Professional Documents
Culture Documents
Bangal B Vidyadhar Et. Al PDF
Uploaded by
elenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bangal B Vidyadhar Et. Al PDF
Uploaded by
elenCopyright:
Available Formats
Bangal V B et. al.
/ JPBMS, 2011, 12 (05)
Available online at www.jpbms.info
ISSN NO- 2230 7885
Research article CODEN JPBSCT
JPBMS
JOURNAL OF PHARMACEUTICAL AND BIOMEDICAL SCIENCES
Incidence of oligohydramnios during pregnancy and its effects on maternal and
perinatal outcome
* Vidyadhar B. Bangal1, Purushottam A. Giri2, Bhushan M. Sali3
1Professor and Head, Dept. of Obstetrics and Gynaecology (OBGY), Rural Medical College & Pravara Rural Hospital of
Pravara Institute of Medical Sciences (Deemed University), Loni, Dist. Ahmednagar, Maharashtra, India.
2Assistant Professor, Dept. of Community Medicine (PSM), Rural Medical College & Pravara Rural Hospital of
Pravara Institute of Medical Sciences (Deemed University), Loni Dist. Ahmednagar, Maharashtra, India.
3Postgraduate student, Dept. of Obstetrics and Gynaecology (OBGY), Rural Medical College & Pravara Rural Hospital of
Pravara Institute of Medical Sciences (Deemed University), Loni Dist. Ahmednagar, Maharashtra, India.
Abstract: Oligohydramnios or reduced amount of amniotic fluid volume is a commonly observed obstetric problem
during third trimester of pregnancy. It accompanies a broad range of reproductive disorders including anomalies of fetus
and functional disorders of mother, fetus and placenta. Reduced amniotic fluid volume is associated with adverse perinatal
outcome. A prospective hospital based study of total 100 cases of oligohydramnios coming for delivery to Pravara Rural
Hospital, Loni was undertaken over a period of two years from October 2007 to September 2009. The information
regarding bio-social characteristics, maternal and perinatal outcome were collected and results were analyzed by using
percentage and proportion. In the present study, the majority of the cases( 78%) were unbooked and belonged to the age
group of 20-30 years and had associated maternal or fetal complications. Postdated pregnancy, pregnancy induced
hypertension and fetal congenital anomalies were the commonest complications associated with oligohydramnios. Forty
four percent cases were delivered by caesarean section. Overall perinatal mortality was 24%. Cases with severe
oligohydramnios and anhydramnios were associated with intrapartum fetal heart rate abnormalities, (16%) low Apgar
score and (8%) meconium aspiration syndrome. Every case of oligohydramnios needs careful evaluation, parental
counseling and individualized decision regarding timing and mode of delivery. Continuous intrapartum fetal monitoring
and good neonatal care support is essential for optimum perinatal outcome.
Keywords: Maternal outcome, perinatal outcome, Oligohydramnios
Introduction:
Oligohydramnios or reduced volume of amniotic fluid Medical College and Pravara Rural Hospital- a tertiary
poses challenge to obstetrician, when it is diagnosed level health care referral centre in Loni, Maharashtra,
before term. Oligohydramnios can develop in any India over a period of 2 years from October 2007 to
trimester, although it is more common in third trimester. September 2009. Hundred pregnant women in 3rd
[1] About 12% of women, whose pregnancies continue for trimester of pregnancy, diagnosed as oligohydramnios
two weeks beyond expected date of delivery; develop with amniotic fluid index (AFI) less than 5 cm and intact
oligohydramnios due to declining placental function. membranes were included in the study. Findings were
Oligohydramnios accompanies a broad range of analyzed with the special emphasis on bio-social
reproductive disorders including anomalies of fetus and characteristics of the patient and maternal and perinatal
functional disorders of mother, fetus and placenta. outcome. The ethical committee of the institute had
Decreased amount of amniotic fluid, particularly in third approved the study. Results were analyzed by using
trimester, has been associated with multiple fetal risks percentage and proportion.
like, pulmonary hypoplasia and intrauterine growth
restriction. Oligohydramnios may cause compression of Results:
umbilical cord, leading to fetal distress during labour. It was observed (table 1) that, 78% women with
Oligohydramnios is found to be associated with an oligohydramnios were in the age group of 20-29 years.
increased risk of caesarean delivery for fetal distress, low The mean ( SD) maternal age was 22.8 4.2 years. By
Apgar score and high perinatal morbidity and mortality [2]. gestational age, 22% of women were in the gestational
Hence, the present study was carried out to find out the age group of 34-36 weeks followed by 20% women in 38-
incidence of oligohydramnios during pregnancy and its 40 and >40 weeks. The mean gestational age was 36.7
effect on maternal and perinatal outcome. 4.1 weeks. By parity, 54% women were primigravidas
followed by 46% multigravidas.
Material & Methods:
A retrospective hospital based study was carried out in the It was observed that (table 2), pregnancy induced
department of Obstetrics and Gynaecology of Rural hypertension (16%), postdated pregnancy (16%) and
1 Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 12, Issue 12
Bangal V B et. al. / JPBMS, 2011, 12 (05)
anhydramnios (10%) were commonly seen in women with [5]found that the mean maternal age were 23.6 6.5 years,
oligohydramnios. As regards to mode of delivery, it was 28.4 3.4 years and 23.8 5.7 years respectively.
observed that, 56% had spontaneous vaginal delivery and The mean gestational age in the present study was 36.7
44% had operative/assisted delivery. Birth asphyxia 4.1 weeks. Similar studies by Jun Zhang et. al. [4], Casey B et
(Apgar score of <7 at one minute and five minute) was al .[6] , Everett F et. al. [5] and Iffath A et. al.[ 7] found that, the
more common in the babies delivered in cases of mean gestational age were 38.1 3.3 weeks, 37.5 2
oligohydramnios. Neonatal morbidity was mainly due to weeks, 34.3 2.1 weeks, and (mean SD) was 36.3 2
meconium aspiration and neonatal sepsis. High perinatal weeks respectively. These findings indicate that the
mortality (24%) was observed in the present study. problem of oligohydramnios was more common in the
later part of pregnancy. It is mainly due to physiological or
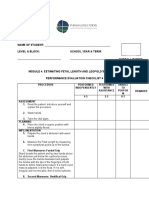
Bio-social characteristics Oligohydramnios women pathological causes of reduced placental perfusion near
(n=100) term.
1. Maternal age
<20 yrs 16 In the present study, the incidence of oligohydramnios
20 - 29 yrs 78 was 0.67%. Similar study by Jun Zhang et. al. [4] reported
30 yrs 06 the incidence as 1.5%. Divon M et. al. [8] found
Mean SD 22.88 yrs 4.24 yrs oligohydramnios in 1.2% in their cases. Casey B et al.6
2. Gestational age
30-32 weeks 08
found that 2.3% cases were complicated by
32-34 weeks 14 oligohydramnios. Elliot H et. al. [9] found that, the incidence
34-36 weeks 22 of oligohydramnios was 3.9% in their study. Varma T R et.
36-38 weeks 16 al. [10] found that, the incidence was 3.1% in their study.
38-40 weeks 20
>40 weeks 20
Chauhan P et. al. [19] studied two groups of patients. First
Mean SD 36.72 weeks 4.11 weeks group had AFI less than 5cm and second with AFI less than
3. By Amniotic Fluid Index 5th percentile for that gestational age. The mean amniotic
0 10 fluid index was 3.9 2.1 cm (AFI less than 5th percentile)
1 06 and 3 1.5 cm in patients with AFI less than 5cm.
2 28
3 06 The mean amniotic fluid index (AFI) in the present study
4 30 was 3.00 1.04cm. Sadovsky Y et. al. [20] in their study,
5 20 found that the mean amniotic fluid index was 2.9 cm.
Mean SD 3.00 1.04 Obstetrical complications frequently associated with
4. By birth weight oligohydramnios were pregnancy induced
<1000 gms 02 hypertension(PIH), postdatism, intrauterine growth
1000-2000 gms 38 restriction, fetal renal anomalies, prematurity and
2000-3000 gms 58
>3000 gms 02 intrauterine death of the fetus. In the present study 78%
Mean SD 2140.00 gms 0.51 gms cases had associated obstetrical complications; acting
5. Parity singly or in combination for causing oligohydramnios. PIH
Primigravidas 54 was present in 16% cases. Golan A et al.12 in his study,
Multigravidas 46
Mean SD 1.2 1.5
found maternal hypertension in 22.1% cases. Cesarean
(Data indicates both number and percentage) section was performed in 35.25% of these cases. Mercer L
J et. al. [13] found that preeclampsia was present in 24.7%
Table 2: Maternal and perinatal outcome in of cases with decreased fluid. Study by Chauhan P et. al. [3]
oligohydramnios (n=100) reported, preeclampsia in 12% cases. They concluded that
Variables No. of cases the incidence of oligohydramnios ranges from 10 to 30 %
1. Maternal complications in hypertensive patients requiring hospitalization. Sixteen
Pregnancy induced hypertension 16
percent cases had postdated pregnancies in the present
Postdate 16
Intrauterine growth restriction 14 study. Clement D et. al. [21] studied six cases of postdatism,
Preterm delivery 14 in which amniotic fluid volume diminished abruptly over
Anhydramnios 10 24 hours. Bowen Chattoor JS et. al. [22], in their study
Fetal anamolies 08
evaluated the relationship between amniotic fluid index
2. Mode of delivery
Spontaneous vaginal delivery 56 and perinatal outcomes in fifty five postdate pregnancies.
Operative/assisted delivery 44 Oligohydramnios was noted in four (7.2%) cases. In the
3 Neonatal morbidity present study, intra uterine growth restriction was
Meconium aspiration 04 present in 20% cases and the rate of caesarean section
Neonatal sepsis 04
was 44% and that of vaginal delivery was 56%. Study by
4. Apgar score (< 7)
At 1 minute 10 Casey B et. al. [6] found that, there was increased rate of
At 5 minute 16 induction of labour (42%) and Cesarean section (32%) in
5. Perinatal mortality oligohydramnios cases. Jun Zhang et al.4 found that, the
Still births 08 overall cesarean delivery rates were similar between
Early neonatal death 16
women with oligohydramnios and the controls (24% Vs
(Data indicates both number and percentage) 19%). Golan A et. al. [12] et al found that, the cesarean
section was performed in 35.2% of pregnancies. In the
Discussion:
present study, the apgar score was noted at 1 and 5
In the present study, 78% of cases were in the age group minutes after birth. Sixteen babies (16%) had low Apgar
20 to 29 years, as compared to other age groups, reflecting score (less than 7 at 5 min). Out of 16 babies with low
the child bearing age of most of the women with the mean Apgar score, eight died during neonatal period. Three
(SD) maternal age of 22.8 4.2 years. Similar studies by babies with low Apgar score were delivered by caesarian
Chauhan P et. al. [3], Jun Zhang et. al. [4] and Everett F et. al.
2 Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 12, Issue 12
Bangal V B et. al. / JPBMS, 2011, 12 (05)
section. Out of these 3 babies, one died during neonatal intrapartum fetal distress, meconium aspiration syndrome
period due to non-immune hydrops fetalis. In a similar and birth asphyxia. Adverse perinatal outcome can be
study by Casey B et. al.[6] (6%) babies had Apgar score of avoided by careful intrapartum fetal heart rate
less than 3 at 5 minute. Out of these nine babies, seven monitoring. Every case of oligohydramnios needs careful
died during neonatal period. Jun Zhang et. al. [4] found that antenatal evaluation, parental counseling, individualized
an Apgar score of <7 at 1 minute was present in fifteen Six decision regarding timing and mode of delivery.
babies had Apgar score of <7 at 5 minute. Desai P et. al. [14] Continuous intrapartum fetal monitoring and good
found that three babies with Apgar score less than 7 at 5 neonatal care are necessary for better perinatal outcome.
minute as against only one in control group. In a similar
study by Locatelli A et. al. [15] of 341 patients with Acknowledgement:
oligohydramnios, found no significant difference for Apgar We acknowledge the cooperation extended by
score of less than 7 at 5 minute in study and control group. Management of Pravara Medical Trust and The Principal,
In the present study, four (8%) babies developed Rural Medical College, Loni, Maharashtra, India
meconium aspiration. All four babies were admitted in
NICU for further management. Three babies were References:
delivered by caesarean section and one by vaginal route. 1.Park K. Preventive medicine in obstetric, Paediatrics and
Two babies died in neonatal period. Causes of deaths were geriatrics: Park's Text Book of Preventive and Social
meconium aspiration syndrome and development of Medicine. 20th edition. Jabalpur: M/S Banarasi Das Bhanot;
septicemia. Babies who died due to meconium aspiration 2009; 479-483.
syndrome were of 37.5 weeks and 39.3 weeks of gestation 2.D. C. Dutta: Textbook of Obstetrics, 6th edition 2004:37.
with birth weight of 1.3 kg and 2.5kg respectively. Casey B 3.Chauhan SP, Hendrix NW: Intrapartum oligohydramnios
et. al. [6] studied 6423 patients, who underwent does not predict adverse peripartum outcome among high
ultrasonography at more than 34 weeks gestation and risk parturient. Am J Obstet Gynecol, 1997; 176(6):1130-
found that 147 (2.3%) cases were complicated by 1136.
oligohydramnios. Meconium stained amniotic fluid was 4.Jun Zhang, James Troendle: Isolated oligohydramnios is
identified, less often in pregnancies complicated by not associated with adverse perinatal outcome. Int J
oligohydramnios (6% vs. 15%, P=0.004). Notably; the Gynaecol Obstet Mar 2004;3:220-225.
incidence of meconium aspiration syndrome in infants 5.Everett FM, Thomas EN: Measurement of amniotic fluid
with oligohydramnios was significantly higher despite the volume-Accuracy of ultrasonography technique. Am J
diminished identification of meconium stained amniotic Obstet Gynecol 1992; 167:1533-7.
fluid. 6.Casey Brian M, Donald D McIntire: Pregnancy outcomes
Bowen Chattoor JS et. al. [22] studied perinatal outcome in after antepartum diagnosis of oligohydramnios at or
55 postdate pregnancies. Oligohydramnios was noted in beyond 34 weeks' gestation. Am J Obstet Gynecol, April
four patients. All 4 babies were admitted with meconium 2000; 182(4): 909-912.
aspiration. One died due to this complication. 7.Hoskins IA, Friden FJ: Variable deceleration in reactive
In the present study, there were 92% live births and 8% non stress test with decreased amniotic fluid index
still births. Sixteen percent babies died in neonatal period. predicts fetal compromises. Am J Obstet Gynecol 1991;
The gross perinatal mortality was 24% in present study. 165(4):1094-1098.
Out of 12 perinatal deaths, 11 deaths were seen in 8.Divon MY, Marks, Henderson CE: Longitudinal
unregistered cases. Chhabra S et. al. [16] reported very high measurement of amniotic fluid index in post term
(87.7%) perinatal mortality in their study. Wolff F et. al. pregnancies and its association with fetal outcome. Am J
[17] found that the perinatal mortality in their study was
Obstet Gynecol 1995; 172:142.
7.2%. Apel-Sarid L et. al. [18] found that the perinatal 9.Elliot H. Phillipson, Robert J. Sokol: Oligohydramnios
mortality was 9.9%. Chamberlin PF et. al. [23] calculated the Clinical association and predictive value for intrauterine
gross and corrected perinatal mortality rate in patients growth retardation. Am J Obstet Gynecol 1983; 146:271.
with decreased qualitative amniotic fluid volume and 10.Varma TR, Bateman S: Ultrasound evaluation of
found it to be 188/1000 and 109/1000 respectively. amniotic fluid -outcome of pregnancies with severe
Overall, the perinatal mortality is markedly increased in oligohydramnios. Int J Gynaecol Obstet Oct 1988;
patients with oligohydramnios. The lack of amniotic fluid 27(2):185-92.
allows compression of fetal abdomen, which limits the 11.Corosu R, Moretti S: Clinical considerations on
movement of the diaphragm. oligohydramnios. Minerva Ginecol Jun 1999; 51(6):219-
22.
Conclusion: 12.Golan A, Lin G : Oligohydramnios - maternal
Oligohydramnios is being detected more often these days, complications and fetal outcome in 145 cases. Gynecol
due to routinely performed obstetric ultrasonography. Obstet Invest 1994; 37(2):91-5.
Pregnancy induced hypertension and post dated 13.Mercer Lane, L.G. Brown: A survey of pregnancies
pregnancies are the commonest causes of reduced complicated by decreased amniotic fluid. Am J Obstet
amniotic fluid during third trimester of pregnancy. Gynecol 1984; 149:355-361.
Anomalies of the fetal renal system are responsible for 14.Desai P, Patel P, Gupta A: Decreased amniotic fluid
oligohydramnios in second and third trimester. The time index in low risk pregnancy Any significance? J Obstet
and mode of delivery of these cases depends on severity of Gynecol Int Sep 2004; 54(5): 464:466.
oligohydramnios and status of fetal wellbeing. Caesarean 15.Locatelli A, Vergani P et al: Perinatal outcome
section is mostly required for cases with anhydramnios associated with oligohydramnios in uncomplicated term
and intrapartum fetal heart rate abnormalities. Babies are pregnancies. Arch Gynecol Obstet 2004; 269(2):130-133.
relatively more prone for certain complications, like
3 Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 12, Issue 12
Bangal V B et. al. / JPBMS, 2011, 12 (05)
16.Chhabra S, Dargan R : Oligohydramnios - a potential 20.Sadovsky Y, Christensen MW: Cord containing amniotic
marker for serious obstetric complications. J Obstet fluid pocket-a useful measurement in the management of
Gynecol Oct 2007; 27(7):680-3. oligohydramnios. Obstet Gynecol Nov. 1992; 80 (5):775-7.
17.Wolff F, Schaefer R: Oligohydramnios-perinatal 21.Clement D, Barry MD: Acute oligohydramnios in
complications and diseases in mother and child. postdate pregnancy. Am J Obstet Gynecol 1987; 157:884-
Geburtshilfe Frauenheilkd Mar.1994; 54(3):139-43. 886.
18.Apel-Sarid L, Levy A: Placental pathologies associated 22.Browen-Chatoor JS, Kulkarni SK: Amniotic fluid index
fetal growth restriction; complicated with and without in the management of postdates pregnancy. West Indian
oligohydramnios. Arch Gynecol Obstet Feb 2009. Med J Jun 1995; 44(2):64-6.
19.Chauvan SP, Nancy W. Hendrix: Perinatal outcome and 23.Chamberlin PF, Manning FA et al: Ultrasound
amniotic fluid index in the antepartum and intrapartum evaluation of amniotic fluid volume. The relationship of
periods A meta analysis. Am J Obstet Gynecol 1999; marginal and decreased amniotic fluid volume to perinatal
181:1473. outcome. Am J Obstet Gynecol 1984; 150:245.
Conflict of Interest: - None
Source of funding: - Not declared
*Corresponding Author:-
Dr. Vidyadhar B. Bangal.,
Professor and Head,
Dept. of Obstetrics and Gynaecology (OBGY),
Rural Medical College, Loni, Dist. Ahmednagar,
Maharashtra, India Pin- 413736 Quick response code (QR- Code) for mobile user to
Contact no- (+91) 02422- 273600, 09822096723. Assess JPBMS website electronically.
.
4 Journal of Pharmaceutical and Biomedical Sciences (JPBMS), Vol. 12, Issue 12
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Novel Technique For Management of Bartholin Gland CystsnDocument3 pagesNovel Technique For Management of Bartholin Gland CystsnelenNo ratings yet
- Anomaly Scan ReportDocument26 pagesAnomaly Scan ReportMichael Idowu100% (1)
- (DHEA) Replacement Decreases Insulin Resistance and Lower Inflamatory CytokineDocument10 pages(DHEA) Replacement Decreases Insulin Resistance and Lower Inflamatory CytokineelenNo ratings yet
- A Review Leptin Structure and Mechanism Actions"Document8 pagesA Review Leptin Structure and Mechanism Actions"elenNo ratings yet
- Pid FaqDocument3 pagesPid FaqLili ManaoNo ratings yet
- 03 Bartholin Gland Procedure + Inform ConsentDocument4 pages03 Bartholin Gland Procedure + Inform ConsentelenNo ratings yet
- Adrenal Androgen Excess and Body Mass Index in PCOSDocument9 pagesAdrenal Androgen Excess and Body Mass Index in PCOSelenNo ratings yet
- Gynecology and Minimally Invasive Therapy: Case ReportDocument5 pagesGynecology and Minimally Invasive Therapy: Case ReportelenNo ratings yet
- Bar Tho LinDocument6 pagesBar Tho LinArwin OkwandiNo ratings yet
- Bartholin Cyst or Abscess - Leaflet v3 April 17Document2 pagesBartholin Cyst or Abscess - Leaflet v3 April 17elenNo ratings yet
- Obstetric Anal Sphincter Lacerations.8Document6 pagesObstetric Anal Sphincter Lacerations.8elenNo ratings yet
- Drainage of Bartholin Cyst Abscess ML46071Document4 pagesDrainage of Bartholin Cyst Abscess ML46071elenNo ratings yet
- Distribution of Infertility Factors Among Infertile Couples in YemenDocument4 pagesDistribution of Infertility Factors Among Infertile Couples in YemenelenNo ratings yet
- Drainage of Bartholin Cyst Abscess ML46071Document4 pagesDrainage of Bartholin Cyst Abscess ML46071elenNo ratings yet
- Thyroid Autoimmunity and Female Infertility: Kris Poppe, Daniel Glinoer, Brigitte VelkeniersDocument16 pagesThyroid Autoimmunity and Female Infertility: Kris Poppe, Daniel Glinoer, Brigitte VelkenierselenNo ratings yet
- Clinical Impact of Postsurgical Adhesions1 PDFDocument10 pagesClinical Impact of Postsurgical Adhesions1 PDFTito AlhoNo ratings yet
- Diagnosis and Management of Graves' Disease: Review SynthèseDocument11 pagesDiagnosis and Management of Graves' Disease: Review Synthèsedanil armandNo ratings yet
- Stem Cells Ray of Hope in InfertilityDocument2 pagesStem Cells Ray of Hope in InfertilityelenNo ratings yet
- Causes of Infertility in Women at Reproductive Age PDFDocument8 pagesCauses of Infertility in Women at Reproductive Age PDFelenNo ratings yet
- Diagnostic Value of The Risk of Malignancy Index (RMI) For Detection of Pelvic Malignancies ComparedDocument6 pagesDiagnostic Value of The Risk of Malignancy Index (RMI) For Detection of Pelvic Malignancies ComparedelenNo ratings yet
- Thyroid Autoimmunity and Female Infertility: Kris Poppe, Daniel Glinoer, Brigitte VelkeniersDocument16 pagesThyroid Autoimmunity and Female Infertility: Kris Poppe, Daniel Glinoer, Brigitte VelkenierselenNo ratings yet
- Is There Any in Women Consulting Fertility TXDocument7 pagesIs There Any in Women Consulting Fertility TXelenNo ratings yet
- Comparison of Visual Inspection and Papanicolau (PAP) SmearsDocument8 pagesComparison of Visual Inspection and Papanicolau (PAP) SmearselenNo ratings yet
- Effect of A High-Fat Diet On 24-h Pattern of Circulating LevelsDocument8 pagesEffect of A High-Fat Diet On 24-h Pattern of Circulating LevelselenNo ratings yet
- Cervical CancerDocument60 pagesCervical CancerNova Yuli PrasetyoNo ratings yet
- Alo AjogDocument1 pageAlo AjogelenNo ratings yet
- Amenorrhoea Long Version PDFDocument7 pagesAmenorrhoea Long Version PDFelenNo ratings yet
- Clinical Impact of Postsurgical Adhesions1 PDFDocument10 pagesClinical Impact of Postsurgical Adhesions1 PDFTito AlhoNo ratings yet
- Enteral Nutrition Therapy For The Surgical PatientDocument52 pagesEnteral Nutrition Therapy For The Surgical PatientelenNo ratings yet
- b2 20Document6 pagesb2 20elenNo ratings yet
- Pituitary Tumors BrochureDocument20 pagesPituitary Tumors BrochureAnonymous M6HzvK6bNo ratings yet
- B. Within 24 Hours After DischargeDocument15 pagesB. Within 24 Hours After DischargeRichard SonsingNo ratings yet
- 2024.sifilis CongenitaDocument12 pages2024.sifilis CongenitaWILLIAM ROSALES CLAUDIONo ratings yet
- Antepartum HaemorrhageDocument23 pagesAntepartum HaemorrhageSutanti Lara DewiNo ratings yet
- Patent Ductus Arteriosus: Pathophysiology and Management: Original ArticleDocument10 pagesPatent Ductus Arteriosus: Pathophysiology and Management: Original ArticleYanny LabokNo ratings yet
- Fetal Well BeingDocument23 pagesFetal Well BeingKrishnaveni Murugesh100% (1)
- 2016 Specimen Paper 3 Mark Scheme PDFDocument8 pages2016 Specimen Paper 3 Mark Scheme PDFvickyNo ratings yet
- Midterm Coverage - NCM 108 Health Care Ethics NotesDocument10 pagesMidterm Coverage - NCM 108 Health Care Ethics NotesAudrie Allyson GabalesNo ratings yet
- US LAW Maternal Tort LiabilityDocument33 pagesUS LAW Maternal Tort Liabilityshivamjain391No ratings yet
- (Ronald W. Dudek) High-Yield Embryology 2nd (B-Ok - Xyz) PDFDocument156 pages(Ronald W. Dudek) High-Yield Embryology 2nd (B-Ok - Xyz) PDFSruthi priyavadhanaNo ratings yet
- (Entrance-Exam - Net) - MD Ayurveda All DetailDocument111 pages(Entrance-Exam - Net) - MD Ayurveda All Detailrocky006600No ratings yet
- Part I سنه القمله 2016Document20 pagesPart I سنه القمله 2016Aloah122346No ratings yet
- Paediatric Nursing BooksDocument50 pagesPaediatric Nursing Bookskavisubbu50% (2)
- NCP - Acute PainDocument4 pagesNCP - Acute PainCharmin AlegreNo ratings yet
- 10 General Anatomy of The Cardiovascular SystemDocument140 pages10 General Anatomy of The Cardiovascular SystemSuzana VoiculescuNo ratings yet
- Assessment of Fetal Growth and DevelopmentDocument10 pagesAssessment of Fetal Growth and DevelopmentAira Jane BasuelNo ratings yet
- Cerebral Palsy Practice Essentials: Signs and SymptomsDocument11 pagesCerebral Palsy Practice Essentials: Signs and SymptomsTahsinur RahmanNo ratings yet
- De HomunculoDocument5 pagesDe HomunculoMahaotNo ratings yet
- FG Midwifery II FinalDocument242 pagesFG Midwifery II Finalfakii muhusiniNo ratings yet
- Abortion and Organ Donation-Patricia Beattie JungDocument34 pagesAbortion and Organ Donation-Patricia Beattie JungSinjini Mukherjee100% (1)
- Iugr Presentation DefrieceDocument16 pagesIugr Presentation Defrieceapi-536242704No ratings yet
- INTRODUCTIONDocument3 pagesINTRODUCTIONSoumya Suguna TripathyNo ratings yet
- Jordie-Prenatal Care StudygramDocument7 pagesJordie-Prenatal Care StudygramNoreen Hannah GabrielNo ratings yet
- CV MDG Progress Report As of 032707 - FinalDocument58 pagesCV MDG Progress Report As of 032707 - FinalStella AcuinNo ratings yet
- Pregnancy Toxemia PaperDocument4 pagesPregnancy Toxemia Paperbmc5321No ratings yet
- NleDocument12 pagesNleJohn Haider Colorado Gamol50% (2)
- Antepartum Fetal Surveillance - ACOG - 2019Document8 pagesAntepartum Fetal Surveillance - ACOG - 2019Gabriel R Muñoz MNo ratings yet
- Leopold's Manuever ChecklistDocument3 pagesLeopold's Manuever ChecklistMelchizeder Solis LumanogNo ratings yet
- Pregnancy Induced Hypertension PathophysiologyDocument2 pagesPregnancy Induced Hypertension PathophysiologyCamille Grace100% (1)
- ObstetricsDocument55 pagesObstetricsKristine Alejandro100% (1)