Professional Documents
Culture Documents
Validação Teste de Marcha
Uploaded by
JohnnatasMikaelLopesCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Validação Teste de Marcha
Uploaded by
JohnnatasMikaelLopesCopyright:
Available Formats
http://dx.doi.org/10.1590/1809-9823.2015.
14163
Brief Communication
Validation of the two minute step test for diagnosis of the functional
capacity of hypertensive elderly persons
Marcello Barbosa Otoni Gonalves Guedes1
Johnnatas Mikael Lopes1
Achilles de Sousa Andrade2
Thais Sousa Rodrigues Guedes3
Jos Marcio Ribeiro4
Luana Caroline de Assuno Cortez5
Abstract
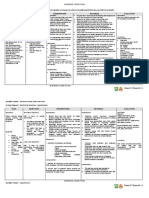
Objectives: To analyze the accuracy of the 2 minute step test in the diagnosis of the normal
functional capacity (FC) of hypertensive elderly individuals or hypertensive elderly
individuals with other associated chronic conditions (ACC). Methods: An observational
diagnosis type study of 101 subjects, 41 of whom were hypertensive and 60 of whom
were normotensive, was carried out. Receiver Operating Characteristic curves (ROC)
were constructed based on the normal FC variable. Results: For hypertensive patients, the
2MST, with an under the ROC curve area of 0.7 (95% CI: 0.50 to 0.87, p = 0.04), proved
to be accurate at diagnosing FC. Among hypertensive individuals with an elevation of
69, sensitivity of 80% and specificity of 54% were observed. The 2MST was accurate at
predicting normal FC among hypertensive patients with ACC, with an under the ROC
curve area of 0.88 (95% CI: 0.69 to 1.00, p= 0.02). With an elevation of 65 the sensitivity
was 83% and the specificity was 67%. Conclusions: The 2MST revealed good sensitivity and
specificity when assessing the FC of elderly hypertensive individuals and elderly hypertensive
patients with ACC, which was not the case among normotensive elderly persons.
Universidade Federal do Rio Grande do Norte, Departamento de Sade Coletiva, Programa de Psgraduao em Sade Coletiva. Natal, RN, Brasil.
2
Universidade Federal do Rio Grande do Norte, Faculdade de Cincias da Sade do Trairi, Santa Cruz,
RN, Brasil.
3
Faculdade Maurcio de Nassau, Curso de Fisioterapia. Natal, RN, Brasil.
4
Faculdade de Cincias Mdicas de Minas Gerais, Curso de Medicina. Belo Horizonte, MG, Brasil.
5
Universidade Federal do Rio Grande do Norte, Faculdade de Cincias da Sade do Trairi, Curso de
Fisioterapia. Santa Cruz, RN, Brasil.
1
Correspondence
Marcello Barbosa Otoni Gonalves Guedes
E-mail: marcelloguedes21@hotmail.com
921
Key words: Validation
Studies; Elderly;
Hipertension.
922
Rev. Bras. Geriatr. Gerontol., Rio de Janeiro, 2015; 18(4):921-926
INTRODUCTION
The data generated by assessments of functional
capacity (FC) improve our understanding of the
profile of elderly individuals, with a view to
delaying or preventing disabilities.1 Activities of
daily living (ADLs), instrumental activities of daily
living (IADL) and functional mobility (FM) are the
most frequently used measurements to assess the
functional capacity of an individual.2 However, the
assessment of FC using practical tests of functional
performance provides only a basic analysis of FM,
creating a need for studies that validate these
practical tests with different instruments that also
assess other aspects, including ADLs.
In this context, there is a correlation between
chronic diseases, particularly systemic hypertension
(SH), and functional capacity (FC). High blood
pressure, as well as its associated chronic conditions,
can lead to low levels of FC and have a direct effect
on the quality of life of elderly individuals.3-5
Validated and easy-to-apply instruments are
important when assessing elderly individuals, either
in research projects or in the daily clinical practice
of health professionals. Significantly, they also
reduce the information and memory bias that is
inherent to many questionnaires.
The two-minute step test (2MST) involves
advantages related to the practicality and speed of
its application, as well as its easy reproducibility and
the small space required to perform the test. The
2MST can be used instead of other performance
tests that are more difficult to apply, including
the timed up and go test or the 6-minute walk
test.6 Until now, studies that address the validation
of the 2MST for the Brazilian population have
been scarce,6,7 particularly for hypertensive elderly
individuals with associated chronic conditions
(a sedentary lifestyle, an elevated BMI or other
chronic diseases).
Therefore, the aim of the present study was to
analyze the accuracy of the 2MST when diagnosing
normal FC among normotensive elderly individuals,
hypertensive elderly individuals with no associated
chronic conditions and hypertensive elderly
individuals with associated chronic conditions.
METHODS
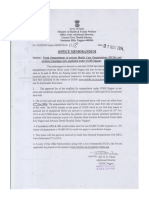
The present study is part of the project Blood
pressure and functional capacity in the elderly
and was approved by the relevant Research Ethics
Committee under protocol number 010/2011. It
deals with diagnostic validity and has a crosssectional design. The sample (106 elderly
individuals) was non-probabilistic and was selected
based on convenience. All of the participants
signed a free and informed consent form.
The assessments were carried out between
January and March 2011. The volunteers were
approached while waiting to be seen in a medical
center or during random visits to their homes
in Belo Horizonte. The visits were conducted
in residential buildings in a neighborhood in
the center of the city. The presence of elderly
individuals in the building was determined,
followed by their interest in participating in the
research. The household sample was significant in
terms of reducing the possibility of selection bias.
Based on the application of the inclusion and
exclusion criteria, 101 subjects participated fully
in the study, during which the following variables
were analyzed: blood pressure (BP); the 2MST; the
Katz index; the practice of physical activity; the
presence of other chronic diseases and the BMI. In
total, there were 41 hypertensive individuals (blood
pressure > 139/89mmHg) and 60 normotensive
individuals (blood pressure < 140/90mmHg). A
casual measurement parameter was adopted.8 The
main inclusion criteria were as follows: appropriate
Validation of two minute step test
age; able to perform the proposed tests without
great risks; able to understand the questionnaires.
The main exclusion criteria were as follows: a
high risk of falls and a lack of collaboration in
relation to the questionnaires. All of the criteria
are listed below:
Inclusion criteria: aged 60 years or more;
no cardiovascular diseases that would limit the
performance of the proposed tests; no respiratory
diseases that would limit the performance of
the proposed tests; no clinical diagnosis of
neurological diseases that could affect the
cognitive levels of individuals. Exclusion criteria:
significant vestibular disorders that could lead
to a risk of falls; a high potential risk of falls
(history of three or more falls in the previous
year, leading to fractures); not responding to all
of the proposed questions.
Research instruments: (a) the two-minute step
test (2MST) to measure the number of elevations,
one knee was chosen as a reference. The maximum
number of elevations of the knee that the individual
could perform in two minutes was recorded. When
a signal was given, the participant began the minute
step (without running). The minimum height of
the knee was set at a mean point between the
patella and the anterosuperior iliac spine,7,9 (b) the
Kats Index for ADLs the Katz index has been
validated, perfected and transculturally adapted for
Brazilian Portuguese. This questionnaire consists
of six questions that assess independence in the
performance of different activities of daily living
and as such, it is more than just a simple assessment
of mobility as the only criteria of functional
capacity. The score is based on the sum of all
positive responses for independence, where a score
of 0 indicates complete independence and a score
of 6 points indicates complete dependence during
ADLs.10,11 In the present study, a score above zero
was considered a functional disability.
Statistical analysis: the data was analyzed
descriptively using mean and standard deviation
values for the continuous variables and percentage
values for categorical variables. In order to
establish the validity of the minute step test in
relation to the Katz index, Receiver Operating
Characteristic (ROC) curves were created, using
functional capacity as a state variable. The validity
was estimated by stratifying normotensive and
hypertensive individuals, considering physical
activity, the body mass index and the presence of
chronic conditions associated with hypertension.
The level of significance was set at 5% to minimize
type I errors. Version 20.0 of SPSS software
(IBM) was used.
RESULTS AND DISCUSSION
The age of the individuals in the sample ranged
from 60 to 89 years, with a mean age of 69.80
(SD 7.55). Of these, 73 (72.3%) were women.
Hypertension was confirmed in 41 (40.6%) of the
individuals, while 54 (53.5%) were overweight/
obese and 64 (63.4%) suffered from another
associated chronic disease. Overweight/obese
individuals were slightly more common among
those with hypertension (63.4%). In total, 82.9% of
the hypertensive participants were sedentary and of
these, 65.9% suffered from an associated chronic
condition. The results of the 2MST were better
among normotensive participants (mean=88.68,
SD 24.63) than among hypertensive participants
(mean= 78.41, SD25.78).
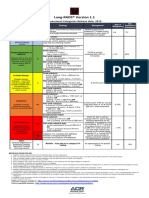
Concerning the accuracy of the 2MST in terms
of diagnosing normal FC, it was found that the
area under the ROC curve was 0.61 (CI95:0.42 to
0.75; p=0.12) for normotensive individuals, which
did not enable us to distinguish (beyond chance)
individuals with functional disabilities (Figure
1A). Conversely, among the hypertensive elderly
individuals, the minute step test confirmed an area
923
924
Rev. Bras. Geriatr. Gerontol., Rio de Janeiro, 2015; 18(4):921-926
under the ROC curve of 0.7 (CI95%:0.50 to 0.87;
p=0.04), thereby demonstrating validity in terms
of diagnosing FC (Figure 1B).
For hypertensive elderly individuals, it was
found that 69 elevations was an excellent cutoff
point when seeking to identify normal functional
capacity, providing a sensitivity value of 80% (0.80)
and a specificity value of 54% (0.46). If a lower
cutoff point was used, the diagnostic test would be
more sensitive and ideal for tracking. The opposite
is also true for specificity, in that a higher cutoff
point would make the test more specific.
Considering other factors such as AF, high
BMI and associated chronic diseases, Figure 1C
shows that the 2MST did not provide an accurate
diagnosis of normal FC among normotensive
individuals (area=0.59; CI95: 0.30 to 0.87; p=0.52).
Conversely, among hypertensive elderly individuals
with associated chronic conditions, the validity of
the 2MST, in terms of predicting normal FC, was
confirmed, given that the area under the ROC
curve was 0.88 (CI95%: 0.69 to 1.00; p=0.02),
(Figure 1D).
Between the cutoff points for the diagnosis of
normal FC among hypertensive individuals with
associated chronic conditions, the ideal cutoff point
would be 65 elevations, which provides a sensitivity
value of 83% and a specificity rate of 67%. In cases
of more sensitive assessments, a lower quantity
of elevations should be used, whereas a greater
quantity of elevations should be used when seeking
more specificity.
During treatment or rehabilitation, flaws in
the functional assessment process used for elderly
individuals are common. The functional level may
be underestimated by certain health professionals,
while others can overestimate functionality, and
some may even forget to assess these levels entirely.
Accurate tests can reduce malpractice during the
assessment process.12
When seeking to diagnose a functional disability,
the ideal scenario would involve the selection of a
cutoff point with high sensitivity, which we were
able to do among hypertensive individuals and
hypertensive individuals with associated chronic
conditions. When seeking to confirm a diagnosis,
the ideal scenario would involve the selection of
a cutoff point with high specificity. In this case,
only the group of hypertensive individuals with
associated chronic conditions exhibited satisfactory
specificity for the suggested cutoffs.12 Therefore,
the selection of the most appropriate cutoff point
for the criteria of the clinical assessment will
depend on the profile of the individual and the
objective of the examiner.
Arterial hypertension can have a negative effect
on the functional disability of elderly indivisuals.3-5,13
Thus, effectively tracking hypertension among the
individuals affected could enable an earlier and
more specific intervention.
Validation of two minute step test
Legend: A ROC* curve for normotensive individuals (dotted); B ROC curve for hypertensive individuals (dashed); C ROC for normotensive,
sedentary, overweight/obese individuals with associated chronic diseases; D ROC curve for hypertensive, sedentary, overweight/obese
individuals with associated chronic diseases. *ROC (Receiver Operating Characteristic).
Figure 1. Validity of the minute step test to diagnose functional capacity using the Katz Index as the
standard of comparison. Belo Horizonte, 2011.
925
926
Rev. Bras. Geriatr. Gerontol., Rio de Janeiro, 2015; 18(4):921-926
CONCLUSIONS
The 2MST exhibited satisfactory sensitivity
and moderate specificity in the assessments of
hypertensive elderly individuals, particularly those
with associated chronic conditions, a sedentary
lifestyle or a high BMI. The cutoff point for this
group was 65 elevations. In the hypertensive
group, the test only demonstrated a satisfactory
sensitivity and specificity when the cutoff point
was 69 elevations. The diagnostic validity of
the 2MST was not confirmed for normotensive
elderly individuals.
Therefore, the 2MST seems to be a valid, fast
and inexpensive method of diagnosing functional
disabilities in hypertensive elderly individuals. The
results are more accurate when the hypertension
is accompanied by comorbidities, which is more
common in the current population. The 2MST
is ideal for clinical outpatient and primary health
care contexts.
REFERENCES
1. Fiedler MM, Peres KG. Capacidade funcional e
fatores associados em idosos do Sul do Brasil: um
estudo de base populacional. Cad Sade Pblica
2008;24(2):409-15.
7. Robortella CN, Rocha SM, Wildner WR, Gorgatti
MG. Reprodutibilidade de uma bateria de testes de
atividade de vida diria para indivduos idosos com
deficincia visual. Rev Bras Cinc Mov 2008;16(4):1-21.
2. Paixo CM Jnior, Reicheenheim EM. Uma reviso
sobre instrumentos de avaliao do estado funcional
do idoso. Cad Sade Pblica 2005;21(1):7-19.
8. Sociedade Brasileira de Cardiologia. 6 Diretrizes
Brasileiras de Hipertenso Arterial. Rev Bras
Hipertens 2010;17(1):4.
3. Ramos RA, Guimares FS, Cordovil I, De S
Ferreira A. The six-minute walk distance is a marker
of hemodynamic-related functional capacity in
hypertension: a case-control study. Hypertens Res
2014;37(3):746-52.
9. Rikli RE, Jones CJ. Development and validation of a
functional fitness test for community residing older
adults. J Aging Phys Act 1999;7:129-61.
4. Zattar LC, Boing AF, Giehl MWC, Dorsi E.
Prevalncia e fatores associados presso arterial
elevada, seu conhecimento e tratamento em idosos no
sul do Brasil. Cad Sade Pblica 2013;29(3):507-21.
5. Hajjar I, Lackland DT, Cupples LA, Lipsitz LA. The
association between concurrent and remote blood
pressure and disability in older adults. Hypertension
2008;50(6):1026-32.
6. Pedrosa R, Holanda G. Correlao entre os testes da
caminhada, marcha estacionria e tug em hipertensas
idosas. Rev Bras Fisioter 2009;13(3):252-6.
Received: July 01, 2014
Revised: February 27, 2015
Accepted: April 14, 2015
10. Katz S, Ford AB, Moskowitz RW, Jackson BA,
Jaffe MW. Studies of illness in the aged. The index
of ADL: a standardized measure of biological and
psychosocial function. JAMA 1963; 12:914-9.
11. Lino VTS, Pereira SEM, Camacho LAB, Ribeiro ST
Filho, Buksman S. Adaptao transcultural da Escala
de Independncia em Atividades da Vida Diria
(Escala de Katz). Cad Sade Pblica 2008; 24(1):103-12.
12. Medronho RA, Perez MA. Testes diagnsticos. In:
Medronho RA, Carvalho DM, editores. Epidemiologia.
2 ed. So Paulo: Atheneu; 2009. p. 389-402.
13. Guedes MBOG, Guedes TSR, Ribeiro JM.
Correlao entre hipertenso arterial e capacidade
funcional de idosos: uma reviso da literatura. Rev
APS 2013;6(4):455-9.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Definition of NephrolithiasisDocument30 pagesDefinition of Nephrolithiasiszz_13No ratings yet
- Lesson 1Document20 pagesLesson 1Irish Jean AgsawayNo ratings yet
- Cardiology Case 1Document2 pagesCardiology Case 1vil62650% (2)
- Significance of Facebow Transfer: January 2020Document6 pagesSignificance of Facebow Transfer: January 2020Mahmoud Ibrahem maanNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument4 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsNovanza RayhanNo ratings yet
- Mini-implant molar intrusion caseDocument1 pageMini-implant molar intrusion caseVesna AndreevskaNo ratings yet
- Lung RADS® Version 1.1: Assessment Categories Release Date: 2019Document1 pageLung RADS® Version 1.1: Assessment Categories Release Date: 2019S Francisco MotNo ratings yet
- Acute Kidney Injury W/ Hyperkalemia NCPDocument5 pagesAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNo ratings yet
- Lesson 3 ReviewDocument4 pagesLesson 3 ReviewHo Yong WaiNo ratings yet
- Anterior Cruciate Ligament InjuryDocument3 pagesAnterior Cruciate Ligament InjuryAdrian Nazario PragachaNo ratings yet
- Jomi 7657Document27 pagesJomi 7657casto.carpetasmiaNo ratings yet
- Expression of MDM2 and p16 in AngiomyolipomaDocument7 pagesExpression of MDM2 and p16 in AngiomyolipomaTiago TavaresNo ratings yet
- Infectiile Grave Extensive Ale Partilor MoiDocument49 pagesInfectiile Grave Extensive Ale Partilor MoiLoredana BoghezNo ratings yet
- HomeostasisDocument12 pagesHomeostasisTimothy StanleyNo ratings yet
- Ligibel JA Et Al. 2022 Exercise, Diet and Weight Management During Cancer Treatment - ASCO GuidelineDocument20 pagesLigibel JA Et Al. 2022 Exercise, Diet and Weight Management During Cancer Treatment - ASCO GuidelineJasmyn KimNo ratings yet
- Askep CKD Bhs InggrisDocument15 pagesAskep CKD Bhs InggrisFitri MulyaNo ratings yet
- Important Classifications PDFDocument42 pagesImportant Classifications PDF330 Himank MehtaNo ratings yet
- Anticestodal Drugs for Tapeworm TreatmentDocument3 pagesAnticestodal Drugs for Tapeworm TreatmentAbiHa YousaufNo ratings yet
- Health and IllnessDocument2 pagesHealth and IllnessLize Decotelli HubnerNo ratings yet
- Asthma Attack Nursing Care Plan for Married Female PatientDocument5 pagesAsthma Attack Nursing Care Plan for Married Female PatientMarivic Yuson MalagarNo ratings yet
- Prostaglandins: An Overview of Structure and FunctionDocument33 pagesProstaglandins: An Overview of Structure and FunctionMuhammad JamalNo ratings yet
- List of Empanelled Hospitals in CGHS NagpurDocument58 pagesList of Empanelled Hospitals in CGHS NagpurRajatNo ratings yet
- History of HIVDocument4 pagesHistory of HIVHyrum KamandeNo ratings yet
- US Elsevier Health Bookshop - Mosby, Saunders, Netter & MoreDocument4 pagesUS Elsevier Health Bookshop - Mosby, Saunders, Netter & MoreWilmer Zambrano GuerreroNo ratings yet
- Oral Health During Pregnancy - An Analysis of Information CoDocument8 pagesOral Health During Pregnancy - An Analysis of Information CoElena IancuNo ratings yet
- Role of Autologous Platelet-Rich Plasma in Z-PlastyDocument3 pagesRole of Autologous Platelet-Rich Plasma in Z-PlastyasclepiuspdfsNo ratings yet
- Foot reflexology chart shows how hand acupressure points relate to body partsDocument3 pagesFoot reflexology chart shows how hand acupressure points relate to body partsgautamlipika100% (2)
- Source Control in Emergency General SurgeryDocument21 pagesSource Control in Emergency General SurgerylaviniaNo ratings yet
- Abnormal PuerperiumDocument65 pagesAbnormal PuerperiumNigus AfessaNo ratings yet
- Dental Public HealthDocument264 pagesDental Public HealthCorina Manole DanielaNo ratings yet