Professional Documents
Culture Documents
Primary Care Position
Uploaded by
Tyler McLeanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Primary Care Position
Uploaded by
Tyler McLeanCopyright:
Available Formats
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CAREDOCTORS
IN NOVA SCOTIA
NOVA SCOTIA
2017 Position Paper
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS
TO IMPROVE PRIMARY CARE IN
NOVA SCOTIA
1 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
ACKNOWLEDGMENTS
Thank you to the members of the Doctors Nova Scotia Policy and
Health Issues Committee (PHIC), General Practitioner (GP) Council
and Board of Directors, who provided the concepts for this
document.
PHIC members Drs. Melanie Adams, Monika Dutt, Gary Ernest
(chair), Leo Fares, Alyson Holland, Tim Holland, Tammy Keough-
Ryan, Rod McGory, Elwood McMullin, Maria Migas, David Milne,
Sanju Mishra, Leslie Ribeiro, John Sullivan, Manoj Vohra and Howard
Wightman
GP Council members Drs. Peter Brennan, Michel Chiasson, Alban
Comeau (chair), Alana Cormier, Gary Ernest, John Ginn, Mary Gor-
man, Ajantha Jayabarathan, Stephanie Langley, Erica Lasher, Patty
Menard, Mary Frances Moriarty, Barb ONeil, Colette Sauveur and
Ehab Soliman
Board of Directors Drs. Minoli Amit, Andr Bernard (Board Chair),
Michelle Dow (President), Kathy Gallagher, John Ginn, Tim Holland,
Todd Howlett, Heather Johnson, Robyn MacQuarrie, Scott Mawds-
ley, David Milne (Past-President), Alex Mitchell, Norah Mogan, John
Murdoch, Manoj Vohra (President-Elect), Mike Wadden and Celina
White, and medical student Matthew Lowe
A special thank you to the following physician leaders, who provided
ongoing counsel during the development of this position paper:
Dr. Melanie Adams, Glace Bay
Dr. Lisa M. Bonang, Musquodoboit
Dr. Fred Burge, Halifax
Dr. Jeff Colp, Prospect
Dr. Esther Dias, Glace Bay
Dr. Michelle Dow, Meteghan
Dr. Michael J. Fleming, Fall River
Dr. Gary Ernest, Liverpool
Dr. Zaida Fragoso-Alvarez, Lower Sackville
Dr. Timothy Holland, Dartmouth
Dr. Ajantha Jayabarathan, Halifax
Dr. Tammy Keough-Ryan, Halifax
Dr. Stephanie Langley, North Sydney
Dr. Shelagh Leahey, Yarmouth
Dr. James MacKillop, Sydney
Dr. Tim Matheson, Bedford
Dr. Mary Frances Moriarty, Dartmouth
Dr. Katherine Quackenbush, Upper Tantallon
Dr. Leslie Ribeiro, Middleton
Dr. Rebecca Taylor-Clarke, Port Williams
Dr. Lianne Yoshida, Halifax
2 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
EXECUTIVE Doctors Nova Scotia (DNS) engaged family physicians throughout the province
to develop a position paper on primary care. As the association representing all
SUMMARY physicians, residents and medical students in the province, we know that there
is not a one-size-fits-all approach to providing primary care. We also know how
important it is that every Nova Scotian has access to a family physician, most
often (but not exclusively) as part of a collaborative primary health care team.
Having access to primary care is an important way to improve the health of Nova
Scotians, manage chronic diseases and create a more sustainable health-care
system. Creating an environment where all Nova Scotians have access to primary
care will require our health-care system to evolve. Primary care teams will need to
be developed and organized differently, and the way physicians practise and are
compensated will need to change. Family physicians understand and support the
need for change, and want to be part of reforming the primary care system.
Based on the feedback provided by family physicians, the Policy and Health
Issues Committee (PHIC) and the General Practitioners (GP) Council, as well as
a study of literature and primary care models in other provinces, DNS makes the
following recommendations to improve primary care in Nova Scotia immediately.
We recommend that physicians be improve access for their patients
given the opportunity to choose where appropriate.
what type of practice they want to We recommend that the DHW,
work in and develop. NSHA, physician recruiters and Dal-
We recommend that the housie Medical School work with
Department of Health and Well- DNS to develop a recruitment and
ness (DHW) and the Nova Scotia retention strategy.
Health Authority (NSHA) implement We recommend the DHW, NSHA,
patient rostering as part of a new physicians and other providers
payment model for primary care. develop creative and flexible solu-
We recommend that the DHW and tions that produce timely results for
NSHA work with DNS to develop a patients.
new blended-payment model to We recommend that walk-in clinics
better support patient care, fair be maintained during the transi-
compensation and good steward- tion to a better primary health-care
ship of public funds. system.
We recommend the DHW ensure We recommend that alternative
that compensation is not a disin- payment plans (APPs) be main-
centive for physicians to tained during the transition to a
WE RECOMMEND THE DHW provide non-face-to-face new primary health care system
ENSURE THAT COMPENSATION services, and that physi- with opportunities to evolve to a
cians leverage opportuni- blended payment model mecha-
IS NOT A DISINCENTIVE FOR ties to provide non-face- nism.
PHYSICIANS TO PROVIDE NON- to-face services in their We recommend the DHW, NSHA
FACE-TO-FACE SERVICES, AND practices. and IWK prioritize and invest in the
We recommend that development of a secure electronic
THAT PHYSICIANS LEVERAGE the DHW and NSHA sup- health record that is accessible by
OPPORTUNITIES TO PROVIDE NON- port family physicians in all health-care providers.
FACE-TO-FACE SERVICES IN THEIR implementing same-day/ We recommend that the DHW, the
next-day access in their NSHA and the IWK engage physi-
PRACTICES practices, and that physi- cians in transforming the primary
cians use this support to care system in Nova Scotia.
3 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
DR. HOLLY ZWICKER
TANTALLON
We try to see our patients as much as possible,
says Dr. Zwicker. She and her colleagues use online
booking software, an EMR and the services of a
family practice nurse to ensure their patients have
same-day/next-day access to primary care.
INTRODUCTION
Primary health care is the backbone of Nova It is not possible or feasible for every service
Scotias health-care system. Primary health to be available in every community; however,
care is the first place people go for health-care every Nova Scotian should be able to access a
or wellness advice and programs, treatment primary health care team that includes a family
of a health issue or injury, or diagnosis and physician. Today, this is not the case in our
management of a health condition. It is the province.
foundation of any health-care system, and In order for every Nova Scotian to have ac-
nations with strong primary health care have cess to a family doctor, the primary health care
better health than those without (Universi- system needs to be restructured. Attempts
ty of Ottawa, 2016). Countries with a strong have been made in the past to improve access
primary care orientation have demonstrably to services, but barriers to providing the
better health outcomes, lower mortality rates best possible care to patients remain. These
and lower overall health-care costs (Aggarwal, barriers are frustrating for Nova Scotians,
2012). Primary care also improves and sustains physicians and the provincial government.
the health-care system at other levels. Primary Nova Scotia has made some improvements
care providers, as the gatekeepers of health- in primary care, such as the introduction of
care delivery, can reduce unnecessary costs Collaborative Emergency Centres, investments
and the need for specialty care by improving in a small number of collaborative care teams,
the quality of prevention, coordination and and the creation of residency teaching sites,
continuity of care (Canadian Health Services which aim to train more family physicians in ru-
Research Foundation, 2012). Yet Canadas ral medicine, in South West Nova, the Annapo-
performance in primary care trails that of many lis Valley and Sydney. Yet our province contin-
other high-income countries, and Nova Scotia ues to fall behind in many areas. For example,
lags behind many Canadian provinces (Aggar- provinces such as New Brunswick, Quebec,
wal, 2012). Manitoba, Alberta and British Columbia have
A high-functioning and efficient primary developed programs and structures to support
health care system will ensure Nova Scotians the advancement of primary health care and
can access primary care when they need it. collaborative care, while many Nova Scotians
4 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
are unable to find a family physician and face as are innovation, creativity, the courage to try
long wait times for services, and physicians in new things and the wisdom to accept lessons
the province are dealing with recruitment and learned in other jurisdictions. This paper out-
retention challenges and a fractured electronic lines the principles that the physicians of Nova
medical record (EMR) environment. Scotia believe must guide primary care reform,
The physicians of Nova Scotia, through DNS, while being mindful of each of these keys to
want to improve the primary health care system success, as well as the barriers and oppor-
in the province. Physicians know the biggest tunities we foresee. This paper also includes
barriers to effective and accessible primary a proposal for a payment model to support
care, and how these barriers are affecting Nova high-functioning primary health care teams.
Scotians. Physicians are essential to the suc-
cess of transforming the health care system,
BACKGROUND
Having access to a family doctor is a critical often access primary care through walk-in
component of a primary care system. Unfor- clinics and emergency departments, these
tunately, many Nova Scotians are unable to patients do not have access to one provider
find a family doctor. While Nova Scotia has who knows their medical history. Patients
the highest physician-to-patient ratio in the receiving episodic care through walk-in clinics
country, with 260 physicians per 100,000 and emergency department visits do not have
people (Canadian Medical Association, 2014); access to the comprehensive care that many of
the distribution (by specialty and geography) them need to manage their health. In addition,
of these physicians remains unbalanced in those who do have a family physician often
the province. The high physician-to-patient struggle to see their doctor in a reasonable
ratio can be attributed in part to the facts period of time; some patients need to wait sev-
that Nova Scotia provides tertiary care to eral days to see their family doctor when they
people from all of the Atlantic provinces, and are ill. In many cases, even patients with family
that Dalhousie Medical School is the largest physicians end up accessing care in a walk-in
medical education site in the Maritimes. Even clinic or emergency department.
with a high physician-to-patient Patients continually express their con-
THE PROVINCIAL GOVERNMENT ratio, there are still approximately cerns with their level of access to primary
PHYSICIAN RESOURCE PLAN 90,000 Nova Scotians without a care services in Nova Scotia. These concerns
family doctor (Statistics Canada, are shared by family physicians throughout
IDENTIFIES THE NEED TO RECRUIT 2014). The provincial government the province. Nova Scotia has an aging pop-
512 FULL-TIME EQUIVALENT (FTE) physician resource plan identifies ulation, and many individuals are living with
FAMILY PHYSICIANS OVER THE the need to recruit 512 full-time chronic diseases and multiple morbidities.
equivalent (FTE) family physicians This is straining not only primary health care
NEXT 10 YEARS over the next 10 years. Of those, but the provinces emergency departments,
465 FTEs are to replace existing in-hospital care and long-term care systems.
practising family physicians and 47 are new As the first stop for patients when they are ill,
family physicians needed to address increased family physicians are being asked to provide
patient need (Nova Scotia Department of more services in their practices, including
Health and Wellness, 2016). palliative care, mental health services, chronic
Those without a family doctor have been plan management, pediatric care and geriatric
left feeling frustrated and uneasy about the care, accessing specialist care as appropriate.
level of care they are receiving. Although they This helps alleviate strain in other areas of the
5 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
system, but continues to overburden primary in their practices, they end up taking on more
health care providers. Although it is appropri- work with fewer resources, which results in
ate for family physicians to provide these types longer wait times and shorter appointments for
of care, it can be challenging for them to do patients, and increased workloads for primary
so without the proper supports. When family health-care providers.
physicians are providing more complex care
CRITICAL SUCCESS FACTORS
NOVA SCOTIA PHYSICIAN PERSPECTIVES
Nova Scotian physicians, including members to multi-disciplinary teams/resources.
of the associations PHIC and GP Council, have In order for primary care to be effective, all
identified critical factors that are essential to system stakeholders including patients
the success of an effective primary health-care and communities; the DHW, NSHA and
system. These factors build upon the work IWK; and stakeholder groups such as DNS
done by other organizations and jurisdictions. must work well together.
These critical success factors are: Not all communities will need the same
Every Nova Scotian must have access to a type of primary care providers and ser-
primary health care team that includes a vices; however, every community does
family doctor. This is important for patients require access to primary care. System
and for the sustainability of the system. planning must take community needs and
Better access and greater attachment to gaps in services into account.
a family physician lead to better health When responding to community needs,
outcomes, which in turn reduce cost by family physicians should be able to com-
reducing hospital- mit to one or more clinical areas as major
EVERY NOVA SCOTIAN MUST HAVE ACCESS izations, re-admis- components of their practice to best serve
TO A PRIMARY HEALTH CARE TEAM THAT sion rates, unnec- their patent population.
essary diagnostic The concepts outlined by the College of
INCLUDES A FAMILY DOCTOR. tests, professional Family Physicians of Canada (CFPC) in their
visits and emer- Patients Medical Home (PMH) should
gency department be a starting point for restructuring prima-
use (and, indirectly, by increasing employ- ry health care. The concepts include:
ment, productivity and economic growth). o Providing patient-centred care
The unique doctor-patient relationship o Ensuring every patient has a per-
should be respected. sonal family physician
Family physicians must not only treat ill- o Providing a broad scope of services
ness, but also work with their patients and carried out by teams or networks of
communities to prevent diseases. Family providers
physicians want to play a role not only in o Increasing timely access
treating illness but also in preventing it. o Improving continuity of care,
Patients must be engaged in defining what relationships and information for
effective primary care is. patients
Primary care should be patient-centred, o Maintaining EMRs for patients
provide continuity of care, and be efficient o Training medical students, family
and effective. Patients should have access medicine residents and those in
6 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
other health professions sional satisfaction for physicians, helps
o Evaluating the PMHs effectiveness recruit and retain new medical graduates,
in continuous quality improve- and provides more opportunities for
ments ongoing professional development among
o Working within governance and health-care providers.
management structures defined by Physician recruitment and retention should
stakeholders such as government, be a priority. Policies, payments and
patients, the public, and other actions should reflect an awareness of
medical and health professions and the need for more family physicians in the
their organizations across Canada province.
Team-based care should be supported. It
enhances patient care, increases profes-
PRIMARY CARE CHALLENGES
Primary care reform must be undertaken with team-based primary care.
these critical success factors as guiding prin- However, moving toward more team-based
ciples. One key element is to move to more care is not without challenges.
team-based care. Team-based care offers
many potential advantages, including ex- PAYMENT STRUCTURE
panded access to care (more hours of cover- BARRIERS
age, shorter wait times) [and] more effective The way physicians are compensated can
and efficient delivery of additional services be a barrier to providing patient-centred
that are essential to providing high-quality care in a collaborative environment. Doctors
care, such as patient education, behavioral in Nova Scotia are currently paid primarily
health, self-management support, and care under three models: fee-for-service (FFS),
coordination (Schottenfeld, 2016, p. 3). alternative payment plans (APP) and aca-
There is a growing body of demic funding plans (AFP); in addition, a
UNDER THE FFS PAYMENT Canadian research that demon- limited number of physicians working in
strates the value of collaborative Collaborative Emergency Centers (CECs) have
MODEL, DOCTORS ARE USUALLY
primary health care. For example, unique payment structures. Although each
COMPENSATED FOR THE NUMBER in 2014 the Association of Family of these models works for certain practice
OF SERVICES THEY PROVIDE, NOT Health Teams of Ontario released environments solo practice, under-serviced
an external evaluation report on areas or a teaching environment, for example
THE LENGTH OF TIME THEY SPEND
family health teams (FHT) that they do not always support collaboration
WITH PATIENTS OR COLLABORATING demonstrated improvements between care providers.
WITH OTHER HEALTH-CARE over the study period in the Under the FFS payment model, doctors
areas of access to same-day ap- are usually compensated for the number of
PROVIDERS, SUCH AS NURSES OR
pointments and chronic disease services they provide, not the length of time
PHARMACISTS management (Conference Board they spend with patients or collaborating
of Canada, 2014). Other reports, with other health-care providers, such as
such as the Evaluation of the Full Service nurses or pharmacists. Doctors are indepen-
Family Practice Incentive Program and the dent contractors responsible for paying their
Practice Support Program (Hollander, 2013), staff and overhead costs (such as rent and
have also identified promising findings for office equipment). Physicians need to be able
7 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
to work enough hours to cover their staffs sala- patient care with other providers, rather than
ries, their practice-related expenses and their financially penalizing them for seeing fewer
own salary. It can be challenging for them to patients in a day. As we learn more about the
make unpaid time available to collaborate with best ways to provide care to patients and com-
other providers. munities, it is important that the compensation
Additionally, as other health-care providers models for family physicians also evolve.
are expanding their scopes of practice and Nova Scotian doctors have identified the
providing more services to patients, family phy- need to shift compensation to mechanisms
sicians are more seeing patients with complex that better support preventative medicine and
conditions in their offices and fewer patients chronic disease management. Over the past
for short visits for preventative medicine, such two decades this shift has occurred in other
as immunizations. It is appropriate for family provinces, where different payment models
physicians to provide complex care and for have been developed to support collaborative
other providers to work to their full scope of models of care. Nova Scotias funding models
practice. However, the system must compen- must evolve to support more effective primary
sate doctors for spending more time with pa- care delivery.
tients when that is needed and for coordinating
ELECTRONIC MEDICAL RECORDS
Electronic medical records (EMRs) are the information system for health system use and
backbone of primary health care and collab- direct patient care. The project has been de-
orative care teams. Approximately 60 percent layed but now appears to be moving forward.
of family physicians in the province use an The province also moved forward with
EMR. However, Nova Scotia does not have an MyHealthNS, a secure system that allows Nova
effective way to share medical records among Scotians to receive, view and manage their per-
health-care providers, hospitals and medical sonal health information online. MyHealthNS
zones. The current hospital-based systems are is an important step toward a less fractured
poorly integrated and, in some cases, outdat- e-health system; however, it does not replace
ed. This is a major obstacle the province needs a system that shares electronic health records
to overcome before it can significantly improve among providers. The lack of integration within
how primary care is delivered. the province is causing significant challenges
The provincial government has tried to for improving collaborative care. A system that
improve e-health systems in Nova Scotia. One allows one secure electronic health record to
of the most recent efforts is One Patient One be accessed by care providers as appropri-
Record (OPOR). OPOR is intended to improve ate would improve care, reduce unnecessary
patient care and safety by providing clinicians testing, improve patient safety and increase
with a single, province-wide electronic medical system efficiency.
THE LACK OF INTEGRATION WITHIN THE PROVINCE IS CAUSING
SIGNIFICANT CHALLENGES FOR IMPROVING COLLABORATIVE CARE.
A SYSTEM THAT ALLOWS ONE SECURE ELECTRONIC HEALTH RECORD TO
BE ACCESSED BY CARE PROVIDERS AS APPROPRIATE WOULD IMPROVE
CARE, REDUCE UNNECESSARY TESTING, IMPROVE PATIENT SAFETY AND
INCREASE SYSTEM EFFICIENCY
8 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
PRIMARY CARE RECOMMENDATIONS
TRANSITIONING SAFELY TO A BETTER PRIMARY HEALTH CARE SYSTEM
NEW INTIATIVES THAT NEED TO BE IMPLEMENTED
Nova Scotia is lagging behind other provinces physicians, working with DNS, to collaborate
in advancing primary health care reform. For with the DHW, NSHA and IWK to work together
example, in 2015 British Columbia released its to advance a shared vision for primary care in
vision for primary care in the document Pri- Nova Scotia.
mary and Community Care in BC: A Strategic New models of care and physician payment
Policy Framework and in 2012 New Brunswick models will need to be considered if Nova Sco-
released A Primary Health Care Framework tia hopes to establish a primary care system
for New Brunswick. Alberta uses primary care that addresses the principles of primary care
networks, and Ontario use several models, outlined above.
including family health groups, family health After looking at primary health care and
networks, family health organizations, family collaborative care team structures in other
health teams, and community health centres. provinces and reviewing feedback from family
The recent restructuring of the Nova Scotia physicians, DNS makes the following recom-
heath-care system presents opportunities for mendations.
FLEXIBILITY IN THE It is important to remember that there is while in other areas a collaborative team may
SYSTEM not a one-size-fits-all approach to providing best serve a population. In some instances,
primary care. Physicians, patients and commu- a patient may only want to receive care from
We recommend that physi- nities throughout Nova Scotia require flexibility their family physician, while others may prefer
cians be given the oppor- in how they deliver and receive care. In some accessing the expertise of multiple providers.
tunity to choose what type cases, a solo family practice as part of a larger The health-care system needs to allow for
of practice they want to network might best meet a communitys needs, these (and other) variations in practice types.
work in and develop.
PATIENT ROSTERING Patient rostering is a commonly used model and other team members, which is a critical
We recommend that the of organizing patients and providers for collab- factor contributing to better health outcomes,
DHW and NSHA implement orative care. The CFPC defines patient roster- particularly for chronic disease management.
patient rostering as part of ing in family practice as a process by which Patient rostering with a family physician and
a new payment model for patients register with a family practice, family team also facilitates effective preventive care
primary care. physician, or team. Patient rostering facilitates and supports CQI [continuous quality improve-
accountability by defining the population for ment] activities in the practice (CFPC, 2012,
which the primary care organization or provid- p.1).
er is responsible and facilitates an ongoing Physicians who work in a patient rostering
relationship between the patient and provider model are not compensated through an FFS,
(CFPC, 2012, p.1). APP or AFP payment model, but through a
Many provinces, including British Columbia, model that combines FFS billing and capita-
Manitoba, Ontario, Quebec, New Brunswick tion/negation. Additionally, physicians should
and Prince Edward Island, have implemented be provided administrative supports to help
some form of patient rostering. Provinces with establish, maintain and monitor their patient
better developed primary health care have roster. Efforts should be made to ensure phy-
endorsed patient rostering because it can fa- sicians are not overburdened with increased
cilitate the development and strengthening of administrative or overhead costs or unmanage-
the continuing relationship between patients able amounts of paperwork.
and their personal family physician, nurses,
9 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
PRIMARY CARE RECOMMENDATIONS
BLENDED PAYMENT Blended payment models are required to to work in a collaborative practice with a blend-
MODEL support patient rostering. There are several ed payment model. Physicians should not be
We recommend that the different models used throughout the country. financially penalized for decisions made by pa-
DHW and NSHA work with They usually combine elements of capitation, tients when the physician is providing appro-
DNS to develop a new negation and FFS payment models. Each of priate access. Physicians need to be engaged
blended payment model these payment mechanisms presents challeng- in the development of the negation process to
to better support patient es and benefits, but used in combination they ensure that it fosters appropriate care, does
care, fair compensation provide a comprehensive payment structure not deter physicians from patient rostering and
and good stewardship of that supports better patient care, fair compen- reflects the realities of family practice.
public funds. sation for physicians and good stewardship of Nova Scotia will need to develop its own
public funds. version of capitation that supports communi-
ties; however, we will not have to start from
Capitation scratch. Other provinces have learned lessons
Capitation is a payment structure in which a that can help Nova Scotia develop an effective
physician is paid a fixed amount to provide blended payment model.
care to a defined group of patients under his or
her care. The remuneration unit is the individu- Fee-for-service
al patient, not a service or procedure. As some Capitation is usually combined with an FFS
patients require more attention than others, payment model to encourage productivity and
capitation systems usually do not pay the ensure that data is being collected to track the
same for every patient but take the patients services being provided. Data is an import-
health needs into account (University of Otta- ant way to safeguard against inaccurate age
wa, 2016). Payments for rostering an individual and sex modifiers in capitation, and to gain
can vary drastically depending on predeter- a better understanding of the patient profiles
mined modifiers such as age and sex. in geographical areas (NBMS, 2016). This can
help better develop collaborative care teams
Negation to ensure the most appropriate health-care
It is not possible to have capitation without providers are offering the right services for the
checks in the system to ensure the steward- community they serve.
ship of public funds. This is usually done In a capitation model, doctors do not
through a mechanism called negation. Nega- receive full FFS compensation for the services
tion is a market-based incentive which avoids they bill as FFS because they already receive
over-measurement and over-management of capitation payments for their enrolled patients.
physicians by government, while ensuring Capitation is considered the base for providing
government does not pay twice for the same all services. The family physician bills for every
medical service (NBMS, 2016). If a rostered patient they see and every service they pro-
patient receives a capitated service from a vide, but the services are paid at a discounted
primary care physician outside of their usual rate (NBMS, 2016).
family practice, the capitated physician who In a blended payment model, all three com-
has enrolled the patient could be financially ponents capitation, negation and FFS need
penalized (Sweetman, 2014). For example, if a to work together to encourage productivity,
patient rostered to a certain physician visits a support advanced access and ensure good
walk-in clinic rather than their family physician stewardship of public funds. Other provinces
for their care, the fee paid to the walk-in clinic have been able to adopt blended payment
is recouped from the family physicians next models. Nova Scotia has an opportunity to
capitated payment, with a clearly indicated learn from the work that has already been done
reason (NBMS, 2016). It will be important that and develop a solution specific to the prov-
capitation is not a disincentive for physicians inces needs.
10 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
PRIMARY CARE RECOMMENDATIONS
NON-FACE-TO-FACE The most common approach to health Research indicates that non-face-to-face
PAYMENT MODELS care delivery is through face-to-face contact services can produce cost savings through the
We recommend the DHW between a health-care provider and a patient. provision of better care, which reduces the
ensure that compensation There is, however, an increasing trend toward frequency and/or cost of subsequent health
is not a disincentive for the provision of health-care in the absence of care services. It also provides greater access
physicians to provide non- personal contact, which is known as non-face- to quality care, better management of chronic
face-to-face services, and to-face care (Stylus Consulting, 2015). Non- diseases, and a solution to critical physician
that physicians leverage face-to-face care refers to linking patients to a shortages in both urban and rural areas (Stylus
opportunities to provide health-care team through a videoconferencing Consulting, 2015).
non-face-to-face services platform, or by phone, email or other forms of Helping physicians provide non-face-to-face
in their practices in order electronic communication. services is a key component of addressing
to increase access for their In a 2014 Stylus Consulting study of more many of the challenges facing the provinces
patients. than 4,200 patient appointments, it was found health-care system, such as an aging pop-
that e-visits have the potential to fundamen- ulation, high rates of chronic disease, and
tally improve the way doctors provide clinical recruitment and retention issues. Doctors Nova
care. On average, 22 percent of all appoint- Scotia recommends that the DHW support
ments would have been appropriate (in part adjustments to the Fee Schedule to support
or whole) for an e-visit instead. Doctors also any appropriate non-face-to-face interaction
reported that providing an e-visit takes them between physicians and patients, whether
less time than an in-person appointment and by phone, email, videoconferencing or other
that the use of e-visits could open up about forms of electronic communication.
two appointment slots each day.
SAME-DAY/
NEXT-DAY ACCESS In high-quality health-care systems, people 2012). There are different ways for family phy-
should be able to see their primary care phy- sicians to implement this model. For example,
We recommend that the sicians in a timely manner when they become a practice with an elderly or chronically ill
DHW and NSHA support ill, including on the same day when clinically population may need to reserve some appoint-
family physicians in appropriate (Kiran, 2015). Canada is failing ments for routine care, in addition to accepting
implementing same-day/ at providing timely access for many patients. patients who call for an appointment that day.
next-day access in their According to the Commonwealth Fund (Health There are several practices in Nova Scotia al-
practices, and that physi- Council of Canada, 2014), only 41 percent of ready offering this service to patients. In most
cians use this support to Canadians said they could get an appointment cases, family practices offer both same-day
improve access for their on the same or next day when they were sick or and scheduled appointments.
patients where appropri- needed medical attention. This was the lowest To increase the number of family physicians
ate. reported percentage among the 11 high-income offering same-day/next-day access, several
countries included in the study (Kiran, 2015). supports should be implemented, such as in-
As a result, many Canadians access primary creased funding for providing after-hours care,
health care services in emergency care support to address patient backlogs, increased
settings. access to collaborative care teams, increased
Same-day scheduling typically requires that access to PHRs, recruitment of sufficient
practices do todays work today by offering numbers of physicians to meet community
the majority of patients the opportunity to need, and increased access to non-face-to-face
book their appointments on the day they call, services.
regardless of the reason for the visit (CFPC,
11 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
PRIMARY CARE RECOMMENDATIONS
DR. JOHN KEELER
SHELBURNE
Rural family physician Dr. Keeler helps his patients
get the treatment they need and gives them the
security of having a family doctor in their corner.
When people have a family physician theyre com-
fortable with, it makes their care a lot simpler, he
says. It gives them peace of mind.
RECRUITMENT AND In order for Nova Scotia to reform its prima- Previous iterations of practice environments do
RETENTION ry health care system, the province will need to not work for the majority of new family physi-
We recommend that the recruit and retain physicians to work in com- cians entering practice. The province will need
DHW, NSHA, physician munities throughout the province. The NSHA to develop creative solutions to ensure that
recruiters and Dalhou- should work with doctors and other providers Dalhousie Medical School graduates choose to
sie Medical School work to determine what practice structures best practise in Nova Scotia.
with DNS to develop a support primary care in specific communities. Nova Scotia is not, for the most part, a net
recruitment and retention Providing physicians with the flexibility to help importer of physician talent. In the national
strategy. design their practices is a critical component in marketplace, Nova Scotia is not overly com-
recruiting and retaining doctors in Nova Scotia. petitive, largely because our physicians are
Making the province more inviting to medi- among the lowest paid in Canada. This makes
cal students and residents is a critical factor in it even more critical that we train and retain
reaching the provinces recruitment goals. Ac- young physicians here in Nova Scotia. We
cording to the 2012 DNS membership survey, encourage the DHW, the NSHA, the IWK, physi-
most medical students and residents identified cian recruiters and Dalhousie Medical School
their ideal practice type as a group practice to work with DNS to develop a recruitment
with physicians and other health-care provid- and retention strategy that meets the needs of
ers. They also indicated they value having a Nova Scotians.
turn-key office with amenities such as EMRs.
12 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
PRIMARY CARE RECOMMENDATIONS
FLEXIBILITY IN Developing primary care teams will take sician. The DHW, NSHA, physicians and other
PRIMARY CARE time. For example, it takes time to implement health-care providers need to develop creative
the infrastructure needed to support large and flexible solutions that produce timely
We recommend the DHW, group practices, such as EMRs and office results for patients.
NSHA, physicians and space. It will also take time to find health-care Additionally, health-care providers need to
other providers develop providers who have the interest and training to have options to choose from when deciding
creative and flexible solu- work in a collaborative primary care setting. what type of practice and payment model they
tions that produce timely In the interim, there needs to be flexibility would like to work in. Many family physicians
results for patients. in the system to allow for creative solutions will prefer to work in a collaborative care team;
to address immediate gaps in services. The however, that may not be the best fit for all
provision of primary care cannot slow down to providers and communities. Physicians should
make time for needed changes in the system. have flexibility in deciding their practice types,
It is important that the long-term vision for pri- as long as the services they provide align with
mary care does not detract from the immediate the needs of the community.
need for improved access for patients currently
without a primary care team and/or family phy-
TRANSITIONING SAFELY TO A BETTER PRIMARY HEALTH CARE SYSTEM
CURRENT INTIATIVES THAT NEED TO BE CONTINUED
Primary health care access issues, recruit- Time will be required to develop and evaluate
ment and retention challenges and increasing an optimal primary health care system. While
health-care budgets demonstrate the need moving toward a provincial vision for health
to change how primary health care is deliv- care, some of the current systems will need to
ered in Nova Scotia. However, these changes remain in place to ensure that patient care is
cannot and should not be made overnight. not jeopardized.
WALK-IN CLINICS Walk-in clinics provide episodic care to the pillars of the PMH, they do service a need
patients who do not have a family physician in communities. Ideally, all Nova Scotians
We recommend that or who are unable to access care from their would be able to access care from their own
walk-in clinics be main- regular provider in an appropriate time frame. family physician working with other providers;
tained during the transi- When accessing care through a walk-in clin- however, we are far from achieving this goal.
tion to a better primary ic, patients rarely see the same provider. In the meantime, as we work toward improved
health-care system. This makes it very challenging for patients to access, patients still need care. Walk-in clinics
receive continuity of care. Patients who do not can serve as a transition tool, ensuring
have continuity of care are more likely to be patients can access primary care (if not conti-
hospitalized, visit the emergency department nuity of care) while we work on improving the
and be less satisfied with the health-care primary health care system.
system (Van Walraven, 2010). Five of seven While we recognize the shortcoming of
studies found increased continuity of care walk-in clinics, health-care stakeholders are
improved patient satisfaction. Walk-in clinics increasing the level of oversight and working to
are not the best way for most individuals to ensure the clinics deliver the best care possi-
access primary care it might be acceptable ble. For example, the College of Physicians and
for a healthy 20-year-old, but not for an elderly Surgeons of Nova Scotia has developed the
person living with chronic diseases. Professional Standard on the Standard of Care
Although walk-in clinics do not align with for Walk-in Clinics (updated 2015).
13 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
PRIMARY CARE RECOMMENDATIONS
Alternative payment plans (APPs) are indi- create a disincentive to treat more patients.
ALTERNATIVE vidual or group physician funding agreements Additionally, physicians working in an APP
PAYMENT PLANS for the provision of clinical services. Approx- structure are constrained to many of the same
We recommend alter- imately 100 family physicians are funded limitations as FFS physicians through a process
native payment plans through this payment model in Nova Scotia. called shadow billing. Shadow billing requires
(APPs) be maintained Well-designed APPs support collaborative care physicians working in an APP environment to
during the transition to a because family physicians are not financially record the services they provide using the FFS
new primary health care penalized for working with other health-care billing structure. APP physicians are required
system, with opportunities providers. They can remove the competitive- to meet shadow billing thresholds and targets.
to evolve to a blended pay- ness that is sometimes felt between providers These targets detract from many of the bene-
ment model. when one is compensated for a service and the fits of the APP structure, such as being able to
other is not. This encourages all members of a spend more time with complex patients, and
team to work to their full scope of practice. encourage physicians to reach metrics based
Unfortunately, APPs as currently structured on volume rather than quality of care.
in Nova Scotia present challenges because Ideally, Nova Scotia would implement
of their fixed payment structure. Doctors are blended payment models throughout the prov-
not incentivized to take on more patients. For ince to encourage family physicians to collab-
example, if family physicians take on more orate and treat more patients. However, this
patients, they face an associated increase transition will take time. In the meantime, APPs
in costs for supplies, but they are unable to can provide an interim step toward a blended
generate more income for their clinic to cover payment model.
the additional costs. In some cases, this can
PERSONAL HEALTH A personal health record (PHR) contains example, in some instances physicians lose
RECORD health data and information; it is shared opportunities to generate income when they
between a patient and their physician. Using use PHRs because they are seeing fewer pa-
We recommend the DHW, a PHR helps patients take greater control of tients in their office and they are not remuner-
NSHA and IWK prioritize managing their health, while also providing ated for treating patients without a face-to-face
and invest in the de- doctors with important health information visit. Compensation issues must be addressed
velopment of a secure about their patients. Personal health records in order to enable physicians to fully leverage
electronic health record are the first step in enabling physicians and technology in their practices. When compensa-
accessible by all health- patients to interact using technology. As our tion issues have been addressed appropriate-
care providers. e-health system grows, its important that ly, the PHR will be an important tool for improv-
e-health technologies such as PHRs, EMRs, ing physician access.
the drug information system and the hospital In the coming years, Nova Scotia will need
information system are integrated. to develop an e-health system that connects
It is also important that physicians are all providers and health-care institutions; but
supported in using available technology. This until then, the PHR called MyHealthNS is an
includes removing disincentives that limit important first step.
physicians use of e-health technologies. For
14 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
PRIMARY CARE RECOMMENDATIONS
DR. CATHY FELDERHOF
PICTOU LANDING
I want all my patients to feel empowered to play
a role in their own health, says Dr. Felderhof. By
empowering instead of enabling, my patients build
on their strengths and can become healthier.
PHYSICIAN Physicians are vital members of all health- most likely to experience improved outcomes
ENGAGEMENT care teams and have broad training and capa- (Denis, 2013). Understandably, physicians
bilities. They play a critical role in health-care cannot and do not typically support health
We recommend that the delivery. They direct, coordinate and deliver care changes or initiatives that they have not
DHW, NSHA and IWK en- patient care, and their perspective reveals the been permitted to take part in shaping or that
gage physicians in trans- physicians experience as well as reflecting the did not consider their perspective. Effective
forming the primary care needs of patients. physician engagement is essential to effecting
system in Nova Scotia. Physicians have a vested interest in trans- change within any health-care organization
forming Nova Scotias health-care system in and the health system as a whole. As the prov-
order to ensure safe, high-quality health-care ince moves forward with transitioning primary
services. It has been well established that or- health care, physicians, through DNS, should
ganizations that effectively engage physicians be viewed as critical stakeholders by the DHW,
in health system design, change processes the NSHA and the IWK.
and leadership development opportunities are
CONCLUSION
Physicians have growing concerns about the primary health care system in Nova Scotia. The
recommendations outlined in this document are only a portion of the work that will need to
happen to shift the current system. Physicians want to work with other health-care providers,
patients, the government and the health authorities to fix the primary health care system.
Doctors Nova Scotia and the DHW, NSHA and IWK must find innovative and fiscally responsible
ways to support physicians, and all health-care providers, in providing primary health care to
Nova Scotians. By investing in primary health care teams, adopting new payment models for
physicians, improving e-health systems, and recruiting and retaining physicians, Nova Scotia will
be able to improve its primary health care system.
15 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
REFERENCES
Alberta Health. (2016). Primary Care Networks Review. Retrieved from http://www.health.alberta.ca/documents/
PCN-Review-2016.pdf
Alberta Health. (n.d.). Primary Care Services: Primary Care Networks. Retrieved from http://www.health.alberta.ca/
services/primary-care-networks.html
Aggarwal, M., & Hutchison, B. (2012). Toward a Primary Care Strategy for Canada. Canadian Foundation for Healthcare
Improvement. Retrieved from http://www.cfhi-fcass.ca/Libraries/Reports/Primary-Care-Strategy-EN.sflb.ashx
Canadian Health Services Research Foundation. (2012). The Economic Impact of Improvements in Primary Health-care
Performance. Retrieved from http://www.cfhi-fcass.ca/Libraries/Commissioned_Research_Reports/Dahrouge-
EconImpactPHC-E.sflb.ashx
Canadian Institute for Health Information. (2006). Pan-Canadian Primary Health Care Indicators. 1(2). Retrieved from
https://secure.cihi.ca/free_products/PHC_Indicator_Report_1-Volume_2_Final_E.pdf
Canadian Institute for Health Information. (2016). Wait Times for Priority Procedures in Canada. Retrieved from https://
secure.cihi.ca/estore/productFamily.htm?locale=en&pf=PFC3108
Canadian Medical Association. (2015). Physician Data Centre: Canadian Physician Statistics. Retrieved from https://www.
cma.ca/Assets/assets-library/document/en/advocacy/12-Phys_per_pop.pdf
College of Family Physicians of Canada. (2012). Best Advice: Patient rostering in family practice. Retrieved from http://
www.cfpc.ca/uploadedFiles/Health_Policy/CFPC_Policy_Papers_and_Endorsements/CFPC_Policy_Papers/BestAdvice_
RosteringFINALOct30.pdf
College of Family Physicians of Canada. (2012). Best Advice: Timely access to appointments in family practice. Retrieved
from http://www.cfpc.ca/uploadedFiles/Health_Policy/_PDFs/2012_Final_Best_Advice_Enhancing_Timely_Access.pdf
College of Family Physicians of Canada. (2011). A Vision for Canada: Family Practice, The Patients Medical Home.
Retrieved from http://patientsmedicalhome.ca/resources/resources-for-health-care-providers/2011-pmh-vision-paper/
College of Physicians and Surgeons of Nova Scotia. (2015). Professional Standard on the Standard of Care for Walk-in
Clinics. Retrieved from https://www.cpsns.ns.ca/DesktopModules/Bring2mind/DMX/Download.aspx?
PortalId=0&TabId=129&EntryId=21
Conference Board of Canada. (2014). Final Report: An External Evaluation of the Family Health Team (FHT) Initiative. Re-
trieved from http://www.conferenceboard.ca/temp/accf26d8-e115-433c-94a3-7b7ea5be6fb7/6711_familyhealthteam_rpt.
pdf
Denis, J.L., Baker, G.R., Black, C., Langley, A., Lawless, B., Leblanc, D., Lusiani, M., Hepburn, C.M., Pomey, M.P., & Tr, G.
(2013). Exploring the Dynamics of Physician Engagement and Leadership for Health System Improvement. Retrieved from
http://www.cfhi-fcass.ca/sf-docs/default-source/reports/Exploring-Dynamics-Physician-Engagement-Denis-E.pdf?
sfvrsn=0
Doctors Nova Scotia. (2012). Doctors Nova Scotia 2012 Membership Survey. Unpublished internal document.
Health Council of Canada. (2005). Primary Health Care. Retrieved from http://www.healthcouncilcanada.ca/tree/2.44-
BkgrdPrimaryCareENG.pdf
16 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
FIXING NOVA SCOTIAS PRIMARY HEALTH CARE PROBLEM:
PHYSICIANS RECOMMENDATIONS TO IMPROVE PRIMARY CARE IN NOVA SCOTIA
Health Council of Canada. (2014). Where you live matters: Canadian views on health care quality. Canadian Health Care
Matters, Bulletin 8. Retrieved from https://secure.cihi.ca/free_products/HCC_CMWF_Bulletin_8_Eng.pdf
Health Force Ontario. (2016). Family Practice Compensation Models. Retrieved from http://www.healthforceontario.ca/
en/Home/Physicians/Training_%7C_Practising_in_Ontario/Physician_Roles/Family_Practice_Models/Family_Practice_
Compensation_Models
Hollander, M.J. (2013). Evaluation of the Full Service Family Practice Incentive Program and the Practice Support Program.
http://www.gpscbc.ca/sites/default/files/Synthesis-Report-2_2013-06-13.pdf
Kiran, T., & OBrien, P. (2015). Challenges of same-day access in primary care. Canadian Family Physician, 61, 399-400.
Retrieved from http://www.cfp.ca/content/61/5/399.full.pdf+html
Manitoba Health. (n.d.). A Vision for My Health Teams. Retrieved from http://www.gov.mb.ca/health/primarycare/
providers/pcn/index.html
New Brunswick Medical Society. (2016). Family Medicine New Brunswick model. Unpublished internal document.
Nova Scotia Department of Health and Wellness. (2016). Physician Resource Plan: Base Forecast Summary by Spe-
ciality by Zone. Retrieved from http://novascotia.ca/dhw/ShapingPhysicianWorkforce/docs/BASECASE-Forecast-TO-
TAL-2016-to-2025.pdf
Schottenfeld, L., Petersen, D., Peikes, D., Ricciardi, R., Burak, H., McNellis, R., & Genevro, J. (2016) Creating Patient-cen-
tered Team-based Primary Care. Agency for Healthcare Research and Quality Pub. No. 16-0002-EF. Retrieved from https://
pcmh.ahrq.gov/sites/default/files/attachments/creating-patient-centered-team-based-primary-care-white-paper.pdf
Stylus Consulting. (2014). Nova Scotia Personal Health Record Demonstration Project: Benefits Evolution Report. Re-
trieved from https://www.infoway-inforoute.ca/en/component/edocman/1995-nova-scotia-personal-health-
record-demonstration-project-benefits-evaluation-report/view-document
Stylus Consulting. (2015). Virtually There, Physician Funding and Non-F2F Patient Care: An Options Analysis for Nova
Scotia. Internal document prepared for the Department of Health and Wellness and Doctors Nova Scotia.
Statistics Canada. (2012). Access to regular medical doctor, 2012. Retrieved from http://www.statcan.gc.ca/pub/82-
625-x/2013001/article/11832-eng.htm
Sweetman, A., & Buckley, G. (2014). Ontarios Experiment with Primary Care Reform. School of Public Policy SPP Research
Papers, 7(11), 1-38. Retrieved from https://www.policyschool.ca/wp-content/uploads/2016/03/ontario-health-care-
reform.pdf
Van Walraven, C., Oake, N., Jennings, A., & Forster, A. J. (2010). The association between continuity of care and outcomes:
a systematic and critical review. Journal of Evaluation in Clinical Practice, 16(5), 947956. Retrieved from http://online
library.wiley.com/doi/10.1111/j.1365-2753.2009.01235.x/abstract;jsessionid=572E556D9ACBF748E6E65F11440D0365.
f02t02
University of Ottawa. (2016). Primary Care: Definitions and Historical Developments. Retrieved from http://www.med.
uottawa.ca/sim/data/Primary_Care.htm
World Health Organization. (1978). Declaration of Alma-Ata. International Conference on Primary Health Care, Alma-Ata,
U.S.S.R. Retrieved from www.who.int/hpr/NPH/docs/declaration_almaata.pdf
17 Doctors Nova Scotia | 2017 PRIMARY CARE POSITION
You might also like
- The Process Manifesto: Improving Healthcare in a Complex WorldFrom EverandThe Process Manifesto: Improving Healthcare in a Complex WorldNo ratings yet
- The Patient Priority: Solve Health Care's Value Crisis by Measuring and Delivering Outcomes That Matter to PatientsFrom EverandThe Patient Priority: Solve Health Care's Value Crisis by Measuring and Delivering Outcomes That Matter to PatientsNo ratings yet
- Medical Ethics: A Physician's Guide to Clinical MedicineFrom EverandMedical Ethics: A Physician's Guide to Clinical MedicineNo ratings yet
- ProvenCare: How to Deliver Value-Based Healthcare the Geisinger WayFrom EverandProvenCare: How to Deliver Value-Based Healthcare the Geisinger WayNo ratings yet
- Hospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsFrom EverandHospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsNo ratings yet
- Ethical Diversity in Healthcare Delivery: Ethics in Healthcare & BeyondFrom EverandEthical Diversity in Healthcare Delivery: Ethics in Healthcare & BeyondNo ratings yet
- Guide to Medical Education in the Teaching Hospital - 5th EditionFrom EverandGuide to Medical Education in the Teaching Hospital - 5th EditionNo ratings yet
- A Maternal and Child's Nurses Quest Towards ExcellenceDocument78 pagesA Maternal and Child's Nurses Quest Towards Excellencedecsag06No ratings yet
- ETT SUCTION DEWASA ACI14 - Suction - 2-2 PDFDocument46 pagesETT SUCTION DEWASA ACI14 - Suction - 2-2 PDFAde Rahmah YuliaNo ratings yet
- One Body-One Life: Health Screening Disease Prevention Personal Health Record Leading Causes of DeathFrom EverandOne Body-One Life: Health Screening Disease Prevention Personal Health Record Leading Causes of DeathNo ratings yet
- Aging Well: Solutions to the Most Pressing Global Challenges of AgingFrom EverandAging Well: Solutions to the Most Pressing Global Challenges of AgingNo ratings yet
- National Guidelines For The Use of Complementary Therapies in Supportive and Palliative CareDocument112 pagesNational Guidelines For The Use of Complementary Therapies in Supportive and Palliative Caredorothywyn50% (2)
- Called to Care: A Medical Provider's Guide for Humanizing HealthcareFrom EverandCalled to Care: A Medical Provider's Guide for Humanizing HealthcareNo ratings yet
- ACI14 Suction 2 2 DikonversiDocument46 pagesACI14 Suction 2 2 DikonversiMelika Azzahra INo ratings yet
- Reigniting the Human Connection: A Pathway to Diversity, Equity, and Inclusion in HealthcareFrom EverandReigniting the Human Connection: A Pathway to Diversity, Equity, and Inclusion in HealthcareNo ratings yet
- Clinical Practice Guidelines For Quality Palliative Care (National Consensus Project)Document76 pagesClinical Practice Guidelines For Quality Palliative Care (National Consensus Project)NCP86% (7)
- TeamworkDocument37 pagesTeamworkNurnadia OmerNo ratings yet
- A Practical Guide to Palliative Care in Paediatrics: Paediatric Palliative Care for Health ProfessionalsFrom EverandA Practical Guide to Palliative Care in Paediatrics: Paediatric Palliative Care for Health ProfessionalsNo ratings yet
- India's Public Health Care Delivery: Policies for Universal Health CareFrom EverandIndia's Public Health Care Delivery: Policies for Universal Health CareNo ratings yet
- A Practical Guide to Palliative Care in PaediatricsFrom EverandA Practical Guide to Palliative Care in PaediatricsRating: 5 out of 5 stars5/5 (1)
- Wonca 270917Document30 pagesWonca 270917yusuf awaluddinNo ratings yet
- CP Cholecystitis With Cholethiasis, Mild Dehydration CAPDocument181 pagesCP Cholecystitis With Cholethiasis, Mild Dehydration CAPArianna Jasmine MabungaNo ratings yet
- 358-2686264-ED-C - Job Description and Person Specification - PHEM 2020Document14 pages358-2686264-ED-C - Job Description and Person Specification - PHEM 2020Daniyal AzmatNo ratings yet
- Advances in Critical Care Pediatric Nephrology: Point of Care Ultrasound and DiagnosticsFrom EverandAdvances in Critical Care Pediatric Nephrology: Point of Care Ultrasound and DiagnosticsSidharth Kumar SethiNo ratings yet
- The Evidence Based Fundamentals of Health Care ChaplaincyFrom EverandThe Evidence Based Fundamentals of Health Care ChaplaincyNo ratings yet
- Obstetric and Gynecologic Nephrology: Women’s Health Issues in the Patient With Kidney DiseaseFrom EverandObstetric and Gynecologic Nephrology: Women’s Health Issues in the Patient With Kidney DiseaseMala SachdevaNo ratings yet
- DEAN Foundation - Corporate Brochure 2021Document12 pagesDEAN Foundation - Corporate Brochure 2021Logeswari KumarNo ratings yet
- Gastrointestinal and Liver Disorders in Women’s Health: A Point of Care Clinical GuideFrom EverandGastrointestinal and Liver Disorders in Women’s Health: A Point of Care Clinical GuidePoonam Beniwal-PatelNo ratings yet
- Non-Invasive Ventilation Guidelines For Adult Patients With Acute Respiratory FailureDocument44 pagesNon-Invasive Ventilation Guidelines For Adult Patients With Acute Respiratory Failureganda gandaNo ratings yet
- Leadership Behaviors of Frontline Staff NursesDocument9 pagesLeadership Behaviors of Frontline Staff NursessatmayaniNo ratings yet
- Making Patient-Centered Care Come Alive: Achieving Full Integration of The Patient's PerspectiveDocument9 pagesMaking Patient-Centered Care Come Alive: Achieving Full Integration of The Patient's PerspectiveBrooke RoseNo ratings yet
- Spiritual Healing in Hospitals and Clinics: Scientific Evidence that Energy Medicine Promotes Speedy Recovery and Positive OutcomesFrom EverandSpiritual Healing in Hospitals and Clinics: Scientific Evidence that Energy Medicine Promotes Speedy Recovery and Positive OutcomesRating: 1 out of 5 stars1/5 (1)
- Knowledge For Graduate Practice 527197: Chronic ConditionsDocument36 pagesKnowledge For Graduate Practice 527197: Chronic ConditionsSofia Krylova-SmithNo ratings yet
- Changing For The Health Of It: A Simple and Sensible Guide To Heart-Healthy Diet and ExerciseFrom EverandChanging For The Health Of It: A Simple and Sensible Guide To Heart-Healthy Diet and ExerciseNo ratings yet
- Nurse Practitioner: NwkkwkkekdDocument15 pagesNurse Practitioner: Nwkkwkkekdxhuana temaNo ratings yet
- The Art and Science of Physician Wellbeing: A Handbook for Physicians and TraineesFrom EverandThe Art and Science of Physician Wellbeing: A Handbook for Physicians and TraineesNo ratings yet
- Kidney Disease Management: A Practical Approach for the Non-Specialist Healthcare PractitionerFrom EverandKidney Disease Management: A Practical Approach for the Non-Specialist Healthcare PractitionerNo ratings yet
- Guideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementDocument26 pagesGuideline No. 426: Hypertensive Disorders of Pregnancy: Diagnosis, Prediction, Prevention, and ManagementYo Me100% (1)
- Gerontological Nursing: Scope and Standards of Practice, 2nd EditionFrom EverandGerontological Nursing: Scope and Standards of Practice, 2nd EditionNo ratings yet
- ACI Physical Activity Movement Guideline Critically Ill AdultsDocument44 pagesACI Physical Activity Movement Guideline Critically Ill AdultsAsmaa GamalNo ratings yet
- Age-Friendly Health Systems: A Guide to Using the 4Ms While Caring for Older AdultsFrom EverandAge-Friendly Health Systems: A Guide to Using the 4Ms While Caring for Older AdultsNo ratings yet
- Vitamedicine: Foundations for Optimising Health and WellbeingFrom EverandVitamedicine: Foundations for Optimising Health and WellbeingNo ratings yet
- Overcoming Selective Blindness: Improving Services from the Bedside to the Boardroom and BeyondFrom EverandOvercoming Selective Blindness: Improving Services from the Bedside to the Boardroom and BeyondNo ratings yet
- Critical Care for Anorexia Nervosa: The MARSIPAN Guidelines in PracticeFrom EverandCritical Care for Anorexia Nervosa: The MARSIPAN Guidelines in PracticeNo ratings yet
- Public Health Nursing: Scope and Standards of PracticeFrom EverandPublic Health Nursing: Scope and Standards of PracticeRating: 5 out of 5 stars5/5 (1)
- Physician Engagement PositionDocument6 pagesPhysician Engagement PositionTyler McLean100% (1)
- 20170719, Media Release, J. Armand Bombardier Foundation Establishes New Scholarship For Lakehead University Business StudentsDocument3 pages20170719, Media Release, J. Armand Bombardier Foundation Establishes New Scholarship For Lakehead University Business StudentsTyler McLeanNo ratings yet
- Chill Affiliate With Richmond Hill Press ReleaseDocument2 pagesChill Affiliate With Richmond Hill Press ReleaseTyler McLeanNo ratings yet
- Chill Affiliate With Richmond Hill Press ReleaseDocument2 pagesChill Affiliate With Richmond Hill Press ReleaseTyler McLeanNo ratings yet
- Fact Sheet Pre-Primary EnglishDocument1 pageFact Sheet Pre-Primary EnglishTyler McLeanNo ratings yet
- High School Scholarship 2017 Winners AnnouncementDocument1 pageHigh School Scholarship 2017 Winners AnnouncementTyler McLeanNo ratings yet
- RCMP Quarterly Report 2016 Quarter 4Document18 pagesRCMP Quarterly Report 2016 Quarter 4Tyler McLeanNo ratings yet
- Media Release - Thunder Bay Fire Rescue Starts Home Fire Safety ProgramDocument1 pageMedia Release - Thunder Bay Fire Rescue Starts Home Fire Safety ProgramTyler McLeanNo ratings yet
- CBSA News Release - Three Firearms Seized at Ports of Entry in Northwestern OntarioDocument2 pagesCBSA News Release - Three Firearms Seized at Ports of Entry in Northwestern OntarioTyler McLeanNo ratings yet
- OCC Skills Mismatch Report 2017Document1 pageOCC Skills Mismatch Report 2017Tyler McLeanNo ratings yet
- Sisson Mines ProjectDocument1 pageSisson Mines ProjectTyler McLeanNo ratings yet
- Media Release - Canada Research ChairsDocument3 pagesMedia Release - Canada Research ChairsTyler McLeanNo ratings yet
- Media Release - Strong Budgetary Performance Raises City's Credit RatingDocument1 pageMedia Release - Strong Budgetary Performance Raises City's Credit RatingTyler McLeanNo ratings yet
- Moncton Housing Needs StudyDocument4 pagesMoncton Housing Needs StudyTyler McLeanNo ratings yet
- 2017-2018 District CalendarDocument1 page2017-2018 District CalendarTyler McLeanNo ratings yet
- Media Release - Thunder Bay Dining in The Dark in Support of CNIBDocument1 pageMedia Release - Thunder Bay Dining in The Dark in Support of CNIBTyler McLeanNo ratings yet
- Scanned From A Xerox Multifunction PrinterDocument1 pageScanned From A Xerox Multifunction PrinterTyler McLeanNo ratings yet
- PDFDocument1 pagePDFTyler McLeanNo ratings yet
- 2017-06-19 - FINAL REPORT - Transportation Dispersal PlanDocument24 pages2017-06-19 - FINAL REPORT - Transportation Dispersal PlanTyler McLeanNo ratings yet
- PDFDocument1 pagePDFTyler McLeanNo ratings yet
- Scanned From A Xerox Multifunction PrinterDocument1 pageScanned From A Xerox Multifunction PrinterTyler McLeanNo ratings yet
- DAHC Final Report May 8, 2017Document33 pagesDAHC Final Report May 8, 2017Tyler McLeanNo ratings yet
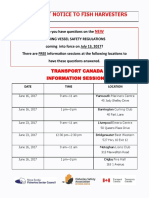
- TC Info SessionDocument1 pageTC Info SessionTyler McLeanNo ratings yet
- Moncton City Council Agenda June 5th, 2017Document3 pagesMoncton City Council Agenda June 5th, 2017Tyler McLeanNo ratings yet
- DAHC Final Report May 8, 2017Document33 pagesDAHC Final Report May 8, 2017Tyler McLeanNo ratings yet
- Early Vote WebDocument1 pageEarly Vote WebTyler McLeanNo ratings yet
- Downtown Centre May UpdateDocument1 pageDowntown Centre May UpdateTyler McLeanNo ratings yet
- DAHC Final Report May 8, 2017Document33 pagesDAHC Final Report May 8, 2017Tyler McLeanNo ratings yet
- DAHC Final Report May 8, 2017Document33 pagesDAHC Final Report May 8, 2017Tyler McLeanNo ratings yet
- NR Begg Keeash May 17, 2017Document2 pagesNR Begg Keeash May 17, 2017Tyler McLeanNo ratings yet
- Media Release - River Safety Audits Being ConductedDocument1 pageMedia Release - River Safety Audits Being ConductedTyler McLeanNo ratings yet
- Full Download Ebook PDF Introductory Econometrics A Modern Approach 7th Edition by Jeffrey PDFDocument42 pagesFull Download Ebook PDF Introductory Econometrics A Modern Approach 7th Edition by Jeffrey PDFtimothy.mees27497% (39)
- TRAVEL POLICY CARLO URRIZA OLIVAR Standard Insurance Co. Inc - Travel Protect - Print CertificateDocument4 pagesTRAVEL POLICY CARLO URRIZA OLIVAR Standard Insurance Co. Inc - Travel Protect - Print CertificateCarlo OlivarNo ratings yet
- Quiz 2 I - Prefix and Suffix TestDocument10 pagesQuiz 2 I - Prefix and Suffix Testguait9No ratings yet
- WellaPlex Technical 2017Document2 pagesWellaPlex Technical 2017Rinita BhattacharyaNo ratings yet
- Edtpa Lesson 3Document3 pagesEdtpa Lesson 3api-299319227No ratings yet
- Mini Project A-9-1Document12 pagesMini Project A-9-1santhoshrao19No ratings yet
- Subject: PSCP (15-10-19) : Syllabus ContentDocument4 pagesSubject: PSCP (15-10-19) : Syllabus ContentNikunjBhattNo ratings yet
- MPPSC ACF Test Paper 8 (26 - 06 - 2022)Document6 pagesMPPSC ACF Test Paper 8 (26 - 06 - 2022)Hari Harul VullangiNo ratings yet
- Walton Finance Way Strategy (MO)Document12 pagesWalton Finance Way Strategy (MO)AshokNo ratings yet
- B.e.eeeDocument76 pagesB.e.eeeGOPINATH.MNo ratings yet
- Verilog GATE AND DATA FLOWDocument64 pagesVerilog GATE AND DATA FLOWPRIYA MISHRANo ratings yet
- Chandigarh Distilers N BotlersDocument3 pagesChandigarh Distilers N BotlersNipun GargNo ratings yet
- Newsela Teacher Review - Common Sense EducationDocument1 pageNewsela Teacher Review - Common Sense EducationJessicaNo ratings yet
- Master Data FileDocument58 pagesMaster Data Fileinfo.glcom5161No ratings yet
- 5000-5020 en PDFDocument10 pages5000-5020 en PDFRodrigo SandovalNo ratings yet
- 6 RVFS - SWBL Ojt Evaluation FormDocument3 pages6 RVFS - SWBL Ojt Evaluation FormRoy SumugatNo ratings yet
- Hydrogen Production by Steam ReformingDocument10 pagesHydrogen Production by Steam ReformingramiarenasNo ratings yet
- Retailing PPT (Shailwi Nitish)Document14 pagesRetailing PPT (Shailwi Nitish)vinit PatidarNo ratings yet
- 2021-01-01 - Project (Construction) - One TemplateDocument1,699 pages2021-01-01 - Project (Construction) - One TemplatemayalogamNo ratings yet
- Approved College List: Select University Select College Type Select MediumDocument3 pagesApproved College List: Select University Select College Type Select MediumDinesh GadkariNo ratings yet
- One and Half SindromeDocument4 pagesOne and Half SindromeYulia DamayantiNo ratings yet
- Routine Maintenance For External Water Tank Pump and Circulation Pump On FID Tower and Rack 2017-014Document5 pagesRoutine Maintenance For External Water Tank Pump and Circulation Pump On FID Tower and Rack 2017-014CONVIERTE PDF JPG WORDNo ratings yet
- (QII-L2) Decorate and Present Pastry ProductsDocument30 pages(QII-L2) Decorate and Present Pastry ProductsLD 07100% (1)
- OMM 618 Final PaperDocument14 pagesOMM 618 Final PaperTerri Mumma100% (1)
- Frequently Asked Questions: Lecture 7 To 9 Hydraulic PumpsDocument5 pagesFrequently Asked Questions: Lecture 7 To 9 Hydraulic PumpsJatadhara GSNo ratings yet
- Merging Shapes - 10 Minutes To Better Painting - Episode 1Document12 pagesMerging Shapes - 10 Minutes To Better Painting - Episode 1Nguyên HàNo ratings yet
- Course: Introduction To Geomatics (GLS411) Group Practical (2-3 Persons in A Group) Practical #3: Principle and Operation of A LevelDocument3 pagesCourse: Introduction To Geomatics (GLS411) Group Practical (2-3 Persons in A Group) Practical #3: Principle and Operation of A LevelalyafarzanaNo ratings yet
- Crusader Castle Al-Karak Jordan Levant Pagan Fulk, King of Jerusalem MoabDocument3 pagesCrusader Castle Al-Karak Jordan Levant Pagan Fulk, King of Jerusalem MoabErika CalistroNo ratings yet
- Deloitte - Introduction To TS&A - CloudDocument2 pagesDeloitte - Introduction To TS&A - Cloudsatyam100% (1)
- Jaiib QpapersDocument250 pagesJaiib Qpapersjaya htNo ratings yet