Professional Documents
Culture Documents
Semj 17 03 36286 PDF
Uploaded by
Rosyta VelayantiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Semj 17 03 36286 PDF
Uploaded by
Rosyta VelayantiCopyright:
Available Formats
Shiraz E-Med J. 2016 March; 17(3):e36286.
doi: 10.17795/semj36286.
Published online 2016 March 27.
Research Article
The Effects of Lidocaine and Mefenamic Acid on Post-Episiotomy Pain:
A Comparative Study
Masoumeh Delaram,1,* Lobat Jafar Zadeh,2 and Sahand Shams3
1
Faculty of Nursing and Midwifery, Shahrekord University of Medical Sciences, Shahrekord, IR Iran
Faculty of Medicine, Shahrekord University of Medical Sciences, Shahrekord, IR Iran
Faculty of Veterinary Medicine, Shahrekord University, Shahrekord, IR Iran
2
3
*
Corresponding author: Masoumeh Delaram, Faculty of Nursing and Midwifery, Shahrekord University of Medical Sciences, Shahrekord, IR Iran. Tel: +98-3813335648, Fax:
+98-3813346714, E-mail: masoumehdelaram@yahoo.com
Received 2016 January 13; Revised 2016 February 29; Accepted 2016 March 04.
Abstract
Background: Most women suffer pain following an episiotomy and oral non-steroidal anti-inflammatory drugs are commonly used
for pain relief. Due to the gastrointestinal side effects of oral drugs, it seems that women are more accepting of topical medications
for pain relief.
Objectives: Therefore, the aim of this study was to compare the effects of lidocaine and mefenamic acid on post-episiotomy pain.
Patients and Methods: This clinical trial was carried out in 2011. It involved sixty women with singleton pregnancy who were given
an episiotomy at 38 to 42 weeks of gestation. The participants were randomly divided into two groups. One group received 2% lidocaine cream (n = 30), while the other group received 250 mg of mefenamic acid (n = 30). The data were collected via a questionnaire
and a visual analog scale. Pain intensity was compared from the first complaint by the mother and at 6, 12, and 24 hours after the
delivery in both groups. The data were analyzed using SPSS (version 16), the t-test, and the paired t-test, and a P value of less than
0.05 was considered significant.
Results: The mean intensity of pain at the first compliant was 4.92 1.9 in the lidocaine group and 4.90 1.5 in the mefenamic acid
group, and the difference was not statistically significant (P = 0.20). Additionally, there was no significant difference in the mean
intensity of post-episiotomy pain between the two groups at 6 (P = 0.05), 12 (P = 0.36), and 24 (P = 0.98) hours after childbirth.
Conclusions: The effects of the lidocaine cream and mefenamic acid were similar in terms of the relief of post-episiotomy pain.
Lidocaine cream therefore represents a good alternative to mefenamic acid, which is commonly used to reduce pain following an
episiotomy, especially in women who are breastfeeding and who wish to avoid oral analgesic drugs being secreted in their milk.
Keywords: Lidocaine, Mefenamic Acid, Post-Episiotomy Pain
1. Background
Episiotomy is a common surgical procedure that is performed during childbirth, although little evidence supports its routine use (1, 2). At least 35 45% of women
in developing countries who give birth in a hospital setting are given an episiotomy (3). The perineal pain experienced due to receiving an episiotomy is severe during
the first few days after delivery, and it can lead to limitations in movement and difficulties with urination and
defecation (2). Studies have also shown that episiotomyrelated pain may affect sexual contact (4). Different pharmacological methods are commonly used for the relief of
perineal pain following an episiotomy, including aspirincodeine, acetaminophen-codeine, sodium diclofenac, and
non-steroidal anti-inflammatory drugs (NSAIDS). The nonmedicinal methods applied for pain relief include cold
and heat, acupressure, acupuncture, relaxation, distraction, and music therapy (5). The use of oral analgesics is
common, although their adverse effects include constipation, nausea, abdominal pain, and dizziness, all of which
limit their use. Due to the adverse effects of oral analgesics,
topical pain relief methods have been considered, including hot and cold compresses, topical anesthetic, and radiation. Lidocaine gel is one of the local anesthetics used for
pain relief. It blocks the sensory neurons of neuronal membranes by inhibiting sodium, thereby preventing the transmission of nerve messages and the sensation of pain. Indeed, 2% lidocaine gel influences the structure of the perineal nerve through the skin or membrane (6). In obstetrics, lidocaine gel is used to anesthetize the perineum during the second stage of labor, and its benefits include less
systemic absorption and increased ease of administration
(7). In terms of the effect of lidocaine on post-episiotomy
pain, previous studies have reported conflicting results.
For example, one study reported that the severity of the
perineal pain in the group that received lignocaine gel in
Copyright 2016, Shiraz University of Medical Sciences. This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0
International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the
original work is properly cited.
Delaram M et al.
the first 48 hours after childbirth was less than that in the
group that received a placebo (7). However, another study
reported opposite results (8).
Non-steroidal anti-inflammatory drugs are analgesic
agents that are commonly used worldwide, and their effectiveness in the treatment of acute pain has previously been
studied (9). Such drugs inhibit the oxygenase cycle and reduce the production of prostaglandins (10). Their physiological effects involve protecting the gastric mucosa, regulating the renal blood flow, and setting the tone of the vascular endothelium (11). They also play an important role
in inflammation, although the mechanism of this action
has not yet been fully explained (12). Mefenamic acid is
one of the NSAIDS used for the relief of pain following an
episiotomy. It is more commonly used in the treatment of
primary dysmenorrhea, headache, toothache, and postoperative pain. It has been suggested that mefenamic acid
should not be taken for more than seven days. The typical
adult dose is 500 mg three times a day, although the dose
is different for children. After ingestion, mefenamic acid
is rapidly absorbed and it has a short half-life of approximately 2 hours (9). A review of four studies that involved
a total of 842 people reported that the degree of pain experienced after receiving 500 mg of mefenamic acid was
reduced in 50% of patients, whereas the pain reduction
was 20% in the group that received a placebo (13). Little
research has previously been conducted comparing the effects of lidocaine and mefenamic acid in reducing the perineal pain experienced after an episiotomy.
2. Objectives
Since no prior study has compared the effects of lidocaine cream and mefenamic acid on post-episiotomy
pain in primiparous women, this study was carried out
to compare the impact of the two methods of pain relief on episiotomy-related pain in a teaching hospital in
Shahrekord, Iran.
3. Patients and Methods
This study involved a randomized controlled trial that
was conducted from February 2011 to December 2011 at the
antenatal clinic and post-delivery ward of Hajar hospital, a
university hospital and referral center for obstetric care in
Shahrekord, Iran. Permission to conduct the study was received from the deputy of research and the ethics board of
Shahrekord University of Medical Sciences (code of ethics:
90-4-9). The study also received a clinical trial code from
the Iranian registry of clinical trials (IRCT201104253078N7).
During the study period, a total of 420 women who gave
2
birth at Hajar hospital experienced perineal trauma during childbirth that required repair. Some 280 of those
women gave written informed consent to take part in the
study and 118 of them were found to be potentially eligible to participate. Of those, 58 women were excluded from
the study, while 60 women who underwent a normal vaginal delivery and mediolateral episiotomy, and who met
the inclusion criteria, were selected by convenience sampling. They were randomly allocated into the two groups.
One group (n = 30) received 250 mg of mefenamic acid,
while the other group (n = 30) received 2% lidocaine cream
(Figure 1). The randomization was performed according to
a random number table. The exclusion criteria included
women who had a postpartum hemorrhage, manual removal of the placenta, severe asthma, gastric or duodenal
ulcer, and preeclampsia. Women with a known sensitivity to non-steroidal anti-inflammatory drugs, a laceration
of the perineum, an episiotomy longer than 5 cm, and an
adverse reaction to local anesthetics were also excluded.
The participants received written and verbal information
about the study at 37 weeks at the antenatal clinic and
they were given the same information on admission to the
postnatal ward by the ward midwife. All participants who
agreed with the study procedures and volunteered to participate signed the free and informed consent form. Neither the women nor the investigators could be blinded to
the purpose of the study, although the individual responsible for data analysis was blinded.
After the birth and at the time of admission to the
post-delivery ward, the intensity of the perineal pain was
assessed by the ward midwife using a visual analog scale
(VAS) at the time of first complaint by the women and prior
to them taking the first dose of their allocated medication. Then, 250 mg of mefenamic acid was administered
to the patients in the first group, while the patients in the
second group received 5 ml of 2% lidocaine cream on the
episiotomy line. The topical lidocaine cream was manufactured by the Tehran Chemie Pharmaceutical Company
(Tehran, Iran) and each 100 g of the cream contained 2.5 g
of lidocaine and 2.5 g of prilocaine. The mefenamic acid
was manufactured by the Raha Pharmaceutical Company
(Esfahan, Iran). The drugs were available in the hospital
pharmacy. Socio demographic information was provided
by the patient records. The visual analog scale asked the
women to score their pain from 0 = no pain to 10 = worst
possible pain (5). The primary outcomes were pain scores
at 6, 12, and 24 hours after birth and with rest. The secondary outcomes relating to pain were the frequency of
use of the allocated medication, use of additional analgesia, time from birth to first analgesia, dosing intervals, and
any adverse effects of the therapeutic medications. The
data were analyzed using SPSS (version 16). The categoriShiraz E-Med J. 2016; 17(3):e36286.
Delaram M et al.
Gave Birth at Hajar's Hospital and Had Perineal
Trauma Requiring Reparing (n = 420)
Gave Written Informed Consent (n = 280)
Eligible for Taking Part in the Trial (n = 118)
Providing Meeting Inclusion Criteria (n = 60)
Random Allocation
Lidocaine Group (n = 30)
Analysed (n = 30)
Mefenamic Acid Group (n = 30)
Excluded the Study Due to:
1.Not Experiencing the Perineal Pain (n = 28)
2. Postpartum Hemmorrhage (n = 6)
3. Manual Removal of Placenta (n = 3)
4. severe Asthma (n = 2)
5. Gastric or Duodenal Ulcer (n=3)
6. Preeclampsia (n = 4)
7. Sensitivity to Anti-inflammatory Drugs (n = 2)
8. laceration of Perineum(n = 6)
9. length of Episiotomy Larger than 5 cm (n = 3)
10. Adverse Reaction to a Local Anesthetics (n = 1)
Analysed (n = 30)
Figure 1. Flowchart of the Study Protocol
cal variables were compared using the 2 and Fishers exact
tests, while the continuous variables as measured on the
visual analog scale were compared using the independent
samples t-test. A P value of less than 0.05 was considered
to be statistically significant with a confidence interval of
95%. The individual responsible for analyzing the data was
blinded to the treatment groups.
4. Results
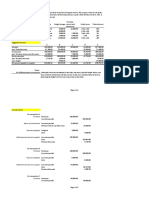
The two groups were well balanced in terms of their
demographic characteristics upon entry into the study, as
well as their labor and birth outcomes (Table 1). The study
outcome data were available for 100% of the women at 6,
12, and 24 hours after birth. A comparison of the mean intensity of pain in the two groups is presented in (Table 2),
which shows that there is no statistically significant difference in the intensity of pain at the point of first compliant
following rest between the two groups (P = 0.20). Additionally, no significant difference in the intensity of pain at 6
hours after childbirth was found between the two groups
(P = 0.05). The mean intensity of the post-episiotomy pain
was also not significantly different at 12 hours after childbirth between the two groups (P = 0.36). Further, the difShiraz E-Med J. 2016; 17(3):e36286.
ference was still not significantly different at 24 hours after
childbirth between the two groups. There was no significant difference in the incidence of using the medications
during the 24 hours after delivery (P = 0.98), receiving additional analgesic for pain relief, and the time from birth to
the first additional analgesia (Table 3). No adverse effects of
the therapeutic drugs were reported in the two groups.
The mean birth weight was 3071 439 g in the group
that received lidocaine and 3016 419 g in the group that
received mefenamic acid, and the difference was not significant (P = 0.62). No significant difference was found in
the Apgar score at 1 minute after birth and upon admission
to the neonatal intensive care unit (NICU). The mean frequency of drug use was 3.20 1.9 in the lidocaine group
and 3.22 1.7 in the mefenamic acid group, and again the
difference was not significant (P = 0.40). No adverse effects
of the drugs were reported.
5. Discussion
The findings of the present study showed that both lidocaine cream and mefenamic acid were able to reduce
the severity of post-episiotomy pain over time, and there
was no significant difference in the intensity of pain be3
Delaram M et al.
Table 1. Demographic Characteristics of the Participantsa
Group Treatment
Lidocaine, n = 30
Mefenamic Acid, n
= 30
P Value
23.6 4.6
24.2 3.8
0.56
Demographic
characteristics
Age, y
Height, cm
160 5.2
162 4.4
0.05
Weight, kg
57.9 11.4
57.9 8.6
0.99
1.4 0.5
1.6 0.8
0.46
Parity
0.3 0.4
0.2 0.6
0.47
Gestational age
based on LMP,
week
39.4 0.59
39 0.89
0.07
Gestational age
based on
sonography, week
39.8 0.48
39.5 1
0.004
3.2 0.8
3.60.9
0.10
Abortion
Length of
episiotomy, cm
a
Values are expressed as mean SD.
Table 2. Pain Intensity at the Time of First Complaint and 6, 12, And 24 Hours After
Birth in the Two Groupsa
Group Treatment
Lidocaine
Mefenamic Acid
P Value
At first complaint of
pain
4.92 1.9
4.90 1.5
0.20
6 hours after birth
3.26 1.3
3.10 1.6
0.05
12 hours after birth
2.26 1.7
2.86 1.4
0.36
24 hours after birth
1.46 1.2
1.49 1.2
0.98
Time of assessing pain
Values are expressed as mean SD.
Table 3. Comparison of Additional Analgesia Prior to Discharge, Time From Birth to
First Additional Analgesia, and Frequency of Use of the Therapeutic Drugs Between
the Two Groupsa
Variables
Lidocaine, n = 30
Mefenamic Acid, n
= 30
P Value
Additional
analgesia prior to
discharge
11 (36)
12 (40)
0.35
Time from birth
to first additional
analgesia (h)
5.2 1.1
4.9 0.9
0.19
Frequency of use
of therapeutic
drugs (24 h)
0.84
Values are expressed as mean SD or No. (%) of women.
tween the two groups. Only a limited number of studies
have previously been conducted to compare the effects of
4
two sedative pain following an episiotomy. In this regard,
a study conducted in Ireland reported mefenamic acid and
lignocaine to have similar effects on the severity of postepisiotomy pain (14), which is consistent with our findings.
Delaram et al. cited Abedzadeh (5) when noting that lidocaine gel reduced the intensity of pain at 6 and 12 hours after administration. Another study showed that lidocaine
cream was able to reduce the severity of pain after an episiotomy within 15 minutes of delivery, although this effect was not present at 30, 60, and 90 minutes after birth
(15). Yet, in another study, although the recipients of lignocaine gel reported less pain than the placebo recipients,
the difference was only significant at 48 hours after delivery (7). Further, a study reported that lidocaine gel and a
diclofenac suppository have the same effect on episiotomy
pain relief during the first day postpartum (16). Studies
that examined the effect of mefenamic acid on dysmenorrhea reported the drug to reduce the pain in primary
dysmenorrhea (17). In a study conducted with the aim of
reducing acute pain following surgery using mefenamic
acid, the recipients reported at least 50% pain reduction
with 500 mg of mefenamic acid after 6 hours, while this
rate was 4% for the placebo group (9). The need for an additional analgesic was also lower in the group that received
mefenamic acid than in the placebo group (9). Another
study reported that the administration of 500 mg of mefenamic acid is effective in relieving moderate to severe pain
after surgery (13).
The mode of delivery (i.e., normal delivery, forceps, or
vacuum) can affect post-episiotomy pain; however, in the
present study there was no significant difference in the
mode of delivery between the two groups. A study from
Colombia reported that when forceps are used for delivery,
there is a greater need to use an analgesic to reduce pain after an episiotomy (18). The type of episiotomy can also be
effective in reducing pain. Since we only used a mediolateral episiotomy in the present study, this confounder variable did not affect the results.
Additionally, the effect of the analgesic drugs used
during labor and after giving birth could affect the outcome of the study, although there was no significant difference between the two groups in this regard. Although
the present study found no significant difference between
the effects of lidocaine cream and mefenamic acid on
post-episiotomy pain and hence determined that lidocaine
cream is a good alternative to mefenamic acid, it should
be noted that some patients may prefer the oral form of
a drug to the local form (19). Although the study did not
report any adverse effects of the utilized drugs, the potential side effects of these drugs should still be noted and the
necessary care provided.
The strengths of the present study were the random asShiraz E-Med J. 2016; 17(3):e36286.
Delaram M et al.
signment of participants to the study groups and the measuring of the side effects of the medications. The relatively
small sample size and the inability to follow the patients
and assess their pain intensity at 48 hours and during the
first week after delivery can be seen as limitations of the
present study.
5.1. Conclusion
The effects of lidocaine cream and mefenamic acid on
the relief of post-episiotomy pain were similar. Lidocaine
cream is therefore a good alternative to mefenamic acid,
which is commonly used to reduce pain following an episiotomy, especially in women who are breastfeeding and
who want to avoid oral analgesic drugs being secreted in
their milk.
Acknowledgments
This work was supported by grants from the medical
research council of Shahrekord University of Medical Sciences in Iran (grant NO.976). The authors especially wish to
thank the women who participated in the study. The study
was registered at www.clinicaltrials.gov. The protocol registration system was IRCT201104253078N7.
References
1. Nalbanski A, Nikolov A. [Routine episiotomya five year practice
at University Hospital "Majchin Dom"]. Akush Ginekol (Sofiia).
2009;48(5):114. [PubMed: 20198790].
2. Albers LL, Borders N. Minimizing genital tract trauma and related pain following spontaneous vaginal birth. J Midwifery Womens
Health. 2007;52(3):24653. doi: 10.1016/j.jmwh.2006.12.008. [PubMed:
17467591].
3. Dodd JM, Hedayati H, Pearce E, Hotham N, Crowther CA. Rectal analgesia for the relief of perineal pain after childbirth: a randomised controlled trial of diclofenac suppositories. BJOG. 2004;111(10):105964.
doi: 10.1111/j.1471-0528.2004.00156.x. [PubMed: 15383107].
4. Ejegard H, Ryding EL, Sjogren B. Sexuality after delivery with episiotomy: a long-term follow-up. Gynecol Obstet Invest. 2008;66(1):17.
doi: 10.1159/000113464. [PubMed: 18204265].
5. Delaram M, Dadkhah NK, Jafarzadeh L. Comparison of indomethacin
suppository and lidocaine cream on post-episiotomy pain: A randomized trial. Iran J Nurs Midwifery Res. 2015;20(4):4503. doi: 10.4103/17359066.160995. [PubMed: 26257799].
Shiraz E-Med J. 2016; 17(3):e36286.
6. Sakai T, Tomiyasu S, Yamada H, Ono T, Sumikawa K. Quantitative and
selective evaluation of differential sensory nerve block after transdermal lidocaine. Anesth Analg. 2004;98(1):24851. [PubMed: 14693629]
table of contents.
7. Corkill A, Lavender T, Walkinshaw SA, Alfirevic Z. Reducing postnatal
pain from perineal tears by using lignocaine gel: a double-blind randomized trial. Birth. 2001;28(1):227. [PubMed: 11264625].
8. Fyneface-Ogan S, Mato CN, Enyindah CE. Postpartum perineal pain in
primiparous women: a comparison of two local anaesthetic agents.
Niger J Med. 2006;15(1):7780. [PubMed: 16649459].
9. Moore RA, Derry S, Moore M. Single dose oral tiaprofenic acid for acute
postoperative pain in adults. Cochrane Database Syst Rev. 2009(4) doi:
10.1002/14651858.cd007542.
10. Lim SS, Tan PC, Sockalingam JK, Omar SZ. Oral celecoxib versus oral diclofenac for post-perineal repair analgesia after spontaneous vaginal
birth: a randomised trial. Aust N Z J Obstet Gynaecol. 2008;48(1):717.
doi: 10.1111/j.1479-828X.2007.00808.x. [PubMed: 18275575].
11. Aydinli B, Yildirgan MI, Ozturk G, Atamanalap SS, Polat KY, Basoglu
M, et al. The role of sildenafil citrate in the protection of gastric mucosa from nonsteroidal anti-inflammatory drug-induced damage.
Ulus Travma Acil Cerrahi Derg. 2007;13(4):26873. [PubMed: 17978907].
12. Green T, Rodriguez J, Navar LG. Augmented cyclooxygenase-2 effects
on renal function during varying states of angiotensin II. Am J Physiol
Renal Physiol. 2010;299(5):F95462. doi: 10.1152/ajprenal.00609.2009.
[PubMed: 20668099].
13. Moll R, Derry S, Moore RA, McQuay HJ. Single dose oral mefenamic
acid for acute postoperative pain in adults. Cochrane Database Syst Rev.
2011(3):CD007553. doi: 10.1002/14651858.CD007553.pub2. [PubMed:
21412904].
14. Harrison RF, Brennan M. Comparison of two formulations of lignocaine spray with mefenamic acid in the relief of post-episiotomy
pain: a placebo-controlled study. Curr Med Res Opin. 1987;10(6):3759.
doi: 10.1185/03007998709111106. [PubMed: 3552457].
15. Seckin B, Avsar F, Parlakyigit E, Aksakal O. Effects of indomethacin suppository and lidocaine pomade for the relief of post-episiotomy pain.
Int J Gynaecol Obstet. 2002;78(2):15961. [PubMed: 12175719].
16. Sharma JB, Ghosh B, Kumar P, Mittal S, Kumar S, Roy KK. Comparison
of lignocaine gel-soaked Falope rings vs rectal diclofenac suppository
for pain relief in laparoscopic sterilization. J Minim Invasive Gynecol.
2011;18(1):437. doi: 10.1016/j.jmig.2010.08.695. [PubMed: 21094099].
17. Zeraati F, Shobeiri F, Nazari M, Araghchian M, Bekhradi R. Comparative evaluation of the efficacy of herbal drugs (fennelin and vitagnus)
and mefenamic acid in the treatment of primary dysmenorrhea. Iran
J Nurs Midwifery Res. 2014;19(6):5814. [PubMed: 25558254].
18. Peter EA, Janssen PA, Grange CS, Douglas MJ. Ibuprofen versus acetaminophen with codeine for the relief of perineal pain after
childbirth: a randomized controlled trial. CMAJ. 2001;165(9):12039.
[PubMed: 11706909].
19. Harris LR, Roberts L. Treatments for irritable bowel syndrome:
patients attitudes and acceptability. BMC Complement Altern Med.
2008;8:65. doi: 10.1186/1472-6882-8-65. [PubMed: 19099570].
You might also like
- Cupping TherapyDocument8 pagesCupping TherapySaputra Hermawan GabroNo ratings yet
- Effect of Massage Therapy On Severity of Pain and Outcome of Labor in PrimiparaDocument5 pagesEffect of Massage Therapy On Severity of Pain and Outcome of Labor in PrimiparaputriNo ratings yet
- Effect of Massage Therapy On Severity of Pain andDocument5 pagesEffect of Massage Therapy On Severity of Pain andSafrina Widya HastutiNo ratings yet
- BiblioDocument6 pagesBiblioJohann Mark BagcalNo ratings yet
- 与扑热息痛联用增效Document5 pages与扑热息痛联用增效zhuangemrysNo ratings yet
- PDF IJWHR 478 PDFDocument7 pagesPDF IJWHR 478 PDFSusan HandrayaniiNo ratings yet
- The Use The Use of Metformin Is Associated With Decreased Lumbar Radiculopathy Painof Metformin Is Associated With Decreased Lumbar Rad 120613Document9 pagesThe Use The Use of Metformin Is Associated With Decreased Lumbar Radiculopathy Painof Metformin Is Associated With Decreased Lumbar Rad 120613เพียงแค่ แอนโทนี่No ratings yet
- E1252 FullDocument7 pagesE1252 FullwawanNo ratings yet
- 198-Article Text-400-2-10-20210427Document8 pages198-Article Text-400-2-10-20210427rachmatrizqaNo ratings yet
- The Effect of Benson's Muscle Relaxation Technique On Severity of Pregnancy NauseaDocument6 pagesThe Effect of Benson's Muscle Relaxation Technique On Severity of Pregnancy NauseavioletavrsNo ratings yet
- 5400-Article Text-7860-1-10-20161212Document4 pages5400-Article Text-7860-1-10-20161212Van DaoNo ratings yet
- Annotated BibliographyDocument3 pagesAnnotated BibliographyDeena MelvinNo ratings yet
- A ComparativeDocument5 pagesA ComparativedeadanandaNo ratings yet
- Isx No EffectDocument6 pagesIsx No EffectThomas Regina PutraNo ratings yet
- International Conference On Applied Science and HealthDocument6 pagesInternational Conference On Applied Science and HealthDerison MarsinovaNo ratings yet
- Qureshi 2005Document4 pagesQureshi 2005Susana BetancourtNo ratings yet
- Efecto de La Medicina Complementaria Sobre El Alivio Del Dolor y La Cicatrización de Heridas Después de Una Cesárea - Una Revisión SistemáticaDocument13 pagesEfecto de La Medicina Complementaria Sobre El Alivio Del Dolor y La Cicatrización de Heridas Después de Una Cesárea - Una Revisión SistemáticacumbredinNo ratings yet
- Septorinoplastia 2019Document7 pagesSeptorinoplastia 2019Zara DekeNo ratings yet
- A Comparison of Midazolam and Diazepam For Intravenous Sedation in DentistryDocument5 pagesA Comparison of Midazolam and Diazepam For Intravenous Sedation in DentistryGu GuuNo ratings yet
- The Effect of Bensons Muscle Relaxation Technique On Severity of Pregnancy Nausea 7528Document7 pagesThe Effect of Bensons Muscle Relaxation Technique On Severity of Pregnancy Nausea 7528Lusi YantiNo ratings yet
- Jurnal 5Document6 pagesJurnal 5Yoga RadityaNo ratings yet
- 10.1007@s00404 017 4409 6Document7 pages10.1007@s00404 017 4409 6Leonardo VellosoNo ratings yet
- Effect of Boron-Based Gel On Postpartum Episiotomy Wound Healing in Primiparous Pregnant WomenDocument9 pagesEffect of Boron-Based Gel On Postpartum Episiotomy Wound Healing in Primiparous Pregnant WomenariniNo ratings yet
- The Prophylactic Effect of Rectal Diclofenac Versus Intravenous Pethidine On Postoperative Pain After Tonsillectomy in ChildrenDocument7 pagesThe Prophylactic Effect of Rectal Diclofenac Versus Intravenous Pethidine On Postoperative Pain After Tonsillectomy in ChildrenNi Komang Suryani DewiNo ratings yet
- Clinical Effects of Fennel Essential Oil On Primary DysmenorrheaDocument5 pagesClinical Effects of Fennel Essential Oil On Primary DysmenorrheaPaulkik22No ratings yet
- JP2014 129208 PDFDocument8 pagesJP2014 129208 PDFarjun sureshNo ratings yet
- 1122 JurnalDocument6 pages1122 JurnalM Arif YudhiantoroNo ratings yet
- Comparison of Effects of Ginger, Mefenamic Acid, and Ibuprofen On Pain in Women With Primary DysmenorrheaDocument4 pagesComparison of Effects of Ginger, Mefenamic Acid, and Ibuprofen On Pain in Women With Primary DysmenorrheaRizky KurniawanNo ratings yet
- 100combined AcetaminophenDocument9 pages100combined AcetaminophenalayNo ratings yet
- AnestesiDocument17 pagesAnestesibodroNo ratings yet
- Trivedi. Post Laparascopic Treatment of Endometriosis With DYDDocument5 pagesTrivedi. Post Laparascopic Treatment of Endometriosis With DYDRuth RachmawatyNo ratings yet
- MitraDocument6 pagesMitraVan DaoNo ratings yet
- Assignment 1Document5 pagesAssignment 1maryamNo ratings yet
- Accepted Manuscript: 10.1016/j.ctcp.2016.05.014Document19 pagesAccepted Manuscript: 10.1016/j.ctcp.2016.05.014Frida RasyidNo ratings yet
- Pain Management in The Emergency Department 1Document20 pagesPain Management in The Emergency Department 1api-525378665No ratings yet
- 404 2019 Article 5260Document7 pages404 2019 Article 5260Farida SiggiNo ratings yet
- PCCM Suppl Mar 2016Document13 pagesPCCM Suppl Mar 2016Xavier AbrilNo ratings yet
- Jurnal Perineal Care Nisa PDFDocument11 pagesJurnal Perineal Care Nisa PDFNur Annisa FitriNo ratings yet
- Dr. - Nataraj - EJCM 132 1888 1893 2023Document7 pagesDr. - Nataraj - EJCM 132 1888 1893 2023vithz kNo ratings yet
- Artigo Bula - Naratriptan Is Effective and Well Tolerated in The Acute Treatment of Migraine - HeadDocument6 pagesArtigo Bula - Naratriptan Is Effective and Well Tolerated in The Acute Treatment of Migraine - HeadJackson Pereira de SaNo ratings yet
- Journal 3Document9 pagesJournal 3Suryanti SultanNo ratings yet
- Proposal For The Inclusion of Anti-Emetic Medications (For Children) in The Who Model List of Essential MedicinesDocument44 pagesProposal For The Inclusion of Anti-Emetic Medications (For Children) in The Who Model List of Essential MedicinesJennifer FaustinNo ratings yet
- Urogynecology JURNALDocument15 pagesUrogynecology JURNALFeliana ApriliaNo ratings yet
- Anes 10 3 9Document7 pagesAnes 10 3 9ema moralesNo ratings yet
- Effectiveness of Tramadol/paracetamol Compared With Etoricoxib As Postoperative Analgesia in Daycare SurgeryDocument6 pagesEffectiveness of Tramadol/paracetamol Compared With Etoricoxib As Postoperative Analgesia in Daycare SurgerydesantosalbaNo ratings yet
- Effect of Misoprostol With and Without Evening Primrose On Induction of Missed AbortionDocument9 pagesEffect of Misoprostol With and Without Evening Primrose On Induction of Missed AbortionmozhganNo ratings yet
- Comparative Effect of Nature-Based Sounds Intervention and Headphones Intervention On Pain Severity After Cesarean SectionDocument11 pagesComparative Effect of Nature-Based Sounds Intervention and Headphones Intervention On Pain Severity After Cesarean SectionDwi AndayaniNo ratings yet
- Impact of Intra-Operative Dexamethasone After Scheduled Cesarean Delivery: A Retrospective StudyDocument8 pagesImpact of Intra-Operative Dexamethasone After Scheduled Cesarean Delivery: A Retrospective StudyMiftah Furqon AuliaNo ratings yet
- Journal ObgynDocument4 pagesJournal ObgynFeby AnggreiniNo ratings yet
- 1 s2.0 S2214139121000500 MainDocument6 pages1 s2.0 S2214139121000500 MainpfhmakatubacNo ratings yet
- Effect of Cryotherapy Versus AromatherapDocument11 pagesEffect of Cryotherapy Versus Aromatherapasmaa elnabawy1No ratings yet
- AsxDocument11 pagesAsxBuzzinga CooperNo ratings yet
- Prin 17Document5 pagesPrin 17JULIANINo ratings yet
- The Comparison of Intraincisional Injection Tramadol, Pethidine and Bupivacaine On Postcesarean Section Pain Relief Under Spinal AnesthesiaDocument6 pagesThe Comparison of Intraincisional Injection Tramadol, Pethidine and Bupivacaine On Postcesarean Section Pain Relief Under Spinal AnesthesiaSyukron AmrullahNo ratings yet
- The Efficacy of Non-Narcotic Analgesics On Post Operative Endodontic PainDocument22 pagesThe Efficacy of Non-Narcotic Analgesics On Post Operative Endodontic PainArturo Trejo VeraNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument7 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Tramadol en NiñosDocument5 pagesTramadol en NiñosElias Vera RojasNo ratings yet
- Literature Review On Postoperative Pain ManagementDocument6 pagesLiterature Review On Postoperative Pain Managementea4c954qNo ratings yet
- The Effectiveness of Acupressure On Severity of Depression in Hemodialysis Patients: A Randomized Controlled TrialDocument8 pagesThe Effectiveness of Acupressure On Severity of Depression in Hemodialysis Patients: A Randomized Controlled TrialpangaribuansantaNo ratings yet
- Assessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsFrom EverandAssessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsNo ratings yet
- Rocephin PrescribingDocument23 pagesRocephin PrescribingRosyta VelayantiNo ratings yet
- F24 - Epilepsy After StrokeDocument6 pagesF24 - Epilepsy After StrokeplocnicuNo ratings yet
- Hirschsprung's Disease 8.28a.2006 PDFDocument10 pagesHirschsprung's Disease 8.28a.2006 PDFArumDesiPratiwiNo ratings yet
- Anaemia in Systemic Lupus Erythematosus: From Pathophysiology To Clinical AssessmentDocument5 pagesAnaemia in Systemic Lupus Erythematosus: From Pathophysiology To Clinical AssessmentRosyta VelayantiNo ratings yet
- Jurnal NsaidDocument5 pagesJurnal NsaidRosyta VelayantiNo ratings yet
- DDDT 10 2477Document5 pagesDDDT 10 2477Rosyta VelayantiNo ratings yet
- The Effects of Lidocaine and Mefenamic Acid On Post-Episiotomy Pain: A Comparative StudyDocument5 pagesThe Effects of Lidocaine and Mefenamic Acid On Post-Episiotomy Pain: A Comparative StudyRosyta VelayantiNo ratings yet
- North-South Railway Project - South LineDocument49 pagesNorth-South Railway Project - South LinesuperNo ratings yet
- Different Models of EIDocument13 pagesDifferent Models of EIneena686236No ratings yet
- Research Proposal Sample OutlineDocument17 pagesResearch Proposal Sample OutlineGuidance and Counseling OfficeNo ratings yet
- Guidance UDI Compliance DatesDocument13 pagesGuidance UDI Compliance DatesGigi EssegiNo ratings yet
- ACI 318M-11 RC Bracket and Corbel Design - v0.03 - 2017-04-10Document5 pagesACI 318M-11 RC Bracket and Corbel Design - v0.03 - 2017-04-10arken123No ratings yet
- Hal Foster Vision and Visuality Discussions in Contemporary Culture PDFDocument75 pagesHal Foster Vision and Visuality Discussions in Contemporary Culture PDFEd GomesNo ratings yet
- LADA Niva 1600rebuild1Document39 pagesLADA Niva 1600rebuild1Douglas Antonio Paredes MarquinaNo ratings yet
- TLE CapsLet G10Document5 pagesTLE CapsLet G10Larnie De Ocampo PanalNo ratings yet
- Argumentative EssayDocument7 pagesArgumentative EssayHoang Thi Huyen DieuNo ratings yet
- Obat Keras N0vember 2021Document137 pagesObat Keras N0vember 2021antonNo ratings yet
- Sa Inc HCP English d10840Document64 pagesSa Inc HCP English d10840Ayu AfiantyNo ratings yet
- Chemistry Module 3Document14 pagesChemistry Module 3MASHNo ratings yet
- Sullair VARIABLE SPEED - 1800-2200-1800V-1809V-2200V-25-30HPDocument70 pagesSullair VARIABLE SPEED - 1800-2200-1800V-1809V-2200V-25-30HPJose MontielNo ratings yet
- Ifrs 15Document24 pagesIfrs 15Madhu Sudan DarjeeNo ratings yet
- Danielson Observation FormDocument5 pagesDanielson Observation Formapi-242909722No ratings yet
- Handout No. 03 - Purchase TransactionsDocument4 pagesHandout No. 03 - Purchase TransactionsApril SasamNo ratings yet
- Position Trading Maximizing Probability of Winning TradesDocument91 pagesPosition Trading Maximizing Probability of Winning Tradescarlo bakaakoNo ratings yet
- Metric Conversion WorksheetDocument3 pagesMetric Conversion WorksheetKaiden HughesNo ratings yet
- How Do I Predict Event Timing Saturn Nakshatra PDFDocument5 pagesHow Do I Predict Event Timing Saturn Nakshatra PDFpiyushNo ratings yet
- Utah Vaccine AdministrationDocument1 pageUtah Vaccine AdministrationOffice of Utah Gov. Spencer J. CoxNo ratings yet
- Lux Level Calculation: WILSON ELECTRICAL ENGINEERING BOOKS (Simplified Edition 2020)Document1 pageLux Level Calculation: WILSON ELECTRICAL ENGINEERING BOOKS (Simplified Edition 2020)Wilson (Electrical Engineer)No ratings yet
- Purchase Spec. For Bar (SB425)Document4 pagesPurchase Spec. For Bar (SB425)Daison PaulNo ratings yet
- BasicCalculus12 Q3 Ver4 Mod3 The Derivatives V4Document34 pagesBasicCalculus12 Q3 Ver4 Mod3 The Derivatives V4karren100% (1)
- Dry Docking QuotationDocument4 pagesDry Docking Quotationboen jayme100% (1)
- CH 3 TestDocument50 pagesCH 3 TestVK ACCANo ratings yet
- UKAYUNIK Chapter 1 To 12Document31 pagesUKAYUNIK Chapter 1 To 12Chiesa ArellanoNo ratings yet
- FPA 03-A.01 Permohonan Akreditasi LP LK LI LM PUP PBADocument595 pagesFPA 03-A.01 Permohonan Akreditasi LP LK LI LM PUP PBAabimanyubawonoNo ratings yet
- Sagittarius ProfileDocument3 pagesSagittarius ProfileWAQAS SHARIFNo ratings yet
- 02 Height and Distance - NIMCET Free Study MatrerialDocument2 pages02 Height and Distance - NIMCET Free Study MatrerialIshang VashishthaNo ratings yet
- Kibera Mirror JULYDocument8 pagesKibera Mirror JULYvincent achuka maisibaNo ratings yet