Professional Documents
Culture Documents
Maternal Asthma Management Strategies
Uploaded by
Roberto López MataCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Maternal Asthma Management Strategies
Uploaded by
Roberto López MataCopyright:
Available Formats
REVIEW
SUCHARITA KHER, MD, FCCP PRERNA MOTA, MD
Assistant Professor of Medicine, Pulmonary and Critical Care Medicine,
Tufts University School of Medicine; Medical Lawrence General Hospital, Lawrence, MA
Director, Pulmonary Clinic, Division of Pulmonary,
Critical Care, and Sleep Medicine, Tufts Medical
Center, Boston, MA
Maternal asthma:
Management strategies
ABSTRACT
Asthma in pregnancy is common, and its prevalence is
T he incidence of maternal asthma is ris-
ing. Based on US national health surveys,
the prevalence of asthma during pregnancy is
rising. Internists need to be aware of the effects of mater- between 3.7% and 8.4%.1 It is the most com-
nal asthma control on the health of the expectant mother mon respiratory illness of pregnancy.2 Hence,
and the baby. With the ever-present worry about medica- clinicians need to know how asthma affects
tion use and teratogenicity in pregnant women, these pa- the mother and the fetus. Appropriate care of
tients are often undertreated for their asthma. This review asthma during pregnancy is based on several
focuses on effects of uncontrolled maternal asthma as management principles, as reviewed here, and
well as appropriate management of maternal asthma in is key to ensuring good outcomes for the moth-
the outpatient setting and during exacerbations. er and the baby.
KEY POINTS EFFECT OF PREGNANCY
ON ASTHMA CONTROL
The benefits of good adherence to asthma regimens
during pregnancy outweigh the risks associated with the Asthma control can vary in pregnancy. About
a third of asthmatic women experience a
medications used.
worsening of asthma control with pregnancy,
a third remain unchanged, and another third
For treatment of reflux disease in pregnant women with have improvement in asthma symptoms.3 The
asthma, antacids (but not sodium bicarbonate, for fear of peak worsening of asthma tends to occur in
metabolic alkalosis) and sucralfate should be considered the sixth month.4 Asthma control also tends
before a histamine 2 receptor antagonist such as raniti- to be better in the last month of pregnancy.3
dine. Proton pump inhibitors should be considered only if The peak expiratory flow rate was noted to
reflux symptoms are refractory to other therapies. increase with each trimester in a small study of
43 women.5 The authors speculated that a ris-
ing progesterone level stimulates cyclic adenos-
Uncontrolled maternal asthma contributes to poor ma-
ine monophosphate to cause bronchodilation,
ternal and fetal outcomes. Management by a multidisci- thereby improving the expiratory flow rate and
plinary team, including internist, obstetrician, pharmacist, asthma control. Asthma control tends to follow
nurse, allergist, and pulmonologist, improves care and the pattern experienced in the previous preg-
outcomes. nancy: ie, if asthma worsened during the previ-
ous pregnancy, the same will be likely in the
subsequent pregnancy.3
Two maternal factors that adversely affect
asthma severity during pregnancy are the
use of asthma medications contrary to guide-
lines such as those of the Global Initiative
for Asthma (http://ginasthma.org/2017-gina-
doi:10.3949/ccjm.84a.15046 report-global-strategy-for-asthma-manage-
296 CLEV ELA N D C LI N I C JOURNAL OF MEDICINE VOL UME 84 N UM BE R 4 AP RI L 2017
KHER AND MOTA
ment-and-prevention) and inadquate con- TABLE 1
trol of asthma before becoming pregnant.6
Pregnancy can bring on stress, and stress is Uncontrolled asthma in pregnancy:
known to worsen asthma. In addition, when Effects on mother and fetus
patients themselves were interviewed to
elucidate the reasons for poor adherence to Maternal effects
Preeclampsia
asthma medications during pregnancy, con- Pregnancy-induced hypertension
cerns about medication use, especially cor- Gestational diabetes
ticosteroids, stood out.7 A study based on Premature rupture of membranes
prescription claims data showed that in the Cesarean birth
first trimester, there was a significant decline Chorioamnionitis
in asthma prescription medications (a 23% Hyperemesis
decline in inhaled corticosteroids, a 13% de- Postpartum hemorrhage
cline in short-acting bronchodilator agents, Fetal effects
and a 54% decline in rescue corticosteroids).8 Perinatal death
Lack of physician education about manage- Preterm birth
ment of asthma in pregnancy and discomfort Low birth weight
with prescribing to pregnant women also af- Intrauterine growth restriction
fect asthma control. Congenital malformations
Admission to neonatal intensive care unit
Hyperbilirubinemia
EFFECT OF ASTHMA ON MATERNAL Respiratory distress syndrome
AND FETAL OUTCOMES Transient tachypnea of the newborn
Studies of the effects of asthma on fetal and Asphyxia
maternal outcomes have yielded mixed and Increased risk of intracerebral hemorrhage, anemia
conflicting results.9 Adverse outcomes that Based in part on information in reference 9.
have been shown to be associated with ma-
ternal asthma are listed in Table 1. Other Benefits
studies have not demonstrated an association pregnancy outweigh the risks associated with of adherence
between asthma in pregnancy and maternal frequent symptoms and exacerbations caused
or fetal adverse events.9 Such discrepant find- by untreated asthma.12 to asthma
ings are due to differences in study population regimens
characteristics that make comparisons dif- OUTPATIENT MANAGEMENT
ficult. A meta-analysis involving more than during
OF MATERNAL ASTHMA
1.6 million asthmatic women showed mater- pregnancy
nal asthma was associated with a 40% greater Goals
risk of low birth weight and preterm delivery, In the 2004 update of the National Asthma outweigh
a 50% greater risk of preeclampsia, and a 20% Education and Prevention Program (NAEPP) the risks of
greater risk of the baby being small for its ges- Working Group Report on Managing Asthma drug treatment
tational age.10 During Pregnancy, goals focused mainly on
The association of maternal asthma and adequate asthma control for maternal health
preterm birth may pose short-term and long- and quality of life, as well as normal fetal mat-
term health risks to the child associated with uration (Table 2),12 goals similar to those in
prematurity.9 Short-term risks with prema- nonpregnant asthmatic women.
turity include infection, respiratory distress
syndrome, brain injury, and necrotizing en- Assessment and monitoring
terocolitis. Long-term risks include neuro Monthly physician visits during pregnancy are
developmental and behavioral sequelae. recommended for assessment of symptoms and
Furthermore, asthma exacerbations during pulmonary function. If symptoms are uncon-
pregnancy are associated with a twofold high- trolled, therapy must be stepped up, and any
er risk of low birth weight.11 The benefits of trigger for exacerbation, such as gastroesopha-
good adherence to asthma regimens during geal reflux disease (GERD), exposure, or rhi-
CL EVELAND CL I NI C J O URNAL O F M E DI CI NE V O L UM E 84 NUM BE R 4 AP RI L 2017 297
MATERNAL ASTHMA
TABLE 2 as elevating the head of bed, avoiding eating
too close to bedtime, and avoiding foods that
A definition of asthma control cause heartburn may be adequate.15,16 If medi-
cations are needed, antacids (but not sodium
Minimal or no chronic symptoms day or night
bicarbonate, for fear of metabolic alkalosis)
Minimal or no exacerbations and sucralfate should be considered before us-
ing a histamine 2 receptor antagonist such as
No limitation on activities ranitidine. Proton pump inhibitors should be
Maintenance of normal or near-normal pulmonary considered only if reflux symptoms are refrac-
function tory to other therapies.
Minimal use of short-acting beta-agonists Allergic rhinitis
Minimal or no adverse effects from medications Intranasal corticosteroids are effective against
allergic rhinitis in pregnancy (Table 3).12
Based on information in reference 12. Montelukast, a leukotriene receptor antago-
nist, can be used, but data to support its use
nitis, must be treated and eliminated. NAEPP for allergic rhinitis in pregnancy are limited.
Among antihistamines, second-generation
guidelines recommend baseline spirometry at
drugs such as cetirizine or loratadine can be
the time of initial assessment.12 At follow-up
considered.12 Oral decongestants such as pseu-
visits, spirometry is preferred, but measure-
doephedrine in early pregnancy are associated
ment of the peak expiratory flow rate usually
with a rare congenital fetal abnormality called
suffices. Such objective data can help differen-
gastroschisis, caused by vascular disruption.17
tiate dyspnea from asthma and from dyspnea Hence, if a nasal decongestant is required in
that usually accompanies the physiologic early pregnancy, a local therapy such as an in-
changes of pregnancy. In addition, patients tranasal corticosteroid, short-term oxymetazo-
should be advised to monitor for adequate fe- line, or an external nasal dilator may be consid-
tal activity. If asthma is uncontrolled or poorly ered.12 These therapies must be combined with
Avoiding controlled, serial fetal ultrasonography should avoidance of allergens whenever possible.
asthma be considered from 32 weeks of gestation, as
well as after recovery from an asthma exacer- Allergies
triggers
bation. Regular monitoring of the pregnant Diagnostic allergy and skin tests during preg-
eg, dander, asthmatic patient by a multidisciplinary team nancy pose a risk of anaphylaxis and thus
dust mites, can improve outcomes.13 should be avoided. Instead, the focus should
be on obtaining a thorough medical history
smoke Avoiding triggers about exposures and eliminating specific asth-
can decrease Patients should be advised to avoid asthma ma triggers. It is also inadvisable to start al-
triggers such as pet dander, dust mites, pol- lergen immunotherapy during pregnancy be-
symptoms len, smoke, mold, and perfumes, as this can cause of the risk of anaphylaxis and the effect
and allow decrease symptoms and allow for use of lower of treatment on the mother and fetus.18 How-
for lower doses doses of medications.12 Additionally, smoking ever, maintenance doses of allergen immuno-
cessation must be strongly encouraged, not therapy can be continued during pregnancy.18
of medications only to control maternal asthma, but also to
prevent harm to the fetus. Patient education
Because of concern about the risks of taking
MANAGEMENT OF SPECIFIC TRIGGERS medications during pregnancy, many women
with asthma stop using their inhalers during
GERD pregnancy, thus compromising asthma con-
Reflux disease often worsens during pregnancy, trol.8,13 The physician and multidisciplinary
and it can coexist with asthma and can also ex- team must use every opportunity to empha-
acerbate it.14 Optimal control of GERD helps size the importance of good asthma control
maintain adequate asthma control. For mild during pregnancy. Inhaler technique should
reflux symptoms, lifestyle modifications such also be reviewed and, if defective, corrected.
298 CLEV ELA N D C LI N I C JOURNAL OF MEDICINE VOL UME 84 N UM BE R 4 AP RI L 2017
KHER AND MOTA
Again, trigger avoidance and tobacco cessa- TABLE 3
tion should be addressed.
Drug therapy of maternal asthma:
Drugs Former pregnancy risk categories
The NAEPP recommendations state that
asthma therapy should be continued during Drug Categorya
pregnancy, as it is safer both for mother and Short-acting beta-agonist
fetus to avoid exacerbations and uncontrolled Albuterol C
asthma.12 Despite this, 25% of primary care
physicians instruct their patients to decrease Long-acting beta-agonists
Formoterol C
or discontinue their inhaled corticosteroid
Salmeterol C
during pregnancy.19 As with asthma in gener-
al, treatment should involve using the lowest Inhaled corticosteroids
dose of drugs that achieves adequate control Budesonide (inhalation) B
of symptoms. Fluticasone (inhalation) C
In 2015, the US Food and Drug Admin- Leukotriene modifiers
istration (FDA) amended the labeling rule Montelukast, zafirlukast B
for medications used in pregnancy and lacta- Zileuton C
tion. The previous risk categories A (safest), Monoclonal antibody
B, C, D, and X (highest risk) are in the pro- Omalizumab B
cess of being removed from labels for all hu-
Xanthine derivative
man prescription drugs and biologic products, Theophylline C
to be replaced with a summary of the risks of
taking the drug during pregnancy and lacta- Intranasal corticosteroids
tion, a discussion of the data supporting the Intranasal budesonide B
Intranasal fluticasone C
use, and relevant information to help health-
Intranasal mometasone C
care providers make prescribing decisions and Intranasal triamcinolone C
counsel women about the use of drugs during Based on a
pregnancy and lactation (www.fda.gov/Drugs/ a
Former US Food and Drug Administration risk category systematic
DevelopmentApprovalProcess/Developmen- (see Drugs, this page).
tResources/Labeling/ucm093307.htm). review, 20%
Inhaled beta-agonists of pregnant
ROLES OF CONTROLLER THERAPY
Inhaled beta-agonists, both short-acting and women with
AND RESCUE THERAPY
long-acting, are used for rescue therapy. Al
buterol is the preferred short-acting agent for
asthma require
Inhaled corticosteroids
Inhaled corticosteroids are the mainstay of rescue therapy in pregnant women with asth- an intervention
asthma controller therapy during pregnancy. ma.12 Meta-analysis has shown no increased for an exacer-
A meta-analysis of 16 studies showed no in- risk of major or minor congenital malforma-
creased risk of congenital malformations, ce- tions in pregnant patients who use broncho- bation during
sarean delivery, or stillbirth among mothers dilators.20 Long-acting beta-agonists typically pregnancy
who used these agents during pregnancy.20 Be- are used as add-on therapy when asthma can-
cause there are more safety data for budesonide, not be controlled by an inhaled corticosteroid.
it is currently the preferred inhaled corticoste- They should not be used without a controller
roid during pregnancy.9 However, if a patients medication (ie, an inhaled corticosteroid).
asthma is controlled with a different cortico- Guidelines for rescue therapy are similar to
steroid before pregnancy, that agent may be those for nonpregnant asthmatic patients. Al-
continued during pregnancy, especially if it is though data are limited as to the gestational ef-
thought that switching formulations could ad- fects of long-acting beta-agonists (ie, formoterol,
versely affect asthma control.12 This is mainly salmeterol), it can be assumed that the toxico-
because current data do not prove that other logic and pharmacologic profiles are similar to
inhaled corticosteroids are unsafe. those of the short-acting bronchodilators. Thus,
CL EVELAND CL I NI C J O URNAL O F M E DI CI NE V O L UM E 84 NUM BE R 4 AP RI L 2017 299
MATERNAL ASTHMA
TABLE 4 steroids (Table 3). An analysis of the omali-
zumab pregnancy registry25 found no signifi-
Management of asthma cant increase in the rate of major congenital
exacerbations in pregnancy malformations, prematurity, or babies small
for gestational age in asthmatic women taking
Monitor to ensure the maternal oxygen saturation omalizumab 8 weeks before conception or dur-
remains above 95%
ing pregnancy vs pregnant asthmatic women
Consider systemic (oral) corticosteroids not taking omalizumab. However, this drug
Administer rescue therapy with a short-acting carries a risk of anaphylaxis and so should not
beta-agonist be started during pregnancy.25
Consider hospital admission if symptoms Theophylline
do not improve with emergency room care Because of potential toxicity, use of the-
onsider admission to intensive care unit
C ophylline during pregnancy requires careful
and mechanical ventilation if symptoms are severe monitoring to ensure the serum concentra-
or if patient shows signs of impending respiratory tion remains between 5 and 12 g/mL.12 Drug
failure interactions are also common: for example,
Carefully monitor fetal health
alcohol may increase the serum concentra-
tion of theophylline, and theophylline may
increase the toxic effect of formoterol.
the safety of albuterol can be extended poten- Systemic corticosteroids
tially to the long-acting beta-agonists.12 Pregnant women with asthma that is not well
Combining controller and rescue therapy controlled despite the therapies described
When asthma is not adequately controlled on above may require a daily oral corticosteroid
inhaled corticosteroids, a long-acting beta- such as prednisone to achieve adequate con-
agonist can be added or the dose of cortico- trol. Oral steroids are also a mainstay of treat-
steroid can be increased. The 2004 NAEPP ment of asthma exacerbation.
Exacerbations Although use of corticosteroids in the first
guidelines stated that based on available liter-
are more ature, there was no clear advantage of one op- trimester was associated with orofacial cleft in
common late tion over the other.12 A study that compared infants,12 these studies did not include many
the 2 approaches found no difference in rates women with asthma. In 2011, a nationwide
in the second of congenital malformations.21 cohort study from Denmark showed no in-
trimester crease in the risk of orofacial cleft with the use
Leukotriene receptor antagonists of corticosteroids during pregnancy.26
and are unlikely There is little in the literature regarding the Preeclampsia, low birth weight, and pre-
to occur use of leukotriene receptor antagonists during term delivery have been described with cor-
pregnancy. However, animal safety data are re- ticosteroid use in pregnancy. It is not known
during labor assuring,12 and human studies have not found whether these problems were a result of corti-
or delivery a higher risk of major congenital malforma- costeroid use or were due to the uncontrolled
tions.22,23 Thus, they are an alternative for pa- nature of the underlying condition that led to
tients whose asthma has been well controlled the steroid use. Since the risk of uncontrolled
on these agents before pregnancy. Montelu- asthma to mother and fetus outweighs the risk
kast and zafirlukast are in former FDA preg- of systemic corticosteroids, these drugs are rec-
nancy risk factor category B (probably safe) ommended when indicated for management
(Table 3). However, 5-lipoxygenase inhibitors of maternal asthma.12
such as zileuton are contraindicated based on
animal studies showing teratogenicity.24 ACUTE EXACERBATIONS REQUIRE
Omalizumab AGGRESSIVE MANAGEMENT
Omalizumab, a recombinant anti-immuno- Based on a systematic review, 20% of pregnant
globulin E antibody, can be used for allergic women with asthma require some intervention
asthma not controlled with inhaled cortico- for an asthma exacerbation during pregnancy,
300 CLEV ELA N D C LI N I C JOURNAL OF MEDICINE VOL UME 84 N UM BE R 4 AP RI L 2017
KHER AND MOTA
and 5.8% are admitted to the hospital for an nant patient include a partial pressure of arterial
exacerbation.11 Exacerbations were associated oxygen less than 70 mm Hg or a partial pressure
with a higher risk of low birth weight com- of carbon dioxide greater than 35 mm Hg.
pared with rates in women without asthma. In a multicenter study comparing nonpreg-
Exacerbations are more common late in the nant and pregnant women visiting the emergen-
second trimester and are unlikely to occur dur- cy room for asthma exacerbations,28 pregnant
ing labor and delivery.2 The incidence of exac- women were less likely to be prescribed systemic
erbations increases with the severity of asthma, corticosteroids either in the emergency room or
from 8% in mild asthma, to 47% in moderate at the time of hospital discharge, and they were
asthma, to 65% in severe asthma.27 Risk factors also more likely to describe an ongoing exacer-
for exacerbations include poor prenatal care, bation at 2-week follow-up. However, a recent
obesity, and lack of appropriate treatment with study showed a significant increase in systemic
inhaled corticosteroids.2 The main triggers are corticosteroid treatment in the emergency room
viral respiratory infections and noncompliance (51% to 78% across the time periods, odds ra-
with inhaled corticosteroid therapy.11 tio 3.11, 95% confidence interval 1.277.60,
Asthma exacerbations during pregnancy P = .01). There was also an increase in steroid
should be managed aggressively (Table 4),12 as treatment at discharge (42% to 63%, odds ratio
the risk to the fetus of hypoxia far outweighs 2.49, 95% confidence interval 0.976.37, P =
any risk from asthma medications. Close col- .054), though the increase was not statistically
laboration between the primary care physician significant.29 Although emergency room care for
and the obstetrician allows closer monitoring pregnant asthmatic women has improved, this
of mother and fetus. group concluded that further improvement is
The goal oxygen saturation must be above still warranted, as 1 in 3 women is discharged
95%.12 Signs of acute respiratory failure in a preg- without corticosteroid treatment.
REFERENCES update. J Allergy Clin Immunol 2005; 115:3446.
1. Kwon HL, Belanger K, Bracken MB. Asthma prevalence among preg- 13. Lim AS, Stewart K, Abramson MJ, Walker SP, Smith CL, George J.
nant and childbearing-aged women in the United States: estimates Multidisciplinary Approach to Management of Maternal Asthma
from national health surveys. Ann Epidemiol 2003; 13:317324. (MAMMA): a randomized controlled trial. Chest 2014; 145:1046
2. Powell H, Murphy VE, Taylor DR, et al. Management of asthma in 1054.
pregnancy guided by measurement of fraction of exhaled nitric 14. Harding SM. Gastroesophageal reflux: a potential asthma trigger.
oxide: a double-blind, randomised controlled trial. Lancet 2011; Immunol Allergy Clin North Am 2005; 25:131148.
378:983990. 15. Ahmad S, Mokaddas E. Recent advances in the diagnosis and
3. Schatz M, Harden K, Forsythe A, et al. The course of asthma during treatment of multidrug-resistant tuberculosis. Respir Med 2009;
pregnancy, post partum, and with successive pregnancies: a prospec- 103:17771790.
tive analysis. J Allergy Clin Immunol 1988; 81:509517. 16. van der Woude CJ, Metselaar HJ, Danese S. Management of gastro-
4. Gluck JC, Gluck PA. The effect of pregnancy on the course of intestinal and liver diseases during pregnancy. Gut 2014; 63:1014
asthma. Immunol Allergy Clin North Am 2006; 26:6380. 1023.
5. Beckmann CA. Peak flow values by gestation in women with 17. Werler MM. Teratogen update: pseudoephedrine. Birth Defects Res
asthma. Clin Nurs Res 2008; 17:174181. A Clin Mol Teratol 2006; 76:445452.
6. Belanger K, Hellenbrand ME, Holford TR, Bracken M. Effect of preg- 18. Cox L, Nelson H, Lockey R, et al. Allergen immunotherapy: aprac-
nancy on maternal asthma symptoms and medication use. Obstet tice parameter third update. J Allergy Clin Immunol 2011; 127(suppl
Gynecol 2010; 115:559567. 1):S1S55.
7. Lim AS, Stewart K, Abramson MJ, Ryan K, George J. Asthma during 19. Lim AS, Stewart K, Abramson MJ, George J. Management of asthma
pregnancy: the experiences, concerns and views of pregnant women in pregnant women by general practitioners: a cross sectional sur-
with asthma. J Asthma 2012; 49:474479. vey. BMC Fam Pract 2011; 12:121.
8. Enriquez R, Wu P, Griffin MR, et al. Cessation of asthma medication 20. Murphy VE, Wang G, Namazy JA, et al. The risk of congenital mal-
in early pregnancy. Am J Obstet Gynecol 2006; 195:149153. formations, perinatal mortality and neonatal hospitalisation among
9. Bain E, Pierides KL, Clifton VL, et al. Interventions for manag- pregnant women with asthma: a systematic review and meta-analy-
ing asthma in pregnancy. Cochrane Database Syst Rev 2014; sis. BJOG 2013; 120:812822.
10:CD010660. 21. Eltonsy S, Forget A, Beauchesne MF, Blais L. Risk of congenital
10. Murphy VE, Namazy JA, Powell H, et al. A meta-analysis of adverse malformations for asthmatic pregnant women using a long-acting
perinatal outcomes in women with asthma. BJOG 2011; 118:1314 beta2-agonist and inhaled corticosteroid combination versus higher-
1323. dose inhaled corticosteroid monotherapy. J Allergy Clin Immunol
11. Murphy VE, Clifton VL, Gibson PG. Asthma exacerbations during 2015; 135:123130.
pregnancy: incidence and association with adverse pregnancy out- 22. Nelsen LM, Shields KE, Cunningham ML, et al. Congenital malfor-
comes. Thorax 2006; 61:169176. mations among infants born to women receiving montelukast,
12. National Heart, Lung, and Blood Institute; National Asthma Educa- inhaled corticosteroids, and other asthma medications. J Allergy Clin
tion and Prevention Program Asthma and Pregnancy Working Immunol 2012; 129:251254.e1e6.
Group. NAEPP expert panel report. Managing asthma during 23. Sarkar M, Koren G, Kalra S, et al. Montelukast use during preg-
pregnancy: recommendations for pharmacologic treatment2004 nancy: a multicentre, prospective, comparative study of infant
CL EVELAND CL I NI C J O URNAL O F M E DI CI NE V O L UM E 84 NUM BE R 4 AP RI L 2017 301
MATERNAL ASTHMA
outcomes. Eur J Clin Pharmacol 2009; 65:12591264. 28. Cydulka RK, Emerman CL, Schreiber D, Molander KH, Woodruff PG,
24. Namazy JA, Schatz M. The safety of asthma medications during Camargo CA Jr. Acute asthma among pregnant women presenting
pregnancy: an update for clinicians. Ther Adv Respir Dis 2014; to the emergency department. Am J Respir Crit Care Med 1999;
8:103110. 160:887892.
25. Namazy J, Cabana MD, Scheuerle AE, et al. The Xolair Pregnancy 29. Hasegawa K, Cydulka RK, Sullivan AF, et al. Improved management
Registry (EXPECT): the safety of omalizumab use during pregnancy. of acute asthma among pregnant women presenting to the ED.
J Allergy Clin Immunol 2015; 135:407412. Chest 2015; 147:406414.
26. Hviid A, Molgaard-Nielsen D. Corticosteroid use during pregnancy
and risk of orofacial clefts. CMAJ 2011; 183:796804. ADDRESS: Sucharita Kher, MD, FCCP, Division of Pulmonary, Critical Care,
27. Murphy VE, Gibson P, Talbot PI, Clifton VL. Severe asthma exacerba- and Sleep Medicine, Tufts Medical Center, 800 Washington Street, Box
tions during pregnancy. Obstet Gynecol 2005; 106:10461054. 369, Boston, MA 02111; skher@tuftsmedicalcenter.org
CME CALENDAR
CME
CREDIT
2017 JUNE 18TH ANNUAL INTENSIVE REVIEW
OF CARDIOLOGY
29TH ANNUAL INTENSIVE REVIEW August 1923
MAY Cleveland, OH
OF INTERNAL MEDICINE
June 49
CHALLENGING CONCEPTS CONTROVERSIES IN ENDOMETRIOSIS,
Cleveland, OH
IN ELECTROPHYSIOLOGY AND PACING ADENOMYOSIS, AND FIBROIDS
May 9 August 2526
Chicago, IL PERIOPERATIVE CARDIOTHORACIC
Cleveland, OH
ULTRASOUND COURSE
June 1011
LEARN TO DIAGNOSE MALNUTRITION
Cleveland, OH SEPTEMBER
May 9
Cleveland, OH
DEMENTIA 2017: INTENSIVE REVIEW FOR THE GI BOARDS
THE BRAIN UNDER ASSAULT September 811
LEAD MANAGEMENT 2017: Las Vegas, NV
June 10
A CASE-BASED APPROACH
Las Vegas, NV
May 10 FUNDAMENTAL TO ADVANCED
Chicago, IL
MELLEN CENTER UPDATE ECHOCARDIOGRAPHY
IN MULTIPLE SCLEROSIS September 1517
CARDIAC RESYNCHRONIZATION Cleveland, OH
June 16
THERAPY 2017 Cleveland, OH
May 11 2ND ANNUAL HEART RHYTHM CARE
Chicago, IL
8TH ANNUAL INTERNAL MEDICINE IN THE 21ST CENTURY
BOARD REVIEW September 2223
CLEVELAND BREAST CANCER Cleveland, OH
June 2125
SYMPOSIUM 2017 Sunrise, FL
May 1112 CLEVELAND CLINIC EPILEPSY UPDATE
Cleveland, OH
JULY AND REVIEW COURSE
September 2325
22ND ANNUAL DIABETES DAY Cleveland, OH
May 12 CLEVELAND SPINE REVIEW:
Cleveland, OH HANDS-ON 2017
July 1118 12TH ANNUAL OBESITY SUMMIT
Cleveland, OH September 2829
THE 2017 CLEVELAND CLINIC Cleveland, OH, and Biloxi, MS
PARATHYROID AND THYROID
AUGUST
CONFERENCE OCTOBER
May 13
Cleveland, OH 2017 NEUROLOGY UPDATE:
A COMPREHENSIVE REVIEW PULMONARY HYPERTENSION SUMMIT
FOR THE CLINICIAN 2017
ULTRASOUND: October 67
FROM BASICS TO BEDSIDE August 46
Washington, DC Cleveland, OH, and Fort Lauderdale, FL
DIAGNOSIS AND PROCEDURES
May 1920
Cleveland, OH
FOR FULL UP-TO-DATE SCHEDULE AND TO REGISTER, VISIT WWW.CCFCME.ORG
302 CLEV ELA N D C LI N I C JOURNAL OF MEDICINE VOL UME 84 N UM BE R 4 AP RI L 2017
You might also like
- Hyperglycemic CrisisDocument9 pagesHyperglycemic CrisisRoberto López MataNo ratings yet
- Hepatitis B Vaccination, Screening, and Linkage To Care - Best Practice Advice From The American College of Physicians and The Centers For Disease Control and PreventionDocument12 pagesHepatitis B Vaccination, Screening, and Linkage To Care - Best Practice Advice From The American College of Physicians and The Centers For Disease Control and PreventionRoberto López MataNo ratings yet
- Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of The 2017 American College of Cardiology:American Heart Association Hypertension GuidelineDocument10 pagesPrevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of The 2017 American College of Cardiology:American Heart Association Hypertension GuidelineRoberto López MataNo ratings yet
- 2017 ACC Expert Consensus Decision Pathway For Optimization of Heart Failure TreatmentDocument30 pages2017 ACC Expert Consensus Decision Pathway For Optimization of Heart Failure TreatmentRoberto López MataNo ratings yet
- Atrial Fibrillation and HypertensionDocument17 pagesAtrial Fibrillation and HypertensionRoberto López MataNo ratings yet
- Diagnosis and Treatment of HyperkalemiaDocument9 pagesDiagnosis and Treatment of HyperkalemiaRoberto López MataNo ratings yet
- HTN Emergencies and UrgenciesDocument14 pagesHTN Emergencies and UrgenciesRoberto López MataNo ratings yet
- Top 10 Myths Regarding The Diagnosis and Treatment of CellulitisDocument8 pagesTop 10 Myths Regarding The Diagnosis and Treatment of CellulitisRoberto López MataNo ratings yet
- ADA 2018 Diabetes CareDocument150 pagesADA 2018 Diabetes CareRoberto López Mata100% (1)
- Update On The Management of Venous ThromboembolismDocument8 pagesUpdate On The Management of Venous ThromboembolismRoberto López MataNo ratings yet
- Necrotizing Soft-Tissue InfectionsDocument13 pagesNecrotizing Soft-Tissue InfectionsRoberto López MataNo ratings yet
- Sudden Cardiac Arrest During Participation in Competitive SportsDocument11 pagesSudden Cardiac Arrest During Participation in Competitive SportsRoberto López MataNo ratings yet
- Best Clinical Practice: AnaphylaxisDocument6 pagesBest Clinical Practice: AnaphylaxisputriNo ratings yet
- Uric Acid Is A Strong Risk Marker For Developing Hypertension From PrehypertensionDocument16 pagesUric Acid Is A Strong Risk Marker For Developing Hypertension From PrehypertensionRoberto López MataNo ratings yet
- Fluid Therapy Options and Rational SelectionDocument13 pagesFluid Therapy Options and Rational SelectionRoberto López MataNo ratings yet
- Pathophysiology of Septic ShockDocument19 pagesPathophysiology of Septic ShockRoberto López MataNo ratings yet
- The Role of Nitroglycerin and Other Nitrogen Oxides in Cardiovascular TherapeuticsDocument18 pagesThe Role of Nitroglycerin and Other Nitrogen Oxides in Cardiovascular TherapeuticsRoberto López MataNo ratings yet
- The Use of Cephalosporins in Penicillin-Allergic Patients - A Literature ReviewDocument9 pagesThe Use of Cephalosporins in Penicillin-Allergic Patients - A Literature ReviewRoberto López MataNo ratings yet
- 2015 ESC Guidelines For The Diagnosis and Management of Pericardial DiseasesDocument44 pages2015 ESC Guidelines For The Diagnosis and Management of Pericardial DiseasesRoberto López MataNo ratings yet
- Rivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeDocument10 pagesRivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeRoberto López MataNo ratings yet
- The Dark Sides of Fuid Administration in The Critically Ill PatientDocument3 pagesThe Dark Sides of Fuid Administration in The Critically Ill PatientRoberto López MataNo ratings yet
- Diuretic Treatment in Heart FailureDocument12 pagesDiuretic Treatment in Heart FailureRoberto López Mata100% (1)
- A Test in Context - D-DimerDocument10 pagesA Test in Context - D-DimerRoberto López MataNo ratings yet
- Effects on the Incidence of Cardiovascular Events of the Addition of Pioglitazone Versus Sulfonylureas in Patients With Type 2 Diabetes Inadequately Controlled With Metformin (TOSCA.it)- A Randomised, Multicentre TrialDocument11 pagesEffects on the Incidence of Cardiovascular Events of the Addition of Pioglitazone Versus Sulfonylureas in Patients With Type 2 Diabetes Inadequately Controlled With Metformin (TOSCA.it)- A Randomised, Multicentre TrialRoberto López MataNo ratings yet
- Effects of Acarbose On Cardiovascular and Diabetes Outcomes in Patients With Coronary Heart Disease and Impaired Glucose Tolerance (ACE) - A Randomised, Double-Blind, Placebo-Controlled TrialDocument10 pagesEffects of Acarbose On Cardiovascular and Diabetes Outcomes in Patients With Coronary Heart Disease and Impaired Glucose Tolerance (ACE) - A Randomised, Double-Blind, Placebo-Controlled TrialRoberto López MataNo ratings yet
- Synopsis of The 2017 U.S. Department of Veterans Affairs: Management of Type 2 Diabetes MellitusDocument10 pagesSynopsis of The 2017 U.S. Department of Veterans Affairs: Management of Type 2 Diabetes MellitusRoberto López MataNo ratings yet
- Evaluation and Management of Lower-Extremity UlcersDocument9 pagesEvaluation and Management of Lower-Extremity UlcersRoberto López MataNo ratings yet
- Acute Monocular Vision LossDocument9 pagesAcute Monocular Vision LossRoberto López MataNo ratings yet
- Dual Antithrombotic Therapy With Dabigatran After PCI in Atrial FibrillationDocument12 pagesDual Antithrombotic Therapy With Dabigatran After PCI in Atrial FibrillationRoberto López MataNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- TELFAST 120 MG Film-Coated Tablets: Fexofenadine HydrochlorideDocument2 pagesTELFAST 120 MG Film-Coated Tablets: Fexofenadine HydrochlorideAfsana AfrinNo ratings yet
- Dr. Khairiyadi, M.Kes., Sp.A Departemen Ilmu Kesehatan Anak RSUD Ulin BanjarmasinDocument78 pagesDr. Khairiyadi, M.Kes., Sp.A Departemen Ilmu Kesehatan Anak RSUD Ulin BanjarmasinEldhaNo ratings yet
- 21 May 1Document10 pages21 May 1Trần HuyNo ratings yet
- Free Recipes Download 2012Document18 pagesFree Recipes Download 2012Talia Bradshaw100% (1)
- Allergic Rhinitis PPT-By AllenDocument58 pagesAllergic Rhinitis PPT-By AllenAllyna Samantha LucasNo ratings yet
- Braintainment - September-October 2015Document84 pagesBraintainment - September-October 2015Győrössi TímeaNo ratings yet
- Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 UpdateDocument153 pagesAllergic Rhinitis and its Impact on Asthma (ARIA) 2008 UpdateincaudasemperNo ratings yet
- Allergic Rhinitis and Chronic Suppurative Otitis Media: Archives of Oto-Rhino-Laryngology January 2011Document6 pagesAllergic Rhinitis and Chronic Suppurative Otitis Media: Archives of Oto-Rhino-Laryngology January 2011tiaNo ratings yet
- Ulangan Tengah Semester Gasal TAHUN PELAJARAN 2019/2020 Mata Pelajaran: Bahasa Inggris Kelas: IX Kode ADocument16 pagesUlangan Tengah Semester Gasal TAHUN PELAJARAN 2019/2020 Mata Pelajaran: Bahasa Inggris Kelas: IX Kode APrincess RaniaNo ratings yet
- RCPCH Allergy Care Pathways Project: Taking An Allergy Focused Clinical HistoryDocument14 pagesRCPCH Allergy Care Pathways Project: Taking An Allergy Focused Clinical HistoryBipin Bhagath.LNo ratings yet
- PDFDocument2 pagesPDFIamIvy Donna PondocNo ratings yet
- Pharmacognosy guide for pharmacy techniciansDocument61 pagesPharmacognosy guide for pharmacy techniciansKumar rajesh Kumar rajeshNo ratings yet
- The Nose, Upper Airway, and Obstructive Sleep ApneaDocument7 pagesThe Nose, Upper Airway, and Obstructive Sleep ApneaDaniel Celestino DiazNo ratings yet
- Naskah Soal: Ujian MadrasahDocument6 pagesNaskah Soal: Ujian MadrasahRizki MuhammadNo ratings yet
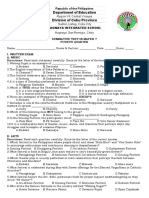
- Department of Education Division of Cebu ProvinceDocument5 pagesDepartment of Education Division of Cebu ProvinceNelsie FernanNo ratings yet
- Pathophysiology of Nasal CongestionDocument11 pagesPathophysiology of Nasal CongestionLussie_varetaNo ratings yet
- Revised RRLDocument5 pagesRevised RRLJoshua ArcairaNo ratings yet
- Isopathy PDFDocument11 pagesIsopathy PDFkiran_kandruNo ratings yet
- Written by Yamin Khan, PHD and Sarah Tilly: NtroductionDocument10 pagesWritten by Yamin Khan, PHD and Sarah Tilly: NtroductionChikezie OnwukweNo ratings yet
- International Journal of Pharmtech ResearchDocument5 pagesInternational Journal of Pharmtech Researchrosnita sidabalokNo ratings yet
- DYMISTA®Document8 pagesDYMISTA®ธัญญภัทร์ ทะหมุนNo ratings yet
- Pollen Allergy in Botany Classs NotesDocument7 pagesPollen Allergy in Botany Classs NotesAbhimanyu PandeyNo ratings yet
- Mm7246a2 HDocument5 pagesMm7246a2 Hsofy dewiNo ratings yet
- Allergic Rhinitis Diagnosis TreatmentDocument2 pagesAllergic Rhinitis Diagnosis TreatmentDengz MendozaNo ratings yet
- 20) Unit V Natural AllergensDocument32 pages20) Unit V Natural AllergensAnuj DesaiNo ratings yet
- Allergic Rhinitis - Causes, Symptoms, and DiagnosisDocument5 pagesAllergic Rhinitis - Causes, Symptoms, and DiagnosisArchies NayakNo ratings yet
- Aerius Syrup PIDocument9 pagesAerius Syrup PITerrence LiNo ratings yet
- Week 13 Inflammatory Ncma219 Lec Finals ReviewerDocument4 pagesWeek 13 Inflammatory Ncma219 Lec Finals ReviewerWynahNo ratings yet
- Desloratadine - A New, Nonsedating, Oral AntihistamineDocument12 pagesDesloratadine - A New, Nonsedating, Oral AntihistamineAnonymous so6ZnlKywNo ratings yet
- HEENT Focused Exam Soap NoteDocument5 pagesHEENT Focused Exam Soap Noteariel sparkmanNo ratings yet