Professional Documents
Culture Documents
8 PATHO6 - Cerebrovascular Disease 2015B
Uploaded by
Miguel Cuevas DolotOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
8 PATHO6 - Cerebrovascular Disease 2015B
Uploaded by
Miguel Cuevas DolotCopyright:
Available Formats
6.8.
2 CEREBROVASCULAR DISEASES
Dr. Tilbe
CEREBROVASCULAR DISEASE
Any abnormality of the brain due to an underlying
pathology in the blood vessels
Impaired blood supply
rapidly developing loss of brain function.
Clinically present as "Stroke or CVA (cerebrovascular
accident)
STROKE
Medical emergency and can cause permanent neurological
damage, complications, and death.
Leading cause of adult disability in the US, Europe and Figure 2: Embolism may cause obstruction of CNS vessels resulting to
even in the Philippines. death of brain tissue due to lack of blood supply.
No. 2 cause of death worldwide
CEREBRAL BLOOD FLOW
TWO UNDERLYING PATHOLOGIC PROCESSES
CBF delivers a constant supply of glucose and oxygen
RESPONSIBLE FOR STROKE:
1) Impairment of blood supply of CNS tissue Brain:
hypoxia, ischemia, and infarction 1- 2% of BW,
2) Rupture of CNS vessels hemorrhage Receives 15% of the resting CO
Accounts for 20% of the total body O2
Impaired blood supply and hemorrhage will lead to consumption.
ischemia (lack of glucose and oxygen supply) Normal CBF: about 50 mL/ minute for each 100 gm of
Affected area is unable to function, leading to tissue
hemiplegia and other neurologic deficits
regional variations between white and gray matter
and among different portions of the gray matter
COMMON CEREBROVASCULAR DISORDERS:
1) Thrombosis CBF remains constant over a wide range of BP and ICP
2) Embolism Ischemic stroke because of auto-regulation of vascular resistance.
3) Intraparenchymal Causes of decreased oxygen to the brain:
hemorrhage due to HPN A low partial pressure of oxygen (pO2) (functional
4) Subarachnoid Hemorrhagic hypoxia),
hemorrhage secondary to stroke Impaired oxygen-carrying capacity of the blood,
ruptured aneurysm inhibition of oxygen use by tissue
Ischemia after interruption of the normal blood flow.
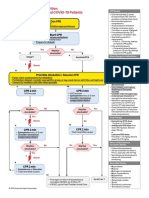
A. Ischemic Stroke is due to a reduction of blood flow most
Special responses to ischemia in the CNS.
commonly due to occlusion (an obstruction) brought
Excitatory amino acid neurotransmitters (e.g. Glutamate)
about by thrombosis or embolism.
released overstimulates and result in persistent opening
B. Hemorrhagic stroke (or intracranial hemorrhage) of specific membrane channels including N-methyl-D-
due to rupture of blood vessel in the brain aspartate and kainate receptors.
spilling blood into the spaces surrounding the Cell death results from
brain cells 1) Uncontrolled influx of calcium ions or
due to rupture of cerebral aneurysm 2) Toxic effects of nitrous oxide
The mortality and long-term morbidity prognosis is
generally worse for hemorrhagic strokes than for
ischemic strokes.
Figure 1: Two processes in CVS: (1) Hypoxia, ischemia and infarction
resulting from impairment of blood supply and oxygenation if CNS
tissue. (2) Hemorrhage resulting from rupture of CNS vessels.
Figure 3: This diagram shows how the CNS responds to ischemia.
Mattus Medina Pamintuan Panday Parabuac Rejante Page 1 of 6
TWO TYPES OF ACUTE ISCHEMIC INJURY
A. GLOBAL CEREBRAL ISCHEMIA
Due to severe hypotensive episode leading to a
generalized reduction of cerebral perfusion (cardiac arrest,
shock, and severe hypotension.)
Clinical outcome: Diffuse hypoxic/ischemic
encephalopathy:
o Mild cases: no irreversible tissue damage
Eventual complete recovery
o Severe cases: can result in irreversible damage to
CNS tissue.
Occur in parts of the brain that lie at the boundary Figure 6: Gross picture of global cerebral ischemia. Brain is
between zones of arterial distribution from different swollen. Gyri are widened, and the sulci are narrowed. Poor
arteries. demarcation between gray and white matter.
Normally, border zones are hypoperfused because they
are the last to receive blood from main arterial trunk. Microscopic Findings:
With hypotension watershed areas are more Mild global ischemia : neurons(most sensitive
susceptible to damage than other areas of the brain. cells ) are affected first
Severe global cerebral ischemia: widespread
PATHOLOGIC CONSEQUENCES:
neuronal death
Focal neuronal death that follows pattern of
selective vulnerability. Preferentially affects B. FOCAL CEREBRAL ISCHEMIA/INFARCTION
Sommer Sector of Hippocampus and Purkinje cells Due to reduction or cessation of blood flow to a localized
Watershed infarcts area of the brain
Laminar necrosis Focal ischemia: obstruction of local blood supplies not
enough to cause necrosis.
Infarction: tissue necrosis due to sustained, obstruction
of local blood supply (further discussed below);
CAUSES:
a) Large-vessel disease (such as embolic or
thrombotic arterial occlusion)
i. Thrombotic Arterial Occlusion - causes
bland/white type of infarct
ii. Embolic Arterial Occlusion - causes
hemorrhagic type of infarct
b) Small-vessel disease (such as vasculitis or
occlusion secondary to arteriosclerotic lesions seen
in HPN)
CEREBRAL INFARCTS
Focal brain necrosis due to complete and prolonged
ischemia that affects all tissue elements
Figure 4: Bilaterally symmetric dark discolored areas (superior
and just lateral to the midline) representing recent infarction in CAUSES:
the watershed zone (overlapping area) supplied by ACA and A. THROMBOTIC INFARCTS
MCA circulation Are due to atherosclerosis
The most common sites:
CORTICAL LAMINAR NECROSIS Carotid bifurcation,
A specific type of cortical infarction, which the origin of the middle cerebral artery,
usually develops as a result of generalized either end of the basilar artery.
ischemia Frequently associated with hypertension and diabetes.
Typically affects the deep layers of the cerebral
cortex (area receiving blood from blood vessels
entering the cortex from the surface of the brain
(short penetrators)
Figure 7: Majority of thrombotic occlusions is due to atherosclerosis.
Figure 5: Gross picture of laminar necrosis. The gray matter
has six layers. The third layer is the most vulnerable to
depletion of oxygen and glucose.
Mattus Medina Pamintuan Panday Parabuac Rejante Page 2 of 6
Due arteriolar sclerosis (due to HPN) of
deep penetrating arterioles of Basal
ganglia and brainstem.
Maybe clinically silent or cause severe
neurologic impairment depending on
location.
Figure 8: Progressive narrowing of the lumen may be accompanied Figure 10: Lakelike spaces (<15 mm), in the lenticular nucleus,
by embolization resulting to obstruction = stroke. thalamus, internal capsule, deep white matter, caudate
nucleus, and pons.
Figure 9: Thrombosis of the internal carotid artery (black
arrow). .
Figure 11: Cystic spaces from resolved liquefactive necrosis
B. EMBOLIC INFARCTS with scattered fat-laden macrophages and surrounding gliosis.
Embolism is the most frequent cause of ischemic
infarction. D. OTHER CAUSES OF ARTERIAL OCCLUSION AND
Embolic infarcts have an abrupt onset. INFARCTION
Origin: 1. Vasculitis
1) Cardiac mural thrombi are the most common o Inflammation of blood vessels luminal narrowing
sources. Predisposing factors: MI, valvular disease, infarcts
and AF. o Examples: PAN, giant cell (temporal) arteritis,
2) Thromboemboli arising in arteries, most often granulomatous arteritis, SLE, infectious vasculitis
originating over atheromatous plaques within the (pyogenic meningitis, tuberculous meningitis, CNS
carotid arteries. syphilis, fungal vasculitis); primary angitis of CNS
3) Other sources: Emboli of other material (tumor,
fat, or air). INFARCT: CLINICAL FEATURES
Clinical presentation depends on location and size of infarct.
C. SMALL VESSEL DISEASE Maybe asymptomatic
Primarily seen in HPN and DM Develops a hemiplegia, a sensory deficit,
Also known as: blindness, aphasia, or some other deficits
"small artery arteriosclerosis", Outcome:
"hyaline arteriolosclerosis Maybe fatal
"lipohyalinosis". May show slow improvement during a period of
Pathogenesis: months.
HPN: endothelial injury and leakage of plasma
proteins in and around vessels; INFARCTS: CLINICAL FINDINGS
DM: glycation of pr- and diffuse BM Embolic infarcts: abrupt onset
thickening. Atherothrombotic infarcts:
Vessels walls thicken, becomes Evolve over a period of time, usually hours.
homogenous and hyalinized Often preceded by transient ischemic attacks
Lumen becomes narrowed (TIAs).
Vessels become tortous TIA (focal neurological deficit that lasts less
Outcome: than 24 hours and resolves) - due to
SMALL INFARCTS (LACUNAR INFARCTS) temporary decrease of perfusion impairs
which affects small penetrating arteries and neurological function but not enough to cause
arterioles that supply the BG, thalamus, deep permanent damage (probably due to lysis of
white matter, and the BS emboli soon after occlusion)
Account for about 20% of all strokes.
Single or multiple, small, cavitary infarcts
Mattus Medina Pamintuan Panday Parabuac Rejante Page 3 of 6
An infarct has: 10 days to 3 weeks:
Central core of total ischemia and necrosis tissue liquefies, eventually leaving a fluid-filled
(irreversible). cavity lined by dark gray tissue
Ischemic penumbra: A zone of borderline ischemic
tissue surrounding the central core (reversible)
Window of opportunity for salvaging the
penumbra is very short therefore an ischemic
stroke is an emergency.
If within 3 hours adequate blood supply is not
restored necrosis extends to the penumbra.
Restoration of perfusion in the penumbra and
then to resorption of cerebral edema recovery
of function, after an infarct
TWO TYPES OF INFARCTS: Figure 14: Intermediate infarct of the frontal lobe: liquefactive
A. Hemorrhagic (red) infarction necrosis with formation of cystic spaces as resolution begins.
Multiple, sometimes confluent, petechial
hemorrhages
INFARCTION: MICROSCOPIC FEATURES
Hemorrhage is probably secondary to reperfusion
1. Early changes (12 to 24 hours after the insult)
of damaged vessels and tissue either via collaterals
Acute neuronal cell change (red neurons)
or direct clot dissolution.
Microvacuolization eosinophilia of the
neuronal cytoplasm nuclear pyknosis and
karyorrhexis
Neutrophilic emigration progressively increases
then decreases
Figure 15: Acute ischemic injury: diffuse eosinophilia of
neurons, which are beginning to shrink.
Figure 12: Hemorrhagic Infarct: edematous infarcted tissue
produces a mass effect decrease in size of the left ventricle
with shift of the midline. Arterial embolus often leads to a
hemorrhagic appearance.
B. Non-hemorrhagic (pale, bland, anemic) infarcts
usually associated with thrombosis
Figure 16: Infiltration of a cerebral infarct by neutrophils
begins at the edges of the lesion
2. Subacute changes (24 hours to 2 weeks)
Necrosis of tissue, influx of macrophages, vascular
proliferation, and reactive gliosis
Figure 13: A bland infarct with punctate hemorrhages, Phagocytic cells (circulating monocytes and activated
consistent with ischemia-reperfusion injury microglia) are seen at 48 hours and become the
predominant cell type in the next 2 to 3 weeks.
GROSS (Non-hemorrhagic infarct): 3. Repair (after 2 weeks)
Macrophages (peak reaction: 3-4 weeks) stuffed with
1st 6 hours of irreversible injury:
the products of myelin breakdown or blood may
minimal change
persist for months to years.
48 hours: Removal of all necrotic tissue loss of normally
the tissue becomes pale, soft, and swollen, and organized CNS structure Astrocytes from the
the corticomedullary junction becomes indistinct. surrounding undamaged brain proliferate and form a
2 to 10 days glial scar around the infarct (completed in approximately
brain becomes gelatinous and friable 2 months).
Mattus Medina Pamintuan Panday Parabuac Rejante Page 4 of 6
Histo: Focal tissue destruction, pigment-laden
macrophages, and gliosis.
HYPERTENSIVE INTRAPARENCHYMAL HEMORRHAGE
Putamen (50% to 60% of cases)
Thalamus, pons, cerebellar hemispheres (rarely), and
other regions of the brain .
Early lesion:
- Central core of clotted blood surrounded by a
rim of edematous brain tissue showing anoxic
neuronal and glial changes
Later lesion:
- Pigment and lipid-laden macrophages with
proliferated reactive astrocytes at the periphery
Figure 17: Resolution of the liquefactive necrosis in a cerebral
of clot.
infarction leads to the formation of a cystic space.
Clinical Features:
o Clinical symptoms depend on location and size
of the bleed
Large portions of the brain affected with
involvement of the ventricular system >>
fatal
Maybe clinically silent
May produce neurologic deficits
o Hemorrhage may gradually resolve over weeks or
months.
Figure 18: Cystic infarct showing destruction of the cortex with
cavitation.
HEMORRHAGIC STROKES
Accounts for 15% to 20% of strokes
Due to rupture of blood vessels with intracerebral or
subarachnoid hemorrhage. Figure 19: Massive hypertensive hemorrhage rupturing into a
3 major causes of hemorrhagic strokes are lateral ventricle.
1. Hypertensive bleed
2. Ruptured arterial aneurysms SUBARACHNOID HEMORRHAGE
3. Arteriovenous malformations
Common cause of hemorrhagic stroke
Most common cause: rupture of a saccular (berry)
INTRACEREBRAL (INTRAPARENCHYMAL)
aneurysm.
HEMORRHAGE
Other causes:
Spontaneous (nontraumatic) intraparenchymal - Extension of a traumatic hematoma
hemorrhages - Rupture of a hypertensive intracerebral
Most common cause of hemorrhage in middle to late hemorrhage into the ventricular system,
adult life - Vascular malformation,
Most are caused by rupture of a small intraparenchymal - Hematologic disturbances
vessel - Tumors
Hypertension : the most common underlying cause PATHOGENESIS OF SACCULAR ANEURYSMS
((Hypertensive Bleed) - Etiology: unknown.
- Accounts for more than 50% of clinically significant - Majority occur sporadically
hemorrhages - Genetic factors may play a role in their
Due to HPN induced vessel wall abnormalities: pathogenesis.
Hyaline arteriolosclerosis in small vessels - Predisposing factors:
Proliferative changes and frank necrosis of Cigarette smoking
arterioles HPN
Lipohyalinosis promoting the development of - Basic underlying defect: defect in the media of the
rupture prone Charcot-Burhard aneurysms vessel (maybe present since birth)
CHARCOT-BOUCHARD MICROANEURYSMS
o Minute aneurysms, which are prone to rupture seen in
patients with chronic HPN.
o CB aneurysms, occur in vessels that are less than 300 m
in diameter
o Most common within the basal ganglia.
HPN: SLIT HEMORRHAGES
Slit-like cavity (slit hemorrhages) surrounded by brownish
discoloration upon resorption
Due to rupture of the small-caliber penetrating vessels Figure 19: Common sites of saccular aneurysm in the
damaged by HPN.
circle of willis.
Mattus Medina Pamintuan Panday Parabuac Rejante Page 5 of 6
Figure 20: Berry aneurysm: Outpouchings (few mm - 3cm in
diameter) at an arterial branch point along the circle of Willis. Figure 22: Vascular malformation: dilated, tortuous, worm-like
Have bright red shiny surface and a thin translucent wall. The blood vessels separated by gliotic tissue
wall or lumen may contain atheromatous plaques, calcification,
or thrombus. CEREBRAL EDEMA
Caused by the release of osmotically active substances
SAH: Clinical Features: (arachidonic acid, electrolytes, lactic acid) from the
- Most frequent in the 5th decade necrotic brain tissue
- Slightly more frequent in females Vascular injury and leakage of proteins in the interstitial
- Aneurysms > 10 mm in diameter: 50% risk of bleeding space aggravates edema
per year. By 3-4 days (most dangerous period for large infarct)
- 1/3 cases it is associated with acute increases in interstitial fluid accumulates in the infarct and around it.
intracranial pressure, such as with straining at stool or Increase tissue volume ( edema or hemorrhage)
sexual orgasm. increase pressure inside fixed capacity of skull damage
- Sx: sudden, excruciating headache, then rapidly lose to brain by:
consciousness. Decreasing perfusion
Displace tissue across dural barriers or through
Complications of SAH: openings (herniation)
1) Acute events ( hours to days)
Vasospasm increased risk of further
damage
2) Late sequelae
Meningeal fibrosis and scarring can lead
obstruction of CSF flow.
ARTERIOVENOUS MALFORMATION
Most common type of vascular malformation.
M:F ratio 2:1
Clinically presents between the ages of 10 and 30 years as:
Seizure disorder
Intracerebral hemorrhage
Subarachnoid hemorrhage
Most common site: territory of the MCA, particularly its Figure 23: Swelling of the left cerebral hemisphere a shift
posterior branches with herniation of the uncus of the hippocampus through the
Developmental abnormalities of cerebral vessels. Tangle tentorium uncal grooving (white arrow.)
of abnormal vessels interposed between a feeding artery
and a draining vein.
Chronic compression ischemia of brain tissue
seizures and neurologic deficits
HISTO: Greatly enlarged blood vessels separated by
gliotic tissue
Figure 24: Acute cerebral swelling producing herniation of the
cerebelllar tonsils into the foramen magnum.
Figure 21: GROSS morphology - tangled network of wormlike Acute brain swelling in the closed cranial cavity is serious
irregular, tortuous vessels with prominent, pulsatile can be fatal. Cause of death from a massive hemispheric
arteriovenous shunt. infarct:
Cerebral edema and herniations
--- End---
Mattus Medina Pamintuan Panday Parabuac Rejante Page 6 of 6
You might also like
- PSB 368Document6 pagesPSB 368Miguel Cuevas DolotNo ratings yet
- Effectiveness of Transdermal MagnesiumDocument2 pagesEffectiveness of Transdermal MagnesiumMiguel Cuevas Dolot100% (1)
- (MED) COVID-19 Trans V. 2.0Document6 pages(MED) COVID-19 Trans V. 2.0Isabel VinasNo ratings yet
- How Can Patients Visitors Help - May18Document2 pagesHow Can Patients Visitors Help - May18Miguel Cuevas DolotNo ratings yet
- ACLS Cardiac Arrest Algorithm For Suspected or Confirmed COVID-19 PatientsDocument1 pageACLS Cardiac Arrest Algorithm For Suspected or Confirmed COVID-19 PatientsMariuxi Tatiana ChocoNo ratings yet
- Covid 19 CPR 7 RulesDocument21 pagesCovid 19 CPR 7 RulesMiguel Cuevas DolotNo ratings yet
- Covid 19 CPR 7 RulesDocument21 pagesCovid 19 CPR 7 RulesMiguel Cuevas DolotNo ratings yet
- Clinical Examination of The Ear, Nose and Throat: Dave Pothier ST Mary's 2003Document30 pagesClinical Examination of The Ear, Nose and Throat: Dave Pothier ST Mary's 2003Ekambaram TrmNo ratings yet
- Physical Examination in ENT: Ussana Promyothin, MDDocument60 pagesPhysical Examination in ENT: Ussana Promyothin, MDMiguel Cuevas DolotNo ratings yet
- Covid 19 PDFDocument18 pagesCovid 19 PDFMiguel Cuevas DolotNo ratings yet
- Physical Examination in ENT: Ussana Promyothin, MDDocument60 pagesPhysical Examination in ENT: Ussana Promyothin, MDMiguel Cuevas DolotNo ratings yet
- Physical Assessment: Ear, Nose, Mouth, and ThroatDocument59 pagesPhysical Assessment: Ear, Nose, Mouth, and ThroatMiguel Cuevas DolotNo ratings yet
- Vertigo Gail Ishiyama 1 13 10Document40 pagesVertigo Gail Ishiyama 1 13 10Myname Rama LienNo ratings yet
- Cook Book (Filipino) 13 PDFDocument23 pagesCook Book (Filipino) 13 PDFAdina AnghelNo ratings yet
- Clinical AbstractDocument4 pagesClinical AbstractMiguel Cuevas DolotNo ratings yet
- Pedia Tickler Update 2017Document2 pagesPedia Tickler Update 2017Tani BokNo ratings yet
- Active Listening HANDOUT PDFDocument26 pagesActive Listening HANDOUT PDFMiguel Cuevas DolotNo ratings yet
- A Case-Control Study of The Association of Diet and Obesity With Gout in Taiwan PDFDocument12 pagesA Case-Control Study of The Association of Diet and Obesity With Gout in Taiwan PDFMiguel Cuevas DolotNo ratings yet
- HEMAreviewDocument3 pagesHEMAreviewMiguel Cuevas DolotNo ratings yet
- Benign Paroxysmal Positional Vertigo: Waseem WatadDocument37 pagesBenign Paroxysmal Positional Vertigo: Waseem WatadnoviNo ratings yet
- A Case-Control Study of The Association of Diet and Obesity With Gout in Taiwan PDFDocument12 pagesA Case-Control Study of The Association of Diet and Obesity With Gout in Taiwan PDFMiguel Cuevas DolotNo ratings yet
- Drug IndexDocument2 pagesDrug IndexMiguel Cuevas DolotNo ratings yet
- Nocturnals Physiology 2018Document14 pagesNocturnals Physiology 2018Miguel Cuevas DolotNo ratings yet
- Neurologic ExamDocument1 pageNeurologic ExamMiguel Cuevas DolotNo ratings yet
- History Taking ExaminationDocument7 pagesHistory Taking ExaminationIndunil AnuruddhikaNo ratings yet
- Community-Acquired Pneumonia - CPG 2016Document26 pagesCommunity-Acquired Pneumonia - CPG 2016Jamie SebastianNo ratings yet
- TCVS - Cardiac Surgery Part 2 Dr. de AsisDocument8 pagesTCVS - Cardiac Surgery Part 2 Dr. de AsisMiguel Cuevas DolotNo ratings yet
- Anesthesia Pocket Cards 7 18 18Document6 pagesAnesthesia Pocket Cards 7 18 18Miguel Cuevas DolotNo ratings yet
- Kerosene PDFDocument31 pagesKerosene PDFRudyMLanaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Cristy Santos BOMDocument111 pagesCristy Santos BOMLito ObstaculoNo ratings yet
- Pediatrics Care Plan Kawasaki Disease Final Draft and CorrectedDocument9 pagesPediatrics Care Plan Kawasaki Disease Final Draft and CorrectedValencia Vickers50% (4)
- Austere Medicine Books PDFDocument10 pagesAustere Medicine Books PDFmorrischuck100% (1)
- The Black PlagueDocument3 pagesThe Black PlagueKevin MoralesNo ratings yet
- COVID-19: Simple Answers To Top Questions: Risk Communication Field Guide Questions and Key MessagesDocument128 pagesCOVID-19: Simple Answers To Top Questions: Risk Communication Field Guide Questions and Key MessagesJazzyNo ratings yet
- Cause & Effect - Louise Joseph G. PeraltaDocument4 pagesCause & Effect - Louise Joseph G. PeraltaLouise Joseph G. PeraltaNo ratings yet
- InTech-Molar Incisor Hypomineralization Morphological Aetiological Epidemiological and Clinical ConsiderationsDocument25 pagesInTech-Molar Incisor Hypomineralization Morphological Aetiological Epidemiological and Clinical ConsiderationsNeagu EmaNo ratings yet
- Chapter 2Document14 pagesChapter 2JM ElleNo ratings yet
- Child Attitude Joward Jllness Scale: EspaňDocument1 pageChild Attitude Joward Jllness Scale: EspaňAvinash ToraneNo ratings yet
- Dengue Lecture For SibalomDocument48 pagesDengue Lecture For SibalomCzerwin JualesNo ratings yet
- Domestic Rabbits Diseases and ParasitesDocument31 pagesDomestic Rabbits Diseases and ParasitesAlvaro Pauchard Pino100% (1)
- Diagnostic Terms For Pulp Conditions - JoE 2009Document13 pagesDiagnostic Terms For Pulp Conditions - JoE 2009Bicho Angel LisseaNo ratings yet
- Jurnal Case Report - Hemangioma KavernosaDocument12 pagesJurnal Case Report - Hemangioma KavernosaMaulida Ayu NorizaNo ratings yet
- Cocci VexDocument18 pagesCocci VexNona AlyNo ratings yet
- BMC Public Health: Which Preventive Measures Might Protect Health Care Workers From SARS?Document8 pagesBMC Public Health: Which Preventive Measures Might Protect Health Care Workers From SARS?Rahel YaserNo ratings yet
- Handbook of Disease Burdens and Quality of Life Measures - V. Preedy, R. Watson (Springer, 2010) WWDocument4,278 pagesHandbook of Disease Burdens and Quality of Life Measures - V. Preedy, R. Watson (Springer, 2010) WWRiska Indriani100% (1)
- Carcinogenesis: Robbins Basic Pathology, 7 Kumar, Cotran, RobbinsDocument29 pagesCarcinogenesis: Robbins Basic Pathology, 7 Kumar, Cotran, RobbinsHairon DhiyaulhaqNo ratings yet
- Navel DisplacementDocument4 pagesNavel Displacementdinesh100% (1)
- Parasites, How To Eliminate Them NaturallyDocument44 pagesParasites, How To Eliminate Them NaturallyXuxuxel100% (3)
- Catastrophic Health Expenditure of Middle Class in India Due To Covid-19Document3 pagesCatastrophic Health Expenditure of Middle Class in India Due To Covid-19Ashwini PoojaryNo ratings yet
- CKD (F&e)Document110 pagesCKD (F&e)Al-nazer Azer Al100% (1)
- Glomerular DiseaseDocument24 pagesGlomerular DiseasemadhuNo ratings yet
- Keilitis Eksfoliatif JurnalDocument7 pagesKeilitis Eksfoliatif JurnalLeni Aria NastaNo ratings yet
- ManiaaDocument3 pagesManiaaadityanarang147No ratings yet
- Jen Ipcr 1st QuarterDocument4 pagesJen Ipcr 1st QuarterJairolla ObayNo ratings yet
- Entry Form: Hospital Best Practices in Infection Prevention and Control Awards Year ViDocument1 pageEntry Form: Hospital Best Practices in Infection Prevention and Control Awards Year ViPeepsNo ratings yet
- WHY NOT BHARAT RATNA TO GREAT MEDICAL SCIENTIST AND MAN OF MIRACLE DRUGS DR - YELLAPRAGADA SUBBA RAO ?Document13 pagesWHY NOT BHARAT RATNA TO GREAT MEDICAL SCIENTIST AND MAN OF MIRACLE DRUGS DR - YELLAPRAGADA SUBBA RAO ?Anumakonda JagadeeshNo ratings yet
- Dyspepsia (Gastritis) Case StudiesDocument9 pagesDyspepsia (Gastritis) Case StudiesJessica Nurin Graman100% (1)
- School Entry Health Exam Form FL (Sample)Document2 pagesSchool Entry Health Exam Form FL (Sample)chase1828No ratings yet
- Comparison of Goldmann Applanation Tonometer, Tono-PenDocument19 pagesComparison of Goldmann Applanation Tonometer, Tono-PenLidiasilambaNo ratings yet