Professional Documents
Culture Documents
11 Status Epilepticus PDF
Uploaded by
ChiciEndahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
11 Status Epilepticus PDF
Uploaded by
ChiciEndahCopyright:
Available Formats
58
SUPPLEMENT TO Journal of the association of physicians of india august 2013 VOL. 61
Status Epilepticus
Ramshekar Menon*, Ashalatha Radhakrishnan**, Kurupath Radhakrishnan***
Abstract
Status epilepticus (SE) is a neurological emergency resulting from prolonged clinical or electroencephalographic
seizure activity. Refractory SE refers to the persistence of seizure activity despite the initiation of first- and secondline anticonvulsant therapy. Sinister outcomes are often attributed to the etiology of SE. Despite randomized
multicentre trials of established and promising therapeutic options, the management and prognostication in SE are
fraught with challenges. Neither the duration of SE nor time-delay to initiation of therapy should discourage the
aggressive approach to the management of SE. Neurointensive care of patients with SE consists of an algorithmic
approach tailored to the etiology and systemic complications that arise as a consequence. This approach is also
driven by the persistence of electrographic seizure activity, which is best followed with continuous EEG monitoring.
The extent of patient support has to be augmentative to the degree of encephalopathy/coma and impairment of
vital functions. Potential interactions of anticonvulsant drugs with other co-medications need to be considered
during the course of treatment. This review discusses the existing literature on the epidemiological aspects, clinical
approach, treatment and prognostication of SE.
Introduction
Convulsive SE
tatus epilepticus (SE) in simple terms is used to describe
a series of uninterrupted seizures which result in an
impairment of normal brain function, which if not treated as a
medical emergency results in high morbidity and mortality.1-3 SE
is one of the most common medical emergencies, with an overall
annual incidence of 10-41 per 100,000.1-6 The incidence of SE has
shown a decreasing trend in both developing and developed
countries over the years. Age-specific incidence rates of SE show
a U-shaped curve with a bimodal distribution peaking in very
young and the elderly.7
Convulsive SE generally refers to the generalized tonicclonic SE which is the most dangerous type of SE. Generalized
convulsive SE classically has been defined as recurrent
generalized convulsions without full and complete recovery
of consciousness between seizures or as a single prolonged
convulsion without the characteristic evolution of a single
discrete seizure.11 The definition of duration of convulsive SE
has been a subject of controversy over the years. Most authors
have suggested a seizure activity lasting 30 minutes for defining
SE. However, for practical purposes, a duration of 5 minutes as
proposed by Lowenstein et al.11 may be better adopted for adults
and children aged above 5 years.
Definition and Classification
The International League against Epilepsy (ILAE) has defined
SE as a seizure that persists for a sufficient length of time, or
repeated frequently enough that recovery between attacks does
not occur.8 However, the definitions and classifications are still
evolving and an ILAE task force is currently developing a new
draft on a definition and classification of SE.9 For the purpose
of this review, we classify SE based on the presence or absence
of motor manifestation into convulsive and non-convulsive
(Figure 1).10 A third category is often recognized comprising the
boundary syndromes including epileptic encephalopathies and
acute forms of coma with status-like electroencephalography
(EEG) patterns.
Fig. 1 : Classification of status epilepticus
Assistant Professor, **Associate Professor, ***Senior Professor,
Department of Neurology, R Madhavan Nayar Center for
Comprehensive Epilepsy Care, Sree Chitra Tirunal Institute for Medical
Sciences and Technology, Trivandrum 695 011.
Non-convulsive SE
Non-convulsive SE is a state of electromechanical dissociation
where the epileptiform discharges evident on the EEG are not
accompanied by clinical manifestations other than obtundation,
hardly discernible motor manifestations or coma. 12 Nonconvulsive SE has long been subdivided into 2 categories:
absence status and complex partial status. Patients with nonconvulsive SE need to be managed as convulsive SE, using EEG
as a guide rather than clinical observations as the determinant
of response to treatment.
Phases of SE
The physiological changes in SE evolve in
two phases: the first is the compensated stage
during which cerebral damage is prevented by
the physiologic mechanisms which compensate
the increased metabolic demands because of
seizures. After 30 to 60 minutes of continuous
seizures, the patient moves into the second or the
decompensated stage when these compensatory
mechanisms are overwhelmed and there is potential
for neuronal injury with persistence of seizures.13
The cerebral damage is caused by systemic and
metabolic disturbances (hypoxia, hypoglycemia, acidosis and
raised intracranial pressure) and also by the direct excitotoxic
effect of seizure discharges, which result in calcium inux
into neurons and a cascade of events resulting in necrosis and
SUPPLEMENT TO Journal of the association of physicians of india august 2013 VOL. 61
59
of the membrane potential.18,19 But once the
SE becomes established, only certain drugs
remain effective especially those inhibiting the
glutamatergic transmission.20 Those acting via
potentiating GABAergic transmission have 20
times reduction in potency after 30 minutes
of seizure activity.21 Basic pathophysiologic
mechanisms which operate during SE are due to
changes at the molecular level mainly involving
protein phosphorylation. The initial changes
occur at the level of the neurotransmitter
receptors and neuronal plasticity which
Fig. 2 : Etiologies of status epilepticus. Abbreviations: CVT- Cortical vein thrombosis;
alter the protein expression. There is also a
SOL - Space occupying lesion; CNS - Central nervous system; MELAS - Mitochondrial
encephalopathy with lactic acidosis and stroke-like episodes; AED - Antiepileptic drugs; receptor trafficking taking place in the form
FIRES - Febrile infection-related epilepsy syndrome
of externalization or internalization of the
receptors.
During
SE, there is decrease in the GABA receptor
apoptosis. Understanding this concept is pertinent to the timing
subunits and increase in the NMDA glutamate receptor
of therapeutic interventions in SE.
subunits on the membrane surface.22 In addition, recent data
have implicated other mechanisms operating at the receptor
Duration
level like acute down-regulation of adenosine A1activity, which
The duration of seizures which qualifies for SE has long been
contributes to ovrexcitation.23 Changes in gene expression come
a subject of debate. New evidences are now coming up based on
to play later and are partly annulled by the inhibition of protein
animal research as well as anecdotal evidence from humans. Data
synthesis. Maladaptive changes occur in protein expression
from animal studies indicated that repetitive seizures become
which may contribute to the self-sustaining nature of the
self-sustaining and pharmacoresistant and can produce neuronal
events There is depletion in hippocampus of the predominantly
14
injury within a period of 15 to 30 minutes.
inhibitory peptides dynorphin, galanin, somatostatin, and
neuropeptide Y, whereas the expression of the proconvulsant
Stages
tachykinins, substance P and neurokinin B is increased. SeizureAs there is time-dependent development of pharmacoresistance
induced neuronal death continues to occur even when motor
and ongoing neuronal injury in SE, it is prudent not to delay the
manifestations are absent due to excitotoxic mechanisms which
treatment till the status becomes established. The concept of
produce cell death.22,23
SE evolving in three sequential stages is useful in deciding the
management strategies.15
Etiology
Impending SE: This is defined as continuous or intermittent
seizures lasting more than 5 minutes without full recovery of
consciousness between the seizures. In the study by Theodore
et al.,16 it was noted that the duration of a single seizure never
exceeded 2 minutes and a cut-off of 5 minutes is 18 standard
deviations from the mean duration. In the Richmond study,
40% of seizures lasting between 10 to 29 minutes were shown
to stop spontaneously without treatment, thereby indicating
that all seizures exceeding the 5 minute mark may not proceed
to established SE, but still pose a high risk for it.17
Established SE: This is defined as clinical or electrographic
seizures lasting more than 30 minutes without full recovery of
consciousness between the episodes. Animal data has proven
that by 30 minutes, the seizures become self-sustaining; produce
distinct seizure-induced neuronal damage and become more
pharmacoresistant.18
Subtle SE: When a generalized convulsive SE is prolonged or
after treatment in an active manner, both the motor as well as
electrographic activity becomes subtle although there is likely
to be continuing neuronal damage warranting an active ongoing
treatment.19
Pathophysiology
In experimental settings, recurrent seizures exhibit the
tendency to become self-sustaining even after the removal of
the epileptogenic stimulus in the mature brain. The available
data leads us to assume that similar mechanisms operate in
human brain. The initial phases of SE can be easily terminated
by drugs which augment inhibition or depress excitation
According to etiology, SE can be classified into: 1) Acute
symptomatic: SE related to an acute medical or neurological
illness; 2) Remote symptomatic: SE owing to conditions resulting
in a static encephalopathy or an antecedent insult such as stroke;
3) Cryptogenic: SE presumed to be symptomatic, but the cause
is unclear; and 4) On the background of an established epilepsy.
The etiologies causing SE is distinctly different in
developing and developed countries, although in both
scenarios acute symptomatic etiology ranks as the major cause
of SE. Cerebrovascular disease is the predominant etiology in
developed countries, whereas in developing countries CNS
infections accounts for the majority, varying between 20-67%
in various studies.24-31 A systematic review by Neligan and
Shorovon showed that the most common underlying causes
were cerebrovascular disease and low antiepileptic drugs (AED)
levels. A relatively good outcome was noted when the etiology
is low AED levels, metabolic conditions and alcohol-related SE,
whereas a worse prognosis was seen when the etiology was acute
symptomatic with cerebrovascular disease or CNS infections
especially in the setting of cerebral anoxia.6 The common
etiologies are enlisted in Figure 2.
In a prospective study from India by Murthy et al31 the
etiology was acute symptomatic in 54%, remote symptomatic
in 7%, and cryptogenic in 19%. In 20% of patients, it was
due to antiepileptic medication non-compliance. Of the
acute symptomatic SE, central nervous system infections
(neurocysticercosis, encephalitis or menigoencephalitis) were
the risk factor in 52% patients.31
60
SUPPLEMENT TO Journal of the association of physicians of india august 2013 VOL. 61
Table 1 : Antiepileptic drugs used in the treatment of status
epilepticus and their doses
Antiepileptic drug
First Line (IV)
Lorazepam
Diazepam
Midazolam
Second Line(IV)
Phenytoin
Fosphenytoin
Third Line (IV)
Levetiracetam
Sodium Valproate
Phenobarbitone (ventilator on
stand-by)
Lacosamide
Fourth Line (cIV)
Midazolam (optional third line
treatment if ventilator
on stanby)
Fig. 3 : Algorithm for management of status epilepticus [Refer to
Table 1 for drug dosing]. Abbreviations: Min - time in minutes;
IV- Intravenous; PHT- Phenytoin; fosPHT - Fosphenytoin; BPBlood pressure; EEG - Electroencephalography; AED - Antiepileptic
drug; BS - Burst suppression on EEG; cIV- Continuous intravenous
infusion therapy
Treatment
Thiopental sodium
The principles of management of recurrent seizures are to
identify and correct reversible causes, maintenance of cerebral
and systemic homeostasis and prompt termination of SE.
Prehospital Management
The studies which have looked into the prehospital
management of SE have shown that rectal diazepam (15-20 mg
as rectal gel) to be useful and safe in both adults and children.
Other drugs which have been tried are intravenous lorazepam
(2 mg) and diazepam (5 mg) which have a relatively good safety
profile. Although these drugs are preferred intravenously if
possible, intramuscular route is also found to be effective in the
prehospital setting.32 However, these should be administered
only by trained paramedical personnel. The other alternatives
which are being used recently are buccal or nasal midazolam.
Propofol
Topiramate (PO)
Dose
0.1mg/kg bolus @ 2mg/min
0.2mg/kg bolus @ 4mg/min
0.05-0.2mg/kg @ 2mg/min
15-20mg/kg @ 50mg/min;
Maintenance= 4-7mg/kg/day (IV/
PO)
15-20mg/kg PE @ 75-150mg/min
Target Phenytoin level= 15-20 g/
ml
20-30 mg/kg bolus over 15
minutes, followed by maintenance
dosing 1500 mg BID (IV/PO)
15-30 mg/kg bolus @ up to 6 mg/
kg/min, followed by maintenance
dosing 500 mg TID(IV/PO)
Target Valproate Level= 50-100
g/ml
20 mg/kg bolus @ 75 mg/min,
followed by initial maintenance
dosing 60 mg TID (IV/PO)
Target Phenobarbitone Level=
20-40 mcg/mL
200mg @50mg/min; 200mg BID
(IV/PO)
Loading: 0.1-0.2 mg/kg (max, 10
mg at a time) Repeat bolus - If
clinical seizures persist 5 min
after initial bolus, then administer
additional bolus of 0.2 mg/
kg bolus & continue infusion.
Repeat bolus every 5 min till total
midazolam bolus dose reaches 2
mg/Kg
Maintenance cIV dose: 0.05-0.4
mg/kg/h
Maximum cIV dose: increase
infusion rate (with each bolus)of
midazolam by 0.05 to 0.1 mg/kg/
hr to a maximum infusion rate of
upto 3 mg/kg/hr).
Loading: 3 to 5 mg/kg at 0.2-0.4
mg/kg/min
Maintenance cIV dose: 3.0 -5.0
mg/kg/h
Maximum cIV dose: 5.0 mg/kg/h
Loading: 1-2 mg/kg at 10 mg/min
Maintenance cIV dose: 2-10 mg/
kg/h
Maximum cIV dose: 15 mg/kg/h
10 mg/kg NG loading dose
followed by 5 mg/kg NG divided
b.i.d. Dose range: 300 mg -1,600
mg.
IV- Intravenous route of administration; cIV- Continuous intravenous
infusion; BID- twice daily; TID- thrice daily; PE Phenytoin equivalent
dose (1.5 times of phenytoin dose); PO- Peroral route; NG- Nasogastric
route of administration
SUPPLEMENT TO Journal of the association of physicians of india august 2013 VOL. 61
General Emergency Measures
The maintenance of airway, breathing and circulation is the
priority in patients presenting with SE. The reversible factors
which should be kept in mind that include hypoglycemia,
hyponatremia, hypocalcemia, hypomagnesemia, acidosis,
hyperthermia and hypoxia. If alcoholism is suspected, patient
should be given a bolus dose of 100 mg thiamine followed by
dextrose infusion. Hypoxia may not be clinically manifest and
oxygen supplementation is recommended in all patients in SE.
Emergency investigations should include the following: blood
gases, glucose, renal and hepatic functions, calcium, magnesium,
full blood count, clotting screen, and AED concentrations. Serum
should be stored for toxicology or virology or other future
analyses. An electrocardiogram should be performed.
Antiepileptic Drug Therapy in SE
All treatment protocols in SE are based on a staged approach
(33,34). The AEDs used in SE can be broadly divided into first
and second line drugs. The detailed protocol of therapy and the
dosages are provided in Figure 3 and Table 1.
First-line drugs
Randomized controlled trials comparing the efficacy of firstline medications in SE are scarce and hence the protocols for
management are heterogeneous. In early SE, the drug of choice
is intravenous benzodiazepines.33 Administration of intravenous
benzodiazepines, lorazepam or diazepam has shown similar
benefits in studies although the safety profile may be slightly
in favor of the former. Intravenous midazolam is also being
increasingly used, but has not been studied in any double-blind
randomized trial.35 Pertinent to the first-line management would
be the issue of respiratory or hemodynamic compromise that
may be incurred during bolus dosing with benzodiazepines
or phenytoin, especially in children and the elderly. Recent
studies including an open labelled randomized study from
India have emphasized equivalence of efficacy and safety of
levetiracetam in comparison to first line AED like lorazepam.36,37
Though cost of therapy is an issue, availability as an intravenous
preparation, favourable pharmacokinetic profile and longer
duration of action of levetiracetam could make it an acceptable
alternative as a first line agent during a cluster of seizures or SE
in a hemodynamically unstable patient.
Second-line drugs
Once the SE is established, intravenous AEDs need to be
administered. The agents available are phenytoin, valproate
and levetiracetam.33 Intravenous fosphenytoin or phenytoin is
generally preferred world-over as first choice if the seizures are
not controlled with benzodiazepines. Fosphenytoin is preferred
over phenytoin due to the favorable side effect profile especially
lack of thrombophlebitis. In a comparative trial of phenytoin,
valproate and levetiracetam, phenytoin was not statistically
different in efficacy from the other two and levetiracetam was
found to be less efficient than valproate to control SE.38
The other parenteral AEDs available recently is lacosamide,
but data on its effectiveness and its comparative efficacy
with other drugs are not available presently.39,40 There are no
head to head comparative prospective trials between them.
A few randomized studies from India with either one or two
of them displayed almost similar efficacy especially between
phenytoin and valproic acid,41,42 although there are no studies
comparing levetiracetam or lacosamide with these agents from
India. Topiramate orally was compared with phenytoin in
61
one randomized trial and was found to be equally effective in
adults.43 Therefore, in the absence of clear rational evidence so
far, an experienced physician can choose pragmatically from
one among them as the clinical situation warrants. They have to
be continued in the oral form once the seizures are controlled.
Refractory SE
There is no single well-accepted definition for refractory SE.
For practical purposes, when adequate doses of two intravenous
anticonvulsants fail to terminate seizures, the status is said to be
refractory. At this stage general anesthetic medications are used
for the control of seizures after intubating the patient.33 With the
use of these agents, majority of SE will get controlled, and hence
the failure of therapy is usually attributable to dose-limiting side
effects or due to an inadequate target dose. Withdrawal seizures
while tapering the drugs are reported in 0.3% to 9% cases.33
The various drugs used in refractory SE are midazolam,
thiopental sodium/pentobarbital and propofol.33,44 Of these,
there is a trend towards more preference for midazolam in
that the control of seizures, lesser rate of withdrawal seizures
and fewer side effects are exhibited by this drug as compared
to the other two.44 Propofol is associated with potentially fatal
propofol infusion syndrome produced by depression of cellular
and mitochondrial functions and is commonly seen in children
and patients co-medicated with catecholamines and steroids.
Thiopentone anesthesia was more commonly associated with
death, which may be a reflection of the severity of the status.
The end point of anesthetic treatment in SE is to achieve burstsuppression pattern in the EEG.
Super-refractory SE
Super-refractory SE is a relatively newer terminology used to
define SE that continues for 24 hours or more after the initiation
of anesthesia, including those cases in which the SE recurs on
the reduction or withdrawal of anesthesia.45 Ketamine infusion
was studied in a small group of patients with super-refractory SE
and 82% achieved satisfactory control. Inhalational anesthetics,
isoflurane and desflurane were also found to be useful for initial
control in small case series.45
Intravenous magnesium has excellent efficacy in the treatment
of seizures due to eclampsia and in congenital or acquired
hypomagnesemia. Serum magnesium level should be done in all
patients with refractory SE. Pyridoxine is effective in SE related
to pyridoxine deficiency. Immunosuppressive regimens like
steroids, intravenous immunoglobulin, and plasma exchange
may are effective as many of the refractory seizures have occult
immunologic causes. Ketogenic diet has effect in SE related
to epileptic encephalopathies. Hypothermia of 32 to 35C,
preferably delivered by endovascular cooling is an effective
measure and affords neuroprotection as well, but one should
be aware of the various systemic complications.45
Neurosurgery has been used in many centers for refractory
SE and is mainly targeted against the etiology of the seizures.
Resection of cortical dysplasia is the most frequently performed
surgery. Magnetic and electrical stimulation therapies like
transcranial magnetic stimulation, vagus nerve stimulation,
deep brain stimulation and electroconvulsive therapy are
experimental forms of treatment used in SE.45
Outcome
Mortality from SE in various studies is up to 20%.1,5,33 Major
determinant of the outcome in SE is the underlying etiology and
62
SUPPLEMENT TO Journal of the association of physicians of india august 2013 VOL. 61
is not related to the type of medications used or duration of SE.31,44
In one study which specifically looked into the duration elapsed
before instituting correct treatment in SE, a duration of less than
10 hours was associated with a better overall outcome, but this
was not significant once etiology, presentation in a comatose state
and type of SE were accounted for.46 In a study on convulsive SE
from India by Murthy et al.,31 the overall mortality was 10.5%,
with lack of response to first-line treatment being a predictor
of mortality (p < 0.001). Also, longer duration of seizures was
associated with increased morbidity (p=0.001).31 These facts
reflect on the importance of emergent treatment of SE by medical/
para-medical staff at the primary health care contact point.
Study of SE in 84 patients from our Institute over a period of
10 years showed the distribution of types of SE as convulsive SE
in 90.7%, non-convulsive SE in 6.5%, and myocloinc SE in 2.8%.
Majority (60%) events were remote symptomatic. Mean delay
between onset of SE and initiation of treatment was 12.8 hours
and only in 11% events, appropriate treatment was started within
1 hour of onset of SE. In 79% of events, SE could be aborted
with use of first- and second-line drugs. Case fatality rate was
11%, 22% developed neurological sequelae and 67% returned
to baseline. Acute symptomatic SE, older age, sensorium at the
time of admission and delayed hospitalization were predictors
of poor outcome.
Conclusions
For the general physician, recognition of SE in both its
convulsive and non-convulsive or subtle forms is of paramount
importance. Prompt initiation of first- and second-line therapy is
critical for management of this devastating condition and early
referral is important when ventilatory care and intravenous
anesthesia are anticipated. The role of emergent EEG cannot be
overemphasized not only in the recognition of non-convulsive SE
but also when continuous intravenous therapy is to be initiated
with midazolam or barbiturates. Diagnosis and management
of the precipitating event are likely to determine the outcome
of SE related to acute symptomatic etiologies. Primary health
care centers should be equipped with basic facilities for the
initial management of SE. With more and more governmental
and nongovernmental ambulance service facilities becoming
available in major cities and towns, pre-hospital treatment of
SE needs emphasis. These measures, hopefully, will improve
the outcome of SE in terms of both the morbidity and mortality
during the coming years.
References
1. DeLorenzo RJ, Hauser WA, Towne AR. A prospective, populationbased epidemiologic study of status epilepticus in Richmond,
Virginia. Neurology 1996;46:102935.
2.
Hesdorffer DC, Logroscino G, Cascino G, Annegers JF, Hauser WA.
Incidence of status epilepticus in Rochester, Minnesota, 19651984.
Neurology 1998;50:73541.
3. Coeytaux A, Jallon P, Galobardes B, Morabia A. Incidence ofstatus
epilepticus in French-speaking Switzerland: EPISTAR. Neurology
2000;55:6937.
4.
Knake S, Rosenow F, Vescovi M, Oertel WH, Mueller HH, WirbatzA,
Katsarou N, Hamer HM, Status Epilepticus Study Group Hessen
(SESGH). Incidence of status epilepticus in adults in Germany: a
prospective, population-based study. Epilepsia 2001;40:75962.
5.
Vignatelli L, Tonon C, DAlessandro R. Bologna Group for theStudy
of Status Epilepticus. Incidence and short-term prognosis of status
epilepticus in adults in Bologna, Italy. Epilepsia 2003;44:9648.
6.
Neligan A, Shorvon S. Frequency and prognosis of convulsive
status epilepticus of different causes: A systematic review. Arch
Neurol 2010;67:931-40.
7.
Chin RF, Neville BG, Peckham C, Bedford H, Wade A, Scott RC.
Incidence, cause, and short-term outcome of convulsive status
epilepticus in childhood: prospective population-based study.
Lancet 2006;368:2229.
8.
Commission on Classification and Terminology of the International
League Against Epilepsy. Proposal for revised clinical and
electroencephalographic classification of epileptic seizures. Epilepsia
1981;22:489501.
9.
Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van
Emde Boas W, Engel J, French J, Glauser TA, Mathern GW,
MosheSL,Nordli D, Plouin P, Scheffer IE. Revised terminology and
concepts for organization of seizures and epilepsies: report of the
ILAE Commission on Classification and Terminology, 20052009.
Epilepsia 2010;51:67685.
10. Trinka E, Hfler J, Zerbs A. Causes of status epilepticus. Epilepsia
2012;53:12738.
11. Lowenstein DH, Bleck T, Macdonald RL. Its time to revise the
definition of status epilepticus. Epilepsia 1999;40:120-2.
12. Husain AM, Horn GJ, Jacobson MP. Non-convulsive status
epilepticus: usefulness of clinical features in selecting patients for
urgent EEG. J Neurol Neurosurg Psychiatry 2003;74:189-91.
13. Shorvon S. The management of status epilepticus. J Neurol Neurosurg
Psychiatry 2001;70(suppl II):227.
14. Mazarati AM, Wasterlain CG, Sankar R, Shin D. Self-sustaining
status epilepticus after brief electrical stimulation of the perforant
path. Brain Res 1998;801:2513.
15. Chen J, Wasterlain C. Status epilepticus: pathophysiology and
management in adults. Lancet Neurol 2006;5:24656.
16. Theodore WH, Porter RJ, Albert P, Kelley K, Bromfield E, Devinsky
O, Sato S: The secondarily generalized tonic-clonic seizure: a
videotape analysis. Neurology 1994;44:1403-7.
17. Delorenzo RJ, Garnett LK, Towne AR, DeLorenzo RJ, Garnett LK,
Towne AR, Waterhouse EJ, Boggs JG, Morton L, Choudhry MA,
Barnes T, Ko D. Comparison of status epilepticus with prolonged
seizure episodes lasting from 10 to 29 minutes. Epilepsia 1999;40:164
9.
18. WasterlainCG, Mazarati AM, Naylor D, Niquet J, Liu H,
Suchomelova L, Baldwin R, Katsumori H, Shirasaka Y, Shin D,
Sankar R. Short-term plasticity of hippocampal neuropeptides
and neuronal circuitry in experimental status epilepticus. Epilepsia
2002;43(suppl 5):209.
19. Treiman DM, Walton NY, Kendrick C. A progressive sequence of
electroencephalographic changes during generalized convulsive
status epilepticus. Epilepsy Res 1990;5:4960.
20. Mazarati AM, Wasterlain CG. N-methyl-D-asparate receptor
antagonists abolish the maintenance phase of self-sustaining status
epilepticus in rat. Neurosci Lett 1999;265:18790.
21. Kapur J, Macdonald RL. Rapid seizure-induced reduction of
benzodiazepine and Zn2+ sensitivity of hippocampal dentate
granule cell GABAA receptors. J Neurosci 1997;17:753240.
22. Naylor DE, Liu H, Wasterlain CG. Trafcking of GABA(A) receptors,
loss of inhibition, and a mechanism for pharmacoresistance in status
epilepticus. J Neurosci 2005;25:772433.
23. Hamil NE, Cock HR, Walker MC. Acute down-regulation of
adenosine A(1) receptor activity in status epilepticus. Epilepsia
2012;53:177-88.
24. Aminoff MJ, Simon RP. Status epilepticus: causes, clinical features
and consequences in 98 patients. Am J Med 1980;69:65966.
25. Lowenstein DH, Alldredge BH. Status epilepticus at an urban
publichospital in the 1980s. Neurology 1993;143:4838.
26. DeLorenzo RJ, Pellock JM, Towne AR, Bogges JG. Epidemiologyof
status epilepticus. J ClinNeurophysiol1995;12:31625.
SUPPLEMENT TO Journal of the association of physicians of india august 2013 VOL. 61
27. Fountain NB. Status epilepticus: risk factors and complications.
Epilepsia 2000;41(Suppl.2):S23S30.
28. Vignatelli L, Tonon C, DAlessandro R. Bologna Group for the Study
of Status Epilepticus. Incidence and short-term prognosis of status
epilepticus in adults in Bologna, Italy. Epilepsia 2003;44:9648.
29. Mhodj I, Nadiaye M, Sene F, Sow PS, Sow HD, Diagana M, Diaye IP,
Diop AG. Treatment of status epilepticus in a developing country.
Neurophysiol Clin 2000;30:1659.
30. Garzon E, Fernandes RM, Sakamoto AC. Analysis of clinical
characteristicand risk factors for mortality in human status
epilepticus. Seizure 2003;12:23745.
31.
Murthy JMK, Jayalaxmi S, Kanikannan M. Convulsive status
epilepticus: clinical prole in a developing country. Epilepsia
2007;48:221723.
63
37. Mctague A, Kneen R, Kumar R, Spinty S, Appleton R. Intravenous
levetiracetam in acute repetitive seizures and status epilepticus in
children: Experience from a childrens hospital. Seizure 2012;21:529534.
38. AlvarzV,Januel J-M, Burnand B, Rossetti AO. Second line status
epilepticus treatment: comparison of phenytoin, valproate and
levetiracetam. Epilepsia 2011;52;1292-6.
39. Hfler J, Unterberger I, Dobesberger J, Kuchukhidze G, Walser G,
Trinka E. Intravenous lacosamide in status epilepticus and seizure
clusters. Epilepsia 2011;52:14852.
40. Trinka E. What is the evidence to use new intravenous AEDs in
status epilepticus? Epilepsia 2011;52(Suppl. 8):358.
41. Misra UK, Kalitha J, Rajesh P. Sodium valproate versus phenytoin
in status epilepticus: a pilot study. Neurology 2006;67:340-2.
32. Silbergleit R, Durkalski V, Lowenstein D, Conwit R, Pancioli A,
PaleschY, Barsan W. Intramuscular versus intravenous therapy for
prehospital status epilepticus. N Engl J Med 2012;366:591600.
42. Agarwal P, Kumar N,Chandra R,Gupta G, Antony A,Garg N.
Randomised study of intravenous valproate and phenytoin in status
epilepticus. Seizure 2007;16;527-32.
33. Shorvon S, Baulac M, Cross H, Trinka E, Walker M. The drug
treatment of status epilepticus in Europe: censensus document from
a workshop at the first London Colloquium on Status Epilepticus.
Epilepsia 2008;49:127785.
43. Synowiec AS, Yandora KA, Yenugadhati V. The efficacy of
topiramatein adult refractory status epilepticus: experience of a
tertiary care center. Epilepsy Res 2012;98:232-7.
34. Cock HR, ESETT Group. Established status epilepticus treatment
trial (ESETT). Epilepsia 2011;52(Suppl. 8):502.
35. Claassen J. Treatment of refractory status epilepticus with
pentobarbital, propofol, or midazolam: a systematic review.
Epilepsia 2002;43:146153.
36. Misra UK, Kalita J, Maurya PK. Levetiracetam versus lorazepam in
status epilepticus: a randomized, open labeled pilot study. J Neurol
2012;259:645-8.
44. Shorvon S, Trinka E. Status epilepticus making progress. Epilepsia
2011;52(Suppl.8):1-2.
45. Shorvon S, Ferlisi M. The treatment of super-refractory status
epilepticus: a critical review of available therapies and a clinical
treatment protocol. Brain 2011;134:280218.
46. Drislane F, Blum A, Lopez M, Gautam S, Schomer D. Duration of
refractory status epilepticus and outcome: Loss of prognostic utility
after several hours. Epilepsia 2009;50:1566-71.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Gastric Ulcer Nursing CareDocument6 pagesGastric Ulcer Nursing CareAesthea BondadNo ratings yet
- The Stages of Adlerian TherapyDocument3 pagesThe Stages of Adlerian TherapyRirika MomobamiNo ratings yet
- The Ashtavaidya Medical Tradition of KeralaDocument5 pagesThe Ashtavaidya Medical Tradition of Keralahari haraNo ratings yet
- Aapm TG 66Document31 pagesAapm TG 66Anjiharts100% (2)
- Extinction Operant Conditioning PDFDocument2 pagesExtinction Operant Conditioning PDFNateNo ratings yet
- Axillary Clearance in MRMDocument58 pagesAxillary Clearance in MRMGanesh VlNo ratings yet
- Cancer Perspective and Molecular BasisDocument36 pagesCancer Perspective and Molecular BasisPRAGAATHYRAJANNo ratings yet
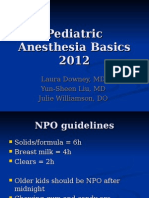
- Pediatric Anesthesia BasicsDocument24 pagesPediatric Anesthesia Basicsvani_kalai005No ratings yet
- Gestalt TherapyDocument6 pagesGestalt TherapyLily lyka PranillaNo ratings yet
- Doctors & DietDocument19 pagesDoctors & Dietrufus_400143616No ratings yet
- Model Curriculum Handbook RadiotDocument157 pagesModel Curriculum Handbook RadiotYuda FhunkshyangNo ratings yet
- Tranquil Eyes Kit User ManualDocument27 pagesTranquil Eyes Kit User ManualJj TreyNo ratings yet
- A Case of Tramadol Dependence and Successful Treatment With Buprenorphine/naloxoneDocument3 pagesA Case of Tramadol Dependence and Successful Treatment With Buprenorphine/naloxoneAdichita Khaira RidatasatriaNo ratings yet
- Attachment and InterventionDocument13 pagesAttachment and InterventioneducacionchileNo ratings yet
- SituationDocument32 pagesSituationEnzoyessaBilly ManauisNo ratings yet
- Oral Health IndicesDocument105 pagesOral Health IndicesTeerawat OffNo ratings yet
- What Are Anxiety Disorder/depression?Document4 pagesWhat Are Anxiety Disorder/depression?Joanna Mæ Nuñez SaysønNo ratings yet
- Rober, ListeningDocument11 pagesRober, ListeningMatias RiosNo ratings yet
- From A Pathologist's DeskDocument33 pagesFrom A Pathologist's DeskDr Suvarna NalapatNo ratings yet
- TAT Counselling techniquesDocument5 pagesTAT Counselling techniquesdhyandevNo ratings yet
- Cabg Case Study FormDocument9 pagesCabg Case Study FormVlad ConstantinNo ratings yet
- 7 Simple Yoga Stretches To Soothe Sciatica Back Pai1Document31 pages7 Simple Yoga Stretches To Soothe Sciatica Back Pai1Nemanja Peric100% (1)
- Synthesis Project Group Final-FallsDocument18 pagesSynthesis Project Group Final-Fallsapi-290381420No ratings yet
- Mindfulness Meditation for Short-Term PsychotherapyDocument11 pagesMindfulness Meditation for Short-Term PsychotherapyKy LyNo ratings yet
- Clinical Case PresentationDocument25 pagesClinical Case Presentationapi-246186340No ratings yet
- Current Concepts of Plyometric ExerciseDocument27 pagesCurrent Concepts of Plyometric ExerciseMustafid Alwi AlvaroNo ratings yet
- CDC guidelines for treating syphilisDocument27 pagesCDC guidelines for treating syphilisGabrielaGushikenNo ratings yet
- Bioscalar Energy: The Healing PowerDocument4 pagesBioscalar Energy: The Healing PowerSagarsinh RathodNo ratings yet
- Bronchitis: Kelompok IDocument14 pagesBronchitis: Kelompok ILinda Permata Sari100% (1)
- Paediatric Cleaning Toys Games and Play Equipment On The Paediatric WardDocument8 pagesPaediatric Cleaning Toys Games and Play Equipment On The Paediatric WarddidikNo ratings yet