Professional Documents
Culture Documents
Fluidos y Electrolitos
Uploaded by
JavierCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fluidos y Electrolitos
Uploaded by
JavierCopyright:
Available Formats
Article
fluid & electrolytes
Fluid and Electrolytes:
Parenteral
Fluid Therapy
Kenneth B. Roberts, MD*
Objectives
After completing this article, readers should be able to:
1. Relate maintenance fluid and electrolyte needs to metabolic rate rather than to body
weight.
2. Recognize the differences in mild, moderate, and severe deficits among infants
compared with children or adults when expressed as percentage of body weight.
3. Describe the indication for a bolus and specify the amount and composition.
4. Specify a rehydration plan without the use of a calculator for an infant who has
moderate dehydration.
5. List the measures most valuable for monitoring the state of hydration.
Introduction
Parenteral fluid therapy is a basic component of the care of hospitalized infants and
children. Clinicians who care for inpatients must be able to assess the need for parenteral
fluid therapy and to specify the composition of fluid and rate of administration. Fluid and
electrolyte problems can be challenging but generally can be tamed by an organized
approach, application of a few principles of physiology, and careful monitoring of the
patient. It can be useful to consider separately the amount of fluid needed and the
electrolyte composition for maintenance needs, deficit, and ongoing losses (Table 1).
Because maintenance is not as directly related to weight as deficit or as directly measureable
as ongoing losses, it tends to cause the most confusion. It will, therefore, be discussed first
and in more detail than deficit or ongoing losses.
Maintenance: Fluid
The key to understanding maintenance fluid and electrolyte needs is recognizing that they
stem from basal metabolism (Fig 1). Metabolism creates two by-products, heat and solute,
that need to be eliminated to maintain homeostasis. Heat is dissipated largely by the
insensible evaporation of water from the skin surface. (Active sensible skin loss
sweatingis added only when there is an additional heat burden and is not considered part
of maintenance.) Elimination of warmed water vapor from the upper respiratory tract
during exhalation also contributes to insensible fluid loss. Soluble waste by-products of
metabolism are excreted in the urine.
Metabolic rate is not related directly to weight and is expressed in units of energy (kcal
or joules). When compared with body weight, basal metabolic rate is high in the newborn
period and much lower in adulthood, and the transition is not linear (Fig 2). Because
metabolic rate per unit of body weight declines with increasing age, children generate less
heat and solute from basal metabolism than do infants and, therefore, need less fluid and
electrolytes per unit of body weight. Adolescents and adults generate less heat and solute
from basal metabolism than do children or infants and, therefore, need less fluid and
electrolytes per unit of body weight. Although the amount of fluid and electrolytes declines
per unit of body weight, it remains constant per kilocalories of basal metabolism.
Because it is difficult to remember basal metabolic rates for various ages and sizes during
childhood, several methods have been proposed to relate maintenance needs to body
weight, including the surface area method, the basal calorie method, and the HollidaySegar system. All three systems work when used by knowledgeable individuals, but each
*Department of Pediatrics, Moses Cone Health System, Greensboro, NC.
380 Pediatrics in Review Vol.22 No.11 November 2001
fluid & electrolytes parenteral fluid therapy
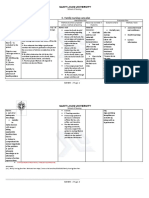
Approach to a Fluid and Electrolyte Problem
tion in urine) each can be considered
as representing 50% of maintenance
needs. This simple principle is a great
Fluid
Electrolytes
(Amount of Water)
(Composition)
aid in the management of children
who have anuric renal failure. MainMaintenance
Determined by a system:
D50.2NS 20 mEq/L
tenance fluid needs decrease by 50%
Holliday-Segar formula, surface
K
area, or basal calorie method
because the only fluids needing to be
Deficit
Determined by acute weight change
Determined by tables
replaced are insensible losses.
or clinical estimate
(generally D50.45NS
Are maintenance fluid and
20 mEq/L K )
electrolytes
all that children at bed
Ongoing Losses
Determined by measuring
Determined by tables or
rest in the hospital need? All chilmeasuring
dren have maintenance needs, but
most hospitalized children have
also has its problems. The surface area method requires a
more than maintenance needs. They may be febrile,
table to determine surface area and ideally knowledge of
needing fluid to dissipate additional heat; they may be in
the patients height and weight, different proponents
a catabolic state, producing additional solute to be exadvocate different estimates of fluid to be administered
creted; or they may be sequestering fluid in a third
per m2, and the system does not address deviations from
space as a result of inflammation or low intravascular
normal activity. The basal calorie method also requires a
colloid pressure. In addition, nutrition includes and cretable, it involves the most calculations, and it is drier
ates additional osmoles that need to be excreted, requirthan the other methods. The Holliday-Segar system, as
ing additional fluid.
generally applied, does not address deviations from norIn the absence of disease, should intake and output be
mal activity, but it is used most frequently because of the
equal, or should urine output always equal half of what
ease with which the formula can be remembered and
is taken in? Intake and the output that is measured
applied (Table 2).
(mainly urine) should not be equal because insensible
The Holliday-Segar formula estimates kilocalories
losses contribute to losses but are not measured. The
that, for practical purposes, can be equated with millihalf-half rule applies when the child has only mainteliters of fluid. (For each 100 kcal expended, approxinance needs and the amount of fluid being provided
mately 50 mL of fluid is required to provide for skin,
matches those needs. Normal kidneys have the ability to
respiratory tract, and basal stool losses, and 55 to 65 mL
modulate the amount of water excreted, but insensible
of fluid is required for the kidneys to excrete an ultrafillosses come off the top. Therefore, as demonstrated in
trate of plasma at 300 mOsm/La specific gravity of
Table 3, if more fluid is provided than is needed for
1.010 without having to concentrate the urine. The
maintenance, urine will be dilute and exceed 50% of the
sum generally is rounded to 100 mL of fluid per 100 kcal
intake; if less fluid is provided than is needed for mainteexpended, permitting kilocalories and milliliters to be used
nance, urine will be concentrated and be less than 50% of
interchangeably.) The two functions of maintenance fluid
intake.
(heat dissipation through insensible losses and solute excreShould maintenance fluids be administered evenly
each hour? The convention of infusing maintenance fluids at a uniform hourly rate is convenient for
the individual making the calculation and for the staff monitoring
the infusion, but it is only a convention. Maintenance fluids certainly
are not ingested at an even rate
when consumed orally, and they do
not need to be provided evenly
when infused parenterally. Flexibility is encouraged when it is not
Figure 1. Maintenance fluid and electrolytes are required because of losses that stem convenient for fluids to be infusing
from basal metabolism.
or when the intravenous access
Table 1.
Pediatrics in Review Vol.22 No.11 November 2001 381
fluid & electrolytes parenteral fluid therapy
Should the sodium concentration of maintenance fluids provided to adolescents and adults differ from that generally provided to
infants and children? The sodium
concentration need not differ.
Both the amount of electrolyte and
the amount of water for maintenance needs are based on metabolic
rate, not on body weight. The ratio
of electrolyte to water is fixed, so
the composition of maintenance
fluids should remain constant:
D50.2NS 20 mEq/L K. Adolescents and adults frequently are
Figure 2. Basal metabolic rate, estimated total expenditure with normal activity, and provided D50.45NS, based on a
caloric expenditure of the average hospitalized patient.
presumed need for sodium of 3
mEq/kg, when the actual need is 3
mEq/100 kcal. The error of calcuneeds to be used for a different purpose, such as the
lating sodium based on weight results in a linearly inadministration of a medication that needs to be infused
creasing amount with increasing weight, when fluid
slowly (eg, vancomycin). Acceptance of the convention
needs actually decrease with advancing weight (Fig 2).
to infuse maintenance fluids at an even rate can make
This results in adults generally being provided more
rehydration calculations unnecessarily difficult.
sodium than needed for maintenance support, as was
recognized nearly 50 years ago. To illustrate the differMaintenance: Electrolytes
ence, a teenager or adult weighing 70 kg would receive
Fluid is lost from the skin largely by evaporation, and that
2,500 mL/d of fluid, based on the Holliday-Segar forlost from the respiratory tract consists of water vapor.
mula. At 3 mEq/100 kcal, the individual would receive
Hence, insensible loss contains virtually no electrolytes.
75 mEq/d of sodium (1.7 g), but at 3 mEq/kg, the
For clinical purposes, all electrolyte loss can be considindividual would receive 210 mEq/d of sodium (nearly
ered to be urinary. This further informs the treatment of
5 g), which is much more than is required to meet
patients who have anuric renal failure. Because their
maintenance needs.
sodium and potassium are recycled, no sodium or
Deficit: Fluid
potassium administration is required. (If the patient is
A deficit is the amount of water (and electrolytes) lost
oliguric rather than totally anuric, the amount of sodium
before treatment is begun. For practical purposes, it is a
lost in the urine can be determined in the laboratory and
one-time estimate, and additional abnormal losses are
replaced as an ongoing loss.)
considered in the category of ongoing losses. Acute weight change is
Table 2.
the most direct basis for determining the amount of deficit fluid; a
loss of body weight greater than 1%
per day almost always must be fluid.
Weight (kg)
kcal/d or mL/d
kcal/h or mL/h
However, weight change can be
misleading. For example, retention
0 to 10 kg
100/kg per day
4/kg per hour
of fluid in a third space may lead
11 to 20 kg
1,000 (50/kg per day)*
40 (2/kg per hour)*
>20 kg
1,500 (20/kg per day)
60 (1/kg per hour)
to intravascular depletion without
a corresponding drop in body
*For each kg 10.
For each kg 20.
weight. Clinical estimates of dehyFrom Holliday MG, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics.
dration are useful when a preillness
1957;19:823 832
weight is not available or the differ-
Holliday-Segar Formula for Determining
Calories (and Fluid Volume) for Average
Hospitalized Patient at Maintenance
382 Pediatrics in Review Vol.22 No.11 November 2001
fluid & electrolytes parenteral fluid therapy
Relationship of Intake and Urine Output in a
10-kg Child Receiving Various Volumes of Fluid*
hemodynamic instability; hypernatremia maintains circulatory sufficiency at the expense of intracellular depletion.
At
More Than
Less Than
The rapidity with which the defMaintenance
Maintenance
Maintenance
icit is replaced depends on the deVolume
1,000 mL
2,000 mL
750 mL
gree of dehydration and on how
Insensible loss
500 mL
500 mL
500 mL
long it has taken for dehydration to
Fluid available for urine
500 mL
1,500 mL
250 mL
develop. (Hippocrates: Those
*Note that urine output is half of intake only if the maintenance amount is provided.
bodies which have been slowly
emaciated should be slowly recruited; and those which have been
ence between the current weight and the preillness
quickly emaciated should be quickly recruited.) Rapid
weight does not seem to reflect the childs clinical conrecruitment not only restores intravascular volume and
dition accurately (Table 4). Dry mucous membranes in
diminishes myocardial work, but it also promotes an
association with normal hemodynamic measurements
improved sense of well-being that often literally reindicate mild dehydration; early hemodynamic signs of
cruits the child to be able to drink and ends the need for
intravascular depletion (eg, tachycardia) define moderate
parenteral fluid. If signs of hypovolemia are present (eg,
dehydration; and signs of more profound hypovolemia
tachycardia, hypotension), a rapid infusion of fluid (bo(eg, hypotension, poor perfusion) are considered evilus) is indicated. The amount generally administered in
dence of severe dehydration. Mild, moderate, and severe
a single bolus is 20 mL/kg for infants and children and
degrees of dehydration in infants correspond roughly to
10 mL/kg for teenagers.
a loss of 5% (50 mL/kg), 10% (100 mL/kg), and 15%
By convention, dehydration often is expressed as per(150 mL/kg) of body weight, respectively. In teenagers
cent of body weight, and bolus replacement is considered
and adults, however, the loss generally is only half as
in milliliters per kilogram of body weight. This mismatch
great. Some authors suggest an estimate of 3% (30 mL/
of units is unfortunate. Recognizing that 20 mL/kg is
kg), 5% (50 mL/kg), and 7% (70 mL/kg) for mild,
equivalent to 2% of body weight permits the clinician to
moderate, and severe dehydration, respectively; others
set expectations for the impact of a bolus of fluid. For
recommend 3% (30 mL/kg), 6% (60 mL/kg), and 9%
example, an infant who is estimated to have lost 10% of
(90 mL/kg). For children between the newborn period
body weight and is tachycardic can be expected to have a
and adolescence, intermediate values should be applied.
lower heart rate after a single 20 mL/kg bolus, but an
Serum sodium concentration affects the clinical signs
infant who is estimated to have lost 15% of body weight
of dehydration. Hyponatremia causes an exaggeration of
Table 3.
Table 4.
Clinical Assessment of Dehydration in Infants and Adolescents
Infant
Adolescent
EWL mL/kg EWL
mL/kg
Severity of
Dehydration Clinical Data
5%
30
Mild
50
3%
10% 100
5% to 6% 50 to 60 Moderate
15% 150
7% to 9% 70 to 90 Severe
Dry mucous
membranes
Oliguria
Problems in Assessment
Oral mucosa may be dry in chronic mouth
breathers
Frequency and amount of urination may be
difficult to assess during diarrhea, especially in
infant girls
Marked oliguria
See oliguria above
Poor skin turgor
Affected by serum [Na ]
Sunken fontanelle Infants only
Tachycardia
Affected by fever, [Na ], underlying disease
Hypotension
Both may be affected by [Na ], underlying disease
Poor perfusion
EWL estimated weight loss
[Na] 150 mEq/L gives falsely low estimate of severity; [Na] 130 mEq/L exaggerates clinical estimate of severity
Pediatrics in Review Vol.22 No.11 November 2001 383
fluid & electrolytes parenteral fluid therapy
will require more than one such
bolus to regain a comparable degree of hemodynamic stability.
Deficit: Electrolytes
Table 5.
Two Methods of Rehydration*
Combined Deficit/
Maintenance
First 8 hours
remaining deficit 13 daily
1 2
Sequential Deficit/
Maintenance
Remaining deficit: 400 mL
Normal saline or Ringer lactate is
after bolus
maintenance 367 mL
12 remaining deficit 23 daily
Next 16 hours
Daily maintenance: 500 mL
used when a bolus of fluid is adminmaintenance 533 mL
istered because the sodium concenTotal
900 mL
900 mL
tration is comparable to serum, so
*A 5-kg infant who has moderate dehydration (10%, 500 mL deficit) following a 20 mL/kg bolus (100
intravascular volume is bolstered
mL). Remaining deficit is 400 mL; maintenance is 500 mL/d.
without fluid shifts. The remainder
of the deficit rarely requires such a
high sodium concentration. In the
tent of normal saline or Ringer lactate, and radiant losses
usual situation, in which the deficit has been incurred
are sodium-free.
because of excessive gastrointestinal losses or a short
period of reduced intake or both, the total sodium loss is
Parenteral Rehydration Without a Calculator
approximately 80 to 100 mEq/L. Particularly when a
of a Moderately Dehydrated Infant
bolus of normal saline or Ringer lactate has been proAn initial bolus of 20 mL/kg is provided to restore
vided, the remaining deficit is approximated by halfnormal hemodynamics; adequacy of the bolus can be
normal saline (D50.45NS).
Only sodium needs are calculated. The amount and
assessed by resolution of hypovolemia-induced tachycarrate of potassium administered is governed by safety,
dia. After the bolus, there are options. A common apand full replacement is not achieved acutely. Once
proach is to provide 50% of the remainder of the deficit in
urine output is assured, and, therefore, it is considered
the next 8 hours along with 8 hours worth of maintesafe to administer potassium, 20 mEq/L is added to
nance fluid; the remainder of the deficit is administered
the replacement solutions. If hypokalemia is a concern,
in the subsequent 16 hours, along with the usual hourly
the concentration of potassium in replacement fluids
maintenance requirement. Such calculations work,
can be increased, but the rate of infusion must be
but they are unnecessarily complex and may be so dauntconsidered as well. The limiting factor is the amount of
ing as to discourage any calculations, particularly in the
potassium infused per unit time, which should not
middle of the night.
exceed 1 mEq/kg per hour without appropriate monAn easier alternative is to recognize that the bolus of
itoring.
20 mL/kg represents 2% of body weight. If the initial
deficit was estimated to be 10%, the remainder after the
bolus is 8%. This can be replaced conveniently over
Ongoing Losses: Fluid
8 hours at an hourly rate of 10 mL/kg (1% body weight
Ongoing losses represent the abnormal losses that occur
per hour), a number that is easy to calculate mentally.
after the one-time determination of a deficit. Examples
The days worth of maintenance fluid then is provided in
include continued diarrhea or vomiting, aspirates from a
16 hours. Administering 24 hours worth in 16 hours renasogastric tube attached to suction, or the polyuria of an
quires a rate of 1.5 times the usual hourly maintenance rate
osmotic diuresis. These losses can be measured directly.
(24 16 1.5). By this method, calculations are simpliOther losses, such as abnormal internal collections with
fied, and the amount of fluid administered hourly is close to
an ileus, peritonitis, or edema and external radiant losses,
the same as the more complex way, with slightly more at an
are more difficult to estimate and require experience and
early point (Table 5). As noted previously, rapid recruitcareful monitoring of the patient.
ment is desirable and often obviates the need to provide
the parenteral infusion longer than overnight.
Ongoing Losses: Electrolytes
The bolus is normal saline or Ringer lactate; the
Tables are available to estimate the composition of onremainder of the deficit is provided as D50.45NS
going losses according to the source of the loss. As a rule
20 mEq/L K, and the maintenance fluid is D50.2NS
20 mEq/L K. In summary, the rehydration plan is for
of thumb, gastrointestinal losses can be replaced with
20 mL/kg of normal saline for hour 1, 10 mL/kg of
half-normal saline, transudates reflect the composition of
D50.45NS 20 mEq/L K for hours 2 to 9, 1.5 times
the intravascular space and have the higher sodium con384 Pediatrics in Review Vol.22 No.11 November 2001
fluid & electrolytes parenteral fluid therapy
Table 6.
Signs and Tests to Monitor State of Hydration
Sign or Test
Problem
1. Physical signs of dehydration on
physical examination
2. Body weight
3. Urine volume
May be deceiving if [Na] is abnormal; may be influenced by fever (especially
pulse)
Can be fooled by third spacing
Output also low in syndrome of inappropriate secretion of antidiuretic
hormone (SIADH), renal failure
Concentrating ability of infant kidney limited; SG also high in SIADH, renal
failure; SG low in pyelonephritis
Must estimate maintenance; cannot measure third space loss
4. Urine specific gravity (SG)
5. Input and output, with direct measure
of all losses
6. Urea nitrogen (BUN)
7. Hematocrit
8. Concurrent serum and urine
osmolalities
9. Serum electrolyte concentrations
Glomerular filtration rate severely reduced before BUN rises; elevated by blood
in gastrointestinal tract; infant measure normally lower than adult
measure; may mean renal disease
Useful serially but not as single value and not if patient is bleeding
Good for detecting SIADH problem
By themselves, reveal little about state of hydration
From Roberts K. Fluid and electrolyte disorders in infants and children. In: Beers M, Berkow R, eds. The Merck Manual of Diagnosis and Therapy. 17th ed.
Whitehouse Station, NJ: Merch & Co; 1999
the usual maintenance amount of D50.2NS
20 mEq/L K for the next 16 hours, and usual maintenance thereafter.
Hypertonic Dehydration
Hypertonic dehydration is an exception to the foregoing
approach. In hyperosmolar states, fluid is drawn into the
intravascular space from the intracellular space, bolstering the circulation. The rapid administration of fluid, as
recommended for isotonic states, can create fluid shifts
that result in cerebral edema and intracranial bleeding.
Finberg described a rehydration protocol that permits
fluid and electrolytes to be administered safely and has
been widely accepted. A bolus may or may not be needed
because the contribution of the intracellular space may
have maintained an effective circulating volume. The
calculated deficit fluid and electrolyte needs are added to
2 days (48 h) worth of maintenance fluid and electrolyte
requirements; the sum is divided by 48 and administered
at a constant hourly rate for 48 hours.
Monitoring the Effectiveness of Parenteral
Fluid and Electrolyte Therapy
The best monitoring tests are the simple ones that all
too frequently are overlooked, such as the resolution of
signs of dehydration apparent on physical examination:
tachycardia and dry mucous membranes (Table 6). Serial
weights provide valuable information, as long as there is
no third-spacing. Measurement of urine volume and
specific gravity are also helpful. In situations in which the
blood urea nitrogen concentration is increased, it is
comforting to see a return to normal, but generally blood
tests have little to offer compared with the bedside
tests noted previously. In particular, electrolyte concentrations do not reflect the state of hydration.
Summary
When planning to rehydrate a dehydrated child parenterally, it is useful to consider the fluid and electrolyte needs
separately for maintenance, deficit, and ongoing losses.
For maintenance, both fluids and electrolytes are based
on metabolic rate. The composition, therefore, is fixed
(D50.2NS 20 mEq/L K). Systems, such as the
Holliday-Segar formula, relate fluid needs to body
weight.
In assessing the extent of dehydration clinically, the
rule of 5 to 10 to 15 (mild dehydration5%, moderate
dehydration10%, severe dehydration15%) applies
only to infants. For adolescents and adults, the rule
estimates are 3% to 5% to 7% or 3% to 6% to 9%.
Intermediate values should be used for school-age children.
A bolus of fluid that is similar to extracellular fluid
(ECF) is administered if signs of hypovolemia are
present. The amount generally provided to infants and
small children is 20 mL/kg (2% of body weight); the
volume for adolescents is 10 mL/kg (1% of body
weight). If an infants degree of dehydration is estimated
to be 15%, a single 20-mL/kg bolus will improve circulation but not normalize the hemodynamics. For timely
Pediatrics in Review Vol.22 No.11 November 2001 385
fluid & electrolytes parenteral fluid therapy
restoration of cardiovascular sufficiency, one or more
additional boluses of 20 mL/kg will be required.
Isotonic dehydration estimated to be 10% of body
weight can be corrected by 20 mL/kg per hour of
ECF-like fluid followed by 8 hours of D50.45NS
20 mEq/L K at 10 mL/kg per hour. Maintenance
fluids, D50.2NS 20 mEq/L K, subsequently are
provided, initially at 1.5 times the usual rate for 16 hours,
followed by the usual maintenance rate (although, by
then, parenteral therapy may not be needed).
Ongoing losses, if significant, should be measured and
replaced. When it is not possible to measure the losses,
extra diligence must be applied in patient monitoring.
Monitoring should focus on readily available mea-
386 Pediatrics in Review Vol.22 No.11 November 2001
sures because they are the most helpful: physical examination (to see if the signs of dehydration have improved),
weight, urine volume, and specific gravity.
Suggested Reading
Finberg L. Hypernatremic (hypertonic) dehydration in infants.
N Engl J Med. 1973;289:196 198
Holliday MA, Segar WE. The maintenance need for water in
parenteral fluid therapy. Pediatrics. 1957;19:823 832
Roberts K. Fluid and electrolyte disorders in infants and children.
In: Beers M, Berkow R, eds. The Merck Manual of Diagnosis and
Therapy. 17th ed. Whitehouse Station, NJ: Merck & Co; 1999
Welt LG. Clinical Disorders of Hydration and Acid-base Equilibrium. Boston, Mass: Little, Brown; 1955
fluid & electrolytes parenteral fluid therapy
PIR Quiz
Quiz also available online at www.pedsinreview.org.
9. A 6-year-old girl is admitted for elective removal of a mesenteric cyst. Physical examination reveals a
well-hydrated child whose weight is 23 kg and height is 115 cm. She is afebrile and appears healthy.
Which of the following is the most appropriate parenteral maintenance fluid and electrolytes regimen for
her?
A.
B.
C.
D.
E.
5%
5%
5%
5%
5%
Dextrose
Dextrose
Dextrose
Dextrose
Dextrose
with
with
with
with
with
0.20%
0.20%
0.45%
0.45%
0.90%
saline
saline
saline
saline
saline
20
40
20
40
40
mEq/L
mEq/L
mEq/L
mEq/L
mEq/L
KCl
KCl
KCl
KCl
KCl
at
at
at
at
at
65
95
65
95
65
mL/h.
mL/h.
mL/h.
mL/h.
mL/h.
10. A 2-year-old child presents with a 24-hour history of 10 to 12 large, watery stools and vomiting.
Physical examination reveals sunken eyes, weight of 12.5 kg, temperature of 36.8C (98.2F), heart rate of
144 beats/min, respirations of 26 breaths/min, and blood pressure of 78/40 mm Hg. His extremities are
cool, and the capillary refill time is 3 seconds. Of the following, the most appropriate initial intravenous
bolus to be administered over the next hour is:
A.
B.
C.
D.
E.
125
250
250
125
250
mL
mL
mL
mL
mL
Ringer lactate.
0.9% saline.
5% Dextrose.
5% Dextrose with Ringer lactate.
5% Dextrose with 045% saline.
11. A 6-month-old girl presents with vomiting and loose stools of 3 days duration. Physical examination
reveals an axillary temperature of 37.2C (99F), respiratory rate of 32 breaths/min, heart rate of
126 beats/min, and blood pressure of 98/68 mm Hg. The anterior fontanelle and eyes are sunken, the lips
and oral mucous membranes are dry, and the skin appears doughy. Results of laboratory studies include:
serum sodium, 168 mEq/L (168 mmol/L); potassium, 5.2 mEq/L (5.2 mmol/L); chloride, 136 mEq/mL
(136 mmol/L); and bicarbonate, 10 mEq/L (10 mmol/L). A true statement about this girls condition is
that:
A.
B.
C.
D.
E.
A 20 mL/kg bolus of 5% dextrose should be administered over 1 h.
Extracellular fluid is depleted more than intracellular fluid.
Rehydration should occur over 48 h at a constant rate.
Total body potassium is increased.
Total body sodium is increased.
Pediatrics in Review Vol.22 No.11 November 2001 387
You might also like
- How Much Water To Drink When Fasting - Based On The Teachings Of Dr. Eric Berg: Ensuring Proper Water Consumption While FastingFrom EverandHow Much Water To Drink When Fasting - Based On The Teachings Of Dr. Eric Berg: Ensuring Proper Water Consumption While FastingNo ratings yet
- Fluid and Electrolytes JoyDocument10 pagesFluid and Electrolytes JoyM Rizal IsburhanNo ratings yet
- Why Your Body Water Balance Is a Key to Health and Great Shape?From EverandWhy Your Body Water Balance Is a Key to Health and Great Shape?No ratings yet
- Fluid and ElectrolytesDocument10 pagesFluid and ElectrolytesYunisa IrenNo ratings yet
- Fluid and ElectrolytesDocument8 pagesFluid and ElectrolytesCaz SamNo ratings yet
- Supercharging Autophagy - Based On The Teachings Of Dr. Eric Berg: Unleashing Its Full PotentialFrom EverandSupercharging Autophagy - Based On The Teachings Of Dr. Eric Berg: Unleashing Its Full PotentialNo ratings yet
- Maintenance Intravenous Fluid Therapy in Children - UpToDateDocument19 pagesMaintenance Intravenous Fluid Therapy in Children - UpToDaterolland_arrizaNo ratings yet
- The #1 Danger Of Prolonged Fasting You Have To Know About - Based On The Teachings Of Dr. Eric Berg: The Most Important Risk To UnderstandFrom EverandThe #1 Danger Of Prolonged Fasting You Have To Know About - Based On The Teachings Of Dr. Eric Berg: The Most Important Risk To UnderstandNo ratings yet
- Fluids and Electrolytes For PediatricsDocument31 pagesFluids and Electrolytes For PediatricsJeno Luis J. ACUBNo ratings yet
- Metabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentFrom EverandMetabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentCarole IchaiNo ratings yet
- Maintenance Fluid Therapy in ChildrenDocument4 pagesMaintenance Fluid Therapy in ChildrenNicole_0No ratings yet
- Author: Section Editor: Deputy EditorDocument11 pagesAuthor: Section Editor: Deputy EditorVictor Lima AraujoNo ratings yet
- F E T C: Luid AND Lectrolyte Herapy IN HildrenDocument12 pagesF E T C: Luid AND Lectrolyte Herapy IN HildrenHartantoRezaGazaliNo ratings yet
- Fluid TherapyDocument27 pagesFluid TherapyRashed ShatnawiNo ratings yet
- The Water Prescription: For Health, Vitality, and RejuvenationFrom EverandThe Water Prescription: For Health, Vitality, and RejuvenationRating: 5 out of 5 stars5/5 (2)
- Dehydration: Body-Fluid CompositionDocument5 pagesDehydration: Body-Fluid CompositionThegreat Mokz Mokz ThegreatNo ratings yet
- Hypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 4.fluid and ElectrolytesDocument23 pages4.fluid and ElectrolytesManju KumariNo ratings yet
- Fluid Calculation For Iv InfusionDocument8 pagesFluid Calculation For Iv InfusionAsma SaleemNo ratings yet
- Paed IVFDocument10 pagesPaed IVFnaga tanoojNo ratings yet
- Metabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMetabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Fluids and Electrolytes - PaediatricsDocument52 pagesFluids and Electrolytes - PaediatricsZweNo ratings yet
- Fluid and ElectrolytesDocument137 pagesFluid and ElectrolytesNano Baddour100% (1)
- Fluid and Electrolyte Therapy in NewbornsDocument10 pagesFluid and Electrolyte Therapy in NewbornsJaner BanosNo ratings yet
- Tony - Electrolytes Lect NCMDocument84 pagesTony - Electrolytes Lect NCMJoseph Nawen SindiongNo ratings yet
- Final Report of Importance of WaterDocument5 pagesFinal Report of Importance of WaterTanistha KhandelwalNo ratings yet
- Perioperative Intravenous Fluid Therapy For Adults: Rob Mac Sweeney, Rachel Alexandra Mckendry, Amit BediDocument8 pagesPerioperative Intravenous Fluid Therapy For Adults: Rob Mac Sweeney, Rachel Alexandra Mckendry, Amit BediAnnisa Chaerani BurhanuddinNo ratings yet
- F E T C: Luid and Lectrolyte Herapy in HildrenDocument12 pagesF E T C: Luid and Lectrolyte Herapy in HildrenTania Febria AzizahNo ratings yet
- Fluid and Electrolyte BalanceDocument5 pagesFluid and Electrolyte BalanceBumi Zulheri HermanNo ratings yet
- Test Bank For Lutzs Nutrition and Diet Therapy 7th by MazurDocument15 pagesTest Bank For Lutzs Nutrition and Diet Therapy 7th by Mazurtracywilsonjftmrqknys100% (28)
- Fluid Management For The Pediatric Surgical Patient POWERPOINTDocument34 pagesFluid Management For The Pediatric Surgical Patient POWERPOINTDipta Anggara100% (2)
- Perioperative Fluid ManagementDocument123 pagesPerioperative Fluid ManagementAnonymous 86gki5No ratings yet
- Fluid and Electrolytes.3Document43 pagesFluid and Electrolytes.3Medic PediatruNo ratings yet
- Test Bank Lutzs Nutrition and Diet Therapy 7th Edition Erin e MazurDocument16 pagesTest Bank Lutzs Nutrition and Diet Therapy 7th Edition Erin e Mazurjeremiahhartfozxmbqayn100% (11)
- Hipotonicos VS IsotonicosDocument13 pagesHipotonicos VS IsotonicosYeison Duban Gomez CastilloNo ratings yet
- Fluid and Electrolyte Therapy in Newborns PDFDocument7 pagesFluid and Electrolyte Therapy in Newborns PDFdocbinNo ratings yet
- What Is Plasma Osmolality?:, 23 Mei 2007 Fluid and Electrolyte TherapyDocument17 pagesWhat Is Plasma Osmolality?:, 23 Mei 2007 Fluid and Electrolyte TherapyRani ChesarNo ratings yet
- ACFrOgCEv6W8PZIOChX2ac TB PsVqkwB2LLEUA - nz2imEUDlJJqTMiew0fEYsQLz7I hoxDAHunIFV - PnnXqTDHrgpAsGRo2r9aPQF4UMBSoquxza - oenQBKFcGXpRcMCDKlMwgjULOtJeC9idDocument14 pagesACFrOgCEv6W8PZIOChX2ac TB PsVqkwB2LLEUA - nz2imEUDlJJqTMiew0fEYsQLz7I hoxDAHunIFV - PnnXqTDHrgpAsGRo2r9aPQF4UMBSoquxza - oenQBKFcGXpRcMCDKlMwgjULOtJeC9idCenitserNo ratings yet
- Nursing Fluids and ElectrolytesDocument14 pagesNursing Fluids and Electrolytesaga1028100% (18)
- Fluids SummaryDocument3 pagesFluids Summarymicheal1960No ratings yet
- 10 Fluids and Electrolytes: Cleveland Clinic Intensive Review of Pediatrics, The, 2nd EditionDocument12 pages10 Fluids and Electrolytes: Cleveland Clinic Intensive Review of Pediatrics, The, 2nd EditionaeyousefNo ratings yet
- IV Fluids (What Nurses Need To Know)Document9 pagesIV Fluids (What Nurses Need To Know)ChelseaLovell100% (2)
- Liquidos y Electrolitos 2Document4 pagesLiquidos y Electrolitos 2Jorge MBNo ratings yet
- Dehydration and Rehydration Chapter From The Wilderness Medicine TextbookDocument17 pagesDehydration and Rehydration Chapter From The Wilderness Medicine TextbookcmonBULLSHITNo ratings yet
- Fluid and ElyctrolyteDocument49 pagesFluid and Elyctrolyteuuuhbnb lplhgh100% (2)
- Fluid Electrolyte and AcidBase BalanceDocument33 pagesFluid Electrolyte and AcidBase Balancemoncalshareen3No ratings yet
- Filston 1992Document17 pagesFilston 1992Nilamsari KurniasihNo ratings yet
- Lect 02Document5 pagesLect 02Iptysam Al-AlawiNo ratings yet
- Fluid Electrolytes Bablance 150308Document16 pagesFluid Electrolytes Bablance 150308Shruthi RathishNo ratings yet
- Fluid Replacement GOODocument13 pagesFluid Replacement GOOMansoor TariqNo ratings yet
- Fluid Lec.9Document14 pagesFluid Lec.9ahmed.kald896No ratings yet
- WaterDocument11 pagesWaterAhmed JabbarNo ratings yet
- Perioperative Fluid Management in ChildrenDocument31 pagesPerioperative Fluid Management in ChildrenRashmi SahaNo ratings yet
- Fluid and ElyctrolyteDocument49 pagesFluid and Elyctrolyteuuuhbnb lplhghNo ratings yet
- Kyphosis & LordosisDocument14 pagesKyphosis & LordosisTrixie Marie Sabile Abdulla100% (3)
- Ethical Care 2 Nurs 217Document9 pagesEthical Care 2 Nurs 217api-283946728No ratings yet
- C. Family Nursing Care Plan: Saint Louis UniversityDocument2 pagesC. Family Nursing Care Plan: Saint Louis UniversityLEONELLGABRIEL RAGUINDIN0% (1)
- Breech PresentationDocument27 pagesBreech PresentationNurkamilawati AristaNo ratings yet
- Health Problems MyselfDocument54 pagesHealth Problems MyselfKrishnaveni Murugesh100% (2)
- Tongue Diagnosis in Chinese Medicine (TCM)Document8 pagesTongue Diagnosis in Chinese Medicine (TCM)nepretip50% (2)
- AmysaDocument14 pagesAmysaawanisfauzi90No ratings yet
- Genetic Dis & AnaesthDocument19 pagesGenetic Dis & AnaesthaksinuNo ratings yet
- Asuhan Keperawatan Pada Pasien Dengan Chronic Kidney DiseasesDocument24 pagesAsuhan Keperawatan Pada Pasien Dengan Chronic Kidney DiseasestidaktahudiriNo ratings yet
- Healthcare Statistic in MalaysiaDocument13 pagesHealthcare Statistic in MalaysiaMOZAIDNo ratings yet
- Admission Nursing AssessmentDocument20 pagesAdmission Nursing Assessmentmonir61No ratings yet
- tmpB433 TMPDocument9 pagestmpB433 TMPFrontiersNo ratings yet
- VM in BpocDocument19 pagesVM in BpocAndreea Livia DumitrescuNo ratings yet
- MedStart UMAT Sample and Practice QuestionsDocument55 pagesMedStart UMAT Sample and Practice QuestionsLyn JiangNo ratings yet
- SURESH Testing ProfileDocument3 pagesSURESH Testing Profilefreecharge momNo ratings yet
- The Basal Ganglia and Movement Disorders 2015 RevisedDocument19 pagesThe Basal Ganglia and Movement Disorders 2015 RevisedJoan ChoiNo ratings yet
- Uji Resistensi Antibiotik Terhadap Kultur Bakteri Staphylococcus Aureus PADA RUANG Intensive Care Unit (ICU) RUMAH Sakit Y Kota JambiDocument7 pagesUji Resistensi Antibiotik Terhadap Kultur Bakteri Staphylococcus Aureus PADA RUANG Intensive Care Unit (ICU) RUMAH Sakit Y Kota JambiObrilian Waisman MNo ratings yet
- Observational DescriptiveDocument21 pagesObservational DescriptiveAgus wawaNo ratings yet
- Efektifitas Pelatihan High Alert Medication Terhadap Pengetahuan Dan Sikap Petugas Di RS KIA PKU Muhammadiyah KotagedeDocument4 pagesEfektifitas Pelatihan High Alert Medication Terhadap Pengetahuan Dan Sikap Petugas Di RS KIA PKU Muhammadiyah KotagedeNindy C AbriantyNo ratings yet
- Case StudyDocument2 pagesCase StudyElmer Alberto Lopez PonceNo ratings yet
- KINESIOTHERAPHYDocument40 pagesKINESIOTHERAPHYJeyarajasekar TtrNo ratings yet
- EPC Referral FormDocument1 pageEPC Referral FormCarlos GuerrettaNo ratings yet
- Lithium Use in Pregnancy and The Risk of Cardiac MalformationsDocument10 pagesLithium Use in Pregnancy and The Risk of Cardiac MalformationsRoberto López MataNo ratings yet
- Special - NCLEX - Exam - Jakarta - Students - PDF Filename UTF-8''Special NCLEX Exam - Jakarta StudentsDocument23 pagesSpecial - NCLEX - Exam - Jakarta - Students - PDF Filename UTF-8''Special NCLEX Exam - Jakarta Studentsrizqi100% (1)
- Bag TechniqueDocument23 pagesBag TechniqueMamta Rajput83% (12)
- Insomnia: Management of Underlying ProblemsDocument6 pagesInsomnia: Management of Underlying Problems7OrangesNo ratings yet
- SPC 138523Document4 pagesSPC 138523Pankaj ArgalNo ratings yet
- Texas Has The Highest Maternal Mortality Rate in The Developed WorldDocument5 pagesTexas Has The Highest Maternal Mortality Rate in The Developed WorldDixanetNo ratings yet
- App Ashcraft's Pediatric Surgery 5th EditionDocument8 pagesApp Ashcraft's Pediatric Surgery 5th EditionAndri Feisal NasutionNo ratings yet
- Lomba HHD IgdDocument34 pagesLomba HHD IgdIndra nugrahaNo ratings yet
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouFrom EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouRating: 3.5 out of 5 stars3.5/5 (5)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Power of 10: The Once-A-Week Slow Motion Fitness RevolutionFrom EverandPower of 10: The Once-A-Week Slow Motion Fitness RevolutionRating: 3.5 out of 5 stars3.5/5 (11)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsFrom EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsRating: 5 out of 5 stars5/5 (96)
- Aging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayFrom EverandAging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayNo ratings yet
- Whole Body Barefoot: Transitioning Well to Minimal FootwearFrom EverandWhole Body Barefoot: Transitioning Well to Minimal FootwearRating: 4 out of 5 stars4/5 (16)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!From EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Rating: 4.5 out of 5 stars4.5/5 (22)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (66)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (111)
- Mind Your Body: 4 Weeks to a Leaner, Healthier LifeFrom EverandMind Your Body: 4 Weeks to a Leaner, Healthier LifeRating: 4.5 out of 5 stars4.5/5 (5)
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- Relentless: From Good to Great to UnstoppableFrom EverandRelentless: From Good to Great to UnstoppableRating: 5 out of 5 stars5/5 (784)
- Buteyko Breathing Course Manual: For use with the Advanced Buteyko CourseFrom EverandButeyko Breathing Course Manual: For use with the Advanced Buteyko CourseRating: 5 out of 5 stars5/5 (1)
- Easy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportFrom EverandEasy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportRating: 4.5 out of 5 stars4.5/5 (17)
- 80/20 Running: Run Stronger and Race Faster by Training SlowerFrom Everand80/20 Running: Run Stronger and Race Faster by Training SlowerRating: 4.5 out of 5 stars4.5/5 (97)
- Music For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicFrom EverandMusic For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicRating: 5 out of 5 stars5/5 (1)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesFrom EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesNo ratings yet
- The Yoga Sutras of Patanjali: The Final Guide for the Study and Practice of Patanjali's Yoga SutrasFrom EverandThe Yoga Sutras of Patanjali: The Final Guide for the Study and Practice of Patanjali's Yoga SutrasNo ratings yet
- Weight Lifting Is a Waste of Time: So Is Cardio, and There’s a Better Way to Have the Body You WantFrom EverandWeight Lifting Is a Waste of Time: So Is Cardio, and There’s a Better Way to Have the Body You WantRating: 4.5 out of 5 stars4.5/5 (38)
- If You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsFrom EverandIf You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsRating: 4.5 out of 5 stars4.5/5 (7)
- Endure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceFrom EverandEndure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceRating: 4.5 out of 5 stars4.5/5 (237)
- Structural Integration and Energy Medicine: A Handbook of Advanced BodyworkFrom EverandStructural Integration and Energy Medicine: A Handbook of Advanced BodyworkRating: 4 out of 5 stars4/5 (1)
- Not a Diet Book: Take Control. Gain Confidence. Change Your Life.From EverandNot a Diet Book: Take Control. Gain Confidence. Change Your Life.Rating: 4.5 out of 5 stars4.5/5 (124)
- Fascial Training: With Easy Exercises To More Mobility And Less Pain (10 Minutes Fascia Workout For Home)From EverandFascial Training: With Easy Exercises To More Mobility And Less Pain (10 Minutes Fascia Workout For Home)Rating: 5 out of 5 stars5/5 (3)
- The Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandThe Yamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (19)