Professional Documents
Culture Documents
Depression Management Strategies
Uploaded by
Robert FordCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Depression Management Strategies
Uploaded by
Robert FordCopyright:
Available Formats
Depression Management Strategies
What is depression?
People experience depression in many different ways; however a depressed
person will normally have at least two of three of the following core symptoms
for more than two weeks:
An unusually sad mood or anxious state that does not go away (may
be worse in the morning).
Loss of enjoyment and interest in activities that used to bring pleasure.
Lack of energy and tiredness despite rest.
Other typical signs of depression include trouble with sleeping or early
wakening, feeling constantly tired or overwhelmed, pessimistic negative
thoughts, difficulty concentrating or making decisions, change in appetite, loss
of interest or avoidance behaviours.
There are different types of depressive reaction ranging from mild to moderate
to severe clinical depression. At the severe end of the scale people often
experience more marked physical symptoms and it is thought that this is
related to biochemical changes in the brain.
For most people a depressive reaction is triggered by a set of life events
which they are finding difficult to cope with. For example, bereavement,
relationship breakdown, financial difficulties, physical illness etc. Depression
is not easy to overcome, but there are ways that you can gradually free
yourself from depression.
Vulnerability to depression
Some people are more vulnerable to depression than others. A number of
protective factors have been identified which can decrease vulnerability to
depression. These include:
A high self-esteem based on self-worth, not achievements.
Practising positive thinking habits.
Assertively expressing your needs, thoughts and feelings.
Using an established social support network.
Stress management balancing demands and resources/ coping skills
and looking after yourself
The depressive spiral thoughts, mood, behaviour
Research has established that depressed people are prone to continuous,
automatic, negative thoughts. Thinking becomes distorted and they practice
recognised thinking errors such as: catastrophising, personalising, focusing
on the negative and jumping to conclusions.
These negative patterns of thinking produce a low mood state which results in
reduced activity. Reduced activity produces less rewarding experiences,
which leads to further negative thoughts and low mood.
A vicious spiral of thoughts, feelings and behaviour is created.
To stop this downward spiral a number of things are necessary:
Understand the problem. Understand the many factors both in the
present and the past that have led you to feel the way you do. Educate
yourself about the illness. The more you know the easier it may be to
feel in control of your recovery.
Challenge negative thinking. Recognise that the way you think
determines the way you feel. Identify distorted thinking patterns and
replace with more rational thoughts. Keep a thought mood diary.
Increase activity levels. Gradually increase your activity levels
particularly physical activity. Identify and work towards short and
longer-term goals and develop a routine.
Use support systems. A close confiding relationship is the single most
effective protection against depression. Talk about how you feel with
someone you trust. Tell a friend, partner, relative, GP. Try not to
isolate yourself.
Assert yourself. Express yourself assertively. Say no to excessive
demands. Look after your own needs.
Expect setbacks. Be aware that you will have good days and bad days
and that this is normal in recovery.
If you are feeling very bad or desperate you may need to talk to someone
immediately. You could consider the following:
Try to get an emergency appointment with your GP explaining the
circumstances.
If it is out of hours contact on-call GP services or visit your local A&E.
If in work speak to a Welfare Officer/ Carecall/ Line Manager or contact
OHS for advice.
Phone the Samaritans UK 08457 909090 or ROI 1850609090 or
Lifeline NI 0808 808 8000.
How feelings change
Beliefs and thoughts
Events themselves do not cause us to feel upset or depressed; it is our beliefs
about these events that determine our emotional reaction. These personal
beliefs influence our view of the world and our thinking patterns.
It is important to be mindful about what we are thinking and to examine our
underlying beliefs. We are thinking all the time.
Selective bias in depression
When we feel low in mood our thinking takes on a selective bias and we are
more likely to think about negative experiences from the past. Low mood
reactivates old negative thinking patterns. We then view the present more
negatively and view the future through a selective bias.
Recognise negative thinking.
If you are feeling low you are more likely to interpret events negatively and
ignore any other possibilities/ circumstances. The challenge when you are
depressed is to step back and become mindful of this process. Challenge the
process of thinking negatively automatically.
Types of treatment
Medication Your GP may prescribe an anti-depressant. Ensure you read
the information leaflet and raise any queries with your GP. Anti-depressants
usually take between two and six weeks to begin to work and should be taken
in the correct dosage as prescribed and continued for at least 4 months after
the depression has lifted or otherwise advised by your doctor.
Counselling/ Therapy Also known as talking treatment/ therapy, it will also
you the opportunity to share and explore your thoughts, emotions and
behaviours. Ask your GP about counselling or your employer may have an
Employee Assistance Programme to provide counselling.
Computerised Cognitive Behavioural Therapy (CCBT) This is a type of self-
help guided by the use of CD, DVD or website and is based on the principles
of Cognitive Behavioural Therapy. Your GP may be able to provide access to
the CCBT programme called Beating the Blues. It has been shown to be
effective in the treatment of mild or moderate depression and anxiety
conditions. Users work through modules identifying and challenging
automatic thoughts, negative thinking errors, maladaptive behaviours,
distractions and core beliefs which in some way feed into their depression or
anxiety.
Seven keys to mental health
1. Take responsibility
You are responsible for your own life and everything in it, including your own
happiness. Try not to blame your parents, your childhood, society, others or
life events.
2. Be flexible in your thinking
Beware of absolutist, all or nothing, black and white, rigid thinking, with an
over-emphasis on the words should, must, ought and cant. Loosen up
your thinking, look at alternative views, avoid perfectionism.
3. Confront rather than avoid difficulties and frustration
Treat problems as challenges, as useful in helping you build up tolerance and
experience. Expect change and challenges and for life to be unfair at times.
4. Look after your own needs
Be assertive in identifying and meeting your own needs, whether it be for
food, exercise, relaxation, work or pleasure. Have good self-care skills.
5. Express yourself
Feel free to express both positive feelings of enjoyment and excitement, but
also negative feelings of anger, sadness and disappointment. Be willing to,
try not bottle things up or avoid issues.
6. Strive for balance
Feel in control of your life by making active choices and decisions about how
spend your time. Fill your life with a balance of work and play, time alone and
with others, and physical and mental activity.
7. Develop and maintain relationships
Value and work on relationships. Develop a network of social support and
confiding relationships as they act as an insulator against stress. Accept
others for how they are, rather than trying to change them.
Activity planning
Keeping an activity diary can be especially useful when you are depressed
because it helps to focus on how you are spending your time, reminds you
what you have done, and is a useful way of planning ahead.
1. Plan what you are going to do the next day.
2. Plan activities that are absorbing and not too difficult.
3. Plan a mixture of activities that have a balance between duty and
pleasure.
4. Prioritise: identify what needs to be done first.
4. Break tasks down into smaller steps.
5. Plan activities that increase your physical activity levels.
6. Be flexible: if you have missed an activity proceed to the next one.
7. Increase frequency: build up the number of activities gradually.
8. Work towards goals: this helps increase motivation.
9. Anticipate difficulties and try to overcome them.
10. Reward yourself for your success. Tick off the things that you have
achieved and add small rewards throughout the day such as coffee, watching
a TV programme or reading the newspaper.
Make copies of and use the weekly diary sheet on the next page.
(The Mental Health Handbook T Powell 2009)
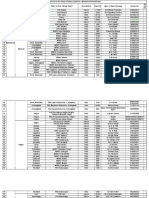
WEEKLY ACTIVITY SCHEDULE WEEK BEGINNING:
MONDAY TUESDAY WEDNESDAY THURSDAY FRIDAY SATURDAY SUNDAY
Wake - 9am
9am 10am
10am 11am
11am 12 noon
12 noon 1pm
1pm 2pm
2pm 3pm
3pm 4pm
4pm 5pm
5pm 6pm
6pm 7pm
7pm 8pm
8pm 9pm
9pm - bed
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Solution Focused Practice ToolkitDocument114 pagesSolution Focused Practice ToolkitEnrique Puebla Rosales100% (2)
- Solution Focused Practice ToolkitDocument114 pagesSolution Focused Practice ToolkitEnrique Puebla Rosales100% (2)
- Phoenix Command - Miniature Rules Modern Warfare - Complete Unofficial Resources (552pages) PDFDocument552 pagesPhoenix Command - Miniature Rules Modern Warfare - Complete Unofficial Resources (552pages) PDFperfect LibraryNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Compromise AgreementDocument4 pagesCompromise AgreementChen C AbreaNo ratings yet
- Letter of Appointment (HKDocument4 pagesLetter of Appointment (HKSikkandhar JabbarNo ratings yet
- Historical Development of Philippine Democratic PoliticsDocument40 pagesHistorical Development of Philippine Democratic PoliticsClaudette Nicole Gardoce0% (1)
- Family Therapy Stuff - Sample Chapter PDFDocument29 pagesFamily Therapy Stuff - Sample Chapter PDFRobert FordNo ratings yet
- Talking Therapies For MaoriDocument68 pagesTalking Therapies For MaoriRobert Ford100% (2)
- Talking Therapies For MaoriDocument68 pagesTalking Therapies For MaoriRobert Ford100% (2)
- Present Perfect Tense QuizDocument4 pagesPresent Perfect Tense QuizrennalisationNo ratings yet
- Practising Critical ReflectionDocument234 pagesPractising Critical ReflectionRobert FordNo ratings yet
- The Way of The ShepherdDocument5 pagesThe Way of The ShepherdMark AbiloNo ratings yet
- Corpuz v. Sto. TomasDocument1 pageCorpuz v. Sto. TomasDon SalamidaaNo ratings yet
- Petition for Nullity Ruling on Psychological IncapacityDocument4 pagesPetition for Nullity Ruling on Psychological IncapacitykeziahcorporalNo ratings yet
- PGK Precision Artillery KitDocument2 pagesPGK Precision Artillery KithdslmnNo ratings yet
- Alfaro Et Al vs. Sps DumalaganDocument2 pagesAlfaro Et Al vs. Sps DumalaganDominique Pobe100% (1)
- Social Work With Older People - CrawfordDocument203 pagesSocial Work With Older People - CrawfordRobert FordNo ratings yet
- Overnight OatsDocument1 pageOvernight OatsRobert FordNo ratings yet
- Family Walks in The WaikatoDocument24 pagesFamily Walks in The WaikatoRobert FordNo ratings yet
- Trout Fishing in The Waikato River PDFDocument1 pageTrout Fishing in The Waikato River PDFRobert FordNo ratings yet
- Depression: Caring For A Person ExperiencingDocument6 pagesDepression: Caring For A Person ExperiencingRobert FordNo ratings yet
- Trout Fishing in The Waikato River PDFDocument1 pageTrout Fishing in The Waikato River PDFRobert FordNo ratings yet
- Guidelines For Writing New Zealand Competence Assessment ApplicationsDocument6 pagesGuidelines For Writing New Zealand Competence Assessment ApplicationsRobert Ford100% (1)
- Depression: Caring For A Person ExperiencingDocument6 pagesDepression: Caring For A Person ExperiencingRobert FordNo ratings yet
- The Quest of the Cat and DragonDocument18 pagesThe Quest of the Cat and DragonRobert FordNo ratings yet
- 1 Page DSM - Anxiety and Trauma PDFDocument1 page1 Page DSM - Anxiety and Trauma PDFRobert FordNo ratings yet
- COMPETENCE APPLICATION AND ASSESSMENTDocument6 pagesCOMPETENCE APPLICATION AND ASSESSMENTRobert FordNo ratings yet
- Chapter 3 Code of Ethics PDFDocument14 pagesChapter 3 Code of Ethics PDFRobert FordNo ratings yet
- Social Work Management and Leadership PDFDocument211 pagesSocial Work Management and Leadership PDFRobert FordNo ratings yet
- P He Mapping ManualDocument105 pagesP He Mapping ManualRobert FordNo ratings yet
- History of Welfare State PDFDocument9 pagesHistory of Welfare State PDFRobert FordNo ratings yet
- A Primer On Social ProblemsDocument860 pagesA Primer On Social ProblemsRobert FordNo ratings yet
- OCC State of Care 2015Document62 pagesOCC State of Care 2015Robert FordNo ratings yet
- G 8 - Ethics and Dual Relationships 2012 PPT - GottliebDocument14 pagesG 8 - Ethics and Dual Relationships 2012 PPT - GottliebRobert FordNo ratings yet
- History of Welfare State PDFDocument9 pagesHistory of Welfare State PDFRobert FordNo ratings yet
- Trout Fishing in The Waikato RiverDocument1 pageTrout Fishing in The Waikato RiverRobert FordNo ratings yet
- G 8 - Ethics and Dual Relationships 2012 PPT - GottliebDocument14 pagesG 8 - Ethics and Dual Relationships 2012 PPT - GottliebRobert FordNo ratings yet
- Sample Chapter Home VisitsDocument14 pagesSample Chapter Home VisitsRobert FordNo ratings yet
- Sample ScreendumpDocument1 pageSample ScreendumpRobert FordNo ratings yet
- Partnership REPORTDocument4 pagesPartnership REPORTAiza A. CayananNo ratings yet
- MahaDocument4 pagesMahaKinjal KapadiaNo ratings yet
- Article III Judicial Power ExplainedDocument5 pagesArticle III Judicial Power ExplainedKyla HayesNo ratings yet
- Court of Appeals Decision on Insurance Claim ReversedDocument21 pagesCourt of Appeals Decision on Insurance Claim Reversedcrizalded0% (1)
- Guide to Intercountry Adoption from the PhilippinesDocument3 pagesGuide to Intercountry Adoption from the Philippinesjp_gucksNo ratings yet
- Arya Samaj Mandir Provides Inter - Religion Marriage Registration and Cerificate SupportDocument2 pagesArya Samaj Mandir Provides Inter - Religion Marriage Registration and Cerificate SupportaryasamajmandirmarriageNo ratings yet
- United States v. Alberto Valenzuela-Cueves, 4th Cir. (2013)Document3 pagesUnited States v. Alberto Valenzuela-Cueves, 4th Cir. (2013)Scribd Government DocsNo ratings yet
- NTT Application Form (APAC)Document3 pagesNTT Application Form (APAC)RahulNo ratings yet
- Future Tenses WorkshopDocument6 pagesFuture Tenses WorkshopJader loboNo ratings yet
- People'S Aircargo and Warehousing Co. Inc. vs. Court of AppealsDocument8 pagesPeople'S Aircargo and Warehousing Co. Inc. vs. Court of AppealsMike E DmNo ratings yet
- New Starter FormDocument5 pagesNew Starter FormRajagopal BojanapalliNo ratings yet
- Seyla Benhabib Another CosmopolitianismDocument8 pagesSeyla Benhabib Another CosmopolitianismDelcea Sky SergiuNo ratings yet
- Reading Passage - Worksheet 3Document2 pagesReading Passage - Worksheet 3Aishath AfzaNo ratings yet
- CG Power and Industrial Solutions LimitedDocument27 pagesCG Power and Industrial Solutions LimitedMani KandanNo ratings yet
- Headway: Clil WorksheetsDocument2 pagesHeadway: Clil WorksheetsAmina VeladžićNo ratings yet
- Search of A Moving VehicleDocument3 pagesSearch of A Moving VehicleKleyr De Casa AlbeteNo ratings yet
- The Impact of Bullying in School On The Adolescent's Sense of SelfDocument175 pagesThe Impact of Bullying in School On The Adolescent's Sense of Selfgina dunggonNo ratings yet
- Peak Ebpp DescriptionDocument4 pagesPeak Ebpp Descriptionapi-259241412No ratings yet
- Guaranty Agreement For Corporate Guarantor Dcma Form 1620Document2 pagesGuaranty Agreement For Corporate Guarantor Dcma Form 1620Tira MagdNo ratings yet
- Legal Aspects of Business: Indian Institute of Management, Rohtak Post Graduate ProgrammeDocument5 pagesLegal Aspects of Business: Indian Institute of Management, Rohtak Post Graduate ProgrammeAKANKSHA SINGHNo ratings yet