Professional Documents
Culture Documents
Pathological Biomineralization in The Calcific Aortic Valve
Uploaded by
Peertechz Publications Inc.Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pathological Biomineralization in The Calcific Aortic Valve
Uploaded by
Peertechz Publications Inc.Copyright:
Available Formats
Journal of Cardiovascular Medicine and Cardiology
eertechz
Elena Cavarretta1* and Adriana Maras2
Editorial
Department of Medical-Surgical Sciences and
Biotechnologies, Sapienza University of Rome, corso
della Repubblica 79, 04100 Latina, Italy.
2
Department of Earth Sciences, Sapienza University
of Rome, piazzale Aldo Moro 5, Rome, Italy
Pathological Biomineralization in the
Calcific Aortic Valve
Dates: Received: 28 September, 2016; Accepted:
21 October, 2016; Published: 22 October, 2016
*Corresponding author: Elena Cavarretta, MD,
PhD, Department of Medical-Surgical Sciences and
Biotechnologies, Sapienza University of Rome, corso
della Repubblica 79, 04100 Latina, Italy, E-mail:
www.peertechz.com
ISSN: 2455-2976
Editorial
The prevalence of moderate to severe calcific aortic valve
stenosis in patients 75 years old is 2.8% and only 40% of patients
with surgical indication undergo aortic valve replacement because
of high perioperative risk, older age, lack of symptoms, and patient/
family refusal [1]. In the absence of hemodynamically significant
left ventricular (LV) outflow obstruction, calcific aortic valve
disease (CAVD) prevalence raises up to 25% in patients aged from
65 to 74 years old [2,3] and independently predicts cardiovascular
(CV) event, overall and CV mortality. As the population ages and
CAVD incidence and prevalence increase, it is crucial a deeper
understanding of the patho-physiology of heart valve calcification
that could provide novel insight into medical therapeutic approaches
to delay or modify the disease course. In the human body, several
physiological processes of calcification take places and mineralized
deposits are present, as bones, enamel and dentin. More than that,
pathological mineralization can lead to ectopic calcification and
pathologies as urinary stones, vascular calcification and calcific heart
valve stenosis. Macroscopically, in aortic valve sclerosis there is
an initial thickening of the valve leaflets and formation of calcium
nodules, usually corresponding to the nodules of Arantio near the
aortic surface, in association to angiogenesis, while end-stage calcific
aortic stenosis is characterized by large, heavily calcific, nodular
masses within the aortic cusps that protrude into the sinuses of
Valsalva, thus interfering with valve opening along the aortic surface.
While in the past heart valve calcification was seen as a passive,
degenerative course of aging, evidences have shown that is an active,
cell-mediated process with similarities to bone development (osseus
metaplasia) [4]. In fact all of the markers of bone differentiation
including the non-collagenous bone matrix proteins osteopontin,
osteocalcin, bone sialoprotein and the osteoblast transcription factor
Cbfa1 were found increased in the calcific aortic valve that express
an osteoblast phenotype [5]. Studies on the pathobiology of CAVD
showed that the calcific process begins deep into the valve tissue, near
the margins of attachment. As for vascular calcification, oxidized lowdensity lipoproteins (LDL) play an important role in the initiation
[6], in association with angiotensin-converting enzyme (ACE) and
its product, angiotensin II. ACE has been found colocalized with
apolipoprotein B, the primary protein found on LDL, in aortic valve
lesions and also associated with plasma LDL, which may deliver ACE
to aortic valve lesions [7]. In addition, oxidative stress is increased in
calcified aortic valves, due to reduction in expression and activity of
antioxidant enzymes and perhaps to uncoupled nitric oxide synthases
(NOS) activity [8]. The presence of reactive oxygen species associated
to inflammatory cytokines, growth factors, altered shear stress and
hypertension could be the triggers for valvular interstitial cells (VICs)
pathological differentiation in myofibroblasts and osteoblasts. The
so activated VICs produce matrix metalloproteinases, involved in
extracellular matrix remodeling, and increase angiogenic activity, thus
creating the perfect microenvironment to promote mineralization.
In particular valve calcification is composed of calcium phosphate
crystals that form biominerals, deposited on a bone-like matrix of
collagen, osteopontin, and other minor bone matrix proteins. The
spatial organization of fibrils can create the crystal-growing niche,
where pathological biomineralization can take place because of
the specific physical-chemical characteristics that lead to mineral
precipitation so that crystal can grow with a regular shape [9].
Nowadays bioapatite is the term most used in different scientific
fields to indicate the mineral component of normal mineralized
tissues and pathological calcification. This term is considered as
indicative of an impure carbonate-containing apatite but, at present,
the International Mineralogical Association Commission on New
Minerals, Nomenclature and Classification (IMA-CNMNC) has
not fully accepted it. We used infrared and Raman spectroscopy to
demonstrate the exact crystallographic structure of bioapatite. In
fact, in the calcified deposits, after calcium [Ca] and phosphorus [P],
the carbonate group [CO3] is the most important constituent. The
percentage of [CO3] ranges from 5 to 10% in weight and its dominant
location is in place of [PO4] [10]. The [CO3] substitution is linked to
the major solubility and chemical reactivity of the inorganic phase
both in vitro and in vivo. Moreover, nanometer scale investigations
revealed that the pathological crystals are closely bound with the
organic matrix and are characterized by variable size and shape,
organized on different spatial scale. There is a high heterogeneity within
calcific aortic valve nodules, where fully mineralized and partially
mineralized areas are both present, representing two different stages
of pathological mineralization [11]. Moreover, slightly but significant
differences in terms of Ca and P amount exist between tricuspid and
bicuspid CAVD. Even if macroscopically bicuspid valves show an
accelerated and heavier calcification, chemically the concentration of
Ca:P and their the mean weight % are significantly reduced compared
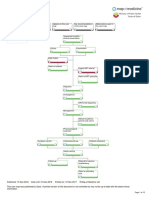
to tricuspid aortic valve or calcific mitral valve (Figure 1).
Citation: Cavarretta E, Maras A (2016) Pathological Biomineralization in the Calcific Aortic Valve. J Cardiovasc Med Cardiol 3(1): 045-046. DOI:
10.17352/2455-2976.000032
045
Cavarretta and Maras. (2016)
References
1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. (2016) Heart
Disease and Stroke Statistics-2016 Update: A Report From the American
Heart Association. Circulation 133 :e38-60.
2. Vlzke H, Haring R, Lorbeer R, Wallaschofski H, Reffelmann T, et al.
(2010) Heart valve sclerosis predicts all-cause and cardiovascular mortality.
Atherosclerosis 209: 606-610.
3. Owens DS, Budoff MJ, Katz R, Takasu J, Shavelle DM, et al. (2012) Aortic
valve calcium independently predicts coronary and cardiovascular events in
a primary prevention population. JACC Cardiovasc Imaging 5: 619-625.
Figure 1: Schematic diagram of pathologic biomineralization in cardiac
valve stenosis. Oxidatively modified lipids promote inflammation with release
of inflammatory cytokines to stimulate osteo-condrogenic differentiation
of valvular interstitial cells (VICs) and stiffening of their extracellular matrix
(ECM) with synthesis of new and less compliant matrix proteins. The newer
ECM spatial disposition supports the development of compartmental niches
with specific physico-chemical condition. In the niche the accumulation of
high concentrated extracellular fluids takes place, leading to the mineral
precipitation and crystallization of bioapatite.
Our nanoscale observations indicate that the formation of
pathological bioapatite nanocrystals within heart valves is related to
the presence of a highly heterogeneous bioapatite. Growth processes
may occur in different microenvironments (each one with its own
physico-chemical characteristics) influencing the shape of the
biomineralization.
The presence of compartmental niches within the extracellular
matrix assumes a relevant role in the formation of ectopic
biomineralization in human heart valves as well as the action of the
organic substrate on the crystals features.
These innovative findings at nanometer scale unveil novel insight
into pathological calcification and could open new perspective to
promote further studies on a novel medical approach to treat aortic
valve calcification.
4. Rajamannan NM, Evans FJ, Aikawa E, Grande-Allen KJ, Demer LL, et al.
(2011) Calcific aortic valve disease: not simply a degenerative process: A
review and agenda for research from the National Heart and Lung and Blood
Institute Aortic Stenosis Working Group. Executive summary: Calcific aortic
valve disease-2011 update. Circulation 124: 1783-1791.
5. Caira FC, Stock SR, Gleason TG, McGee EC, Huang J, et al. (2006) Human
degenerative valve disease is associated with up-regulation of low-density
lipoprotein receptor-related protein 5 receptor-mediated bone formation. J
Am Coll Cardiol 47: 1707-1712.
6. Olsson M, Thyberg J, Nilsson J (1999) Presence of oxidized low density
lipoprotein in nonrheumatic stenotic aortic valves. Arterioscler Thromb Vasc
Biol 19: 1218-1222.
7. OBrien KD, Shavelle DM, Caulfield MT, McDonald TO, Olin-Lewis K, et
al. (2002) Association of angiotensin-converting enzyme with low-density
lipoprotein in aortic valvular lesions and in human plasma. Circulation 106:
2224-2230.
8. Miller JD, Chu Y, Brooks RM, Richenbacher WE, Pea-Silva R, et al. (2008)
Dysregulation of antioxidant mechanisms contributes to increased oxidative
stress in calcific aortic valvular stenosis in humans. J Am Coll Cardiol 52: 843850.
9. Cottignoli V, Relucenti M, Agros G, Cavarretta E, Familiari G, et al.
(2015) Biological Niches within Human Calcified Aortic Valves: Towards
Understanding of the Pathological Biomineralization Process. Biomed Res
Int 2015: 542687.
10. Mangialardo S, Cottignoli V, Cavarretta E, Salvador L, Postorino P, et al.
(2012) Pathological biominerals: Raman and infrared studies of bioapatite
deposits in human heart valves. Appl Spectrosc 66: 1121-117.
11. Cottignoli V, Cavarretta E, Salvador L, Valfr C, Maras A (2015) Morphological
and chemical study of pathological deposits in human aortic and mitral valve
stenosis: a biomineralogical contribution. Patholog Res Int 2015: 342984.
Copyright: 2016 Cavarretta E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
046
Citation: Cavarretta E, Maras A (2016) Pathological Biomineralization in the Calcific Aortic Valve. J Cardiovasc Med Cardiol 3(1): 045-046. DOI:
10.17352/2455-2976.000032
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Cancer Industry, The Classic Expose of The - Moss, Ralph WDocument546 pagesCancer Industry, The Classic Expose of The - Moss, Ralph Wpdf ebook free download80% (5)
- 6.01 Clinical Formulation: Gillian Butler University of Oxford, Warneford Hospital, UKDocument24 pages6.01 Clinical Formulation: Gillian Butler University of Oxford, Warneford Hospital, UKLynda Hernandez100% (1)
- Steroid in EntDocument113 pagesSteroid in Entdrazmy2006100% (1)
- Diagnosis and Treatment of Traumatic Brain InjuryDocument22 pagesDiagnosis and Treatment of Traumatic Brain InjuryAmandaNo ratings yet
- Osce PDFDocument228 pagesOsce PDFOnur Temizsoylu100% (1)
- Case Study For Peri-Appendiceal AbcessDocument79 pagesCase Study For Peri-Appendiceal Abcessmarife100% (5)
- Taking History Exam in ENTDocument7 pagesTaking History Exam in ENTLumos NoxNo ratings yet
- Bracket PositionDocument10 pagesBracket PositionBarsha ThapaNo ratings yet
- Decreased Fetal MovementDocument4 pagesDecreased Fetal MovementYwagar YwagarNo ratings yet
- A Survey of Solid Waste Management in Chennai (A Case Study of Around Koyambedu Market and Madhavaram Poultry Farms)Document4 pagesA Survey of Solid Waste Management in Chennai (A Case Study of Around Koyambedu Market and Madhavaram Poultry Farms)Peertechz Publications Inc.100% (1)
- Angiosarcoma of The Scalp and Face: A Hard To Treat TumorDocument4 pagesAngiosarcoma of The Scalp and Face: A Hard To Treat TumorPeertechz Publications Inc.No ratings yet
- MEK Inhibitors in Combination With Immune Checkpoint Inhibition: Should We Be Chasing Colorectal Cancer or The KRAS Mutant CancerDocument2 pagesMEK Inhibitors in Combination With Immune Checkpoint Inhibition: Should We Be Chasing Colorectal Cancer or The KRAS Mutant CancerPeertechz Publications Inc.No ratings yet
- PLGF, sFlt-1 and sFlt-1/PlGF Ratio: Promising Markers For Predicting Pre-EclampsiaDocument6 pagesPLGF, sFlt-1 and sFlt-1/PlGF Ratio: Promising Markers For Predicting Pre-EclampsiaPeertechz Publications Inc.No ratings yet
- Fishing Condition and Fishers Income: The Case of Lake Tana, EthiopiaDocument4 pagesFishing Condition and Fishers Income: The Case of Lake Tana, EthiopiaPeertechz Publications Inc.No ratings yet
- International Journal of Aquaculture and Fishery SciencesDocument4 pagesInternational Journal of Aquaculture and Fishery SciencesPeertechz Publications Inc.No ratings yet
- Imaging Journal of Clinical and Medical SciencesDocument7 pagesImaging Journal of Clinical and Medical SciencesPeertechz Publications Inc.No ratings yet
- BursitisDocument8 pagesBursitisAgeededin HartNo ratings yet
- Brain Development of Children From 0 To 6 Years How The Brain LearnsDocument1 pageBrain Development of Children From 0 To 6 Years How The Brain Learnssyarifah wardah el hilwaNo ratings yet
- PintoOCPDtreatmentchapter PDFDocument16 pagesPintoOCPDtreatmentchapter PDFSabrina HortopanNo ratings yet
- Schizophrenia Case StudiesDocument3 pagesSchizophrenia Case StudiesVierman BalweelNo ratings yet
- FluidotherapyDocument21 pagesFluidotherapyProtantagonist67% (6)
- 06 2016 Biomedical Instrumentation - Blood Pressure MeasurementDocument27 pages06 2016 Biomedical Instrumentation - Blood Pressure Measurementviki mikiNo ratings yet
- Structured Nursing Rounds (SNR) Training Module On The Level of Patient SatisfactionDocument5 pagesStructured Nursing Rounds (SNR) Training Module On The Level of Patient SatisfactionMalarvizhi SureshNo ratings yet
- 5 Processes of LaborDocument2 pages5 Processes of LaborElla Rene MartinNo ratings yet
- Brochure Balanzas ADEDocument40 pagesBrochure Balanzas ADEArquitecta Angela Mamani VillafuerteNo ratings yet
- Resume - Taylor BrewerDocument2 pagesResume - Taylor Brewerapi-348143543No ratings yet
- Antibiotic Prophylaxis For Patients After Total Joint ReplacementDocument3 pagesAntibiotic Prophylaxis For Patients After Total Joint ReplacementyeyennyaygadygtaNo ratings yet
- Pediatric Nursing: Prepared By: Adahlia T. Basco RN, MANDocument226 pagesPediatric Nursing: Prepared By: Adahlia T. Basco RN, MANMika SamsonNo ratings yet
- MonitorDocument3 pagesMonitorestebanNo ratings yet
- The AVPU ScaleDocument10 pagesThe AVPU ScalePrateek YadavNo ratings yet
- Nursing Research Synthesis Paper - 1Document8 pagesNursing Research Synthesis Paper - 1api-308407014No ratings yet
- Ban Xuất Huyết BatemanDocument7 pagesBan Xuất Huyết BatemanhoangNo ratings yet
- The Way To The RemedyDocument29 pagesThe Way To The RemedyIvana BlagojevicNo ratings yet
- Tonsillitis Inggris PDFDocument18 pagesTonsillitis Inggris PDFRiris RaudyaNo ratings yet
- 82medical NegligenceDocument35 pages82medical Negligencepcarsten-1No ratings yet
- Med SurgChapter 38Document10 pagesMed SurgChapter 38Leila Acero Salinas100% (1)
- MCP AbxDocument34 pagesMCP AbxShynne RPhNo ratings yet