Professional Documents
Culture Documents
Trichinella Spiralis
Uploaded by
JayricDepalobosOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Trichinella Spiralis
Uploaded by
JayricDepalobosCopyright:
Available Formats
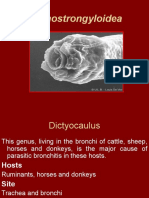
APHASMID NEMATODES
Dr. Ayochok
*Phasmids =receptors located at anterior portion of
parasite
when encysted, digestive tract has the same level of
maturity with that of the adult
causes much of the pathology of Trichinosis
Subclass Adenophora (Aphasmid Nematodes)
reduced/absent caudal papillae (also fxn as
receptor)
no lateral excretory canal
esophageal area: cylindrical with esophageal
gland forming stichosome (composed of
stichocytes)
egg: unsegmented (FERTILIZED but
unembryonated/immature) with plug at either
pole
Order Trichinata
I. Trichinella spiralis
II. Trichuris trichuria
III. Capillaria philippinensis
! Note: in all the three, male adult worms are smaller with
coiled posterior ends.
Life Cycle
I. Trichinella spiralis
common name: Trichina worm
disease caused: Trichinosis or Trichiniasis
Morphology
1. Adult worms
anterior end: w/ protrusible stylet inside the
papillated mouth (papilae- important for
sensing stimuli)
anterior portion: filled with stichosomes
which are composed of stichocytes (linearly
arranged strand-like cells)
esophagus: begins anterior to stichosome
intestine: posterior to esophagus, simple
tube that leads to the anus/cloaca
cloaca: serves as an opening to both
digestive and reporductive systems of the
worm
1.
2.
3.
4.
5.
a. Male Worms
delicate anterior end with cephalic papillae
posterior portion: 2 caudal/copulatory appendages
reproductive tract: single testes with its own tube that
will run anteriorly and go down posteriorly to open in the
cloaca
cloaca: evertible during copulation
b. Female Worms
Simple reproductive system: single ovary which starts
posteriorly then goes anteriorly to join with other
reproductive structures
Vulva: located at the anterior 5th of the body
Viviparous
1 adult female capable of producing 500 larvae in a
month
2. Larva
equipped with spear-like burrowing tip which is seen at
the anterior end
Trichinellosis is acquired by ingesting meat
containing cysts (encysted larvae) of Trichinella.
(infective stage)
After exposure to gastric acid and pepsin, the
larvae are released from the cysts and
invade/burrow into the intestinal mucosa
In the small bowel mucose, they develop into
adult worms (female 2.2 mm in length, males 1.2
mm; life span in the small bowel: 4 weeks)
After 1 week, the females release larvae that
migrate trhough the lymphatics, then the
bloodstream to finally reach the skeletal muscles.
! Skeletal muscle biopsy: deltoids, biceps,
pectorals since they are more accessible
Encystation in the muscles. Encystment is
completed in 4 to 5 weeks and the encysted
larvae may remain viable for several years.
Hence, man can serve as a dead-end host.
! Encapsulation takes place on the 3rd week from
the onset of infection
! Capsule is induced and not secreted, meaning,
the capsule is not produced by the larva but
comes from the skeletal muscle of the host.
! Capsule is penetrable
! Nurse cell- larva complex = Trichinella larva +
host skeletal muscle; calcifies in time
! includes other cycles for maintenance of
survival
o
Pig-to-pig
o
Rat-to-rat
o
Sylvatic cycle- maintained by wild
rodents
Epidemiology
Cosmopolitan distribution
Rare; absent in Australia
main reservoir: pig
Pathology and Symptomatology
3 Clinical Manifestations
1. Intestinal phase
From time of pork ingestion to GI
symptoms
Inflammation of duodenal and jejunal
mucosa
Non-specific symptoms: abdominal pain,
nausea, body malaise
Lasts up to 3 days
2. Muscle invasion phase
Muscle fibers: increase in size,
edematous, basophilic degeneration
Nuclei increase in size and number
Fever (remittent, up to 40C)
Periorbital edema, Generalized facial
edema
Tender lymphadenopathy
CBC: eosinophilia (prominent feature)
50 to 60% but can go as high as 90%
Myocarditis: most common grave
manifestation
Elevated cardiac markers
Takes place up to the 3rd week
3. Convalescence Phase
Larval encapsulation
Fever subsides
Muscular symptoms decrease
Diuresis, appetite returns
Diagnosis
History of poorly cooked or raw meat ingestion
CPK, LDH
CBC: Eoosinophilia (progressively increasing as
disease progresses until Convalescence phase
Bachman intradermal test: if result is (+),
supplement with any serologic test
Inject diluted solution with antigen of parasite
(+): white swelling surrounded by a wheal which
is not raised (5cm)
Serologic test: Bentonite flocculation (standard
test in some countries)
Muscle biopsy: definitive diagnosis; look for
free/encapsulated larva
Treatment
Mebendazole
Thiabendazole
Steroids: for allergic reaction and myocarditis
Prognosis
Generally good, except with Myocarditis
Absent/ low grade eosinophilia makes the
prognosis WORSE
Prevention
Freezing of pork
Avoid feeding raw garbage to hogs
Proper cooking of pork
Extermination of rats in farms
Notetaker: Stephanie Abnasan
You might also like
- Roundworms: Characteristics, Types & DiseasesDocument257 pagesRoundworms: Characteristics, Types & Diseasessummer dj100% (1)
- Tissue and Blood Parasites LectureDocument53 pagesTissue and Blood Parasites LectureVincent ManganaanNo ratings yet
- Phylum NematodaDocument285 pagesPhylum NematodaBrielleNo ratings yet
- CestodesDocument34 pagesCestodesمصطفي خندقاويNo ratings yet
- TrematodesDocument10 pagesTrematodesUhjafwnuijhnfa Kmerkgoe100% (1)
- Intestinal NematodesDocument88 pagesIntestinal NematodesVincent Manganaan100% (1)
- Para-Transes Prelim Exam - Unit 2Document20 pagesPara-Transes Prelim Exam - Unit 2Aysha AishaNo ratings yet
- Granulosus and E. Multilocularis (Hydatid) .: Tenia Solium or T. Saginata (Teniasis)Document7 pagesGranulosus and E. Multilocularis (Hydatid) .: Tenia Solium or T. Saginata (Teniasis)moosNo ratings yet
- Lecture on Parasitic Nematodes and AcanthocephalaDocument3 pagesLecture on Parasitic Nematodes and AcanthocephalaNa KhanNo ratings yet
- Trichinella and TrichurisDocument36 pagesTrichinella and TrichurisCristine BarrozaNo ratings yet
- N M To Es: Dr. Wafaa Ezz ElarabDocument31 pagesN M To Es: Dr. Wafaa Ezz Elarabshoroq zaki100% (1)
- Trichinella Spiralis Parasite: Symptoms, Life Cycle & TreatmentDocument15 pagesTrichinella Spiralis Parasite: Symptoms, Life Cycle & TreatmentBenjamin DanielNo ratings yet
- Taenia solium(1)Document7 pagesTaenia solium(1)n41995639No ratings yet
- Veterinary ParasitologyDocument157 pagesVeterinary ParasitologyPwaveno Bamaiyi75% (4)
- ParaDocument73 pagesParaeasysleezeNo ratings yet
- Trematodes General CharacteristicsDocument17 pagesTrematodes General CharacteristicsFreyja PaddamNo ratings yet
- Cestode SDocument79 pagesCestode SVincent Manganaan67% (3)
- Platheminthes. CestoideaDocument11 pagesPlatheminthes. CestoideaAdnan SosiNo ratings yet
- Platyhelminthes (Trematodes and Cestodes)Document6 pagesPlatyhelminthes (Trematodes and Cestodes)Julianna Rheaven JoreNo ratings yet
- Outline: 1. General Characteristics of Platyhelminthes 2. Classification of Platyhelminthes 3. Cestodes 4. TrematodesDocument73 pagesOutline: 1. General Characteristics of Platyhelminthes 2. Classification of Platyhelminthes 3. Cestodes 4. TrematodesAsxe CeeNo ratings yet
- TrematodesDocument9 pagesTrematodesJoseph PerezNo ratings yet
- TRICHINELLADocument27 pagesTRICHINELLARajkishor YadavNo ratings yet
- THE HELMINTHS: KEY PARASITIC WORMSDocument9 pagesTHE HELMINTHS: KEY PARASITIC WORMSMomo ShinNo ratings yet
- CESTODESDocument10 pagesCESTODEScole_danielleNo ratings yet
- Intestinal Parasitism: ProtozoansDocument10 pagesIntestinal Parasitism: ProtozoansdtimtimanNo ratings yet
- Amphistomate & Distomate FlukeDocument12 pagesAmphistomate & Distomate FlukeJayricDepalobosNo ratings yet
- Prof. DR Fahim ShaltoutDocument55 pagesProf. DR Fahim ShaltoutSumit SharmaNo ratings yet
- Parasitic Flatworms and Tapeworms Classification and CharacteristicsDocument54 pagesParasitic Flatworms and Tapeworms Classification and CharacteristicsMewa MahartaNo ratings yet
- Schistosomiasis: A Chronic Wasting DiseaseDocument5 pagesSchistosomiasis: A Chronic Wasting DiseaseJane GarciaNo ratings yet
- Lecture 3 para Summer 2023-1Document47 pagesLecture 3 para Summer 2023-1محمود سليمانNo ratings yet
- Exercise 7 ParasitDocument6 pagesExercise 7 ParasitIvanNo ratings yet
- Capillaria PhilippinenensisDocument4 pagesCapillaria PhilippinenensisnadalabelNo ratings yet
- Parasitology PresentationDocument28 pagesParasitology PresentationSamuel WilliamsNo ratings yet
- INTESTINAL NEMATODES Hand Out 10 - 11Document6 pagesINTESTINAL NEMATODES Hand Out 10 - 11microperadeniyaNo ratings yet
- Other AphasmidsDocument4 pagesOther AphasmidsJayricDepalobosNo ratings yet
- Beef Tapeworm Infection GuideDocument39 pagesBeef Tapeworm Infection GuideMicah MatibagNo ratings yet
- (MICROBIO) Liver Fluke NewDocument100 pages(MICROBIO) Liver Fluke NewMadhu MithaNo ratings yet
- Schistosomiasis & FascioliosisDocument40 pagesSchistosomiasis & FascioliosisWahyudi YusmanNo ratings yet
- Phylum Platyhelminthes (Flatworms) : Important InformationDocument26 pagesPhylum Platyhelminthes (Flatworms) : Important InformationYoussef EmadNo ratings yet
- Ascaris LumbricoidesDocument15 pagesAscaris LumbricoidesJyoti DasNo ratings yet
- RingwormsDocument5 pagesRingwormsCitrusNo ratings yet
- Assignment 1613490437 SmsDocument15 pagesAssignment 1613490437 Smsruksharbgp66No ratings yet
- Selma CestodesDocument23 pagesSelma CestodesAhmed EisaNo ratings yet
- 3) TrematodesDocument38 pages3) Trematodesmisgshlove1No ratings yet
- Parasitology Lecture 11 - AphasmidsDocument4 pagesParasitology Lecture 11 - Aphasmidsmiguel cuevasNo ratings yet
- General Properties of CestodesDocument42 pagesGeneral Properties of CestodesNicole NipasNo ratings yet
- 1st Lecture - Cestodes - Clinical ParasitologyDocument29 pages1st Lecture - Cestodes - Clinical ParasitologyAhmed MoghazyNo ratings yet
- Subkingdom Metazoa 2Document28 pagesSubkingdom Metazoa 2Ahmed OrabyNo ratings yet
- Larva Migrants and Trichinella SpiralisDocument8 pagesLarva Migrants and Trichinella Spiraliskenhamman wangilaNo ratings yet
- AscarisDocument42 pagesAscarisمصطفي خندقاوي100% (1)
- Template para Lab Exe 4 The TREMATODES 1 PDFDocument11 pagesTemplate para Lab Exe 4 The TREMATODES 1 PDFCharlie Magne GarciaNo ratings yet
- AscariasisDocument44 pagesAscariasisMuhammad AuliaNo ratings yet
- Chap5 UpdatedDocument32 pagesChap5 UpdatedROZZANE LOVELY RODNEY MoeNo ratings yet
- CoccidiosisDocument88 pagesCoccidiosisVenkatapradeepNo ratings yet
- Revision: Types of Life Cycle in Trematoda and CestodaDocument71 pagesRevision: Types of Life Cycle in Trematoda and CestodaMicroscopeGeekNo ratings yet
- TrichostrongyloideaDocument30 pagesTrichostrongyloideahisto anatomyNo ratings yet
- Proceedings of the First International Congress of Parasitology: Roma, 21-26 September 1964From EverandProceedings of the First International Congress of Parasitology: Roma, 21-26 September 1964Augusto CorradettiNo ratings yet
- Camp's Zoology by the Numbers: A comprehensive study guide in outline form for advanced biology courses, including AP, IB, DE, and college courses.From EverandCamp's Zoology by the Numbers: A comprehensive study guide in outline form for advanced biology courses, including AP, IB, DE, and college courses.No ratings yet
- Computer ModuleDocument8 pagesComputer ModuleJayricDepalobosNo ratings yet
- The LightDocument2 pagesThe LightJayricDepalobosNo ratings yet
- Music Order for Northern Luzon Adventist CollegeDocument1 pageMusic Order for Northern Luzon Adventist CollegeJayricDepalobosNo ratings yet
- Medical Ward 1 Service 2 CensusDocument13 pagesMedical Ward 1 Service 2 CensusJayricDepalobosNo ratings yet
- Medical Ward 1 Service 2 CensusDocument13 pagesMedical Ward 1 Service 2 CensusJayricDepalobosNo ratings yet
- Shipping Confirmation 1264941Document1 pageShipping Confirmation 1264941JayricDepalobosNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- WWW SlidDocument1 pageWWW SlidJayricDepalobosNo ratings yet
- FWD: Schedule Change AdvisoryDocument2 pagesFWD: Schedule Change AdvisoryJayricDepalobosNo ratings yet
- FWD: Schedule Change AdvisoryDocument2 pagesFWD: Schedule Change AdvisoryJayricDepalobosNo ratings yet
- The Church Must Stand TogetherDocument7 pagesThe Church Must Stand TogetherJayricDepalobosNo ratings yet
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- Acquaintance Party ParticipantsDocument1 pageAcquaintance Party ParticipantsJayricDepalobosNo ratings yet
- Sample Child Dedication ProgramDocument1 pageSample Child Dedication ProgramJayricDepalobos100% (2)
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 pagesConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNo ratings yet
- Peer Evaluation For Group 5Document1 pagePeer Evaluation For Group 5JayricDepalobosNo ratings yet
- Chapter 01 ChoicesDocument9 pagesChapter 01 ChoicesJayricDepalobosNo ratings yet
- "Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."Document3 pages"Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."JayricDepalobosNo ratings yet
- Census TemplateDocument3 pagesCensus TemplateJayricDepalobosNo ratings yet
- YHH Strategic Plan 2016-2017Document5 pagesYHH Strategic Plan 2016-2017JayricDepalobosNo ratings yet
- CAA Concert ProgramDocument2 pagesCAA Concert ProgramJayricDepalobosNo ratings yet
- What's in A Birthday?: I. We Can Be Mixed Blessings To OthersDocument2 pagesWhat's in A Birthday?: I. We Can Be Mixed Blessings To OthersJayricDepalobosNo ratings yet
- Psalm 23 SermonDocument5 pagesPsalm 23 SermonJayricDepalobosNo ratings yet
- Understanding Thalassemia: Causes, Symptoms and TreatmentDocument19 pagesUnderstanding Thalassemia: Causes, Symptoms and TreatmentJayricDepalobosNo ratings yet
- General Anesthesia in Caesarean SectionDocument7 pagesGeneral Anesthesia in Caesarean SectionJayricDepalobosNo ratings yet
- Tally Sheeth Per 10 HouseholdsDocument14 pagesTally Sheeth Per 10 HouseholdsJayricDepalobosNo ratings yet
- Clinical Pastoral OrientationDocument3 pagesClinical Pastoral OrientationJayricDepalobos100% (1)
- Pneumonia Antibiotics PDFDocument1 pagePneumonia Antibiotics PDFRudy KurniawanNo ratings yet
- Teen Parenting Brochure AssignmentDocument1 pageTeen Parenting Brochure AssignmentJayricDepalobosNo ratings yet
- Tally Sheeth Per 10 HouseholdsDocument14 pagesTally Sheeth Per 10 HouseholdsJayricDepalobosNo ratings yet
- Alien RPG Custom Character Sheet Mono FF-1Document1 pageAlien RPG Custom Character Sheet Mono FF-1Alexey PopkovNo ratings yet
- REKAP TITIK TEST PILE Borepile Dan Daya Dukung RencanaDocument4 pagesREKAP TITIK TEST PILE Borepile Dan Daya Dukung RencanaHendra RaitNo ratings yet
- CPH Bicycle-Account-2016Document24 pagesCPH Bicycle-Account-2016Alexandra NeculaNo ratings yet
- Ultimate Mortal Kombat 3: FinishersDocument29 pagesUltimate Mortal Kombat 3: FinishersFinil SonNo ratings yet
- Flex UK - February 2018Document132 pagesFlex UK - February 2018安建平 澳门南湖区100% (1)
- Big Ballin MB PDFDocument19 pagesBig Ballin MB PDFTony AvilaNo ratings yet
- Awop ReadmeDocument15 pagesAwop ReadmesilenceindigoNo ratings yet
- GRUNDFOS INSTRUCTIONS MULTIlift M/MD AND MOGDocument7 pagesGRUNDFOS INSTRUCTIONS MULTIlift M/MD AND MOGParveez HusnooNo ratings yet
- Health - Related Physical Fitness ComponentsDocument9 pagesHealth - Related Physical Fitness Componentsyaoi yuriNo ratings yet
- Absent Candidates of Aptitude TestDocument518 pagesAbsent Candidates of Aptitude TestManmohan SinghNo ratings yet
- Santos Concejero 2015Document7 pagesSantos Concejero 2015kan6de6jayNo ratings yet
- Icha MainanDocument118 pagesIcha Mainanrasah trial11No ratings yet
- Tabulasi Data SMD Pilar 2023 KUALARAWADocument7 pagesTabulasi Data SMD Pilar 2023 KUALARAWALisa LisaNo ratings yet
- Cricket Scorecard 1Document3 pagesCricket Scorecard 1Dery YanwarNo ratings yet
- Pipe Friction Loss Charts Guide Flow Rates & VelocitiesDocument1 pagePipe Friction Loss Charts Guide Flow Rates & Velocities45saulNo ratings yet
- AFC Club Ranking 2011-2014: Top 100 Clubs by PointsDocument2 pagesAFC Club Ranking 2011-2014: Top 100 Clubs by PointsSuraedi TambakNo ratings yet
- Modal Verbs: Los Verbos Modales YsuDocument28 pagesModal Verbs: Los Verbos Modales YsuNiltze DianaNo ratings yet
- Results Book Track & FieldDocument370 pagesResults Book Track & FieldDaniel Reinoso RojoNo ratings yet
- RC Truggy V2: By: 3dimensionsDocument21 pagesRC Truggy V2: By: 3dimensionsAlisson Barreto de AbreuNo ratings yet
- Sabang National High School Physical Education Summative AssessmentDocument2 pagesSabang National High School Physical Education Summative AssessmentCherrina AguilaNo ratings yet
- Popcap Games Keys and SerialsDocument5 pagesPopcap Games Keys and SerialsTerrance Thien45% (11)
- Installation Instructions: Trail Jack-54" (PART # 2722)Document3 pagesInstallation Instructions: Trail Jack-54" (PART # 2722)popescucvNo ratings yet
- How To Play TennisDocument8 pagesHow To Play TennisAbel BayartNo ratings yet
- Basic Sock TutorialDocument7 pagesBasic Sock TutorialTawafuq FmNo ratings yet
- Module Six Wellness PlanDocument12 pagesModule Six Wellness PlanConnor GayNo ratings yet
- 2017 Second Quarter CurriculumDocument10 pages2017 Second Quarter CurriculumRobert Allen RippeyNo ratings yet
- Gymnastics Lesson PlanDocument10 pagesGymnastics Lesson Planapi-486232490No ratings yet
- Eevee Traits and EvolutionsDocument4 pagesEevee Traits and EvolutionsErica FieldNo ratings yet
- The Seeker v4 Nº1 (October 2002)Document4 pagesThe Seeker v4 Nº1 (October 2002)rumtariNo ratings yet
- Kirloskar Pump 4R1040 Maintenance SheetDocument95 pagesKirloskar Pump 4R1040 Maintenance SheetArun ShyamrajNo ratings yet