Professional Documents
Culture Documents
Giant Encephalocele A Study of 14 CASES
Uploaded by
Sayyid Hakam PerkasaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Giant Encephalocele A Study of 14 CASES
Uploaded by
Sayyid Hakam PerkasaCopyright:
Available Formats
Original Paper
Pediatr Neurosurg 2011;47:406411 Received: July 15, 2010
Accepted after revision: April 17, 2012
DOI: 10.1159/000338895
Published online: July 7, 2012
Giant Encephalocele: A Study of 14
Patients
A.K. Mahapatra
Department of Neurosurgery, AIIMS, New Delhi, India
Key Words shunt for increasing hydrocephalus. Results: Other associ-
Giant encephalocele Surgery Outcome Cranioplasty ated anomalies recorded were acquired Chiari malformation
in 3 patients, secondary craniostenosis with microcephaly in
5, and syringomyelia in 1 patient. All the patients underwent
Abstract repair of encephalocele and 4 had suturectomy of coronal
Background: Giant encephalocele is a rare condition and suture for the secondary craniostenosis. There were 2 post-
few published reports are available in the English literature. operative deaths due to hypothermia. Among the 12 surviv-
It is a challenge to neurosurgeons, even today. This series ing patients, 9 had a good outcome and 3 had poor mental
consists of 14 patients with giant encephaloceles treated at development. The present study shows overall good out-
our institute. Material and Observation: Over a period of 8 comes in 9/14 (66%) patients. Copyright 2012 S. Karger AG, Basel
years, from 2002 to 2009, 110 patients with encephaloceles
were managed at our institute. Amongst them, 14 were chil-
dren with giant encephaloceles. All patients had CT/MRI or
both prior to surgery, and all were operated upon. Four pa- Introduction
tients were neonates, under 1 month of age, and 9/14 pa-
tients (64%) were under 3 months. The youngest child was a Giant encephalocele is a rare clinical condition. Even
newborn baby aged 2 days. Except for 1 with an anterior en- today it is a formidable challenge to neurosurgeons [1, 2].
cephalocele, the rest were patients with occipital encepha- The challenge is due to the amount of brain tissue, which
loceles. A CT scan was performed on 5 and an MRI on 1 pa- forms the content of the encephalocele, intraoperative
tient. Both CT and MRI scans were performed on the other 8 blood loss and intra- and postoperative hypothermia.
patients. MRI/CT showed hydrocephalus in 10/14 patients. The condition is rarely reported in the literature. Except
Of these, 7 required ventriculoperitoneal (VP) shunt, and the for a few case reports [15], no series has been published
remaining 3 with mild to moderate hydrocephalus did not. in the literature. Current analysis deals with 14 cases of
Of the 7 patients who underwent VP shunt, 5 had a shunt giant encephaloceles treated at our center.
during the encephalocele repair and 2 had a postoperative
36.69.228.119 - 8/6/2017 4:09:04 PM
2012 S. Karger AG, Basel Prof. Dr. A.K. Mahapatra
10162291/11/04760406$38.00/0 Department of Neurosurgery
Fax +41 61 306 12 34 AIIMS
E-Mail karger@karger.ch Accessible online at: New Delhi 110029 (India)
www.karger.com www.karger.com/pne Tel. +91 112 658 8927, E-Mail akmahapatra_22000@yahoo.com
Downloaded by:
Color version available online
Color version available online
Fig. 1. Clinical photograph of a case of occipital giant encephalo- Fig. 2. Clinical photograph of a case of anterior fontanel encepha-
cele. locele.
Fig. 3. CT scan showing occipital giant encephalocele with bone Fig. 4. MRI of occipital encephalocele.
defect.
Materials and Methods occipital or suboccipital location (fig.1). In the 1 patient with an-
terior encephalocele, the encephalocele was coming through the
This was a retrospective study at our institute, over an 8-year anterior fontanel (fig.2).
period, from 2002 to 2009. During this period, a total of 110 en- All the patients had imaging by CT or MRI (fig.3). Five pa-
cephaloceles were treated, among them 14 patients with giant en- tients had CT and 1 patient had MRI only. The remaining 8 pa-
cephaloceles. All patients had CT, MRI or both, to evaluate the tients had both MRI and CT. CT provided additional information
associated brain anomalies and to plan the surgical procedure. All regarding the bony defect. Imaging revealed hydrocephali in 10
patients were followed up at the outpatient department. patients, of which 7 were gross or significant, and in 3 patients
The patients ranged in age from 2 days to 4 years. Nine patients ventriculomegaly was considered mild to moderate. Three pa-
were under 3 months and among them 4 were neonates of less tients had Chiari II malformation and 1 patient had syringomy-
than 30 days. All the neonates weighed between 2 and 2.5 kg. Only elia. Five patients had associated secondary craniostenosis, all
2 patients were over 1 year of age. Boys outnumbered girls, as there with fused coronal suture and closed anterior fontanel. MRI re-
were 9 boys and 5 girls. Except for 1 patient who had anterior fon- vealed the content of the encephalocele (fig.4), and in 3 patients
tanel encephalocele, the remaining 13 had encephalocele in an there was no brain tissue inside the sac. CT scans were performed
36.69.228.119 - 8/6/2017 4:09:04 PM
Giant Encephalocele: A Study of 14 Pediatr Neurosurg 2011;47:406411 407
Patients
Downloaded by:
to evaluate the size of the bone defect. In 3 patients the defect in
Color version available online
the occipital bone was small and measured less than 3 cm in di-
ameter. In these 3 patients MRI/CT did not show brain matter as
the content of the sac.
Surgical Procedure and Outcome
All the patients were subjected to surgical repair. In 2 patients,
hemoglobin was low; hence they were discharged and admitted
later when hemoglobin was normalized. Amongst the 10 patients
with hydrocephalus, 7 were considered suitable for ventricular
diversion. Five patients had low-pressure ventriculoperitoneal
(VP) shunt insertion during surgery for the repair of the enceph-
aloceles. Two patients required VP shunt procedure within 2
weeks of surgical repair and before discharge from the hospital,
as their postoperative noncontrast CT revealed further enlarge- a
ment of the ventricle.
All the patients underwent repair of the encephalocele. In 3 pa-
tients, where there was no brain tissue, repair was simple closure
after excising the sac. In 1 patient, torcula and part of the transverse
sinuses were in the encephalocele sac, which was gently pushed
forward and repair was done. In the remaining 9 patients with oc-
cipital encephaloceles, the herniating brain was partially excised
and the rest was pushed gently into the cranial cavity (fig.5ac). In
the 5 cases of craniostenosis, wide craniectomy was carried out
around the coronal suture by a separate bicoronal skin incision
(fig.6a, b). This was to avoid raised intracranial pressure (ICP) in
the postoperative period. In 4 patients, cranioplasty was carried
out to cover occipital bone defect, either by removing the bone
around the coronal suture (2) or using methyl methacrylate (2).
Two patients who developed cardiac arrest during surgery were
successfully revived and surgery was completed. Both patients had
good postoperative recovery and were discharged within 7 days.
There were 2 postoperative deaths, both due to hypothermia
during surgery, despite the use of a warming blanket. The remain- b
ing 12 patients had an average 7-day postoperative stay in the hos-
pital. The duration of the stay ranged from 3 to 15 days. The 2
patients who required a postoperative VP shunt remained in hos-
pital for 10 and 13 days, respectively. One patient with a wound
infection required prolonged antibiotics and was discharged after
15 days. Follow-up ranged from 6 months to 6 years. The patient
with an anterior fontanel encephalocele required two shunt revi-
sions in the first 2 years. However, his mental development was
poor when last followed up at the age of 6 years. One patient with
occipital encephalocele who had VP shunt required shunt revi-
sion 4 years after surgery. Overall, mental development was satis-
factory in 9 and poor in 3 patients. Thus, 33% of patients had a
significantly poor mental development. A clinical profile of all
patients can be seen in table1.
Discussion
c
Encephaloceles are not uncommon; however, giant en-
cephalocele, where the encephalocele reaches a large vol-
Fig. 5. a Intraoperative photograph of a case of occipital encepha-
ume, is rare [1, 3, 4, 6]. These conditions can be termed
locele showing flap dissection. b Intraoperative photograph
massive encephalocele [6], large encephalocele [1, 7] and showing dissection of sac containing occipital giant encephalo-
giant encephalocele [25], which of course mean the same cele. c Intraoperative photograph of occipital giant encephalocele
thing with similar challenges [1, 2, 4, 7]. They pose a great after excision of sac.
36.69.228.119 - 8/6/2017 4:09:04 PM
408 Pediatr Neurosurg 2011;47:406411 Mahapatra
Downloaded by:
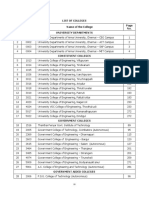
Table 1. Clinical profile of the patients
No. Name of Site of CT; MRI Associated finding Surgery Immediate result Long-term
patient, encepha- follow-up
age, year of locele
admission
1 B.Z., 2 days, anterior CT; MRI hydrocephalus VP shunt and repair discharged 7 days; 6-year follow-up: fits;
2004 fontanel good mental retardation; 2
shunt revisions
20042006
2 Ans, 5 occipital CT hydrocephalus; excision repair; discharged on 5th day; 2 years: mental
months, anterior craniostenosis craniectomy; good retardation
2005 fontanel cranioplasty by
closed autologous bone graft;
VP shunt
3 Aman, occipital CT; small no brain tissue inside excision; 2nd surgery; postoperative good outcome at 4
26 days, occipital the sac; VP shunt ventilated; shunt on years
2002 bone defect hydrocephalus 7th day; discharged on
postoperative day 14
4 Asha, 3 occipital CT; MRI no hydrocephalus; craniectomy; excision; discharged on 7th day; good outcome at 3
months, craniostenosis cranioplasty by methyl good years
2006 methacrylate
5 K.S., occipital MRI no hydrocephalus excision and repair expired due to patient expired 1st
10 days, hypothermia postoperative day
2003
6 S.S., occipital CT; MRI polygyria; microgyria excision and repair; postoperative stay 10 5-year follow-up:
9 months, craniostenosos; no craniectomy; days poor mental state
2003 hydrocephalus cranioplasty by
autologous bone
7 Neetin, occipital CT; small hydrocephalus; no VP shunt; excision and discharged on 5th day; good outcome at
2 months, occipital defect brain tissue in sac repair good 4-year follow-up
2004
8 S.M., 4 occipital CT no hydrocephalus; excision and repair; discharged on 5th 3-year follow-up:
months, craniostenosis craniectomy postoperative day; good condition
2005 good
9 S.G., 3 occipital CT; MRI hydrocephalus VP shunt; repair of discharged on 7th patient was well;
months, encephalocele postoperative day; shunt block 2006; VP
2002 good shunt revised; good
mental development
10 K.S., 1 occipital CT; MRI hydrocephalus VP shunt; excision and discharged on 3rd day good at 2-year
month, repair follow-up
2007
11 B.S., 1 year, occipital CT; MRI hydrocephalus excision and repair; discharged on 12th day 1-year follow-up:
2008 postoperative shunt 4th good
day
12 S.B., 4 years occipital CT; MRI no hydrocephalus repair of encephalocele discharged on 8th day good condition at 1
2008 year
13 S.F., 4 occipital CT; MRI microcephaly; excision and repair; discharged on 3rd day 6-month follow-up:
months, craniostenosis; small craniectomy good normal
2009 bone defect; no development so far
hydrocephalus
14 R.K., occipital CT; MRI microcephaly; no excision repair, patient ventilated; died on 1st expired 24 h
20 days, hydrocephalus had intraoperative postoperative day following surgery
2009 hypothermia
36.69.228.119 - 8/6/2017 4:09:04 PM
Giant Encephalocele: A Study of 14 Pediatr Neurosurg 2011;47:406411 409
Patients
Downloaded by:
Color version available online
Fig. 6. a Postoperative clinical photograph
showing occipital wound following exci-
sion and repair of giant occipital encepha-
locele. b Bicoronal skin closure after cra-
niectomy in a patient with giant occipital a b
encephalocele with craniostenosis.
challenge to the neurosurgeon, neuroradiologist and MRI is the most important modality of imaging; how-
neuroanesthetist during surgery. This series highlights ever, most of the patients were already investigated prior
the clinical features and management problems of these to coming to our center. In this study, both MRI and CT
patients. were performed on 8 patients, CT scan only was carried
The exact incidence of giant encephalocele is not out on 5 and MRI only was done on 1 patient. It is impor-
known. The literature only provides case reports [13, 7]. tant to understand that CT not only gives radiation risk
This is the only series of giant encephaloceles analyzed in to the neonate, but it has less value in delineating soft tis-
the world literature so far apart from one previous series sue anomalies like micro- and macrogyria and heteroto-
published by our institute in abstract form [5]. The cur- pia. CT has the only distinct advantage of showing bone
rent study includes 14 patients with giant encephaloceles, defects, which is the limitation in MRI and tentorial
amongst a series of 110 patients with encephaloceles, anomaly. The other reason why CT was performed before
treated during the period 20022009. The vast majority the patients came to us was that CT scans are less expen-
of patients (11/14) were under 6 months, and 4 were neo- sive, less time-consuming and easily accessible in small
nates. Only 2 patients were over 1 year of age. By and large towns, where an MRI facility may not be available.
these patients typically present as neonates and infants [3, Large numbers of brain anomalies are associated with
4, 6] as the external swelling produces nursing and feed- encephaloceles, especially with giant encephaloceles [3, 4,
ing problems. One of our patients was a 2-day-old baby 69]. In cases of occipital giant encephaloceles, the evalu-
admitted with a leaking anterior fontanel encephalocele ation of the transverse sinus and torcula are also impor-
[3]. Generally, the patients relatives seek advice at birth; tant. In one of our giant occipital encephalocele, the ve-
however, as the experience is limited, proper advice can- nous sinuses and torcula were inside the encephalocele
not be offered; hence many patients do not present either sac. This information helps the surgeon to plan the sur-
at birth or during the neonatal period. However, by the gery well and handle the structures during surgery with-
time the baby is between 3 and 6 months of age, they at- out damaging them. Chiari II malformation was present
tend our institute having taken advice from several doc- in 3 patients and 10 patients had associated hydrocepha-
tors and even neurosurgeons. The relatives seek dedicat- lus. In 3 patients MRI did not reveal any brain tissue in-
ed pediatric neurosurgical and neuroanesthetic care, side the encephalocele sac.
which is offered at our institute. Surgical repair is a great challenge in patients with low
2 patients had a history of CSF leak and 4 had micro- birth weight and with prolonged anesthesia [1, 2, 4, 7].
cephaly as the coronal sutures were fused. One patient Intubating the patient is difficult with giant occipital en-
also had a cleft lip, which was repaired before the patient cephaloceles. In 50% of these children partial aspiration
was referred to the neurosurgery unit. of CSF was carried out to reduce the volume, which fa-
cilitated the intubation process during anesthesia. Seven
36.69.228.119 - 8/6/2017 4:09:04 PM
410 Pediatr Neurosurg 2011;47:406411 Mahapatra
Downloaded by:
of our patients required VP shunt, 5 at the time of repair method helped the patients and none of them had post-
of encephalocele. In 2 patients postoperative shunt inser- operative or long-term problems.
tion was undertaken as the ventricle further dilated. Two Intraoperative blood loss, hypothermia, bradycardia
of our patients had transient cardiac arrest during anes- and cardiac arrest are well known [2, 4, 7]. Two of our
thesia. Both patients were successfully revived, surgery patients had cardiac arrest; however, both did well and
was completed and there were no postoperative compli- were discharged within 7 days. Two patients with severe
cations. hypothermia approaching 32 C did not recover and ex-
During the repair of encephalocele it is important to pired within 24 h. One of our patients had a wound infec-
make a judgement to excise the brain partially or to try tion and remained in hospital for 2 weeks postoperative-
to return all the contents into the intracranial cavity. ly. At long-term follow-up, 66% of the patients had good
Sometimes the head is small and the volume of the herni- mental function.
ated brain is large so that it is not possible to close the sac
without excising the brain tissue. In 7 (50%) patients a
significant amount of herniated brain (5070%) was ex- Conclusions
cised to achieve a lax brain, at the time of closure. Some
authors have described closure without excising the brain Giant encephaloceles are rare and pose a unique chal-
by providing expansible cranioplasty [1]. In the present lenge. The present study is the largest series in the English
study, craniectomy performed around the coronal suture literature. With dedicated effort good results are likely in
and an anterior fontanel was created in 5 patients to avoid 6570% of cases. We recommend early surgery to avoid
postoperative raised ICP, even though VP shunt was car- rupture or skin excoriation. MRI is the investigation of
ried out. The management of postoperative raised ICP in choice, which can delineate all intracranial anomalies.
a newborn is unpredictable and the baby can develop sud- Large encephaloceles can be aspirated under anesthesia
den respiratory arrest. In 4 patients cranioplasty was car- to facilitate intubation and the positioning of the patient
ried out at the site of the occipital bone defect. In 2 of these in the operating room. A liberal craniectomy is ideal in
cases an autologous bone graft was taken from the region patients with secondary craniostenosis to avoid postop-
of the anterior fontanel, and in the remaining 2 a methyl eratively raised ICP. Judicious management of intraop-
methacrylate mould was made to cover the bone defect, erative blood loss and hypothermia are the keys to suc-
to protect the brain and to prevent reherniation. This cess.
References
1 Bozinov O, Tirakotai W, Sure V, Bertalanffy 4 Mahapatra AK, Gupta PK, Dev EJ: Posterior 8 Morika T, Hashiguchi K, Samura K, Yoshida
H: Surgical closure and reconstruction of a fontanelle giant encephalocele. Pediatr Neu- J, et al: Detailed anatomy and intracranial
large occipital encephalocele without paren- rosurg 2002; 36:4043. venous anomalies associated with atretic pa-
chymal excision. Childs Nerv Syst 2005; 21: 5 Mahapatra AK: Giant encephalocele. A se- rietal encephalocele revealed by high-resolu-
144147. ries of 21 cases (abstract). Childs Nerv Syst tion 3D-CISS and high-field T2-weighted re-
2 Satyarthee GD, Mahapatra AK: Craniofacial 2007;27:1082. versed MR image. Childs Nerv Syst 2009;25:
surgery for giant frontonasal encephalocele 6 Mohanty A, Biswas A, Reddy M, Shastry KS: 309315.
in neonate. J Clin Neurosci 2002;9:593595. Expansile cranioplasty for massive occipital 9 Reddy AT, Hedlund GL, Percy AK: Enlarged
3 Todo T, Usui M, Araki F: Dandy-Walker syn- encephalocele. Childs Nerv Syst 2006; 22: parietal foramina: association with cerebral
drome forming a giant occipital meningo- 11701176. venous and cortical anomalies. Neurology
cele case report. Neurol Med Chir (Tokyo) 7 Bharti N, Dash HH, Mahapatra AK: Recur- 2000;54:11751178.
1993;33:845850. rent brady-cardia and delayed recovery in a
neonate following repair of nasofrontal en-
cephalocele with hosopresencephaly and
single cerebral ventricle. J Neurosurg Anes-
thesiol 2003;15:140143.
36.69.228.119 - 8/6/2017 4:09:04 PM
Giant Encephalocele: A Study of 14 Pediatr Neurosurg 2011;47:406411 411
Patients
Downloaded by:
You might also like
- Association With Grade and Outcome: Apoptotic Activity and bcl-2 Immunoreactivity in MeningiomasDocument9 pagesAssociation With Grade and Outcome: Apoptotic Activity and bcl-2 Immunoreactivity in MeningiomasSayyid Hakam PerkasaNo ratings yet
- Aminmansour - Cerebral Vasospasm Following Traumatic Subarachnoid HemorrhageDocument8 pagesAminmansour - Cerebral Vasospasm Following Traumatic Subarachnoid HemorrhageSayyid Hakam PerkasaNo ratings yet
- Pediatric Encephaloceles A Series of 20 CasesDocument4 pagesPediatric Encephaloceles A Series of 20 CasesSayyid Hakam PerkasaNo ratings yet
- Pattern of Encephaloceles A Case SeriesDocument4 pagesPattern of Encephaloceles A Case SeriesSayyid Hakam PerkasaNo ratings yet
- A Giant Occipital Encephalocele With Spontaneous Hemorrhage Into The Sac - A Rare Case ReportDocument3 pagesA Giant Occipital Encephalocele With Spontaneous Hemorrhage Into The Sac - A Rare Case ReportSayyid Hakam PerkasaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Https Emedicine - Medscape.com Article 1831191-PrintDocument59 pagesHttps Emedicine - Medscape.com Article 1831191-PrintNoviatiPrayangsariNo ratings yet
- IIT JEE Physics Preparation BooksDocument3 pagesIIT JEE Physics Preparation Booksgaurav2011999No ratings yet
- Feng Shui GeneralDocument36 pagesFeng Shui GeneralPia SalvadorNo ratings yet
- 1 Piling LaranganDocument3 pages1 Piling LaranganHannie Jane Salazar HerreraNo ratings yet
- Pigeon Racing PigeonDocument7 pagesPigeon Racing Pigeonsundarhicet83No ratings yet
- 19-Microendoscopic Lumbar DiscectomyDocument8 pages19-Microendoscopic Lumbar DiscectomyNewton IssacNo ratings yet
- Fort - Fts - The Teacher and ¿Mommy Zarry AdaptaciónDocument90 pagesFort - Fts - The Teacher and ¿Mommy Zarry AdaptaciónEvelin PalenciaNo ratings yet
- 059 Night of The Werewolf PDFDocument172 pages059 Night of The Werewolf PDFomar omar100% (1)
- Food Combining PDFDocument16 pagesFood Combining PDFJudas FK TadeoNo ratings yet
- PS4 ListDocument67 pagesPS4 ListAnonymous yNw1VyHNo ratings yet
- Specification - Pump StationDocument59 pagesSpecification - Pump StationchialunNo ratings yet
- Academic Decathlon FlyerDocument3 pagesAcademic Decathlon FlyerNjeri GachNo ratings yet
- GooseberriesDocument10 pagesGooseberriesmoobin.jolfaNo ratings yet
- Introduction To Astronomical PhotometryDocument452 pagesIntroduction To Astronomical PhotometrySergio Alejandro Fuentealba ZuñigaNo ratings yet
- ANI Network - Quick Bill Pay PDFDocument2 pagesANI Network - Quick Bill Pay PDFSandeep DwivediNo ratings yet
- TNEA Participating College - Cut Out 2017Document18 pagesTNEA Participating College - Cut Out 2017Ajith KumarNo ratings yet
- Lesson 17 Be MoneySmart Module 1 Student WorkbookDocument14 pagesLesson 17 Be MoneySmart Module 1 Student WorkbookAry “Icky”100% (1)
- Item AnalysisDocument7 pagesItem AnalysisJeff LestinoNo ratings yet
- 5f Time of Legends Joan of Arc RulebookDocument36 pages5f Time of Legends Joan of Arc Rulebookpierre borget100% (1)
- Img - Oriental Magic by Idries Shah ImageDocument119 pagesImg - Oriental Magic by Idries Shah ImageCarolos Strangeness Eaves100% (2)
- Mohak Meaning in Urdu - Google SearchDocument1 pageMohak Meaning in Urdu - Google SearchShaheryar AsgharNo ratings yet
- Ikramul (Electrical)Document3 pagesIkramul (Electrical)Ikramu HaqueNo ratings yet
- TIMELINE - Philippines of Rizal's TimesDocument46 pagesTIMELINE - Philippines of Rizal's TimesAntonio Delgado100% (1)
- CALIDocument58 pagesCALIleticia figueroaNo ratings yet
- Pharmaniaga Paracetamol Tablet: What Is in This LeafletDocument2 pagesPharmaniaga Paracetamol Tablet: What Is in This LeafletWei HangNo ratings yet
- Responsive Docs - CREW Versus Department of Justice (DOJ) : Regarding Investigation Records of Magliocchetti: 11/12/13 - Part 3Document172 pagesResponsive Docs - CREW Versus Department of Justice (DOJ) : Regarding Investigation Records of Magliocchetti: 11/12/13 - Part 3CREWNo ratings yet
- Placement TestDocument6 pagesPlacement TestNovia YunitazamiNo ratings yet
- Chapter 6 Bone Tissue 2304Document37 pagesChapter 6 Bone Tissue 2304Sav Oli100% (1)
- Marriot CaseDocument15 pagesMarriot CaseArsh00100% (7)
- Simplified Electronic Design of The Function : ARMTH Start & Stop SystemDocument6 pagesSimplified Electronic Design of The Function : ARMTH Start & Stop SystembadrNo ratings yet