Professional Documents
Culture Documents
1 s2.0 S008525381546106X Main
Uploaded by
Eka RahmawatiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1 s2.0 S008525381546106X Main
Uploaded by
Eka RahmawatiCopyright:
Available Formats
Kidney International, Vol. 55 (1999), pp.
15091517
Kidney transplanted children come of age
GISELA OFFNER, KAY LATTA, PETER F. HOYER, HANS-JURGEN BAUM, JOCHEN H.H. EHRICH,
RUDOLF PICHLMAYR,1 and JOHANNES BRODEHL
Kinderklinik der Medizinischen Hochschule Hannover, and Klinik fur Abdominal-und Transplantationschirurgie,
Kinderklinik der Medizinischen Hochschule Hannover, Hannover, Germany
Kidney transplanted children come of age.
Background. The aim of renal replacement therapy in children is to restore their potential for normal growth and development in order to reach mature adulthood. Because pediatric
kidney transplantation started in the late 1960s, it is now possible to document the progress and outcome of these patients
from transplantation in childhood to survival into adulthood.
Methods. In this single-center study, all 150 children born
before December 1977 and having received a kidney transplant
between 1970 and 1993 were selected for long-term follow-up.
The mean age at transplantation was 12.1 years (range 3.2 to
16.7), and the mean follow-up was 13.1 years (range 2.0 to
25.0). In December 1995, 124 grown-up patients with a mean
age of 25.4 years (range 18.4 to 40.3) were alive, 89 with a
functioning graft. Fifty had the first graft functioning longer
than 10 years. The fate of all patients was traced, and those
living were analyzed in regard to their somatic and socioeconomic states.
Results. The actuarial 25-year survival rate for the patients
was 81%, and for the first graft it was 31%. The best graft
survival rates were observed after living related donation, preemptive transplantation, and immunosuppression with cyclosporine. The latter benefit, however, vanished after eight years.
The mean creatinine clearance declined over the years from
76 to 45 ml/min/1.73 m2, and the incidence of hypertension
increased to more than 80% of the patients. Malignancies occurred in 2.6%. Final height was stunted in 44% of noncystinotic patients, whereas all patients with cystinosis were extremely growth retarded. Twenty-seven percent suffered from
additional disabilities. A majority of adult patients were rehabilitated in regard to education and socioeconomic status, and
14% were unemployed.
Conclusions. The results indicate that renal transplantation
in children leads to a high degree of rehabilitation in adulthood.
The life of a kidney transplant, however, is limited, which
points out the need for more specific immunosuppression with
fewer side-effects in order to reach the goal of lifelong graft
function.
1
Deceased
Key words: pediatric kidney transplantation, living related organ donation, creatinine clearance, growth, immunosuppression, graft function,
end-stage renal failure.
Received for publication March 3, 1998
and in revised form November 3, 1998
Accepted for publication November 5, 1998
1999 by the International Society of Nephrology
When the first pediatric kidney transplantations were
performed in the late 1960s [1], it was uncertain whether
there would be a realistic chance for children with endstage renal failure to reach mature adulthood. In the
subsequent 30 years, experience in pediatric kidney
transplantation increased dramatically. The use of immunosuppressive drugs improved to such an extent that
today kidney transplantation has become the treatment
of choice for children with end-stage renal failure [25].
It has become obvious that the degree of medical and
psychosocial rehabilitation depends mainly on the quality of graft function [68]. There are, however, only a
few reports on the long-term results of patients who
received a renal transplantation in childhood and had
reached adulthood [911]. We therefore evaluated the
long-term results of children transplanted at our unit.
Factors influencing graft survival, graft function longer
than 10 years, the final height, and the social rehabilitation of the adult patients are analyzed.
METHODS
From 1970 to 1993, 150 children born before December 1977 received a total of 186 renal transplantations at
the Childrens Hospital of the Medical School Hannover.
The primary renal diseases leading to terminal renal
failure is outlined in Table 1. Characteristics of all 150
patients, including these who died between 1975 and
1995, and grafts are summarized in Table 2. The immunosuppressive therapy between 1970 and 1982 consisted of
azathioprine (Aza) and high-dose prednisolone [12] and
between 1982 and 1995 of cyclosporine A (CsA) and lowdose prednisolone [13]. Twenty-seven transplantations
were performed pre-emptively. All but two patients had
a minimum follow-up of at least four years. The mean
time was 13.1 years (range 2 to 25 years).
In December 1995, 124 patients were alive, with a
mean age of 25.4 years (range 18 to 40 years). Twentytwo died at a mean age of 16.5 years (range 6.0 to 32.2
years), and four were lost to follow-up. Fifty patients
were living with the first graft functioning longer than
1509
1510
Offner et al: Kidney transplanted children come of age
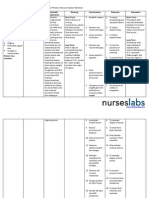
Table 1. Primary renal diseases in 150 children (aged 3.2 to 16.7
years) born before 1977 and transplanted between 19701993
with the potential to reach adulthood (age . 18 years)
after first kidney transplantation
Congenital/inherited N 5 104
(69%)
Acquired N 5 46
(31%)
Nephronophthisis N 5 28
Dysplasia/hypoplasia N 5 21
Obstructive uropathy N 5 20
Cystinosis N 5 19
Alports syndrome N 5 9
Hyperoxaluria type I N 5 3
ARPKD N 5 2
Congenital NS N 5 2
FSGS N 5 13
HUS N 5 10
Henoch-Schonlein nephritis N 5 6
MPGN N 5 6
IgA nephritis N 5 1
RPGN N 5 1
Undefined glomerulonephritis N 5 3
Other N 5 6
Abbreviations are: ARPKD, autosomal recessive polycystic kidney disease;
NS, nephrotic syndrome; FSGS, focal segmental glomerulosclerosis; HUS, hemolytic uremic syndrome; MPGN, membranoproliferative glomerulonephritis;
RGN, rapid progressive glomerulonephritis; other, unilateral Wilms tumor and
kidney trauma, amyloidosis in juvenile rheumatoid arthritis, hypersensitive vasculitis, membranous glomerulonephritis.
10 years. Twenty-five patients with a mean age of 21.3
years (range 18.4 to 29.7 years) were still under the care
of the Pediatric Transplantation Unit of the Childrens
Hospital, Medical School of Hannover, and 99 patients
were transferred to adult nephrological care at a mean
age of 26.8 years (range 19.1 to 40.3 years). For socioeconomic evaluation, 120 patients were contacted by telephone, whereas four could not be reached. The final
adult height was available in 100 patients.
For statistical analysis, PC-Statistik 3.0 (Lambda, Topsoft, Graz, Hannover, 1993) was used. Actuarial survival
rates calculated according to Kaplan and Meier [14] were
compared by the Mantel-Haenszel x2 test. The death of
a patient was computed as graft loss even though the
graft was still functioning. The MannWhitney and Fisher
tests were used for comparison of unpaired groups. Differences were defined as significant by a P of less than
0.05. Height was expressed by standard deviation scores
(SDS) in correlation to the height of age- and sexmatched children of Germany [15]. The socioeconomic
status of the German population in the age group from 25
to 35 years was drawn from the 1994 statistics of the Statistisches Bundesamt (85180 Wiesbaden, Germany) [16].
RESULTS
Survival rates
The actuarial survival rate of the 150 children after 25
years was 81%, and the survival rate of the first grafts
was 31% (Fig. 1). The calculated half-life of a first graft
functioning is therefore 10.5 years. Among those who
lost their grafts, 36 retransplantations were performed,
which had a worse outcome with a half-life of 7.5 years. A
comparison of the results under Aza immunosuppression
(N 5 79) and CsA immunosuppression (N 5 71) revealed a significant superiority of CsA over Aza during
the first seven years after transplantation, which vanished
Table 2. Characteristics of all transplanted children (RTx)
born before 1977
Patients
Age of RTx years
Male/female
Number of grafts
1/2/3/4 grafts
LRD/CD (1st grafts)
Aza/CsA (1st grafts)
Preemptive transplantation
Patients alive at December 1995
Age of living patients
Follow-up time after RTx of living patients years
150
12.1 6 3.2a
74/76
186
150/29/6/1
35/115
79/71
27 (18%)
124 (83%)
25 6 44.4a
13.1 6 4.5a
Data are mean 6 sd
The different immunosuppressive regimens consisted either of azathioprine
and high dose prednisolone (Aza), or cyclosporine and low dose prednisolone
(CsA). Abbreviations are: LRD, living related donors; CD, cadaveric donors.
a
thereafter (Fig. 2). A comparison between living related
donor (LRD) grafts (N 5 35) and cadaveric (CD) grafts
(N 5 115) demonstrated a slightly, but insignificantly,
better outcome of LRD grafts (Fig. 3). The outcome of
pre-emptively transplanted grafts (N 5 27), regardless
of LRD (N 5 12) or CD (N 5 15), was at least as good
as for those grafted with prior dialysis (Fig. 4).
A 10-year follow-up of patients living with first graft
Fifty adult patients transplanted in childhood had the
first graft functioning longer than 10 years. Thirty-five of
these were treated with Aza and high-dose prednisolone,
and 15 patients were treated with CsA and low-dose
prednisolone. Complete data of renal function and blood
pressure were available for 40 patients. Glomerular filtration rate (GFR), calculated by serum creatinine and
height [17], deteriorated over the years in both immunosuppressive groups (Table 3). The mean initial GFR was
higher in the Aza group than in the CsA group (86 vs.
67 ml/min/1.73 m2, P , 0.03). After 10 years, the difference of GFR between both groups was not significant
(50 vs. 41 ml/min/1.73 m2). With the deterioration of
GFR, the rate of hypertension increased in the Aza
group from 54% at time of transplantation to 89% after
10 years, and in the CsA group from 58% to 83%. The
difference between mean GFR at six weeks after transplantation of all 10-year graft survivors (79 ml/min/1.73
m2) and those who did not survive 10 years (52 ml/min/
1.73 m2) was significant (P , 0.001).
Graft failure
During the 25 years of observation, 90 first grafts and
26 regrafts were lost. Most of the graft failures occurred
during the first decade, especially in the first year after
transplantation because of acute rejection episodes, vascular complications, primary nonfunction, recurrence of
primary disease, cytomegalovirus infection, and CsA
toxicity (Fig. 5). Graft failures after 10 years were rare
Offner et al: Kidney transplanted children come of age
1511
Fig. 1. Survival rates according to Kaplan
and Meier of 150 patients (s), 150 first grafts
( ), and 36 regrafts (m).
Fig. 2. Survival rates according to Kaplan
and Meier of 150 first renal grafts comparing
between azathioprine (Aza) immunosuppression (N 5 79; j) and cyclosporine A (CsA)
immunosuppression (N 5 79; s). P values at
one, five, and eight years after transplantation
were 0.0007, 0.022, and 0.107, respectively.
Fig. 3. Survival rates according to Kaplan
and Meier of 150 first renal grafts comparing
between living related donor grafts (LRD 5
35; s) and cadaveric grafts (CD 5 115; j).
The P value is 0.293.
1512
Offner et al: Kidney transplanted children come of age
Fig. 4. Survival rates according to Kaplan
and Meier of 150 first renal grafts comparing
between pre-emptive transplantation (N 5 27;
s) and transplantation after prior dialysis
(N 5 123; j). The P value is 0.13.
Table 3. Glomerular filtration rate (GFR) and hypertension (%)
in adult patients transplanted in childhood with 10 year
graft function
6 weeks after RTx
GFR ml/min/1.73 m2
Aza (N 5 28)
86 6 26
CsA (N 5 12)
67 6 15
Percentage of patients with
arterial hypertension
Aza (N 5 28)
54%
CsA (N 5 12)
58%
5 years
after 10 years
65 6 18
49 6 15
50 6 25
41 6 21
82%
67%
89%
83%
The comparison is between Aza and CsA immunosuppression.
Patient deaths
Twenty-two patients died, seven of whom in the first
year after transplantation (Fig. 5). Four patients died
with uremia after their graft failed after the decision not
to re-establish dialysis treatment. In the first decade of
kidney transplantation, the most frequent cause of death
was an infection related to high-dose immunosuppressive treatment with glucocorticoids. Cardiovascular complications accounted for 23% of deaths. Beyond 10 years,
six patients died, two from complications of retransplantation, one each from a T-cell lymphoma, cerebral
insult caused by cystinosis, cardiovascular complication,
and suicide after the fourth graft failure (Table 4).
Transplanted children becoming adults
Fig. 5. Number of renal graft failures (N 5 90; ) and patient deaths
(N 5 22; j) in correlation to the time after kidney transplantation.
and were largely due to chronic graft failure. In a few
cases, acute rejection caused by noncompliance, recurrence of membranoproliferative glomerulonephritis, malignancy (T-Non-Hodgkin lymphoma), de novo glomerulopathy, and death with functioning graft led to graft
failures even after 10 years post-transplantation (Table 4).
In December 1995, 124 patients who were transplanted
in childhood lived to a mean age of 25.4 years (range 18
to 40 years). Their medical profile is summarized in Table
5. Eighty-nine lived with a functioning graft, 60 with the
first graft. Thirty-five were waiting for retransplantation
on dialysis, 24 on hemodialysis, 11 on peritoneal dialysis.
Twenty-five patients were still under the care of the
transplant team of the Childrens Hospital, whereas 99
had been transferred to adult nephrological clinics.
Seventy-eight percent of the patients with functioning
graft and 73% of patients on dialysis needed antihypertensive medications. There was a significant correlation
between serum creatinine and hypertension in the patients with functioning grafts (P 5 0.0027). Sixty-four
patients with hypertension had a mean serum creatinine
of 150 6 86 mmol/liter, and 18 patients with normal blood
pressure showed a normal graft function with a mean
serum creatinine of 98 6 37 mmol/liter.
Twenty-nine out of 108 patients developed additional
disabilities, which were in the main part of their primary
1513
Offner et al: Kidney transplanted children come of age
Table 4. Causes for 90 graft failures and 22 patient deaths
Grafts N 5 90
Causes
Acute rejection
Chronic rejection
Cardiovascular complications
Severe infection
Primary non-function
Surgical complications
CsA toxicity
T cell lymphoma
Recurrence of renal disease
De novo glomerulonephritis
Cerebral insult
Suicide
Patients N 5 22
Years after RTx
14
48
7
5
3
3
1
1
5
2
1
Years after RTx
2.0 (0.0111.7)
6.2 (0.714.5)
0.7 (0.014.0)
2.6 (0.016.9)
0
0
0
11.0
3.5 (0.0114.2)
2.3 and 15.1
13.5
2
2c
6b
7a
1
1
0.3 and 1.0
3.4 and 4.0
7.6 (1.917.1)
4.2 (0.0114.2)
0 and 8.6
11.2
13.5
12.2
Data are mean (range).
a
Four and b 2 patients died with functioning grafts
c
Dialysis not re-established following graft failure
Table 5. Medical profile of adult patients who received a kidney transplantation in childhood and were alive on December 1995
Actual age yearsa
at childrens hospital
at adult nephrology
Serum creatinine lmol/literb
Serum cholesterol mg/dl b
Serum triglycerides mg/dl b
Hypertensionc
Additional disabilities
Patients number Tx/dialysis
Patients with functioning grafts
Patients with dialysis
24/1
65/34
84/35
62/11
59/11
82/22
80/28
21.3 (18.429.7)
27.5 (19.140.3)
139 6 81
219 6 53
159 6 76
63/82 (78%)
21/80 (26%)
20.3
25.7 (20.435.0)
.800
215 6 46
268 6 120
16/22 (73%)
8/28 (29%)
Tx is transplantation.
a
Mean values (range)
b
Mean values 6 sd
c
Patients with antihypertensive medications, diuretics not included
disease. Diabetes mellitus (N 5 2), visual impairment
(N 5 5), muscle weakness (N 5 2), and neurological
disorders (N 5 4) occurred in patients with cystinosis
and nephronophthisis. A hearing defect (N 5 3) occurred
in patients with Alports syndrome. There was an impairment of liver function (N 5 4) in patients with ARPKD,
and hyperoxaluria was found in one patient who needed
a liver transplant. Three patients with uropathy required
an ileum conduit. Bone disease (N 5 3) was not specific
to primary disease. Gout (N 5 2) was considered as a
side-effect of CsA. In one patient suffering from polyarthritis complicated by amyloidosis, the disease continued
after transplantation.
Adult height
The final height was evaluated in 100 patients (84
noncystinotic and 16 cystinotic patients) and compared
with the immunosuppressive therapy. This is detailed in
Table 6. Noncystinotic males (N 5 41) reached a mean
final height of 168.7 6 9.9 cm, and noncystinotic females
(N 5 43) reached a mean final height of 158.5 6 8.0 cm.
The mean final height of cystinotic males (N 5 6) was
147.5 6 13.6 cm, and that of cystinotic females (N 5 10)
Table 6. Final height of 84 non-cystinotic and 16 cystinotic patients
with kidney transplantation in childhood, separated by
immunosuppressive therapy
Aza
Non-cystinotic patients
Number of patients
Age of RTx yearsa
Height SDS at RTxa
Years with graft functiona
Final height SDSa
D height SDS
Cystinotic patients
Number of patients
Age of RTx years
Height SDS at RTxa
Years with graft functiona
Final height SDSa
D height SDS
CsA
P value
35
12.2 6 2.9
21.55 6 1.52
12.0 6 7.1
22.20 6 1.53
20.65
49
13.8 6 2.5
21.66 6 1.42
7.5 6 3.1
21.63 6 1.70
10.03
0.029
0.342
0.0002
0.046
0.038
11
9.6 6 1.7
25.78 6 1.91
9.3 6 6.3
26.15 6 1.64
20.37
5
10.6 6 1.9
25.04 6 1.14
6.4 6 4.5
24.16 6 1.46
10.88
0.145
0.223
0.187
0.018
0.267
Abbreviations are: Aza, azathioprine; CsA, cyclosporine; RTx, renal transplantation; SDS, standard deviation score.
a
Data are mean 6 sd
was 140.8 6 7.7 cm. The percentage of patients with
stunted final height (height SDS below 22.0) was 44%
in noncystinotic patients and 100% in cystinotic patients.
1514
Offner et al: Kidney transplanted children come of age
Table 7. Socioeconomic status of 120 adult patients (age $ 18 years)
with renal transplantation in childhood
Social condition
Occupation
School/university
Vocational training
Employed
Unemployeda
Unable to work
Housewife
At parental home
Alone
Partnership
N 5 54 (45%) N 5 41 (34%) N 5 25 (21%)
10
17
19
5
3
8
6
22
4
1
15
4
1
5b
Table 8. Professional profile of 61 adult patients with renal
transplantation in childhood
Occupation
Public service
Office worker
Healthcare professional (1 physician)
Manual laborer
Craftsman
Tailor, housekeeper
Unskilled worker (3 included from sheltered workshops)
Housewife
18
16
6
5
1
2
8
5
a
The rate of unemployment was 14% compared to 9% of the German population in the age group between 25 and 35 years 1994
b
Three mothers had given birth to healthy children
Seven patients were treated with recombinant human
growth hormone (rhGH) late in puberty, three noncystinotic patients and four cystinotic patients (three Aza,
one CsA). The noncystinotic patients treated with rhGH
reached a mean final height SDS of 21.88, and the cystinotic patients with rhGH reached a mean final height
SDS of 26.77.
Malignancy
Four adult patients (2.6%) transplanted in childhood
developed malignant tumors (one neoplasm per 491 patient years). As already mentioned, one patient with
T-cell lymphoma 11 years after transplantation died
without chemotherapy. Two patients with carcinoma of
the thyroid gland and uterine cervix each survived with
surgical removal of the tumor, but lost their grafts some
years later because of chronic rejection. One patient with
a testicular tumor was successfully operated and is still
living with the first graft functioning after 20 years.
Socioeconomic status
One hundred and twenty patients could be contacted
to evaluate their socioeconomic status as defined by community of life, schooling, and employment (Table 7).
Three housewives gave birth to three children, and one
male recipient became a father. The professional profile
of the 61 patients with employment is listed in Table 8.
The economic profile of the transplanted patients was
quite similar to the general German population of the
age between 25 and 35 years, in which 9% were registered as unemployed in 1995 [16]. Ten of 35 patients
(29%) requesting dialysis postgraft failure were unemployed or unable to work, compared with 8 of 89 patients
(9%) with functioning grafts. This was a significant difference in the levels of unemployment (P 5 0.0045). Other
factors, such as the year of transplantation, did not influence the socioeconomic outcome.
DISCUSSION
The aim of treatment in chronic diseased children is
always to alleviate symptoms of their illness and to sup-
port them into becoming adults. Often evaluation of
outcome is hampered by the fact that adolescents are
transferred to adult units. This may be why only a few
reports exist on the long-term outcome of children with
end-stage renal failure into adulthood. Most reports regarding long-term results are focused on graft function
[7, 18, 19], and less is known about other factors that
determine the lifestyle of young adults who received
transplants during childhood [9, 20]. In our study, we
could follow the majority of children transplanted at
our unit during the 25 years and evaluate them into
adulthood.
The mortality rate of pediatric kidney transplantation
is low. In our study, 22 patients died either in childhood
or at adult age. The main causes of death were cardiovascular complications or severe infections, as described by
others [21]. In accordance to the observation by Reiss,
Wingen and Scharer [22], death can occur at any time
after transplantation. Single-center reports [24] as well
as cooperative registries in Europe (European Dialysis
and Transplant Association) [23] and North America
(North American Pediatric Renal Transplant Cooperative Study) [24] confirm more or less excellent survivals
(more than 80%) of children with end-stage renal failure
following kidney transplantation. As a result of this, the
number of young adults living with renal replacement
therapy increases continuously.
Graft survival is influenced by several factors such as
histocompatibility, ischemia time, immunosuppression,
and graft quality (for example, donor age, and living or
cadaveric sources) [24]. In our population, the best graft
survival rates were observed after living related donation, CsA immunosuppression, and pre-emptive transplantation. The benefit of CsA versus Aza immunosuppression is statistically significant only for the first seven
years after transplantation. Thereafter, the superior graft
survival under CsA disappeared. It is noteworthy that
under Aza, no further graft loss was observed after 15
years. The disappointing long-term results of CsA could
be caused either by CsA toxicity or chronic rejection.
Sutherland et al showed the evidence of CsA toxicity
[25], which was not confirmed by Burke et al [26]. Noncompliance is another important risk factor of late rejec-
Offner et al: Kidney transplanted children come of age
tion with graft failure especially in adolescent recipients
[27, 28]. We also observed an increase of graft loss 10
years after transplantation, which could be due to noncompliance in the age group between 15 and 20 years. However, no special investigations concerning noncompliance
were performed. The superiority of living related transplantation over cadaveric grafts was not significant. This
is in contrast to earlier reports from our own center [2]
and other cooperative studies [24], but confirms the data
from the Collaborative Transplant Study by Opelz [29].
The role of pre-emptive transplantation is discussed
controversially in the literature [30, 31]. Our results indicate that pre-emptive transplantation had no adverse influence on transplant outcome, but rather showed better
graft survival rates. This could not be explained by the
higher rates of LRD grafts in the pre-emptive group, as
a matched-pair analysis of our patients demonstrated [32].
This was also observed by Fine, Tejani and Sullivan [33].
Serum creatinine at six months after successful kidney
transplantation was postulated to be the best predicting
factor for long-term graft function [34, 35]. Our patients
with 10 or more years graft survival had a significantly
higher GFR at six weeks after transplantation than survivors below 10 years.
Hypertension is reported to be a further predictor of
long-term function [34]. In transplanted children, the
reported percentage of hypertension is high, about 70 to
80% [36, 37]. There was a significant correlation between
serum creatinine and hypertension in our adult recipients
transplanted in childhood. Patients with a normal blood
pressure had a normal serum creatinine concentration
below 100 mmol/liter, whereas the others showed elevated serum creatinines.
Hyperlipidemia is a further risk factor for cardiovascular complications [38]. In our analysis, serum cholesterol
was increased in both transplanted and dialyzed grownup patients (Table 5). Triglycerides were raised in only
dialyzed patients. Until now, our treatment of hyperlipidemia consisted of only dietetic recommendations, but
this approach needs re-evaluation in the context of more
effective lipid-lowering drugs [39].
One major effect of renal failure in children is growth
retardation [40]. Our study confirms this in long-term survivors on renal replacement therapy. With CsA immunosuppression combined with low-dose prednisolone, growth
retardation could be reduced significantly when compared
with Aza and a high-dose prednisolone regimen (P 5
0.038). In fact, the Aza prednisolone combination even
deteriorated height SDS (D height SDS 20.65), whereas
CsA and low-dose prednisolone showed a slight increase
from childhood to final height in adulthood (D height
SDS 10.03). Although the number of cystinotic patients
is small, the effect of the two immunosuppressive regimens was similar. These findings highlight the influence
of high-dose steroids on growth in children, but also
1515
demonstrate that CsA and low-dose prednisolone reveal
a tendency to normalize final height in noncystinotic
patients. Most reports with long-term results, which usually used higher steroid dosages, showed more pronounced growth retardation [18, 41]. Only seven of our
patients were treated with recombinant human growth
hormone (rhGH), because in the early years, the treatment was not available. Growth hormone after kidney
transplantation is effective and is often necessary especially if graft function is reduced, but there is still a
certain risk for graft rejection even in those with longterm stable graft function [42].
The risk of malignancy is a well-known complication
after organ transplantation, which is related to the intensity of immunosuppression [43]. In the Cincinnati Transplant Tumor Registry, a total of 316 tumors in 308 pediatric transplant recipients was reported by Penn in 1996
[44]. A German registry reported 18 tumors after kidney
transplantation [45]. In both studies, lymphomas were
the most common tumors. We observed a mixture of
tumor types but no skin cancers, unlike the Cincinnati
Transplant Tumor Registry [44].
Another aim of this study was to evaluate whether
children after renal transplantation have a realistic
chance to reach mature adulthood with good rehabilitation. The inquiry of 120 adult recipients, living in December 1995, exemplified an almost normal social rehabilitation after renal transplantation. Although most of the
young adults in this study were still living with their
parents, this seems to be characteristic for young adults
with chronic renal failure [46], in contrast to the German
population of the same age group [16]. The percentage
of employment is comparable with the age-matched population. Unemployment of 14% is very low considering
the background of chronic illness, frequent hospitalizations, clinic visits, and dialysis. Thirty percent of the
patients suffered from additional disabilities. Data from
the EDTA registry and from a single center described
unemployment of young adults with renal transplantation to range between 25 and 65%, depending on the
presence of concomitant disabilities, that is, hearing,
sight, or motor deficits [9, 47]. Successful pregnancies
are convincing indications of an adequate rehabilitation.
A questionnaire from EDTA concerning this topic gathered 820 successful pregnancies, with marked differences
between the several countries [48]. In Germany, the percentage of pregnancies was low as compared with Great
Britain, which is confirmed by our experience with only
three pregnancies in 72 female recipients and one offspring from a male transplant recipient.
In conclusion, the long-term survival rates of children
after renal transplantation and their degree of rehabilitation is encouraging, although the long-term graft function is still limited. Most of the long-term survivors have
experienced a declining graft function or even graft fail-
1516
Offner et al: Kidney transplanted children come of age
ures. The positive impact of renal transplantation on
quality of life is obvious and highlighted by our findings
of patient survival into adulthood. By improving graft
survival and function, and aiming for lifelong graft tolerance, these benefits could be sustained further.
18.
19.
ACKNOWLEDGMENTS
The successful renal replacement therapy of children and adolescents was only possible with the support and organization of Kuratorium
fur Heimdialyse und Nierentransplantation (KfH) in Neu-Isenburg,
Germany, and Eurotransplant in Leiden, Netherlands. In addition, we
thank Dr. Nadeem Moghal for his critical review and comments.
Reprint requests to Gisela Offner, M.D., Kinderklinik, Kinderklinik
der Medizinischen Hochschule Hannover, Carl Neubergstrasse 1, 30623
Hannover, Germany.
20.
21.
22.
23.
REFERENCES
1. Starzl TL, Marchioro TL, Porter KA, Faris TD, Carey TA:
The role of organ transplantation in pediatrics. Clin North Am
13:381422, 1966
2. Offner G, Hoyer PF, Pichlmayr R, Brodehl J: Langfristige Prognose nach Nierentransplantation im Kindesalter. Monatsschr Kinderheilkd 10:488492, 1996
3. Potter DE, Najarian J, Belzer F, Holliday MA, Horn G, Salvatierra JRO: Long-term results of renal transplantation in children.
Kidney Int 40:752756, 1991
4. Lee HM, Posner MP, King AL, Brown KB, Reams DR: Status
of long-term (25 years) survivors of kidney transplant patients.
Transplant Proc 24:27112713, 1997
5. McDonald RA, Watkins SL: Progress in renal transplantation
for children. Adv Renal Replace Ther 3:154165, 1997
6. Laine J, Holmberg C, Hayry P: Chronic rejection and late renal
allograft dysfunction. Pediatr Nephrol 10:221229, 1996
7. Ruder H: Nierentransplantation im Kindes-und Jugendalter.
Monatsschr Kinderheilkd 144:951964, 1996
8. Paul LC: Chronic renal transplant loss. Kidney Int 47:14911499,
1995
9. Querfeld U, Korten B, Naumann G, Michalk DV: Medical
and psychosocial rehabilitation of young adults receiving renal
replacement therapy since childhood: A single-centre experience.
Nephrol Dial Transplant 12:3337, 1997
10. Reynolds JM, Morton MJ, Gerralda ME, Postlethwaite RJ,
Goh D: Psychosocial adjustment of adult survivors of a pediatric
dialysis and transplant programme. Arch Dis Child 68:104110,
1993
11. Morel P, Almond PS, Matas AJ, Gillingham KJ, Chau C,
Brown A, Kashtan CE, Mauer SM, Chavers B, Nevins TE,
Dunn DL, Sutherland der Payne WD, Najarian JS: Long-term
quality of life after kidney transplantation in childhood. Transplantation 52:4753, 1991
12. Offner G, Brandis M, Brodehl J, Krohn HP, Pichlmayr R,
Tidow G: Nierentransplantation bei Kindern in Hannover. Dtsch
Med Wochenschr 104:393401, 1979
13. Offner G, Hoyer PF, Brodehl J, Pichlmayr R: Cyclosporine A
in paediatric kidney transplantation. Pediatr Nephrol 1:125130,
1987
14. Kaplan EL, Meier P: Nonparametric estimation from incomplete
observations. J Am Stat Assoc 53:457481, 1958
15. Reinken L, van Oost G: Longitudinale Korperentwicklung gesunder Kinder von 0 bis 18 Jahre. Klin Padiatr 204:129133, 1992
16. Statistisches Bundesamt: Bevolkerung im April 1994 nach Beteiligung am Erwerbsleben, Familienstand, uberwiegenden Lebensunterhalt und Altersgruppen, in Statistisches Jahrbuch 1995 fur die
Bundesrepublik Deutschland. edited by Statistisches Bundesamt,
Stuttgart, Metzler & Poeschl, 1995, p 39
17. Hoyer PF, Krohn HP, Offner G, Byrd DJ, Brodehl J, Wonigeit
K, Pichlmayr R: Renal function after kidney transplantation in
children: A simple estimate of glomerular filtration rate in children
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
derived from body length and plasma creatinine. Transplantation
43:489493, 1987
Hokken-Koelega ACS, Van Zaal MAE, Van Bergen W, De
Ridder MAJ, Stijnen T, Wolff ED, De Jong RCJW, Donckerwolcke RA, Keizer-Schrama SM, Drop SLS: Final height and
its predictive factors after renal transplantation in childhood. Pediatr Res 36:323328, 1994
Chavers B, Kim E-M, Matas AJ, Gillingham KJ, Najarian JS,
Mauer SM: Causes of kidney allograft loss in a large pediatric
population at a single center. Pediatr Nephrol 8:5761, 1994
Gamperli A, Leumann E, Neuhaus TJ, Schlumpf R, Largiader
F: 25 years of pediatric dialysis and transplantation in Zurich.
Schweiz Med Wochenschr 126:7785, 1996
Neiberger R, Schwalbe M, Pena D, Fennell R, Massengill SF,
Cantor A: Cause of death for children on chronic dialysis: A 20year analysis. Dial Transplant 24:7891, 1997
Reiss U, Wingen A-M, Scharer K: Mortality trends in pediatric
patients with chronic renal failure. Pediatr Nephrol 10:4145, 1996
Broyer M, Chantler C, Donckerwolcke R, Ehrich JHH, Rizzoni G, Scharer K: The paediatric registry of the European Dialysis and Transplant Association: 20 years experience. Pediatr
Nephrol 7:758768, 1993
Avner ED, Chavers B, Sullivan EK, Sutherland DER: Renal
transplantation and chronic dialysis in children and adolescents:
The 1993 annual report of the North American Pediatric Renal
Transplant Cooperative Study. Pediatr Nephrol 9:6173, 1995
Sutherland F, Burgess E, Klassen J, Buckle S, Paul LC: Posttransplant conversion from cyclosporin to azathioprine: Effect on
cardiovascular risk profile. Transplant Int 6:129132, 1993
Burke JF jr, Pirsch JD, Ramos EL, Salomon DR, Stablein DM,
Van Buren DH, West JC: Long-term efficacy and safety of
cyclosporine in renal transplant recipients. N Engl J Med 331:358
363, 1994
Meyers KEC, Thomson PD, Weiland H: Noncompliance in children and adolescents after renal transplantation. Transplantation
62:186189, 1996
Warady BA, Mudge C, Wiser B, Wiser M, Rader B: Transplant
allograft loss in the adolescent patient. Adv Renal Replace Ther
3:154165, 1996
Opelz G: Collaborative transplant study: 10-year-report. Transplant Proc 24:23422355, 1992
Cole BR: The psychosocial implication of pre-emptive transplantation. Pediatr Nephrol 5:158161, 1991
Nevins TE, Danielson G: Prior dialysis does not affect the outcome of pediatric renal transplantation. Pediatr Nephrol 5:211214,
1991
Offner G, Hoyer PF, Meyer B, Pichlmayr R, Brodehl J: Preemptive renal transplantation in children and adolescents. Transplant Int 6:244249, 1993
Fine RN, Tejani A, Sullivan EK: Pre-emptive transplantation in
children: Report of North American Pediatric Renal Transplant
Cooperative Study (NAPRTCS). Clin Transplant 8:474478, 1994
Cole E, Naimark D, Cattran D, Pei Y, Fenton S, Robinette M,
Zaltsman J, Bear R, Cardella C: An analysis of predictors of
long-term cadaveric renal allograft survival. Clin Transplantation
9:282288, 1995
Yilmaz S, Yilmaz A, Havry P: Chronic renal allograft rejection
can be predicted by area under the serum creatinine versus time
curve (AUCcr). Kidney Int 9:251258, 1995
Gordjani N, Offner G, Hoyer PF, Brodehl J: Hypertension after
renal transplantation in patients with cyclosporin and azathioprine.
Arch Dis Child 65:275279, 1990
Broyer M, Gagnadoux MF, Guest G, Beurton D, Niaudet P,
Habib R, Busson M: Kidney transplantation in children: Results
of 383 grafts performed at Enfants Malades Hospital from 1973
to 1984. Adv Nephrol 16:307334, 1987
Sharma AK, Myers TA, Hunninghake DB, Matas AJ, Kashtan
CE: Hyperlipidemia in long-term survivors of pediatric renal transplantation. Clin Transplant 8:252257, 1994
Massy ZA, Kasiske BL: Hyperlipidemia and its management in
renal disease. Curr Opin Nephrol Hypertens 5:141146, 1997
Toenshoff B, Mehls O: Growth retardation in children with
Offner et al: Kidney transplanted children come of age
41.
42.
43.
44.
chronic renal insufficiency: Current aspects of pathophysiology and
treatment. J Nephrol 8:133142, 1995
Fine RN, Stablein DM, Tejani A: Do children exhibit catch-up
growth post transplant: North American Pediatric Renal Transplant Cooperative Study special study. Pediatr Nephrol 9:S66S68,
1995
Broyer M: Results and side-effects of treating children with growth
hormone after kidney transplantation: A preliminary report. Acta
Paediatr 417:7679, 1996
Warady BA, Hebert D, Sullivan EK, Alexander SR, Tejani
A: Renal transplantation, chronic dialysis, and chronic renal insufficiency in children and adolescents. The 1995 annual report of the
North American Pediatric Renal Transplant Cooperative Study.
Pediatr Nephrol 11:4964, 1997
Penn I: Malignancy in children, in Pediatric Renal Transplantation,
edited by Tejani AH, Fine RN, New York, Toronto, Singapore,
Wiley-Liss, 1994, p 461
1517
45. Wingen A-M: German multicenter analysis of malignancies following renal replacement therapy in children, in Cancer in Transplantation, Prevention and Treatment, edited by Touraine JL, Amsterdam, Kluwer Academic, 1996, p 25
46. Rosenkranz J, Bonzel KE, Bulla M, Michalk D, Offner G,
Reichwald-Klugger E, Scharer K: Psychosocial adaptation of
children and adolescents with chronic renal failure. Pediatr Nephrol
6:459463, 1992
47. Rizzoni G, Ehrich JHH, Broyer M, Brunner FP, Brynger H,
Fassbinder W, Geerling W, Selwood NH, Tufveson G, Wing AJ:
Rehabilitation of young adults during renal replacement therapy in
Europe. 1. The presence of disabilities. Nephrol Dial Transplant
7:573578, 1992
48. Ehrich JHH, Loirat C, Davison JM, Rizzoni G, Wittkop B,
Selwood NH: Repeated successful pregnancies after kidney transplantation in 102 women (report by the EDTA Registry). Nephrol
Dial Transplant 11:13141317, 1996
You might also like
- Signal Trunduction2Document6 pagesSignal Trunduction2Eka RahmawatiNo ratings yet
- PJT PM KwidDocument64 pagesPJT PM KwidEka RahmawatiNo ratings yet
- Stunting (EDIT)Document62 pagesStunting (EDIT)Eka RahmawatiNo ratings yet
- Contoh Gambar ShabuDocument2 pagesContoh Gambar ShabuEka RahmawatiNo ratings yet
- PHMT 15305 Physical Growth in Children With Transfusion Dependent Thala 020811Document7 pagesPHMT 15305 Physical Growth in Children With Transfusion Dependent Thala 020811Eka RahmawatiNo ratings yet
- Principal of Clinical CytogeneticsDocument21 pagesPrincipal of Clinical CytogeneticsEka RahmawatiNo ratings yet
- Jpids Piu107 Full-1Document6 pagesJpids Piu107 Full-1Eka RahmawatiNo ratings yet
- Ballard Score PDFDocument1 pageBallard Score PDFEka RahmawatiNo ratings yet
- Parathyroid Hormone in Pediatric Patients With B-Thalassemia Major and Its Relation To Bone Mineral Density A Case Control StudyDocument4 pagesParathyroid Hormone in Pediatric Patients With B-Thalassemia Major and Its Relation To Bone Mineral Density A Case Control StudyEka RahmawatiNo ratings yet
- Compensatory Kidney Growth in Children With Urinary Tract Infection and Unilateral Renal Scarring: An Epidemiologic StudyDocument6 pagesCompensatory Kidney Growth in Children With Urinary Tract Infection and Unilateral Renal Scarring: An Epidemiologic StudyEka RahmawatiNo ratings yet
- Long-Term Results of Renal Transplantation in ChildrenDocument5 pagesLong-Term Results of Renal Transplantation in ChildrenEka RahmawatiNo ratings yet
- Parathyroid Hormone in Pediatric Patients With B-Thalassemia Major and Its Relation To Bone Mineral Density A Case Control StudyDocument4 pagesParathyroid Hormone in Pediatric Patients With B-Thalassemia Major and Its Relation To Bone Mineral Density A Case Control StudyEka RahmawatiNo ratings yet
- Contoh Gambar ShabuDocument2 pagesContoh Gambar ShabuEka RahmawatiNo ratings yet
- Monte Lucas TDocument12 pagesMonte Lucas TEka RahmawatiNo ratings yet
- The Importance of MTHFR, MTR, MTRRDocument30 pagesThe Importance of MTHFR, MTR, MTRREka RahmawatiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Proteinuria During Dengue Fever In: ChildrenDocument13 pagesProteinuria During Dengue Fever In: ChildrenSameeh MohNo ratings yet
- The Hepatorenal Syndrome: 11 Pathophysiology and Treatment Ofascites andDocument27 pagesThe Hepatorenal Syndrome: 11 Pathophysiology and Treatment Ofascites andJose JulcaNo ratings yet
- Maternal Adaptations To PregnancyDocument3 pagesMaternal Adaptations To PregnancyHeidi Paola Estoista100% (1)
- RhubarbDocument16 pagesRhubarbAN MarcosNo ratings yet
- Recording of Fluid Balance Intake-Output PolicyDocument7 pagesRecording of Fluid Balance Intake-Output PolicyRao Rizwan ShakoorNo ratings yet
- The Dialysis of Drugs 2011 PDFDocument68 pagesThe Dialysis of Drugs 2011 PDFVashistmohan A.P.No ratings yet
- QIMP14 AppendixDocument12 pagesQIMP14 AppendixShahriar MostafaNo ratings yet
- Nursing Care of Patients With Diabetes MellitusDocument43 pagesNursing Care of Patients With Diabetes MellitusRashida RuwaNo ratings yet
- StatgoodDocument8 pagesStatgoodArpanpatelNo ratings yet
- Pex 09 03 PDFDocument4 pagesPex 09 03 PDFGrelsarianiNo ratings yet
- Focus Charting of FDocument12 pagesFocus Charting of FRobert Rivas0% (2)
- Kidney Health PDFDocument77 pagesKidney Health PDFAnonymous CQSNUSNo ratings yet
- Diabetic Nephropathy BaruDocument24 pagesDiabetic Nephropathy BaruRobiyanti Nur Chalifah HattaNo ratings yet
- MS Exam 2Document34 pagesMS Exam 2David LopezNo ratings yet
- Biochemical Profiles and Individual Biochemical ParametersDocument13 pagesBiochemical Profiles and Individual Biochemical Parametersbiotech_vidhyaNo ratings yet
- Fluid Volume Excess CRFDocument3 pagesFluid Volume Excess CRFDana Fajardo RezanoNo ratings yet
- Medicine June 2009: Fcps Part1 Q BankDocument14 pagesMedicine June 2009: Fcps Part1 Q Bankqudsia_niaziNo ratings yet
- 60-2005 - Pregestational Diabetes MellitusDocument11 pages60-2005 - Pregestational Diabetes MellitusGrupo Atlas100% (1)
- Peroxisome Proliferato-Activated Receptor AlphaDocument10 pagesPeroxisome Proliferato-Activated Receptor Alphaadam shingeNo ratings yet
- Acute Renal Failure TeoriDocument24 pagesAcute Renal Failure TeoriVera Andri YaniNo ratings yet
- PolitzerDocument47 pagesPolitzerMuhammad Ahyad FaqihNo ratings yet
- Pedia Notes Compilation MKDoseDocument18 pagesPedia Notes Compilation MKDosemefav7778520No ratings yet
- 21 TranslatedDocument71 pages21 TranslatedMerry MonroeNo ratings yet
- Sindrome Uremico UptodateDocument14 pagesSindrome Uremico UptodateArmin El Kallo PalmaNo ratings yet
- Blood Test of KFTDocument3 pagesBlood Test of KFTRaghvendra RathoreNo ratings yet
- Empagliflozin Metformin HCL: Jardiance Duo®Document2 pagesEmpagliflozin Metformin HCL: Jardiance Duo®Lord Carlo CabangalNo ratings yet
- Insuficiencia Renal CronicaDocument13 pagesInsuficiencia Renal CronicaCarlos DNo ratings yet
- Workshop CRRT PDFDocument88 pagesWorkshop CRRT PDFDesy rahmatNo ratings yet
- Normal GFR in ChildDocument8 pagesNormal GFR in ChildbobbypambudimdNo ratings yet
- AmLyte 13 Package Insert-EnDocument21 pagesAmLyte 13 Package Insert-EnGuneyden GuneydenNo ratings yet