Professional Documents
Culture Documents
Glycemic 2010 PDF
Uploaded by
Siva SankarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Glycemic 2010 PDF
Uploaded by
Siva SankarCopyright:
Available Formats
Schultz et al.
Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
REVIEW
Clinical review: Strict or loose glycemic control in
critically ill patients - implementing best available
evidence from randomized controlled trials
Marcus J Schultz1,2*, Robin E Harmsen1,2 and Peter E Spronk1,3
Abstract
Glycemic control aiming at normoglycemia, frequently
referred to as strict glycemic control (SGC), decreased
mortality and morbidity of adult critically ill patients in
two randomized controlled trials (RCTs). Five successive
RCTs, however, failed to show benefit of SGC with one
trial even reporting an unexpected higher mortality.
Consequently, enthusiasm for the implementation
of SGC has declined, hampering translation of SGC
into daily ICU practice. In this manuscript we attempt
to explain the variances in outcomes of the RCTs of
SGC, and point out other limitations of the current
literature on glycemic control in ICU patients. There
are several alternative explanations for why the five
negative RCTs showed no beneficial effects of SGC,
apart from the possibility that SGC may indeed
not benefit ICU patients. These include, but are not
restricted to, variability in the performance of SGC,
differences among trial designs, changes in standard
of care, differences in timing (that is, initiation) of SGC,
and the convergence between the intervention groups
and control groups with respect to achieved blood
glucose levels in the successive RCTs. Additional factors
that may hamper translation of SGC into daily ICU
practice include the feared risk of severe hypoglycemia,
additional labor associated with SGC, and uncertainties
about who the primarily responsible caregiver should
be for the implementation of SGC.
Background
Strict glycemic control (SGC) decreased mortality and
morbidity of ICU patients in two randomized controlled
*Correspondence: m.j.schultz@amc.uva.nl
1
Department of Intensive Care, Academic Medical Center, University of
Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, the Netherlands
Full list of author information is available at the end of the article
2010 BioMed Central Ltd
2010 BioMed Central Ltd
trials (RCTs) [1,2]. Five successive RCTs, however, failed
to show benet of SGC [3-7], with one trial even
suggesting SGC to cause harm since it was associated
with an unexpected higher late mortality rate [6].
After the publication of the rst RCT on SGC [1], the
ICU community seemed divided on the best method of
glycemic control. On the one hand, study results were
criticized: that is, it was suggested that the original study
results lacked generalizability, at least in part because of
the fact that it was a single-center study, and because
patients frequently received parenteral calories, which
was not common practice. On the other hand, several
professional associations adopted the strategy by proposing guidelines, and it was stated that hyperglycemia
should no longer be tolerated [8]. As a consequence,
many ICUs implemented some form of glycemic control,
although frequently the applied regimens tolerated
higher blood glucose levels than those used in the SGC
strategy as studied in the original trial [1]. After publication of the second RCT on SGC, which showed less
strong though still signicant benets of SGC [2], the
community continued to propagate glycemic control
with insulin [9]. Since the publication of ve successive
negative RCTs [3-7], however, enthusiasm for implementation of SGC has declined, hampering the translation of
SGC into daily ICU practice.
Apart from the inuence of the negative RCTs, several
other factors may hinder implementation of SGC. Fear of
severe hypoglycemia hindered, at least in part, broad
implementation of SGC [10]. Also, SGC mandates frequent blood glucose measurements, which may be considered labor intensive. In addition, although SGC in the
two positive RCTs was solely applied by ICU nurses [1,2],
it is often suggested that these caregivers lack sucient
background knowledge to safely apply SGC (in particular
when aiming at the lower normal limits of blood glucose
levels) [11].
There are several alternative explanations for why the
ve negative RCTs of SGC showed no benecial eects.
In addition, risks of severe hypoglycemia should be
rationalized. And also one may wonder whether SGC is
Schultz et al. Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
really that labor intensive [12]. In this manuscript we
attempt to explain the variances in outcomes of the RCTs
of SGC and discuss the limitations of the current
literature.
Glucose metabolism in the critically ill
Critical illness-induced hyperglycemia was long believed
a benecial, adaptive response to provide those organs
that predominantly rely on glucose as metabolic substrate
(brain and blood cells) with additional energy. However,
critical illness-induced hyperglycemia is also associated
with adverse outcome [13-16]. Hyperglycemia has been
suggested to be acutely toxic in critically ill patients
because of accentuated cellular glucose overload and
pronounced toxic side eects of glycolysis and oxidative
phosphorylation [17]. During severe illness, the expression of glucose transporters on the membranes of several
cell types is upregulated, which during reperfusion after
ischemia may allow high circulating glucose levels to
overload and damage these cells. Besides cellular glucose
overload, vulnerability to glucose toxicity may be due to
increased generation of and/or decient scavenging
systems for reactive oxygen species produced by activated
glycolysis and oxidative phosphorylation.
In the context of threatened organ function due to
critical illness, hyperglycemia-induced cellular injury
could reect a preventable risk. Establishing a causal
relationship between hyperglycemia and adverse
outcomes, however, requires RCTs to assess the impact
of preventing and/or treating hyperglycemia in critically
ill patients.
Glycemic control aiming at normoglycemia
Randomized controlled trials on strict glycemic control
Table 1 presents a summary of the RCTs reported to date
on SGC. The rst single-center RCT from Leuven
showed SGC to signicantly decrease mortality in
surgical ICU patients (4.6% in the intervention group
versus 8.0% in the control group) [1]. SGC also reduced
the incidence of bloodstream infections, acute renal
failure requiring dialysis or hemoltration, red-cell
transfusions and critical illness polyneuropathy. In
addition, SGC was associated with a shorter time of
ventilatory support. The second single-center RCT from
Leuven showed SGC to reduce morbidity, but not
mortality in medical ICU patients [2]. Of note, the power
analysis for this trial was based on the number of patients
requiring 3 days of stay in the ICU. Since the trial
recruited only 767 patients who stayed 3 days in the
ICU, and not 1,200 patients as calculated in the power
analysis, this trial was not powered to detect a dierence
in mortality in the intention to treat population. However,
while no impact on in-hospital mortality was found in
the intention to treat analysis (37.3% in the intervention
Page 2 of 9
group versus 40.0% in the control group), a per protocol
analysis of patients who stayed in the ICU 3 days did
show a dierence in mortality (43.0% in the intervention
group versus 52.5% in the control group).
A Saudi Arabian single-center RCT revealed no
signicant dierence in ICU mortality (13.5% in the
intervention group versus 17.1% in the control group) [3].
Also, after adjustment for baseline characteristics, SGC
was not associated with a mortality dierence. In a
Colombian single-center RCT, 28-day mortality rate was
not aected by SGC (36.6% in the intervention group
versus 32.4% in the control group) [4]. Also, ICU
mortality was not dierent between study groups in this
trial. A German multi-center RCT, in which patients with
severe sepsis were randomly assigned to receive either
SGC or conventional therapy and either 10% pentastarch,
a low molecular weight hydroxyethyl starch, or modied
Ringers lactate for uid resuscitation, was stopped
prematurely for safety reasons (increased incidence of
severe hypoglycemia with SGC, higher rates of acute
renal failure and need for renal-replacement therapy with
pentastarch) [5]. At 28 and 90 days, there was neither a
dierence in mortality (24.7% and 39.7% in the inter vention group versus 26.0% and 35.4% in the control group),
nor a dierence in the mean score for organ failure
between the study groups. In a RCT from Australia/New
Zealand and Canada, unexpectedly, 90-day mortality was
even higher with SGC (27.5% in the intervention group
versus 24.9% in the control group) [6]. There were no
dierences between the intervention group and the
control group in the median number of days in the ICU
or hospital, or the median number of days of mechanical
ventilation or renal replacement therapy. Finally, a multicenter RCT from Europe (Austria, Belgium, Spain,
France, Italy, Slovenia, and the Netherlands) and Israel,
which was stopped prematurely because of lack of dierence regarding blood glucose control, again SGC was not
associated with mortality reduction (15.3% in the intervention group versus 17.2% in the control group) [7].
Meta-analyses of randomized controlled trials of strict
glycemic control
Two meta-analyses, of which the rst included the rst
ve RCTs [18], and the second all trials except the last
RCT [19], showed SGC not to be associated with signicantly reduced hospital mortality. However, dierent
primary outcome measures were used in the successive
RCTs (that is, 28-day mortality, 90-day mortality, ICU
mortality and/or hospital mortality). This is not a trivial
comment, since, for instance, discharge criteria and
follow-up beyond ICU and hospital discharge may vary
and, as such, may have aected outcome. This makes
correct interpretation of the meta-analyses dicult, if
not impossible.
Schultz et al. Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
Page 3 of 9
Table 1. Randomized controlled trials on strict glycemic control (target blood glucose levels of 80 to 110 mg/dl)
Main results of the trial
Reference
Year What was compared?
Study population
van den Berghe
et al. [1]
2001 SGC versus standard therapy
(target blood glucose level
of 180 to 200 mg/dl if
exceeded 215 mg/dl)
2006 SGC versus standard therapy
(target blood glucose level
of 180 to 200 mg/dl if
exceeded 215 mg/dl)
2008 SGC versus standard therapy
(target blood glucose level
of 180 to 200 mg/dl)
2008 SGC versus standard therapy
(target blood glucose level
of 180 to 200 mg/dl)
2008 SGC versus standard therapy
(target blood glucose level
of 180 mg/dl if exceeded
200 mg/dl)
2009 SGC (target blood glucose
level of 81 to 108 mg/dl)
versus standard therapy
(target blood glucose level
of <180 mg/dl)
2009 SGC (target blood glucose
level of 80 to 110 mg/dl)
versus standard therapy (140
to 180 mg/dl)
1,548 surgical critically SGC decreased mortality
ill patients
(4.6versus 8.0%)
SGC raised the incidence
of severe hypoglycemia
(5.1versus 0.8%)
Yes
1,200 medical critically SGC decreased mortality of
ill patients
patients who stayed in ICU
3 days (43.0 versus 52.2%)
SGC raised the incidence
of severe hypoglycemia
(18.7versus 3.1%)
Yes
523 mixed medicalsurgical critically ill
patients
504 mixed medicalsurgical critically ill
patients
488 mixed medicalsurgical critically ill
patients
SGC raised the incidence
of severe hypoglycemia
(28.6versus 3.1%)
SGC raised the incidence
of severe hypoglycemia
(8.5versus 1.7%)
SGC raised the incidence
of severe hypoglycemia
(17.0versus 4.1%)
No
van den Berghe
et al. [2]
Arabi et al. [3]
De la Rosa
etal. [4]
Brunkhorst
etal.[5]
Finfer
et al. [6]
Preiser
et al. [7]
6,104 mixed medicalsurgical critically ill
patients
1,101 mixed medicalsurgical critically ill
patients
Differences between randomized controlled trials
of strict glycemic control - grading the evidence
There are several alternative explanations for why the ve
negative RCTs do not show benecial eects of SGC,
apart from the possibility that SGC may indeed not
benet ICU patients. These include, but are not restricted
to, variability in the performance of SGC, dierences
between trial designs, changes in standard of care,
dierences in timing (that is, initiation) of SGC, and the
convergence between the intervention groups and
control groups with respect to achieved blood glucose
levels in the successive RCTs.
Variability in the performance of strict glycemic control
SGC may seem an easy to implement strategy, but there
are several aspects of SGC that might be important and
are frequently overlooked [20]. Indeed, SGC is a complex
intervention that involves several sequential steps that
may all contain potential sources of variability (Figure 1).
In the two positive RCTs from Leuven, ICU nurses
were using accurate blood gas analyzers to measure
blood glucose in arterial blood at strict time points, and
in between those time points whenever deemed
necessary. Notably, in the second RCT from Leuven a
variety of glucose analyzers were used, not just blood gas
analyzers. SGC comprised a reliable continuous infusion
Mortality
SGC did not affect ICU
mortality (13.5% versus
17.1%)
SGC did not affect 28-day
mortality (36.6% versus
32.4%)
SGC did not affect 28-day
mortality (24.7 versus 26.0%);
SGC did not affect 90-day
mortality (39.7 versus 35.4%)
SGC did not affect 28-day
mortality (22.3 versus 20.8%);
SGC increased 90-day
mortality (27.5 versus 24.9%)
SGC did not affect 28-day
survival (17.2 versus 15.3%)
Severe hypoglycemia
Do results
support the
use of SGC?
No
No
SGC raised the incidence
of severe hypoglycemia
(6.8versus 0.5%)
No
SGC raised the incidence
of severe hypoglycemia
(8.7versus 2.7%)
No
of insulin exclusively via a central venous line, using
accurate syringe-driven infusion pumps. Delicate insulin
dose adaptations were to be performed exclusively by
ICU nurses who were especially trained to implement
this complex strategy (that is, executing insulin dose
adaptations), while based on a guideline, aiming for blood
glucose levels close to the lower normal limit, and also
requiring a high level of intuitive decision making. And,
nally, patients were kept in a non-fasting state at all
times - glucose was administered on the rst day, and
thereafter balanced enteral nutrition, supplemented
where needed by parenteral nutrition, was provided
during the entire stay in the ICU.
Several of the above mentioned methodological aspects
of SGC often diverged substantially in successive RCTs.
Indeed, blood glucose levels could be checked using
capillary whole blood samples, using less accurate
glucose analyzers [3-7]. Notably, this was also the case in
the second RCT from Leuven - this may be one of the
reasons that the rate of severe hypoglycemia was so much
higher in this trial. Instead of accurate syringe-driven
infusion pumps, volumetric infusion pumps could be, or
were exclusively, used [3,4], or this was not mentioned
[7]. Also, training of ICU nurses in the guideline was
either not mentioned (and thus possibly not done in a
structured way) [5,7], or seemed to be restricted to
Schultz et al. Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
Page 4 of 9
Figure 1. Methodological aspects of strict glycemic control, which may contain potential sources of variability in the performance of
this strategy. Items are categorized into the following subjects: monitoring, insulin delivery, algorithm, and experience. Items are also roughly
positioned on a line from easy, simple, distinct and/or clear to implement towards obscure, indistinct, complex and/or difficult to translate from
one center to another. Specific elements per item indicated with an asterisk are as performed in the single-center RCTs from Leuven. SGC, strict
glycemic control.
training related more to the prevention and correction of
hypoglycemia [3]. It was either not stated whether ICU
nurses exclusively titrated insulin, or it was stated that
both ICU nurses and ICU physicians decided on insulin
dose adaptations [5], which may be inappropriate. And
nally, glucose administration on the rst day was
frequently not mentioned and thus probably not a part of
the protocol [3,5,7].
Most challenging in this context, however, is the
expertise-based control system as applied by the ICU
nurses from Leuven. While the algorithm from Leuven
contains no more than a set of simple rules (that is, there
is an absence of explicit rules, such as present in closedloop systems, computer-based decision support systems,
and paper-based systems using sliding scales), it required
a high level of intuitive decision making by its users. It is
dicult, if not impossible, to identify the specic
elements of this intuitive control system that contributed
to the outcome observed in the trials from Leuven. The
same may apply for the skill and motivation of ICU
nurses from Leuven. Their talent in implementing SGC,
as well as motivation to apply it, may very well not have
been copied in trials beyond their ICU. In this context it
is important to note that the interventional arms of some
of the multi-center RCTs contained very low numbers of
patients. For instance, the German multi-center RCT
included 247 patients from 18 centers, which means that
only 14 patients were in the interventional arm of the
study in each center [5]. A similar calculation for the
European multi-center RCT suggests that only 26 patients
from each center were in the interventional arm [7]. It
can also be questioned whether the practitioners in these
trials were truly skilled in SGC.
We consider all these dierences from the two positive
RCTs to be potentially responsible, at least in part, for the
diverse outcomes of the ve negative RCTs. As indicated
in Figure 1, methodological aspects of SGC can be scored
from relatively easy, simple, distinct and/or clear to
obscure, indistinct, complex and/or dicult with
regard to translation from one ICU (or study) to another
Schultz et al. Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
Page 5 of 9
Figure 2. Blood glucose levels (mean or median in the control or conventional group (closed bars) and strict glycemic control group
(open bars) of seven randomized controlled trials. Original single-center randomized controlled trials (RCTs) from Leuven [1,2]; single-center
RCTs [3,4]; multi-center RCTs [5-7]. Dotted lines indicate the blood glucose levels in the two original single-center RCTs from Leuven.
ICU (or study). For example, decisions on blood glucose
monitoring are easily made, simple, distinct and clear;
whereas an intuitive control system for SGC is obscure,
indistinct, very complex and dicult, if not impossible to
translate into another setting. All other aspects can be
scored in between these extremes.
Study design
One issue with the three smaller RCTs is that they were
all statistically underpowered to detect a reasonable
mortality dierence [3-5]. Especially the early termination of the German study was rather inopportune [5]:
while this study performed best in the intervention
group, with blood glucose levels closer to the upper limit
of SGC than the other negative trials, the study protocol
allowed for early termination because of safety. The
increase in the incidence of severe hypoglycemia forced
the investigators to stop the study, leaving us with underpowered trial results. Although the last RCT specically
addressed the issue of statistical power, this trial was
possibly also underpowered, as outlined below.
Change in standard of care
Glycemic control has changed over the past decade. A
policy of insulin therapy to target lower blood glucose
levels has been adopted in many ICUs since the publication of the rst RCT of SGC [1]. Accordingly, SGC was
compared with distinct control targets (Figure 2).
Indeed, in all the trials except for two, glycemic control
had improved in the control group when compared to the
rst RCT. In addition, an increase was noticed in the
number of patients who received insulin, or there was an
increase in the amount of infused insulin in the control
group [2-7]. This diversity makes the successive trials
fundamentally dierent from the rst RCT. Indeed, these
RCTs were executed in the attened part of the observed
blood glucose level-mortality risk curve [13]. The hypothesized eect size in the last two RCTs [6,7] (3 to 4%
absolute reduction in risk of death, similar to what was
observed in the original two RCTs [1,2]) was, therefore,
too optimistic: according to the pooled analysis of the
original two RCTs [21], the absolute reduction in mortality that could have been expected from further lowering blood glucose levels compared to the standard care
level was only roughly 1%. This would mean that tens of
thousands of patients would be needed to show this eect
in a multi-center setting (and not thousands of patients,
as in the RCT from Australia/New Zealand and Canada
[6]).
Timing of the intervention
In most trials time till reaching the preset blood glucose
level target is insuciently reported. When time till
target is too long, the time window for prevention of
toxicity of hyperglycemia may have passed and irreversible damage may already have occurred [22]. This
phenomenon has also been suggested by the pooled
analysis of the two original RCTs [21]. The time lag
between onset of hyperglycemia (which is usually present
on admission to ICU) and the time that blood glucose
levels are within the target range may depend on several
factors, including a delay in identifying eligible patients,
randomization and initiation of SGC, the SGC algorithm
itself, and the quality of its implementation. All these
factors could be an issue of study design. Of note, for one
RCT we can conclude this to be an important factor, as
Schultz et al. Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
initiation of SGC in that trial was delayed by more than
13 hours because of randomization [6].
Achieved blood glucose levels
It is notable that none of the RCTs completed after the
two original trials managed to achieve the strict degree of
glycemic control achieved by the Leuven investigators
[1,2]. Indeed, no trial had a median or mean blood
glucose level in the intervention group below the upper
normal target of blood glucose (Figure 2). Of note, one
meta-analysis suggests that studies that managed to
achieve the blood glucose target showed a reduced
mortality whereas studies that did not succeed in
reaching the target reported no benet or even an
increased mortality [19]. This nding underlines that
SGC, though basically simple, is not an easy to implement
strategy.
Uncertain factors
Other, yet uncertain factors may explain the divergent
trial results, for instance, the variability of blood glucose
levels. SGC algorithms, if properly applied, should
decrease both the mean blood glucose level and its
variability. Recent studies showed signicant associations
between variability of blood glucose levels and patient
outcomes [23-25]. From personal experience we know
that implementation of SGC takes considerable time.
Variability of blood glucose levels in the multi-center
RCTs, therefore, is not unlikely as some ICUs in these
trials must have recruited only a limited number of
patients [5-7]. Variability of blood glucose levels has
neither been studied and reported nor compared between
the RCTs. Many other metrics of successful glycemic
control exist, but were neither measured nor compared
among the RCTs [26].
Implementation of SGC - rationalizing fears and
consequences of a strict regimen
The issue of severe hypoglycemia
Severe hypoglycemia is a feared complication of SGC.
Undoubtedly, with implementation of SGC the incidence
of severe hypoglycemia increases. Reported incidences of
severe hypoglycemia (blood glucose level <40 mg/dl) rise
by ve- to ten-fold compared to conventional blood
glucose control in RCTs (Table 1).
Neuroglycopenia may cause cerebral damage, epileptic
insults or even coma [27]. However, how deep does hypoglycemia need to be, and how long its duration, to cause
these eects [28]? In the former century, repeated episodes of insulin-induced hypoglycemic coma for periods
ranging from 45 minutes to 3 hours for the treatment of
opiate addiction and schizophrenia have been found to
have minimal long-term eects and a mortality of less
than 1% [29]. In addition, long-term follow up of patients
Page 6 of 9
with diabetes mellitus in large prospective trials failed to
detect any association between the frequency of severe
hypoglycemia and cognitive decline [30,31]. Only subtle,
reversible impairments of attention could be detected in
non-diabetic patients undergoing dynamic pituitary
function assessment using hypoglycemic stress with
blood glucose levels of 29 mg/dl [32].
At present we cannot conclude with certainty that
severe hypoglycemia with SGC harms critically ill patients.
Two retrospective studies identied (severe) hypoglycemia as an independent predictor of mortality [13,33].
However, 30% of patients with severe hypoglycemia in
one of the above cited retrospective studies were not on
insulin therapy in the preceding 12 hours, and only a
minority of patients was on intravenous insulin therapy
[33]. Therefore, this study hardly oers an answer to the
question of whether severe hypoglycemia with SGC
inuences outcome. Similar problems exist with the
interpretation of the results from the other retrospective
study, in which the impact of early (that is, <24 hours
after admission) hypoglycemia (not severe hypoglycemia)
was studied. First, the occurrence of hypoglycemia may
very well relate to severity of disease on admission.
Second, the studied ICUs did not apply SGC [13]. Nevertheless, multivariable regression analysis of the second
RCT of SGC in Leuven conrmed that severe hypoglycemia was independently associated with mortality, and
may have diminished the benet of the intervention [2].
Of interest, one experiment performed in rodents
showed that brain damage was not associated with the
duration of severe hypoglycemia, but instead with its
correction with intravenous dextrose, causing formation
of radicals [34]. Indeed, brain damage correlated to the
concentration and amount of dextrose used to correct
severe hypoglycemia. Hypothetically, in practice, bolus
glucose reperfusion of the depleted brain may cause more
damage then the period of severe hypoglycemia itself.
Finally, rapid administration of concentrated glucose
solution for the correction of hypoglycemia may cause
dangerous arrhythmias, potentially via hyperkalemia
from the rapid administration of a concentrated glucose
solution [35].
Which caregiver should be responsible for the
implementation of SGC?
One nal question on SGC concerns who should be
responsible for its implementation in daily practice? In
the hospital where the two positive RCTs of SGC were
performed, without doubt SGC was (and still is) a
completely nurse-driven strategy without the interference
of ICU physicians, who are not at the bedside as frequently as ICU nurses [36]. Although several arguments
plea for SGC being a nurse-driven strategy, one could
argue that ICU nurses lack sucient background
Schultz et al. Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
information to safely apply this strategy, especially when
blood glucose control aims at the lower limits of
normoglycemia (that is, with an increased risk of severe
hypoglycemia). Of similar importance may be the fact
that ICU nurses may feel legally unprotected when
applying SGC [10]. However, a nested case-control study
revealed that many of the predisposing factors for hypoglycemia in ICU patients were in fact easy to recognize
[37]. Predisposing factors included decreases of nutrition
without adjustment for insulin infusion, sepsis, and
changes in inotropic support. These are all earlier and
better recognized by bedside ICU nurses than by ICU
physicians taking care of many patients at the same time.
We cannot be certain whether inadequacies in
performing safe (that is, preventing severe hypoglycemia)
and eective (that is, achieving the target) SGC is an
important factor in explaining the dierences between
the positive and negative RCTs. However, as pointed out
above, studies suggest that blood glucose variability does
have an impact on outcome [25]. One advantage of
nurse-driven SGC may be that there is less blood glucose
variability, since ICU nurses can respond earlier to
changes in the blood glucose level, and since ICU nurses
can titrate insulin without the interference of ICU
physicians, who are not at the bedside as frequently as
ICU nurses.
Discussion and future perspectives
During critical illness, glucose should not be seen as an
innocent bystander. Indeed, lowering blood glucose levels
has the potential to prevent injury to already threatened
vital organs. However, the optimum level as well as the
optimal mode to reach that level still needs to be dened.
The observations that SGC exerted both positive [1,2] and
negative eects [6] poses a fascinating impasse.
Of course, it should be recognized that the singlecenter RCTs may have suered from several drawbacks.
First, known, unknown and/or unrecognized dierences
between study settings may obstruct generalizability of
results. Second, motivational eects of investigators can
never be ruled out, in particular when investigators
cannot be blinded. Such factors all apply to the singlecenter trials on SGC. However, one may also argue from
a methodological standpoint that the single-center design
of the two original RCTs was preferable. It could be
dicult, if not impossible, to identify all important
factors of this complex intervention that contributed to
the outcome as observed in the RCTs from Leuven. In
particular, poorly identied factors, as discussed above,
may not have been transferred to other ICUs. However,
as such, the two original RCTs, as well as a third positive
RCT of SGC in pediatric patients from the same
investigators [38], remain to have internal validity but fail
to have external validity. Nevertheless, rather than
Page 7 of 9
concluding that SGC does not benet critically ill
patients based on the successive negative RCTs in other
ICUs, we prefer rst to search for dierences between the
designs of the positive and negative RCTs.
There are several possible ways to go from here. We
could accept the lack of evidence on the optimum level of
glycemic control. The currently available evidence from
the seven RCTs does not allow us to condently make an
overall recommendation. Indeed, the question of one
optimal target for glycemic control in ICU patients
remains unanswered. Consequently, any advice remains
pragmatic: assess whether the hypothesized benet was
realistic, assess whether statistical power was sucient,
assess the level of evidence of the studies, assess whether
the tools to measure and control blood glucose were
adequate, assess whether the targets were achieved, and
nally assess whether the levels of glycemic control
diverged relevantly. Clinicians should also determine
how comparable the patients in the dierent RCTs are to
their own and decide on what is their best target for
glycemic control.
Alternatively, we perform another RCT, using the same
targets as in the positive RCTs [1,2], both for the
interventional and the control groups. This, however,
may be unethical if not impossible for several reasons.
First, standard of care regarding glycemic control has
denitely changed over the past decade (that is, can we
speak of conventional therapy when targeting a higher
threshold than commonly applied?). How to explain that
we should perform a new trial in which we deliberately
expose critically ill patients to the risks of hyperglycemia?
On the other hand, one may say that the negative trials
on SGC did not show that mild hyperglycemia harmed
ICU patients (although in most trials hyperglycemia was
less severe than in the two positive RCTs). However, one
could also posit that it is unethical to discard the evidence
from the two positive RCTs, and we are obliged to repeat
this study.
Given the substantial evidence for the generation of
harm from hyperglycemia [13-16] and the conicting
results from the seven RCTs [1-7], considerable work
remains to be done in identifying the confounding factors
in the clinical application of SGC. This process needs to
be explicit and systematic, and should at least include the
points raised in this commentary. An individual patient
data meta-analysis examining the discrepancies between
studies may be a good start. If new RCTs are to be
performed, investigators should recognize the several
shortcomings of the recent negative trials, as previously
described. Most important, glucose levels in the
intervention groups in any new trials should indeed reach
targets between 80 and 110 mg/dl.
Perhaps one other step in this eld of ICU medicine
will involve the next generation of (continuous or
Schultz et al. Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
near-continuous) glucose monitors and treatment algorithm technology [39]. These may reduce the incidence of
severe hypoglycemia, glycemic variability and the nursing
work burden.
What should those caregivers do who want to implement this strategy? As outlined above, key aspects of
SGC should be recognized: accurate blood gas analyzers
to measure blood glucose in arterial blood at strict time
points; reliable continuous infusion of insulin exclusively
via a central venous line; accurate syringe-driven infusion
pumps; insulin dose-adaptations performed exclusively
by specially trained ICU nurses, with high levels of intuitive
decision making; and non-fasting state at all times. Results
from animal studies point us to potential risks associated
with overcorrection of severe hypoglycemia.
Conclusion
While SGC decreased mortality and morbidity of adult
critically ill patients in two RCTs, ve successive RCTs
failed to show a benet of this strategy, with one trial
even reporting unexpected higher mortality. There are
several alternative explanations for the ve negative RCTs
that showed no benecial eects of SGC, apart from the
possibility that SGC may indeed not benet critically ill
patients. The currently available evidence from the seven
RCTs, however, does not allow us to condently make an
overall recommendation regarding glycemic control.
Clinicians should determine how comparable the patients
in the dierent RCTs are to their own and decide on what
is their best target for glycemic control. More RCT
evidence is needed, but it is questionable whether there
will ever be a new trial using the same targets as in the
original RCTs.
Page 8 of 9
3.
4.
5.
6.
7.
8.
9.
10.
Abbreviations
RCT = randomized controlled trial, SGC = strict glycemic control.
11.
Competing interests
The authors declare that they have no competing interests.
12.
Authors contributions
MJS searched the literature, interpreted the results and drafted the
manuscript. REH participated in drafting and reviewing the manuscript. PS
participated in drafting the manuscript. All authors approved the final version
of the manuscript.
Author details
1
Department of Intensive Care, Academic Medical Center, University
of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, the Netherlands.
2
Laboratory of Experimental Intensive Care and Anesthesiology, Academic
Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ
Amsterdam, the Netherlands. 3Department of Intensive Care, Gelre Hospitals,
location Lukas, Albert Schweitzerlaan 31, 7334 DZ Apeldoorn, the Netherlands
13.
14.
15.
16.
17.
18.
Published: 7 June 2010
19.
References
1. Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M,
Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R: Intensive insulin therapy
in the critically ill patients. N Engl J Med 2001, 345:1359-1367.
2. Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants
20.
I, Van Wijngaerden E, Bobbaers H, Bouillon R: Intensive insulin therapy in the
medical ICU. N Engl J Med 2006, 354:449-461.
Arabi YM, Dabbagh OC, Tamim HM, Al-Shimemeri AA, Memish ZA, Haddad
SH, Syed SJ, Giridhar HR, Rishu AH, Al-Daker MO, Kahoul SH, Britts RJ, Sakkijha
MH: Intensive versus conventional insulin therapy: a randomized
controlled trial in medical and surgical critically ill patients. Crit Care Med
2008, 36:3190-3197.
De La Rosa Gdel C, Donado JH, Restrepo AH, Quintero AM, Gonzlez LG,
Saldarriaga NE, Bedoya M, Toro JM, Velsquez JB, Valencia JC, Arango CM,
Aleman PH, Vasquez EM, Chavarriaga JC, Yepes A, Pulido W, Cadavid CA;
Grupo de Investigacion en Cuidado intensivo: GICI-HPTU: Strict glycaemic
control in patients hospitalised in a mixed medical and surgical intensive
care unit: a randomised clinical trial. Crit Care 2008, 12:R120.
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N,
Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S,
Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C,
Natanson C, Loeffler M, Reinhart K; German Competence Network Sepsis
(SepNet): Intensive insulin therapy and pentastarch resuscitation in severe
sepsis. N Engl J Med 2008, 358:125-139.
NICE-SUGAR Study Investigators, Finfer S, Chittock DR, Su SY, Blair D, Foster D,
Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hbert PC, Heritier S,
Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R,
Potter J, Robinson BG, Ronco JJ: Intensive versus conventional glucose
control in critically ill patients. N Engl J Med 2009, 360:1283-1297.
Preiser JC, Devos P, Ruiz-Santana S, Melot C, Annane D, Groeneveld J,
Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J, Joannidis M,
Stecher A, Chiolro R: A prospective randomised multi-centre controlled
trial on tight glucose control by intensive insulin therapy in adult
intensive care units: the Glucontrol study. Intensive Care Med 2009,
35:1738-1748.
Angus DC, Abraham E: Intensive insulin therapy in critical illness. Am J
Respir Crit Care Med 2005, 172:1358-1359.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K,
Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey
M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT,
Townsend S, Vender JS, Zimmerman JL, Vincent JL; International Surviving
Sepsis Campaign Guidelines Committee; American Association of CriticalCare Nurses; American College of Chest Physicians; American College of
Emergency Physicians; Canadian Critical Care Society; European Society of
Clinical Microbiology and Infectious Diseases, et al.: Surviving Sepsis
Campaign: international guidelines for management of severe sepsis and
septic shock: 2008. Crit Care Med 2008, 36:296-327.
Schultz MJ, Royakkers AA, Levi M, Moeniralam HS, Spronk PE: Intensive
insulin therapy in intensive care: an example of the struggle to implement
evidence-based medicine. PLoS Med 2006, 3:e456.
Schultz MJ, de Graaff MJ, Royakkers AA, van Braam Houckgeest F, van der
Sluijs JP, Kieft H, Spronk PE: Practice of strict glycemic control in critically ill
patients. Med Sci Monit 2008, 14:RA191-197.
Aragon D: Evaluation of nursing work effort and perceptions about blood
glucose testing in tight glycemic control. Am J Crit Care 2006, 15:370-377.
Bagshaw SM, Egi M, George C, Bellomo R: Early blood glucose control and
mortality in critically ill patients in Australia. Crit Care Med 2009, 37:463-470.
Finney SJ, Zekveld C, Elia A, Evans TW: Glucose control and mortality in
critically ill patients. JAMA 2003, 290:2041-2047.
Krinsley JS: Association between hyperglycemia and increased hospital
mortality in a heterogeneous population of critically ill patients. Mayo Clin
Proc 2003, 78:1471-1478.
Falciglia M, Freyberg RW, Almenoff PL, DAlessio DA, Render ML:
Hyperglycemia-related mortality in critically ill patients varies with
admission diagnosis. Crit Care Med 2009, 37:3001-3009.
Van den Berghe G: How does blood glucose control with insulin save lives
in intensive care? J Clin Invest 2004, 114:1187-1195.
Wiener RS, Wiener DC, Larson RJ: Benefits and risks of tight glucose control
in critically ill adults: a meta-analysis. JAMA 2008, 300:933-944.
Griesdale DE, de Souza RJ, van Dam RM, Heyland DK, Cook DJ, Malhotra A,
Dhaliwal R, Henderson WR, Chittock DR, Finfer S, Talmor D: Intensive insulin
therapy and mortality among critically ill patients: a meta-analysis
including NICE-SUGAR study data. CMAJ 2009, 180:821-827.
Van den Berghe G, Schetz M, Vlasselaers D, Hermans G, Wilmer A, Bouillon R,
Mesotten D: Clinical review: Intensive insulin therapy in critically ill
patients: NICE-SUGAR or Leuven blood glucose target? J Clin Endocrinol
Schultz et al. Critical Care 2010, 14:223
http://ccforum.com/content/14/3/223
Metab 2009, 94:3163-3170.
21. Van den Berghe G, Wilmer A, Milants I, Wouters PJ, Bouckaert B, Bruyninckx F,
Bouillon R, Schetz M: Intensive insulin therapy in mixed medical/surgical
intensive care units: benefit versus harm. Diabetes 2006, 55:3151-3159.
22. Ceriello A, Ihnat MA, Thorpe JE: Clinical review 2: The metabolic memory:
is more than just tight glucose control necessary to prevent diabetic
complications? J Clin Endocrinol Metab 2009, 94:410-415.
23. Krinsley JS: Glycemic variability: a strong independent predictor of
mortality in critically ill patients. Crit Care Med 2008, 36:3008-3013.
24. Bagshaw SM, Bellomo R, Jacka MJ, Egi M, Hart GK, George C: The impact of
early hypoglycemia and blood glucose variability on outcome in critical
illness. Crit Care 2009, 13:R91.
25. Egi M, Bellomo R, Reade MC: Is reducing variability of blood glucose the
real but hidden target of intensive insulin therapy? Crit Care 2009, 13:302.
26. Eslami S, de Keizer NF, de Jonge E, Schultz MJ, Abu-Hanna A: A systematic
review on quality indicators for tight glycaemic control in critically ill
patients: need for an unambiguous indicator reference subset. Crit Care
2008, 12:R139.
27. Vriesendorp TM, De Vries JH, van Santen S, Moeniralam HS, de Jonge E, Roos
Y, Schultz MJ, Rosendaal FR, Hoekstra JBL: Outcome and short-term
consequences of hypoglycemia in the intensive care unit. Crit Care Med
2006, 34:2714-2718.
28. Mackenzie I, Ingle S, Zaidi S, Buczaski S: Hypoglycaemia? So what! Intensive
Care Med 2006, 32:620-621.
29. Sargant W, Slater E: Physical Methods of Treatment in Psychiatry. Edinburgh:
Livingstone; 1944.
30. Austin EJ, Deary IJ: Effects of repeated hypoglycemia on cognitive function:
a psychometrically validated reanalysis of the Diabetes Control and
Complications Trial data. Diabetes Care 1999, 22:1273-1277.
31. Diabetes Control and Complications Trial/Epidemiology of Diabetes
Interventions and Complications Study Research Group, Jacobson AM,
Musen G, Ryan CM, Silvers N, Cleary P, Waberski B, Burwood A, Weinger K,
Page 9 of 9
32.
33.
34.
35.
36.
37.
38.
39.
Bayless M, Dahms W, Harth J: Long-term effect of diabetes and its
treatment on cognitive function. N Engl J Med 2007, 356:1842-1852.
Osorio I, Arafah BM, Mayor C, Troster AI: Plasma glucose alone does not
predict neurologic dysfunction in hypoglycemic nondiabetic subjects.
Ann Emerg Med 1999, 33:291-298.
Krinsley JS, Grover A: Severe hypoglycemia in critically ill patients: risk
factors and outcomes. Crit Care Med 2007, 35:2262-2267.
Suh SW, Gum ET, Hamby AM, Chan PH, Swanson RA: Hypoglycemic
neuronal death is triggered by glucose reperfusion and activation of
neuronal NADPH oxidase. J Clin Invest 2007, 117:910-918.
Bhatia A, Cadman B, Mackenzie I: Hypoglycemia and cardiac arrest in a
critically ill patient on strict glycemic control. Anesth Analg 2006,
102:549-551.
de Graaff MJ, Spronk PE, Schultz MJ: Tight glycaemic control: intelligent
technology or a nurse-wise strategy? Crit Care 2007, 11:421.
Vriesendorp TM, van Santen S, DeVries JH, de Jonge E, Rosendaal FR, Schultz
MJ, Hoekstra JB: Predisposing factors for hypoglycemia in the intensive
care unit. Crit Care Med 2006, 34:96-101.
Vlasselaers D, Milants I, Desmet L, Wouters PJ, Vanhorebeek I, van den Heuvel
I, Mesotten D, Casaer MP, Meyfroidt G, Ingels C, Muller J, Van Cromphaut S,
Schetz M, Van den Berghe G: Intensive insulin therapy for patients in
paediatric intensive care: a prospective, randomised controlled study.
Lancet 2009, 373:547-556.
Krinsley JS, Preiser JC: Moving beyond tight glucose control to safe
effective glucose control. Crit Care 2008, 12:149.
doi:10.1186/cc8966
Cite this article as: Schultz MJ, et al.: Strict or loose glycemic control in
critically ill patients - implementing best available evidence from the
randomized controlled trials. Critical Care 2010, 14:223.
You might also like
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderFrom EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNo ratings yet
- Assessment and Treatment of Hyperglycemia in Critically IllDocument6 pagesAssessment and Treatment of Hyperglycemia in Critically IllYousif ElmasryNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Song 2014Document11 pagesSong 2014Ayssa WitjaksonoNo ratings yet
- Ajtr0014 4757Document20 pagesAjtr0014 4757Eyal RobinsonNo ratings yet
- Management of Inpatient Hyperglycemia: 2011 Endocrine Society MeetingDocument5 pagesManagement of Inpatient Hyperglycemia: 2011 Endocrine Society MeetingDirga Rasyidin LNo ratings yet
- Articulo Chingon E.FDocument4 pagesArticulo Chingon E.FRuggery LeonNo ratings yet
- Co 2019 Controle Glicemico IntDocument8 pagesCo 2019 Controle Glicemico InthauhauNo ratings yet
- 10 Glycemic Control in Perioperative PeriodDocument5 pages10 Glycemic Control in Perioperative PeriodAna-Maria CroitoruNo ratings yet
- Implications of The United Kingdom Prospective Diabetes StudyDocument5 pagesImplications of The United Kingdom Prospective Diabetes StudyAgustin MendezNo ratings yet
- 349 FullDocument3 pages349 FullsenkonenNo ratings yet
- Mayo Clinic Proceedings: Critical Glucose Control: The Devil Is in The DetailsDocument4 pagesMayo Clinic Proceedings: Critical Glucose Control: The Devil Is in The DetailstfurrahmanNo ratings yet
- Eckert 2021Document10 pagesEckert 2021Igor EckertNo ratings yet
- Predicting The Severity of Acute PancreatitisDocument25 pagesPredicting The Severity of Acute PancreatitisAdrianaIDCNo ratings yet
- 2012 Best Parctice Medical O Grady TH en FHADocument7 pages2012 Best Parctice Medical O Grady TH en FHASol Del Mar SarmientoNo ratings yet
- Using The EQ-5D Index Score As A Predictor of Outcomes in Patients With Type 2 Diabetes - Clarke May08Document20 pagesUsing The EQ-5D Index Score As A Predictor of Outcomes in Patients With Type 2 Diabetes - Clarke May08Haneesha MuddasaniNo ratings yet
- FFE33 F5 Ad 01Document4 pagesFFE33 F5 Ad 01m_kamenovaNo ratings yet
- DCC White PaperDocument7 pagesDCC White PaperSteveEpsteinNo ratings yet
- Plasmaexchange LupusDocument26 pagesPlasmaexchange LupusCristina ElenaNo ratings yet
- The "Trea T To Ta Rge T" (17415)Document18 pagesThe "Trea T To Ta Rge T" (17415)YoaAguilarCastilloNo ratings yet
- P .001) and A Shorter Hospitalization: Reprints: Sergio Amadori, Department of Hematology, University "TorDocument9 pagesP .001) and A Shorter Hospitalization: Reprints: Sergio Amadori, Department of Hematology, University "TordradrianramdhanyNo ratings yet
- Full TextDocument8 pagesFull TextJeNeth RevilNo ratings yet
- Sepsis ArticuloDocument7 pagesSepsis ArticuloJose Adriel Chinchay FrancoNo ratings yet
- Tight Glycemic Control in Critically Ill PediatricDocument11 pagesTight Glycemic Control in Critically Ill Pediatricbella friscaamaliaNo ratings yet
- 2022 - Cytokine Hemoadsorption During Cardiac Surgery Versus Standard Surgical Care For Infective Endocarditis (REMOVE) - Results From A Multicenter, Randomized, Controlled Trial - BDocument2 pages2022 - Cytokine Hemoadsorption During Cardiac Surgery Versus Standard Surgical Care For Infective Endocarditis (REMOVE) - Results From A Multicenter, Randomized, Controlled Trial - Brodrigo sacchiNo ratings yet
- Glutamina IVDocument11 pagesGlutamina IVBLADIMIR ALEJANDRO GIL VALENCIANo ratings yet
- Impact of Community-Based Cardiac Rehabilitation On Clinical Parameters of Patients With Cardiovascular DiseasesDocument7 pagesImpact of Community-Based Cardiac Rehabilitation On Clinical Parameters of Patients With Cardiovascular DiseasesAfrizal FauziansyahNo ratings yet
- Kol Ditz 2016Document3 pagesKol Ditz 2016Lanna HarumiyaNo ratings yet
- Cytotoxics or Biologics in The Treatment of Sjogren's Syndrome Biological AgentsDocument10 pagesCytotoxics or Biologics in The Treatment of Sjogren's Syndrome Biological AgentsPablo Isaias Jaramillo FrancoNo ratings yet
- SUultima EvidenciaDocument8 pagesSUultima Evidenciasalvado moyanoNo ratings yet
- Lheureux 2014Document6 pagesLheureux 2014Kaustav LahiriNo ratings yet
- 10 1152@ajpendo 00512 2019Document52 pages10 1152@ajpendo 00512 2019Aldo González SalinasNo ratings yet
- Health20100700010 64690396Document5 pagesHealth20100700010 64690396MellTandiNo ratings yet
- How Do We Balance The Risk?Document14 pagesHow Do We Balance The Risk?Ghea Ananta AdrianNo ratings yet
- Korti Ko SteroidDocument7 pagesKorti Ko SteroidSisca AndrianyNo ratings yet
- The Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsDocument9 pagesThe Efficacy and Safety of Triple Vs Dual Combination of ARB, CCB, and DiureticsLucky PratamaNo ratings yet
- Pmls ArticleDocument8 pagesPmls ArticleEd dela PenaNo ratings yet
- Zhou2019 Article InsulinDegludecANovelUltra-LonDocument18 pagesZhou2019 Article InsulinDegludecANovelUltra-LonmehakNo ratings yet
- Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-Analysis - PMCDocument24 pagesGlobal Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-Analysis - PMCtrimardiyanaisyanNo ratings yet
- The COURAGE (Clinical Outcomes UtilizingDocument3 pagesThe COURAGE (Clinical Outcomes UtilizingAgim KrasniqiNo ratings yet
- NR Endo 201421Document6 pagesNR Endo 201421Lucia VillacrizNo ratings yet
- Reduccion de Lactato en Shock Septico 2015Document2 pagesReduccion de Lactato en Shock Septico 2015mayraNo ratings yet
- AbstractDocument10 pagesAbstractVanakia DaustinNo ratings yet
- 5 Recent Trials in Stress Ulcer ProphylaxisDocument6 pages5 Recent Trials in Stress Ulcer ProphylaxisCharan Teja Reddy AvulaNo ratings yet
- Management of Diabetes Mellitus in Patients With Chronic Kidney DiseaseDocument9 pagesManagement of Diabetes Mellitus in Patients With Chronic Kidney DiseasezakyNo ratings yet
- Vol 3 6 Sym9 Egi PDFDocument7 pagesVol 3 6 Sym9 Egi PDFCherryNo ratings yet
- The Metabolic Syndrome: Comparison of Newly Proposed IDF, Modified ATP III and WHO Criteria and Their AgreementsDocument6 pagesThe Metabolic Syndrome: Comparison of Newly Proposed IDF, Modified ATP III and WHO Criteria and Their AgreementsjoelNo ratings yet
- Keywords: Autoimmune Disease, Homeostasis, Immune-Modulation, Immunosuppressive DrugsDocument7 pagesKeywords: Autoimmune Disease, Homeostasis, Immune-Modulation, Immunosuppressive DrugsStefan PopoviciNo ratings yet
- Tight GlycemicDocument10 pagesTight GlycemicIsmail Mohammed AbdelgawadNo ratings yet
- Efficacy of Lifestyle Interventions in Patients With Type 2 Diabetes - A Systematic Review and Meta-AnalysisDocument11 pagesEfficacy of Lifestyle Interventions in Patients With Type 2 Diabetes - A Systematic Review and Meta-AnalysisDara Agusti MaulidyaNo ratings yet
- Antibiotics 02 00001Document10 pagesAntibiotics 02 00001Jenny AlmagroNo ratings yet
- Nuclearoption For InsulinomaDocument3 pagesNuclearoption For Insulinomadantheman123No ratings yet
- Lactate MonitoringDocument6 pagesLactate Monitoringaliv8s3624No ratings yet
- Hypoglycemia - The Neglected ComplicationDocument23 pagesHypoglycemia - The Neglected Complication4g5xwdvh9sNo ratings yet
- In Patients With Acute Myocardial Infarction, The Impact of Hyperglycemia As A Risk Factor For Mortality Is Not Homogeneous Across Age-GroupsDocument3 pagesIn Patients With Acute Myocardial Infarction, The Impact of Hyperglycemia As A Risk Factor For Mortality Is Not Homogeneous Across Age-Groupsatika_No ratings yet
- Saxagliptin 453Document4 pagesSaxagliptin 453Oana MariaNo ratings yet
- 2015 Article 215Document15 pages2015 Article 215alerta.bfcmNo ratings yet
- Comparison of Scores in AclfDocument9 pagesComparison of Scores in AclftahayaseenfcpsgastroNo ratings yet
- Article AmalDocument16 pagesArticle Amalsaliha mharchiNo ratings yet
- Eur Heart J 2013Document13 pagesEur Heart J 2013nikeNo ratings yet
- Co MonitoringDocument9 pagesCo MonitoringSiva SankarNo ratings yet
- Transfer Professional LicenseDocument8 pagesTransfer Professional LicenseSiva SankarNo ratings yet
- My Garden Class 1Document20 pagesMy Garden Class 1Siva SankarNo ratings yet
- ANACONDADocument3 pagesANACONDASiva SankarNo ratings yet
- ARDSDocument7 pagesARDSSiva SankarNo ratings yet
- Elsevier Opinion Piece Nov2017Document3 pagesElsevier Opinion Piece Nov2017Jilani ShaikNo ratings yet
- Guidelines For PhysiciansDocument38 pagesGuidelines For PhysiciansSiva SankarNo ratings yet
- Ultrasound Guided Regional Nerve BlocksDocument32 pagesUltrasound Guided Regional Nerve BlocksSiva SankarNo ratings yet
- DNB Final BS Revised 2016Document68 pagesDNB Final BS Revised 2016Kaustubh LanjeNo ratings yet
- Indian Bank ChallanDocument1 pageIndian Bank ChallanSiva SankarNo ratings yet
- Perioperative Management of Acquired Hemophilia A: A Case Report and Review of LiteratureDocument3 pagesPerioperative Management of Acquired Hemophilia A: A Case Report and Review of LiteratureSiva SankarNo ratings yet
- Sedation and Anesthesia in GI Endoscopy 2008Document12 pagesSedation and Anesthesia in GI Endoscopy 2008Siva SankarNo ratings yet
- An Unusual Cause of Fat Embolism Syndrome.36Document3 pagesAn Unusual Cause of Fat Embolism Syndrome.36Siva SankarNo ratings yet
- H, C Radiolabeled Compounds and Their Applications in Metabolism StudyDocument5 pagesH, C Radiolabeled Compounds and Their Applications in Metabolism StudySiva SankarNo ratings yet
- Br. J. Anaesth.-2010-Hong-506-10Document5 pagesBr. J. Anaesth.-2010-Hong-506-10Siva SankarNo ratings yet
- SR-JR Leave FormDocument5 pagesSR-JR Leave FormSiva SankarNo ratings yet
- Obesity 2Document12 pagesObesity 2Siva SankarNo ratings yet
- Fox - Appendix R-Cox-regressionDocument18 pagesFox - Appendix R-Cox-regressionlinadiazbejarNo ratings yet
- Br. J. Anaesth.-2013-Desmet-445-52Document8 pagesBr. J. Anaesth.-2013-Desmet-445-52Siva SankarNo ratings yet
- Uterine Dehiscence During Initiation of Spinal.1Document2 pagesUterine Dehiscence During Initiation of Spinal.1Siva SankarNo ratings yet
- Tranexa Topical IVDocument5 pagesTranexa Topical IVSiva SankarNo ratings yet
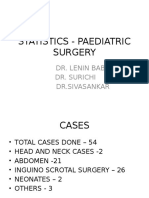
- Statistics - Paediatric SurgeryDocument9 pagesStatistics - Paediatric SurgerySiva SankarNo ratings yet
- Ot 1 &2 Total Time Jan 2014Document6 pagesOt 1 &2 Total Time Jan 2014Siva SankarNo ratings yet
- Bank StatementDocument3 pagesBank Statementsaravanan_sfp100% (1)
- Death SummaryDocument3 pagesDeath SummarySiva SankarNo ratings yet
- AllotemntResultMedical PDFDocument170 pagesAllotemntResultMedical PDFShoyeb KhanNo ratings yet
- Log Book JuneDocument10 pagesLog Book JuneSiva SankarNo ratings yet
- Case of Adverse Cardiac EventDocument17 pagesCase of Adverse Cardiac EventSiva SankarNo ratings yet
- Statistics - Paediatric SurgeryDocument9 pagesStatistics - Paediatric SurgerySiva SankarNo ratings yet
- OT1&2time-ASA, Surgery Stat FormDocument1 pageOT1&2time-ASA, Surgery Stat FormSiva SankarNo ratings yet
- Blind Chinese SoldiersDocument2 pagesBlind Chinese SoldiersSampolNo ratings yet
- Synthesis - Mind Rubrics: Moderator Dr.P.Satyaveni M.D.Homoeo Dept of RepertoryDocument79 pagesSynthesis - Mind Rubrics: Moderator Dr.P.Satyaveni M.D.Homoeo Dept of RepertorySharika BachuNo ratings yet
- Educational Psychology EDU-202 Spring - 2022 Dr. Fouad Yehya: Fyehya@aust - Edu.lbDocument31 pagesEducational Psychology EDU-202 Spring - 2022 Dr. Fouad Yehya: Fyehya@aust - Edu.lbLayla Al KhatibNo ratings yet
- Future Dusk Portfolio by SlidesgoDocument40 pagesFuture Dusk Portfolio by SlidesgoNATALIA ALSINA MARTINNo ratings yet
- Overpressure Prediction From PS Seismic DataDocument10 pagesOverpressure Prediction From PS Seismic DataSevinj HumbatovaNo ratings yet
- Erotic Massage MasteryDocument61 pagesErotic Massage MasteryChristian Omar Marroquin75% (4)
- Never Can Say Goodbye Katherine JacksonDocument73 pagesNever Can Say Goodbye Katherine Jacksonalina28sept100% (5)
- The Saving Cross of The Suffering Christ: Benjamin R. WilsonDocument228 pagesThe Saving Cross of The Suffering Christ: Benjamin R. WilsonTri YaniNo ratings yet
- Ponty Maurice (1942,1968) Structure of BehaviorDocument131 pagesPonty Maurice (1942,1968) Structure of BehaviorSnorkel7No ratings yet
- Meditation On God's WordDocument26 pagesMeditation On God's WordBeghin BoseNo ratings yet
- PREETI and RahulDocument22 pagesPREETI and Rahulnitinkhandelwal2911No ratings yet
- CPARDocument9 pagesCPARPearl Richmond LayugNo ratings yet
- History RizalDocument6 pagesHistory RizalIrvin LevieNo ratings yet
- Chapter 7: Identifying and Understanding ConsumersDocument3 pagesChapter 7: Identifying and Understanding ConsumersDyla RafarNo ratings yet
- TSH TestDocument5 pagesTSH TestdenalynNo ratings yet
- EntropyDocument38 pagesEntropyPreshanth_Jaga_2224No ratings yet
- Abcs Booklet Kidney-Stones PDFDocument20 pagesAbcs Booklet Kidney-Stones PDFDendhy Dwi Handana SagitaNo ratings yet
- Upload Emp Photo ConfigDocument14 pagesUpload Emp Photo Configpaulantony143No ratings yet
- Urban Design ToolsDocument24 pagesUrban Design Toolstanie75% (8)
- Pemahaman Sastra Mahasiswa Bahasa Dan Sastra Arab UIN Imam Bonjol Padang: Perspektif Ilmu SastraDocument31 pagesPemahaman Sastra Mahasiswa Bahasa Dan Sastra Arab UIN Imam Bonjol Padang: Perspektif Ilmu Sastrailham nashrullahNo ratings yet
- Chapter 2Document14 pagesChapter 2Um E AbdulSaboorNo ratings yet
- Final For Influence of OJTDocument39 pagesFinal For Influence of OJTAnthony B. AnocheNo ratings yet
- ElectionDocument127 pagesElectionRaviKumar50% (2)
- LESSON 6 Perfect TensesDocument4 pagesLESSON 6 Perfect TensesAULINO JÚLIONo ratings yet
- Catalyst 3750 Series Switches TroubleshootDocument19 pagesCatalyst 3750 Series Switches TroubleshootSugumar DuraisamyNo ratings yet
- Suicide Prevention BrochureDocument2 pagesSuicide Prevention Brochureapi-288157545No ratings yet
- Tutorial Getting Started With Code Aster PDFDocument12 pagesTutorial Getting Started With Code Aster PDFEnriqueNo ratings yet
- Models of CommunicationDocument20 pagesModels of CommunicationTrisha Ray60% (5)
- Quality of Life After Functional Endoscopic Sinus Surgery in Patients With Chronic RhinosinusitisDocument15 pagesQuality of Life After Functional Endoscopic Sinus Surgery in Patients With Chronic RhinosinusitisNarendraNo ratings yet
- Description of Medical Specialties Residents With High Levels of Workplace Harassment Psychological Terror in A Reference HospitalDocument16 pagesDescription of Medical Specialties Residents With High Levels of Workplace Harassment Psychological Terror in A Reference HospitalVictor EnriquezNo ratings yet