Professional Documents
Culture Documents
Neurogenic Neuroinflammation - Inflammatory CNS Reactions in Response To Neuronal
Uploaded by
Gustavo CabanasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neurogenic Neuroinflammation - Inflammatory CNS Reactions in Response To Neuronal
Uploaded by
Gustavo CabanasCopyright:
Available Formats
PERSPECTIVES
Second, astrocytes, microglia andin
OPINION
some regions of the CNSmast cells are
the innate, parenchymal immune cells
Neurogenic neuroinflammation: of the CNS58. Their activation is actively
depressed under non-pathological condi-
inflammatory CNS reactions in tions. Finally, the permeability of microves-
sels in the CNS for extravasation of large
response to neuronal activity molecules and blood cells is reduced in
comparison to the rest of the body by the
bloodCNS barrier. Hence, it is much
Dimitris N.Xanthos and Jrgen Sandkhler more difficult to activate complement
cascades and to recruit cells involved in
Abstract | The CNS is endowed with an elaborated response repertoire termed the adaptive immunity response, such as
neuroinflammation, which enables it to cope with pathogens, toxins, traumata leucocytes, into the CNS parenchyma. With
and degeneration. On the basis of recent publications, we deduce that the notable exception of activated Tcells,
orchestrated actions of immune cells, vascular cells and neurons that constitute which readily penetrate the intact blood
CNS barrier, CNS innate immune cells thus
neuroinflammation are not only provoked by pathological conditions but can also
do not as efficiently recruit the machin-
be induced by increased neuronal activity. We suggest that the technical term ery of the adaptive immune response as
neurogenic neuroinflammation should be used for inflammatory reactions in the do dendritic cells in peripheral tissues9.
CNS in response to neuronal activity. We believe that neurogenic neuro- Therefore, resident innate immune cells
inflammation maintains homeostasis to enable the CNS to cope with enhanced of the CNS must often deal directly with
pathogens and tissue damage, and it is only
metabolic demands and increases the computational power and plasticity of CNS
under severe conditions that inflammatory
neuronal networks. However, neurogenic neuroinflammation may also become cells such as infiltrating Tcells are involved
maladaptive and aggravate the outcomes of pain, stress and epilepsy. (see REF.10 for a review).
The mild inflammatory tissue reac-
The integrity of all body tissues is endan- of exogenous or endogenous antigens and tions in the CNS protect neuronswith
gered by microbial pathogens, toxins, trau- activation of the complement system. In their low regenerative capacityfrom the
mata and degeneration. In response to such peripheral tissues, dendritic cells provide destructive inflammatory responses that are
situations, innate and adaptive immune information to cells of the adaptive immune readily induced in regenerating peripheral
cells, vascular cells and neurons take con- system, leading to vigorous inflamma- tissues. This has led to the introduction of
certed and finely tuned defence actions to tory responses, such as phagocytosis (and the term neuroinflammation to distinguish
maintain or restore tissue integrity. Initially, eventually necrosis), the formation of new inflammatory reactions in the CNS from
innate immune cells, such as macrophages, connective tissue and granulomas. Diverse inflammation in other tissues. From the pre-
mast cells and dendritic cells, are activated communication channels link the immune sent literature, it is not always clear which
and respond in a nonspecific manner to system to the CNS and enable it to support criteria must be met to qualify for the label
exogenous or endogenous danger signals. host defence by promoting fever, increased neuroinflammation. Numerous studies have
This leads to tissue reactions that range sleep and enhanced pain sensitivity (hyper- assessed individual responses such as the
from mild homeostatic responses (some- algesia)2. The spectrum of actions and production and the release of pro-inflam-
times known as para-inflammation) that responses that occur strongly depends matory cytokines or disturbances of the
are close to the basal, non-stressed state to upon the type, intensity and duration of bloodbrain barrier. For example, it is well
a transition into full-scale inflammation1. the initial trigger signal, the tissue affected established that epileptic seizures lead to the
In the full inflammatory response, the and the phase of the reaction. Collectively, release of cytokines in the affected brain tis-
vasculature reacts with vasodilation and this multitude of tissue reactions is termed sue11,12. In our opinion, whether the release
extravasation of plasma components and inflammation. of a pro-inflammatory cytokine alone is
blood cells, establishing three of the four Inflammatory reactions within the indicative of an inflammatory reaction is
classical signs of inflammation: rubor (red- CNS differ substantially from those of debatable. The term immune signalling
ness), calor (warmth) and tumour (swell- other tissues in several ways. First, the seems to be more appropriate to describe
ing). The fourth sign is dolor (pain). The CNS parenchyma lacks resident dendritic the isolated release of immune-relevant
most violent of these reactions are usually cells; perivascular macrophages3 and molecules without any concomitant expres-
seen during an infection or in an inflam- vascular pericytes4 take over the func- sion of other signs of neuroinflammation.
matory disease and involve presentation tions of mature dendritic cells in the CNS. However, when the respective literature is
NATURE REVIEWS | NEUROSCIENCE VOLUME 15 | JANUARY 2014 | 43
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
reviewed as a whole, it may become clear forms of neuroinflammation1821 (FIG.3). are of particular interest as they lead to
that under a given experimental condi- We thus propose the technical term neu- long-term changes in the processing of
tion, the full spectrum of the inflammatory rogenic neuroinflammation to describe sensory information in the spinal dorsal
response involving immune cells, vascular those inflammatory reactions within the horn and are identical to those that trigger
cells and neurons takes place; as occurs, for CNS that are triggered by neuronal activity. neurogenic inflammation in the peripheral
example, in the course of epilepsy13. We suggest that neurogenic neuroinflam- tissues (FIG.2). Effective stimuli in rodent
It is often believed that neuroinflamma- mation may have beneficial effects such as hindpaws include direct electrical nerve
tion is induced only by a pathological state, enabling the nervous system to cope with stimulation at intensities sufficient to acti-
usually in the form of a microbial infection, enhanced metabolic demands, increasing vate Cfibres, selective activation of pepti-
exposure to toxins or degeneration (FIG.1) its computational power and promoting dergic primary afferents that express the
(see REFS8,10,14 for reviews). However, regeneration. Neurogenic neuroinflam- transient receptor potentialV1 (TRPV1)
we feel that neuroinflammation and its mation may become maladaptive when it receptor by capsaicin and chemically
mechanisms do not have to be by definition persists for longer than necessary or when induced inflammation. As in the periphery
pathological and may encompass immune it spreads to remote sites (FIG.1), and it may (FIG.2), activation of peptidergic primary
signalling as long as immune cells, vascu- be relevant to conditions as diverse as pain, afferent C fibres also leads to the spinal
lar cells and neurons act in concert. This psychological stress and epileptic seizures. release of various mediators, including
concerted action does not necessarily have glutamate, substanceP, calcitonin gene-
to be synergistic at all times: pro- and anti- Neurogenic neuroinflammation related peptide (CGRP), brain-derived neu-
inflammatory processes may occur simul- Classical neurogenic inflammation in rotrophic factor (BDNF), fractalkine and
taneously. FIGURE1 illustrates the concept peripheral tissues is triggered by action- ATP (FIG.3). Receptors for these neurotrans-
of parallel and interacting homeostatic and potential-dependent release of substances mitters and neuropeptides are present in
pathological processes and outcomes. from the peripheral terminals of peptider- nearby cells of the immune system, vascular
Many studies demonstrate that, in addi- gic, sensory nerve fibres and involves vaso- cells and higher-order neurons.
tion to the classical instigators of inflam- dilation, plasma extravasation, recruitment
mation described above, enhanced levels of of white blood cells and mast cell degranu- Immune responses to neuronal activity.
neuronal activity can trigger inflammatory lation (BOX1; FIG.2). A number of studies Glial cells can be directly activated by
reactions in peripheral tissues, where it has have now shown that similar substances substances that are released from primary
long been known as neurogenic inflam- are released from synapses in the CNS in afferent nerve fibres upon stimulation.
mation (REFS1517) (BOX1; FIG.2). Here, we response to neuronal activity; however, few This includes substance P acting on the
discuss emerging evidence suggesting that studies have considered this response profile neurokinin1 receptor (NK1; also known as
neuronal activity may also be sufficient to as awhole. substanceP receptor), ATP acting on P2X
trigger the concerted actions of immune We focus here on spinal changes in purinoceptor 7 (P2X7) and glutamate act-
cells, vascular cells and neurons within response to stimulation of peptidergic, ing on metabotropic glutamate receptors
the CNS in a manner that resembles other nociceptive nerve fibres. These stimuli (mGluRs) (also see below). Consequently,
Triggers Actions Outcomes
Classical Homeostatic Adaptation
Infectious microbes Release of gliotransmitters, neurotrophic Microbe elimination
+
Viral factors, cytokines Synaptic plasticity
Bacterial Vasodilation Enhanced perfusion
Fungal and Phagocytosis Neuroprotection, repair, regeneration
protozoal
Autoimmunity Maladaptive Dysfunction
Toxins +
Release of pro-inammatory factors Hyperexcitability and/or impaired
Environmental Plasma extravasation inhibition
Disease proteins Reduced computational power
and danger signals Neuroinammation
Neurotoxic Degeneration
Release of pro-inammatory factors Progressive CNS loss of function
Neurogenic
States of enhanced + Excitotoxicity, apoptosis Chronic disease
neuronal activity BloodCNS-barrier breakdown
Noxious stimuli
Psychological stress Anti-inammatory Resolution
Epileptic seizure Release of anti-inammatory cytokines, Termination of inammatory
neuroprotectins, resolvins, neurotrophic response
+
factors, neurotransmitters, neuropeptides,
cell adhesion molecules
Vasodilation
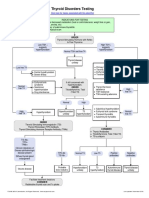
Figure 1 | Triggers, actions and outcomes of neuroinflammation. homeostatic, leading to adaptation, or dysfunctional and/or
Nature Reviews neurotoxic,
| Neuroscience
Neuroinflammation can be triggered by classical factors (infection, autoim- leading to pathology. Anti-inflammatory mechanisms may be triggered in
munity or toxins) but also by factors that lead to enhanced neuronal activity parallel and serve to terminate neuroinflammation and reduce pathological
(including noxious stimuli, psychological stress and epileptic seizures). outcomes (indicated by minus signs). Treatments and interventions may be
Immune cells, vascular cells and neurons promote various independent as targeted at various levels to inhibit the triggers and neuroinflammatory
well as interacting responses (indicated by plus signs). These can be processes, or to promote the resolution of inflammation.
44 | JANUARY 2014 | VOLUME 15 www.nature.com/reviews/neuro
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
Box 1 | Neurogenic inflammation
in response to neuronal activity)35,36. In
addition, Tcells are activated by serotonin35
Neurogenic inflammation is a local inflammatory state in peripheral tissues induced by neuronal and dopamine37, substances that are also
activity. Upon stimulation, sensory nerve fibres transmit action potentials not only released in spinal dorsal horn upon affer-
orthodromically to the CNS but also antidromically into inactive branches of the afferent fibre ent stimulation38,39 (FIG.3). Furthermore,
(FIG.2). Experimentally, various noxious stimuli, such as direct electrical nerve stimulation or
naive, antigen-inexperienced Tcells can be
activation of transient receptor potential V1 (TRPV1) channels by capsaicin, lead to the
excitation of Cfibres (unmyelinated, nociceptive nerve fibres) and induce neurogenic
recruited to the CNS by chemoattractant
inflammation. At the peripheral endings of peptidergic Cfibres, neuropeptides such as signals produced by activated neurons or
substanceP, calcitonin gene-related peptide (CGRP) and neuropeptideY are released and trigger glia and by stressed endothelial cells40.
inflammatory tissue reactions (FIG.2). Mast cells are particularly implicated, as they rapidly Mast cells are usually activated by
degranulate and release a large number of substances such as cytokines, prostaglandins, immunoglobulinE (IgE) binding to its
serotonin and histamine. Pro-inflammatory mediators, as well as released glutamate, will sensitize receptor FcRI. However, substances that
nociceptive nerve endings, leading to pain. Further tissue reactions include vasodilation, plasma are released in the spinal cord upon pri-
extravasation and recruitment of leucocytes to the tissue1517,171. The entire process may be mary afferent stimulationincluding sub-
self-amplifying, leading to continuous neuropeptide release. Participation of the CNS is not stance P, CGRP, nerve growth factor and
required for peripheral neurogenic inflammation, although it can clearly amplify it. Neurogenic
vasoactive intestinal polypeptide41can
inflammation has initially been described in the skin but has now also been identified in a wide
range of tissues and organs, including peripheral nerves, soft tissue, joints, airway, eye, gums,
also trigger mast-cell degranulation (the
meninges, pancreas and viscera (see REF.16 for a comprehensive overview). In the skin, neurogenic release of molecules from secretory vesicles
inflammation leads to the classical inflammatory signs of rubor (redness), tumour (swelling), calor known as granules) (FIG.3). Activation of
(warmth) and dolor (pain). Neurogenic inflammation thus resembles other forms of inflammation in TRPV1expressing primary afferent Cfibres
many aspects. Neurogenic inflammation may have beneficial effects168,172 or may amplify disease by capsaicin, which leads to the spinal
states such as psoriasis, arthritis, asthma, ocular trauma, periodontitis, migraine, pancreatitis, release of substance P, enhances the number
inflammatory bowel disease, colitis, neuropathic pain, sepsis and cardiovascular disease16. of degranulated spinal dural mast cells42.
Neurons thus seem to be powerful trig-
gers of innate and adaptive immune-cell
markers of activation are upregulated in spi- in the absence of neuronal activity. Glial activation in the CNS. However, it is worth
nal microglia and astrocytes within minutes cells switch to distinct and finely tuned noting that neuronal activity may also trig-
of enhanced neuronal activity. For example, executive phases in response to neuronal ger anti-inflammatory reactions in the CNS,
phosphorylated p38 mitogen-activated activity 6,7. Thus, in addition to the well- as outlinedbelow.
protein kinase is increased in microglia described activation of spinal glial cells
after stimulation of sensory nerve fibres in the course of peripheral neuropathies Vascular responses to neuronal activity.
with formalin in conscious rats22. Microglial or spinal-cord injuries (see REFS31,32 for Noxious mechanical stimulation, formalin
SRC-family kinases23 are upregulated after reviews), neuronal activity is also sufficient and capsaicin injections into a rat hindpaw
electrical stimulation of Cfibres, and con- to activate glial cells in the spinal cord and direct electrical nerve stimulation all
nexin dephosphorylation occurs in astro- (FIG.3). However, other peripheral triggers increase spinal blood flow 20,43,44. The cou-
cyte gap junctions after capsaicin or Cfibre of glial-cell activation in the CNS must not pling between neuronal activity and vascular
stimulation in anaesthetized rats24. High- be ignored. For example, cytokines such as responses is mediated by the neurovascular
frequency discharges in primary afferent tumour necrosis factor (TNF) may be unit, which is comprised primarily of neu-
Cfibres induce a rise in intracellular Ca2+ transported in an anterograde direction in rons, astrocytes and endothelial cells (FIG.3).
concentrations ([Ca2+]i) in spinal astrocytes sensory nerve fibres from the peripheral Vascular cells constitutively express cytokine
within seconds, and enhanced expression of tissues to the spinal cord33, where they receptors such as interleukin1 (IL1) recep-
immunohistochemical markers of microglia could activate glia. Whether glial-cell acti- tors45, purinergic receptors46, NK1 and CGRP
activation in spinal-cord slices within min- vation and the release of cytokines alone receptors, and soluble guanylyl cyclase (which
utes18. Electrical nerve stimulation induces meet the criteria for being classified as forms part of the signalling pathway activated
morphological changes in microglia and in neuroinflammation is debatable. However, by nitric oxide). Many vasoactive substances
astrocytes in rat spinal-cord and trigeminal as outlined below, neuronal activity also are released from primary afferents, activated
nuclei19,25. Hence, glial activation constitutes recruits additional components of an glial cells and vascular cells in the CNS in
mainly an innate immune response with a inflammatory reaction, and we believe response to primary afferent activity. For
phagocytic macrophage phenotype26 and that together these constitute neurogenic example, spillover beyond the synaptic cleft
probably also involves activation of pat- neuroinflammation. of substance P and other neurokinins that
tern- and danger-recognition receptors Under resting conditions, Tcells are cause enhanced capillary permeability 47 and
(such as Toll-like receptor4)27,28, which are present in the CNS parenchyma in rela- of CGRP, an extremely potent vasodilator 48, is
thought to trigger innate immune responses tively low numbers. CD4+ Tcells and, to a known to occur in the spinal cord in response
in theCNS29. greater extent, CD8+ Tcells are found in the to afferent nerve stimulation49,50. ATP is
It is becoming increasingly clear intact spinal-cord parenchyma34. Like glial another potent vasodilator 51 in the CNS that
that activation of microglia is not an cells, these Tcells express a large number of is released in an activity-dependent manner
allornone process and does not take a neurotransmitter receptors and can be acti- in the spinal cord52,53. Other potentially vaso-
linear path with fixed uniform outcomes6. vated in an antigen-independent fashion by active substances, including prostaglandins
Instead, it seems that glial cells are per- glutamate, substanceP, CGRP, somatosta- from spinal endothelial cells54 and potassium
manently active but remain in a surveil- tin, BDNF and neuropeptideY (all of which ions55, are also released in response to neu-
lance mode and are even highly motile30 are released directly from primary afferents ronal activity 56 (FIG.3).
NATURE REVIEWS | NEUROSCIENCE VOLUME 15 | JANUARY 2014 | 45
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
CNS
CB Complement Macrophage Peripheral tissue
Complement Cytokines
Cytokines NO DRG
DAMP PG
END Ion channel or ionotropic
IgE receptor
NO Antidromic
PAF Metabotropic receptor
action
PG Orthodromic
ATP GABA potential
SP action potential Plasmalemmal transporter
CB Glu
Complement Resolvins
Cytokines and lipoxins
DAMP SP
Peptidergic
C-bre terminal
Endothelial cell
Noxious stimuli,
inammation,
Mast cell Ca2+ CD4+ Glu wound, trauma
Cytokines
Dendritic
Cytokines ATP BK cell
DAMP BDNF Complement
His CGRP Cytokines T-cell
NGF DAMP END
NO Glu NO Pericyte
PAF NPY Resolvins ATP Glu
PG SOM and lipoxins CD8+ NGF
ATP Glu BDNF
Serotonin SP CB NA CB NPY CGRP
TRP CGRP NO CGRP Resolvins Complement
Complement PG Complement and lipoxins Cytokines
Cytokines Resolvins Cytokines Serotonin DAMP
DA and lipoxins DA SOM Resolvins
DAMP Serotonin DAMP SP and lipoxins
END SP Cytokines END SP
Figure 2 | Neuronal activity triggers neurogenic inflammation in periph- boxes), creating the inflammatory milieu. Immune cells, plasma and various
Nature Reviews | Neuroscience
eral tissues. The figure shows a primary afferent, peptidergic nerve fibre mediators can also extravasate into tissue (not shown). Sensory nerve fibres
and elements that contribute to neurogenic inflammation at peripheral can become sensitized and also lower their threshold for further neuro-
nerve terminals. Neurogenic inflammation in the periphery is initiated by transmitter and neuropeptide release. Pro- and anti-inflammatory sub-
neuronal activity generated by a wide range of highly specific (such as tran- stances and signalling molecules that are released (shown in light yellow
sient receptor potential V1 (TRPV1) activation) and less-specific stimuli (such boxes) from various sources bind to receptors on the different cells and
as traumatic injury). This results in the generation of orthodromic action modulate their function. Signalling from higher-order CNS centres (not
potentials that conduct towards the CNS, as well as antidromic action shown) may also dampen or aggravate peripheral neurogenic inflamma-
potentials at branch points that conduct towards the peripheral terminals tion. BDNF, brain-derived neurotrophic factor; BK, bradykinin; CB, cannabi-
to induce neurogenic inflammation. Neurogenic inflammation results from noid; CD, T-cell surface glycoprotein CD; CGRP, calcitonin gene-related
the release of neurotransmitters and neuropeptides from peripheral nerve peptide; DA, dopamine; DAMP, danger-associated molecular patterns;
terminals (blue box). These rapidly affect various cell types, including vascu- DRG, dorsal root ganglia; END, endothelin; Glu, glutamate; His, hista-
lar cells (endothelial cells), mast cells, macrophages and other immune cells mine; IgE, immunoglobulinE; NA, noradrenaline; NGF, nerve growth fac-
(not shown). Tcells and dendritic cells may also be recruited. The different tor; NO, nitric oxide; NPY, neuropeptideY; PAF, platelet activating factor;
cell types themselves also begin to release substances (shown in coloured PG, prostaglandin; SOM, somatostatin; SP, substance P; TRP, tryptase.
Although neuronal activity readily However, a more robust afferent barrage in Contribution of higher-order neurons.
enhances regional blood flow in the CNS, Cfibres, which is triggered by direct sciatic Neuronal activity is by definition the pri-
the integrity of the bloodCNS barrier nerve capsaicin application, induces wide- mary trigger for neurogenic neuroinflam-
is substantially more resistant to change. spread disruption of the bloodspinal-cord mation. Peptidergic Cfibres are, however,
Formidable neuronal activity is required for barrier 24hours after stimulation21. not the only logical source for the induction
such changes to occur. For example, the tight Vascular cells in the CNS not only of neurogenic neuroinflammation in the
junction protein occludin is altered in spinal respond to pro-inflammatory sub- spinal cord. In fact, microglia60,61 and CNS
endothelial cells and mild IgG extravasation stances but can also release cytokines and endothelial cells61,62 express receptors for
is detected no earlier than 72hours after chemokines58,59, possibly contributing to the a wide range of neurotransmitters, some
hindpaw inflammation with carrageenan57. inflammatory process. of which are released from higher-order
46 | JANUARY 2014 | VOLUME 15 www.nature.com/reviews/neuro
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
ATP Glu
BDNF NGF T cell
CB NPY
CGRP Resolvins ATP ATP Glu
Complement and lipoxins BDNF CB Gly Descending
Cytokines Serotonin CD8+ Cytokines CGRP NA neuron
DA SOM DAMP Complement NGF
DAMP SP D-Ser Cytokines Resolvins
END Cytokines GABA DA and lipoxins ATP
ADO Glu Glu DAMP PG Cytokines
ATP NA PG END Serotonin DA
Glu
CB NPY CD4+ GABA SP NA
Complement Resolvins Serotonin
Cytokines and
DA lipoxins
DAMP Serotonin Postsynaptic Astrocyte
ATP
END SOM CB
Fractalkine SP Cytokines
GABA ATP Fractalkine
Glu
ATP CB GABA
BDNF K+ CGRP Glu
Complement Complement Gly
Cytokines Cytokines NO
H2O DA
DAMP
Glu ATP DAMP
Presynaptic
NO BDNF END
PG Ca2+ CGRP Glu
Microglial Glu NA
cell CB Astrocyte NO
Cytokines NPY
CGRP endfoot PG
DAMP SOM
Complement Endothelial Resolvins
His SP
Cytokines cell and lipoxins
NGF
DAMP Cytokines Serotonin
NO
END DAMP SP
PAF
IgE Fractalkine
PG
NGF Cytokines
Serotonin Pericyte
NO END
TRP
Mast cell NPY Neurovascular unit NO
PAF PG Interneuron
PG
BloodCNS barrier SP CNS
Peripheral tissue
Soma Orthodromic
action potential Plasmalemmal
transporter
Ion channel or
ionotropic receptor
Peptidergic C-bre terminal Metabotropic
receptor
Nature Reviews | Neuroscience
Figure 3 | Neuronal activity triggers neurogenic neuroinflammation effects against excitotoxicity. However, they may also participate in neu-
in the CNS. This figure illustrates neurogenic neuroinflammation at spi- rogenic neuroinflammation to release pro-inflammatory mediators. As in
nal or trigeminal terminals. In the CNS, enhanced neuronal activity com- the periphery, both pro- and anti-inflammatory mediators, and signalling
ing from peripheral sources will result in neurogenic neuroinflammation molecules and forces can be released from all cell types (key substances
owing to vesicular and non-vesicular release of neurotransmitters and shown in boxes of the respective colour of cell type) in the multipartite
neuropeptides from the primary afferent fibre (blue boxes). This will synaptic region to further affect receptors or channels present on all cell
induce concerted and interacting immune responses, vascular responses types shown (key substances acting on cells shown in light yellow boxes).
and higher-order neuronal network responses in the multipartite synapse. Ongoing neurogenic neuroinflammation may serve to amplify neuronal
This includes, but is not limited to, microglia, astrocytes, the neurovascular network activity and the resulting long-term potentiation may spread far
unit (composed of endothelial cells, other vascular cells such as pericytes, along the neuraxis, enhancing computational power of the neuronal net-
the presynaptic neuron and the astrocyte endfeet) and second-order neu- work. This can serve to elicit appropriate protective responses and behav-
rons within the neuronal network (including interneurons, ascending iours from the organism. In some cases, it may also trigger or aggravate an
neurons and descending neurons), all of which are primary players in the established pathology. Signalling from higher-order CNS centres
response to enhanced Cfibre activity. Mast cells on the dura, perivascular (descending neurons) can serve to dampen or aggravate neurogenic neu-
macrophages, and CD4+ and CD8+ Tcells may also participate and release roinflammation. ADO, adenosine; BDNF, brain-derived neurotrophic fac-
substances. With strong neuronal activity, recruitment of peripheral tor; CB, cannabinoid; CGRP, calcitonin gene-related peptide; DA,
immune cells (including macrophages, T cells and mast cells), and changes dopamine; DAMP, danger-associated molecular patterns; dSer, dserine;
at the bloodCNS barrier (for specific substances or involving a regional END, endothelin; Gly, glycine; His, histamine; IgE, immunoglobulin E; NA,
breakdown) can occur, creating further CNS neuroinflammatory noradrenaline; NGF, nerve growth factor; NO, nitric oxide; NPY, neuropep-
responses. Astrocytes found exclusively in the CNS serve to take up exces- tideY; PAF, platelet activating factor; PG, prostaglandin; SOM, somatostatin;
sive glutamate (Glu) and potassium, thereby providing neuroprotective SP, substance P; TRP, tryptase.
NATURE REVIEWS | NEUROSCIENCE VOLUME 15 | JANUARY 2014 | 47
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
neurons but not from primary afferents. synapses7375. The list of relevant synaptic to a rise in InsP3 levels and [Ca2+]i in neu-
Examples are the inhibitory neurotransmit- partners is likely to increase as we broaden rons, microglia and astrocytes, resulting in
ters glycine and GABA, both of which are our knowledge of the mechanisms of neu- glial-cell activation85 and LTP86. However,
released from spinal interneurons, and the rogenic neuroinflammation. Eventually, mGluR5 activation in spinal microglia inhib-
monoamines noradrenaline, serotonin and this growth in knowledge will culminate in its the release of inflammatory mediators
dopamine, which are released from descend- the concept of a multipartite synapse. The (cytokines or free radicals) both invitro87
ing-tract neurons. These neurotransmitters actual number of critical cellular and extra- and invivo88 and a specific group I mGluR
may modulate the functions of both glial and cellular elements modulating the transmis- agonist induces long-term depression at
vascular cells. Monoamines are vasoactive in sion at multipartite synapses will depend spinal Afibre synapses89. Evidence from
the CNS63,64 but they also affect the functions upon the context and is likely to differ experiments using invitro oxidative stress
of immune cells (see REF.65 for a review). between CNS regions. and excitotoxicity protocols also suggests
In addition, activation of type A GABA anti-inflammatory roles for mGluR1 activa-
receptors leads to the production of oxygen Overlapping signalling pathways. The vari- tion90, and specific stimulation of groupI
radicals in rodent microglia66. Noradrenaline ous intracellular signalling pathways that mGluRs in astrocytes leads to increased glu-
causes retraction of microglial processes contribute to neurogenic neuroinflamma- tamate and potassium uptake91. In addition,
through activation of the 2adrenergic tion exist in more than one type of cell in vascular cells in the CNS express mGluRs92
receptor under resting conditions and the multipartite synapse. Pharmacologically and it has been suggested that activation
through activation of the adrenergic 2A modulating these signalling pathways of groupI mGluRs can increase vascu-
receptor under pro-inflammatory conditions systemically or regionally (but not cell spe- lar permeability 93, although these effects
in tissue culture and brain slices67. Serotonin cifically) may therefore result in complex remain to be investigated further. Hence, the
promotes microglial motility but reduces synergistic and/or antagonist interactions. downstream effects of activity-dependent
phagocytic activity 68. For example, the binding of substanceP glutamate release are likely to result in both
In summary, the available evidence sug- to NK1 receptors in spinal neurons after pro- and anti-inflammatory actions.
gests that neuronal activity in primary affer- stimulation of Cfibres activates the phos-
ent nerve fibres or higher-order neurons pholipaseC and inositol triphosphate Therapeutic resolution
is sufficient to activate innate and adaptive (InsP3) signalling pathway, leading to Most inflammatory conditions are of lim-
immune cells, vascular cells and neurons in increased [Ca2+]i and synaptic long-term ited duration. Resolution of inflammation
the spinal cord. It thus resembles other trig- potentiation (LTP)76. Activation of NK1 is an active process that involves the actions
gers of neuroinflammation in the CNS8,10, receptors on astrocytes can also lead to of anti-inflammatory mediators such as
and we therefore suggest that the term neu- increases in [Ca2+]i levels77 and NK1 recep- IL10 (REF. 94), neuroprotectin D1 (REF.95),
rogenic neuroinflammation should be used tor antagonists can reverse spinal astrocyte resolvins96, neurotrophic factors, and TNF
to describe this phenomenon. activation78. Activation of microglial NK1 and fractalkine (under some conditions)97,
receptors leads to the activation of the pro- produced by immune, vascular and/or neu-
The multipartite synapse inflammatory nuclearfactor-B pathway 79. ronal cells (FIG.1). Anti-inflammatory actions
All the elements of neurogenic neuroinflam- NK1 receptor activation in endothelial cells, have been described for dopamine acting
mation described above interact in a com- as in neurons, also leads to phospholipase C on astrocytic dopamine D2 receptors68 (see
plex manner, the details of which have only activation, InsP3 accumulation, and [Ca2+]i REF.65 for a review), and for somatostatin98,
become better understood in recent years. rises80. Thus, substance P exerts synergistic neuropeptideY99 and adenosine acting on
For example, neurons and microglia interact pro-inflammatory actions on various cell adenosine A2A receptors on microglia100.
bidirectionally, and the dialogue between types of the multipartite synapse through Other anti-inflammatory responses
these cells involves fractalkine (also known NK1 receptors. to neuronal activity involve major histo-
as CX3CL1), a transmembrane chemokine Release of cytokines may likewise have compatibility complex (MHC) molecules.
that is expressed by neurons and acts synergistic effects. For example, after Upon exposure to interferon, neurons
through a receptor (CX3CR1) that is exclu- peripheral nerve stimulation56, activation can express MHC molecules at their surface
sively present on microglia69,70. Fractalkine of TNF and IL1 receptors present on to interact with CD8+ cytotoxic Tcells101.
is biologically active both as a membrane- superficial dorsal horn neurons, glial cells18 Neuronal activity dampens the neuronal101
bound adhesion molecule and in its soluble and endothelial cells81, can induce prosta- and glial102 expression of MHC molecules
form. For the soluble form of fractalkine to glandin release through cyclooxygenase 1 in part by increasing the release of nerve-
bind CX3CR1, its extracellular domain must (COX1; also known as PTGS1) and COX2 growth factor and BDNF102. Consequently,
be cleaved by cathepsin S, which is released (also known as PTGS2) activation in these silencing neuronal activity by blocking some
from activated microglia. Activity in pri- cell types8183. This can then drive further voltage-gated sodium channels with tetrodo-
mary afferent nerve fibres can activate spinal primary afferent glutamate, substanceP and toxin (TTX) induces upregulation of MHC
microglia, as described above, which in turn CGRP release56. molecules in microglia invivo103,104 and
releases cathepsin S. This liberates soluble By contrast, the actions of glutamate on activates glial cells30. This finding cannot be
fractalkine from neurons, which boosts cellular signalling are considerably more explained by the expression of TTX-sensitive
microglia activation and is proposed to cause mixed. An example of this is provided sodium channels on glial cells, as blockade of
hyperalgesia (see REFS71,72 for reviews). by groupI mGluRs, which are expressed glial TTX-sensitive sodium channels reduces
In addition, astrocytes, Tcells, and the on a wide variety of cell types84, includ- rather than increases cytokine release from
extracellular matrix have profound effects ing neurons, astrocytes, microglia, Tcells glia105. The loss of physiologic neuronal and
on synaptic transmission. This has led to and endothelial cells. Activation of groupI synaptic activity may also underlie activation
the concepts of tri-, tetra- and pentapartite mGluRs (and particularly mGluR5) leads of microglia after deafferentation106. This is
48 | JANUARY 2014 | VOLUME 15 www.nature.com/reviews/neuro
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
consistent with one of the known impor- and antiepileptic drugs that depress Cfibre synapses in the spinal dorsal horn
tant roles of activated microglia, which is nuclearfactor-B pathways121. Similarly, can- invitro132 and invivo133 (see REF.134 for a
to maintain functional neuronal circuits by nabinoids act on cannabinoid 1 and 2 recep- review). Recent studies have revealed that
eliminating inactive synapses107,108. tors on neuronal, immune and endothelial mediators of neurogenic neuroinflamma-
Neuronal activity may also exert inhibi- cells of the CNS, the effects of which may tion such as BDNF, ATP, TNF and IL1
tory influences on parenchymal microglia collaborate to reduce neuroinflamma- are also all essential for LTP induction in
through contact-dependent inhibition tion122,123. Conversely, opioids activate innate spinal-cord dorsal horn (see REFS134,135
involving adhesion moleculereceptor immune cells in the CNS, which contributes for reviews).
pairs (such as CD200CD200 receptor, to opioid tolerance124, opioid withdrawal Neurogenic neuroinflammation also
CD22CD45 or HSP60TREM2 (coupled to LTP125 and paradoxical opioid-induced affects synaptic inhibition in the spinal cord,
DAP12)), soluble adhesion molecules (such hyperalgesia126. which has five essential effects on nocicep-
as intercellular adhesion molecule 5 or extra- Interestingly, anti-inflammatory dietary tion: it prevents hyperalgesia, radiating pain,
cellular fractalkine), neuron-derived IgG109 elements such as omega3 polyunsaturated allodynia and spontaneous pain, and reduces
or anti-inflammatory cytokines110,111. fatty acids, neuroprotectin 1 or resolvins can the risk of pain chronicity 134. However, the
Some cytokines exert both pro- and anti- reduce neuroinflammation in the brain127 release of BDNF from central terminals of
inflammatory actions, depending upon the and spinal cord128, block LTP at spinal afferent nerve fibres136, or from spinal glial
context and the CNS region. For example, Cfibre synapses95 and reduce pain-related cells (in peripheral neuropathy)137 results in
soluble fractalkine has pro-inflammatory behaviour 128 (see REF.96 for review). impaired inhibition of nociception137,138 (see
and pronociceptive actions in the spinal REF.139 for a review). Both LTP and reduced
dorsal horn (see REFS71,72 for reviews). Friend or foe? inhibition can be adaptive if the result-
Conversely, both soluble and membrane- Evidence suggests that neurogenic neuroin- ing hyperalgesia enables better protection
bound forms of fractalkine attenuate flammation has roles in tissue metabolism, of injured tissues. However, they can also
lipopolysaccharide-induced activation of synaptic plasticity, modulation of neuronal become maladaptive when they persist after
microglia in primary cortical glialneuronal excitability, glutamate excitotoxicity, and healing of the tissue or spread to somatotopi-
cocultures112 and reduce microglial neu- degeneration and regeneration. Neurogenic cally inappropriate (uninjured) sites.
rotoxicity invivo in a murine Parkinsons neuroinflammation may be beneficial
disease model70. Furthermore, fractalkine- and/or detrimental: the prevailing effect Transitions to pathology. As with other forms
stimulated microglia exert neuroprotective depends on the context and the phase of of inflammation, neurogenic neuroinflam-
effects invitro through adenosine produc- the responses (FIG.1). It is therefore possible mation can become pathological (FIG.1).
tion113 (see REF.5 for a review). Similarly that broad anti-inflammatory interventions During normal neuronal activity, such as
the cytokineTNF (usually assumed to be may not only reduce the unwanted effects of that occurring in response to a touch or
pro-inflammatory) may have a physiological neuroinflammation but may also impede its brief pinch, glial cells and the vasculature
and neuroprotective role when present at the beneficial components. perform housekeeping functions. With
low tissue concentrations that are sufficient enhanced levels of activity (such as that fol-
for the activation of TNF receptor 2. Only at Effects in stressed tissue. Enhanced neu- lowing a minor injury), glial and vascular
higher concentrations, which are required ronal activity, such as that occurring during cells become activated in order to cope with
for TNF receptor 1 activation, does TNF encoding of a noxious stimulus or during enhanced metabolic demands. Synaptic
become a neurotoxic signal (see REF.114 for psychological stress, increases the metabolic spillover of neurotransmitters and accu-
a review). demands of the neuronal tissue. Neurogenic mulation of toxic metabolites or nitrogen
Thus, the available evidence suggests neuroinflammation, which increases regional and free oxygen radicals140,141 can occur.
that moderate levels of neuronal activity blood flow in the CNS can therefore provide Vasodilation will be engaged without any
exert anti-inflammatory reactions. It may the appropriate oxygen supply and transport detectable extravasation. LTP will be induced
therefore be speculated that the therapeutic capacity for metabolites. Beyond this, neu- at Cfibre synapses, resulting in hyperalgesia
use of electrical nerve stimulation such as rogenic neuroinflammation has a number of that initially fulfils the homeostatic functions
transcutaneous electrical nerve stimulation, additional effects. described above. With more persistent activ-
electroacupuncture115,116 or transcranial Enhanced activity at glutamatergic syn- ity in peptidergicCfibres (in the case of a
direct-current stimulation117 may exert ben- apses may result in excessive extracellular chronic inflammation or wound and in some
eficial effects in part by modulating neuroin- glutamate concentrations that can become forms of peripheral neuropathy), a transition
flammation and promoting neuroprotective highly toxic to neurons129. Astrocytes express to maladaptive forms of neuroinflamma-
and regenerative mechanisms in theCNS. glutamate transporters that remove gluta- tion starts with changes in the bloodCNS
The emerging roles of neuroinflamma- mate from the extracellular space and that barrier, leading to the presence of novel
tion in CNS functions (and dysfunctions) are upregulated by neuronal activation130 and pro- and/or anti-inflammatory mediators or
likewise call for a fresh look at old drugs. It is groupI mGluR signalling 91. Hence, activated cells. Neuroinflammation may reach neigh-
likely that some drugs may exploit their full astrocytes can potentially avoid or reduce bouring areas beyond the termination zones
therapeutic potential by modulating neuro- glutamate excitotoxicity. of activated primary afferents. Finally, a
inflammation rather than by their tradition- Neuroplasticity allows the nervous breakdown of the bloodCNS barrier results
ally ascribed modes of action only. Examples system to adapt to changing conditions. in the excessive extravasation of large mol-
include COX inhibitors (which have antino- Usually, this involves direct interactions ecules and recruitment of immune cells into
ciceptive effects in both the periphery and between neurons. A prominent example the CNS parenchyma, which can damage the
the spinal cord118), antipsychotics119, antide- of such an interaction is the induction of neuronal network. Higher-order neurons,
pressants that reduce neuroinflammation120, LTP at glutamatergic synapses131, including including descending-tract neurons, may
NATURE REVIEWS | NEUROSCIENCE VOLUME 15 | JANUARY 2014 | 49
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
amplify neurogenic neuroinflammation in Repetitive sessions of experimental normal resting mode even if classical mor-
the spinal cord and maintain immune-cell restraint in rats induce chronic stress and phological or immunohistochemical mark-
activation, as well as releasing and promoting lead to an increase in allograft inflammatory ers would suggest so. Instead, it has been
the release of further pro-inflammatory sub- factor1 IBA1 (also known as AIF1), a micro- proposed that microglia may still bear long-
stances. Glial cells may no longer reduce glu- glia marker, in a number of stress-related lasting (that is, plastic) changes that may
tamate excitotoxicity by uptake mechanisms brain nuclei156. Repeated defeat stress also alter their future responses to similar and/or
but may now release excessive amounts of increases the number of mast cells in the different challenges6, indicating that not only
glutamate (at least when challenged invitro), brain157. Chronic stress as a result of social neurons and Tcells express memory func-
causing excitotoxicity 142 and hyperalgesia in dominance paradigms leads to higher levels tions (see REF.170 for a review). Furthermore,
non-injured tissues. of inducible nitric oxide synthase and COX2 it is likely that neurogenic neuroinflamma-
gene expression in the rat spinal cord and tion and other forms of inflammation in the
Role in pain, stress and epilepsy to a lowered pain threshold over a similar CNS interact, possibly leading to priming of
Neurogenic neuroinflammation is likely to time course158. Chronic unpredictable stress CNS inflammatory reactions by conditions
have a role in a wide variety of conditions and methamphetamine further disrupt such as pain, psychological stress or epilepsy.
in the normal and diseased CNS, includ- the integrity of the bloodCNS barrier 159. This would be similar to the proposed impact
ing inflammatory and injury-related pain, Interestingly, chronic stress may also increase of systemic infection on the progression of
psychological stress and epilepsy. It may also gastrointestinal permeability with bacterial neurodegenerative disease121.
affect other functions and conditions such lipopolysaccharide translocation leading to An increasing body of literature shows
as neuropathic pain31, migraine143, sleep144, the release of inflammatory mediators in that neuronal activity leads to the activation
learning and memory formation145, mood the CNS160. Thus, neuronal activity patterns of glial cells and to the release of cytokines
disorders146 and autism147. that encode psychological stress responses and chemokines in the CNS. However,
and peripheral immune responses may act whether these responses alone fulfil the cri-
Neurogenic neuroinflammation in pain. synergistically to trigger neuroinflammation teria for inflammation has been a matter for
Neurogenic neuroinflammation boosts in thebrain. debate. The evidence described here dem-
nociception, as outlined above. Astrocyte onstrates that these reactions are not evoked
signalling through gap junctions and the Neurogenic neuroinflammation in epilepsy. in isolation but that neuronal activity trig-
diffusion of pro-inflammatory mediators Experimental induction of epileptic sei- gers finely orchestrated response patterns in
through spinal cord tissue may lead to zures by kainic-acid injections into rodent CNS areas that involve innate and adaptive
spreading of neurogenic neuroinflamma- cortical areas of the brain11 or electrical immune cells, vascular cells and neurons.
tion beyond the spinal projection zones of stimulation in the CA3 region of the hip- Although it may still be debatable whether
activated Cfibres. This may then contribute pocampus161 leads to mRNA upregulation the earliest and mildest responses deserve
to hyperalgesia in uninjured sites (second- of several cytokines (such asTNF, IL1 the label neuroinflammation, stronger and
ary hyperalgesia), mirror-image pain (pain and IL6) and classI MHC162 in brain areas longer-lasting neuronal activity clearly leads
at corresponding contralateral sites) and within hours of stimulation. Similarly, a to classical inflammatory signs, includ-
widespread pain134,148. single epileptic seizure in human patients ing plasma extravasation and activation of
Some forms of neuropathy lead to ectopic raises serum levels of IL1 receptor and IL6 immune cells. Homeostatic and maladap-
discharges in small afferent nerve fibres, (REF.163). Surgical removal of the epileptic tive reactions may be active simultaneously
including Cfibres149,150. It is therefore possible focus by anterior temporal lobectomy not with anti-inflammatory responses. In some
to speculate that some types of neuropathic only prevents any further epileptic seizures cases, it may not be possible to decide to
pain involve neurogenic neuroinflammation in these patients but also markedly reduces which category a given response should
in the spinal cord. Indeed, most animal mod- circulating levels of TNF and IL1164. Even be assigned. It therefore seems that no
els of peripheral neuropathy are character- brief epileptic seizures lead to perturbations unequivocal criteria would draw an objec-
ized by the activation of spinal glial cells (see of the bloodCNS barrier, with considerable tive line between homeostatic, physiological
REFS31,32 for reviews) and by the impair- extravasation of plasma proteins and recruit- para-inflammation on one hand and patho-
ment of the bloodspinal-cord barrier 151, ment of white blood cells into the brain logical neuroinflammation on the other.
including the recruitment of Tcells152. parenchyma165. Simultaneously, regenerative Furthermore, evidence suggests that classi-
processes are triggered, and these are also cal neuroinflammation also has a homeo-
Neurogenic neuroinflammation in stress. thought to involve classI MHC162,166. Taken static function. We therefore propose that
It is now becoming increasingly clear that together, the available data suggest that neurogenic neuroinflammation comprises
psychological stress involves not only neu- neuronal activity during epileptic seizures all of the responses outlined in FIG.1.
rohormonal responses153 but also compo- not only activates glial cells and leads to the In summary, the elaborated inflamma-
nents of neuroinflammation. For example, release of pro-inflammatory cytokines but tory response repertoire of CNS tissue may
in rats, acute stress as a result of immobi- also engages several additional parameters not only be used to deal with infectious,
lization activates mast cells and leads to of neurogenic neuroinflammation. Together, toxic or degenerative processes but also to
plasma extravasation in the diencephalon154. this further enhances the frequency and cope with the demands of increased levels
Inescapable footshock also causes upregu- severity of epileptic seizures27,167,168 (also see of neuronal activity and to enhance the
lation of the microglia activation marker REFS13,169 for reviews). computational power of neuronal networks
MHCII and downregulation of the neuronal in the CNS. However, neurogenic neuroin-
cell adhesion molecule CD200, which nor- Summary and outlook flammation may become maladaptive and
mally holds microglia in a non-activated It is possible that after a transient glial-cell aggravate clinical conditions such as pain,
state155. response, microglia may not return to their stress and epilepsy.
50 | JANUARY 2014 | VOLUME 15 www.nature.com/reviews/neuro
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
Dimitris N.Xanthos and Jrgen Sandkhler are at the by Src-family kinases in microglia: the role of tumor 48. McCulloch,J., Uddman,R., Kingman,T.A. &
Department of Neurophysiology, Center for Brain necrosis factor. Brain Behav. Immun. 24, 874880 Edvinsson,L. Calcitonin gene-related peptide:
(2010). functional role in cerebrovascular regulation. Proc.
Research, Medical University of Vienna, Spitalgasse 4,
24. Li,W.E. & Nagy,J.I. Activation of fibres in rat sciatic Natl Acad. Sci. USA 83, 57315735 (1986).
A-1090 Vienna, Austria. nerve alters phosphorylation state of connexin43 at 49. Duggan,A.W., Morton,C.R., Zhao,Z.Q. &
Correspondence to J.S. astrocytic gap junctions in spinal cord: evidence for Hendry,I.A. Noxious heating of the skin releases
email: juergen.sandkuehler@meduniwien.ac.at junction regulation by neuronalglial interactions. immunoreactive substance P in the substantia
Neuroscience 97, 113123 (2000). gelatinosa of the cat: a study with antibody
doi:10.1038/nrn3617 25. Kuroi,T. etal. Alterations in microglia and astrocytes microprobes. Brain Res. 403, 345349 (1987).
Published online 26 November 2013 in the trigeminal nucleus caudalis by repetitive TRPV1 50. Morton,C.R. & Hutchison,W.D. Release of sensory
stimulation on the trigeminal nociceptors. Neuroreport neuropeptides in the spinal cord: studies with
1. Medzhitov,R. Origin and physiological roles of 23, 560565 (2012). calcitonin gene-related peptide and galanin.
inflammation. Nature 454, 428435 (2008). 26. Town,T., Nikolic,V. & Tan,J. The microglial activation Neuroscience 31, 807815 (1989).
2. Maier,S.F., Goehler,L.E., Fleshner,M. & continuum: from innate to adaptive responses. 51. Xu,H.L. & Pelligrino,D.A. ATP release and
Watkins,L.R. The role of the vagus nerve in cytokine- J.Neuroinflammation 2, 24 (2005). hydrolysis contribute to rat pial arteriolar dilatation
tobrain communication. Ann. NY Acad. Sci. 840, 27. Maroso,M. etal. Toll-like receptor 4 and high- elicited by neuronal activation. Exp. Physiol. 92,
289300 (1998). mobility group box1 are involved in ictogenesis and 647651 (2007).
3. Hickey,W.F. & Kimura,H. Perivascular microglial cells can be targeted to reduce seizures. Nature Med. 16, 52. Tsuda,M., Ueno,S. & Inoue,K. Evidence for the
of the CNS are bone marrow-derived and present 413419 (2010). involvement of spinal endogenous ATP and P2X
antigen invivo. Science 239, 290292 (1988). 28. Liu,T., Gao,Y.J. & Ji,R.R. Emerging role of Toll-like receptors in nociceptive responses caused by
4. Balabanov,R., Beaumont,T. & Dore-Duffy,P. Role of receptors in the control of pain and itch. Neurosci. formalin and capsaicin in mice. Br. J.Pharmacol. 128,
central nervous system microvascular pericytes in Bull. 28, 131144 (2012). 14971504 (1999).
activation of antigen-primed splenic Tlymphocytes. 29. Nicotra,L., Loram,L.C., Watkins,L.R. & 53. Fields,R.D. & Burnstock,G. Purinergic signalling in
J.Neurosci. Res. 55, 578587 (1999). Hutchinson,M.R. Toll-like receptors in chronic pain. neuronglia interactions. Nature Rev. Neurosci. 7,
5. Ransohoff,R.M. & Cardona,A.E. The myeloid cells of Exp. Neurol. 234, 316329 (2012). 423436 (2006).
the central nervous system parenchyma. Nature 468, 30. Grinberg,Y.Y., Milton,J.G. & Kraig,R.P. Spreading 54. Yashiro,Y. & Ohhashi,T. Flow- and agonist-mediated
253262 (2010). depression sends microglia on Lvy flights. PLoS ONE nitric oxide- and prostaglandin-dependent dilation in
6. Kettenmann,H., Hanisch,U.K., Noda,M. & 6, e19294 (2011). spinal arteries. Am. J.Physiol. 273, H2217H2223
Verkhratsky,A. Physiology of microglia. Physiol. Rev. 31. Milligan,E.D. & Watkins,L.R. Pathological and (1997).
91, 461553 (2011). protective roles of glia in chronic pain. Nature Rev. 55. Heinemann,U., Schaible,H.G. & Schmidt,R.F.
7. Aguzzi,A., Barres,B.A. & Bennett,M.L. Microglia: Neurosci. 10, 2336 (2009). Changes in extracellular potassium concentration in
scapegoat, saboteur, or something else? Science 339, 32. Marchand,F., Perretti,M. & McMahon,S.B. Role of cat spinal cord in response to innocuous and noxious
156161 (2013). the immune system in chronic pain. Nature Rev. stimulation of legs with healthy and inflamed knee
8. Skaper,S.D., Giusti,P. & Facci,L. Microglia and mast Neurosci. 6, 521532 (2005). joints. Exp. Brain Res. 79, 283292 (1990).
cells: two tracks on the road to neuroinflammation. 33. Shubayev,V.I. & Myers,R.R. Axonal transport of 56. Vanegas,H. & Schaible,H.G. Prostaglandins and
FASEB J. 26, 31033117 (2012). TNF in painful neuropathy: distribution of ligand cyclooxygenases in the spinal cord. Prog. Neurobiol.
9. Melchior,B., Puntambekar,S.S. & Carson,M.J. tracer and TNF receptors. J.Neuroimmunol. 114, 64, 327363 (2001).
Microglia and the control of autoreactive Tcell 4856 (2001). 57. Xanthos,D.N., Pngel,I., Wunderbaldinger,G. &
responses. Neurochem. Int. 49, 145153 (2006). 34. Bradl,M., Bauer,J., Flgel,A., Wekerle,H. & Sandkhler,J. Effects of peripheral inflammation on
10. Ransohoff,R.M. & Brown,M.A. Innate immunity in Lassmann,H. Complementary contribution of CD4 the bloodspinal cord barrier. Mol. Pain 8, 44 (2012).
the central nervous system. J.Clin. Invest. 122, and CD8 T lymphocytes to Tcell infiltration of the 58. Kovac,A., Erickson,M.A. & Banks,W.A. Brain
11641171 (2012). intact and the degenerative spinal cord. Am. J.Pathol. microvascular pericytes are immunoactive in culture:
11. Minami,M., Kuraishi,Y. & Satoh,M. Effects of kainic 166, 14411450 (2005). cytokine, chemokine, nitric oxide, and LRP1
acid on messenger RNA levels of IL1 IL6, TNF and 35. Levite,M. Neurotransmitters activate Tcells and elicit expression in response to lipopolysaccharide.
LIF in the rat brain. Biochem. Biophys. Res. Commun. crucial functions via neurotransmitter receptors. Curr. J.Neuroinflammation 8, 139 (2011).
176, 593598 (1991). Opin. Pharmacol. 8, 460471 (2008). 59. Verma,S., Nakaoke,R., Dohgu,S. & Banks,W.A.
12. Vezzani,A. etal. Interleukin1 immunoreactivity and 36. Prodhomme,T., Weber,M.S., Steinman,L. & Release of cytokines by brain endothelial cells:
microglia are enhanced in the rat hippocampus by Zamvil,S.S. A neuropeptide in immune-mediated a polarized response to lipopolysaccharide. Brain
focal kainate application: functional evidence for inflammation, Y? Trends Immunol. 27, 164167 (2006). Behav. Immun. 20, 449455 (2006).
enhancement of electrographic seizures. J.Neurosci. 37. Flierl,M.A., Rittirsch,D., Huber-Lang,M., 60. Pocock,J.M. & Kettenmann,H. Neurotransmitter
19, 50545065 (1999). Sarma,J.V. & Ward,P.A. Catecholamines-crafty receptors on microglia. Trends Neurosci. 30,
13. Vezzani,A., French,J., Bartfai,T. & Baram,T.Z. The weapons in the inflammatory arsenal of immune/ 527535 (2007).
role of inflammation in epilepsy. Nature Rev. Neurol. inflammatory cells or opening Pandoras box? Mol. 61. Khakh,B.S. & North,R.A. P2X receptors as cell-
7, 3140 (2011). Med. 14, 195204 (2008). surface ATP sensors in health and disease. Nature
14. Combes,V., Guillemin,G.J., Chan-Ling,T., Hunt,N.H. 38. Sorkin,L.S. & McAdoo,D.J. Amino acids and 442, 527532 (2006).
& Grau,G.E. The crossroads of neuroinflammation in serotonin are released into the lumbar spinal cord of 62. Krizbai,I.A. etal. Expression of glutamate receptors
infectious diseases: endothelial cells and astrocytes. the anesthetized cat following intradermal capsaicin on cultured cerebral endothelial cells. J.Neurosci. Res.
Trends Parasitol. 28, 311319 (2012). injections. Brain Res. 607, 8998 (1993). 54, 814819 (1998).
15. Roosterman,D., Goerge,T., Schneider,S.W., 39. Men,D.S. & Matsui,Y. Peripheral nerve stimulation 63. Palmer,G.C. Neurochemical coupled actions of
Bunnett,N.W. & Steinhoff,M. Neuronal control of increases serotonin and dopamine metabolites in rat transmitters in the microvasculature of the brain.
skin function: the skin as a neuroimmunoendocrine spinal cord. Brain Res. Bull. 33, 625632 (1994). Neurosci. Biobehav. Rev. 10, 79101 (1986).
organ. Physiol. Rev. 86, 13091379 (2006). 40. Krakowski,M.L. & Owens,T. Naive T lymphocytes 64. Wang,J.X., Ikomi,F. & Ohhashi,T.
16. Berczi,I. & Szentivnyi,A. Neuroimmune Biology traffic to inflamed central nervous system, but require 5Hydroxytryptamine-induced endothelium-dependent
(Elsevier, 2009). antigen recognition for activation. Eur. J.Immunol. 30, and -independent relaxations in isolated dog anterior
17. Chiu,I.M., von Hehn,C.A. & Woolf,C.J. Neurogenic 10021009 (2000). spinal small arteries. Can. J.Physiol. Pharmacol. 75,
inflammation and the peripheral nervous system in 41. Kulka,M., Sheen,C.H., Tancowny,B.P., 357362 (1997).
host defense and immunopathology. Nature Neurosci. Grammer,L.C. & Schleimer,R.P. Neuropeptides 65. Beck,G.C. etal. Clinical review: immunomodulatory
15, 10631067 (2012). activate human mast cell degranulation and chemokine effects of dopamine in general inflammation. Crit. Care
18. Gruber-Schoffnegger,D. etal. Induction of thermal production. Immunology 123, 398410 (2008). 8, 485491 (2004).
hyperalgesia and synaptic long-term potentiation in 42. Xanthos,D.N. etal. Central nervous system mast cells 66. Mead,E.L. etal. Microglial neurotransmitter
the spinal cord lamina I by TNF and IL1 is mediated in peripheral inflammatory nociception. Mol. Pain 7, receptors trigger superoxide production in microglia;
by glial cells. J.Neurosci. 33, 65406551 (2013). 4258 (2011). consequences for microglial-neuronal interactions.
19. Hathway,G.J., Vega-Avelaira,D., Moss,A., Ingram,R. 43. Toda,H., Maruyama,H., Budgell,B. & Kurosawa,M. J.Neurochem. 121, 287301 (2012).
& Fitzgerald,M. Brief, low frequency stimulation of rat Responses of dorsal spinal cord blood flow to noxious 67. Gyoneva,S. & Traynelis,S.F. Norepinephrine
peripheral Cfibres evokes prolonged microglial- mechanical stimulation of the skin in anesthetized modulates the motility of resting and activated
induced central sensitization in adults but not in rats. J.Physiol. Sci. 58, 263270 (2008). microglia via different adrenergic receptors. J.Biol.
neonates. Pain 144, 110118 (2009). 44. Zhao,F. etal. fMRI investigation of the effect of local Chem. 288, 1529115302 (2013).
20. Zochodne,D.W., Sun,H. & Li,X.Q. Evidence that and systemic lidocaine on noxious electrical 68. Shao,W. etal. Suppression of neuroinflammation by
nitric oxide- and opioid-containing interneurons stimulation-induced activation in spinal cord. Pain astrocytic dopamine D2 receptors via B-crystallin.
innervate vessels in the dorsal horn of the spinal cord 145, 110119 (2009). Nature 494, 9094 (2013).
of rats. J.Physiol. 532, 749758 (2001). 45. Ching,S. etal. Endothelial-specific knockdown of 69. Verge,G.M. etal. Fractalkine (CX3CL1) and
21. Beggs,S., Liu,X.J., Kwan,C. & Salter,M.W. interleukin1 (IL1) type1 receptor differentially alters fractalkine receptor (CX3CR1) distribution in spinal
Peripheral nerve injury and TRPV1expressing primary CNS responses to IL1 depending on its route of cord and dorsal root ganglia under basal and
afferent Cfibers cause opening of the bloodbrain administration. J.Neurosci. 27, 1047610486 (2007). neuropathic pain conditions. Eur. J.Neurosci. 20,
barrier. Mol. Pain 6, 7479 (2010). 46. Burnstock,G. Dual control of vascular tone and 11501160 (2004).
22. Svensson,C.I. etal. Activation of p38 mitogen- remodelling by ATP released from nerves and 70. Cardona,A.E. etal. Control of microglial
activated protein kinase in spinal microglia is a critical endothelial cells. Pharmacol. Rep. 60, 1220 (2008). neurotoxicity by the fractalkine receptor. Nature
link in inflammation-induced spinal pain processing. 47. Annunziata,P., Cioni,C., Santonini,R. & Paccagnini,E. Neurosci. 9, 917924 (2006).
J.Neurochem. 86, 15341544 (2003). Substance P antagonist blocks leakage and reduces 71. Clark,A.K. & Malcangio,M. Microglial signalling
23. Zhong,Y. etal. The direction of synaptic plasticity activation of cytokine-stimulated rat brain mechanisms: cathepsin S and fractalkine. Exp. Neurol.
mediated by Cfibers in spinal dorsal horn is decided endothelium. J.Neuroimmunol. 131, 4149 (2002). 234, 283292 (2012).
NATURE REVIEWS | NEUROSCIENCE VOLUME 15 | JANUARY 2014 | 51
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
72. Milligan,E.D., Sloane,E.M. & Watkins,L.R. Glia in 96. Ji,R.R., Xu,Z.Z., Strichartz,G. & Serhan,C.N. is there a mutual influence? Pharmacol. Rep. 59,
pathological pain: a role for fractalkine. Emerging roles of resolvins in the resolution of 129138 (2007).
J.Neuroimmunol. 198, 113120 (2008). inflammation and pain. Trends Neurosci. 34, 599609 122. Downer,E.J. Cannabinoids and innate immunity:
73. Perea,G., Navarrete,M. & Araque,A. Tripartite (2011). taking a toll on neuroinflammation.
synapses: astrocytes process and control synaptic 97. Suzuki,T. etal. Production and release of ScientificWorldJournal 11, 855865 (2011).
information. Trends Neurosci. 32, 421431 (2009). neuroprotective tumor necrosis factor by P2X7 receptor- 123. Ramirez,S.H. etal. Activation of cannabinoid
74. Dityatev,A. & Rusakov,D.A. Molecular signals of activated microglia. J.Neurosci. 24, 17 (2004). receptor 2 attenuates leukocyteendothelial cell
plasticity at the tetrapartite synapse. Curr. Opin. 98. Pintr,E., Helyes,Z. & Szolcsnyi,J. Inhibitory effect interactions and bloodbrain barrier dysfunction
Neurobiol. 21, 353359 (2011). of somatostatin on inflammation and nociception. under inflammatory conditions. J.Neurosci. 32,
75. Grace,P.M., Rolan,P.E. & Hutchinson,M.R. Pharmacol. Ther. 112, 440456 (2006). 40044016 (2012).
Peripheral immune contributions to the maintenance 99. Solway,B., Bose,S.C., Corder,G., Donahue,R.R. & 124. Hutchinson,M.R. etal. Possible involvement of toll-
of central glial activation underlying neuropathic pain. Taylor,B.K. Tonic inhibition of chronic pain by like receptor 4/myeloid differentiation factor2
Brain Behav. Immun. 25, 13221332 (2011). neuropeptide Y. Proc. Natl Acad. Sci. USA 108, activity of opioid inactive isomers causes spinal
76. Drdla,R. & Sandkhler,J. Long-term potentiation at 72247229 (2011). proinflammation and related behavioral
Cfibre synapses by low-level presynaptic activity 100. Orr,A.G., Orr,A.L., Li,X.J., Gross,R.E. & consequences. Neuroscience 167, 880893 (2010).
invivo. Mol. Pain 4, 18 (2008). Traynelis,S.F. Adenosine A2A receptor mediates 125. Drdla,R., Gassner,M., Gingl,E. & Sandkhler,J.
77. Miyano,K. etal. Activation of the neurokinin1 microglial process retraction. Nature Neurosci. 12, Induction of synaptic long-term potentiation after
receptor in rat spinal astrocytes induces Ca2+ release 872878 (2009). opioid withdrawal. Science 325, 207210 (2009).
from IP3sensitive Ca2+ stores and extracellular Ca2+ 101. Neumann,H., Cavalie,A., Jenne,D.E. & Wekerle,H. 126. Ferrini,F. etal. Morphine hyperalgesia gated through
influx through TRPC3. Neurochem. Int. 57, 923934 Induction of MHC classI genes in neurons. Science microglia-mediated disruption of neuronal Cl
(2010). 269, 549552 (1995). homeostasis. Nature Neurosci. 16, 183192 (2013).
78. Tumati,S. etal. Tachykinin NK1 receptor antagonist 102. Neumann,H., Misgeld,T., Matsumuro,K. & 127. Orr,S.K. & Bazinet,R.P. The emerging role of
coadministration attenuates opioid withdrawal- Wekerle,H. Neurotrophins inhibit major docosahexaenoic acid in neuroinflammation. Curr.
mediated spinal microglia and astrocyte activation. histocompatibility classII inducibility of microglia: Opin. Investig. Drugs 9, 735743 (2008).
Eur. J.Pharmacol. 684, 6470 (2012). involvement of the p75 neurotrophin receptor. Proc. 128. Lu,Y., Zhao,L. X., Cao,D. L. & Gao,Y. J. Spinal
79. Rasley,A., Bost,K.L., Olson,J.K., Miller,S.D. & Natl Acad. Sci. USA 95, 57795784 (1998). injection of docosahexaenoic acid attenuates
Marriott,I. Expression of functional NK1 receptors in 103. Neumann,H., Boucraut,J., Hahnel,C., Misgeld,T. & carrageenan-induced inflammatory pain through
murine microglia. Glia 37, 258267 (2002). Wekerle,H. Neuronal control of MHC classII inhibition of microglia-mediated neuroinflammation in
80. Davis,M.J. & Sharma,N.R. Calcium-release- inducibility in rat astrocytes and microglia. Eur. the spinal cord. Neuroscience 241, 2231 (2013).
activated calcium influx in endothelium. J.Vasc. Res. J.Neurosci. 8, 25822590 (1996). 129. Dugan,L.L. & Choi,D.W. Excitotoxicity, free
34, 186195 (1997). 104. Neumann,H. Control of glial immune function by radicals, and cell membrane changes. Ann. Neurol.
81. Pober,J.S. & Sessa,W.C. Evolving functions of neurons. Glia 36, 191199 (2001). 35, S17S21 (1994).
endothelial cells in inflammation. Nature Rev. 105. Black,J.A., Liu,S. & Waxman,S.G. Sodium channel 130. Benediktsson,A.M. etal. Neuronal activity regulates
Immunol. 7, 803815 (2007). activity modulates multiple functions in microglia. Glia glutamate transporter dynamics in developing
82. Matsui,T. etal. Release of prostaglandin E2 and nitric 57, 10721081 (2009). astrocytes. Glia 60, 175188 (2012).
oxide from spinal microglia is dependent on activation 106. McMahon,S.B. & Malcangio,M. Current challenges 131. Bliss,T.V.P. & Collingridge,G.L. A synaptic model of
of p38 mitogen-activated protein kinase. Anesth. in glia-pain biology. Neuron 64, 4654 (2009). memory: long-term potentiation in the hippocampus.
Analg. 111, 554560 (2010). 107. Wake,H., Moorhouse,A.J., Miyamoto,A. & Nature 361, 3139 (1993).
83. Coderre,T.J., Gonzales,R., Goldyne,M.E., West,J. & Nabekura,J. Microglia: actively surveying and shaping 132. Ikeda,H., Heinke,B., Ruscheweyh,R. & Sandkhler,J.
Levine,J.D. Noxious stimulus-induced increase in neuronal circuit structure and function. Trends Synaptic plasticity in spinal lamina I projection
spinal prostaglandin E2 is noradrenergic terminal- Neurosci. 36, 209217 (2013). neurons that mediate hyperalgesia. Science 299,
dependent. Neurosci. Lett. 115, 253258 (1990). 108. Graeber,M.B. Changing face of microglia. Science 12371240 (2003).
84. Byrnes,K.R., Loane,D.J. & Faden,A.I. Metabotropic 330, 783788 (2010). 133. Ikeda,H. etal. Synaptic amplifier of inflammatory pain
glutamate receptors as targets for multipotential 109. Zhang,J. etal. Neuron-derived IgG protects in the spinal dorsal horn. Science 312, 16591662
treatment of neurological disorders. dopaminergic neurons from insult by 6OHDA and (2006).
Neurotherapeutics 6, 94107 (2009). activates microglia through the FcR I and TLR4 134. Sandkhler,J. Models and mechanisms of
85. Biber,K. etal. Expression and signaling of group I pathways. Int. J.Biochem. Cell Biol. 45, 19111920 hyperalgesia and allodynia. Physiol. Rev. 89,
metabotropic glutamate receptors in astrocytes and (2013). 707758 (2009).
microglia. J.Neurochem. 72, 16711680 (1999). 110. Vitkovic,L., Maeda,S. & Sternberg,E. Anti- 135. Sandkhler,J. & Gruber-Schoffnegger,D.
86. Kumar,V., Fahey,P.G., Jong,Y.J., Ramanan,N. & inflammatory cytokines: expression and action in the Hyperalgesia by synaptic long-term potentiation
OMalley,K.L. Activation of intracellular brain. Neuroimmunomodulation 9, 295312 (2001). (LTP): an update. Curr. Opin. Pharmacol. 12, 1827
metabotropic glutamate receptor 5 in striatal 111. Elenkov,I.J. & Chrousos,G.P. Stress hormones, (2011).
neurons leads to upregulation of genes associated proinflammatory and antiinflammatory cytokines, and 136. Lever,I.J. etal. Brain-derived neurotrophic factor is
with sustained synaptic transmission including Arc/ autoimmunity. Ann. NY Acad. Sci. 966, 290303 released in the dorsal horn by distinctive patterns of
Arg3.1 protein. J.Biol. Chem. 287, 54125425 (2002). afferent fiber stimulation. J.Neurosci. 21, 44694477
(2012). 112. Lyons,A. etal. Fractalkine-induced activation of the (2001).
87. Byrnes,K.R. etal. Metabotropic glutamate receptor 5 phosphatidylinositol3 kinase pathway attentuates 137. Coull,J.A.M. etal. Trans-synaptic shift in anion
activation inhibits microglial associated inflammation microglial activation invivo and invitro. gradient in spinal lamina I neurons as a mechanism of
and neurotoxicity. Glia 57, 550560 (2009). J.Neurochem. 110, 15471556 (2009). neuropathic pain. Nature 424, 938942 (2003).
88. Byrnes,K.R. etal. Activation of metabotropic 113. Lauro,C. etal. Activity of adenosine receptors type1 138. Zhang,W., Liu,L.Y. & Xu,T.L. Reduced potassium-
glutamate receptor 5 improves recovery after spinal Is required for CX3CL1mediated neuroprotection and chloride cotransporter expression in spinal cord
cord injury in rodents. Ann. Neurol. 66, 6374 neuromodulation in hippocampal neurons. J.Immunol. dorsal horn neurons contributes to inflammatory pain
(2009). 180, 75907596 (2008). hypersensitivity in rats. Neuroscience 152, 502510
89. Chen,J., Heinke,B. & Sandkhler,J. Activation of 114. Santello,M. & Volterra,A. TNF in synaptic function: (2008).
group I metabotropic glutamate receptors induces switching gears. Trends Neurosci. 35, 139. Price,T.J., Cervero,F. & De Koninck,Y. Role of cation-
long-term depression at sensory synapses in 638647 (2012). chloride-cotransporters (CCC) in pain and hyperalgesia.
superficial spinal dorsal horn. Neuropharmacology 115. Sun,S. etal. Evidence for suppression of Curr. Top. Med. Chem. 5, 547555 (2005).
39, 22312243 (2000). electroacupuncture on spinal glial activation and 140. Schwartz,E.S., Lee,I., Chung,K. & Chung,J.M.
90. Deng,W., Wang,H., Rosenberg,P.A., Volpe,J.J. & behavioral hypersensitivity in a rat model of Oxidative stress in the spinal cord is an important
Jensen,F.E. Role of metabotropic glutamate monoarthritis. Brain Res. Bull. 75, 8393 (2008). contributor in capsaicin-induced mechanical secondary
receptors in oligodendrocyte excitotoxicity and 116. Wang,Q. etal. Electroacupuncture pretreatment hyperalgesia in mice. Pain 138, 514524 (2008).
oxidative stress. Proc. Natl Acad. Sci. USA 101, attenuates cerebral ischemic injury through 7 141. Salvemini,D., Little,J.W., Doyle,T. & Neumann,W.L.
77517756 (2004). nicotinic acetylcholine receptor-mediated inhibition of Roles of reactive oxygen and nitrogen species in pain.
91. Devaraju,P., Sun,M.Y., Myers,T.L., Lauderdale,K. & high-mobility group box 1 release in rats. Free Radic. Biol. Med. 51, 951966 (2011).
Fiacco,T.A. Astrocytic group I mGluR dependent J.Neuroinflammation 9, 24 (2012). 142. Bal-Price,A. & Brown,G.C. Inflammatory
potentiation of astrocytic glutamate and potassium 117. Rueger,M.A. etal. Multi-session transcranial direct neurodegeneration mediated by nitric oxide from
uptake. J.Neurophysiol. 109, 24042414 (2013). current stimulation (tDCS) elicits inflammatory and activated glia-inhibiting neuronal respiration, causing
92. Gillard,S.E., Tzaferis,J., Tsui,H.C. & Kingston,A.E. regenerative processes in the rat brain. PLoS ONE. 7, glutamate release and excitotoxicity. J.Neurosci. 21,
Expression of metabotropic glutamate receptors in rat e43776 (2012). 64806491 (2001).
meningeal and brain microvasculature and choroid 118. Svensson,C.I. & Yaksh,T.L. The spinal 143. Brack,A., Rittner,H.L. & Stein,C. Neurogenic painful
plexus. J.Comp. Neurol. 461, 317332 (2003). phospholipase-cyclooxygenase-prostanoid cascade in inflammation. Curr. Opin. Anaesthesiol. 17, 461464
93. Collard,C.D. etal. Neutrophil-derived glutamate nociceptive processing. Annu. Rev. Pharmacol. Toxicol. (2004).
regulates vascular endothelial barrier function. J.Biol. 42, 553583 (2002). 144. Zhu,B. etal. Sleep disturbance induces
Chem. 277, 1480114811 (2002). 119. Mller,N., Myint,A.M. & Schwarz,M.J. neuroinflammation and impairment of learning and
94. Moore,K.W., de Waal,M.R., Coffman,R.L. & Immunological treatment options for schizophrenia. memory. Neurobiol. Dis. 48, 348355 (2012).
OGarra,A. Interleukin10 and the interleukin10 Curr. Pharm. Biotechnol. 13, 16061613 (2012). 145. Hein,A.M. & OBanion,M.K. Neuroinflammation
receptor. Annu. Rev. Immunol. 19, 683765 (2001). 120. Hashioka,S. Antidepressants and neuroinflammation: and memory: the role of prostaglandins. Mol.
95. Park,C.K. etal. Resolving TRPV1- and can antidepressants calm glial rage down? Mini Rev. Neurobiol. 40, 1532 (2009).
TNFmediated spinal cord synaptic plasticity and Med. Chem. 11, 555564 (2011). 146. Jones,K.A. & Thomsen,C. The role of the innate
inflammatory pain with neuroprotectin D1. 121. Mlodzikowska-Albrecht,J., Steinborn,B. & immune system in psychiatric disorders. Mol. Cell
J.Neurosci. 31, 1507215085 (2011). Zarowski,M. Cytokines, epilepsy and epileptic drugs-- Neurosci. 53, 5262 (2013).
52 | JANUARY 2014 | VOLUME 15 www.nature.com/reviews/neuro
2014 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
147. Depino,A.M. Peripheral and central inflammation in 157. Cirulli,F., Pistillo,L., De Acetis,L., Alleva,E. & Aloe,L. 166. Oliveira,A.L.R. etal. A role for MHC classI
autism spectrum disorders. Mol. Cell Neurosci. 53, Increased number of mast cells in the central nervous molecules in synaptic plasticity and regeneration of
6976 (2013). system of adult male mice following chronic neurons after axotomy. Proc. Natl Acad. Sci. USA
148. Sandkhler,J. in Wall and Melzacks Textbook of Pain subordination stress. Brain Behav. Immun. 12, 101, 1784317848 (2004).
(eds Koltzenburg,M., McMahon,S., Tracey,I. & 123133 (1998). 167. Rodgers,K.M. etal. The cortical innate immune
Turk,D.C.) 94110 (Elsevier, 2013). 158. Rivat,C. etal. Chronic stress induces transient spinal response increases local neuronal excitability
149. Han,C. H., Lee,D. H. & Chung, J. M. Characteristics neuroinflammation, triggering sensory hypersensitivity leading to seizures. Brain 132, 24782486
of ectopic discharges in a rat neuropathic pain model. and long-lasting anxiety-induced hyperalgesia. Pain (2009).
Pain 84, 253261 (2000). 150, 358368 (2010). 168. Vezzani,A., Friedman,A. & Dingledine,R.J. The role
150. Pan,H.L., Eisenach,J.C. & Chen,S.R. Gabapentin 159. Northrop,N.A. & Yamamoto,B.K. Persistent of inflammation in epileptogenesis.
suppresses ectopic nerve discharges and reverses neuroinflammatory effects of serial exposure to stress Neuropharmacology 69, 1624 (2013).
allodynia in neuropathic rats. J.Pharmacol. Exp. Ther. and methamphetamine on the bloodbrain barrier. 169. Devinsky,O., Vezzani,A., Najjar,S., de
288, 10261030 (1999). J.Neuroimmune Pharmacol. 7, 951968 (2012). Lanerolle,N.C. & Rogawski,M.A. Glia and epilepsy:
151. Echeverry,S., Shi,X.Q., Rivest,S. & Zhang,J. 160. Grate,I. etal. Origin and consequences of brain Toll- excitability and inflammation. Trends Neurosci. 36,
Peripheral nerve injury alters bloodspinal cord like receptor 4 pathway stimulation in an experimental 174184 (2013).
barrier functional and molecular integrity through a model of depression. J.Neuroinflammation 8, 151 170. Jameson,S.C. & Masopust,D. Diversity in Tcell
selective inflammatory pathway. J.Neurosci. 31, (2011). memory: an embarrassment of riches. Immunity 31,
1081910828 (2011). 161. De Simoni,M.G. etal. Inflammatory cytokines and 859871 (2009).
152. Sweitzer,S.M., Hickey,W.F., Rutkowski,M.D., related genes are induced in the rat hippocampus by 171. Katsanos,G.S. etal. Impact of substance P on
Pahl,J.L. & DeLeo,J.A. Focal peripheral nerve injury limbic status epilepticus. Eur. J.Neurosci. 12, cellular immunity. J.Biol. Regul. Homeost. Agents
induces leukocyte trafficking into the central nervous 26232633 (2000). 22, 9398 (2008).
system: potential relationship to neuropathic pain. 162. Corriveau,R.A., Huh,G.S. & Shatz,C.J. Regulation 172. Lee,J., Yamamoto,T., Kuramoto,H. & Kadowaki,M.
Pain 100, 163170 (2002). of classI MHC gene expression in the developing and TRPV1 expressing extrinsic primary sensory neurons
153. Jols,M. & Baram,T.Z. The neuro-symphony of mature CNS by neural activity. Neuron 21, 505520 play a protective role in mouse oxazolone-induced
stress. Nature Rev. Neurosci. 10, 459466 (2009). (1998). colitis. Auton. Neurosci. 166, 7276 (2012).
154. Esposito,P. etal. Acute stress increases permeability 163. Lehtimki,K.A. etal. Increased plasma levels of
of the bloodbrain-barrier through activation of brain cytokines after seizures in localization-related epilepsy.
mast cells. Brain Res. 888, 117127 (2001). Acta Neurol. Scand. 116, 226230 (2007). Acknowledgements
155. Frank,M.G., Baratta,M.V., Sprunger,D.B., 164. Quirico-Santos,T. etal. Resection of the The work was supported in part by grants received by J.S.
Watkins,L.R. & Maier,S.F. Microglia serve as a epileptogenic lesion abolishes seizures and reduces from the Austrian Science Fund (FWF) (project W1205) and
neuroimmune substrate for stress-induced inflammatory cytokines of patients with temporal the Vienna Science and Technology Fund (WWTF). We thank
potentiation of CNS pro-inflammatory cytokine lobe epilepsy. J.Neuroimmunol. 254, 125130 H. Lassmann, Vienna, for useful discussions and helpful
responses. Brain Behav. Immun. 21, 4759 (2007). (2013). comments on an earlier version of the manuscript.
156. Tynan,R.J. etal. Chronic stress alters the density and 165. Marchi,N. etal. Bloodbrain barrier damage, but
morphology of microglia in a subset of stress- not parenchymal white blood cells, is a hallmark of
responsive brain regions. Brain Behav. Immun. 24, seizure activity. Brain Res. 1353, 176186 Competing interests statement
10581068 (2010). (2010). The authors declare no competing interests.
NATURE REVIEWS | NEUROSCIENCE VOLUME 15 | JANUARY 2014 | 53
2014 Macmillan Publishers Limited. All rights reserved
You might also like
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Early Prediction of Poststroke Rehabilitation Outcomes Using Wearable SensorsDocument33 pagesEarly Prediction of Poststroke Rehabilitation Outcomes Using Wearable SensorsGustavo CabanasNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hedman 2018Document8 pagesHedman 2018Gustavo CabanasNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Cervical Joint DysfunctionDocument5 pagesCervical Joint DysfunctionGustavo CabanasNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Mechanisms of AxonDocument8 pagesMechanisms of AxonGustavo CabanasNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Oligodendrocytes Biology and PathologyDocument17 pagesOligodendrocytes Biology and PathologyGustavo CabanasNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Algorithm Hypertension Sci PDFDocument1 pageAlgorithm Hypertension Sci PDFGustavo CabanasNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Pain Neuroscience EducationDocument26 pagesPain Neuroscience EducationGustavo Cabanas100% (1)
- SinapsisDocument4 pagesSinapsisGustavo CabanasNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Anatomical Substrates of Oculomotor Control: Jean A Btittner-Ennever and Anja KE HorntDocument8 pagesAnatomical Substrates of Oculomotor Control: Jean A Btittner-Ennever and Anja KE HorntGustavo CabanasNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- 2 Types Functional Capacity EvaluationDocument6 pages2 Types Functional Capacity EvaluationGustavo CabanasNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Dynamic Gait Index: (Original 8-Item Test)Document2 pagesDynamic Gait Index: (Original 8-Item Test)Gustavo Cabanas0% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Neurobiology of Fut IntakeDocument12 pagesNeurobiology of Fut IntakeGustavo CabanasNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Somatosensory Processes Subserving Perception and ActionDocument51 pagesSomatosensory Processes Subserving Perception and ActionGustavo CabanasNo ratings yet
- FasciaDocument53 pagesFasciaGustavo CabanasNo ratings yet
- A Model For The Evolution of Decussation PDFDocument5 pagesA Model For The Evolution of Decussation PDFGustavo CabanasNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Russian Psychology and Neuropsychotherapy: Comparative AnalysisDocument19 pagesRussian Psychology and Neuropsychotherapy: Comparative AnalysisGustavo CabanasNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Echocardiography in Fontan PhysiologyDocument30 pagesEchocardiography in Fontan PhysiologyNavojit ChowdhuryNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Interaksi Jantung ParuDocument29 pagesInteraksi Jantung ParuSusilo Aja100% (1)
- Jadwal Perkuliahan Minggu 4&5Document4 pagesJadwal Perkuliahan Minggu 4&5Usan DaryamanNo ratings yet
- Thyroid Disorders Testing AlgorithmDocument1 pageThyroid Disorders Testing AlgorithmRezi HelperNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Eksudat:: Fisiologi Dan Cara Pengambilan SampelDocument13 pagesEksudat:: Fisiologi Dan Cara Pengambilan SampelJerry TjoanatanNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Casos EndocrinoDocument72 pagesCasos EndocrinoAlfredo JaureguiNo ratings yet
- Seminar ReportDocument28 pagesSeminar ReportlaxmikantchhipaNo ratings yet
- The Ovarian Cycle.Document20 pagesThe Ovarian Cycle.Salman KhanNo ratings yet
- Female Reproductive Anatomy - KWDocument25 pagesFemale Reproductive Anatomy - KWabyannaybaNo ratings yet
- Ginecologie An.v EngDocument67 pagesGinecologie An.v EngAhmad Abu KushNo ratings yet
- NBDE I-Dental Anatomy High Yield Notes: Study Online atDocument2 pagesNBDE I-Dental Anatomy High Yield Notes: Study Online atSchat ZiNo ratings yet
- Dandy Walker SyndromeDocument9 pagesDandy Walker SyndromeDarshika Vyas MohanNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Understanding Human Sexuality 12th Edition Hyde Test Bank 1Document36 pagesUnderstanding Human Sexuality 12th Edition Hyde Test Bank 1Larry Kershaw100% (42)
- C 39Document8 pagesC 39Tammie Gore100% (2)
- Personal Training Level 3 ManualDocument358 pagesPersonal Training Level 3 ManualAATdale94% (18)
- The Respiratory System: Human AnatomyDocument47 pagesThe Respiratory System: Human AnatomyChelseaNo ratings yet
- Previous IB Exam QuestionsDocument12 pagesPrevious IB Exam QuestionsJohn OsborneNo ratings yet
- Odontogenic and Non Odontogenic PainDocument44 pagesOdontogenic and Non Odontogenic Painjohnjpw 92No ratings yet
- Lab Write-Up Microscopic CLT 202Document3 pagesLab Write-Up Microscopic CLT 202Lisa LovellNo ratings yet
- Renal Session 2 PDFDocument101 pagesRenal Session 2 PDFDokki ScanNo ratings yet
- Common Medical AbbreviationsDocument10 pagesCommon Medical AbbreviationsPrincess MariscotesNo ratings yet
- Questionnaires in Science and Health Quiz BeeDocument4 pagesQuestionnaires in Science and Health Quiz BeeMikale Keoni Wikolia83% (29)
- Muscle Tissue SummaryDocument2 pagesMuscle Tissue SummaryLindenScholesNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Cardiovascular TestDocument4 pagesCardiovascular Testglai RamosNo ratings yet
- Consoling Friend's Grieving Mother in Strange CircumstancesDocument249 pagesConsoling Friend's Grieving Mother in Strange CircumstancesAnonymous pmVnncYJNo ratings yet
- Muscular System Concept MapDocument1 pageMuscular System Concept MapKimsabu Doldam100% (1)
- Leukemia Case StudyDocument10 pagesLeukemia Case StudyQueennieMarelRamos100% (1)
- Worksheet 1 Integumentary SystemDocument2 pagesWorksheet 1 Integumentary SystemSpencer CuencaNo ratings yet
- DigestivesystemDocument35 pagesDigestivesystemComet SkyeNo ratings yet
- Unit - V Chapter-22. Excretory Products and Their EliminationDocument20 pagesUnit - V Chapter-22. Excretory Products and Their EliminationVishal Kumar SinghNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)