Professional Documents
Culture Documents
Status of Lipid Profile in Pregnancy
Uploaded by
yosua simarmataCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Status of Lipid Profile in Pregnancy
Uploaded by
yosua simarmataCopyright:
Available Formats
NATIONAL JOURNAL OF MEDICAL RESEARCH
ORIGINAL ARTICLE
STATUS OF LIPID PROFILE IN PREGNANCY
Deepak Parchwani1, Digisha Patel2
1Associate
Professor, Biochemistry Department, Gujarat Adani Institute of Medical Sciences, Bhuj, Gujarat 2M.Sc
(Medical, Physiology) Student, GSL Medical College, Rajahmundry (AP)
Correspondence:
Dr Deepak Parchwani
H/No-B/17, New G.K.General Hospital,
Gujarat Adani Institute of Medical Sciences , Bhuj (Guj)
E-mail: drdparchwani@gmail.com,
Mobile: 917600024672
ABSTRACT
Pregnancy greatly increases demand for metabolic fuels that are needed for growth and development of the fetus
and its support structures. The total gestation related energy cost has been estimated at approximately 83000 kcal.
The major change in energy expenditure and in the accumulation of fat occurs at different times during pregnancy.
In the current study a serial study of serum lipids was performed in a group of women throughout gestation and six
weeks post partum while they were having their usual diet and unrestricted daily activity. The control group
consisted of non pregnant healthy women of child bearing age. Data was analyzed by SPSS software. All lipid
fractions underwent a gradual and persistent rise throughout pregnancy with the exception of HDL-C i.e. a
progressive rise was observed in serum total cholesterol, serum triglyceride, serum VLDL and LDL-C as pregnancy
advances, while serum HDL-C showed a biphasic pattern, as initial rise and then decline in later third of pregnancy.
However, during early pregnancy the values of all lipid fractions do not differ significantly from those for normal
non pregnant controls. No significant difference was observed in vegetarian and non-vegetarian group in any of the
lipid fractions in different trimester of pregnancyso diet had no significant influence on lipid synthesis during
pregnancy.
KEYWORDS: Lipid profile, pregnancy, fetus, cholesterol
INTRODUCTION
Physiologically, the mother becomes almost a new
person during the period of pregnancy. Profound local
and systemic changes in maternal physiology are
initiated by conception and continued throughout
pregnancy.1Advancement of pregnancy is accompanied
by the extra demand of energy. As pregnancy
progresses, a well-integrated metabolic shift occurs to
ensure an adequate supply of nutrients to a constantly
feeding fetus from an intermittently fasting and feeding
mother. During early pregnancy, maternal metabolic
environment is modified by a rise in serum levels of
estrogen and progesterone, pancreatic beta-cell
hyperplasia occurs and there is an increase in the
secretion of insulin.2 Hyperinsulinemia leads to an
increase in peripheral glucose utilization, a decline in
fasting plasma glucose levels, increased tissue storage of
glycogen, increased storage of fats and decreased
lipolysis. Freinkel3 was the first to describe the maternal
metabolic changes of late pregnancy as accelerated
starvation, when food is unavailable and facilitated
anabolism when food is ingested. Maternal fuel
adjustments during late pregnancy include a sparing of
Vol 1 Issue 1 July Sept 2011 : ISSN 2249 -4995
glucose (for the fetus) and an increased concentration
of fatty acids in plasma.
It is known that high concentrations of many of the
steroids occur as normal pregnancy advances. Since
cholesterol is the source of most of the steroids found
in increased amounts in the circulation of normal
pregnant patients, the part played by lipid metabolism
in pregnancy, becomes all the more intriguing as
cholesterol is a major factor for the development of
atherosclerosis.Chauffard4 in 1911 undertook the first
chemical study of blood lipids during pregnancy and
suggested that an increase occurs in the cholesterol
level. With the development of more modern
techniques various studies observed an increase in
various lipid fractions, though the increase was neither
consistent in time of appearance nor proportion of
changes in various fractions. Most authors believe that
the increase in blood lipids is related to the
requirements of the fetus and to development of the
mammary apparatus. Thus hyperlipidemia is a normal
prenatal finding but many questions in this field
remained unanswered, such as those pertaining to the
exact relationship among the lipid changes during
pregnancy. Thus in the present study an attempt has
been bade to define more precisely the changes in lipid
Page 10
NATIONAL JOURNAL OF MEDICAL RESEARCH
fractions during different periods of gestation and at six
weeks post partum.
MATERIAL AND METHOD
A total of 325 women were enrolled and the study was
carried out from September 2009 to May 2011. They
were divided as:
Control group: Comprised 100 non-pregnant, healthy
women having normal menstrual function with no
evident hormonal deficiency. Among these 59 were
vegetarians, while 41 were non-vegetarians.
Study group: Comprised 225 pregnant women, further
subdivided into two types according to their dietary
habits:
Group I (n=134): Vegetarian women.
Group II (n=91): Non-vegetarian women.
Mean values of age, blood pressure, BMI and other
anthropometric parameters did not significantly differ
between the groups studied. Fasting blood samples
were collected from all the subjects. The blood was
drawn into plain tubes and subjected to estimation of
lipid profile (Serum Cholesterol by modified
Roeschlaus method5, Serum triglyceride by McGrowan
method.6, HDL C by Bursteim et al method7, VLDL
and LDL C was calculated by Friedewalds formula8).
The same lipid profile estimation was also carried out
in study group six weeks post partum.
Data analysis was performed with the SPSS statistical
software. The results for continuous variables are mean
+ S.D. Student t test for independent samples, analysis
of variance (ANOVA) were used in the assessment of
the significance of difference between group means.
RESULTS
Table 1 and 2 shows the mean values of lipid profile in
non-pregnant and pregnant vegetarian and nonvegetarian women respectively, important findings are:
x No significant difference was observed in the values
of serum total cholesterol, serum triglycerides, serum
HDL-C, serum VLDL and LDL-C during early
pregnancy as compared to normal non-pregnant
controls.
x A progressive rise was observed in serum total
cholesterol, serum triglyceride, serum VLDL and
LDL-C as pregnancy advances, while serum HDL-C
showed a biphasic pattern, as initial rise and then
decline in later third of pregnancy.
x No significant difference was observed in vegetarian
and non-vegetarian group in any of the lipid fractions
in different trimester of pregnancy.
x Various lipid fractions decreased considerably at
sixth weeks post partum, but still remained
significantly elevated from control group.
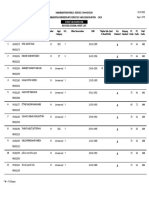
Table 1: Lipid Profile values in non-pregnant and pregnant vegetarian subjects.
Vegetarian
Group I (n=134)
Parameters
control subjects
I trimester
II trimester
III trimester
(n=59)
Total cholesterol (mg/dl)
169.4+32.6
182.9+31.4
222.4+34.7*
251.7+44.6
Triglycerides (mg/dl)
81.3+15.9
84.4+12.2
141.3+25.1*
226.8+43.5
HDL-C (mg/dl)
46.7+5.7
47.0+6.3
55.6+5.5*
51.1+6.3
VLDL-C (mg/dl)
16.2+3.1
16.8+5.8
28.2+8.4*
45.3+9.7
LDL-C (mg/dl)
103.1+19.2
114.1+20.2
132.6+21.6*
154.3+25.2
* p<0.05 (II trimester Vs control group; II trimester Vs I trimester)
p<0.01 (III trimester Vs control group; III trimester Vs I trimester)
p<0.05 (Six weeks post partum Vs control group)
DISCUSSION
Present study shows that serum total cholesterol and
serum triglyceride levels increased markedly during
pregnancy. Although the total cholesterol increased to
maximum in the third trimester, maximum rate of
increase occurred during second trimester. Serum
triglyceride concentration remained constant until the
first trimester, gradually increasing thereafter until
delivery. At this time the triglyceride level was 2.8 times
higher than that of non-pregnant group.
Hypertriglycridemia of pregnancy is distinguished from
other hypertriglyceridemias by an increase or
maintenance of high density lipoprotein cholesterol.
Thus fat appears to be the main form of stored energy
in pregnancyAs fat deposition, increases early during
the first half of pregnancy, reaching a peak before week
30, and finally mobilization and diminish storage in late
gestation. The interpretation for this is that the
Vol 1 Issue 1 July Sept 2011 : ISSN 2249 -4995
Six weeks post
partum
202.9+26.6
117.6+12.4
47.4+6.1
23.8+2.4
132.3+22.5
hypothalamic center somehow becomes awakened to
the degree of maternal adiposity. Although the
mechanism for the more sensitive regulation of
appetite in pregnancy is still unknown, a more
important is that the increases in the adipose tissue
store anticipates the late gestation fetal growth spurt by
beginning in early gestation and reaching a maximum in
mid gestation.9
No significant change in the lipoprotein cholesterol
level occurred during the first trimester. During the
second trimester HDL-C and VLDL increased
progressively. In the third trimester HDL-C showed a
slight decline from the second trimester values, whereas
the LDL-C rose by about 30% from second trimester.
The most striking alternation occurred in the VLDL
which increased approximately 180% above the value
in non-pregnant women. Herrera10, has suggested that
rise in triglyceride provides maternal fuel, saving the
glucose for the fetus. The rise in LDL-C appears to be
Page 11
NATIONAL JOURNAL OF MEDICAL RESEARCH
necessary for placental steroidogenesis. The rise in
triglyceride parallels the rise in estrogen levels during
pregnancy. The rise in triglyceride rich VLDL particles
during pregnancy is dependent more on an increased
rate of synthesis caused by estrogens than on a decrease
in the rate of removal10. The increase in estrogen levels
during late pregnancy theoretically should decrease the
level of LDL-C. This, however, does not occur and
instead, elevations in LDL-C and apo-B are observed.
They could be secondary phenomena caused by
increased conversion of the abundant VLDL. High
progesterone levels during late pregnancy also could be
a contributing factor. The initial increase HDL-C is
estrogen dependent, while falling HDL-C in the last
half of pregnancy, along with LDL-C changes, correlate
with rising levels of human placental lactogen, insulin
and insulin resistance10.
Table 2: Lipid Profile values in non-pregnant and pregnant non-vegetarian subjects.
Parameters
Group II (n=91)
Non-vegetarian
control subjects
I trimester
II trimester III trimester Six weeks post
(n=41)
partum
Total cholesterol (mg/dl)
176.9+27.1
188.3+32.6
225.4+31.6* 253.8+43.9 212.2+24.1
Triglycerides (mg/dl)
97.7+19.4
103.5+17.7
152.1+29.5* 238.2+40.8 125.9+13.4
45.7+5.2
54.1+5.7*
50.4+6.5
46.1+5.7
HDL-C (mg/dl)
45.3+6.1
VLDL-C (mg/dl)
19.2+6.6
22.2+7.0
30.4+9.9*
48.1+10.3
24.8+4.4
123.3+20.4
135.2+23.1* 155.8+24.9 143.3+20.2
LDL-C (mg/dl)
114.1+21.1
* p<0.05 (II trimester Vs control group; II trimester Vs I trimester)
p<0.01 (III trimester Vs control group; III trimester Vs I trimester)
p<0.05 (Six weeks post partum Vs control group)
Serum total cholesterol and triglyceride levels fell after
delivery, but remained elevated in comparison to
control group. Further, it was observed that there was
no significant difference in lipid profile parameters in
vegetarian and non-vegetarian subjectsso diet had no
significant influence on lipid synthesis during
pregnancy.
REFERENCES
1.
2.
3.
Kortenoever
M.
Physiological
changes
in
pregnancy.1960;21:443-5.
Kalkhoff RK. Metabolic effects of progesterone.Am J Obst
Gynae.1982;142:735-7.
Freinkel N. Effect of the conceptus on maternal metabolism
during pregnancy. Excerpta Medica. 1964;12:679-81.
Vol 1 Issue 1 July Sept 2011 : ISSN 2249 -4995
4.
5.
6.
7.
8.
9.
10.
Chauffard A, Laroche G, Grigaut A. Blood lipids in pregnancy.
Obstetriqie. 1911;4:481-2.
Roeschlau P, Bernt E, Gruber WA. Enzymatic analysis of total
cholesterol. Clin Chem Clin Biochem.1974;12:226 8.
Mcgowan MW, Fossati, P, Prencipe L. Enzymatic analysis of
plasma triglyceride. Clin Chem.1982;28:2077 2078.
Burstein M, Scholnic, HR, Morfin R. Enzymatic analysis of
plasma HDL- C. J lipid Res. 970;24:204 6.
Friedwald WY, Levy RI, Fredrickson, DS. Estimation of
concentration of LDL C in plasma without use of the
preparative ultracentrifuge. Clin Chem.1972;18:499 501.
Knopp RH, Saudek CD, Arky RA, Osullivan JB. Two phases
of adipose tissue metabolism in pregnancy. Maternal
adaptations for fetal growth. Endocrinology.1973;92:984-6.
Herrera E. Metabolic adaptations in pregnancy and their
implications for the availability of substrates to the fetus. Eur J
Clin Nutr.2001;54:547-49.
Page 12
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- IGCSE Biology (O610) Workbook: Balanced DietDocument5 pagesIGCSE Biology (O610) Workbook: Balanced DietPatrick Abidra100% (1)
- Uog 22013 PDFDocument21 pagesUog 22013 PDFyosua simarmataNo ratings yet
- 1190922Document48 pages1190922Ahiem ConcoyNo ratings yet
- DR Anna Mira Lubis - Diagnostic Approach of ThrombocytopeniaDocument36 pagesDR Anna Mira Lubis - Diagnostic Approach of Thrombocytopeniayosua simarmataNo ratings yet
- 2013 Thrombocytopenia Pocket Guide PDFDocument4 pages2013 Thrombocytopenia Pocket Guide PDFYessy SuziartyNo ratings yet
- Aspirin in LupusDocument8 pagesAspirin in Lupusyosua simarmataNo ratings yet
- Guideline ACOG Diagnostic Imaging During Pregnancy PDFDocument7 pagesGuideline ACOG Diagnostic Imaging During Pregnancy PDFyosua simarmata100% (1)
- Acr Practice Guideline For Imaging Pregnant or Potentially Pregnant Adolescents and Women With Ionizing RadiationDocument15 pagesAcr Practice Guideline For Imaging Pregnant or Potentially Pregnant Adolescents and Women With Ionizing RadiationBenjamin LimNo ratings yet
- IJHPM - Volume 7 - Issue 12 - Pages 1073-1084 Complex LeadershipDocument12 pagesIJHPM - Volume 7 - Issue 12 - Pages 1073-1084 Complex Leadershipkristina dewiNo ratings yet
- DebateDocument12 pagesDebate•Kai yiii•No ratings yet
- Hospital Pharmacy Communication - NewsletterDocument5 pagesHospital Pharmacy Communication - Newsletterjuveria nausheenNo ratings yet
- Oregon SOS Audit On Child WelfareDocument49 pagesOregon SOS Audit On Child WelfareSinclair Broadcast Group - Eugene100% (1)
- Antibiotics ResistanceDocument8 pagesAntibiotics ResistanceboredtarteelNo ratings yet
- Human and Health Rights in Relation To Sustainable2Document17 pagesHuman and Health Rights in Relation To Sustainable2ptkabworldNo ratings yet
- Teacher EducationDocument32 pagesTeacher Educationsoumya satheshNo ratings yet
- Pro-Oxidant Strategies - Cancer Treatments ResearchDocument71 pagesPro-Oxidant Strategies - Cancer Treatments ResearchSpore FluxNo ratings yet
- Tcharestresumefinal 1009Document2 pagesTcharestresumefinal 1009tcharestNo ratings yet
- The Influence of Music in Horror Games (Final Draft)Document7 pagesThe Influence of Music in Horror Games (Final Draft)Panther LenoXNo ratings yet
- Alternatives To Hydrazine MHI PaperDocument5 pagesAlternatives To Hydrazine MHI PaperjycortesNo ratings yet
- Components of Fitness, PARQ and TestingDocument29 pagesComponents of Fitness, PARQ and TestingLynNo ratings yet
- Maharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019Document59 pagesMaharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019S KatyarmalNo ratings yet
- Letters of Intent (Cover Letters)Document6 pagesLetters of Intent (Cover Letters)anca_ramona_s0% (1)
- Prescribing For Transgender Patients ELHEDocument4 pagesPrescribing For Transgender Patients ELHEGe YgayNo ratings yet
- Tea and Industrial RevolutionDocument4 pagesTea and Industrial RevolutionPhuong NguyenNo ratings yet
- Oral Medicine Dissertation TopicsDocument6 pagesOral Medicine Dissertation TopicsWriteMyPersuasivePaperSingapore100% (1)
- Predicting and Controlling Influenza Outbreaks - Published Article - IJERSTE - Vol.12 Issue 2, Feb 2023Document4 pagesPredicting and Controlling Influenza Outbreaks - Published Article - IJERSTE - Vol.12 Issue 2, Feb 2023dimple kharwarNo ratings yet
- Care ReportDocument23 pagesCare ReportSindi Muthiah UtamiNo ratings yet
- Response To States 4.2 Motion in Limine Character of VictimDocument10 pagesResponse To States 4.2 Motion in Limine Character of VictimLaw of Self DefenseNo ratings yet
- Physiological Changes Postpartum PeriodDocument2 pagesPhysiological Changes Postpartum PeriodEurielle MioleNo ratings yet
- Comprehensive Exam in Nursing Part 2Document41 pagesComprehensive Exam in Nursing Part 2Ariane-Gay Cristobal DuranNo ratings yet
- Mr. Maroof Khan: Speech and Language Pathologist/TherapistDocument15 pagesMr. Maroof Khan: Speech and Language Pathologist/TherapistshamsNo ratings yet
- Lecture in Geriatrics Physical Therapy 1Document27 pagesLecture in Geriatrics Physical Therapy 1S.ANo ratings yet
- Coordination Group For Mutual Recognition and Decentralised Procedures - Human (CMDH)Document12 pagesCoordination Group For Mutual Recognition and Decentralised Procedures - Human (CMDH)aslkdjNo ratings yet
- Blood Testing For DioxinsDocument2 pagesBlood Testing For DioxinstedmozbiNo ratings yet
- Module One Wellness Plan: GO TO FILE - Choose SAVE AS - Save A Copy of This To Your Computer!Document8 pagesModule One Wellness Plan: GO TO FILE - Choose SAVE AS - Save A Copy of This To Your Computer!Marko DesnicaNo ratings yet
- Shisha: GNS By: Lingaiswaran S/O BalasupramaniamDocument13 pagesShisha: GNS By: Lingaiswaran S/O BalasupramaniamLinga IngloriousNo ratings yet
- Bassam Osman ResumeDocument4 pagesBassam Osman ResumeBassam OsmanNo ratings yet