Professional Documents
Culture Documents
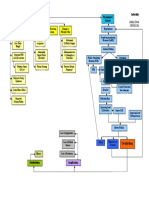
Cholecystitis Concept Map
Uploaded by
nursing concept mapsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cholecystitis Concept Map
Uploaded by
nursing concept mapsCopyright:
Available Formats
Admission date:
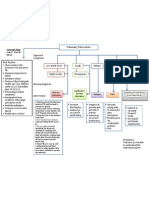
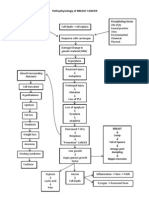
Risk factors Pathophysiology
Admitting diagnosis:
A family history of gallstones on Cholecystitis, an acute complication of cholelithiasis, is an acute infection of the gallbladder. Most patients
Cholesistitis the mother's side of the with cholecystitis have gallstones (calculous cholecystitis). A gallstone obstructs bile outflow and bile in
family. the gallbladder initiates a chemical reaction, resulting in edema, compromise of the vascular supply, and
Surgical procedure: N/A Crohn's disease. gangrene. In the absence of gallstones, cholecystitis (acalculous) may occur after surgery, severe trauma,
Diabetes. or burns, or with torsion, cystic duct obstruction, multiple blood transfusions, and primary bacterial
Pertinent PMH/PSH: infections of the gallbladder. Infection causes pain, tenderness, and rigidity of the upper right abdomen and
Hyperlipidemia.
is associated with nausea and vomiting and the usual signs of inflammation. Purulent fluid inside the gall-
Obesity, HTN, Asthma, CKD, Sepsis, Losing weight rapidly. bladder indicates an empyema of the gallbladder.
Drug rash, A-fib Obesity.
Older age.
Last V/S, including O2 sat and pain
scale Diagnostic tests with discussion of
BP-141/76, HR-74, RR-12, expected/unexpected findings
Patient S/S Lab values with discussion of
SpO2-97%, Temp 36.7C expected/unexpected findings CT scan Abd-pelvic with contrast
Dark urine, distended
Current treatments (IV, medications, gallbladder; fever and palpable Na- 134, K-3.7 , Cr- 1.29, BUN- 21, CT scan of abdomen with contrast
catheters, tubes, drains. O2, abdominal mass; biliary colic
ostomies) with excruciating upper right Hgb- 11.0 , Hct- 33.5, Albumin- 2.7,
abdominal pain, radiating to
O2- NC- 2L RBC- 3.54, WBC- 6.0
back or right shoulder
Biliary drain- Right outer quadrant restlessness and colicky pain
Foley Catheter-
PICC-single lumen-left upper bacillic
IV- left forearm, NS locked
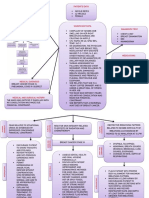
Priority Nursing Diagnoses Priority Assessments
Recommended consults: N/A
1. Anxiety related to present medical condition as evidenced by being Assess health history: Note history of smoking or prior
less cooperative with the staff members and refusing to participate respiratory problems. Assess respiratory status: Note
Nutrition Regular diet shallow respirations, persistent cough, or ineffective or
in activities
adventitious breath sounds. Evaluate nutritional status
PT/OT/Speech: PT, OT (dietary history, general examination, and laboratory
2. Disturbed body image related to being overweight and having not study results). Connect tubes to drainage receptacle and
Mental Health intact skin as a result of hypersensitivity reaction as evidenced by secure tubing to avoid kinking (elevate above abdomen).
low self esteem and anger. Place drainage bag in patients pocket when ambulating.
History of depression Observe for indications of infection, leakage of bile, and
obstruction of bile drainage. Observe for jaundice
Other: Allergies 3. Imbalanced nutrition: less than body requirements related to having (check the sclera). Note and report right upper quadrant
decreased appetite as evidenced by low albumin levels. abdominal pain, nausea and vomiting, bile drainage
around any drainage tube, clay-colored stools, and a
4. Risk for impaired skin integrity related to altered nutritional state change in vital signs. Change dressing frequently, using
ointment to protect skin from irritation.
1. Anxiety related to present medical condition as evidenced by being less cooperative with the staff members and
refusing to participate in activities
Interventions with rationale and citation
Expected Outcomes (2)
1. Patient will discuss realistic 1. Assess the clients level of anxiety and physical reactions to anxiety. Symptoms evaluated are mood, tension,
fear, insomnia, concentration, worry, depressed mood, somatic complaints, and cardiovascular, respiratory,
goals related to medical
gastrointestinal, genitourinary, autonomic, and behavioral symptoms. Anxiety is the risk factor for major
condition within 24 hours adverse cardiac risk events in persons with stable coronary artery disease. (Akley, 2013, p.138
2. Patient will seek help in 2. Use empathy to encourage the client to interpret the anxiety symptoms as normal. The way a nurse
dealing with feelings by interacts with a client influences his/her quality of life. Providing psychological and social support can reduce
the symptoms and problems associated with anxiety. (Akley, 2013, p.138)
verbalizing his need in
3. If irrational thoughts or fears are present, offer the client accurate information and encourage him or her to
support within 24 hours talk about the meaning of the events contributing to the anxiety. Avoid and suppress painful emotions,
thoughts and sensations, and limit their involvement in meaningful activities. (Akley, 2013, p.138)
4. Encourage the client to use meaningful self-talk. Reducing negative self-talk and increasing positive self-talk
can be beneficial for all types of anxiety. (Akley, 2013, p.138)
5. Intervene when possible to remove sources of anxiety. Removing or reducing sources of stress and anxiety
among patients has been shown to decrease hypertension and comorbid conditions. (Akley, 2013, p.138)
6. Explain all activities, procedures and issues that involve the client; use nonmedical terms and calm, slow
speech Do this in advance of procedures when possible and validate the clients understanding. Effective
nurse-client communication is critical to efficient care provision. (Akley, 2013, p.138)
7. Provide backrubs/massage for the client to decrease anxiety. Massage was shown to be an excellent method
for reducing anxiety. (Akley, 2013, p.138)
Evaluation
8. Use therapeutic touch and healing touch techniques. Healing touch may be one of the most useful nursing
interventions available to reduce anxiety. (Akley, 2013, p.138)
9. Guided imagery can be used to decrease anxiety. Anxiety was decreased with the use of guided imagery
Goal partially met: during an intervention for post-operative pain. (Akley, 2013, p.141)
Patient demonstrated some 10. Assess client for pain and provide pain relief measures. (Akley, 2013, p.141)
control of anxiety by using 11. Assist clients with life review and reminiscence. When challenges emerged, the participants implemented
the search to find an acceptable and satisfying completion to this life, engaging family members, friends
recommended techniques by 8
and hospice team in an effort to relieve discomfort and regain a degree of control. (Akley, 2013, p.142)
hours.
12. Encourage clients to pray. Prayer, scripture reading and clergy visits were found to comfort some clients, but
sometimes-specific religious tenets may be troubling and need to be resolved before the client can find
peace. (Akley, 2013, p.142)
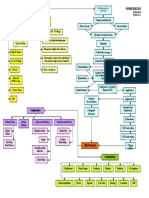
Nursing Process Concept Map
1. Disturbed body image related to being overweight and having not intact skin as a result of hypersensitivity reaction
as evidenced by low self esteem and anger.
Expected Outcomes (2)
Interventions with rationale and citation
1. Client will demonstrate
adaptation to changes in 1. Incorporate psychological questions related to body image as part of nursing assessment to identify clients at risk
physical appearance or body for body image disturbance (those with stomas/ostomies/colostomies or other disfiguring conditions). Assessment
of psychological issues can help to identify clients at risk for body image concerns as a result of a disfiguring
function as evidenced by condition. (Akley, 2013, p.162)
adjustment to lifestyle change 2. Assess for history of childhood maltreatment in clients suffering from body dissatisfaction, anorexia, or other eating
disorders and make appropriate psychosocial referrals if indicated. The result from this study indicates specific forms
by 24 hours of childhood maltreatment (emotional or sexual abuse) are significantly associated with body dissatisfaction,
2. The client will Identify and depressive symptoms, and eating disorders. (Akley, 2013, p.162)
3. Assess for the influence of cultural beliefs, regional norms, and values on the clients body image. Each client
change irrational beliefs and should be assessed for body image based on the phenomenon of communication, time space, social organization,
expectations regarding his environmental control, and biological variations. (Akley, 2013, p.164)
4. Acknowledge that body image disturbances can affect all individuals regardless of culture, race, or ethnicity. (Akley,
medical condition by 24 hours 2013, p.164)
5. Assess clients level of social support, as it is one of the determinants of clients recovery and emotional
health.Males who perceived they have good social support were found to adapt better to changes in body image.
(Akley, 2013, p.164)
6. Encourage client to discuss concerns related to sexuality and provide support or information as indicated. Many
conditions that affect body image also affect sexuality. Brown and Randle found that clients (particularly females)
with stomas often believe they are less sexually attractive after surgery, though their sexual partner may not share
that view. (Akley, 2013, p.164)
7. Use cognitive-behavioral to assist the client to express his emotions and feelings. This study of clients with bulimia
Evaluation used CBT and helped the clients to disentangle themselves regarding body image and weight. (Akley, 2013, p.162)
8. Help client describe ideal self, identity self-criticisms, and give suggestions to support acceptance of self. Job
rehabilitation and body image should be incorporated into daily care of head and neck cancer clients. For example,
participants could learn how to use cosmetic strategies to improve their facial appearance during OPD syndrome
Goal was not met: follow up. Thus, the negative impact might be reduced. (Akley, 2013, p.162)
9. Discuss spirituality as an adjunct to improving bod y satisfaction. (Akley, 2013, p.163)
10. Provide client with list of appropriate community support groups. This study of three different cancer groups
Patient didnt demonstrate showed their perceived benefits were similar; the groups provided information, acceptance, and understanding.
adjustment to the changes in physical (Akley, 2013, p.163)
11. Focus on remaining abilities. Have client make a list of strengths Results from unstructured interviews with women
appearance by verbalizing he didnt aged 61 to 92 years regarding their perceptions and feelings about their aging bodies suggest that women exhibit the
feel comfortable in his skin. internalization of ageist beauty norms, even as they assert that health is more important to them than physical
attractiveness and comment on the naturalness of the aging process. (Akley, 2013, p.163)
12. Refer clients who are having difficulty with personal acceptance, personal and social body image disruption, sexual
concerns, reduced self-care skills, and the management of surgical complications to an interdisciplinary team or
specialist (eg. ostomy nurse) if available. There is sufficient research-based evidence to conclude that intestinal
ostomy surgery exerts a clinically relevant impact on health-related quality of life, and that nursing interventions
can ameliorate this effect. (Akley, 2013, p.164)
References:
1. Ackley, B. J., & Ladwig, G. B. (2010). Nursing diagnosis handbook: an evidence-based guide to planning care (9th ed.). Maryland Heights, Mo.:
Mosby.
NursingJ.Process
2. Johnson, Concept
Y. (2010). Map for Brunner & Suddarth's textbook of medical-surgical nursing (12th ed.). Philadelphia: Wolters
Handbook
Kluwer/Lippincott Williams & Wilkins.
You might also like
- Hypertension Concept MapDocument1 pageHypertension Concept Mapgfhbgfhgf71% (7)
- Hypertension Concept MapDocument1 pageHypertension Concept Mapnursing concept maps100% (1)
- Concept Map of DMDocument2 pagesConcept Map of DMLeslie Marie Rendon100% (9)
- Renal Diseases PathophysiologyDocument6 pagesRenal Diseases PathophysiologyBilly Gayados100% (1)
- Breast Cancer Risk Factors and PathophysiologyDocument1 pageBreast Cancer Risk Factors and PathophysiologyDianne Kate CadioganNo ratings yet
- Brain Cancer Concept MapDocument3 pagesBrain Cancer Concept MapIced Coffee100% (4)
- Final Lung Cancer Concept MapDocument3 pagesFinal Lung Cancer Concept MapKaycee TolingNo ratings yet
- Cholecystitis Nursing Care PlanDocument4 pagesCholecystitis Nursing Care PlanMDCITY83% (6)
- Hypothyroidism Concept MapDocument5 pagesHypothyroidism Concept Mapnursing concept maps0% (1)
- Concept Map Pleural EffusionDocument1 pageConcept Map Pleural Effusionapi-341263362No ratings yet
- Concept MapDocument2 pagesConcept MapCrystal Leigh Malunes Dagting83% (6)
- Concept Map PTBDocument1 pageConcept Map PTBJoan Abardo100% (2)
- Pathophysiology of StrokeDocument3 pagesPathophysiology of StrokeAqeel Al-Mahdaly0% (1)
- Renal and Urinary Concept MapsDocument8 pagesRenal and Urinary Concept Mapsnursing concept maps100% (1)
- Concept MapDocument6 pagesConcept Mapmenickel3100% (1)
- Bipolar Concept MapDocument3 pagesBipolar Concept Mapnursing concept maps100% (2)
- Concept Map COPDDocument2 pagesConcept Map COPDJilian McGugan88% (40)
- Colorectal Concept Map Group 2Document2 pagesColorectal Concept Map Group 2Maria CristinaNo ratings yet
- Lung Cancer Concept Map-Group 2Document2 pagesLung Cancer Concept Map-Group 2Maria Cristina100% (2)
- Pathophysiology - PyelonephritisDocument2 pagesPathophysiology - PyelonephritisFrancis Kevin Sagudo92% (13)
- Small Bowel Obstruction Care PlanDocument11 pagesSmall Bowel Obstruction Care PlanKatie YarnellNo ratings yet
- Pathophysiology of AppendicitisDocument3 pagesPathophysiology of AppendicitisArvin Ian Penaflor100% (3)
- Pathophysiology of Acute PyelonephritisDocument2 pagesPathophysiology of Acute Pyelonephritisgodwinkent888No ratings yet
- Acute Kidney Injury Concept MapDocument1 pageAcute Kidney Injury Concept MapKEn PilapilNo ratings yet
- Asthma Pathophysiology and TreatmentDocument3 pagesAsthma Pathophysiology and TreatmentKaren HutchinsonNo ratings yet
- Pathophysiology of BPH: Risk Factors, Symptoms & TreatmentDocument1 pagePathophysiology of BPH: Risk Factors, Symptoms & TreatmentKevin Jade Herrera0% (2)
- Causes, Signs, Tests and Treatment of Iron Deficiency AnemiaDocument1 pageCauses, Signs, Tests and Treatment of Iron Deficiency AnemiaZam Pamate67% (3)
- BURNS Concept MapDocument1 pageBURNS Concept Mapnursing concept maps100% (2)
- Urinary RetentionDocument6 pagesUrinary Retentionjakenathanielvelasco50% (2)
- Nursing Care Plan for Patient with LymphedemaDocument1 pageNursing Care Plan for Patient with Lymphedemayasira50% (2)
- Clinical Concept Map-7Document1 pageClinical Concept Map-7Brandi Offield100% (1)
- Acute PainDocument1 pageAcute Painnursing concept mapsNo ratings yet
- Breast Cancer Concept MapDocument1 pageBreast Cancer Concept MapKeepItSecret100% (1)
- Fluid and Electrolyte MapsDocument10 pagesFluid and Electrolyte MapsChrFaNo ratings yet
- Hyponatremia Algorhythm Concept MapDocument2 pagesHyponatremia Algorhythm Concept Mapnursing concept mapsNo ratings yet
- Breast Cancer Concept MapDocument2 pagesBreast Cancer Concept MapMaria Cristina100% (1)
- Small Bowel Obstruction Concept MapDocument1 pageSmall Bowel Obstruction Concept MapTessa Claire JaranowskiNo ratings yet
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDocument2 pagesNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- Patho UtiDocument1 pagePatho UtiCarl Mayrina de Jesus100% (1)
- Pathophysiology of Nephrolithiasis, Struvites Stone (Staghorn Calculi)Document2 pagesPathophysiology of Nephrolithiasis, Struvites Stone (Staghorn Calculi)Floyd100% (2)
- Nursing Care Plan Mobility SampleDocument6 pagesNursing Care Plan Mobility Samplen2biologyNo ratings yet
- UTI Patient Concept Map Nursing Diagnosis Interventions OutcomesDocument1 pageUTI Patient Concept Map Nursing Diagnosis Interventions OutcomesDon Rieza100% (1)
- Pa Tho Physiology of PyelonephritisDocument2 pagesPa Tho Physiology of PyelonephritisYuan Li100% (1)
- Concept Map of CellulitisDocument8 pagesConcept Map of CellulitisReese Anne100% (1)
- STUDENT-Eating - Disorder-F&E-UNFOLDING ReasoningDocument14 pagesSTUDENT-Eating - Disorder-F&E-UNFOLDING ReasoningPeggy100% (12)
- Benign Prostatic Hyperplasia Concept MapDocument1 pageBenign Prostatic Hyperplasia Concept MapJason A. AdoyoganNo ratings yet
- Concept Map SeizuresDocument1 pageConcept Map SeizuresMary GiuntiniNo ratings yet
- Reason For Needing Health Care: Key Problem / ND: Noncompliance Key Problem / NDDocument6 pagesReason For Needing Health Care: Key Problem / ND: Noncompliance Key Problem / NDnursing concept mapsNo ratings yet
- Concept Map 3 MM (Abdominal Pain)Document2 pagesConcept Map 3 MM (Abdominal Pain)Matt McKinleyNo ratings yet
- NCP DiverticulitisDocument6 pagesNCP DiverticulitisLovely Cacapit100% (1)
- Acute Gastroenteritis Pathophysiology ExplainedDocument2 pagesAcute Gastroenteritis Pathophysiology ExplainedMareeze Hatta100% (1)
- MALABSORPTIONDocument3 pagesMALABSORPTIONZyra LagatNo ratings yet
- Nursing Care at Mr. A With Digestive System Disorders: AppendicitisDocument20 pagesNursing Care at Mr. A With Digestive System Disorders: AppendicitisAfri YaniNo ratings yet
- NCP Nausea and VomitingDocument4 pagesNCP Nausea and VomitingKingJayson Pacman06No ratings yet
- Epp Bab 1-2Document17 pagesEpp Bab 1-2Ahmad BuchoriNo ratings yet
- Nursing Care Plan at The Gastritis Patient Desease Base ConseptDocument11 pagesNursing Care Plan at The Gastritis Patient Desease Base ConseptAkun NyampahNo ratings yet
- Protocol-ABDOMINAL DISTENTION-ServandoDocument4 pagesProtocol-ABDOMINAL DISTENTION-ServandoAllison Eunice ServandoNo ratings yet
- G4P2 Patient With Severe Abdominal PainDocument5 pagesG4P2 Patient With Severe Abdominal PainJOANA KRIS CABALTERANo ratings yet
- Abdominal TB Causing Intestinal ObstructionDocument10 pagesAbdominal TB Causing Intestinal ObstructionCleoanne GallegosNo ratings yet
- Articulo Abdomen AgudoDocument12 pagesArticulo Abdomen AgudoAlejandra VelezNo ratings yet
- Concept Map TemplateDocument1 pageConcept Map Templatenursing concept mapsNo ratings yet
- Emphysema Pathophysiology ExplainedDocument1 pageEmphysema Pathophysiology ExplainedGil AswiguiNo ratings yet
- Bipolar Concept MapDocument3 pagesBipolar Concept Mapnursing concept maps100% (2)
- Hip FractureDocument3 pagesHip Fracturenursing concept mapsNo ratings yet
- Sleep Apnea Concept MapDocument1 pageSleep Apnea Concept Mapashleydean100% (2)
- Concept Map BlankDocument2 pagesConcept Map Blanknursing concept mapsNo ratings yet
- Diagnostics: Disorder & Basic Patho/Etiology: Clinical ManifestationsDocument1 pageDiagnostics: Disorder & Basic Patho/Etiology: Clinical Manifestationsnursing concept mapsNo ratings yet
- Physiological ChangesDocument1 pagePhysiological ChangesJilian McGuganNo ratings yet
- Bronchial Asthma in Acute Exacerbation BAIAE Pathophysiology Schematic DiagramDocument3 pagesBronchial Asthma in Acute Exacerbation BAIAE Pathophysiology Schematic DiagramVictor Angelo VeraNo ratings yet
- Mental Health Concept MapDocument2 pagesMental Health Concept Mapnursing concept mapsNo ratings yet
- Diabetes Mellitus Type 2 Schematic DiagramDocument1 pageDiabetes Mellitus Type 2 Schematic DiagramJhe Lyn82% (11)
- Patent Ductus Arteriosus PathophsyiologyDocument3 pagesPatent Ductus Arteriosus Pathophsyiologynursing concept mapsNo ratings yet
- Pituitary Adenoma Concept MapDocument1 pagePituitary Adenoma Concept Mapnursing concept mapsNo ratings yet
- ESRD PathophysiologyDocument2 pagesESRD Pathophysiologynursing concept mapsNo ratings yet
- PATHODocument2 pagesPATHOmycoclitNo ratings yet
- Age Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat IntakeDocument3 pagesAge Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat Intakenursing concept mapsNo ratings yet
- PathoPhysiology of Renal Failure OverviewDocument7 pagesPathoPhysiology of Renal Failure Overviewnursing concept maps100% (1)
- Critical Care Concept MapDocument1 pageCritical Care Concept Mapkonniep69100% (1)
- ARF PathophysiologyDocument2 pagesARF Pathophysiologykathy100% (9)
- Bipolar Disorder Concept MapDocument1 pageBipolar Disorder Concept Mapnursing concept maps100% (1)
- Schizophrenia MapDocument1 pageSchizophrenia Mapnursing concept mapsNo ratings yet
- Pathophysiology of Burn InjuryDocument1 pagePathophysiology of Burn InjuryAnonymous XvwKtnSrMR100% (1)
- Pathophysio CRF2 - RevisedDocument1 pagePathophysio CRF2 - Reviseddeborah malnegroNo ratings yet
- Degenerative Disc Disease Concept MapDocument1 pageDegenerative Disc Disease Concept Mapnursing concept mapsNo ratings yet
- Nursing Management Concept MapDocument1 pageNursing Management Concept MapXy-Za Roy Marie100% (1)
- Hypertension Concept MapDocument1 pageHypertension Concept Mapashleydean100% (7)
- Pathophysiology of BREAST CANCERDocument1 pagePathophysiology of BREAST CANCERAlinor Abubacar100% (6)
- Osteoarthritis Concept MapDocument1 pageOsteoarthritis Concept Mapnursing concept maps0% (1)
- Infertility Concept MapDocument1 pageInfertility Concept Mapnursing concept maps50% (2)
- Concept MapDocument1 pageConcept Mapnursing concept mapsNo ratings yet
- Autism Navigator For Primary Care 2pDocument2 pagesAutism Navigator For Primary Care 2pdani moraNo ratings yet
- Berger (1963)Document4 pagesBerger (1963)Debbie Manalili100% (2)
- Chapter 16 LeadershipDocument18 pagesChapter 16 LeadershipRafaelKwongNo ratings yet
- Handle Toxic PeopleDocument7 pagesHandle Toxic Peoplekenayet100% (1)
- Differentiated PDFDocument21 pagesDifferentiated PDFDrAmira El-amir KhaterNo ratings yet
- FYI For Your Improvement™: A Guide For Development and Coaching For Learners, Managers, Mentors, and Feedback GiversDocument8 pagesFYI For Your Improvement™: A Guide For Development and Coaching For Learners, Managers, Mentors, and Feedback Giversnesterpi100% (4)
- DCE 5110 Assignments Sem 1 2018 - 2019Document4 pagesDCE 5110 Assignments Sem 1 2018 - 2019snas2206No ratings yet
- JPSP - 2022 - 236 PDFDocument10 pagesJPSP - 2022 - 236 PDFMa. Angela CastronuevoNo ratings yet
- Thematic Topic ListDocument2 pagesThematic Topic Listapi-262573516No ratings yet
- Culture WebDocument5 pagesCulture WebAlisa SinghNo ratings yet
- Organizational Behavior Model NotesDocument12 pagesOrganizational Behavior Model NotesSanjeevani PandeyNo ratings yet
- Women's Revealing Style of Dress and Its Relation To Blaming The Victims of Sexual ViolenceDocument5 pagesWomen's Revealing Style of Dress and Its Relation To Blaming The Victims of Sexual ViolenceJona AlderiteNo ratings yet
- Feelings & Emotions Final PresentationDocument66 pagesFeelings & Emotions Final PresentationMadiha Akhtar100% (2)
- Edward ThorndikeDocument14 pagesEdward ThorndikeAnonymous 3bB2bytk100% (2)
- Karen HorneyDocument15 pagesKaren Horneyphotocopyshop. rwuNo ratings yet
- The Effects of Bad Parenting On Children: Antisocial BehaviorDocument16 pagesThe Effects of Bad Parenting On Children: Antisocial BehaviorMinh TrịnhNo ratings yet
- Gender Development Theory and IdeologiesDocument22 pagesGender Development Theory and IdeologiesMichelle GensayaNo ratings yet
- Anthony Stevens - The Two Million-Year-Old Self PDFDocument80 pagesAnthony Stevens - The Two Million-Year-Old Self PDFCiprian Cătălin Alexandru0% (1)
- Big Ideas Simply Explained - The Psychology Book PDFDocument354 pagesBig Ideas Simply Explained - The Psychology Book PDFHuyen Nguyen100% (19)
- Filipino Values For Team EffectivenessDocument17 pagesFilipino Values For Team EffectivenessSienna Pingol VenturinaNo ratings yet
- 10 Personality DisorderDocument3 pages10 Personality DisorderaninNo ratings yet
- 0901 Hrm-I (MB2D3)Document29 pages0901 Hrm-I (MB2D3)api-19916064No ratings yet
- Discipline Efficiency Effectivity and Work ProductivityDocument8 pagesDiscipline Efficiency Effectivity and Work ProductivityDwi Ayu Andriani100% (1)
- Distributed LeadershipDocument9 pagesDistributed Leadershipapi-267712423No ratings yet
- NCP FinalDocument22 pagesNCP FinalAlmira Ahamad100% (1)
- ADOS 2 - Revised AlgorithmDocument2 pagesADOS 2 - Revised AlgorithmGoropad50% (2)
- Understanding The Four Stages of Recovery From Sex TraffickingDocument6 pagesUnderstanding The Four Stages of Recovery From Sex TraffickingMartyn PereiraNo ratings yet
- Assessing Coping Strategies: A Theoretically Based ApproachDocument17 pagesAssessing Coping Strategies: A Theoretically Based ApproachGheorghe ZastavneţchiNo ratings yet
- Education ResumeDocument4 pagesEducation Resumeapi-336690274No ratings yet
- Research On Child Psychopathology - Research Designs, Ethical Issues - NOTESDocument11 pagesResearch On Child Psychopathology - Research Designs, Ethical Issues - NOTESMAHIMA DASNo ratings yet