Professional Documents
Culture Documents
Lymph Node Pathology PDF
Uploaded by
Keserovic AdmirOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lymph Node Pathology PDF
Uploaded by
Keserovic AdmirCopyright:
Available Formats
jslum.
com | Medicine
Lymph Node Pathol ogy
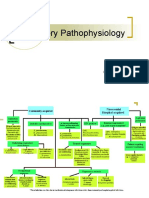
Normal Lymph Node
Lymphadenitis (In fection of Lymph Nodes )
Lymph Nodes u ndergo reactive changes
Acute/ Chronic
Chronic
Follicular Hyperplasia
(Prominent Germinal Centers)
Important Principles
Tissue Diagnosis is Mandatory
Traditionally All considered Malignant
(but wide range of clinical behaviours seen)
B cell in origin (80-85%)
Disrupt Normal regulatory mechanisms
(Lead to frequent Immune Abnormalities)
Monoclonal
(All derived from single transformed cell)
Neoplastic B & T cells tend to Home & Grow in areas where their Normal
Counterparts resides
Disseminated at the time of diagnosis
HL spreads in orderly fashion
(Staging important for Treatment)
Classification
NHL (Working Formulation)
Low Grade
Intermediate Grade
High Grade
Cat-Scratch Disease
Skin Lesion (7-12 days after contact)
Enlargement of Regional Lymph Nodes
History of being Scratched by Cat
Cat-Scratch Disease
Microabscesses of varying sizes
(pink areas)
Clinical Presentation
Depend on anatomical distribution of disease
2/3rd of Non-Hodgkins Lymph oma (NH L) & Hodgkins Lymphoma (H L)
Nontender Nodal Enlargement
o
Localized
o
Generalized
1/3rd are Extranodal
Skin
Stomach
Brain
Multiple Myeloma (MM)
Skeletal Bone Destruction (Pain, Pathological Fracture)
Enlarging Mass(es), typically Painless, at site of Nodal/ Lymphoid tissue
Obstruction, Ulceration of Hollow organs MALT Pain
Interference with Normal Organ Function Solid Organ Infiltration
(Kidneys, Liver, Bone Marrow)
Cat-Scratch Disease
Gram ve
Pleomorphic
Extra-cellular Coccoba cillary
pathogen (Bartonella henselae)
Warthin-Starry Silver stain
Singly, Small Clumps, Chains
(in Necrotic Foci)
2 Syphilis
Florid Follicular Hyperplasia
Partially Fused Lymphoid Follicles assume Bizarre shapes
Microscopic Features of Malignant Lymphomas
Power
Power
Loss of N ormal Architectural
Loss of cellular Heterogeneity
organization
Presence of Absence of Aberrant
Monotonous domination by Single
Follicle Formation
cell type
Immune Cell Antigens detected by Monoclonal Antibodies
Primarily T cell associated
Primarily Monocyte/ Macrophages
CD3
CD13
CD4
CD33
Primarily B cell associated
Primarily Stem cells
CD10
CD34
CD19
CD20
Primarily NK cells
On all Leukocytes
CD16
CD45 (LCA)
CD56
Most Common Lymphoid Neoplasms
Grade Lymphoma cell types
Small lymphocytic
Small cleaved follicular
Toxoplasma Lymphadenitis
Painless Axillary Lymphadenopathy
Confirm by Serologic Tests
Hyperplastic Follicle with reactive germinal center (numerous Macrophages)
Clusters of Epitheloid cells (upper right of follicle)
HL
Nodular Sclerosis
Mixed Cellularity
Lymphocyte Depletion
Lymphocyte Rich /Predominance
jslum.com | Medicine
Non-H odgkins Lymphoma
Follicular Lymphoma (Low Grade Non-Hodgkins Lymphoma )
Most common form among Caucasians (Not common in Malaysia)
Middle age
M=F
Neoplastic cells closely resemble normal germinal centre B cells
Predominantly Nodular/ Nodular & Diffuse growth pattern within lymph node
Almost similar to Reactive Hyperplasia
Predominantly Small Cleaved cells
Lymph node is effaced by Intermediate-sized Lymph oid cells
Mitotic Index
Apoptotic cell death
Starry Sky pattern
(due to scattered benign Macrophages among malignant lymphoid cells)
Intermediate Grade Lymphomas
Large Cell Lymphomas
Large Cell Cleaved
High Grade Lymphomas
Burkitt Lymphoma
Categories
(All Morphologically Identical)
(Some Clinical, Genotype, Virological Difference)
African (Endemic)
Sporadic (Nonende mic)
Aggressive type (HIV individuals)
Associated with Translocations of c-MYC gene on Ch8
IgH locus t(8;14) usually
Endemic tumours are latently infected with EBV
Endemic
Sporadic
Children/ Young Adults
Children/ Young Adults
Manifest at Extranodal sites
Manifest at Extranodal sites
Mass over Mandible, Abdominal
Abdominal Mass
Viscera (Kidneys, Ovaries, Adrenals)
(Ileocaecu m, Peritoneum)
Very aggressive
Very aggressive
Large Cell NonCleaved
Burkitt Lymphoma
Starry Sky pattern
Diffuse Large B-cell Lymphoma
20% of all NHL
Constitute 60-70% of aggressive Lymphoid Neoplasms
Male slightly
Immunoblastic, Plasmacytoid
Clinical
Rapidly enlarging mass
(single nodal/ extranodal site)
(often symptomatic)
(can arise at any site)
Waldeyer ring, Oropharyngeal lymph node, Adenoids, Tonsils
Extranodal sites
Aggressive tumour & rapidly fatal if untreated
Very responsive to Chemotherapy
Complete Remission (60-80%)
Complete Cure (50%)
Therapy
Limited stage
Grade Lymphomas
Disseminated Grade
Lymphomas (90%)
Aggressive Lymphomas
Treated with Radiation Therapy
(can be curative)
No Therapy
Morbidity Limited Chemotherapy
Bone Marrow Transplant
Multiagents ( 5 drugs) Chemotherapy
Complete remission rate 60-80%
30-40% Cured
Large cell size
(4-5x mature lymphocytes)
Diffuse pattern of growth
Some Morphologic Variation
Vesicular nuclei
Prominent 2-3 nuclei
Moderate abundant cytoplasm
Staging (Ann Arbor Staging System) (Hodgkins & Non-Hodgkins)
I
Single Lymph
Node area
Involvement
II
2 or More Lymph
Nodal Areas
(con fined to 1
side of
diaphragm)
III
Involving Lymph
nodes Above &
Below
Diaphragm
Prognosis 5-Year Disease Free Survival Rate (Hodgkins)
90%
75-90%
50-85%
IV
Involvement
outside Lymph
Node areas
Diffuse,
Disseminated
disease of BM,
Liver, Extranodal
40-65%
jslum.com | Medicine
Hodgkins Lymphoma (HL)
Definition
Characteristics
Reed-Sternberg cells (Large, Abnormal cells)
Admixed with Non-Malignant Inflammatory Cells
Reed-Sternberg cells
Distinctive Tumour Giant cell
Bi-Nucleated/ Bi-Lobed
owl-eyed nuclei
Reed-Sternberg cell Variants
Lacunar
Popcorn/ L&H
Mononuclear
Mummified
Epidemiology
Commonly Young Adults (but can present at any age)
Incidence with respect to age bimodal
1st peak Late Adolescence, Young Adulthood
2nd peak 6th Decade
Bimodal Curve shifts to Younger Ages in Undeveloped countries
Male : Female = 2 : 1
Clinical
Painless Lymphadenopathy in Superficial Lymph Nodes involving
Cervical nodes (60-70%)
Axillary nodes (10-15%)
Inguinal nodes (6-12%)
Unexplained Fever > 38C
Night Sweats
Loss of >10% Body Weight in 6 months
Etiology
Unknown
Possible Etiologic Factors
Prior EBV Infection
Frequent BCL-2 Translocations
Epstein-Barr Virus (EBV)
Detected in approximately 40% of cases of classical HL
Clonal
WHO Classification/ Histological Type
Nodular Sclerosing (64% )(worst prognosis)
Lymphocyte-Ri ch/ Predomi nance (7%) (best prognosis)
Mixed Cellularity (25%)
Lymphocyte-Depleted (4%)
Nodular Sclerosis
Most common type of HL (70%)
Women more common
Mediastinal involvement present with stage II disease (80% cases)
Characteristic Feature
Lacunar (Reed -Sternberg variant)
Sclerosing bands of collagenous fibrosis forming a nodular pattern
Fibrosis Thickens the capsule & Divides proliferating processes into nodules
or islands
Numerous Lacunar variants (Classical Reed-Sternberg cells are infrequent)
Most common type in Industrialized countries
Presents in Anterior Mediastinum & Neck (Young Adult Female)
Lymph Node/ Thymu s divided into variably sized nodules
(by collagenous bands sclerosis ) extending from a thickened capsule
Nodules composed of mix of
Lymphocytes
Eosinophils
Histiocytes
Classic Reed-Sternberg cells
Lacunar variant of Reed-Sternberg cells
Lymphocyte-Rich/ Predominant
Mononuclear L&H Hodgkin cells
Popcorn shape d nuclei
Inconspi cuous n uclei
Background of Small Lymphocytes (Lymphocyte predominant)
Classic Reed-Sternberg cells (rare & difficult to find)
May be Diffuse or Nodular
Limited disease in Neck of Young Patients
Associated with
L&H (Lymphocytic & Histiocytic) cell (p opcorn cell) variant Reed-Sternberg cell
Mixed Cellularity
Men (70%) with Late Stage (III-IV) Disease & B-symptoms
Systemic Manifestations (frequently)
Numerous Reed-Sternberg cells
Mixed Inflammatory Background (obliterate normal architecture)
Plasma cells (frequent)
Eosinophils (freq uent)
Fibrosis, Necrosis (small amount present)
Mixture of Lymphocytes, Eosinop hils, Histiocytes, Reed-Sternberg cells
Mononuclear variant of Reed-Sternberg cells
Lymphocyte-Depleted
Associated with HIV Infection
Clinical
Abdominal organs
Retroperitoneal lymph nodes
Bone Marrow
Peripheral Lymph Node (involvement common)
Approximately 70% of patients present have
Advanced Stage
B symptoms (80%)
Characteristics
Reed-Sternberg cells & Variants
Extensive Fibrosis
Small Lymphocytes (virtually absent)
Subtypes
Sarcomatous
Diffuse Fibrosis
Bizarre Reed-Sternberg cells
Extensive Fibrosis
Bizarre Anaplastic
Rare Reed-Sternberg cells
Reed-Sternberg-like variants seen
Present in Retroperitoneum (without peripheral nodal disease)
Tissue contain Precollagenous Sclerosis, Pleomorphic Reed-Sternberg variants
Liver Involvement in Hodgkins Disease
jslum.com | Medicine
Multiple Myeloma
Definition
Plasma cell Neoplasm
Men (common)
Involvement of Skeleton at Multiple sites
Bone involvement predominates
Lymph node Spread & Skin involvement
Clinical Course
Organ Infiltration
Excess Ig
Suppression of Humoral Immunity
HyperCalcaemia
Renal Failure
Prognosis generally Poor
Presentation
Multifocal Destructive Bone Lesions
Vertebral column (66%)
Ribs (44%)
Skull (41%)
Pelvis (28%)
Femur (24%)
Clavicle (10%)
Scapula (10%)
Punched -out lesion on Radiograph (1 -4cm in diameter)
Metastases
Breast
Lungs
Prostate
GIT
Plasma cell neoplasm, Multiple Myeloma, related entities
Lymphoid neoplas m of terminally differentiated B cells
Expansion of single clone of Ig secreting plasma cells
Resulted in serum levels of a single homogenous Ig or its fragments
Hodgkins VS Non-H odgkins
Hodgkins
Usually Localised to Single lymph
node or Chain of node s
Orderly, Contiguous spread to
Adjacent lymph nodes
Peripheral Involvement
Morpholically distinctive
Reed-Sternberg (RS) cells
Non-H odgkins
Not as Localised
Spread often Random &
Unpredictable
Peripheral, Extranodal involvement
No Reed-Sternberg cells
Multiple Myeloma
Multiple Lytic Lesions of Vertebrae
Bone Marrow
Plasmacytosis > 30%
Malignant Plasma Cells
Lab Results
Serum Electrophoresis
Peripheral Blood Film
Rouleaux Formation
Rouleaux Formation
Urine
Bence-Jones Protein excreted by Kidneys (can cause Renal Impairment)
Generally Involves Contiguous Nodes
Rarely Extranodal
Bone Marrow involvement is unusual
(< 5%)
When involves the Spleen or Liver,
presents as Mass rather than Diffuse
involvement
Noncontiguous
Extranodal involvement Frequent
You might also like
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- WBC Lymph Node SpleenDocument12 pagesWBC Lymph Node Spleendr brijesh TiwariNo ratings yet
- A Pattern Based Approach To Nodal Lymphoma: The Critical Role of HistologyDocument55 pagesA Pattern Based Approach To Nodal Lymphoma: The Critical Role of Histologylazy19No ratings yet
- Uworld EndocrineDocument211 pagesUworld Endocrineهنادي رازمNo ratings yet
- Abnormal LFTsDocument2 pagesAbnormal LFTsRenu RosyNo ratings yet
- Liver Function Tests Diagnostic GuideDocument2 pagesLiver Function Tests Diagnostic GuideostarburstoNo ratings yet
- Pathogens of The Female Reproductive System - Leah NechamkinDocument1 pagePathogens of The Female Reproductive System - Leah NechamkinMicroposterNo ratings yet
- Vasculitic Disorders: Dra. MezaDocument47 pagesVasculitic Disorders: Dra. MezaAna Beatriz Meza OntiverosNo ratings yet
- Creatin. Creatin. Creatin. Creatin. Creatin. CreatinDocument2 pagesCreatin. Creatin. Creatin. Creatin. Creatin. CreatinEna PaparićNo ratings yet
- Endocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologyDocument3 pagesEndocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologySamuelNo ratings yet
- Chapter 13 Neoplastic Proliferations of White CellsDocument16 pagesChapter 13 Neoplastic Proliferations of White CellsOmar100% (1)
- Pathogens of The Vagina-Annie Espinosa - This Is The Revised VersionDocument1 pagePathogens of The Vagina-Annie Espinosa - This Is The Revised VersionMicroposterNo ratings yet
- Respiratory Tract InfectionsDocument1 pageRespiratory Tract InfectionsShannon RamsumairNo ratings yet
- Valvular Heart DseDocument8 pagesValvular Heart DseJane Pineda CuraNo ratings yet
- Bethesda System of Reporting Thyroid CytologyDocument131 pagesBethesda System of Reporting Thyroid CytologyMandavi HindNo ratings yet
- EmfizemulDocument19 pagesEmfizemulMirela IoanaNo ratings yet
- Graves' Disease Signs and ManagementDocument11 pagesGraves' Disease Signs and ManagementManisha Sekaran Muniandy100% (1)
- IKD9 - Radiological Evaluation of Renal CystsDocument26 pagesIKD9 - Radiological Evaluation of Renal CystsRenal Association MauritiusNo ratings yet
- Acute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmDocument1 pageAcute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmAudreySlitNo ratings yet
- Protein Synth Inhibs Target Bact RibosomeDocument61 pagesProtein Synth Inhibs Target Bact RibosomegirNo ratings yet
- PnemoniaDocument4 pagesPnemoniadhavalNo ratings yet
- Fatty Liver (1) - General PathologyDocument22 pagesFatty Liver (1) - General PathologyDarien LiewNo ratings yet
- LeukemiasDocument8 pagesLeukemiasharideepNo ratings yet
- Acute Gastroenteritis in Children: Prepared By: Prof. Elizabeth D. Cruz RN, ManDocument12 pagesAcute Gastroenteritis in Children: Prepared By: Prof. Elizabeth D. Cruz RN, ManChaii De GuzmanNo ratings yet
- Pathology of the Digestive SystemDocument28 pagesPathology of the Digestive SystemDianNursyifaRahmahNo ratings yet
- Superficial and Cutaneous Mycoses: 2. Disease CharacteristicsDocument4 pagesSuperficial and Cutaneous Mycoses: 2. Disease CharacteristicsMA. ANGELI DELA CRUZNo ratings yet
- 7sgdfgf PDFDocument438 pages7sgdfgf PDFPratik JadhavNo ratings yet
- Anemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDocument15 pagesAnemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDanielle FosterNo ratings yet
- Systemic Lupus Erythematosus Lecture Salah Abdel BakyDocument8 pagesSystemic Lupus Erythematosus Lecture Salah Abdel Bakyahmed gabrNo ratings yet
- Urological History TakingDocument6 pagesUrological History TakingayuniNo ratings yet
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocument4 pages4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaNo ratings yet
- 20 Pathoma Skin DisordersDocument10 pages20 Pathoma Skin Disordersn alawiNo ratings yet
- Endocrinology PathophysiologyDocument136 pagesEndocrinology PathophysiologyDaniel DiasNo ratings yet
- Pharmacology of EthanolDocument5 pagesPharmacology of EthanolJoshua RemonNo ratings yet
- Pathophysiology Cell Injury GuideDocument7 pagesPathophysiology Cell Injury GuideWendy SuhNo ratings yet
- Opportunistic Infections in HIVDocument50 pagesOpportunistic Infections in HIVamandaNo ratings yet
- Respiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDocument12 pagesRespiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDoc JacqueNo ratings yet
- Red Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisDocument3 pagesRed Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisAnonymous 8hJAATBNo ratings yet
- ENDOCRINE PATHOLOGY WebpathDocument35 pagesENDOCRINE PATHOLOGY Webpathapi-3766657No ratings yet
- Granulomatous Inflammation ThyroidDocument55 pagesGranulomatous Inflammation ThyroidKamlesh PrajapatiNo ratings yet
- Bone Marrow TransplantationDocument21 pagesBone Marrow TransplantationMorrison George100% (1)
- (6-7) PATH - Colonic Polyps and CarcinomaDocument11 pages(6-7) PATH - Colonic Polyps and Carcinomaaaron mbindyoNo ratings yet
- Genetic and Pediatric Diseases Chapter SummaryDocument16 pagesGenetic and Pediatric Diseases Chapter SummaryJustine HungNo ratings yet
- EL Husseiny's Guide to Pulmonary Embryology and AnatomyDocument138 pagesEL Husseiny's Guide to Pulmonary Embryology and AnatomyMuhammad Ahmad bin makruf syammakuNo ratings yet
- Heart BNHADocument13 pagesHeart BNHAX OloGyNo ratings yet
- Cellular Adaptations and Cell DeathDocument4 pagesCellular Adaptations and Cell DeathShuaib SiddiquiNo ratings yet
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Document18 pagesPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiNo ratings yet
- Aiims Discussion 2015Document115 pagesAiims Discussion 2015langhalilafaNo ratings yet
- Rheumatic Fever and Rheumatic Heart Disease 2017 and IeDocument59 pagesRheumatic Fever and Rheumatic Heart Disease 2017 and IeLipi GautamNo ratings yet
- (8!5!13) Cell Injury OutlineDocument9 pages(8!5!13) Cell Injury OutlineBhumiShahNo ratings yet
- Hematology Lectures 1 5 DR - TuyDocument10 pagesHematology Lectures 1 5 DR - TuyMiguel Cuevas DolotNo ratings yet
- (MICROA - 2.1) Myeloid Tissue HistologyDocument6 pages(MICROA - 2.1) Myeloid Tissue HistologyHenryboi CañasNo ratings yet
- Acute Lymphoblastic Leukemia (ALL)Document14 pagesAcute Lymphoblastic Leukemia (ALL)Med PhuongNo ratings yet
- Cell Adaptation and Necrosis: Hypertrophy, Atrophy, MetaplasiaDocument8 pagesCell Adaptation and Necrosis: Hypertrophy, Atrophy, MetaplasiaivankcurryNo ratings yet
- Actinic Keratosis: (Aka Bowen's Disease)Document5 pagesActinic Keratosis: (Aka Bowen's Disease)fadoNo ratings yet
- Pathology - Chapter 14Document14 pagesPathology - Chapter 14Cory GrayNo ratings yet
- Sources of Parasitic InfectionDocument74 pagesSources of Parasitic InfectionCristy Jean100% (1)
- Protozoan Parasites Causing Malaria, Sleeping Sickness, Leishmaniasis and MoreDocument32 pagesProtozoan Parasites Causing Malaria, Sleeping Sickness, Leishmaniasis and MoreFort SalvadorNo ratings yet
- CryptococcosisDocument25 pagesCryptococcosisinvisibleyetinvincibleNo ratings yet
- Adrenal Gland PathologyDocument6 pagesAdrenal Gland PathologyRami ShishanNo ratings yet
- Penicill IN: Praksh Dhakal Public Health Microbiology Tribhuvan UniversityDocument22 pagesPenicill IN: Praksh Dhakal Public Health Microbiology Tribhuvan UniversityKeserovic AdmirNo ratings yet
- Complications of Blood TransfusionDocument6 pagesComplications of Blood TransfusionKeserovic AdmirNo ratings yet
- Chronic Leg Ulcer Post Phlebitic Limb Syndrome: Homan's Sign - Forceful Dorsiflexion of Foot Will Cause Pain in CalfDocument4 pagesChronic Leg Ulcer Post Phlebitic Limb Syndrome: Homan's Sign - Forceful Dorsiflexion of Foot Will Cause Pain in CalfKeserovic AdmirNo ratings yet
- Acutescrotum 141125014842 Conversion Gate01Document18 pagesAcutescrotum 141125014842 Conversion Gate01Keserovic AdmirNo ratings yet
- Biochemical Changes of Diabetes MellitusDocument5 pagesBiochemical Changes of Diabetes MellitusKeserovic AdmirNo ratings yet
- Biochemical Changes of Diabetes MellitusDocument5 pagesBiochemical Changes of Diabetes MellitusKeserovic AdmirNo ratings yet
- Disseminated Intravascular CoagulationDocument2 pagesDisseminated Intravascular CoagulationKeserovic AdmirNo ratings yet
- Drug HaemolysisDocument3 pagesDrug HaemolysisGerardLumNo ratings yet
- CorticosteroidDocument5 pagesCorticosteroidKeserovic AdmirNo ratings yet
- Acute Medical Algorithms Updated Jan.06Document56 pagesAcute Medical Algorithms Updated Jan.06Ashraf Hussein100% (1)
- CPG Management of Venous TromboemlismDocument63 pagesCPG Management of Venous Tromboemlismapalaginih100% (1)
- Pediatric NephrologyDocument10 pagesPediatric NephrologyEarl AriasNo ratings yet
- Nationalcancercontrolprogram 150104100306 Conversion Gate02 PDFDocument94 pagesNationalcancercontrolprogram 150104100306 Conversion Gate02 PDFKeserovic AdmirNo ratings yet
- 161106115611Document3 pages161106115611Keserovic AdmirNo ratings yet
- Uputa Hygroton 25mg Tablete PDFDocument7 pagesUputa Hygroton 25mg Tablete PDFKeserovic AdmirNo ratings yet
- Production of PenicillinDocument16 pagesProduction of PenicillinMeenal KhannaNo ratings yet
- Urology Resident Handbook3380 PDFDocument65 pagesUrology Resident Handbook3380 PDFKeserovic AdmirNo ratings yet
- Genitourinary Emergency: Prof. Dr. Mostafa Sakr Genitourinary SurgeryDocument83 pagesGenitourinary Emergency: Prof. Dr. Mostafa Sakr Genitourinary SurgeryKeserovic AdmirNo ratings yet
- 2013 Hiv Aids PPTX 130505021711 Phpapp01Document25 pages2013 Hiv Aids PPTX 130505021711 Phpapp01Keserovic AdmirNo ratings yet
- CPG Management of Hypertension (3rd Edition)Document44 pagesCPG Management of Hypertension (3rd Edition)patricktiew100% (2)
- Rapid Delayed: Prevent Thrombus Formation No Direct Effect Thrombus Already FormedDocument2 pagesRapid Delayed: Prevent Thrombus Formation No Direct Effect Thrombus Already FormedKeserovic AdmirNo ratings yet
- Examination of Thyroid GlandDocument2 pagesExamination of Thyroid GlandKeserovic Admir100% (1)
- HaematinicsDocument2 pagesHaematinicsGerardLum100% (2)
- HyperthyroidismDocument6 pagesHyperthyroidismNader Smadi100% (2)
- Diabetes IN Pregnanc Y: Presenter: DR Leong Yuh Yang (MD Ukm) Supervisor: DR Noraza AzmeeraDocument45 pagesDiabetes IN Pregnanc Y: Presenter: DR Leong Yuh Yang (MD Ukm) Supervisor: DR Noraza AzmeeraKeserovic AdmirNo ratings yet
- HyperthyroidismDocument6 pagesHyperthyroidismNader Smadi100% (2)
- HyperthyroidismDocument6 pagesHyperthyroidismNader Smadi100% (2)
- Renal Function Assessment & Failure CausesDocument4 pagesRenal Function Assessment & Failure CausesKeserovic AdmirNo ratings yet
- 2013 Hiv Aids PPTX 130505021711 Phpapp01Document25 pages2013 Hiv Aids PPTX 130505021711 Phpapp01Keserovic AdmirNo ratings yet
- F.A.S.T.H.U.G: I W. AryabiantaraDocument35 pagesF.A.S.T.H.U.G: I W. Aryabiantaraarnawaiputu60No ratings yet
- LSM RepairDocument4 pagesLSM RepairDanily Faith VillarNo ratings yet
- Endocrine Exam ReviewDocument2 pagesEndocrine Exam Reviewrockforj3susNo ratings yet
- Balcom Rebecca Functional ResumeDocument2 pagesBalcom Rebecca Functional Resumeapi-360266135No ratings yet
- KENCAP Changzhou 2013Document19 pagesKENCAP Changzhou 2013KencapchangzhouNo ratings yet
- APVS 2005 Proceedings More On PigsDocument258 pagesAPVS 2005 Proceedings More On PigsDulce AmorNo ratings yet
- MInTFM Programme Brochure 2019Document12 pagesMInTFM Programme Brochure 2019Shoban RajNo ratings yet
- Resume Massage Therapist NtewDocument2 pagesResume Massage Therapist NtewPartheebanNo ratings yet
- Case Study - MyomaDocument54 pagesCase Study - Myomauvinr100% (1)
- Pancreas: Anatomy, Histology, Physiology and FunctionsDocument85 pagesPancreas: Anatomy, Histology, Physiology and Functionslungu eduardNo ratings yet
- Influence of Anthropometric Parameters On Aerobic Capacity Among DancersDocument7 pagesInfluence of Anthropometric Parameters On Aerobic Capacity Among DancersAnonymous izrFWiQNo ratings yet
- Clinical Evoked PotentialsDocument13 pagesClinical Evoked PotentialsHerminaElenaNo ratings yet
- Broadline Epar Public Assessment Report enDocument25 pagesBroadline Epar Public Assessment Report enPablo OrricoNo ratings yet
- Dabur VatikaDocument12 pagesDabur Vatikadipdarshan2400% (1)
- Williams ObstetricsDocument2 pagesWilliams Obstetricsmely sandyNo ratings yet
- DylasisDocument3 pagesDylasisyuvi087No ratings yet
- Effects of Boiling Time On Mineral and Vitamin C Content of Three Varieties of Hibiscus Sabdriffa Drink in NigeriaDocument6 pagesEffects of Boiling Time On Mineral and Vitamin C Content of Three Varieties of Hibiscus Sabdriffa Drink in NigeriariniyuliasamosirNo ratings yet
- Canadian Standards For Hospital LibrariesDocument4 pagesCanadian Standards For Hospital LibrariesFernando HernandezNo ratings yet
- Sefcik Ashley Resume 2018Document1 pageSefcik Ashley Resume 2018api-394215168No ratings yet
- Perioperative Nursing (1) 2007Document14 pagesPerioperative Nursing (1) 2007Lorraine BuelvaNo ratings yet
- MMMM 3333Document0 pagesMMMM 3333Rio ZianraNo ratings yet
- Life Calling Map Fillable FormDocument2 pagesLife Calling Map Fillable Formapi-300853489No ratings yet
- Procedure ListDocument20 pagesProcedure ListsoyrolandoNo ratings yet
- Poster ROICAM 2018Document1 pagePoster ROICAM 2018ibrahimNo ratings yet
- Brochure DiseaseDocument2 pagesBrochure Diseaseapi-295870217No ratings yet
- IP Sterility TestingDocument6 pagesIP Sterility TestingVarghese100% (3)
- From Wikipedia, The Free EncyclopediaDocument12 pagesFrom Wikipedia, The Free EncyclopediaCharlie EspinoNo ratings yet
- Mel Tappans Personal Survival Letter Issue 11 (Tappan)Document24 pagesMel Tappans Personal Survival Letter Issue 11 (Tappan)buckonbeach100% (1)
- Eyelid Eversion and Inversion Causes and TreatmentsDocument17 pagesEyelid Eversion and Inversion Causes and TreatmentsmanognaaaaNo ratings yet
- Fundamentals of Tooth Preparation Periodontal AspectsDocument74 pagesFundamentals of Tooth Preparation Periodontal AspectsVica Vitu100% (3)