Professional Documents
Culture Documents
Abstracts From The Difficult Airway Society Meeting 2014 Bja - Aev258.full
Uploaded by
Eugenio Daniel Martinez HurtadoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abstracts From The Difficult Airway Society Meeting 2014 Bja - Aev258.full
Uploaded by
Eugenio Daniel Martinez HurtadoCopyright:
Available Formats
BJA Advance Access published November 17, 2015
British Journal of Anaesthesia, 2015, 118
doi: 10.1093/bja/aev258
Abstracts
A B S T R AC T S
Abstracts from the Difcult Airway Society meeting 2014
(The name of the person presenting the paper is shown in bold type. All authors have certied that, where appropriate, studies have been conducted with the approval of the relevant
Human Ethics Committee or Animal Experimental Review Committee.)
An unusual perioperative complication: a case
of postintubation tracheal rupture
A.
Anwar1,
M.
Hulgar1
and P.
Lanka2
Wrightington and Leigh Hospitals NHS Trust, Wigan, UK,
and 2Hull and East Yorkshire Hospitals NHS Trust, Hull, UK
We discuss a patient who experienced iatrogenic postintubation
tracheal rupture for an L5/S1 discectomy under general anaesthesia. Tracheal rupture is often linked with blunt trauma, but
is a rare complication after intubation with a high morbidity
and mortality. It has a reported incidence of one in 20 000
intubations.
Case report
A 41-yr-old female with a BMI of 38 kg m2 and short stature was
admitted for an L5/S1 discectomy. She was an ASA II patient
with a history of migraine. Anaesthesia was maintained with
desurane, and no nitrous oxide was used. Oral intubation with
a cuffed 7.5 mm reinforced tracheal tube was unremarkable with
Cormack Grade 1 laryngoscopy. The cuff was inated with an
unknown volume of air, and no cuff pressures were measured.
The patient was placed prone for surgery, which lasted 2 h with
normal airway pressures and no desaturations. In recovery, she
had an explosive cough with blood-stained sputum and suddenly
developed a large neck swelling. On examination she was haemodynamically stable with a central trachea, but there was bilateral
surgical emphysema. Initial differential diagnosis included a ruptured bulla or Boerhaave syndrome. A chest X-ray showed a
widened mediastinum with no pneumothorax (Fig. 1). The patient
was transferred to the high-dependency unit with an ear, nose,
and throat review. A computed tomography scan showed a defect
in the posterior wall of the trachea at the level of T1 measuring
2.5 cm in length and 9 mm in diameter (Fig. 1). The patient was
discussed with cardiothoracic surgeons, who advised conservative management. No bronchoscopy was undertaken. The swelling reduced in size after 3 days, and the patient was discharged,
with follow-up showing her to make a full recovery.
Discussion
Patient risk factors for tracheal tears include being female, short
stature, and obesity. Higher prevalence in women is attributable
to a weaker pars membranosa and use of inappropriate tracheal
tube sizes. In this instance, the female patient was of short
height, and prone positioning may have led to pressure of the tracheal tube cuff and thinning of the posterior tracheal membrane.
Over-expansion of the tracheal tube cuff without measurement
of cuff pressures can lead to tears and may be a cause in this patient. Best practice may be to listen when inating the cuff to seal
the leak and to deate and reinate the cuff during long procedures to prevent increases in cuff pressures. Emergency intubation1 is a main risk factor and increases the risk of death
compared with elective intubation. The denitive investigation
is urgent bronchoscopy, allowing for the direct examination of
the trachea, with chest X-rays and computed tomography scans
assisting with diagnosis. There is no consensus for management,
but the current trend is to minimize invasive surgery by conservative management.2
References
1. Miambres E, Burn J, Ballesteros MA, Llorca J, Muos P,
Gonzlez-Castro A. Eur J Cardiothorac Surg 2009; 35: 105662
2. Conti M, Pougeoise M, Wurtz A, Porte H, Fourrier F, Ramon P,
Marquette C-H. Chest 2006; 130: 412418
Oxygen delivery during awake bre-optic
intubation: a case series using high-ow
nasal cannula
S. Badiger, A. Fearnley and I. Ahmad
Guys and St Thomas NHS Foundation Trust, London, UK
Awake bre-optic intubation (AFOI) is a widely practised technique for anticipated difcult airway management. The most frequently used interfaces to provide oxygen during the procedure
are low-ow devices, such as a nasal cannula, a face mask, a
Published by Oxford University Press on behalf of the British Journal of Anaesthesia 2015.
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
Stratford-upon-Avon, UK, November 1214, 2014
| Abstracts
nasal sponge, a suction catheter placed in the nostril, or via the
working channel of the brescope. High-ow humidied nasal
oxygen therapy is an alternative method of delivering oxygen,
and in recent years, has been increasingly adopted across many
clinical areas.
Case series
We reviewed 25 patients for whom AFOI was performed using
Optiow (Fisher & Paykel Healthcare, Maidenhead, UK) to deliver oxygen. All patients were adults with complex oropharyngeal or laryngeal pathology. The mean () BMI of the patients
was 27.25 (7.98) kg m2.
Median [interquartile range (range)] baseline oxygen saturation (SpO2 ) was 98 [9799 (95100)]%. The oropharynx was anaesthetized in all patients using lidocaine 4%, and cocaine 100 mg
was applied to the nasal passage in the 19 patients requiring
nasal intubation. Conscious sedation was administered via target-controlled infusions of remifentanil and propofol. Optiow
3060 l min1 was applied from before the onset of sedation until
successful tracheal intubation was conrmed and the tracheal
tube connected to the anaesthetic circuit, a mean () time of
19.38 (2.82) min. Median [interquartile range (range)] SpO2 and
end-tidal carbon dioxide immediately postintubation was 100
[100100 (99100)]% and 4.8 [4.05.1 (3.56.1)] kPa, respectively.
There were no desaturations during any procedure despite one
instance of oversedation and temporary apnoea. During the routine postoperative visit, all patients reported a comfortable experience in terms of oxygen application.
Discussion
Hypoxaemia is a risk during AFOI because of the pre-existing nature of the pathology, complications such as spasm or bleeding
during the procedure causing airway compromise, the depressant effects of sedation administered, and the local anaesthesia
application itself. Previous AFOI studies have shown the incidence of desaturation below 80% to be 1.5% with a low-ow
nasal cannula,1 and signicant desaturation has been reported
in groups using a nasal probe.2 Using a high ow ensures that a
higher fractional inspired oxygen is delivered and provides a
nasopharyngeal reservoir of oxygen and a low level of positive
expiratory pressure.3 We also found that the high ow helps
the spread of local anaesthetic applied around the nasopharynx.
The humidication of inspired gases ensures patient comfort
and aids mucociliary clearance. Our case series suggests that
high-ow nasal cannulation can be tolerated in patients undergoing AFOI and may minimize the potential risk of desaturation.
References
1. Cook TM, MacDougall-Davis SR. Br J Anaesth 2012; 109(Suppl 1):
i6885
2. Piepho T, Thierbach AR, Gobler SM, Maybauer MO, Werner C.
Eur J Anaesthesiol 2009; 26: 328332
3. Ward JJ. Respir Care 2013; 58: 98122
Pilot feasibility study into the role of virtual
endoscopy in the pre-anaesthetic assessment
of oral and maxillofacial surgery patients
J. Harte1, A. Cartwright1, K. Rajaram1, O. Thomas2,
G. Potter2 and T. Blackburn1
1
Central Manchester NHS Foundation Trust, Manchester, UK,
and 2Salford Royal NHS Foundation Trust, Salford, UK
Fibre-optic intubation is the gold-standard intubation technique
in a suspected difcult airway, but it is invasive and is often
not well tolerated. Computed tomography virtual endoscopy
(CTVE) is an imaging technique that allows non-invasive, threedimensional dynamic assessment of the upper aerodigestive
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
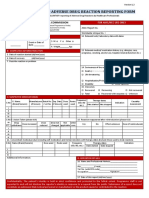
Fig 1 () Chest X-ray showing air in the mediastinum. Computed tomography scan images ( and ) showing a defect in the posterior wall of the trachea at the level
of T1 measuring 2.5 cm in length and 9 mm in diameter.
Abstracts
tract. Over the last decade, CTVE has been used in intubation
training;1 however, there is limited research on its role in airway
assessment. The aim of this study was to evaluate the feasibility
of CTVE in the preoperative anaesthetic assessment of oral and
maxillofacial surgery patients.
| 3
Airway management in patients with critical airway obstruction
is a high-risk procedure.1 A number of airway-management options have been described,2 3 but there is no consensus on how
best to secure the airway. We report ndings from a pilot study
of awake intubation using King Vision video laryngoscope (King
Vision VL) in a cohort of 22 patients.
Methods
Results
The study sample included 11 patients, but two were excluded
because videos were unable to be generated from the computed
tomography scans. Radiologists spent on average 18 min generating each video, whereas anaesthetists spent on average 3 min
reviewing the CTVE, with 9 of 15 questionnaires stating that it
did or would reduce intubation time. The median anaesthetic
score for incorporating CTVE into workow was 9 out of 10
[interquartile range (IQR) 710] compared with 7 [IQR 510] by
the radiologists. The median opinion for ease of use was graded
as 9 [IQR 510] by the anaesthetists and 7 [IQR 58] by the radiologists. Anaesthetists rated CTVE contribution to education as 8
out of 10 [IQR 510], whilst the radiologists rated the same statements as 7 [IQR 47]. There was a marked variation in anaesthetic
opinions on whether CTVE added additional information to
care, with anaesthetists rating this from 0 to 9 with a median
of 7. The opinions of anaesthetists regarding clinical applications
in the future included tumours (13 out of 15), difcult airways (8
out of 15), and previous nasal or cleft surgery (5 out of 15).
Discussion
Computed tomography virtual endoscopy is a potentially useful
non-invasive tool in pre-intubation airway assessment in oral
and maxillofacial surgery patients, and may be feasible in terms
of ease of image production and review, in addition to being a useful educational tool. Clinical value in terms of adding additional information may vary depending on the presence or absence of
airway pathology, and may be of particular value in preoperative
planning in patients with a suspected difcult airway by providing
anaesthetists with a more user-friendly simulation of the airway.
Reference
1. Mayrose J, Kesavadas T, Chung K, Joshi D, Ellis DG. Resuscitation
2003; 59: 1338
A study of awake video laryngoscope-assisted
intubation in patients with periglottic tumour
L. Markova1, T. Luzar1, J. Benedik1, T. Stopar-Pintaric1
and I. Hodzovic2
Methods
After approval of the University Medical Centre ethics committee, 22 patients with periglottic tumour took part in this study.
Patients with mouth opening less than 18 mm, presenting with
stridor requiring urgent airway management, or both were excluded. Xylocaine 10% and lidocaine 4% were used for topical anaesthesia of the airway with remifentanil and midazolam
sedation. We recorded success rate, time to intubation (from
passing the incisors to the rst capnograph trace), number of
attempts (removal of King Vision VL from the airway and reinsertion), and the patients experience on a 100 mm visual
analog scale (0=very unpleasant, 100=very pleasant). Failure of
the procedure was declared if the patient did not tolerate the procedure or if arterial oxygen saturation decreased to <90%.
Intubations were videoed using the King Vision VL.
Results
Twenty-two patients with mean () BMI 33 (6) kg m2, admitted
for diagnostic or radical surgery throughout a period of 7 months,
took part in the study. Four presented with stridor at rest, two had
stridor on lying at, and 16 patients had no stridor.
Two failures were recorded; Patients 2 and 11 could not tolerate the procedure because of inadequate topical anaesthesia. Patient 5 was intubated on the third attempt with a smaller tube
size (stridor at rest patient). Mean () patient satisfaction visual
analog scale score was 79 (29) mm.
Discussion
Awake video laryngoscope-assisted intubation offers a number
of advantages in patients with critical airway obstruction. The
King Vision VL provided wide-angle view, making it possible to
identify the laryngeal opening accurately, often hidden behind
the tumour. Furthermore, advancement of the tube was often associated with relief of the obstruction, adding to the patient acceptance of the technique. The cork-in-a-bottle effect2 and
blind railroading associated with the use of the brescope were
avoided with this technique. Lastly, the King Vision VL created
an airway during intubation, allowing for accurate application
of atomized local anaesthetic and clearance of the secretions
under direct vision. In order to improve the patients acceptance
of the technique, meticulous attention should be paid to
adequate topical anaesthesia of the airway. Awake video laryngoscope-assisted intubation could be a useful technique in patients
with critical airway obstruction.
Table 1 Main study ndings. Values are mean () and number
(%) as appropriate. n=22
Success
First attempt
success
Time to
glottic view (s)
Total time to
intubation (s)
20 (90%)
12 (74%)
19 (5)
55 (23)
University Medical Centre Ljubljana, Ljubljana, Slovenia,
and 2Cardiff University and Aneurin Bevan University Health
Board, Cardiff, UK
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
This prospective pilot study included patients who required diagnostic head and neck computed tomography scans before oral
and maxillofacial surgery, throughout a 10 week period. No ethical approval was required. Three-dimensional dynamic videos
from nostril to glottis were produced using GE Advantage Windows Suite by two neuroradiologists. Videos were reviewed by
15 anaesthetists pre-intubation and four radiologists, who completed 10-point modied Likert questionnaires.
| Abstracts
Declaration of interest
The manufacturers of King Vision video laryngoscope, Ambu A/S,
2750 Ballerup, Denmark provided the King Vision video laryngoscope, disposable blades and the recording cable for this study.
References
1. Cook TM, Woodall N, Frerk C. Br J Anaesth 2011; 106: 61731
2. Patel A, Pearce A. Anaesthesia 2011; 66: 93100
3. Lambert C, Passant C, Hodzovic I. Eur J Anaesthesiol 2013;
30: 258
A. Jain
References
1. Charters P, OSullivan E. Anaesthesia 1999; 54: 7786
2. Elam JO, Titel JH, Feingold F, Weisman H, Bauer RO. Anesth
Analg 1969; 48: 3076
Evaluating the impact of positive
end-expiratory pressure on aspiration
risk with supraglottic airway devices
Manchester Royal Inrmary, Central Manchester NHS
Foundation Trust University Hospitals, Manchester, UK
M. John, I. Ahmad and D. Miller
Case report
Guys and St Thomas NHS Foundation Trust, London, UK
Between 2006 and 2012, I managed a series of patients with difcult or impossible face-mask ventilation, including maxillary
carcinoma, rhabdomyosarcoma of the face, neurobromatosis
of the face, giant rhinopyma of the nose, and severe post-burn
neck contracture, where a binasopharyngeal airway (BNPA) was
successfully used for preoxygenation and safe induction of anaesthesia and to maintain spontaneous or controlled ventilation,
or both, in anaesthetized patients while a denitive airway was
secured with or without bre-optic guidance. The BNPA was prepared using two nasopharyngeal airways, one of 7 mm inner
diameter and the other of 6 mm inner diameter, with connectors
of 7 and 6 mm inner diameter tracheal tubes attached at the
patient end. These were further connected to the Y-shaped connector of a double-lumen tracheal tube to form an assembly.
With adequate pharmacological preparation of the nasal passages, the BNPA was introduced under local anaesthesia. The
breathing circuit was then attached to the airway, and anaesthesia was induced with sevourane or propofol. BagBNPA ventilation was done with the mouth manually occluded by a one-hand
technique. Subsequently, the trachea was secured under direct
laryngoscopy or bre-optic guidance.
Passive regurgitation during anaesthesia may lead to pulmonary
aspiration, which is associated with increased morbidity and
mortality. The application of positive end-expiratory pressure
(PEEP) in order to lessen the risk when using supraglottic airways
is largely unknown. We assessed the impact of PEEP on the performance of different supraglottic airway devices using a simulated passive regurgitation airway model.
Discussion
The present case series described management of seven patients
with impossible face-mask seal or ventilation, or both. The lack of
patient cooperation precluded the option of awake tracheal intubation. Furthermore, with a poor face-mask seal, the options
of induction by inhalation (via face mask) or using i.v. sedative
hypnotic while maintaining spontaneous ventilation to assist
bre-optic techniques were not without risk. In these patients, I
used the BNPA as a dedicated airway for the maintenance of airway patency while other major airway interventions were anticipated or were in progress. The BPNA allowed airway access for
direct laryngoscopy and orotracheal intubation. In instances of
poor vocal cord view, it facilitated bre-optic-assisted orotracheal
intubation while ventilation and oxygenation were in progress.
Unlike other supraglottic airways, the BNPA was easily tolerated
by the awake subjects under local anaesthesia. Oral and nasal
suction was possible. Gastric dilatation was not signicant, and
Methods
Silicone impressions from male cadavers and computed tomography in live male patients were used to reconstruct the
oesophagus, trachea, and pharyngeal airway shapes by computer modelling and then produced by means of a threedimensional printer using a exible thermoplastic elastomer.
A lung-compliance reservoir bag was connected to the trachea,
and a stop-cock controlled the ow of simulated gastric uid
between a water chamber and the oesophagus. The pressure
change during a 500 ml regurgitation was from 10 to 2 cm H2O
pressure. The simulated 500 ml regurgitation was emptied into
the replica oesophagus under gravity via the stop-cock, whilst
a suitably compliant reservoir bag representing the lungs was
ventilated using different supraglottic airway devices. The volume that entered the lungs was then measured, and the mean
of three consecutive values was taken as the nal measurement. Pressure-control ventilation was applied using ination
pressures of 13 cm H2O at a rate of 12 bpm, and measurements
were made with and without the application of 5 cm H2O PEEP.
A cuff pressure of 60 cm H 2 O was set for the supraglottic airways with an inatable cuff.
Results
Table 2 shows the mean volume in millilitres () of the xed
500 ml of simulated gastric uid that entered the lungs.
Discussion
The application of PEEP consistently reduced the volume aspirated into the lungs of the model for all the devices tested.
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
Binasopharyngeal airway: a useful dedicated
airway device in both elective and emergency
difcult or impossible face-mask ventilation
scenarios
gastric contents could be evacuated while ventilation proceded.
The case series demonstrated the BNPA to be a valuable alternative to a face mask in patients with impossible mask seal and an
alternative approach to intubation for patients in whom the use
of another supraglottic device is contraindicated. It provides access to the oral airway for direct laryngoscopy, video laryngoscopy, and bre-optic and laryngeal mask airway insertion. The
BNPA was also used to rescue patients in the cannot intubate,
cannot ventilate scenario.
Abstracts
| 5
Panel 1
Panel 3
Panel 4
Panel 5
Fig 2
These results indicate that application of PEEP improves supraglottic device performance in preventing aspiration from passive
regurgitation. These observations can be explained by an appreciation of how liquid ows down pressure gradients. Given that
regurgitation is accompanied by an increased pressure in the oesophagus, and liquid will only ow down a pressure gradient, the
application of PEEP will oppose this ow into the airway. We recognize that our model has limitations and that real-life airways
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
Panel 2
| Abstracts
Table 2 Mean volume in millilitres () of the xed 500 ml of
simulated gastric uid that entered the lungs with four different
supraglottic devices
Conditions
cLMA
ILMA
i-GeL
Proseal
No PEEP (0 cm H2O)
PEEP (5 cm H2O)
476 (23)
326 (12)
380 (0)
297 (6)
263 (21)
93 (12)
46 (14)
12 (3)
Reference
1. Ramachandran SK, Kumar AM. Respir Care 2014; 59: 92031
Comparison of the A.P. AdvanceTM Video
Laryngoscope and C-MAC Video Laryngoscope
with the Macintosh 3 Blade for intubation of the
difcult airway: a manikin study
O. Davies, E. Kourteli, M. Cecconi, D. Garewel and F. Mir
St Georges Hospital, London, UK
The use of video laryngoscopes has increased signicantly in recent years. We compared the Macintosh 3 blade, against the AP
Advance (APA VLS), which has a guide channel and foregoes
the need for a stylet, and also against the C-MAC VLS, which is
non-channelled. On the manikin, we simulated three difcult
airway scenarios.
Results
The results are shown in Table 3. There was no dental damage,
and the majority of intubations with APA were achieved at the
rst attempt (18 of 20), with two attempts for the remainder (2
of 20).
Discussion
In the difcult laryngoscopy scenario, the time to intubate was
shortest with the CMAC-3 and longest with the CMAC-D. In the
two scenarios of tongue swelling and manual in-line stabilization, the APA 3 had the shortest times. Overall, the longer time
to intubation was statistically signicant with the CMAC-D. Interestingly, VLS size 3 blades performed better than D blades. This
could simplify our airway strategy if we focus on using the
video laryngoscopes with their standard blades until more evidence is gathered. Consistent with previous studies,1 2 viewing
of the vocal cords did not equate to speed of intubation.
References
1. Byhahn C, Iber T, Zacharowski K, Weber CF, Ruesseler M,
Schalk R, Meininger D. Minerva Anestesiol 2010; 76: 57783
2. Aziz MF, Dillman D, Fu R, Brambrink AM. Anesthesiology 2012;
116: 62936
The badge for assessment of difcult grade
airway examination (BADGE) tool for airway
assessment
V. Mistry and P. Jefferson
Methods
Warwick Hospital, South Warwickshire NHS Foundation
Trust, Warwick, UK
On a Trucorp manikin, we simulated a difcult airway attributable to CormackLehane grade 3 laryngoscopy, a difcult airway
attributable to manual in-line stabilization, and lastly, a difcult
airway attributable to tongue swelling (20 ml air used in the tongue of the manikin). Anaesthetic colleagues were asked to perform intubation in all three scenarios using MAC 3, APA and
CMAC with standard and difcult airway (D) blades. Timings
A thorough airway assessment will allow identication of predicted difcult airways and consequent airway management. It
is common for anaesthetists to equate the 6.5 cm cut-off of the
thyromental distance (Patil test) as three ngerbreadths. However, several studies have shown that there is high variation between individuals, and the mean three ngerbreadth distance is
only 5.9 cm, therefore lowering the predictive value of the test.1 2
Table 3 Comparison of intubation times using MAC 3, CMAC and APA laryngoscopes. APA 3, AP Advance size 3; APA DAB, AP Advance
difcult airway blade; CMAC 3, CMAC size 3 blade; CMAC D, CMAC difcult airway blade; IQR, interquartile range; MAC, Macintosh Blade.
*P<0.05. Study blade faster than MAC. The P-values refer to the comparison with the MAC Blade
Difcult airway (grade 3 laryngoscopy)
Time [s; median (IQR)]
P-value
Tongue swelling
Time [s; median (IQR)]
P-value
Mannual inline immobilization
Time [s; median (IQR)]
P-value
MAC 3
APA 3
APA DAB
CMAC 3
CMAC D
19 (2915)
28.75
15 (1118)
0.006*
15 (1419)
0.0927
13 (1020)
0.0258*
42 (3560)
0.0043*
14 (1022)
11 (916)
0.6308
14 (1017)
0.4552
16 (1024)
0.6528
40 (2853)
0.0005
35 (1544)
14 (1116)
0.0002*
15 (1220)
0.004*
21 (1431)
0.948
44 (3481)
0.0038*
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
have greater tissue exibility and variability, which will favourably inuence supraglottic airway seating and seal. A better
seal is likely to lower aspiration risk, so the absolute results
may not accurately indicate performance. But we may conclude
that the consistent benecial effect of PEEP in decreasing aspiration risk is a reliable observation and so is a denite benet.
were recorded for viewing of the vocal cords, number of attempts,
use of bougie, and dental damage. Data were analysed with Wilcoxon paired t-test (for time of intubation).
Abstracts
Thyromental distance
Grade I
Wilson score
Grade II
Risk factors
Weight
0
1
2
< 90 kg
90110 kg
> 110 kg
Head and neck
Above 90
Movement
1
2
0
1
2
Above 90 (i.e. 10)
Below 80
IG > 5 cm or Slux > 0
IG < 5 cm and Slux = 0
IG < 5 cm and Slux < 0
0
1
2
Normal
Moderate
Severe
0
1
2
Normal
Moderate
Severe
Jaw movement
Grade IV
Grade III
Levels
Receding
Mandible
Buck teeth
Fig 3
Another test used in airway assessment is the inter-incisor gap,
which allows identication for intubation and laryngeal mask
airway insertion; an inter-incisor gap of >2.5 cm will allow laryngeal mask airway insertion, and >3.0 cm is required for traditional intubation. In addition, it forms part of the Wilson assessment
for predicting difcult airway, where the cut-off is 5 cm.
Methods
We created a tool the size of the hospital badge swipe card that
includes measurements for airway assessments (Fig. 3). Patil originally used a gauge for measurement, whilst other methods
include radiographs, rulers, and obviously, the three ngerbreadths. We chose a ruler because this increased sensitivity
three-fold and is the easiest to use with a swipe card.1 The length
of the card incorporates a modied ruler 08.5 cm, with colour
coding for important cut-offs for the thyromental distance. The
width of the card is marked 05.5 cm with colour coding for important cut-offs for the inter-incisor gap of airway assessment.
The centre of the card can be modied to include the Mallampati
class and or the Wilsons score assessments.
Discussion
We chose the combination of thyromental distance, Mallampati
class, and Wilson score to feature on the card because this combination of tests gives the greatest sensitivity for predicting difcult intubations.3 We conclude that use of the BADGE tool as a
stand-alone card or sticker for the reverse of swipe cards will
aid novice and senior anaesthetists in performing an accurate
airway assessment. We invite anaesthetists and anaesthetic departments to use the BADGE tool.
References
1. Baker PA, Depuydt A, Thompson JMD. Anaesthesia 2009; 64:
87882
2. Kiser M, Wakim JA, Hill L. AANA J 2011; 79: 158
3. Shiga T, Wajima Z, Inoue T, Sakamoto A. Anesthesiology 2005;
103: 42937
Inter- and intra-rater reliability of the Fremantle
score: a validated method of describing video
laryngoscopy
R. Ramadas1, A. Swann2, J. English3 and E. OLoughlin3
1
Princess Margaret Hospital, Subiaco, Australia, 2Fiona
Stanley Hospital, Murdoch, Australia, and 3Fremantle
Hospital, Fremantle, Australia
Direct laryngoscopy is commonly described using the Cormack
Lehane score. Since the advent of video laryngoscopy, the same
score has been used, but because of the different positioning of
the camera, the view obtained by video laryngoscpy may not accurately reect the ease of intubation. To enable a more useful
description of video laryngoscopy1 and intubation, the Fremantle
score2 was described. This is a system incorporating view, ease of
intubation, and the device/blade. The aim of this study was to
compare the inter- and intra-rater reliability of scoring using
the Fremantle score compared with the CormackLehane score
during video laryngoscopy.
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
Inter-incisor gap
Mallampati class
| 7
| Abstracts
Methods
Results
Seventy-four people scored the videos. A total of 4440 scores were
collected and analysed. When compared with the gold standard,
the Fremantle score was more accurately scored by the raters
(74%) compared with CormackLehane (65%; P<0.05). Comparing
the intra-rater reliability of the scoring systems, both methods
were comparable in reproducibility over time by the same
individuals (P>0.05).
Discussion
Improvements in technology, such as the inux of video laryngoscopes, should lead to improvements in patient care. This new
method shows that the Fremantle score is a more reproducible
system than the CormackLehane score, conveying more instructive information about intubations using video laryngoscopy. This takes into account some of the frustrations of video
laryngoscopy in order to improve the transfer of information.
We recommend that this validated method of documentation
of video laryngoscopy be used when using these devices.
References
1. Ahmed-Nusrath A, Gao-Smith F. Anaesthesia 2011; 66: 86872
2. Swann AD, English JD, OLoughlin EJ. Anaesth Intensive Care
2012; 40: 697701
Apnoeic mass movement oxygenation
for glottic stenosis surgery
D. Falzon1 and D. Ball2
1
NHS Lothian, Edinburgh, UK, and 2NHS Dumfries and
Galloway, Dumfries, UK
Respiratory gas exchange requires delivery of oxygen and removal of carbon dioxide from the alveoli. These are usually
coupled, but oxygenation can be achieved without ventilation
(CO2 clearance) by apnoeic mass movement oxygenation
(AMMO). We report use of this technique for surgical treatment
of glottic stenosis in two patients.
Table 4 Patient B: arterial blood gas values (in kilopascals)
Time
Fractional inspired
oxygen
H+ (mmol litre1)
Arterial partial
pressure of CO2
Arterial partial
pressure of O2
14.30 14.34 14.46 14.52 15.01 15.04
0.21 1.0
37.2
6.3
45.7
7.6
57.5
10.0
60.3
10.7
69.2
12.8
72.4
13.1
10.8
55.9
50.8
44.9
50.8
53.2
(Ravussin 13 gauge). To this, we attached a three-way tap,
which was connected to a Manujet ventilator at one end and oxygen tubing at the other. Oxygen was then insufated at 4 litre
min1. Denitrogenation of the lungs was achieved by spontaneous breathing with a face mask (fractional inspired oxygen=1.0).
Anaesthesia was given with propofol and remifentanil infusions;
mivacurium was used for neuromuscular block. One attempt at
jet ventilation at 1 bar was performed to ensure that this was possible if needed. Throughout the procedure, a patent expiratory
pathway was always maintained. After the surgery, a laryngeal
mask airway was inserted. For Patient A, intermittent measurement of capnography was attempted by addition of a sampling
tube to the assembly, but ow resistance prevented this. For Patient B, the arterial partial pressure of CO2 (PaCO2 ) was measured
by arterial blood gas analysis.
Results
Apnoea times were 48 (Patient A) and 34 min (Patient B). Patient A
did not have PaCO2 concentrations measured, but when ventilation was established the end-tidal CO2 measured via capnography through the laryngeal mask airway was recorded as
8.5 kPa. Results from serial arterial blood gases from Patient B
are shown in Table 4. There were no cardiovascular problems recorded. Each patient made a good recovery.
Discussion
Apnoeic mass movement oxygenation prevents hypoxia provided lung nitrogen is rst cleared and the patients airway is sufciently patent and receives insufated oxygen.1 This is used in
brainstem death tests.2 Carbon dioxide is not cleared; the main
effects are sympathetic stimulation3 with coma at high CO2. Neither complicated our management. We chose AMMO for the following three reasons: any form of transglottic airway would
preclude surgery; it does not require high volume ow across
the stenosis (risking barotrauma); and there is no movement of
the surgical eld. We conclude that AMMO is a reasonable method for selected patients provided the expiratory pathway can
cope with the insufated ow. Extending safe apnoea time
with AMMO could be used for airway management in patients
with an acceptable expiratory pathway.
References
Methods
Institutional and patient consent to report was granted. Each patient (A and B; with no evidence of airway obstruction at rest) had
glottic stenosis needing elective laser reduction. For each, a cannula cricothyroidotomy was performed under local anaesthesia
1. Frumin MJ, Epstein RM, Cohen G. Anesthesiology 1959; 20:
78998
2. Stepehn JM, Zisfein J. Arch Neurol 1990; 47: 10668
3. Kolettas A, Grosomanidis V, Fyntanidou B, et al. The Greek
E-Journal of Perioperative Medicine 2010; 8: 7083
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
De-identied video clips were made of intubations using a CMAC
size 3 blade. A panel of airway enthusiasts reviewed the videos to
provide a gold standard for comparison. Videos of inadequate
quality or those in which there was no consensus achieved by
the panel using either the CormackLehane or the Fremantle
score were removed. The approved 25 original and ve repeat videos were then arranged in a random order. This presentation was
then shown to critical care doctors in two centres in Australia,
after a standardized education programme about scoring of
laryngoscopy. They scored the videos using the CormackLehane
and the Fremantle scores. Statistical analysis of intra- and interrater reliability was undertaken. Ethics approval for the study and
consent from the patients were gained.
Abstracts
| 9
Use of high-ow nasal oxygen to facilitate
awake bre-optic intubation in hypoxic
respiratory failure
Early airway obstruction secondary to abnormal
irrigation uid extravasation during shoulder
arthroscopy
N. Tweed, C. Lynch and C. Janakiraman
I. Davis1 and N. Jones2
University Hospital Wales, Cardiff, UK
Case report
A 56-yr-old woman with a history of oropharyngeal carcinoma,
treated 8 yr ago with surgical resection and radiotherapy, presented with a community-acquired pneumonia, sepsis, and hypoxic respiratory failure. Airway assessment showed one
ngerwidth mouth opening, minimal neck extension, and a Mallampati grade 4. With high-ow face-mask oxygen, she maintained peripheral oxygen saturation of 90%, which reduced
rapidly if this was removed. We used a high-ow nasal oxygen
system, Optiow, to improve and maintain oxygenation during
an awake oral bre-optic intubation.
Discussion
The Optiow was set up in 10 min without previous experience, and with 10 min of use improved the patients peripheral
oxygen saturation to 98%. Using topical lidocaine and a spray
as you go approach, the patient was successfully intubated without sedation. The Optiow device was used continuously during the procedure, maintaining peripheral oxygen saturations at
98% throughout. Despite the requirement of the patient to open
her mouth during AFOI, most of the mechanisms improving
gas exchange could still be expected to be active,3 and this
could explain the maintenance of good oxygenation throughout
the process of intubation.
Case report
A 53-yr-old, otherwise healthy, 65 kg, 165 cm woman presented
for arthroscopic release of right adhesive capsulitis (frozen
shoulder). General anaesthesia was induced via i.v. fentanyl
and propofol and maintained by sevourane in an oxygen and
air mixture, with positive pressure ventilation via a laryngeal
mask airway. Within 5 min of commencement of the irrigation
uid via the arthroscopic port, it was noticed that the right trapezius muscle was swollen and tense, coinciding simultaneously
with elevated airway pressures, and subsequent difculty in ventilating manually. The operation was discontinued, and examination revealed right-sided neck swelling, with tracheal deviation
to the contralateral side (Fig. 4). A cuffed oral tracheal tube was
placed in light of the difculty in ventilating and the risk of impending total airway obstruction.
Laryngoscopy revealed a partly visible glottis deviated to the
left. An urgent chest radiograph excluded tension pneumothorax
and conrmed the tracheal deviation. An ultrasound scan revealed that the neck swelling had an echogenicity consistent
with uid. The patient was transferred ventilated to the intensive
care unit and uneventfully extubated 5 h later. An oupatient
magnetic resonance arthogram with contrast was performed
and demonstrated an abnormal communication between the
glenohumeral joint and supraspinatus. The consensus opinion
of the radiology and orthopaedic teams is that this could explain
the rapid accumulation of uid in the neck and resulting airway
obstruction.
Summary
This hypoxic patient with a known difcult airway was safely
managed with an AFOI. In the authors opinion, this was made
safer with the use of high-ow nasal oxygen, which improved
oxygenation sufciently to allow a controlled AFOI to be performed, and it was demonstrated that this could be achieved
with no formal training in the use of the Optiow device.
References
1. Parke RL, McGuinness SP, Eccleston ML. Respir Care 2011; 56:
26570
2. Lucangelo U, Vassalo F, Marras E, et al. Crit Care Res Pract 2012;
506382
3. Dysart K, Miller T, Wolfson M, et al. Respir Med 2009; 103: 14005
Fig 4
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
The gold-standard approach to anticipated difcult intubation is
the awake bre-optic intubation (AFOI). However, this approach
may be complicated in the event of high oxygen demand,
owing to the difculty of maintaining adequate oxygenation because traditional methods of maintaining high inspired oxygen
concentration require full face masks. The use of high-ow
nasal oxygen has been shown to be of benet in hypoxic intensive therapy unit patients,1 and its use has been reported to
maintain oxygenation during bronchoscopy.2 The authors are
not aware of any previous case reports of its use in AFOI.
Guys Hospital, London, UK, and 2Basingstoke Hospital,
Basingstoke, UK
10 |
Abstracts
Discussion
Discussion
High-pressure-source ventilation ( jet ventilation) may be delivered to a patient using a number of different techniques ranging
from suspension laryngoscopes to transtracheal catheters. In a
number of individuals, distortion of the upper airway prevents
passive expiration. Traditionally, such patients have necessitated abandonment of surgery, insertion of large-bore transcricoid cannulas, or tracheostomy to allow adequate ventilation.
The Ventrain is a single-use ventilation device capable of delivering low-airway-pressure ventilation via a catheter of internal
diameter 2 mm in patients with upper airway obstruction.1 Expiratory ventilatory assistance actively removes gas from the
lungs during the expiratory phase, allowing capnometry and preventing barotrauma and cardiovascular compromise.2
Declaration of interest
References
1. Yoshimura E, Yano T, Ichinose K, Ushijima K. J Anesth 2005; 19:
3257
2. Blumenthal S, Nadig M, Gerber C, Borgeat A. Anesthesiology
2003; 99: 14556
3. Orebaugh SL. Anesthesiology 2003; 99: 14568
Use of the Ventrain in a patient with complete
upper airway obstruction preventing expiration
during high-frequency jet ventilation
A. Fearnley, S. Badiger, R. Oakley and I. Ahmad
Guys and St Thomas NHS Foundation Trust, London, UK
The success of high-pressure-source ventilation is dependent
upon upper airway patency to facilitate passive expiration and
prevent increasing intrathoracic pressure and its associated deleterious sequelae. Distortions in airway anatomy may make passive expiration inadequate or impossible. We describe the use of
the Ventrain device (Dolphys Medical BV, Eindhoven, The Netherlands) to provide ventilation in a clinical setting of upper airway
obstruction in a patient with post-radiation brosis that prevented passive expiration during attempted high-pressuresource ventilation.
Case report
A 58-yr-old man with a previous history of squamous cell carcinoma of the right vocal cord and anterior commissure presented
for a second attempt at laser excision of symptomatic postradiotherapy supraglottic stenosis. Surgery was abandoned
4 weeks previously because of inadequate expiration during
high-frequency jet ventilation attempted via both a subglotically
placed catheter and the suspension laryngoscope. On returning
to theatre, nasal awake bre-optic intubation was performed.
Seeking to avoid wide-bore subglottic cannulation, a 2.0 mm internal diameter Cricath cannula (Dolphys Medical BV) was inserted through the cricothyroid membrane after withdrawal of
the nasal tracheal tube. Ventilation was then commenced using
the Ventrain device. Laser release of laryngeal brosis was
None declared.
Acknowledgements
This abstract is submitted with the full written informed consent
of the patient.
References
1. Hamaekers AEW, Borg PAJ, Enk D. Br J Anaesth 2012; 108:
101721
2. Borg PAJ, Hamaekers AEW, Lacko M, Jansen J, Enk D. Br J
Anaesth 2012; 109: 8334
Bioprinting of human airway using
three-dimensional printing: a concept
for predicting difcult airway
F. Mir1, K. Andi1, E. Kourteli1, A. Patel2 and B. Liban1
1
St Georges Hospital, London, UK, and 2Royal National
Throat, Nose and Ear Hospital, London, UK
Bioprinting, or the process of printing simulated human tissues
through three-dimensional (3D) printers, is a highly researched
area of technological innovation. Three-dimensional printing
has expanded recently to allow printing and fabrication of body
parts using a range of materials from soft hydrogels over polymer
melts to harder materials, such as ceramics and metals.1 In a
clinical setting, patient computed tomography scans are used
to create stereolithography (STL) le formats to print solid 3D
models, which can then be used as templates for clinical needs.
Case report
We report a pilot case study for a known difcult airway in a patient who had surgery for maxillofacial trauma. The 3D model of
the patients airway from the oropharynx to the subglottis was
constructed and printed using his computed tomography
images. The facial tissues were constructed with low-density silicone material. Multiple anaesthetists attempted bre-optic intubation on the model to identify and compare the difculties
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
In the literature, case reports of airway oedema or tracheal compression, deviation, or both as a cause of airway obstruction during shoulder arthroscopy consistently implicate prolonged
surgery and the resultant increased volumes of irrigation uid
administered.1 2 3 In these patients, the earliest onset of airway
compromise was 85 min from commencement of surgery. The
present patient is unusual because of the rapidity of onset of airway obstruction. The likely culprit appears to be abnormal anatomy, providing a potential path for the irrigation uid from the
glenohumeral joint to the infraspinous fossa, and subsequently,
the neck. The authors wish to draw attention to this rare complication of shoulder arthroscopy and recommend vigilance in
checking the neck for swelling at regular intervals, especially
pre-extubation after prolonged procedures, where injudicious removal of a tracheal tube may be met with total airway obstruction. Subsequent ventilation via face mask or supraglottic
airway device may not be possible because of the distorted anatomy, nor may subsequent tracheal intubation or cricothyroid access be possible.
performed for a period of 60 min thereafter, with saturations
maintained at 100% and capnography indicating an end-tidal
CO2 of 5.46.0 kPa.
Abstracts
Discussion
The technique of 3D printing is essentially the deposition of material in three dimensions using pressure. The core materials
used can range from a viscous paste to liquids, and are deposited
using syringes moving in three dimensions.1 Air or mechanical
pressure applied to the syringe deposits the material for the
length of movement and time the pressure is applied. Parallel
strands are deposited in multiple layers. The direction is changed
for each layer, producing a mesh with varied mechanical properties and porosity dened by the settings. The design of the interior of the object will strongly affect its mechanical properties,
which may be changed to mimic the type of tissue it is replacing
or supporting.
Reference
1. Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. Int J Comp
Assist Radiol Surg 2010; 5: 335341
Laryngeal mask airway utility in the
interhospital transport of neonatal patients
with difcult airway: a literature review
K. Thompson, R. Ramadas and S. Resnick
Princess Margaret Hospital, Subiaco, Australia
When combined with congenital airway abnormalities, neonatal
tracheal intubation can prove difcult, requiring subspecialist
airway expert intervention. The laryngeal mask airway (LMA)
has been used as an adjunct in the management of inpatient neonatal difcult airways. The Newborn Emergency Transport Service (NETS) team in Western Australia covers one of the largest
transport areas in the world, transporting unwell infants from
rural health-care facilities to the tertiary neonatal centres in
Perth. The equipment bag contains a size 1 LMA, but this has
not been used by our transport team. We aimed to review the literature to ascertain whether LMAs have been used during the
transport of infants with a difcult airway.
Methods
A search was conducted using Medline, Embase, CINAHL,
PubMed, and Cochrane databases, using search terms including
(neonatal OR newborn OR inborn), (retrieval OR transport), and
(laryngeal OR LMA). Cross-referencing was conducted to maximize yield.
Results
Seventy-six papers were identied; 61 duplications and irrelevant (adult, animal, non-LMA) papers were removed. The remaining 15 papers were read. These included at least ve case
reports of LMAs being used in infants during transfer to tertiary
health care, including those with congenital airway conditions
and those with normal anatomy but a cannot intubate, cannot
oxygenate situation. One case report described an infant with
unplanned extubation during transport, with excellent recovery
after placement of an LMA and continued ventilation via LMA.
In another, an infant deteriorated during helicopter transport
and did not have adequate clinical response to face-mask ventilation. An LMA was used to good effect in this situation. Two of
the case reports described ventilation failure via LMA in infants.
A mannequin study measuring LMA cuff pressure at altitude demonstrated cuff pressures that became elevated to above those
recommended by the manufacturer when at altitude. One
paper suggested that although the LMA has a role in the resuscitation of the infant, tracheal intubation ought to be undertaken
before transport because of difculty in securing an LMA during
movement.
Discussion
While concerns have been raised regarding LMA cuff pressure at
altitude and regarding difculty in securing an LMA during transport, several case reports describe successful transport of infants
with or without abnormal anatomy using an LMA. While tracheal
intubation remains the gold-standard method of securing an airway, the LMA may be useful to the neonatal transport team in the
rare case of cannot intubate, cannot oxygenate or difcult airway in infants.
References
1. Trevisanuto D, Verghese C, Doglioni N, Ferrarese P, Zanardo V.
Pediatrics 2005; 115: e10911
2. Brimacombe JR, De Maio B. J Clin Anesth 1995; 7: 68990
3. Wilson GD, Sitting SE, Schears GJ. J Emerg Med 2008; 34: 171
Randomized comparison trial among I-gelTM,
LMA-ProSealTM, and tracheal intubation with
manual in-line stabilization in simulated
cervical spine-injured patients with rigid
cervical collar immobilization
P. Engsusophon
King Chulalongkorn Memorial Hospital, Bangkok, Thailand
Supraglottic airway devices have a role in difcult airway management and have proved to be easy for new users. Although
the tracheal intubation with manual in-line stabilization (TTMILS) is the standard management for patients with cervical
spine injury, it is not practical for inexperienced personnel.
This study compared the airway management by i-gel, LMAProSeal, and TT-MILS in anaesthetized, paralysed patients with
simulated difcult airway with a rigid cervical collar.
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
encountered with those documented in the anaesthetic chart. A
prospective pilot study is now underway to identify whether potential problems with intubation and face-mask ventilation as
documented in the anaesthetic chart can be predicted using 3D
models, which would then become valuable adjuncts for planning the most appropriate anaesthetic technique. With this, we
aim to have an accurate 3D model of the patients airway,
which can be used before surgery to help plan an airway strategy.
It may be possible to identify one or more components of a difcult airway, such as distorted anatomy, anticipated difcult
laryngoscopy, or difcult bre-optic endoscopy. Furthermore, it
could be used for patient-specic simulation for teaching. The
model can be made from materials of differing consistency to
allow for variations in different tissues, such as the tongue and
cartilages, such that it reects the density of live tissues and
also allowing for bagmask ventilation in dynamic conditions.
| 11
12 |
Abstracts
Methods
Table 5 Comparison of the Intubation difculty score (IDS),
visual analogue score (VAS) and time to intubate between
groups. Values are median (25th 75th percentile) or mean ()
The patients who were to undergo supercial surgery requiring
general anesthesia were recruited and randomized into three
groups as follows; i-gel, LMA-ProSeal, and TT-MILS. The patients
and assessors were blinded. The primary outcome was time to
successful ventilation. Other measurements were insertion attempts, positive leak pressure, bre-optic-assessed glottic view,
and intraoperative and postoperative complications.
Macintosh
(n=53)
McGrath MAC McGrath MAC P-value
direct (n=53)
indirect
(n=52)
IDS
0.10 (0.101.5) 0.10 (0.101.0) 1.0 (0.103.0) 0.001
VAS
2.0 (1.03.3)
2.0 (1.03.9)
3.0 (2.04.4)
0.01
Time (s) 37.2 (8.7)
42.3 (24.2)
43.8 (19.8)
0.12
Results
Conclusion
The i-gel had a shorter insertion time compared with the LMAProSeal and TT-MILS. Regarding concerns of lower leak pressure,
the i-gel might provide a reasonable alternative to the LMAProSeal and TT-MILS in patients with reduced neck movement
and limited mouth opening.
References
1. Theiler LG, Kleine-Brueggeney M, Kaiser D, et al. Anesthesiology
2009; 111: 5562
2. Uppal V, Fletcher G, Kinsella J. Br J Anaesth 2009; 102: 2648
A randomized controlled trial comparing the
ease of tracheal intubation using a McGrath
MAC laryngoscope and a standard Macintosh
laryngoscope
L. Foulds, C. Wallace, G. McLeod and B. McGuire
Methods
Ethical approval for this single-blinded, randomized controlled
trial was obtained from the Tayside Regional Ethics Committee.
A total of 158 patients who consented were randomized to one
of three groups. All patients were anaesthetized by one of ve investigators, and a standard anaesthetic technique was used. The
intubation difculty scale (IDS) was used to evaluate the ease of
intubation; this is a numerical score that summates values for
seven variables associated with difcult intubation.2 A score of
0 indicates easy intubation, 15 indicates slight difculty, and
>5 indicates moderate to major difculty. Secondary outcomes
included the anaesthetists perception of intubation difculty
[expressed using a visual analog scale (VAS)], time taken to intubate successfully, and incidence of complications.
Results
There was no difference in baseline characteristics between groups.
Recorded results can be seen in Table 5 [the values shown are median (25th75th percentile) for IDS and VAS, and mean () for time].
All patients were intubated with the originally allocated laryngoscope, and no complications were recorded in any group.
Discussion
The McGrath MAC performed less well as a direct laryngoscope
when compared with the traditional Macintosh laryngoscope.
However, when used as an indirect or video laryngoscope, it
was comparable with the Macintosh. The familiarity of the
McGrath MAC design, coupled with the educational advantages
of the video screen for shared viewing, make this laryngoscope
well suited to everyday use in both routine and difcult intubations. However, it is important that the clinician is aware of its
limitations as a direct laryngoscope, especially when it is being
used to train novice anaesthetists.
NHS Tayside, Dundee, UK
The rst video laryngoscope became available in 2001. Since
then, we have seen a proliferation of devices appearing on the
market. Many of these devices have an acutely curved blade,
and therefore, require a different insertion technique to the traditional Macintosh laryngoscope and a rigid device to aid tracheal
tube placement. In contrast, the McGrath MAC (Aircraft Medical
Ltd, Edinburgh, UK) combines the familiarity of the Macintoshstyle blade with video laryngoscopy technology, allowing both
direct and indirect viewing. Publications such as the Difcult Airway Society ADEPT guidance1 encourage clinicians to provide
evidence to justify acquisition of novel airway devices. This
study was designed to determine the efcacy and safety of the
McGrath MAC as both a direct and an indirect laryngoscope,
when compared with the Macintosh laryngoscope.
References
1. Pandit JJ, Popat MT, Cook TM, et al. Anaesthesia 2011; 66: 72637
2. Adnet F, Borron SW, Racine SX, et al. Anaesthesiology 1997; 87:
12907
Clinical evaluation of C-Mac D-Blade video
laryngoscope: randomized comparison with
C-Mac Blade and direct laryngoscopy
V. Hostic1, B. Maldini1, Z. Novotny1 and I. Hodzovic2
1
University Hospital Centre Sestre milosrdnice, Zagreb,
Croatia, and 2Cardiff University and Aneurin Bevan
University Health Board, Cardiff, UK
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
Twenty patients were assigned to each group. Times to successful ventilation were not statistically different [i-gel 43.01 (26.94)
sec.; LMA-ProSeal 50.05 (45.73) sec.; and TT-MILS 68.43 (46.69)
sec.; P=0.113]. The success rate for the i-gel was 90% at the rst attempt and 10% at the second attempt vs LMA-ProSeal, 95% at the
rst attempt and 5% at the second attempt (P=0.536). The positive
leak pressure was signicantly higher in the LMA-ProSeal group
than i-gel group [25.55 (3.01) vs 23.35 (3.31) cms H2O; P=0.035].
The glottic views were not statistically different between groups.
The incidence of sore throat and odynophagia was signicantly
lower in the i-gel and LMA-ProSeal groups compared with the
TT-MILS group (P=0.000 and P=0.017, respectively).
Abstracts
Table 6 Main study ndings. Values are median [range] and
mean (), as appropriate. n=140
D-blade
(n=48)
DL
(n=40)
P-value
0 [04]
0 [05]
1 [04] =0.015
98 (7)
4.9 (1.6)
74 (35)
7.1 (4.2)
59 (45)
9.2 (5.8)
<0.001
<0.042
13.6 (6.2)
9.5 (3.3)
9.1 (3.7)
<0.001
18.5 (6.8)
16.6 (5.7)
18.3 (8.1)
2. Cavus E, Neumann T, Doerges V, et al. Anesth Analg 2011; 112:
3825
Differential rates of complications with the
ProSeal laryngeal mask airway in Asian and
non-Asian populations and according to
method of size selection: a meta-analysis
of studies
T. Cook1, A. Robles1 and K. Cheema2
1
NS
Royal United Hospital, Bath, UK, and 2The Quality
Observatory, NHS South East Coast, Horley, UK
Having observed a possible increase in minor complications in
studies of the ProSeal laryngeal mask airway (PLMA) in Asian populations, we performed a systematic review and meta-analysis
to explore this.
C-Mac D-Blade is a recently introduced extension to the existing
C-Mac video laryngoscope system. We could nd no studies
evaluating the two video laryngoscope blades against direct
laryngoscopy (DL). We performed randomized comparison of
the C-Mac D-Blade, C-Mac, and DL using seven-point intubation
difculty scores1 as our primary outcome measure.
Methods
After approval by the University Medical Centre ethics committee, 140 patients undergoing general anaesthesia with tracheal
intubation were invited to take part in the study. Patients with
predicted difcult airway were excluded. We recorded success
rate, time to glottic view, time to tube placement, total time to intubation, ( percentage of glottic opening)2 score, and seven-point
intubation difculty scale.1 Failure of the procedure was declared
if intubation was not successful after 120 s or if arterial oxygen
saturation decreased to <90%. Intubations were recorded using
the C-MAC system. We used SPSS version 20 to analyse the
data, as follows: one-way ANOVA for continuous data, Kruskall
Wallis test for ordinal data, and 2 test for categorical data.
Results
The study enrolled 140 patients with mean () age 58 (17) yr and
BMI 27 (4) kg m2 throughout a period of 9 months.
Two failures were recorded; one with the C-MAC blade and
one in the DL group. In both instances, intubation was unsuccessful after multiple attempts requiring longer than 120 s. The
D-blade was used successfully as a rescue device in both patients.
Discussion
The results of this study suggest that despite statistical differences, there is little clinical benet that the D-Blade or C-Mac
blade provides over conventional DL in patients with normal airways. The success of the D-blade as a rescue device in our study
suggests that the D-blade could be benetial in patients with difcult airways.2
References
1. Adnet F, Borron SW, Racine SX, et al. Anesthesiology 1997; 87:
12907
Methods
Articles were searched from Medline and EMBASE using the following keywords: ProSeal, PLMA, ProSeal laryngeal mask,
weight-based, and gender-based. The articles were scrutinized
and separately assigned to non-Asian and Asian studies. Each
study was further subdivided according to whether size selection
was gender based, weight based, or mixed. Data were extracted
relating to rst time insertion success, overall insertion success,
trauma as indicated by the presence of blood on PLMA removal,
sore throat within 8 h, sore throat within 848 h, sore throat at
any time, and oropharyngeal seal pressure. Statistical signicance was calculated using the 2 test. The effect size for each
measure in all comparison groups was calculated and expressed
as Cohens d. The signicance for oropharyngeal seal pressure
was calculated using a t-test.
Results
We included 24 studies (1549 participants) in an Asian population
and 26 studies (2043 participants) in the non-Asian population.
All groups had >100 patients. The non-Asian participants were
taller and heavier than the Asian participants (166.4 vs 161.3 cm
and 73.0 vs 61.3 kg, respectively). Oropharyngeal leak pressure
did not differ between populations. Mucosal injury was more
common in the Asian participants (20 vs 9%, P<0.001) while
sore throat at 848 h was less common (8 vs 18%, P<0.001). In
the Asian studies, PLMA size selection by weight rather than gender was associated with a lower rate of mucosal injury (12 vs 30%,
P=0.001), sore throat in 848 h (7 vs 18%, P<0.001), but not sore
throat at <8 h (10 vs 0%, P<0.001). In the non-Asian participants,
rates of complications did not differ according to size selection
technique.
Discussion
In the non-Asian population, use of a weight-based or genderbased size selection policy has little impact on performance or
complications. However, in the Asian population use of a
weight-based size selection policy reduces mucosal injury and
later (but not early) sore throat. This is the rst study we are
aware of exploring differential performance of airway devices
in different ethnic populations and may have implications for
other devices.
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
Intubation
difculty scale
POGO score (%)
Time to glottic
view (s)
Time to tube
placement (s)
Total time to
intubation (s)
C-MAC
(n=52)
| 13
14 |
Abstracts
Comparison of two supraglottic airway devices,
the i-gel airway and the ProSeal laryngeal mask
airway, in non-paralysed anaesthetized
patients
A. Jain1, A. Luthra2, I. Bhukal2 and I. Bala2
1
Manchester Royal Inrmary, Central Manchester NHS
Foundation Trust University Hospitals, Manchester, UK, and
2
Postgraduate Institute of Medical Education and Research,
Chandigarh, India
Methods
Results
First attempt and overall insertion success were similar (PLMA,
85 and 100%; i-gel 80 and 100%, respectively). Mean () insertion times were similar [PLMA, 27.40 (11.51) s; i-gel 25.45 (9.03)
s]. Mean oropharyngeal leak pressure was 3.5 cm H2O higher
with the PLMA (P<0.012). The passage of an orogastric tube
through the i-gel airway was easy in all 20 patients of the i-gel
group, whereas it was passed with ease in only 12 patients of
the PLMA group. It was impossible to pass the orogastric tube
in three patients of the PLMA group. Grade I glottic view ( full
view of the vocal cords) was visible in 17 (85%) patients who
were managed with i-gel, whereas only nine (45%) patients
had a Grade I view in the PLMA group. Insertion of the PLMA
and i-gel is similarly easy, but the PLMA forms a more effective
seal for ventilation.
Discussion
Both PLMA and i-gel can be inserted easily and rapidly. The
time required for insertion is similar, but the PLMA forms
a better seal. However, the i-gel is better positioned over
the laryngeal framework and the oesophagus. The i-gel allows
easier passage of an orogastric tube through its drain
channel than the PLMA. The incidence of intraoperative complications is similar; however, the incidence and severity of
postoperative sore throat and hoarseness of voice is higher
with the PLMA.
References
1. Brimacombe J, Keller C, Fullekrug B, et al. Anaesthesiology 2002;
96: 28995
2. Brimacombe J, Keller C, Brimacombe L. Anaesth Analg 2002; 95:
7706
J. Keegan, S. Baker, R. Egglestone, R. Montgomery
and A. Ginn
Dorset County Hospital NHS Foundation Trust, Dorchester,
UK
It is universally accepted that advanced knowledge and warning
of patients with difcult airways can be crucial to safe airway
management.1 2 For clinical and legal reasons, it is important effectively to inform, communicate, and document an episode of
difculty with the airway.1 3 There are a range of ways to impart
this information; little is known, however, about the referral patterns of anaesthetists after identication and management of a
difcult airway within the UK. Twelve years ago, Ball and colleagues1 published their proposed Airway Alert, which has been
available for all hospitals electronically via the Difcult Airway
Society website.
Methods
We have developed and modied Dr Balls Airway Alert letter
with his full support and permission so that it is multifunctional.
A combined letter, sticker, and patient information card (threein-one) system, which is eye catching, easily seen by patients
and staff, within clinical notes, and on anaesthetic charts. A
patient survey was performed on this new proposed system.
Available airway alert systems were reviewed and a regional
questionnaire performed to establish how post-FRCA anaesthetists document, communicate, and follow up patients with difcult airways. The questionnaire nished in September 2014 and
was similar to that published in Anaesthesia 2003, which was
sent to college tutors only. We will present our ndings at the
DAS Conference.
Results
The triple system proposed has been accepted by Dorset County
Hospital Foundation Trust for clinical use. Our patient survey indicated that 100% of potential patients with an average age of
55 yr (38% male and 62% female) thought that the credit card
system was clear and effective in its aims. They thought it
would be easily visible and less likely to be lost. Suggestions included printing information and laminating the cards. Our review into the current databases and registry were similar to
those of the New Zealand group.2 They are not linked and do
not automatically lead to a single source of information. They
often require signicant input from both clinician and patient,
usually with a fee.
Discussion
We wish to propose this standardized Airway Alert system to the
Difcult Airway Society for consideration. In addition, we suggest
that a customized Airway Alert UK difcult airway/intubation
registry should be established in line with other registries, such
as the Organ Donation register, which is free and easily accessible
24 h a day. It is our responsibility to ensure that communication
of information relating to patients with difcult airways is readily
available and guaranteed to future carers.
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
In a randomized, non-crossover study, we tested the hypothesis
that the ease of insertion and efcacy of seal as measured by oropharyngeal leak pressure differ between the i-gel airway and the
ProSeal laryngeal mask airway (PLMA) in non-paralysed anaesthetized subjects. Forty patients in the age group 1865 yr were
studied. Insertion success rate, insertion time, and oropharyngeal leak pressure were measured. The intraoperative orogastric
tube insertion success rate, view of the glottis using bre-optic
laryngoscopy, airway reactions during insertion, and postoperative complications associated with the two devices were
also compared.
Airway alerts: time to modernize how
anaesthetists in the UK disseminate difcult
airway information
Abstracts
References
1. Barron FA, Ball DR, Jefferson P, Norrie J. Anaesthesia 2003; 58:
5085
2. Baker P, Moore C, Hopley L, Herzer K, Mark LJ. Anaesth Intensive
Care 2013; 41: 334341
3. WA State Coroner. Available from www.safetyandquality.
health.wa.gov.au/docs/mortality_review/inquest_nding/
rasmussen_nding.pdf (accessed 7 September 2014)
| 15
likely to improve the management of this situation. We introduced labels on the cannula packages stating Adult, Child,
and Baby (13G, 14G, and 16G, respectively) in order to reduce
delay and selection error. We advocate this modication to be
made by all departments in order to improve the management
of a CICV scenario. We also advocate that the manufacturers
modify their packaging to incorporate the clear labels on the
front of the packaging.
Reference
Reducing human error during needle
cricothyrodotomy
Royal Berkshire Hospital NHS Trust, Reading, UK
Methods
During anaesthetic simulation sessions for anaesthetists and
operating department practitioners (ODPs), incorrect cannula
sizes were frequently selected for needle cricothyroidotomy
during cannot intubate, cannot ventilate (CICV) scenarios. An
additional observation was the time taken to select the appropriate cannula size. We therefore simulated a CICV scenario
for 13 ODPs, who were asked to set up and connect the Manujet
system. They were also asked to select the appropriate cannula
size. The cannulas used in Royal Berkshire Hospital are Ravussen cannulas; 13G for adults, 14G for children, and 16G for
infants.
Results
Nine of 13 ODPs were unfamiliar with the Manujet system, and 12
of 13 ODPs selected the incorrect cannula size. These results led
to our institution of clear labels on the cannula packages stating
Adult, Child, and Baby for the various sized cannulas (13G,
14G, and 16G, respectively) in order to reduce delay and selection
error. It also led to a regular 6 monthly training programme for
theatre staff.
Discussion
The ASA and the Difcult Airway Society have strict guidelines
for managing unanticipated difcult intubation. The nal section in both algorithms ends with the CICV scenario. As this is
a rare occurrence, with an estimated incidence of 0.012 in
10 000 patients, it is challenging to maintain the skills for its
management. During a CICV situation, rapid establishment of
a means of oxygenation is essential to reduce morbidity and
mortality. It is therefore a requirement for anaesthetists to be
competent in managing this rare but serious emergency and
to be familiar with the equipment required. Anaesthetists,
ODPs, and anaesthetic nurses regularly go through simulated
sessions on these rare emergencies in order to maintain their
ability to manage this situation competently and remain familiar with the equipment. In addition to training, it would be essential to have strict processes in place in order to reduce the
risk, errors, and failure attributable to equipment and human
factors. For this reason, departments have clearly labelled difcult airway trolleys and anaphylaxis packs. Regular teaching
is essential, but aids to reduce or eliminate human error are
National survey of anaesthetic departmental
responses to NAP4: 1. dissemination of NAP4,
airway leads, departmental organization,
and governance
T. Cook1, N. Woodall2 and C. Frerk3
1
Royal United Hospital, Bath, UK, 2Norfolk and Norwich
Hospital, Norwich, UK, and 3Northampton General Hospital,
Northampton, UK
NAP41 made recommendations to improve practice, including
introduction of departmental airway leads.2
Methods
A survey was sent to all UK NHS hospitals to determine
current airway practices and changes relevant to NAP4 recommendations. After reminders, the survey was closed in January
2014.
Results
There were 175 responses from 192 hospitals (61.5% returns).
Results are presented as the percentage of respondents. Respondents were as follows: airway lead, 88%; clinical director,
9%; and tutor, 4%. Of all respondents, 99.4% were aware of
NAP4 and its results, including reading original papers (61%),
reading the report online (54%), and hospital presentation
(35%). Respondents reported an average 3.1 exposures to results, and 98% reported this as satisfactory. NAP4 results
were presented in 91% of departments. Overall, 95% of respondents reported changes in practice in response to NAP4 in their
anaesthetic department, and 97% reported changes in anaesthesia, intensive care, or emergency department practice. Reported changes to departmental practice were as follows: not
at all, 2%; a little, 32%; more than a little, 35%; considerably,
28%; and dramatically, 3%. Of all respondents, 95% reported
having a departmental airway lead and 4% planned one; 44%
changed in response to NAP4. Roles included protocol development (88%), procurement (87%), and multidisciplinary training
(89%); these roles changed in 50% in response to NAP4. Of the
departments, 71% have representation on hospital procurement committees, and in 5% this changed in response to
NAP4. Forty-nine per cent report a systematic method for ensuring clinicians competence with new airway equipment,
and in 14% this changed in response to NAP4. Airway management training includes human factors training in 61% of
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
T. Ali, F. Idrees and G. Dix
1. Heard AMB, Green RJ, Eakins P. Anaesthesia 2009; 64: 6018
16 |
Abstracts
departments, and in 24% this changed in response to NAP4. In
65%, multidisciplinary teams who manage difcult airways
train together, and in 26% this changed in response to NAP4.
Of respondents, 79% reported that airway management plans
are always or often discussed during the World Health Organization check before anaesthesia; 79% always or often; and in
28% this changed in response to NAP4. Debrieng after difcult
airway management occurs more commonly in 66% of departments than before NAP4.
Thirty-ve (30%) responders indicated involvement in more
than one CICV scenario.
Notable outcomes
(i) Adverse outcome was seen in one in four patients with a CICV
scenario (fatal in one in six).
Discussion
Acknowledgements
Thanks to those responding and RCoA staff who supported the
survey.
References
1. Cook TM, Woodall N, Frerk C. Br J Anaesth 2011; 106: 61731
2. Cook TM, Woodall N, Frerk C, et al. Bulletin of the Royal College of
Anaesthetists 2012; 76: 378
One hundred and sixteen heads better than one
in a crisis? Corporate experience of the cannot
intubate, cannot ventilate scenario: results of a
survey of the membership of the Difcult
Airway Society
Fig 5
(ii) The CICV scenario was resolved in 42% of patients by front of
neck (FoN) access to the airway. Four methods of FoN airway were
equally popular.
J. Mackenzie
Royal Berkshire Hospital, Reading, UK
Method
The 2700 members of Difcult Airway Society (DAS) were invited
to dene their experience of the cannot intubate, cannot ventilate (CICV) scenario via a Web-based survey containing 25
questions.
Findings
Select nature of responders?
Fourteen per cent of DAS (362 members) replied, mainly consultants with set lists, in post on average for 8.4 yr. Mean caseload
was 442 cases annually. Logbooks or theatre records were the
source of data for 78%. Of the respondents, 95% carry out 300 or
more cases each year, of which 90% are general anaesthetics
(GAs). One-third of these GAs include tracheal intubation,
which was undertaken urgently in one-quarter (equivalent to
8% of all GAs).
Sixty per cent of responders had never witnessed a CICV
event, including three mature anaesthetists with clinical experience totalling 94 yr. One hundred and sixteen (4% of all DAS)
reported experience of CICV, usually as senior participant.
Fig 6
Consultant surgeons and consultant anaesthetists made FoN
interventions with equal frequency. Surgical trainees seem less
likely than trainee anaesthetists to attempt FoN access to the
airway.
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
NAP4 was successfully disseminated and has changed practice in
almost all UK hospitals. Gaps in care quality have been reduced
but not closedin departmental organization, presence of airway leads, and communication around airway difculty or
complications.
Abstracts
| 17
(iii) Neuromuscular block (NMB) was present in 70% of patient at
the time of the event.
Fig 9
Fig 10
Fig 8
Discussion
(iv) At the time of the CICV event, NMB was absent or incomplete
in 33 of 103 patients. Neuromuscular blocking agent was given to
10 of these 33 patients, but was unhelpful in 50% of these previously unrelaxed patients.
Only 14% of DAS members took part in the survey. Most anaesthetists will never witness the rapidly deteriorating clinical situation that culminates in the CICV scenario. The fact that 86% of
DAS members did not respond may have been because of their
lack of experience of CICV. The above ndings reveal how past
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
Fig 7
18 |
Abstracts
instances of CICV have been managed, and suggest that prompt
formation of a FoN airway could generate a good outcome. Although 10 unparalysed patients is a small number on which to
base practice, the observation that giving a neuromuscular blocking agent did not help in 50% could be seen as reecting the similar nding that giving an NMB does not always improve the
efciency of bagvalvemask ventilation.
Table 7 Results
Correct understanding of phrase
Yes (%)
No (%)
Cannot intubate
Cannot ventilate
Cannot intubate or ventilate
71.1
63.2
68.4
28.9
36.8
31.6
Acknowledgements
Reference
1. Goodwin MWP, Pandit JJ, Hames K, Popat M, Yentis SM.
Anaesthesia 2003; 58: 603
Survey of knowledge of airway emergencies
in non-anaesthetic theatre staff
H. Brown and L. Beckmann
Royal Brisbane and Womens Hospital, Brisbane, Queensland,
Australia
An unanticipated difcult airway is an anaesthetic emergency,
which can result in morbidity and even mortality. The NAP4
study identied difcult or delayed intubation, failed intubation,
and cannot intubate, cannot ventilate (CICV) accounting for 39%
of all events during anaesthesia.1 Anaesthetists and anaesthetic
operating department practitioners are familiar with the Difcult
Airway Society guidelines for these airway emergencies and usually have many opportunities in their training to practise these
scenarios in simulations. However, in reality airway emergencies
require the wider support of all theatre staff to help prevent harm
coming to the patient.
airway emergencies and whether they were able to identify simple airway adjuncts.
Results
When asked how many difcult airway trolleys were located,
guesses ranged from zero to ve; 47.4% were correct in saying
that there were three difcult airway trolleys, and 78.9% were
able to determine correctly the location of at least one difcult
airway trolley. Although 92.1% were able to identify a tracheal
tube and laryngeal mask airway correctly, the results were less
positive for a CMAC (video laryngoscope) and emergency cricothyroidotomy kit, with only 42.1 and 65.8%, respectively, identifying them correctly.
Discussion
Teamwork is essential in the emergency setting, especially in an
airway crisis. NAP4 noted that among the human factors most
frequently identied as being poor in an airway emergency
were poor communication, teamwork, leadership, and task xation.1 It has been shown that regular training of skills, either
manikin or simulation based, backed with theoretical knowledge
is vital to having a positive outcome in an airway emergency. The
main aim of this study was to determine the extent of knowledge
of non-anaesthetic staff in the theatre setting and therefore highlight areas that needed to be addressed in future teaching sessions and simulations. The study received positive feedback,
with staff members keen to learn and participate in unexpected
airway emergencies.2 Having already completed one teaching
session, there are plans for more with theatre simulations. It
has highlighted the need for continued education to all theatre
staff and for ongoing sessions about equipment and team
communication.
Methods
We surveyed 38 members of non-anaesthetic theatre staff (theatre nurses, recovery nurses, and theatre support ofcers) at
the Royal Brisbane and Womens Hospital with the aim of assessing their level of understanding of anaesthetic airway emergencies. Questions were posed on their knowledge of different
References
1. Mellanby E, Podmore BM, McNarry AF. J Perioper Pract 2014; 24:
1127
2. Cook TM, Woodall N, Frerk C; Fourth National Audit. Br J
Anaesth 2011; 106: 617631
Downloaded from http://bja.oxfordjournals.org/ at UNIVERSITY OF LJUBLJANA on November 29, 2015
This survey was conceived at DAS 2012 when Professor Pandit
reminded the audience of his 2001 nding that giving a neuromuscular blocking agent to 30 anaesthetized subjects did not
improve the overall efciency of bagvalvemask ventilation. Inspired and expired tidal volumes were measured before and after
NMB; some improved and some deteriorated, with no overall
change.1
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Variable Bleeding Manifestations Characterize Different Types of Surgery in Patients With Severe Factor XI Deficiency Enabling Parsimonious Use of Replacement Therapy Salomon2006Document4 pagesVariable Bleeding Manifestations Characterize Different Types of Surgery in Patients With Severe Factor XI Deficiency Enabling Parsimonious Use of Replacement Therapy Salomon2006Eugenio Daniel Martinez HurtadoNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- IE Visualisation Platform Brochure 496951001 V01 1113Document7 pagesIE Visualisation Platform Brochure 496951001 V01 1113Eugenio Daniel Martinez HurtadoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Mallampati 0 2001Document3 pagesMallampati 0 2001Eugenio Daniel Martinez HurtadoNo ratings yet
- Obstetric Difficult Airway Guidelines - Difficult Airway Society 2015Document9 pagesObstetric Difficult Airway Guidelines - Difficult Airway Society 2015Eugenio Daniel Martinez HurtadoNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Validation of Modified Mallampati Test With Addition of Thyromental Distance and Sternomental Distance To Predict Difficult Endotracheal Intubation in AdultsDocument5 pagesValidation of Modified Mallampati Test With Addition of Thyromental Distance and Sternomental Distance To Predict Difficult Endotracheal Intubation in AdultsEugenio Daniel Martinez HurtadoNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Equipment To ManaEquipment To Manage A Difficult Airway During Anaesthesiage A Difficult Airway During Anaesthesia Anaesth Intens Care 20100567Document19 pagesEquipment To ManaEquipment To Manage A Difficult Airway During Anaesthesiage A Difficult Airway During Anaesthesia Anaesth Intens Care 20100567Eugenio Daniel Martinez HurtadoNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- US in AirwayDocument7 pagesUS in AirwayEugenio Daniel Martinez HurtadoNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Appendix 1 Occupational Therapy Bathing-Showering ToolDocument3 pagesAppendix 1 Occupational Therapy Bathing-Showering ToolNizam lotfiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- OutlineDocument2 pagesOutlineAnnisaNurlatifaFNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Movement DisordersDocument18 pagesMovement DisordersFaisal BudisasmitaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hordeolum - Background, Pathophysiology, EpidemiologyDocument6 pagesHordeolum - Background, Pathophysiology, EpidemiologyKeren SingamNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Effects of Isotretinoin On Meibomian GlandsDocument6 pagesEffects of Isotretinoin On Meibomian GlandsTeddyNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Clinic Handbook of GastroenterologyDocument285 pagesClinic Handbook of Gastroenterologyansarijaved100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Physical Exam, Review of Systems, and ReportsDocument2 pagesThe Physical Exam, Review of Systems, and ReportsJuan DeSantosNo ratings yet
- Implementing Rules and RegulationsDocument3 pagesImplementing Rules and RegulationsVincent De VeraNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Developmental Dysplasia of The Hip: Dr. Bassel El-Osta SPR Trauma & OrthopaedicsDocument71 pagesDevelopmental Dysplasia of The Hip: Dr. Bassel El-Osta SPR Trauma & OrthopaedicsvadimmadanNo ratings yet
- 41 Prep GuideDocument73 pages41 Prep Guidedaljit chahalNo ratings yet
- Slides 6 - ObturationDocument22 pagesSlides 6 - Obturationبراءة أحمد السلاماتNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Hayat Ullah: Nurse (BSN Generic)Document1 pageHayat Ullah: Nurse (BSN Generic)Shafiq Ur RahmanNo ratings yet
- 9 The Post Anesthesia Care UnitDocument77 pages9 The Post Anesthesia Care Unitsanjivdas100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Glaucoma Surgery - Open Angle GlaucomaDocument155 pagesGlaucoma Surgery - Open Angle GlaucomaWilsonNo ratings yet
- American Society For Reproductive MedicineDocument3 pagesAmerican Society For Reproductive MedicineShanti Natalia NababanNo ratings yet
- ADR Reporting FormDocument2 pagesADR Reporting FormApoorva Tatti100% (1)
- Assessment of Knowledge of Public On Coronary Artery Disease, Hypertension and Diabetes MellitusDocument5 pagesAssessment of Knowledge of Public On Coronary Artery Disease, Hypertension and Diabetes MellitusMythili MuthappaNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Porcelain Fused To Metal (PFM) Crowns and Caries in Adjacent TeetDocument5 pagesPorcelain Fused To Metal (PFM) Crowns and Caries in Adjacent Teetbaiq rengganis dewiNo ratings yet
- UntitledDocument33 pagesUntitledapi-257817850No ratings yet
- Approached in Diagnosis of AnemiaDocument41 pagesApproached in Diagnosis of AnemiaAlqodri SetiawanNo ratings yet
- Nursing ReportsDocument13 pagesNursing ReportsNorhidayatNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Volunteering and Health Literature ReviewDocument38 pagesVolunteering and Health Literature ReviewNCVO100% (1)
- Protocol Deviation Tracking Log Ver2!07!17-2015Document3 pagesProtocol Deviation Tracking Log Ver2!07!17-2015Kesava Sumanth ANo ratings yet
- Countercoup Skull FracturesDocument5 pagesCountercoup Skull FracturesVinay KumarNo ratings yet
- Application (30 Points) :: and Monitoring Schedule For The Next Year Based On The Results From The Outside ReviewDocument7 pagesApplication (30 Points) :: and Monitoring Schedule For The Next Year Based On The Results From The Outside Reviewijaz afzalNo ratings yet
- Hospital Services Physical Expansion Plan (Hosp .Masterplan) - DR .MaarofDocument44 pagesHospital Services Physical Expansion Plan (Hosp .Masterplan) - DR .MaarofCharlene Ordoñez Dela CruzNo ratings yet
- Literacy and ReadabilityDocument16 pagesLiteracy and ReadabilityPao Parel100% (2)
- PDF SMR OperationDocument64 pagesPDF SMR OperationRizqulloh Taufiqul Hakim BarsahNo ratings yet
- Hepatitis in Children: DR Hamza BawumiaDocument36 pagesHepatitis in Children: DR Hamza BawumiaHamza BawumiaNo ratings yet
- Rift Valley FeverDocument9 pagesRift Valley Feverapi-390015550No ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)