Professional Documents
Culture Documents
2004 JAMA Subclinical Case
Uploaded by
faisalsyahrilCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2004 JAMA Subclinical Case
Uploaded by
faisalsyahrilCopyright:
Available Formats
SCIENTIFIC REVIEW CLINICIANS CORNER
AND CLINICAL APPLICATIONS
Subclinical Thyroid Disease
Clinical Applications
Nananda F. Col, MD, MPP, MPH
Subclinical hypothyroidism and hyperthyroidism are diagnoses based on labo-
Martin I. Surks, MD ratory evaluation with few if any clinical signs or symptoms. Subclinical hy-
Gilbert H. Daniels, MD pothyroidism is defined as an elevation in serum thyroid-stimulating hor-
mone (TSH) above the upper limit of the reference range (0.45-4.5 mIU/L)
S
UBCLINICAL HYPOTHYROIDISM
and hyperthyroidism repre- with normal serum FT4 concentration; subclinical hyperthyroidism is de-
sent the earliest stages of thy- fined as a decrease in serum TSH below the reference range with normal se-
roid dysfunction. Subclinical rum FT4 and T3 concentrations. Though these conditions represent the ear-
hypothyroidism is defined as an eleva- liest stages of thyroid dysfunction, the benefits of detecting and treating
tion in serum thyroid-stimulating hor- subclinical thyroid disease are not well established. Most persons found to
mone (TSH) above the upper limit of have subclinical thyroid disease will have TSH values between 0.1 and 0.45
the reference range (0.45-4.5 mIU/L)
mIU/L or between 4.5 and 10 mIU/L, for which the benefits of treatment
with a normal serum free T4 (FT4) con-
centration; subclinical hyperthyroid- are not clearly established; treatment may be beneficial in individuals with
ism is defined as a decrease in serum serum TSH lower than 0.1 mIU/L or higher than 10 mIU/L. This article il-
TSH concentration below the refer- lustrates approaches to managing patients with subclinical hypothyroidism
ence range, with normal serum FT4 and and hyperthyroidism through 5 case scenarios that apply the principles of
T3 concentrations. Most patients have evidence-based medicine. Because of the substantial uncertainty concern-
few if any signs or symptoms of thy- ing the consequences of untreated subclinical hypothyroidism and hyper-
roid dysfunction; therefore, it is a di- thyroidism, as well as the benefit of initiating treatment, patient prefer-
agnosis based on laboratory evalua-
ences are important in deciding on management of subclinical disease.
tion. Because the risk for subclinical
JAMA. 2004;291:239-243 www.jama.com
thyroid dysfunction, particularly sub-
clinical hypothyroidism, increases with
age,1 the number of cases should in- than 10 mIU/L are more likely to ben- well as the expense and inconvenience
crease as the US population ages. efit from treatment, though some un- of treatment vs monitoring. FIGURES 1
Management of patients with thy- certainty remains. Subclinical thyroid and 2 depict simplified clinical algo-
roid dysfunction remains controversial dysfunction predicts future progres- rithms for approaching subclinical hy-
because the body of scientific evidence sion to overt disease; however, TSH lev- pothyroidism and hyperthyroidism.
available to guide clinical decisions is els in some individuals with subclini-
limited. Fundamental questions such as cal hypothyroidism or hyperthyroidism Clinical Context
whom to screen and when to initiate return to the reference range. Initiating Patient 1. A 28-year-old aerobics in-
treatment remain largely unanswered. treatment for subclinical hypothyroid- structor in excellent health had labo-
Based on the available data, withhold- ism does not alter the natural history of
ing treatment for individuals with se- the disease but may prevent symptoms Author Affiliations: Division of Womens Health and
Department of Medicine, Harvard Medical School,
rum TSH values that are slightly above and signs of overt disease. Brigham and Womens Hospital, Boston, Mass (Dr Col);
or below the reference range (4.5-10 or In disorders for which the definition Department of Medicine and Pathology, Montefiore
of the condition is imprecise and the ben- Medical Center and the Albert Einstein College of Medi-
0.1-0.45 mIU/L) likely poses no harm, cine, Bronx, NY (Dr Surks); and Thyroid Unit and De-
and initiating treatment likely poses no efits and risks of treatment are not clearly partment of Medicine, Massachusetts General Hos-
clear gains. Individuals with serum TSH established, patient preferences play a pital, Harvard Medical School, Boston (Dr Daniels).
Corresponding Author: Martin I. Surks, MD, Mon-
concentrations lower than 0.1 or higher critical role in treatment decisions. To tefiore Medical Center, 111 E 210th St, Bronx, NY
make informed decisions, patients 10467 (e-mail: msurks@westnet.com).
Reprints: Society Services, The Endocrine Society, 8401
should understand the benefits and risks Connecticut Ave, Suite 900, Chevy Chase, MD 20815
See also p 228.
of initiating vs withholding treatment, as (e-mail: societyservices@endo-society.org).
2004 American Medical Association. All rights reserved. (Reprinted) JAMA, January 14, 2004Vol 291, No. 2 239
Downloaded from www.jama.com on December 13, 2006
SUBCLINICAL THYROID DISEASE
ratory tests performed by her primary amined carefully. The patient should be body positivity predicts an increased
care physician as part of a routine of- asked about previous radioactive io- risk of progressing to overt hypothy-
fice visit. All results were normal, in- dine treatment, thyroid surgery, levo- roidism (2.6% per year if negative, 4.3%
cluding complete blood cell count and thyroxine treatment, a family history of if positive),2 it does not affect the ef-
lipid profile, except for the serum TSH thyroid disease, and her lipid profile fectiveness of treatment. Nonetheless,
concentration of 7.9 mIU/L. should be determined. the increased rate of progression may
Before making a treatment deci- Three months later, the patients se- tip the balance toward treatment in
sion, guidelines recommend repeat- rum TSH was 6.8 mIU/L and FT 4 , some cases. The presence of anti-TPO
ing the serum TSH and measuring FT4 1.4 ng/dL (18 pmol/L); antithyroid per- antibodies does predict an increased
within 2 to 12 weeks, depending on the oxidase (TPO) antibodies were ab- risk of miscarriage as well as postpar-
clinical setting, to exclude transient sent. She was referred to an endocri- tum thyroiditis.3
forms of hypothyroidism. Transient hy- nologist for evaluation and treatment Having confirmed the diagnosis of
pothyroidism is most commonly caused of subclinical hypothyroidism. The pa- subclinical hypothyroidism, deciding
by destructive thyroiditis (including tient reported no symptoms of hypo- whether to initiate levothyroxine would
painful subacute thyroiditis, silent sub- thyroidism. She was taking no medi- depend on her serum TSH concentra-
acute thyroiditis, or postpartum thy- cations other than oral contraceptives, tion, the presence of any signs or symp-
roiditis) or recovery from severe non- her menses occurred regularly, and she toms suggestive of hypothyroidism, her
thyroidal illness. The clinician should was not intending to become preg- risk of progression to overt disease, and
assess the patient for symptoms and nant. Her family history included one her preferences. There is no evidence
signs of hypothyroidism, including fa- maternal aunt with hypothyroidism and that levothyroxine treatment in healthy,
tigue, lethargy, slow cerebration, di- a maternal grandmother with diabetes asymptomatic patients with TSH be-
minished sweating, dry skin, cold in- mellitus. Her examination findings were tween 4.5 and 10 mIU/L results in sig-
tolerance, dry hair, weight gain, unremarkable and her thyroid gland nificant improvements in either qual-
constipation, hoarseness, paresthe- was palpable but not enlarged. ity of life or clinical outcomes. Initiating
sias, menstrual alterations, and muscle Routine measurement of anti-TPO treatment would prevent symptoms and
pain. The thyroid gland should be ex- levels is controversial. Although anti- signs of hypothyroidism should this pa-
tient eventually progress to overt hy-
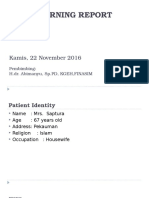
Figure 1. Suggested Approach to Diagnosis and Management of Subclinical Hypothyroidism pothyroidism. The risk of progression
to overt hypothyroidism is 2% to 5% per
Serum TSH >4.5 mIU/L year. However, serum TSH decreases to
the reference range in a similar per-
Repeat Serum TSH Measurement With FT4 centage during the 2 to 4 years after el-
Measurement 2 to 12 Weeks Later
evated serum TSH is discovered.2 No
risks of delaying detection of overt hy-
No Serum TSH Level Within Yes Monitor Every
Reference Range 6 to 12 mo for pothyroidism have been demon-
(0.45 to 4.5 mIU/L)? Several Years
strated as long as individuals are care-
fully monitored.
Serum TSH Level Serum TSH Level
In the absence of symptoms, the only
4.5 to 10 mIU/L >10 mIU/L other benefit of levothyroxine treat-
ment in this patient would be possible
Yes FT4 No Yes FT4 No improvement in cardiac function. Sev-
Level Decreased Level Decreased
(<0.8 ng/dL)? (<0.8 ng/dL)? eral small, unblinded studies suggest that
subclinical hypothyroidism might be as-
Pregnant or Pregnant or
Treat With Yes
Contemplating
No Treat With Yes
Contemplating
No sociated with subtle declines in cardiac
Levothyroxine Levothyroxine
Pregnancy? Pregnancy? contractility.4 However, evidence con-
cerning the impact of subclinical hypo-
Consider Levothyroxine
Treatment With
Yes Signs or Symptoms
Consistent With
No thyroidism, treated or untreated, on clini-
Consider
Periodic Monitoring Hypothyroidism? Levothyroxine cal cardiac end points is limited. Because
Treatment in
Monitor Serum TSH Appropriate
of the lack of clear clinical benefits, rou-
Every 6 to 12 mo Clinical Settings tine treatment with levothyroxine is not
recommended in such patients. There is
The normal range of free T4 (FT4) is 0.8 to 2.0 ng/dL (10-25 pmol/L); the normal range of thyroid-stimulating
hormone (TSH) is 0.45-4.5 mIU/L.
no compelling evidence that low-
*In rare instances a slightly elevated serum TSH represents hypothalamic/pituitary disease. In these situations density lipoprotein (LDL) cholesterol is
the FT4 is extremely low when the TSH is only slightly elevated, in contrast to primary hypothyroidism in which higher in individuals with serum TSH in
the TSH increases exponentially with small decreases in serum FT4 concentration.
the range of 4.5 to 10 mIU/L.
240 JAMA, January 14, 2004Vol 291, No. 2 (Reprinted) 2004 American Medical Association. All rights reserved.
Downloaded from www.jama.com on December 13, 2006
SUBCLINICAL THYROID DISEASE
After discussing the risks and ben- toms than euthyroid patients,1 other tension, type 2 diabetes mellitus, and
efits of treatment, this patient elected studies found no differences between hypercholesterolemia who presents for
not to be treated but to be followed with patients and euthyroid controls.9-11 medical clearance before embarking on
annual determination of serum TSH and There are no data clearly demonstrat- an exercise program is found to have a
to be alert for signs and symptoms of ing that treatment will improve symp- serum TSH of 12 mIU/L. Repeat test-
overt hypothyroidism. toms in patients with elevated serum ing 2 months later reveals a serum TSH
If she were contemplating preg- TSH concentrations higher than 4.5 but of 14 mIU/L, FT 4 of 1.3 ng/dL (17
nancy, treatment with levothyroxine lower than 10 mIU/L. While there ap- pmol/L), and total serum cholesterol of
should be started, and serum TSH pear to be no adverse effects of initiat- 235 mg/dL (6.09 mmol/L). Current
should be restored to the reference ing levothyroxine treatment in this set- medications included metformin, 850
range. Although some data suggest that ting, inadvertent overtreatment occurs mg twice each day, hydrochlorothia-
withholding treatment may result in an in about 20% (range, 14%-21%)12,13 of zide, 25 mg/d, and pravastatin, 20 mg/d.
increased risk of fetal loss and neuro- levothyroxine-treated patients, carry- He reports occasional constipation and
psychological complications in the off- ing the potential risks of osteoporosis fatigue. His physical examination find-
spring,5,6 there is no compelling evi- and atrial fibrillation when serum TSH ings are unremarkable other than obe-
dence that levothyroxine decreases the falls below 0.1 mIU/L. Treatment also sity (body mass index of 35).
risk of miscarriage or improves the neu- involves the costs and inconvenience Among patients with a serum TSH
ropsychiatric complications. The re- of taking a daily medicine for the rest higher than 10 mIU/L and normal se-
quirement for levothyroxine in treated of ones life. Although follow-up diag- rum FT4 who have signs and symp-
hypothyroid patients often increases nostic testing to adjust dosage is also toms possibly consistent with hypo-
during pregnancy and serum TSH necessary, periodic thyroid function thyroidism, there is suggestive evidence
should be monitored each trimester. tests are also necessary in individuals supporting treatment with levothyrox-
Patient 2. During an annual evalu- who are not treated. ine. Potential benefits include a lower-
ation, a healthy 70-year-old woman Patient 3. A 58-year-old sedentary, ing of serum total and LDL choles-
complained of mild fatigue, dry skin, obese man with well-controlled hyper- terol concentrations, an improvement
and constipation. Physical examina-
tion results were normal, including a Figure 2. Suggested Approach to Diagnosis and Management of Subclinical Hyperthyroidism
nonpalpable thyroid gland and nor-
mal relaxation phase of deep tendon re- Serum TSH <0.45 mIU/L
flexes. The serum TSH was 8.1 mIU/L;
serum total cholesterol, 215 mg/dL Yes Signs or Symptoms of Heart Disease (Congestive No
Heart Failure, Atrial Fibrillation, or Arrhythmias)?
(5.57 mmol/L); high-density lipopro-
tein (HDL) cholesterol, 47 mg/dL (1.22
mmol/L); LDL cholesterol, 148 mg/dL Repeat Serum TSH Measurement With Repeat Serum TSH Measurement With
FT4 and T3 or FT3 FT4 and T3 or FT3
(3.83 mmol/L); and triglycerides, 78 Measurements Within 2 Weeks Measurements 3 to 12 Weeks Later
mg/dL (0.88 mmol/L). Repeat testing
Yes No
2 months later revealed a serum TSH FT4 or
T3 Elevated?
of 8.3 mIU/L and an FT4 of 1.4 ng/dL Monitor Serum
(18 pmol/L). No Serum TSH Within Reference Yes TSH Every 12 mo
Evaluate and Treat or Sooner
Up to 20% of women older than 60 Range (0.45 to 4.5 mIU/L)?
if Symptoms
years have subclinical hypothyroid- Develop
ism; 75% of those have serum TSH be-
tween 4.5 and 10 mIU/L.1,7,8 Routine Serum TSH <0.1 mIU/L Serum TSH 0.1 to 0.45 mIU/L
treatment with levothyroxine is not rec-
ommended because data are insuffi- Determine Etiology (Radioactive Iodine Uptake and Scan)
cient to link this degree of hypothy-
roidism with any adverse health Monitor; No
Graves
Yes
No Treatment;
No
Heart Disease,
Yes
Disease or Monitor 3 to 12 mo Osteoporosis, or
outcomes, and no clear benefits of treat- Treatment
Optional
Nodular Later or Sooner if Symptoms of
Goiter? Symptoms Develop Hyperthyroidism?
ment have been demonstrated. How-
ever, because this patient has symp- Monitor;
Heart Disease, Determine Etiology (Radioactive
No Osteoporosis, Yes
toms that may be associated with Treatment
Age >60 y, or Estrogen
Iodine Uptake and Scan);
Consider Treatment
Optional
hypothyroidism, levothyroxine treat- Depleted?
ment may be considered. Although one Consider Treatment
study found patients with subclinical
hypothyroidism to have more symp- TSH indicates thyroid-stimulating hormone; FT4, free T4; FT3, free T3.
2004 American Medical Association. All rights reserved. (Reprinted) JAMA, January 14, 2004Vol 291, No. 2 241
Downloaded from www.jama.com on December 13, 2006
SUBCLINICAL THYROID DISEASE
in cardiac function, and a possible im- is usually low in these situations. tinodular goiter is the likely etiology.
provement in symptoms. However, the Patients with serum TSH levels be- A 24-hour radioiodine uptake and ra-
study suggesting that levothyroxine tween 0.1 and 0.45 mIU/L infre- dionuclide thyroid scan is the most ef-
treatment reduced cholesterol levels quently progress to overt hyperthyroid- ficient method to distinguish the vari-
among individuals with subclinical hy- ism, defined as serum TSH lower than ous etiologies of hyperthyroidism.
pothyroidism did not compare treated 0.1 mIU/L and elevated concentra- Hyperthyroidism due to the various
with untreated groups,14 and the small, tions of FT4 and/or FT3. However, the forms of destructive thyroiditis is tran-
unblinded trials suggesting that treat- rate of progression varies according to sient and self-limited; the 24-hour ra-
ment improved cardiac function exam- the underlying etiology. Patients with dioioidine uptake is close to zero when
ined intermediate end points of uncer- large autonomously functioning ad- these conditions are present. In con-
tain clinical significance.4 No blinded, enomas (3.0 cm diameter) or toxic trast, individuals with Graves hyper-
randomized controlled studies have as- multinodular thyroids are at greater risk thyroidism have normal or elevated 24-
sessed the impact of levothyroxine on for progression to overt hyperthyroid- hour radioiodine uptakes and a
important clinical cardiac end points. ism, especially when exposed to high homogeneous pattern on radionu-
Because the risk of progression to overt concentrations of iodine, most com- clide scan. Autonomous adenomas ap-
hypothyroidism may be higher in these monly after treatment with amioda- pear as hot nodules on scans. Indi-
patients than in patients with serum rone or radiocontrast agents. viduals with toxic nodular goiters may
TSH between 4.5 and 10 mIU/L, treat- Routine treatment is likely not ben- have single or multiple hot areas but
ment may prevent the manifestations eficial in young asymptomatic per- commonly have a heterogeneous pat-
and consequences of hypothyroidism sons because there are no data that this tern of uptake.
in those who would have progressed. condition is associated with adverse Thyroid autonomy in a single-
After discussing the potential ben- health outcomes. Additional studies nodule or multinodular goiter in-
efits of treatment on his serum choles- such as a 24-hour radioiodine uptake creases the likelihood of progression to
terol concentration, exercise toler- and radionuclide thyroid scan to de- subclinical or overt hyperthyroidism,
ance, and constipation, the patient termine the etiology of the subclinical especially if patients receive excess io-
decided to begin treatment with levo- hyperthyroidism are usually not nec- dine such as radiocontrast dyes or amio-
thyroxine. essary in asymptomatic individuals with darone. However, nodules that do not
Patient 4. A 36-year-old healthy serum TSH concentrations in this range, concentrate radioactive iodine (cold
woman was found to have a serum TSH if therapy is not being considered. In nodules) also occur in this setting and
concentration of 0.26 mIU/L, which is older patients, however, treatment in some individuals with Graves dis-
in the low (0.45 mIU/L) but detect- should be based on clinical judgment ease. These nodules may require a fine-
able (0.1 mIU/L) range. She has no because of a possible association of sub- needle aspiration biopsy.
personal or family history of thyroid dis- clinical hyperthyroidism with in- Untreated subclinical hyperthyroid-
ease. She has one child and has monthly creased cardiovascular mortality and os- ism with suppressed serum TSH (0.1
menstrual periods. Her examination re- teoporosis and the higher risk of mIU/L) carries the potential risks of atrial
sults were unremarkable, and her thy- progression to hyperthyroidism. fibrillation,15 cardiovascular mortal-
roid gland was not palpable. Patient 5. An active 77-year-old ity,16 and osteoporosis.17,18 Because these
When the serum TSH concentra- woman with a history of myocardial in- risks are higher among patients older
tion is found to be low but detectable, farction and osteoporosis feels well than 60 years, the balance is shifted to-
the assay should be repeated along with other than experiencing rare exer- ward treatment among older patients.
a serum FT4 and total or free T3 con- tional angina. She takes atenolol and There are no studies that compare the
centration within several months, atorvastatin daily, alendronate weekly. risk of atrial fibrillation in treated vs un-
sooner if any cardiac signs or symp- Her pulse is 75/min and she is normo- treated patients, but bone density is
toms are present such as atrial fibrilla- tensive. Her thyroid gland is difficult higher in treated compared with un-
tion or palpitations. If free thyroid hor- to examine due to kyphosis but feels treated postmenopausal women with
mone concentrations are within their somewhat prominent. Thyroid func- subclinical hyperthyroidism and de-
reference ranges and serum TSH re- tion tests reveal serum TSH concentra- creased serum TSH.19,20 The risks of treat-
mains low, the following causes of low tion lower than 0.01 mIU/L and FT4 and ment include allergic reactions (rash, fe-
serum TSH should be excluded: treat- FT3 within the reference ranges. A thy- ver, arthralgias, agranulocytosis,
ment with levothyroxine, high-dose roid ultrasound reveals a multinodu- hepatotoxicity, vasculitis) after antithy-
glucocorticoid or dopamine therapy, se- lar goiter. She has not received iodin- roid drug administration, and transient
vere nonthyroidal illness, or preg- ated contrast material in the past year. worsening hyperthyroidism, perma-
nancy. Although a low serum TSH may Although other causes of low se- nent hypothyroidism, or worsening
also be due to hypothalamic or pitu- rum TSH should be sought, subclini- Graves ophthalmopathy after therapy
itary disease or anorexia nervosa, FT4 cal hyperthyroidism due to a toxic mul- with iodohippurate sodium I 131.21
242 JAMA, January 14, 2004Vol 291, No. 2 (Reprinted) 2004 American Medical Association. All rights reserved.
Downloaded from www.jama.com on December 13, 2006
SUBCLINICAL THYROID DISEASE
Conclusion It is impossible to assess the merits tion to detect occult thyroid dysfunc-
The definition of subclinical thyroid dys- of determination of serum TSH to tion will be greater among those
function is based on serum TSH deter- screen for occult subclinical disease populations at higher risk for develop-
mination and is of necessity somewhat without addressing the merits of screen- ing overt disease, including women,
arbitrary. There is substantial uncer- ing for occult overt thyroid disease, older persons, and individuals with pre-
tainty concerning the consequences of since both use the same test. Any at- vious or family history of thyroid
untreated subclinical hypothyroidism tempt to screen for overt disease will disease, type 1 diabetes mellitus, radio-
and hyperthyroidism, as well as the ben- likely yield a far greater number of cases active iodine treatment for hyperthy-
efit of initiating treatment. Although of subclinical than overt disease. Un- roidism, recurrent miscarriages, or ad-
treatment may be beneficial in individu- like subclinical disease, the benefits of ministration of medications that may
als with serum TSH lower than 0.1 mIU/L detecting and treating overt thyroid dis- affect thyroid function, such as lithium
or higher than 10 mIU/L, most persons ease are established. Until clear thera- carbonate or interferon. Vigorous case
found to have subclinical thyroid dys- peutic benefits are established for treat- finding is recommended in these popu-
function will have values between 0.1 ing subclinical thyroid dysfunction, lations. Among those found to have
and 0.45 mIU/L or between 4.5 and 10 general population screening for these subclinical disease, patient prefer-
mIU/L, for which the benefits of treat- conditions is not recommended. How- ences are important in deciding on
ment are not clearly established. ever, the benefits of TSH determina- management.
REFERENCES
1. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. rotrophin (TSH) concentrations in the elderly in the J Clin Endocrinol Metab. 2001;86:4860-4866.
The Colorado Thyroid Disease Prevalence Study. Arch United Kingdom. Clin Endocrinol (Oxf ). 1991;34:77- 15. Sawin CT, Geller A, Wolf PA, et al. Low serum
Intern Med. 2000;160:526-534. 83. thyrotropin concentrations as a risk factor for atrial fi-
2. Vanderpump MP, Tunbridge WM, French JM, et 9. Zulewski H, Muller B, Exer P, Miserez AR, Staub brillation in older persons. N Engl J Med. 1994;331:
al. The incidence of thyroid disorders in the com- JJ. Estimation of tissue hypothyroidism by a new clini- 1249-1252.
munity: a twenty-year follow-up of the Whickham cal score: evaluation of patients with various grades 16. Parle JV, Maisonneuve P, Sheppard MC, Boyle P,
Survey. Clin Endocrinol (Oxf ). 1995;43:55-68. of hypothyroidism and controls. J Clin Endocrinol Franklyn JA. Prediction of all-cause and cardiovascu-
3. Muller AF, Drexhage HA, Berghout A. Postpar- Metab. 1997;82:771-776. lar mortality in elderly people from one low serum thy-
tum thyroiditis and autoimmune thyroiditis in women 10. Bemben DA, Hamm RM, Morgan L, Winn P, Davis rotropin result: a 10-year cohort study. Lancet. 2001;
of childbearing age: recent insights and conse- A, Barton E. Thyroid disease in the elderly, part 2: pre- 358:861-865.
quences for antenatal and postnatal care. Endocr Rev. dictability of subclinical hypothyroidism. J Fam Pract. 17. Faber J, Galloe AM. Changes in bone mass dur-
2001;22:605-630. 1994;38:583-588. ing prolonged subclinical hyperthyroidism due to L-
4. Biondi B, Palmieri EA, Lombardi G, Fazio S. Effects 11. Lindeman RD, Schade DS, LaRue A, et al. Sub- thyroxine treatment: a meta-analysis. Eur J Endocri-
of subclinical thyroid dysfunction on the heart. Ann clinical hypothyroidism in a biethnic urban commu- nol. 1994;41:421-424.
Intern Med. 2002;137:904-914. nity. J Am Geriatr Soc. 1999;47:703-709. 18. Uzzan B, Campos J, Cucherat M, et al. Effects on
5. Haddow JE, Palomaki GE, Allan WC, et al. Mater- 12. Ross DS, Daniels GH, Gouveia D. The use and limi- bone mass of long term treatment with thyroid hor-
nal thyroid deficiency during pregnancy and subse- tations of a chemiluminescent thyrotropin assay as a mones: a meta-analysis. J Clin Endocrinol Metab. 1996;
quent neuropsychological development of the child. single thyroid function test in an outpatient endocrine 81:4278-4289.
N Engl J Med. 1999;341:549-555. clinic. J Clin Endocrinol Metab. 1990;71:764-769. 19. Kumeda Y, Inaba M, Tahara H, et al. Persistent
6. Klein RZ, Sargent JD, Larsen PR, Waisbren SE, Had- 13. Parle JV, Franklyn JA, Cross, KW, Jones SR, Shep- increase in bone turnover in Graves patients with sub-
dow JE, Mitchell ML. Relation of severity of maternal pard MC. Thyroxine prescription in the community: clinical hyperthyroidism. J Clin Endocrinol Metab.
hypothyroidism to cognitive development of off- serum thyroid stimulating hormone level assays as an 2000;85:4157-4161.
spring. J Med Screen. 2001;8:18-20. indicator of undertreatment or overtreatment. Br J Gen 20. Pantazi H, Papapetrou PD. Changes in param-
7. Sawin CT, Castelli WP, Hershman JM, et al. The Pract. 1993;43:107-109. eters of bone and mineral metabolism during therapy
aging thyroid: thyroid deficiency in the Framingham 14. Meier C, Staub JJ, Roth CB, et al. TSH-controlled for hyperthyroidism. J Clin Endocrinol Metab. 2000;
Study. Arch Intern Med. 1985;145:1386-1388. L-thyroxine therapy reduces cholesterol levels and clini- 85:1099-1106.
8. Parle JV, Franklyn JA, Cross KW, Jones SC, Shep- cal symptoms in subclinical hypothyroidism: a double- 21. Cooper DS. Hyperthyroidism. Lancet. 2003;362:
pard MC. Prevalence and follow-up of abnormal thy- blind, placebo-controlled trial (Basel Thyroid Study). 459-468.
2004 American Medical Association. All rights reserved. (Reprinted) JAMA, January 14, 2004Vol 291, No. 2 243
Downloaded from www.jama.com on December 13, 2006
You might also like
- 2004 JAMA SubclinicalDocument11 pages2004 JAMA SubclinicalfaisalsyahrilNo ratings yet
- Approach To The Patient With Postpartum Thyroid It IsDocument9 pagesApproach To The Patient With Postpartum Thyroid It IsfaisalsyahrilNo ratings yet
- Subclinical ObstetGynecol 239Document7 pagesSubclinical ObstetGynecol 239faisalsyahrilNo ratings yet
- 2016-04-15 Banjarmasin DisolfDocument41 pages2016-04-15 Banjarmasin DisolffaisalsyahrilNo ratings yet
- Aml AplDocument14 pagesAml AplfaisalsyahrilNo ratings yet
- Morning Report Ferdy SullivanDocument8 pagesMorning Report Ferdy SullivanfaisalsyahrilNo ratings yet
- Editorial: Introduction To The Review Series On Advances in Acute Myeloid Leukemia (AML)Document2 pagesEditorial: Introduction To The Review Series On Advances in Acute Myeloid Leukemia (AML)faisalsyahrilNo ratings yet
- Sensus Pasien Bangsal Periode Oktober2016 Penyakit Dalam PriaDocument3 pagesSensus Pasien Bangsal Periode Oktober2016 Penyakit Dalam PriafaisalsyahrilNo ratings yet
- Sensus Pasien Bangsal Periode Oktober 2016 Penyakit Dalam PriaDocument4 pagesSensus Pasien Bangsal Periode Oktober 2016 Penyakit Dalam PriafaisalsyahrilNo ratings yet
- Aml AplDocument14 pagesAml AplfaisalsyahrilNo ratings yet
- Nej Mo A 1516192Document13 pagesNej Mo A 1516192faisalsyahrilNo ratings yet
- Sensus Pasien Bangsal Periode Oktober 2016 Penyakit Dalam Pria (TEAM 1)Document2 pagesSensus Pasien Bangsal Periode Oktober 2016 Penyakit Dalam Pria (TEAM 1)faisalsyahrilNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2019q123.ev3-Descon Engro Level Gauges-QDocument7 pages2019q123.ev3-Descon Engro Level Gauges-Qengr_umer_01No ratings yet
- Analyse Bacterologique de L EauDocument6 pagesAnalyse Bacterologique de L Eaupeguy diffoNo ratings yet
- Delegate List - 10th IMRC With Contact Details - Removed (1) - Removed (1) - Removed (1) - RemovedDocument100 pagesDelegate List - 10th IMRC With Contact Details - Removed (1) - Removed (1) - Removed (1) - RemovedSharon SusmithaNo ratings yet
- Biography of Anna HazareDocument4 pagesBiography of Anna HazareGenesis FirstNo ratings yet
- 1.6 FSI Inlet Manifold Removal Guide - Audi A2 Owners' ClubDocument3 pages1.6 FSI Inlet Manifold Removal Guide - Audi A2 Owners' Clubdusan jovanovicNo ratings yet
- Rich Gas and Lean GasDocument7 pagesRich Gas and Lean GasManish GautamNo ratings yet
- Automatic Coconut Dehusking MachineDocument12 pagesAutomatic Coconut Dehusking MachineKumaresh Salem0% (1)
- CR-805 Retransfer PrinterDocument2 pagesCR-805 Retransfer PrinterBolivio FelizNo ratings yet
- Data Analyst Chapter 3Document20 pagesData Analyst Chapter 3Andi Annisa DianputriNo ratings yet
- Taxonomy: Family StaphylococcaceaeDocument40 pagesTaxonomy: Family StaphylococcaceaeMarissa Terrado SorianoNo ratings yet
- Theben Timer SUL 181DDocument2 pagesTheben Timer SUL 181DFerdiNo ratings yet
- What On Earth Is A MainframeDocument132 pagesWhat On Earth Is A MainframeCarlos DantasNo ratings yet
- Tip Sheet March 2017Document2 pagesTip Sheet March 2017hoangvubui4632No ratings yet
- L15 PDFDocument15 pagesL15 PDFlesNo ratings yet
- A Control Method For Power-Assist Devices Using A BLDC Motor For Manual WheelchairsDocument7 pagesA Control Method For Power-Assist Devices Using A BLDC Motor For Manual WheelchairsAhmed ShoeebNo ratings yet
- Wind LoadingDocument18 pagesWind LoadingStephen Ogalo100% (1)
- Permutation, Combination & ProbabilityDocument9 pagesPermutation, Combination & ProbabilityVicky RatheeNo ratings yet
- 30xa 100t PDFDocument162 pages30xa 100t PDFleung ka kitNo ratings yet
- Intermediate Programming (Java) 1: Course Title: Getting Started With Java LanguageDocument11 pagesIntermediate Programming (Java) 1: Course Title: Getting Started With Java LanguageRickCy Perucho PccbsitNo ratings yet
- Combat Storm - Shipping ContainerDocument6 pagesCombat Storm - Shipping ContainermoiNo ratings yet
- José Guadalupe PosadaDocument19 pagesJosé Guadalupe PosadaJudy Baca100% (1)
- Expansions Meet Health Care Needs: Economists Question Trump Plan FiguresDocument10 pagesExpansions Meet Health Care Needs: Economists Question Trump Plan FiguresThe Daily Tar HeelNo ratings yet
- Esp Kelompok 2Document19 pagesEsp Kelompok 2Taufiq DiNo ratings yet
- Teccrs 3800Document431 pagesTeccrs 3800Genus SumNo ratings yet
- Perfect Picture SummaryDocument3 pagesPerfect Picture SummaryReiaNo ratings yet
- Sharp Product-Catalogue 2019 enDocument48 pagesSharp Product-Catalogue 2019 enMiki di KaprioNo ratings yet
- Full Download Human Biology 11th Edition Starr Solutions ManualDocument35 pagesFull Download Human Biology 11th Edition Starr Solutions Manualsheathe.zebrinny.53vubg100% (41)
- Misc Ar2019Document207 pagesMisc Ar2019Sharon12 ArulsamyNo ratings yet
- Construction of Perimeter Fence of BFP NHQ PDFDocument133 pagesConstruction of Perimeter Fence of BFP NHQ PDFYalla ChaitanyaNo ratings yet
- Wa200-8 Venss06304 1904 PDFDocument24 pagesWa200-8 Venss06304 1904 PDFOktiano BudiNo ratings yet