Professional Documents
Culture Documents
Hedlund2016 PDF
Uploaded by
Daniel Lago BorgesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hedlund2016 PDF
Uploaded by
Daniel Lago BorgesCopyright:
Available Formats
Physiotherapy Theory and Practice
An International Journal of Physiotherapy
ISSN: 0959-3985 (Print) 1532-5040 (Online) Journal homepage: http://www.tandfonline.com/loi/iptp20
Assessing movement quality in persons with
severe mental illness Reliability and validity of
the Body Awareness Scale Movement Quality and
Experience
Lena Hedlund RPT, PhD, Amanda Lundvik Gyllensten RPT, PhD, Tomas
Waldegren RPT, MSc & Lars Hansson PhD
To cite this article: Lena Hedlund RPT, PhD, Amanda Lundvik Gyllensten RPT, PhD, Tomas
Waldegren RPT, MSc & Lars Hansson PhD (2016): Assessing movement quality in persons with
severe mental illness Reliability and validity of the Body Awareness Scale Movement Quality
and Experience, Physiotherapy Theory and Practice, DOI: 10.3109/09593985.2015.1138008
To link to this article: http://dx.doi.org/10.3109/09593985.2015.1138008
Published online: 06 Apr 2016.
Submit your article to this journal
Article views: 29
View related articles
View Crossmark data
Full Terms & Conditions of access and use can be found at
http://www.tandfonline.com/action/journalInformation?journalCode=iptp20
Download by: [University of California, San Diego]
Date: 12 April 2016, At: 11:02
PHYSIOTHERAPY THEORY AND PRACTICE
http://dx.doi.org/10.3109/09593985.2015.1138008
DESCRIPTIVE REPORT
Assessing movement quality in persons with severe mental illness Reliability
and validity of the Body Awareness Scale Movement Quality and Experience
Lena Hedlund, RPT, PhDa, Amanda Lundvik Gyllensten, RPT, PhDa, Tomas Waldegren, RPT, MScb,
and Lars Hansson, PhDa
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
Department of Health Sciences, Lund University, Lund, Sweden; bThe Country Hospital of Jnkping, Psychiatric Clinic, Jnkping, Sweden
ABSTRACT
ARTICLE HISTORY
Motor disturbances and disturbed self-recognition are common features that affect mobility in
persons with schizophrenia spectrum disorder and bipolar disorder. Physiotherapists in
Scandinavia assess and treat movement difficulties in persons with severe mental illness. The
Body Awareness Scale Movement Quality and Experience (BAS MQ-E) is a new and shortened
version of the commonly used Body Awareness Scale-Health (BAS-H). The purpose of this study
was to investigate the inter-rater reliability and the concurrent validity of BAS MQ-E in persons
with severe mental illness. The concurrent validity was examined by investigating the relationships between neurological soft signs, alexithymia, fatigue, anxiety, and mastery. Sixty-two
persons with severe mental illness participated in the study. The results showed a satisfactory
inter-rater reliability (n = 53) and a concurrent validity (n = 62) with neurological soft signs,
especially cognitive and perceptual based signs. There was also a concurrent validity linked to
physical fatigue and aspects of alexithymia. The scores of BAS MQ-E were in general higher for
persons with schizophrenia compared to persons with other diagnoses within the schizophrenia
spectrum disorders and bipolar disorder. The clinical implications are presented in the discussion.
Received 14 May 2014
Revised 20 July 2015
Accepted 24 July 2015
Background
Patients with mental illness often suffer from a number
of bodily symptoms and dysfunctions due to this illness. They also have a high level of comorbidity with
metabolic syndrome, which is partly due to physical
inactivity (Gyllensten, Ekdahl, and Hansson, 2009;
Hedlund and Gyllensten, 2013; Probst, Knapen, Poot,
and Vancampfort, 2010). Their motivation to be physically active is generally impaired and it has been
found that autonomous motivation, which includes
the experience of physical activity as something enjoyable, is an important dimension for patients with severe
mental illness (Vancampfort et al, 2013; Vancampfort
et al, 2015). There are several reasons for patients with
severe mental illness to not experience physical activity
as enjoyable; these include positive and negative symptomatology and the occurrence of cognitive dysfunctions that may affect both the ability to perform and to
experience body movements (Morrens, Docx, and
Walther, 2014; Vancampfort et al, 2015). Motor function skills are not only based on a complex interplay
between afferent and efferent neurological activity but
also on more cognitive, psychological, and motivational
aspects (Destoop, Bruijn, Hulstijn, and Sabbe, 2009;
CONTACT Lena Hedlund, RPT, PhD
2016 Taylor & Francis
lena.hedlund@med.lu.se
KEYWORDS
Fatigue; motor disturbance;
neurological soft sign;
physiotherapy;
schizophrenia
Kronholm et al, 2011; Price, Dieckman, and HarmonJones, 2012; Schneider et al, 2014). Physiotherapists in
mental health services meet patients with a number of
different movement difficulties that negatively affect
their movement quality, which could lead to musculoskeletal pain (Hedlund and Gyllensten, 2010; Hedlund
and Gyllensten, 2013; Skjrven, Kristoffersen, and
Gard, 2010; Stubbs et al, 2014a). Movement quality is
a clinical phenomenon consisting of four dimensions
that interact in movement: 1) biomechanical; 2) physiological; 3) psycho-sociocultural; and 4) existential. It
has been defined as the way human movements are
executed with respect to the dimensions of time,
space, and intention. The integration of body awareness
and fluency, complexity, and accuracy of movements
makes movement quality a multi-dimensional phenomenon, used to describe movements in different areas of
physiotherapeutic practice like psychosomatic/psychiatric physiotherapy, physiotherapy with children with
cerebral palsy and physiotherapy in non-specific lowback pain (Boyce et al, 1991; Hodges et al, 2013;
Skjrven, Kristoffersen, and Gard, 2008). Good movement quality depends on adequate body awareness
(Skjrven, Kristoffersen and Gard, 2008), but when
working with movement quality in patients with severe
Department of Health Sciences Lund University, P.O. Box 157, 221 00 Lund, Sweden.
L. HEDLUND ET AL.
mental illness, there are two particular research areas
focusing on movement difficulties that need to be highlighted; motor disturbances (MD) and disturbed selfrecognition.
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
Motor disturbances in patients with severe mental
illness
Interest in motor disturbances (MD) among patients
with schizophrenia and bipolar disorder has increased
during the last two decades due to advances in neurological, neurocognitive, and phenomenological research
(Docx et al, 2012; Gallagher, 2004; Sass and Parnas,
2003; Walther and Strik, 2012). One major problem
in studies of these disturbances is the lack of clear
conceptual boundaries between different types of MD.
The concepts overlap and different MD with stipulated
different origins co-exist. Docx et al. (2012) organized
the main MD into five categories: 1) catatonia; 2)
extrapyramidal signs; 3) psychomotor slowing; 4) negative symptoms; and 5) neurological soft signs. Walther
et al. (2009) organized MD into six categories, also
including involuntary movements and negative syndrome connected to passivity, anhedonia, loss of affective experience, and expression. A more integrative
view on motor symptoms in patients with schizophrenia has recently been published (Morrens, Docx, and
Walther, 2014). Up to 66% of people with a first episode of psychosis, who have never previously been
medicated, have at least one motor sign and up to
80% of long-term ill and medicated patients with schizophrenia have MD (Docx et al, 2012; Walther and
Strik, 2012). People with bipolar disorder also show
an increased frequency of MD, however, in a slightly
different way than patients with schizophrenia (Docx
et al, 2012; Zhao et al, 2013). Most patients do have
more than one type of MD (Docx et al, 2012; Morrens,
Docx, and Walther, 2014; Walther and Strik, 2012).
Earlier studies have shown that medication with neuroleptics is not the dominant cause for MD (Docx et al,
2012; Morrens, Docx, and Walther, 2014; Wolff and
ODriscoll, 1999). It has been proposed that the occurrence of MD at an early age might represent a core
underlying vulnerability for psychosis (Kupper et al,
2010; Mittal et al, 2011) and also that the occurrence
of MD in the prodromal phase of psychosis is an
important predictor of later psychosocial functioning
and an intrinsic feature of the schizophrenic and psychotic process (Mittal et al, 2011; Walther and Strik,
2012). The etiology is still unclear but the research is
now focusing on a neurological interplay in the brain,
which is visible in MD (Walther and Strik, 2012).
Disturbances of simple motor coordination, complex
motor sequences, multi-sensory integration, and disinhibition signs are particularly apparent (Zhao et al,
2014). The latter suggests in a meta-analysis that cerebello-thalamo-prefrontal brainwork might be involved
in schizophrenia and related psychotic disorders. There
is also, however, the possibility that MD has only a
loose connection to the illness and is more associated
with a general lack of neurodevelopment (Morrens,
Docx, and Walther, 2014; Walther and Strik, 2012).
Disturbances in self-recognition
Another type of disturbance that affects the experience
of movement and movement quality is the disturbance
in self-recognition or self-awareness (e.g. experiencing
the body as being occupied by an alien force) (van
Veluw and Chance, 2014; Waters and Badcock, 2010).
These disturbances are mainly experienced and communicated by patients themselves, but experimental
studies have lately shown a deviation in the normal
mechanisms behind self-recognition in patients with
schizophrenia (Ferri et al, 2012; Thakkar, Nichols,
McIntosh, and Park, 2011; van Veluw and Chance,
2014; Waters and Badcock, 2010). Self-recognition is
proposed as being reliant on several mechanisms, basically on body ownership, the perception of body as
ones own and on agency, the perception of willed
action (like volitional body movement) as ones own.
These dimensions emanate from cognitions related to
afferent and efferent loops, bottom-up and top-down
dynamics (the two-way interaction of the nervous system), and the ability for multi-sensory integration and
intentional binding (Critchley, 2009; Postmes et al,
2014; Seth, 2013; Waters and Badcock, 2010). The
body scheme (the perception of body in its spatial
context) is also an important basic component of selfrecognition (Waters and Badcock, 2010). Multi-sensory
integration appears to be of great importance and
related to centering the perception of the body toward
the trunk. Furthermore, Serino et al. (2013) have also
described how a stronger experience of body ownership
increases resistance against experimental provocation
of body ownership. Postmes et al. (2014) described
schizophrenia as a self-disorder due to perceptual incoherence resulting in reduced recognition of the body,
declined authorship, impaired emotion processing, and
impaired source discrimination.
In summary, there are several aspects of disturbances in self-recognition and MD in patients with
severe mental illness that affect movement quality
and need to be addressed in physiotherapeutic treatment. The physiotherapist thus needs to assess movement quality, movement dysfunctions, and body
PHYSIOTHERAPY THEORY AND PRACTICE
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
image prior to treatment (Gyllensten, Ekdahl, and
Hansson, 1999; Gyllensten, Skr, Miller, and Gard,
2010; Maggini and Raballo, 2004b; Priebe and
Rhricht, 2001; Roxendal, 1985). The Body
Awareness Scale (BAS) (Roxendal, 1985) and the
BAS-H (Gyllensten, Ekdahl, and Hansson, 1999)
have been used by physiotherapists to assess movement quality, according to the theories of Basic Body
Awareness Therapy (BBAT). For more information
about BBAT, see Hedlund and Gyllensten (2010). A
shorter version of the BAS has been developed,
mainly for clinical reasons, and needs to be psychometrically tested.
Aim of study
The first aim of the present study was to examine the
inter-rater reliability of the Body Awareness Scale
Movement Quality and Experience (BAS MQ-E)
instrument. The second aim was to explore the concurrent validity of the BAS MQ-E (i.e. how BAS MQ-E
co-varies with other a priori hypothesized important
clinical phenomena: neurological soft signs; fatigue;
mastery; alexithymia; and anxiety, in the targeted
group of patients).
Methods
Study design
This clinical study has a cross-sectional design with a
prospective analysis of relationships employing one
novel and five well-used instruments. Health care professionals at eight outpatient mental health care units
asked 120 patients with schizophrenia spectrum disorders or bipolar disorder to participate in the study.
Patients between 18 and 70 years of age diagnosed
with schizophrenia spectrum disorders (ICD-10: F20
F29) or bipolar disorder (ICD-10: F31) were included
in the study. Patients in need of treatment for addiction
and with pervasive brain damage were excluded. The
period of inclusion lasted for 11 months.
Participants
Ethical approval was obtained from Regional Ethical
Review Board, Lund University, Sweden, dnr 2012/
465. Seventy-one patients gave their written consent
to participate. Five patients did not come for the
appointment and four were not included due to logistical difficulties, resulting in 62 patients in the validity
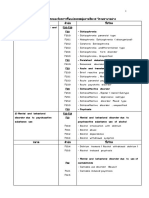
study. Fifty-three of these were included in the interrater reliability study (Figure 1).
120 patients were invited
to participate in the study
48 patients declined
participation
71 patients accepted to
participate and gave their
written consent
5 patients did not show
up at appointment.
4 patients were not
included due to logistical
problems
62 patients were included
in the validity study.
The 53 first
consecutively patients
were included in the
reliability study
Figure 1. Flowchart over study.
Data collection
Three physiotherapists (PTs) with 928 years of work
experience met and tested the patients, two of them
(LH, ALG) worked together in the reliability study
(block 1) and one PT (TW) was responsible for most
of the assessments in the validity study (block 2). The
patients started with either block 1 or block 2 and then
changed to the other. This meant that every other
participant first completed the assessments pertaining
to the validity study and then the assessment in the
reliability study in order to eliminate a systematic
impact of the order of the assessments. Within each
block, the assessments were executed in a standardized
order. In block 1, the physiotherapists changed roles as
test leader and observer for each new participant. All
test leaders had both previous clinical and research
experience of using the assessments in each block.
Assessments
Inter-rater reliability
BAS MQ-E is a development from the BAS and the
BAS-H by Roxendal (Gyllensten, 2001; Gyllensten,
Ekdahl, and Hansson, 1999; Gyllensten, Ekdahl, and
Hansson, 2009; Roxendal, 1985). The assessment consists of three parts: 1) a movement scale where the
physiotherapist moves together with the patient and
gives verbal instructions; 2) a questionnaire about
body experiences, symptoms, and coping strategies;
and 3) a qualitative interview focusing the experiences
of the body and movement in the present. The procedures and scale-steps are described in a manual
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
L. HEDLUND ET AL.
(Gyllensten and Mattsson, 2011). The movement scale
takes about 15 minutes to perform and consists of
movements used in everyday life, including functional
abilities like walking, standing on one leg, stomping,
and stepping up unto a chair. The movement scale
consists of 23 items, rated in a 5-step scale ranging
from 04. A rating of 0 represents good quality in
movements and function indicating that the movements are performed with stability, relaxation and freedom and integrated with the breathing. A rating of 4
represents extreme movement difficulties, indicating
that the person cannot perform the movement. The
BAS MQ-E movement scale captures both assets
(resources) and problems in the persons functional
ability and is structured according to the ICF health
domains: body function/structure; activity; participation; and environmental/personal aspects are all
included in the ratings. The movement scale has been
subjected to factor analysis and three factors have been
identified: 1) stability in function (SF); 2) coordination/
breathing (CB); and 3) relating/awareness (RA)
(Sundn, Ekdahl, Horstman, and Gyllensten, 2014).
The inter-rater reliability and validity of the BAS
MQ-E movement scale for people with Hip osteoarthritis have been found to be adequate (Sundn,
Ekdahl, Horstman, and Gyllensten, 2014). The second
part of the instrument, the questionnaire, consists of
nine questions. Seven of these are assessed quantitatively, a higher score representing a more severe
inconvenience. The final two questions, regarding
faith in recovery and coping strategies, and the qualitative interview are processed and analyzed qualitatively. These qualitative parts of BAS MQ-E are not
included in the present study.
Concurrent validity
Concurrent validity was studied with a set of instruments that are aimed to reflect the aforementioned
hypothesized phenomena. The occurrence of neurological soft signs was assessed by the Neurological
Evaluation Scale, NES-13 (Sanders et al, 1998).
Neurological soft signs are minor neurological abnormalities and identified by clinical examination, referring
to any neurological deviation; motor, sensory, or integrative; and are proposed to be related to the cerebellothalamo-prefrontal brain network (Quitkin, Rifkin, and
Klein, 1976; Zhao et al., 2014). NES-13 is a shortened
version of the original 26-item scale. A three factor
solution is used for analyses in the present study
(Sanders et al, 2005). A substantial relation exists
between factor 1 (repetitive motor) and factor 2 (cognitive/perceptual), while the relation with factor three
(balance) is vague, suggesting that repetitive motor and
cognitive/perceptual factors to some degree assess overlapping constructs (Sanders et al, 2005).
Anxiety was assessed by the State Trait Anxiety
Inventory, STAI (Barnes, Harp, and Jung, 2002),
which consists of two 20-item self-assessments. The
STAI State assesses anxiety as experienced right now
and in general (Spielberger, 1983). STAI has shown
excellent internal consistency and the STAI Trait has
excellent testretest reliability (Spielberger, 1983).
Mastery was assessed by Pearlins mastery scale
(Bengtsson-Tops, 2004; Pearlin and Schooler, 1978).
Mastery concerns the extent to which one regards life
chances as being under control (Pearlin and Schooler,
1978). The instrument has shown satisfactory psychometric properties (Eklund, Erlandsson, and Hagell,
2012) and internal consistency in a Swedish sample of
people with schizophrenia (Bengtsson-Tops, 2004).
Alexithymia refers to difficulties in emotionalizing,
fantasizing, verbalizing, identifying, and analyzing emotions and is assessed by the Toronto Alexithymia Scale
(TAS-20) (Bagby, Parker, and Taylor, 1994). The
Swedish translation by Simonsson-Sarnecki et al.
(2000) has shown good internal consistency. TAS-20
includes four subscales: 1) Deficit in the Identification
of Cenesthesic Sensations (DICS); 2) CommunicativeExpressive Impairment (CEI); 3) Interpersonal
Distance Modulation (IDM); and 4) Adaptive
Acceptance (AA) (Maggini and Raballo, 2004a).
Fatigue was in the present study assessed by
Multidimensional Fatigue Inventory, MFI-20, a selfassessment scale with 20 items developed by Smets,
Garssen, Bonke, and Haes (1995) and translated into
Swedish by Frst and hsberg (2001). It reflects five
dimensions of fatigue: 1) mental fatigue; 2) physical fatigue; 3) general fatigue; 4) reduced motivation; and 5)
reduced activity. A reliability and validity study of MFI20 on patients with schizophrenia and schizophrenia
spectrum disorder showed a satisfactory psychometric
profile (Hedlund, Gyllensten, and Hansson, 2015).
Statistical analysis
A power calculation for the reliability study was performed based on the following hypotheses; anticipating
the inter-rater difference between true agreement and
random agreement to be 0.5, with a relative error of
30%, will result in a necessary sample size of 44 participants. Furthermore, anticipating the drop-out rate to
be 10% will require an initial sample size of 50 participants (Cantor, 1996).
The values of the first writers assessments of BAS
MQ-E were used in all statistical analyses except for the
inter-rater reliability analysis. The statistical analyses
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
PHYSIOTHERAPY THEORY AND PRACTICE
were 2-tailed and used a significance level of p 0.05 (if
not noted otherwise).
The internal consistency of the BAS MQ-E movement
scale was examined by using Cronbachs . An -value of
0.70 was accepted as satisfactory (Bland and Altman,
1997). Weighted kappa was used to evaluate the interrater reliability and scores were grouped according to
Altman into five categories: 1) poor (0.20); 2) fair
(0.210.40); 3) moderate (0.410.60); 4) good (0.61
0.80); and 5) very good (0.811.0) (Bland and Altman,
1997; Gwet, 2012). Spearmans correlations were used to
evaluate the concurrent validity. The distribution of relevant data was checked by analyzing skewness and kurtosis. The results of these analyses showed that it would be
appropriate to use one-way ANOVA in order to investigate differences between diagnostic subgroups. Multiple
linear regressions were further used to analyze the covariation between BAS MQ-E and significant correlations
to the instruments used in the validity analyses. The IBM
SPSS statistical software version 20.0 (IBM Corporation,
Armonk, NY) was used to perform the statistical analyses.
Results
Background characteristics
The characteristics of the included sample are shown in
Table 1. Twenty-seven males and 35 females participated in the study. A majority, 32 people, were according to ICD 10 clinically diagnosed with schizophrenia
(F20.020.9). For each of the other diagnoses (F22, F25,
F29, and F31), there were less than 10 people.
Internal consistency and inter-rater reliability
The internal consistency of each subscale in the
movement assessment of BAS MQ-E showed satisfactory Cronbachs alpha values (stability in function, = 0.82, coordination/breathing, = 0.85,
relating/awareness, = 0.70). The results of the
inter-rater reliability tests showed that fair reliability
was attained six items (0.260.36); moderate reliability eight items (0.450.59); and good reliability
nine items (0.610.73) (Table 2).
Scores on the BAS MQ-E movement scale and NES
The participants scores of the movement assessment
showed that the subscale coordination/breathing had
the highest proportion of participants (77%) attaining
a level of obvious difficulties or worse. Item 11 (centered movement); 14 (turning); and 16 (gait coordination) showed the highest levels of deviation among the
participants. In the subscale stability in function, 40%
of the participants showed obvious to severe difficulties
and in the subscale relating/awareness, 27% showed
obvious to severe difficulties.
Those diagnosed with F 20 had a higher mean value
in all three BAS MQ-E subscales compared to those
diagnosed with F22, F25, F29, and F31. The difference
in mean values (F20, mean 11.5, the others, mean 9.5)
in the subscale relating/awareness was significant (p =
0.01). The mean values for the NES subscales in this
sample were 3.6 for the subscale repetitive motor, 4.2
for the cognitive/perceptual, and 1.6 for balance.
Table 1. Background characteristics of participants (n = 62).
Characteristic
Gender
Male
Female
Primary diagnosis
Schizophrenia F20
Persistent delusional disorders F22
Schizoaffective disorder F25
Unspecified non-organic psychosis F29
Bipolar disorder
Housing
Single
Married/co-habiting
With parents
Other; sheltered accommodation, homeless
Education
Secondary school
Upper secondary school
University
Missing
n (%)
27 (44)
35 (56)
32
9
8
6
7
(51.6)
(14.5)
(12.9)
(9.7)
(11.3)
33
19
6
4
(53.2)
(30.6)
(9.7)
(6.5)
9
29
23
1
(14.5)
(46.8)
(37.1)
(1.6)
Characteristic
Work situation
Regular work
Sheltered employment
Unemployed
Studying
Disability pension
Missing
Medication
Antipsychotic
Antidepressant
Sedative
Mood stabilizer
Sleeping medication
Years in contact with psychiatric care
Mean
SD years
Min-Max
Missing
Age
Mean
SD years
Minmax
n (%)
14
4
10
2
29
3
(22.6)
(6.5)
(16.1)
(3.2)
(46.8)
(4.8)
49
31
21
15
21
(79)
(50)
(33.9)
(24.5)
(33.9)
16.0
11.2
431
1
42.8
10.8
23
66
L. HEDLUND ET AL.
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
Table 2. Inter-rater reliability for each item (n = 53).
BAS MQ-E movement scale, item
Fair reliability
Item 10. Instructed orientation through center
Item 12. Breathing distribution
Item 13. Breathing, integrating
Item 19. Relating mirror
Item 20. Eye contact
Item 21. Handshake
Moderate reliability
Item 1. Stability in standing
Item 5. Shift of bodyweight
Item 7. Sit down, raise
Item 8. Lay down, raise
Item 14. Turning
Item 17. Movement control
Item 18. Motor activity
Item 23. Awareness
Good reliability
Item 2. Stand on a chair
Item 3. Stomp
Item 4. Flexibility in balance
Item 6. Standing on one leg
Item 9. Jump
Item 11. Centered movement
Item 15. Muscular tension
Item 16. Gait coordination
Item 22. Meeting
Weighted
Kappa
0.35
0.34
0.32
0.36
0.26
0.32
0.59
0.48
0.54
0.55
0.58
0.59
0.45
0.49
0.73
0.69
0.63
0.73
0.65
0.66
0.61
0.63
0.64
Concurrent validity, movement scale
There were significant correlations between the BAS MQ-E
subscale stability in function and two NES factors, repetitive motor (0.35); and cognitive/perceptual (0.44), and with
the MFI-20, physical fatigue subscale (0.34) (Table 3). The
BAS MQ-E subscale coordination/breathing showed a significant correlation with NES cognitive/perceptual (0.40)
and MFI-20 physical fatigue (0.27) subscales. BAS MQ-E
subscale relating/awareness showed a significant correlation with the MFI-20 physical fatigue (0.32) subscale. As
shown in Table 3, the different correlations between BAS
MQ-E subscale stability in function and coordination/
breathing were higher when separating the participants in
two groups: 1) participants diagnosed with F20 (n = 32)
and 2) participants with the other four diagnoses, F22, F25,
F29, and F31 (n = 30).
The significant correlations between BAS MQ-E
subscales and MFI-20 disappeared, however, for the
participants with a F20 diagnosis, as well as the
correlation between the BAS MQ-E subscale coordination/breathing and the NES subscale cognitive/
perceptual for participants with other diagnoses,
when the participants were divided into two groups
based on diagnoses.
Concurrent validity, questionnaire
There were significant correlations between the BAS
MQ-E questionnaire and all of the MFI-20 subscales
(0.370.64) (Table 4). The BAS MQ-E questionnaire
also correlated significantly with the two subscales,
Table 3. Spearman correlations between BAS MQ-E movement
subscales, NES subscale repetitive motor, cognitive/perceptual,
and MFI-20 physical fatigues, for total sample (n = 62) and
sample divided into diagnostic subgroups, F 20 n = 32, F 2231
n = 30.
Scale Subscale
BAS MQ-E
Stability in function
BAS MQ-E
NES
Repetitive
motor
0.35**
0.63**
(F 2231)
0.38*
(F 2231)
Coordination/breathing
BAS MQ-E
Relating/awareness
NES Cognitive/
perceptual
0.44**
0.40* (F 20)
0.50**
(F 2231)
0.40**
0.58** (F 20)
MFI-20 Physical
fatigue
0.34**
0.50**
(F 2231)
0.27*
0.52** (F 2231)
0.33*
0.47* (F 2231)
* Correlations are significant at the 0.05 level. ** Correlations are significant
at the 0.01 level.
Table 4. Spearman correlations between BAS MQ-E questionnaire and MFI-20, TAS-20, Mastery, and STAI (n = 62).
Scale
Mastery
MFI-20
TAS-20
STAI
BAS MQ0.37** General F 0.45*
DICS 0.33* State 0.43**
E questionnaire
Physical F 0.64**
Trait 0.45**
Activity F 0.48**
Motivation F 0.37**
Mental F 0.48**
* Correlations are significant at the 0.05 level. ** Correlations are significant
at the 0.01 level.
state anxiety (0.43) and trait anxiety (0.45) of STAI,
as well as with TAS-20, subscale DICS (0.33), and
with Mastery (0.37). Analyses of diagnostic subgroups showed that the correlations with TAS-20,
DICS, STAI, and MFI-20, mental fatigue were no
longer significant for participants diagnosed with
F22, F25, F29, and F31. The correlations with STAI,
both state anxiety (0.54), and trait anxiety (0.74)
remained and were greater for participants with a
F20 diagnosis.
Regression analysis
Regression analysis including the whole sample showed
that the NES cognitive/perceptual subscale accounted
for 18.5% of the variance of BAS MQ-E stability in the
function subscale, and MFI-20, physical fatigue
accounted for a further 9.7% of the variance of BAS
MQ-E stability in function (F = 11.99, p = 0.001). NES
cognitive/perceptual also accounted for 20.7% of the
variance of the BAS MQ-E coordination/breathing subscale (F = 15.69, p = 0.001). The MFI-20, physical
fatigue accounted for 52% of the variance and TAS20, DICS a further 5.3% of the variance (F = 31.97, p =
0.001) in the regression analysis of the BAS MQ-E
questionnaire.
PHYSIOTHERAPY THEORY AND PRACTICE
Discussion
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
Internal consistency and inter-rater reliability
The internal consistency of the BAS MQ-E movement
subscales was satisfactory indicating that the different
subscales are coherent and measure the defined construct. Overall, the inter-rater reliability showed a satisfactory level of agreement. The inter-rater reliability
analysis resulted in 17 items with a moderate or good
level of agreement and six items with a fair level of
agreement. Three of the items with fair agreement
belong to the subscale relating/awareness. The assessment of aspects relating to non-verbal relationship and
non-verbal communication is rather difficult for an
observer not involved in the actual communication
process and standing at a different angle, which might
explain the lower level of inter-rater reliability for this
subscale. When assessing handshake, a more subjectivebased judgment is also involved. The items assessing
breathing are also dependent on the distance between
the observer and the patient, which may explain the
lower level of rater agreement. One item, the orientation through the movement center, is however surprisingly low and needs further investigation.
Scores on the BAS MQ-E movement scale and NES
The results of the present study provide a description of
the difficulties in movement quality for people with
severe mental illness. The number of people with
movement difficulties is not surprisingly high in our
sample compared with earlier studies of MD (Docx
et al, 2012; Walther and Strik, 2012). A high percentage
of people in particular showed severe or pathological
difficulties in the subscale coordination/breathing. The
mean values of all BAS MQ-E subscales were higher for
the F20 subgroup, with a significant difference in the
BAS MQ-E subscale relating/awareness, when the sample was divided into two diagnostic subgroups (F20 and
the others). This is not surprising as negative symptoms
such as passivity and social withdrawal (Kupper et al,
2010) and motor disturbance (Walther et al, 2009;
Walther and Strik, 2012) are more prominent in
patients with schizophrenia. The fact that the subscale
coordination/breathing showed the highest deviances is
in line with the physiotherapists experiences of treating
people with severe mental illness (Hedlund and
Gyllensten, 2013). The trunk is a very complex area
involving many different functions and motor, autonomic and emotional functions are connected to its
central region. Serino et al. (2013) also maintained
that the perceptual importance of the trunk as being
the origin of the implicit multi-sensory integration and
of body image, thus constituting an important foundation for the process of self-recognition. Experiences
connected to emotions and feelings, coordination of
bodily movements, breathing, and autonomous functions such as digestion and sexuality are located here
(Dropsy 1998; Gyllensten, 2001).
Concurrent validity, movement scale
There was a fair to moderate relation between the BAS
MQ-Es subscale stability in function and the NES
subscales repetitive motor and cognitive/perceptual.
There was also a fair to moderate relation between the
BAS MQ-Es subscale coordination/breathing and the
NES subscale cognitive/perceptual. Furthermore, the
regression analysis showed that the cognitive/perceptual subscale accounted for the variance of both stability in function and coordination/breathing. The NES
subscale cognitive/perceptual consists of important
neurological items, including working memory as well
as right-left orientation, audio visual integration and
extinction which are all a part of multi-sensory integration. High scores on the cognitive/perceptual subscale
have also shown to be associated with schizophrenia in
comparison with other forms of psychosis (Chan and
Chen, 2004).
Another moderate relation was between all the subscales of BAS MQ-E and the self-administrated MFI-20,
physical fatigue, which also accounted for 9.7% of the
variance of BAS subscale stability in function. This was
the only significant correlation found between the
movement scale and the different self-administrated
scales: TAS-20; STAI; Mastery; and the MFI-20. Both
mental and physical fatigue often affect the body posture more specifically and alertness in the overall body
movements more generally. One conclusion is thus that
certain aspects of neurological soft signs and experienced physical fatigue or lack of physical vitality influence the performance of voluntary movement in BAS
MQ-E among people with severe mental illness. The
profile of relations for the diagnostic subgroups was,
however, revealed as being somewhat different, thus
suggesting the existence of a slightly different profile
for movement difficulties between people diagnosed
with schizophrenia compared with those with other
diagnoses in the study.
Concurrent validity, questionnaire
The BAS MQ-E questionnaire was associated with
Mastery, the MFI-20 subscales, the TAS-20, DICS and
the STAI subscale state, and trait. Self-administered
scales are known to correlate with a certain degree
L. HEDLUND ET AL.
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
due to the so-called subjective factor (Docx et al, 2012).
There was, however, a strong relation between the BAS
MQ-E questionnaire and STAI for patients with schizophrenia, concerning the trait anxiety (0.74).
The regression analysis of the whole sample showed
that MFI-20, physical fatigue accounted for approximately half of the variance of BAS MQ-E questionnaire
and the TAS-20, DICS for a further few percent. The
deficit in the identification of cenesthesic sensations
(DICS), within the Toronto Alexitymia Scale, has also
shown to be a prominent feature for patients with
schizophrenia (Maggini and Raballo, 2004a). All these
factors focus on bodily experiences in a similar way,
which may explain the co-variance between them.
et al, 2003). The function of multi-sensory integration
is described as being particularly important for the
experience of self-recognition and as a main neurological soft sign deficit for people with severe mental
illness (Ferri et al, 2012; Keshavan et al, 2003; Waters
and Badcock, 2010). The patients stiffness and/or lack
of voluntary control of the trunk were prominent in
our study. In addition to neurological deficiencies,
these might be psychological and physiological ways
of dealing with the bodily level of affects, however, at
the high cost of lost vitality and a contact with the
embodied self and less ability to achieve movement
quality (Gyllensten, Skr, Miller, and Gard, 2010;
Hedlund and Gyllensten, 2013; Postmes et al, 2014).
Clinical implications
Physiotherapeutic treatment in mental health services
are usually individualized and designed to increase the
patients resources and decrease bodily symptoms and
dysfunctions. The latter can have a number of causes and
lead to difficulties, both in relation to other people, the
self, and personal needs. Physically, they entail a greater
risk for various movement difficulties in daily life and
movement related injuries, fractures, tension, and pain
(Stubbs et al, 2014b; Stubbs et al, 2015). They may also
prohibit patients from being physically active and from
preventing increased risks for metabolic diseases by
making movement less pleasant, perhaps even painful,
and thus reducing autonomous motivation for physical
therapy (Vancampfort et al, 2015). It is of great importance that physiotherapists take a leading role in promoting physical activity for people with schizophrenia
(Stubbs et al 2014b, Vancampfort et al, 2015).
Treatments applied for increasing movement quality
may offer a first step in being able to tolerate movements
and/or make them enjoyable. When developing movement quality, it is important to assess the capacity to
perform voluntary movements.
MD such as extrapyramidal signs, catatonia, involuntary movements, motor slowing, and negative syndrome often spontaneously occur when clinically
assessing movement quality, and are noticed and communicated to other professionals. Neurological soft
signs are less evident with bodily movements, thus
making the concurrent validity interesting. When palpable difficulties occur with trunk coordination, it can be
relevant to further investigate and more specifically
assess the occurrence of neurological soft signs. This
assessment can, apart from explaining various movement difficulties, also contribute to clarifying the type
of psychosis and guide the team in the choice of treatment and rehabilitation (Docx et al, 2012; Keshavan
Limitations
There are a number of limitations in this study. Firstly,
we have no knowledge of the characteristics of those
who declined to participate in the study. Secondly, as
there were eight outpatient mental health service units
involved in data collection, there was no way to stringently follow up the recruitment process.
A major limitation is the lack of clear conceptual
boundaries between different types of MD and their
unknown etiology. Furthermore, we introduced
another aspect, movement quality, which is also a complex construct. The physiotherapist needs, however, to
include movement quality and movement control of
daily activities and social life in order to be able to
treat persons with movement difficulties (Hedlund
and Gyllensten, 2010; Hedlund and Gyllensten, 2013).
Another limitation is that the study included patients
with different diagnosis of severe mental illness.
Patients with schizophrenia spectrum disorder and
bipolar disease have both shown to have soft neurological signs, according to earlier studies (Docx et al,
2012; Zhao et al, 2013). The findings in this study
indicate a somewhat different BAS MQ-E profile in
the different populations, which should be targeted in
future research.
In terms of the inter-rater reliability, there were only
9 of 23 items that attained very good reliability. This
can be considered to be not satisfactory. However, the
scale has five levels in order to be clinically useful and
sensitive. We have investigated the disagreements of the
total number of ratings. There was no total agreement
for 33% (those cases had a discrepancy of 1 point),
while less than 1% had a discrepancy of 2 points.
There were only two cases with 3 points disagreement
and none with 4 points. This may thus be considered to
be clinically satisfactory.
PHYSIOTHERAPY THEORY AND PRACTICE
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
Conclusion
BAS MQ-E showed satisfactory psychometrics when
assessing movement quality in people with severe mental
illness. The two parts, the movement scale and the questionnaire, complement each other and provide important
information about aspects of movement quality and body
experience. Furthermore, the movement scale appears to
be able to discriminate movement-related difficulties
between people with schizophrenia and other schizophrenia spectrum disorders and bipolar disorder. Different
parts of MD and disturbed self-recognition appear when
assessing movement quality. The concurrent validity with
neurological soft signs and experienced physical fatigue
was confirmed in terms of the BAS MQ-E movement
scale. There was also a concurrent validity regarding the
BAS MQ-E questionnaire and other self-administrated
assessments such as Mastery, Toronto Alexithymia
Scale, State and Trait anxiety Inventory and
Multidimensional Fatigue Inventory. Further studies of
validity are needed in order to confirm the results of the
present study before making general clinical assumptions
of dimensions related to movement quality.
Declaration of interest
The authors report no conflicts of interest. The authors alone
are responsible for the content and writing of the article.
References
Bagby RM, Parker JD, Taylor GJ 1994 The twenty-item
Toronto Alexithymia Scale-I. Item selection and crossvalidation of the factor structure. Journal of
Psychosomatic Research 38: 2332.
Barnes LL, Harp D, Jung WS 2002 Reliability generalization
of scores on the Spielberger state-trait anxiety inventory.
Educational and Psychological Measurement 62: 603618.
Bengtsson-Tops A 2004 Mastery in patients with schizophrenia living in the community: Relationship to sociodemographic and clinical characteristics, needs for care and
support, and social network. Journal of Psychiatric and
Mental Health Nursing 11: 298304.
Bland JM, Altman DG 1997 Statistics notes: Cronbachs
alpha. British Medical Journal 314: 572.
Boyce WF, Gowland C, Rosenbaum PL, Lane M, Plews N,
Goldsmith C, Russell DJ, Wright V, Zdrobov S 1991
Measuring quality of movement in cerebral palsy: Review
of instruments. Physical Therapy 71: 813819.
Cantor AB 1996 Sample size calculations for Cohens kappa.
Psychological Methods 1: 150153.
Chan RC, Chen EY 2004 Executive dysfunctions and neurological manifestations in schizophrenia. Hong Kong
Journal of Psychiatry 14: 26.
Critchley H 2009 Psychophysiology of neural, cognitive and
affective integration: fMRI and autonomic indicants.
International Journal of Psychophysiology 73: 8894.
Destoop M, Bruijn E, Hulstijn W, Sabbe B 2009 A cognitive
neuropsychiatric analysis of psychomotor symptoms in
major depression and schizophrenia. Acta Neurologica
Belgica 109: 262270.
Docx L, Morrens M, Bervoets C, Hulstijn W, Fransen E, De
Hert M, Baeken C, Audenaert K, Sabbe B 2012 Parsing the
components of the psychomotor syndrome in schizophrenia. Acta Psychiatrica Scandinavia 126: 256265.
Dropsy J 1998 Human expression The coordination of
mind and body. In: Skjrven LH (ed) Quality of
Movement The Art and Health. Lectures on philosophy,
theory and practical implications to basic body awareness
therapy, pp. 820. Bergen, Bergen University College.
Eklund M, Erlandsson L-K, Hagell P 2012 Psychometric
properties of a Swedish version of the Pearlin Mastery
Scale in people with mental illness and healthy people.
Nordic Journal of Psychiatry 66: 380388.
Ferri F, Frassinetti F, Mastrangelo F, Salone A, Ferro F,
Gallese V 2012 Bodily self and schizophrenia: The loss of
implicit self-body knowledge. Consciousness and
Cognition 21: 13651374.
Frst CJ, hsberg E 2001 Dimensions of fatigue during
radiotherapy An application of the multidimensional
fatigue inventory. Support Care Cancer 9: 355360.
Gallagher S 2004 Neurocognitive models of schizophrenia: A
neurophenomenological critique. Psychopathology 37: 819.
Gwet KL 2012 Handbook of inter-rater reliability The
Definitive Guide to Measuring the Extent of Agreement
among Raters. Gaithersburg, MD, Advanced Analytics, LLC.
Gyllensten AL 2001 Basic Body Awareness Therapy,
Assessment, Treatment and Interaction. Thesis, Lund
University, Lund, Sweden.
Gyllensten AL, Ekdahl C, Hansson L 1999 The validity of
body awareness scale-health (BAS-H). Scandinavian
Journal of Caring Science 13: 217226.
Gyllensten AL, Ekdahl C, Hansson L 2009 Long-term effectiveness of Basic Body Awareness Therapy in psychiatric
outpatient care. A randomized control study. Advances in
Physiotherapy 11: 212.
Gyllensten AL, Mattsson M 2011 The manual of Basic Body
Awareness Scale Movement quality and experience. ISBN
978-91-633-9824-7.
Gyllensten AL, Skr L, Miller M, Gard G 2010 Embodied
identity A deeper understanding of body awareness.
Physiotherapy Theory and Practice 26: 439446.
Hedlund L, Gyllensten AL 2010 The experience of basic body
awareness therapy in patients with schizophrenia. Journal
of Bodywork and Movement Therapies 14: 245254.
Hedlund L, Gyllensten AL 2013 The physiotherapists experience of basic body awareness therapy in patients with schizophrenia and schizophrenia spectrum disorders. Journal of
Bodywork and Movement Therapies 17: 169176.
Hedlund L, Gyllensten AL, Hansson L 2015 A psychometric
study of the multidimensional fatigue inventory to assess
fatigue in patients with schizophrenia and schizophrenia
disorders. Community Mental Health Journal 51: 377382.
Hodges PW, Van Dillen LR, McGill S, Brumange S, Hides JA,
Mosely GR 2013 State-of-the art approach to clinical rehabilitation of low back and pelvic pain. In: Hodges,
Cholewicki J, Van Dieen JH (eds) Spine control: The
rehabilitation of back pain: State of the Art and Science,
pp. 243309. Edinburgh, Churchill Livingstone/Elsevier.
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
10
L. HEDLUND ET AL.
Keshavan MS, Sanders RD, Sweeney JA, Diwadkar VA,
Goldstein G, Pettegrew JW, Schooler NR 2003 Diagnostic
specificity and neuroanatomical validity of neurological
abnormalities in first-episode psychoses. American
Journal of Psychiatry 160: 12981304.
Kronholm E, Sallinen M, Era P, Sustama T, Sulkava R,
Partonen T 2011 Psychomotor slowness is associated
with self-reported sleep duration among the general population. Journal of Sleep Research 20: 288297.
Kupper Z, Ramseyer F, Hoffman H, Kalbermatten S,
Tschacher W 2010 Video-based quantification of body
movement during social interaction indicates the severity
of negative symptoms in patients with schizophrenia.
Schizophrenia Research 121: 90100.
Maggini C, Raballo A 2004a. Alexithymia and schizophrenic
psychopathology. Acta Biomedica 75: 4049.
Maggini C, Raballo A 2004b Self-centrality, basic symptoms
model
and
psychopathology
in
schizophrenia.
Psychopathology 37: 6975.
Mittal V, Jalbrzikowski M, Daley M, Roman C, Bearden C,
Cannon T 2011 Abnormal movements are associated with
poor psychosocial function in adolescents at high risk for
psychosis. Schizophrenia Research 130: 164169.
Morrens M, Docx L, Walther S 2014 Beyond boundaries: In
search of an integrative view on motor symptoms in schizophrenia. Frontiers in Psychiatry 5: 145.
Pearlin LI, Schooler C 1978 The structure of coping. Journal
of Health and Social Behavior 19: 221.
Postmes L, Sno HN, Goedhart S, van der Stel J, Heering, HD,
de Haan L 2014 Schizophrenia as a self-disorder due to
perceptual incoherence. Schizophrenia Research 152: 4150.
Price T, Dieckman L, Harmon-Jones E 2012 Embodying
approach motivation: Body posture influence startle eyeblink and event-related potential responses to appetitive
stimuli. Biological Psychology 90: 211217.
Priebe S, Rhricht F 2001 Specific body image pathology in
acute schizophrenia. Psychiatry Research 101: 289301.
Probst M, Knapen J, Poot G, Vancampfort D 2010
Psychomotor therapy and psychiatry: Whats in a name?
Open Complementary Medicine Journal 2: 105113.
Quitkin F, Rifkin A, Klein DF 1976 Neurologic soft signs in
schizophrenia and character disorders. Archives of General
Psychiatry 33: 845853.
Roxendal G 1985 Body Awareness Therapy and the Body
Awareness Scale, Treatment and Evaluation in Psychiatric
Physiotherapy. Thesis, Gothenburg, Sweden.
Sanders RD, Allen DN, D Forman S, Tarpey T, Keshavan MS,
Goldstein G 2005 Confirmatory factor analysis of the
Neurological Evaluation Scale in unmedicated schizophrenia. Psychiatry Research 133: 6571.
Sanders RD, Forman SD, Pierri JN, Baker RW, Kelley ME,
Van Kammen DP, Keshavan MS 1998 Inter-rater reliability of the neurological examination in schizophrenia.
Schizophrenia Research 29: 287292.
Sass A, Parnas J 2003 Schizophrenia, consciousness, and the
self. Schizophrenia Bulletin 29: 427444.
Schneider S, Christensen A, Huinger B, Fallgatter A, Giese
M, Ehlis M 2014 Show me how you walk and I tell you
how you feel A functional near-infrared spectroscopy
study on emotion perception based on human gait.
NeuroImage 85: 380390.
Serino A, Alsmith A, Costantini M, Mandrigin A, TajaduraJimenez A, Lopez C 2013 Bodily ownership and self-location: Components of bodily self-consciousness.
Consciousness and Cognition 22: 12391252.
Seth A 2013 Interoceptive inference, emotion, and the embodied self. Trends in Cognitive Sciences 17: 565573.
Simonsson-Sarnecki M, Lundh LG, Trestad B, Bagby RM,
Taylor G, Parker JA 2000 Swedish translation of the 20item Toronto Alexithymia Scale: Cross-validation of the factor structure. Scandinavian Journal of Psychology 41: 2530.
Skjrven L, Kristoffersen K, Gard G 2008 An eye for movement quality: A phenomenological study of movement
quality reflecting a group of physiotherapists understanding of the phenomenon. Physiotherapy Theory and
Practice 24: 1327.
Skjrven L, Kristoffersen K, Gard G 2010 How can movement quality be promoted in clinical practice? A phenomenological study of physical therapist experts. Physical
Therapy 90: 14791492.
Smets E, Garssen B, Bonke B, Haes J 1995 The multidimensional Fatigue inventory (MFI-20) psychometric qualities
of an instrument to assess fatigue. Journal of
Psychosomatic Research 39: 315325.
Spielberger CD 1983 Manual for the State-Trait Anxiety
Inventory STAI (Form Y Self-Evaluation Questionnaire)
Stubbs B, Gaughran F, Mitchell AJ, Hert M, Farmer R,
Soundy A, Rosenbaum S, Vancampfort D 2015
Schizophrenia and the risk of fractures: A systematic
review and comparative meta-analysis. General Hospital
Psychiatry 37: 126133.
Stubbs B, Mitchell AJ, De Hert M, Correll CU, Soundy A,
Rosenbaum S, Vancampfort D 2014a The prevalence and
moderators of clinical pain in people with schizophrenia:
A systematic review and large scale meta-analysis.
Schizophrenia Research 160: 18.
Stubbs B, Sound A, Probst M, Parker A, Skjrven LH,
Gyllensten AL, Vancampfort D 2014b Addressing the disparity in physical health provision for people with schizophrenia: An important role for physiotherapists.
Physiotherapy 100: 185186.
Sundn A, Ekdahl C, Horstman V, Gyllensten AL 2014
Analyzing movements Development and evaluation of
the Body Awareness Scale Movement Quality (BAS MQ).
Physiotherapy Research International doi/10.1002/pri.1618
[Epub ahead of print].
Thakkar K, Nichols H, McIntosh L, Park S 2011 Disturbances
in body ownership in schizophrenia: Evidence from the
rubber hand illusion and case study of a spontaneous outof-body experience. PLoS ONE 6: e27089.
Vancampfort D, Hert M, Stubbs B, Vansteenkiste M, Herdt
A, Scheewe T, Soundy A, Stubbs B, Probst M 2013 The
importance of self-determined motivation towards physical activity in patients with schizophrenia. Psychiatry
Research 210: 812818.
Vancampfort D, Hert M, Stubbs B, Ward P, Rosenbaum S,
Soundy A, Probst M 2015 Negative symptoms are associated with lower autonomous motivation towards physical
activity in people with schizophrenia. Comprehensive
Psychiatry 56: 128132.
Van Veluw S, Chance S 2014 Differentiating between self and
others: An ALE meta-analysis of fMRI studies of self-
PHYSIOTHERAPY THEORY AND PRACTICE
Downloaded by [University of California, San Diego] at 11:02 12 April 2016
recognition and theory of mind. Brain Imaging and
Behavior 8: 2438.
Walther S, Horn H, Razavi N, Koschorke P, Mller T, Strik
W 2009 Quantitative motor activity differentiates schizophrenia subtypes. Neuropsychobiology 60: 8086.
Walther S, Strik W 2012 Motor symptoms and schizophrenia.
Neuropsychobiology 66: 7792.
Waters F, Badcock J 2010 First-rank symptoms in schizophrenia: Reexamining mechanisms of self-recognition.
Schizophrenia Bulletin 36: 510517.
Wolff A, ODriscoll GA 1999 Motor deficits and schizophrenia: The evidence from neuroleptic-nave patients and
11
populations at risk. Journal of Psychiatry Neuroscience
24: 304314.
Zhao Q, Li Z, Huang J, Yan C, Dazzan P, Pantelis C, Cheung
EFC, Lui S, Chan R 2014 Neurological soft signs are not
soft in brain structure and functional networks: Evidence
from ALE meta-analysis. Schizophrenia Bulletin 40: 626641.
Zhao Q, Ma Y, Lui S, Lui W, Xu T, Yu X, Tan S, Wang Z,
Qu M, Wang Y, Huang J, Cheung E, Dazzan P, Chan R
2013 Neurological soft signs discriminate schizophrenia
from major depression but not bipolar disorder.
Progress in Neuro-psychopharmacoly and Biological
Psychiatry 43: 7278.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Tobin Principles and Practice of Mechanical Ventilation 3rd EditionDocument1,585 pagesTobin Principles and Practice of Mechanical Ventilation 3rd EditionLuis Lopez Reveles75% (20)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- What is mental illness and how can it be treatedDocument6 pagesWhat is mental illness and how can it be treatednaurahimanNo ratings yet
- PADIS Guidelines Teaching Slides ImmobilityDocument25 pagesPADIS Guidelines Teaching Slides ImmobilityDaniel Lago BorgesNo ratings yet
- Woman with schizoaffective disorder brought to ED with jaundice and leg swellingDocument19 pagesWoman with schizoaffective disorder brought to ED with jaundice and leg swellingwalt65No ratings yet
- Effects of Inspiratory Muscle Training Using An Electronic Device On Patients Undergoing Cardiac Surgery: A Randomized Controlled TrialDocument9 pagesEffects of Inspiratory Muscle Training Using An Electronic Device On Patients Undergoing Cardiac Surgery: A Randomized Controlled TrialDaniel Lago BorgesNo ratings yet
- Virtual Reality On Pulmonary Function and Functional Independence After Coronary Artery Bypass Grafting - Clinical TrialDocument7 pagesVirtual Reality On Pulmonary Function and Functional Independence After Coronary Artery Bypass Grafting - Clinical TrialDaniel Lago BorgesNo ratings yet
- Effects of Inspiratory Muscle Training Using An Electronic Device On Patients Undergoing Cardiac Surgery: A Randomized Controlled TrialDocument9 pagesEffects of Inspiratory Muscle Training Using An Electronic Device On Patients Undergoing Cardiac Surgery: A Randomized Controlled TrialDaniel Lago BorgesNo ratings yet
- Lof Scale Cicu PDFDocument20 pagesLof Scale Cicu PDFDaniel Lago BorgesNo ratings yet
- 192 FullDocument20 pages192 FullDaniel Lago BorgesNo ratings yet
- s13054 019 2662 8Document14 pagess13054 019 2662 8Daniel Lago BorgesNo ratings yet
- EffectsDocument6 pagesEffectsDaniel Lago BorgesNo ratings yet
- Icd 10Document4 pagesIcd 10ÜnŶäÜnClubEverydayNo ratings yet
- He Manga RipDocument5 pagesHe Manga Ripkaren.pandhikaNo ratings yet
- IPA BPSD Educational PackDocument161 pagesIPA BPSD Educational PackbloadyroarNo ratings yet
- Wwii and NYCDocument59 pagesWwii and NYCbeemitsuNo ratings yet
- Slachevsky Cuideme 2013Document11 pagesSlachevsky Cuideme 2013Catalina KNo ratings yet
- A Case Study of Person With Schizophrenia With Auditory Hallucinations (Voices) - A Cognitive Behavioral Case Work ApproachDocument13 pagesA Case Study of Person With Schizophrenia With Auditory Hallucinations (Voices) - A Cognitive Behavioral Case Work ApproachHasmine HussainNo ratings yet
- Nurse Labs Practice Test 12 PDFDocument5 pagesNurse Labs Practice Test 12 PDFNatalie Pemberton-ParrisNo ratings yet
- Psychiatric Nursing SlidesDocument27 pagesPsychiatric Nursing SlidesHazel RoseNo ratings yet
- AB ? Pre-Board Exam-1Document20 pagesAB ? Pre-Board Exam-1sdfghNo ratings yet
- 1 2018Document48 pages1 2018Lizz22No ratings yet
- Psychological DisordersDocument44 pagesPsychological DisordersBeatriz Helaena RasonableNo ratings yet
- 5 Schizophrenia (2020)Document57 pages5 Schizophrenia (2020)Shreya ThackerNo ratings yet
- Online CasebookDocument7 pagesOnline Casebookapi-451547301No ratings yet
- My Brother Tom's Schizophrenia: by Marin SardyDocument10 pagesMy Brother Tom's Schizophrenia: by Marin Sardyapi-450510068No ratings yet
- Klinika Za Psihijatriju Slucajevi PrevodDocument24 pagesKlinika Za Psihijatriju Slucajevi PrevodEra69No ratings yet
- Block 4 PDFDocument81 pagesBlock 4 PDFD S ThejeshNo ratings yet
- Effects of The Nursing Psychoeducation Program On The Acceptance of Medication and Condition-Specific Knowledge of PatientDocument6 pagesEffects of The Nursing Psychoeducation Program On The Acceptance of Medication and Condition-Specific Knowledge of PatientEric KatškovskiNo ratings yet
- Test 1.choose The Right AnswerDocument15 pagesTest 1.choose The Right AnswerАлександр ХмельницкийNo ratings yet
- Fast Facts On Catatonic SchizophreniaDocument4 pagesFast Facts On Catatonic SchizophreniakeithevaristoNo ratings yet
- Mental Health Nursing GuideDocument14 pagesMental Health Nursing GuideEsarpy (Nana)No ratings yet
- Mood Disorder GuideDocument18 pagesMood Disorder GuideDwi SeptaNo ratings yet
- Early PsychosisDocument118 pagesEarly Psychosissolomon1234567100% (1)
- 0deec5369d64571d2a000000 PDFDocument11 pages0deec5369d64571d2a000000 PDFWidiya AndreliaNo ratings yet
- Psychiatrist in Pune - Dr. Niket KasarDocument8 pagesPsychiatrist in Pune - Dr. Niket KasarDr. Niket KasarNo ratings yet
- Asestudy 10Document4 pagesAsestudy 10api-292950560No ratings yet
- tcrm0301 003Document11 pagestcrm0301 003paulNo ratings yet
- Asperger's Syndrome in AdulthoodDocument7 pagesAsperger's Syndrome in AdulthoodWillyOaksNo ratings yet
- Psych Abnormal Child Psychology - 6th Edition (2015) - 1-50-3-10-3-8Document6 pagesPsych Abnormal Child Psychology - 6th Edition (2015) - 1-50-3-10-3-8tin_ally9059No ratings yet