal pneumonia
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
29
- infant radiant warmer with target temperature of 36.5 37.5 C
- Nasal CPAP with FiO2 21% PEEP 6, Flow 8 litre/ minute
- Total fluid requirement: 100cc/kgBW/day
Parenteral: 100cc/kgBW/day = 133cc/day
IVFD D10% + Ca Gluconas 10cc = 75.37 cc/day = 3cc/hour
Aminosteril 2gr/kgBW/day: 1.8cc/hour (calori: 10.64/day)
Ivelip 2gr/kgBW/day : 15.3cc/day = 0.5cc/hour (kalori: 23.54/day)
Enteral: 20cc/kgBW/day: 2cc/2hour/OGT (2120kal)
- Heparin 0.2cc/hour
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
22nd July 2016
S
Active movement, cry loud, fever (-) icteric (-)
CNS: stable
Sensorium: CM Temp: 37.2C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 140 bpm, regular without murmur
Pulse: 140 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
Nasal CPAP with FiO2 21% PEEP 6,
Flow 8 litre per minute, regular without ronchi
Metabolic system: unstable
Blood glucose (20/7): 65mg/dL
Infectious : unstable
Fever (-) Temp: 37.2 C
Leucocyte (20/7) : 23 310 PCT: 0.43
Hematologic : unstable
Hb/Ht/T: 17.2/50/391 000
IT Ratio: 0.16 CRP: <0.7
Musculoskeletel: stable
1. Respiratory distress ec dd Hyaline membrane disease
Neonatal pneumonia
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
30
- infant radiant warmer with target temperature of 36.5 37.5 C
- Nasal CPAP with FiO2 21% PEEP 6, Flow 8 litre/ minute
- Total fluid requirement: 100cc/kgBW/day
Parenteral: 80cc/kgBW/day = 133cc/day
IVFD D10% + Ca Gluconas 10cc = 20cc/day = 1cc/hour
Aminosteril 2gr/kgBW/day: 12.74cc/hour (calori: 16/day)
Ivelip 2gr/kgBW/day : 20cc/day = 0.8cc/hour (kalori: 23.54/day)
Enteral: 40cc/kgBW/day: 4cc/2hour/OGT
- Heparin 0.2cc/hour
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
23rd July 2016
S
Active movement, cry loud, fever (-) icteric (-)
CNS: stable
Sensorium: CM Temp: 37C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 144 bpm, regular without murmur
Pulse: 144 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
Nasal CPAP with FiO2 21% PEEP 6,
Flow 8 litre per minute, regular without ronchi
48 bpm
Metabolic system: unstable
Blood glucose (20/7): 65mg/dL
Infectious : unstable
Fever (-) Temp: 37C
Leucocyte (20/7) : 23 310 PCT: 0.43
Hematologic : unstable
Hb/Ht/T: 17.2/50/391 000
IT Ratio: 0.16 CRP: <0.7
Musculoskeletel: stable
1. Respiratory distress ec dd Hyaline membrane disease
Neonatal pneumonia
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
31
- infant radiant warmer with target temperature of 36.5 37.5 C
Parenteral: 80cc/kgBW/day = 133cc/day
IVFD D10% + Ca Gluconas 10cc = 20cc/day = 1cc/hour
Aminosteril 2gr/kgBW/day: 12.74cc/hour (calori: 16/day)
Ivelip 2gr/kgBW/day : 20cc/day = 0.8cc/hour (kalori: 23.54/day)
Enteral: 40cc/kgBW/day: 4cc/2hour/OGT
- Heparin 0.2cc/hour
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
24th July 2016
S
Active movement, cry loud, fever (-) icteric (-)
CNS: stable
Sensorium: CM Temp: 37C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 140 bpm, regular without murmur
Pulse: 140 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
Flow 8 litre per minute,
50 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (20/7): 65mg/dL
Infectious : unstable
Fever (-) Temp: 37C
Leucocyte (20/7) : 23 310 PCT: 0.43
Hematologic : unstable
Hb/Ht/T: 17.2/50/391 000
IT Ratio: 0.16 CRP: <0.7
Musculoskeletel: stable
1.
2.
3.
4.
Respiratory distress ec Hyaline membrane disease
Low Birth Weight
Premature neonate
Suspect sepsis
32
- infant incubator with target temperature of 36.5 37.5 C
- O2 low flow 0.3 litre/minute > oxygen saturation 98 100%
- Total fluid requirement: 120cc/kgBW/day
Parenteral: 80cc/kgBW/day = 133cc/day
IVFD D10% + Ca Gluconas 10cc = 20cc/day = 1cc/hour
Aminosteril 2gr/kgBW/day: 2.74cc/hour (calori: 16/day)
Ivelip 2gr/kgBW/day : 20cc/day = 0.8cc/hour (kalori: 23.54/day)
Enteral: 40cc/kgBW/day: 4cc/2hour/OGT
- Heparin 0.2cc/hour
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
R/ Low flow.
Light therapy 1 x 24hour (starts from 2000 till 2000 (25/7/2016)
25th July 2016
S
Active movement, cry loud, fever (-) icteric (+)
CNS: stable
Sensorium: CM Temp: 36.8C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 142 bpm, regular without murmur
Pulse: 142 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
45 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (20/7): 65mg/dL
Infectious : unstable
Fever (-) Temp: 36.8C
Leucocyte (20/7) : 23 310 PCT: 0.43
Hematologic : unstable
Hb/Ht/T: 17.2/50/391 000
IT Ratio: 0.16 CRP: <0.7
Musculoskeletel: stable
1. Respiratory distress ec Hyaline membrane disease
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
33
- infant incubator with target temperature of 36.5 37.5 C
- O2 low flow 0.3 litre/minute > oxygen saturation 98 100%
- Total fluid requirement: 150cc/kgBW/day
Parenteral: 70cc/kgBW/day = 93.1cc/day
IVFD D10% + Ca Gluconas 10cc +KCl = 1cc/hour
Aminosteril 3gr/kgBW/day: 3cc/hour (calori: 16/day)
Ivelip 2gr/kgBW/day : 20cc/day = 0.9cc/hour
Enteral: 80cc/kgBW/day: 8cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
26th July 2016
S
Active movement, cry loud, fever (-) icteric (-)
CNS: stable
Sensorium: CM Temp: 36.8C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 145 bpm, regular without murmur
Pulse: 145 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
45 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (20/7): 65mg/dL
Infectious : unstable
Fever (-) Temp: 36.8C
Leucocyte (20/7) : 23 310 PCT: 0.43
Hematologic : unstable
Hb/Ht/T: 17.2/50/391 000
IT Ratio: 0.16 CRP: <0.7
Musculoskeletel: stable
1. Respiratory distress ec Hyaline membrane disease
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
34
- infant incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 150cc/kgBW/day
Parenteral: 50cc/kgBW/day = 66.5cc/day
IVFD D10% + Ca Gluconas 10cc = 2cc/hour
Aminosteril 2gr/kgBW/day: 2.3cc/hour
Ivelip 2gr/kgBW/day : 20cc/day = 0.6cc/hour
Enteral: 100cc/kgBW/day: 11cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
27th July 2016
S
Active movement, cry loud, fever (-) icteric (-)
CNS: stable
Sensorium: CM Temp: 36.8C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 143 bpm, regular without murmur
Pulse: 143 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
45 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (20/7): 65mg/dL
Infectious : unstable
Fever (-) Temp: 36.8C
Leucocyte (20/7) : 23 310 PCT: 0.43
Hematologic : unstable
Hb/Ht/T: 17.2/50/391 000
IT Ratio: 0.16 CRP: <0.7
Musculoskeletel: stable
Lab result: Hb/Ht/L/Tr : 17.8/52/14.120/449.000
Bilirubin total: 14.2 Bilirubin direk: 0.6
SGOT/SGPT: 43/6
35
KGD sewaktu: 35mg/dL KGD stick: 59mg/dL
1. Respiratory distress ec Hyaline membrane disease
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
- infant incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 150cc/kgBW/day
Parenteral: 40cc/kgBW/day = 66.5cc/day
IVFD D10% NaCl 0.255% (43cc) + D10% (70cc) +Ca Gluconas 10cc = 2cc/hour
Aminosteril 2gr/kgBW/day: 1.37cc/hour
Ivelip 2gr/kgBW/day : 20cc/day = 0.41cc/hour
Enteral: 110cc/kgBW/day: 11cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
28th July 2016
S
Active movement, cry loud, fever (-) icteric (-)
36
CNS: stable
Sensorium: CM Temp: 36.8C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 143 bpm, regular without murmur
Pulse: 143 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
45 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (27/7): 35mg/dL
Infectious : unstable
Fever (-) Temp: 36.8C
Leucocyte (27/7) : 14120
Hematologic : unstable
Hb/Ht/T: 17.8/52/449 000
Total bilirubin/ direct bilirubin/ SGOT/SGPT : 14.2/0.6/43
Musculoskeletel: stable
1. Respiratory distress ec Hyaline membrane disease
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
- infant incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 150cc/kgBW/day
Parenteral: 40cc/kgBW/day = 66.5cc/day
IVFD D10% NaCl 0.255% (43cc) + D10% (70cc) +Ca Gluconas 10cc = 2cc/hour
Aminosteril 2gr/kgBW/day: 1.37cc/hour
Ivelip 2gr/kgBW/day : 20cc/day = 0.41cc/hour
Enteral: 110cc/kgBW/day: 11cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
- Nystatin drop 4x0.5cc
- Zamel drop 1x0.3cc
29th July 2016
S
Active movement, cry loud, fever (-) icteric (-)
37
CNS: stable
Sensorium: CM Temp: 36.8C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 140 bpm, regular without murmur
Pulse: 140 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
42 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (27/7): 35mg/dL
Infectious : unstable
Fever (-) Temp: 36.8C
Leucocyte (27/7) : 14120
Hematologic : unstable
Hb/Ht/T: 17.8/52/449 000
Total bilirubin/ direct bilirubin/ SGOT/SGPT : 14.2/0.6/43/6
Musculoskeletel: stable
1. Respiratory distress ec Hyaline membrane disease
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
- infant incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 150cc/kgBW/day
Parenteral: 20cc/kgBW/day = 66.5cc/day
IVFD D10% NaCl 0.255% (43cc) + D10% (70cc) +Ca Gluconas 10cc = 1cc/hour
Enteral: 130cc/kgBW/day: 14cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv
- Inj gentamicin 6.5mg/36hour/iv
- Nystatin drop 4x0.5cc
- Zamel drop 1x0.3cc
30th July 2016
38
Active movement, cry loud, fever (-) icteric (-)
CNS: stable
Sensorium: CM Temp: 36.8C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 146 bpm, regular without murmur
Pulse: 146 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
44 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (27/7): 35mg/dL
Infectious : unstable
Fever (-) Temp: 36.8C
Leucocyte (27/7) : 14120
Hematologic : unstable
Hb/Ht/T: 17.8/52/449 000
Total bilirubin/ direct bilirubin/ SGOT/SGPT : 14.2/0.6/43/6
Musculoskeletel: stable
1. Respiratory distress ec Hyaline membrane disease
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
- infant incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 150cc/kgBW/day
Parenteral: 20cc/kgBW/day = 66.5cc/day
IVFD D10% NaCl 0.255% (43cc) + D10% (70cc) +Ca Gluconas 10cc = 1cc/hour
Enteral: 130cc/kgBW/day: 14cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv (H11)
- Inj gentamicin 6.5mg/36hour/iv (H11)
- Nystatin drop 4x0.5cc
- Zamel drop 1x0.3cc
31st July 2016
39
Active movement, cry loud, fever (-) icteric (-)
CNS: stable
Sensorium: CM Temp: 36.8C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 140bpm, regular without murmur
Pulse: 140 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
40 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (27/7): 35mg/dL
Infectious : unstable
Fever (-) Temp: 36.8C
Leucocyte (27/7) : 14120
Hematologic : unstable
Hb/Ht/T: 17.8/52/449 000
Total bilirubin/ direct bilirubin/ SGOT/SGPT : 14.2/0.6/43/6
Musculoskeletel: stable
1. Respiratory distress ec Hyaline membrane disease
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
- infant incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 150cc/kgBW/day
Parenteral: 20cc/kgBW/day = 66.5cc/day
IVFD D10% NaCl 0.255% (43cc) + D10% (70cc) +Ca Gluconas 10cc = 1cc/hour
Enteral: 130cc/kgBW/day: 14cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv (H12)
- Inj gentamicin 6.5mg/36hour/iv (H12)
- Nystatin drop 4x0.5cc
- Zamel drop 1x0.3cc
1st August 2016
40
Active movement, cry loud, fever (-) icteric (-)
CNS: stable
Sensorium: CM Temp: 36.8C
Head: Frontal within normal limit
Eyes: Light reflex (+/+), isochoric pupil, diameter 2mm/2mm,
Pale conjunctiva palpebral inferior: (-)
CVS: stable
HR: 145bpm, regular without murmur
Pulse: 145 bpm, regular, p/v sufficient,
Warm acral, CRT <3
Respiratory system: unstable
46 bpm regular without ronchi
Metabolic system: unstable
Blood glucose (27/7): 35mg/dL
Infectious : unstable
Fever (-) Temp: 36.8C
Leucocyte (27/7) : 14120
Hematologic : unstable
Hb/Ht/T: 17.8/52/449 000
Total bilirubin/ direct bilirubin/ SGOT/SGPT : 14.2/0.6/43/6
Musculoskeletel: stable
1. Respiratory distress ec Hyaline membrane disease
2. Low Birth Weight
3. Premature neonate
4. Suspect sepsis
- infant incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 150cc/kgBW/day
Parenteral: threeway
Enteral: 150cc/kgBW/day: 16cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv (H13)
- Inj gentamicin 6.5mg/36hour/iv (H13)
- Nystatin drop 4x0.5cc
- Zamel drop 1x0.3cc
41
S
O
S
O
2ND 3rd AUGUST 2016
Shortness of breath (-) icteric (-) Active movement, cry loud, fever (-)
Sensorium: CM
Temp: 36.8C
Head: Frontal within normal limit
Eye: Light reflex (+/+), isochoric pupil, pale conjunctiva palpebral inferior (-/-)
E/N/T: within normal limit
Thorax: Symmetric fusiform, retraction (-)
HR: 144 bpm, regular murmur (-)
RR: 40 bpm, regular, ronchi (-)
Abdomen: supple, peristaltic (+), hepar and lien unpalpable
Extremity: pulse 144x/i, warm acral, CRT <3
Laboratorium test: (3rd august)
Hb/Ht/ L/T: 15.2/43/6790/381000
Ca ion: 1.3
Ur/Cr/Uric acid: 30/0.5/2.9
Ca/ Na/K/Phos/Cl/Mg: 3/137/9/7.8/103/1.89
Prolaktin: 100.45 CRP: 0.7
1. Respiratory distress ec Hyaline membrane disease
2. Suspect sepsis
3. Low birth weight
4. Premature neonate - Infant incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 150cc/kgBW/day
Parenteral: threeway
Enteral: 150cc/kgBW/day: 16cc/2hour/OGT
- Inj ceftridine 65mg/12hour/iv (H14 - 15)
- Inj gentamicin 6.5mg/36hour/iv (H14 - 15)
- Nystatin drop 4x0.5cc
- Zamel drop 1x0.3cc
4th 9th AUGUST 2016
Shortness of breath (-) icteric (-) Active movement, cry loud, fever (-)
Sensorium: CM
Temp: 36.8C
Head: Frontal within normal limit
Eye: Light reflex (+/+), isochoric pupil, pale conjunctiva palpebral inferior (-/-)
E/N/T: within normal limit
Thorax: Symmetric fusiform, retraction (-)
HR: 144 bpm, regular murmur (-)
RR: 40 bpm, regular, ronchi (-)
Abdomen: supple, peristaltic (+), hepar and lien unpalpable
Extremity: pulse 144x/i, warm acral, CRT <3
42
S
O
1. Respiratory distress ec Hyaline membrane disease
2. Suspect sepsis
3. Low birth weight
4. Premature neonate - Incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 170cc/kgBW/day
Parenteral: threeway
Enteral: 170cc/kgBW/day: 223cc/day
- Nystatin drop 4x0.5cc
- Zamel drop 1x0.3cc
- Inj Vit K 1mg/IM/once week
- Ferriz drop 1x0.33cc
10TH - 13th AUGUST 2016
Shortness of breath (-) icteric (-) Active movement, cry loud, fever (-)
Sensorium: CM
Temp: 36.8C
Head: Frontal within normal limit
Eye: Light reflex (+/+), isochoric pupil, pale conjunctiva palpebral inferior (-/-)
E/N/T: within normal limit
Thorax: Symmetric fusiform, retraction (-)
HR: 144 bpm, regular murmur (-)
RR: 40 bpm, regular, ronchi (-)
Abdomen: supple, peristaltic (+), hepar and lien unpalpable
Extremity: pulse 144x/i, warm acral, CRT <3
Laboratorium test: (10th august)
Hb/Ht/L/T: 13.1/37/8200/438000
1. Respiratory distress ec Hyaline membrane disease
2. Suspect sepsis
3. Low birth weight
4. Premature neonate - Incubator with target temperature of 36.5 37.5 C
- Total fluid requirement: 160cc/kgBW/day
Parenteral: threeway
Enteral: 160cc/kgBW/day: 240cc/day
- Nystatin drop 4x0.5cc
- Zamel drop 1x0.3cc
- Inj Vit K 1mg/IM/once week
- Ferriz drop 1x0.33cc
43
CHAPTER IV
DISCUSSION
Theory
Case
Definition
Prematurity is a term for the broad The gestational age was 28 weeks.
category of neonates born at less than
37 weeks' gestation. Preterm birth is
the leading cause of neonatal mortality
and the most common reason for
antenatal hospitalization. For premature
infants born with a weight of less than
1000 g, the 3 primary causes of
mortality
are
respiratory
failure,
infection, and congenital malformation
Clinical Manifestation
Patient AD had small amount of ear
Confirmation of gestational age is cartilage and no breast tissue was
based on physical and neurologic
found. The areola barely visible.
characteristics. The Ballard Scoring
System remains the main tool
clinicians use after delivery to confirm
gestational age by means of physical
examination. The major parts of the
anatomy
used
in
determining
gestational age include the following:
-Ear cartilage (eg, a preterm infant
at 28 weeks gestation has a small
amount of ear cartilage and/or a
flattened pinna)
-Sole (eg, a preterm infant at 33
weeks gestation has only an
anterior crease on the sole of the
foot)
-Breast tissue (eg, a preterm infant
at 28 weeks gestation has no breast
tissue, and the areolae are barely
visible)
44
-Genitalia
Diagnosis
Laboratory studies
Initial laboratory studies in cases of
prematurity are performed to identify
issues that, if corrected, improve the
patient's outcome. Such tests include
the following:
Complete blood count (CBC):
May reveal anemia or
polycythemia that is not
clinically apparent
White blood cell (WBC) count:
A high or low WBC count and
numerous immature neutrophil
types may be found; an
abnormal WBC count may
suggest subtle infection
Blood type and antibody testing
(Coombs test): These studies
are performed to detect bloodgroup incompatibilities between
the mother and infant and to
identify antibodies against fetal
red blood cells (RBCs); such
incompatibilities increase the
risk for jaundice and kernicterus
Numerous
found
neutrophil
types
45
Serum electrolyte levels:
Frequent determination of
serum sodium, potassium, and
glucose concentrations, in
conjunction with monitoring of
daily weight and urine output in
extremely low birth weight
(ELBW) infants, assist the
practitioner in determining fluid
requirements
Theory
Definition
Case
Baby AD is a preterm baby with
Neonatal respiratory distress syndrome gestational age 28 week.
(RDS) is a condition of pulmonary
insufficiency that in its natural course
commences at or shortly after birth and
increases in severity over the first 2
days of life. Clinically, RDS presents
with
early
comprising
respiratory
cyanosis,
distress
grunting,
retractions and tachypnea. RDS is due
to a deficiency of alveolar surfactant
along with structural immaturity of the
lung
and
it
is
mainly,
but
not
exclusively, a disease of preterm babies.
However, defining RDS is difficult
when prophylactic surfactant and very
early
continuous
positive
airway
pressure (CPAP) are used.
Clinical Manifestation
Signs of RDS appear immediately after
birth or within 4 hours RDS is
characterized
by
tachypnea
No history of milk feeding till 7
days after birth.
History of turning blue found after
(>60
birth and according to parents, blue
breaths/min), intercostal and subcostal
has been found in lips, fingers and
46
retractions, nasal flaring, grunting, and
cyanosis in room air. Tachypnea is due
toes.
Through
physical
examination
to an attempt to increase minute
found retraction in epigastrial and
ventilation
suprasternal.
to
compensate
for
decreased tidal volume and increased
dead space. Retractions occur as the
infant is forced to generate a high
intrathoracic pressure to expand the
poorly
compliant
lungs.
Grunting
resultsfrom thepartial closure of the
glottis during forced expiration in an
effort to maintain FRC. After an initial
improvement with resuscitation and
stabilization, an uncomplicated course
is often characterized by a progressive
worsening for 48 to 72 h. Recovery
usually coincides with a diuresis after
an initial period of oliguria. Other
clinical
features
hypotension,
hyperkalemia.
may
include
acidosis
and
The
typical
chest
radiograph shows low lung volumes
and a bilateral,
reticular
granular
pattern (ground glass appearance) with
super imposed air bronchograms. In
more severe cases, there is complete
white
out
of
the
lung
fields.
Application of positive airway pressure
may minimize or even eliminate these
radiographic
findings.
Acute
complications include air leaks and
47
intracranial hemorrhage. Long-term,
RDS has been associated with an
increased incidence of chronic lung
disease,
ROP,
and
neurologic
impairment.
Diagnosis
Clinical criteria:
Based on the theory, this patient also
- Cyanosis
fulfilled some of the clinical and
- Apnea
laboratory criteria to be diagnosed as
- Decreased urine output
respiratory distress:
- Nasal flaring
a) Cinical manifestation
- Puffy or swollen arms and legs
- Patient suffers from difficulity in
- Rapid breathing
breathing known as dyspnea.
- Shallow breathing
- Shortness of breath and grunting
sounds while breathing
- Increased oxygen requirement
- Paradoxical chest wall movement
with breathing
- Breath sounds that include rales
- Poor lung aeration
- Accessory muscle usage
- Chest x-ray showing atelectasis, air
bronchograms, and granular
infiltrates
Therapy
Therapy which is given for RDS is:
-Respiratory
management
Therapy that used in this case is:
- Nasal CPAP with PEEP: 6 cmH2O,
Flow 8 liter per minute, FiO2: 30%
through
CPAP
- Antibiotic therapy such as ampicilin
Target of oxygen saturation: 92-96%.
Gentamicin injection 6.5mg/36
hour/iv
48
and gentamicin.
- ceftazidine injection 65mg/12hours/iv
- Thermoregulation such as radiant - Infant Radiant Warmer Theraphy with
warmer.
target skin temperature 36,5-37,5.
SUMMARY
Baby AD, a boy, 1 hour old, with 1.33 kg of BW and 38 cm of BH, came to
RSUP Haji Adam Malik Medan on 20thJuly at 6:30 AM with premature birth as
a chief complaint. No history of milk feeding after birth. History of turning
blue found after birth and according to parents, blue has been found in lips,
fingers and toes. Theres no fever and history of fever also not found. Patient
found to have difficulty in breathing when admitted to Perinatology Division.
Patient was diagnosed with premature birth, Respiratory Distress ec dd/ Hyalin
Membrane Syndrome, neonatal pneumonia, low birth weight and suspect of
sepsis. Patient was treated with Infant Radiant Warmer Theraphy with target
skin temperature 36,5-37,5, total fluid requirement: 150 cc/kgBW/day = 210cc/
day, parenteral 150cc/kgBW/day = 210cc/day, IVFD D5% NaCl 0,225%
(500cc) + D40% (50cc) + KCl 10 mEq + Ca Gluconas 10cc: 4cc/hour ;GIR: 7.3
kg/kgBW/minute (D8%), Aminosteril 6% 2gr/kgBW/day = 2,8 gr/day =
47cc/day = 1,9cc/hour/iv, Enteral: Fasting for 24 hours, Ceftazidime injection
65mg/12 hour/iv, Gentamicin injection 6.5mg/36 hour/iv.
49
REFERENCE
1. Kasap B, Duman N, Ozer E, Tatli M, Kumral A, Ozkan H.Transient tachypnea
of the newborn: predictive factor for prolonged tachypnea. Pediatr Int
2008;501:81-4.
2. Avery ME, Gatewood OB, Brumley G. Transient tachypneaof newborn.
Possible delayed resorption of fluid at birth. AmJ Dis Child 2004;111:380-5.
3. The Reagent Of University of California, 2004
4. Halliday HL, Ehrenkranz RA, Doyle LW:Early (<8 days) postnatal
corticosteroids forpreventing chronic lung disease in preterminfants. Cochrane
Database Syst Rev2010:CD001146.
5. Hermansen C, Lorah K. Respiratory distress in the newborn. Am Fam
Physician.2007;76:987-94.
6. Eichenwald E. Mechanical ventilation. Dalam: Cloherty J, Eichenwald E, Stark
A,penyunting. Manual of neonatal care. Edisi 6. Philadelphia: Lippincott
Williams &Wilkins; 2008. h. 331-42.
7. Rennie JM, Bokhari SA. Recent advances in neonatology. Arch. Dis. Child.
Fetal Neonatal ed. 1999;81:F1-F4
8. March
of
Dimes
Web
site.
Premature
birth.
Available
at:
http://www.marchofdimes.com/21209_11560.asp. Accessed January 21, 2010.
9. Respiratory distress syndrome of the newborn factsheet. American Lung
Association,
2006.
AccessedMay
7,
http://www.lungusa.org/site/pp.asp?c=dvLUK9O0E&b=35693.
2007,
at:
50
10. American College of Obstetricians and Gynecologists. Practice bulletin no.
159: management of preterm labor. Obstet Gynecol. 2016 Jan. 127 (1):e29-38.
11. Ruolin Z, Tao B, Li S, et al. Effect of dexamethasone on intelligence and
hearing in preterm infants: a meta-analysis. Neural Regen Res. 2014. 9(6):63745.
12. Ballard JL, Khoury JC, Wedig K, et al. New Ballard Score, expanded to
include extremely premature infants. J Pediatr. 1991 Sep. 119(3):417-23.
13. Barton L, Hodgman JE, Pavlova Z. Causes of death in the extremely low birth
weight infant. Pediatrics. 1999 Feb. 103(2):446-51.
14. Creasy RK, Gummer BA, Liggins GC. System for predicting spontaneous
preterm birth. Obstet Gynecol. 1980 Jun. 55(6):692-5.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Proposal Form NagDocument1 pageProposal Form Nagnitheesh kumarNo ratings yet
- Chapter 4: Palm Oil and Oleochemical Industries.: Presented By: Lovelyna Eva Nur Aniqah Siti MaryamDocument15 pagesChapter 4: Palm Oil and Oleochemical Industries.: Presented By: Lovelyna Eva Nur Aniqah Siti MaryamdaabgchiNo ratings yet
- Staff Code Subject Code Subject Data FromDocument36 pagesStaff Code Subject Code Subject Data FromPooja PathakNo ratings yet
- Infineon IRFZ44N DataSheet v01 - 01 ENDocument9 pagesInfineon IRFZ44N DataSheet v01 - 01 ENIkram RidhoNo ratings yet
- Department of Mechanical EnginneringDocument11 pagesDepartment of Mechanical EnginneringViraj SukaleNo ratings yet
- MHT-CET 2021 Question Paper: 25 September 2021Document3 pagesMHT-CET 2021 Question Paper: 25 September 2021Sank DamNo ratings yet
- Recipes G.garvin Copy1 Scribd 5Document7 pagesRecipes G.garvin Copy1 Scribd 5Peggy Bracken StagnoNo ratings yet
- Circle Theorems, Class 10Document7 pagesCircle Theorems, Class 10Susan MathewNo ratings yet
- 9 Daftar Pustaka VaricelaDocument2 pages9 Daftar Pustaka VaricelaAfrina FaziraNo ratings yet
- (Studies in American Popular History and Culture) Gail Fowler Mohanty - Labor and Laborers of The Loom - Mechanization and Handloom Weavers, 1780-1840 - Routledge (2006)Document292 pages(Studies in American Popular History and Culture) Gail Fowler Mohanty - Labor and Laborers of The Loom - Mechanization and Handloom Weavers, 1780-1840 - Routledge (2006)Милош Станојловић100% (1)
- Quarter 4 - Week 1Document44 pagesQuarter 4 - Week 1Sol Taha MinoNo ratings yet
- Samuelson and Nordhaus ch22 PDFDocument30 pagesSamuelson and Nordhaus ch22 PDFVictor ManatadNo ratings yet
- Notes StressDocument4 pagesNotes StressRohitKalraNo ratings yet
- HYW-17 T5 S5: Industrial Range MobileDocument6 pagesHYW-17 T5 S5: Industrial Range MobileghostshotNo ratings yet
- How To Build A GreenhouseDocument67 pagesHow To Build A GreenhouseBolarinwaNo ratings yet
- One - Touch Fittings: Series: WP2Document12 pagesOne - Touch Fittings: Series: WP2PrashantNo ratings yet
- CST STUDIO SUITE - High Frequency Simulation PDFDocument128 pagesCST STUDIO SUITE - High Frequency Simulation PDFGenik Podunay100% (2)
- 5 Kingdoms of OrganismsDocument13 pages5 Kingdoms of OrganismsChoirul Anam100% (2)
- Academic Program Required Recommended Academic Program Required RecommendedDocument1 pageAcademic Program Required Recommended Academic Program Required Recommendedonur scribdNo ratings yet
- Steam Purity Considerations For New TurbinesDocument46 pagesSteam Purity Considerations For New Turbinesomertrik100% (1)
- An Infallible JusticeDocument7 pagesAn Infallible JusticeMani Gopal DasNo ratings yet
- ECE 374 - Part - 1c - S2017Document37 pagesECE 374 - Part - 1c - S2017Zakaria ElwalilyNo ratings yet
- 01programming SZGH CNC990TDb (V2.4)Document120 pages01programming SZGH CNC990TDb (V2.4)Rodrigo DiverNo ratings yet
- T60n02rg PDFDocument8 pagesT60n02rg PDFsandor9116100% (2)
- Ligamentele LargiDocument2 pagesLigamentele LargiIoana IonicaNo ratings yet
- Construction Companies in AlbaniaDocument17 pagesConstruction Companies in AlbaniaPacific HRNo ratings yet
- Environmental and Sustainability Issues - 1Document21 pagesEnvironmental and Sustainability Issues - 121. PLT PAGALILAUAN, EDITHA MNo ratings yet
- Textbook of Surgery For Dental Students-smile4DrDocument400 pagesTextbook of Surgery For Dental Students-smile4DrRotariu Ana Maria100% (8)
- VIP45Document92 pagesVIP45Román IsraelNo ratings yet
- Samsung Bd-p4600 SMDocument101 pagesSamsung Bd-p4600 SMIonel CociasNo ratings yet