Professional Documents
Culture Documents
La Terapia Cambia Al Cerebro
Uploaded by
arkangelazulCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
La Terapia Cambia Al Cerebro
Uploaded by
arkangelazulCopyright:
Available Formats
Can you please elaborate on the statement you made at the 2011 U.S.
Psychiatric and
Mental Health Congress
that psychotherapy can literally change the brain?
Jon W. Draud, MD, MS: This is a great question and points out the flaw
in the old dichotomy that psychotherapy is for psychological disorders
whereas medication is reserved for biological disorders. Of course this is
incorrect and there has been much research on plastic brain changes. The
advent of functional magnetic resonance imaging, single-photon emission
computed tomography, and positron emission tomography has truly advanced this area
of study over the last decade.
Nearly 20 studies have been published on brain changes after psychotherapy for
depression, anxiety disorders, and borderline personality disorders. Examining the
various studies, the overall conclusion is that cognitive therapy, behavior therapy,
psychodynamic psychotherapy, and interpersonal therapy alter brain functions in
patients suffering with major depressive disorder (MDD), obsessive-compulsive
disorder (OCD), panic disorder, social anxiety disorder, borderline personality disorder
(BPD), specific phobias, and post-traumatic stress disorder.1-14
Most studies show similar changes after medication and psychotherapy, but some recent
studies show differences. Goldapple et al.3 found increased metabolism at dorsal
cingulate and hippocampus and decreased flow to medial frontal cortex as well as dorsal
and ventral frontal areas in cognitive-behavioral therapy (CBT) applied to patients with
MDD. This is different from medication metabolic changes, which typically show
increases in prefrontal cortex and decreases at hippocampus and subgenual anterior
circulate. There have also been some differences in patterns of metabolism with short-
term psychodynamic therapy and fluoxetine among patients with MDD.15
Many psychotherapies are aimed at enhancing patients abilities to problem solve,
regulate affect, and change their negative views of themselves. Brain areas that are
involved tend to be the dorsolateral, ventrolateral, and medial prefrontal cortices, the
anterior cingulate, the posterior cingulate/precuneus, and the insular cortices.16 Beutel et
al.8 demonstrated a frontal deactivation and amygdala hyper-activation in symptomatic
patients with panic disorder. The prevailing theory of how CBT works is via top
down regulation of hyper-excitable links with formations by prefrontal cortical areas.
Similarly, Schnell and Herpertz13 showed that after dialectical behavior therapy there is
decreased activity in areas that were previously hyperaroused in patients with BPD.
These findings are, of course, interesting and lead us to the notion that all good
clinicians are already aware of: a good therapeutic alliance that combines psychotherapy
and incorporates medications is almost always superior to either modality used alone.
Jon W. Draud, MD, MS
You might also like
- How Psychotherapy Changes the BrainDocument5 pagesHow Psychotherapy Changes the BrainTomas SærmarkNo ratings yet
- Neuropsych of BPD 2001 Murphy SahakianDocument9 pagesNeuropsych of BPD 2001 Murphy SahakianMa Azalea V LaquiNo ratings yet
- Neuropsychology of Bipolar Disorder: References ReprintsDocument9 pagesNeuropsychology of Bipolar Disorder: References ReprintsDedeSumantraNo ratings yet
- From Pro-Inflammatory Molecules To The Brain's Resting-State Connectivity The Future of Clinical Diagnosis of DepressionDocument36 pagesFrom Pro-Inflammatory Molecules To The Brain's Resting-State Connectivity The Future of Clinical Diagnosis of DepressiondgavrileNo ratings yet
- Matter and Its Changes JournalDocument17 pagesMatter and Its Changes JournalMuahmmad Aidil PahleviNo ratings yet
- Neuropsychology of Bipolar DisorderDocument9 pagesNeuropsychology of Bipolar DisorderwulanfarichahNo ratings yet
- Editorial: The Significance of Psychotherapy in The Age of NeuroscienceDocument2 pagesEditorial: The Significance of Psychotherapy in The Age of NeurosciencevinodksahuNo ratings yet
- Drugs and Talk Therapy Impact the Brain DifferentlyDocument2 pagesDrugs and Talk Therapy Impact the Brain DifferentlybgvtNo ratings yet
- Psilocybin Assisted Therapy A Review of A Novel Treatment For Psychiatric DisordersDocument11 pagesPsilocybin Assisted Therapy A Review of A Novel Treatment For Psychiatric DisordersJuanmaNo ratings yet
- The Biological Approach - KJDocument6 pagesThe Biological Approach - KJEshaNo ratings yet
- Bipolar Disorder Pathophysiology and GeneticsDocument11 pagesBipolar Disorder Pathophysiology and GeneticsGirlly AlcantaraNo ratings yet
- A Case Study of A Mental DisorderDocument7 pagesA Case Study of A Mental DisorderMaurine TuitoekNo ratings yet
- Neuroimaging in Bipolar DisorderDocument13 pagesNeuroimaging in Bipolar DisorderAngie GiraldoNo ratings yet
- CASE HISTORY PROCEDURE (1) - RemovedDocument8 pagesCASE HISTORY PROCEDURE (1) - RemovedayaanNo ratings yet
- Voon, Kubu Et Al 2006Document23 pagesVoon, Kubu Et Al 2006Jennifer CaussadeNo ratings yet
- Versão Final Depressão ExecutivasDocument15 pagesVersão Final Depressão ExecutivasGeorgiana PrisoschiNo ratings yet
- The Hippocampus in Major Depression Evidence For TDocument14 pagesThe Hippocampus in Major Depression Evidence For TFrancisco MtzNo ratings yet
- Mood-Stabilizing Drugs: Mechanisms of Action: Robert J. Schloesser, Keri Martinowich and Husseini K. ManjiDocument11 pagesMood-Stabilizing Drugs: Mechanisms of Action: Robert J. Schloesser, Keri Martinowich and Husseini K. ManjiIwan MiswarNo ratings yet
- The Complexity of the Human Brain and Mental Illness DiagnosisDocument5 pagesThe Complexity of the Human Brain and Mental Illness DiagnosisNur Ayu SartikaNo ratings yet
- The Latest Neuroimaging Findings in Borderline 2014Document13 pagesThe Latest Neuroimaging Findings in Borderline 2014me13No ratings yet
- Psychostimulants & Non-ADHD UsesDocument12 pagesPsychostimulants & Non-ADHD UsesBrent Sheardown100% (1)
- Research Paper Topics NeurologyDocument5 pagesResearch Paper Topics Neurologyafeawjjwp100% (1)
- Advances in Understanding and Treating Mood DisordersDocument4 pagesAdvances in Understanding and Treating Mood DisordersAnahí Cortés HerreraNo ratings yet
- Brady 2015Document15 pagesBrady 2015alfredoibcNo ratings yet
- Neuroimage: Clinical: SciencedirectDocument9 pagesNeuroimage: Clinical: SciencedirectMostafa FakhriNo ratings yet
- 007Document3 pages007Ed RibeiroNo ratings yet
- Predictors of Poor Treatment Response ToDocument13 pagesPredictors of Poor Treatment Response ToMaite Novo del valleNo ratings yet
- Antipsychotics and The BrainDocument5 pagesAntipsychotics and The BrainsyamimisdNo ratings yet
- Iseger and Bossong 2015 Schizophrenia ResearchDocument10 pagesIseger and Bossong 2015 Schizophrenia ResearchIgnacia PaezNo ratings yet
- Experience Effects On Brain Development Possible Contributions To PsychopathologyDocument31 pagesExperience Effects On Brain Development Possible Contributions To PsychopathologyShirleuy GonçalvesNo ratings yet
- Dopamine System Dysregulation in Major Depressive DisordersDocument11 pagesDopamine System Dysregulation in Major Depressive Disordersemaildaisadora2No ratings yet
- Godlewska 2019 Cognitive Neuropsychological Theory of Antidepressant Action: A Modern-Day Approach To Depression and Its TreatmentDocument14 pagesGodlewska 2019 Cognitive Neuropsychological Theory of Antidepressant Action: A Modern-Day Approach To Depression and Its TreatmentJahlin HabbeiNo ratings yet
- Neuromodulation For Addiction 082209Document9 pagesNeuromodulation For Addiction 082209hellno1234100% (1)
- Psych 2Document17 pagesPsych 2austinviernes99No ratings yet
- Neural Correlates of Conversion Disorder. Boeckle y Cols. 2016Document15 pagesNeural Correlates of Conversion Disorder. Boeckle y Cols. 2016José ManuelNo ratings yet
- Linking Molecules To Mood: New Insight Into The Biology of DepressionDocument16 pagesLinking Molecules To Mood: New Insight Into The Biology of Depressiondudul pudlianNo ratings yet
- Franz X. Vollenweider and Mark A. Geyer - A Systems Model of Altered Consciousness: Integrating Natural and Drug-Induced PsychosesDocument13 pagesFranz X. Vollenweider and Mark A. Geyer - A Systems Model of Altered Consciousness: Integrating Natural and Drug-Induced PsychosesCortate15gNo ratings yet
- Appi Ajp 2020 20101481Document10 pagesAppi Ajp 2020 20101481sarahNo ratings yet
- Perspectives: The Neurobiology of Psychedelic Drugs: Implications For The Treatment of Mood DisordersDocument10 pagesPerspectives: The Neurobiology of Psychedelic Drugs: Implications For The Treatment of Mood DisordersFilipe Nunes VicenteNo ratings yet
- Neuropsicología de T ÁnimoDocument6 pagesNeuropsicología de T ÁnimoZaira MediNo ratings yet
- 2018 - ARTIGO - Recognizing Depression From The Microbita Gut Axis - 8 Paginas (Tudo)Document16 pages2018 - ARTIGO - Recognizing Depression From The Microbita Gut Axis - 8 Paginas (Tudo)Liliana de SousaNo ratings yet
- Treatment of Bipolar DisorderDocument20 pagesTreatment of Bipolar DisorderShana Wl100% (1)
- Research PaperDocument8 pagesResearch Paperapi-698797022No ratings yet
- Cognition as a Target in Depression: New DevelopmentsDocument17 pagesCognition as a Target in Depression: New DevelopmentsastrogliaNo ratings yet
- TP 2012116Document13 pagesTP 2012116tatataNo ratings yet
- Psilocybin's Potential for Treating OCDDocument11 pagesPsilocybin's Potential for Treating OCDSamuel BallouNo ratings yet
- AnnotatedBibliography - Mcleodrevised 2 1Document20 pagesAnnotatedBibliography - Mcleodrevised 2 1mmasi dennisNo ratings yet
- Functional Neuroanatomy of Bipolar Disorder: Structure, Function, and Connectivity in An Amygdala-Anterior Paralimbic Neural SystemDocument16 pagesFunctional Neuroanatomy of Bipolar Disorder: Structure, Function, and Connectivity in An Amygdala-Anterior Paralimbic Neural SystemLin FernándezNo ratings yet
- JAMA Psychiatry - : Original InvestigationDocument10 pagesJAMA Psychiatry - : Original InvestigationMesianissimoNo ratings yet
- Running Head: The Neurobiology of Boderline Personality DisorderDocument16 pagesRunning Head: The Neurobiology of Boderline Personality Disorderapi-282692758No ratings yet
- Bipolar Pubmed IngDocument10 pagesBipolar Pubmed IngAsdhoNo ratings yet
- Mental Illness Is Like Any Other Medical IllnessDocument9 pagesMental Illness Is Like Any Other Medical IllnessSunny ValeNo ratings yet
- The Neurobiology of Depression: British Medical Bulletin March 2012Document20 pagesThe Neurobiology of Depression: British Medical Bulletin March 2012Aml AmlNo ratings yet
- Tmp439a TMPDocument17 pagesTmp439a TMPFrontiersNo ratings yet
- Neurobiology of Psychedelis 2Document10 pagesNeurobiology of Psychedelis 2Andrea Corina RomoNo ratings yet
- Psych 3Document17 pagesPsych 3austinviernes99No ratings yet
- Del Bello 2004Document10 pagesDel Bello 2004Lin FernándezNo ratings yet
- 1.psychiatric Neuroscience - Incorporating Pathophysiology Into Clinical Case Formulation - ClinicalKeyDocument43 pages1.psychiatric Neuroscience - Incorporating Pathophysiology Into Clinical Case Formulation - ClinicalKeyClaudia0% (1)
- Revisiting The Stress Concept: Implications For Affective DisordersDocument10 pagesRevisiting The Stress Concept: Implications For Affective DisordersJefferson MorenoNo ratings yet
- Aggressive SuicideDocument16 pagesAggressive SuicidearkangelazulNo ratings yet
- Genetic ADocument7 pagesGenetic AarkangelazulNo ratings yet
- La Terapia Cambia Al CerebroDocument1 pageLa Terapia Cambia Al CerebroarkangelazulNo ratings yet
- 8 Things To Remember About Child DevelopmentDocument4 pages8 Things To Remember About Child DevelopmentPaulina Guerra Santa MaríaNo ratings yet
- Most Rapists Are Not SadistsDocument2 pagesMost Rapists Are Not SadistsarkangelazulNo ratings yet
- Smart Pill PDFDocument1 pageSmart Pill PDFarkangelazulNo ratings yet
- Psicosis Primaria Vs Por DrogasDocument11 pagesPsicosis Primaria Vs Por DrogasarkangelazulNo ratings yet
- Genetic ADocument7 pagesGenetic AarkangelazulNo ratings yet
- Smart PillDocument1 pageSmart PillarkangelazulNo ratings yet
- Genetic ADocument7 pagesGenetic AarkangelazulNo ratings yet
- Frontal Executive Functions in Hypnosis and Hypnotic SuggestibilityDocument44 pagesFrontal Executive Functions in Hypnosis and Hypnotic SuggestibilityAlber SánchezNo ratings yet
- Personality and Individual Differences: Mark W.G. Bosmans, Leontien M. Van Der Knaap, Peter G. Van Der VeldenDocument5 pagesPersonality and Individual Differences: Mark W.G. Bosmans, Leontien M. Van Der Knaap, Peter G. Van Der VeldenAndrei BăcanuNo ratings yet
- Wellness Recovery Action Plan WRAPDocument26 pagesWellness Recovery Action Plan WRAPMido Khair100% (1)
- CatharsisDocument6 pagesCatharsisGladys SorianoNo ratings yet
- Psychosocial Occupational Therapy Interventions For Substance Use Disorders A Narrative ReviewDocument19 pagesPsychosocial Occupational Therapy Interventions For Substance Use Disorders A Narrative ReviewJane DNo ratings yet
- Global Assessment of Relational Functioning GarfDocument2 pagesGlobal Assessment of Relational Functioning GarfelamyNo ratings yet
- Attention Deficit/ Hyperactivity Disorder: Changes To The DisorderDocument2 pagesAttention Deficit/ Hyperactivity Disorder: Changes To The DisorderGemanDuenasNo ratings yet
- Sample Article Child and Adolescent Psychiatry and Mental HealthDocument12 pagesSample Article Child and Adolescent Psychiatry and Mental Healthwishfairy67No ratings yet
- Trauma and the Self: A Theoretical and Clinical PerspectiveDocument20 pagesTrauma and the Self: A Theoretical and Clinical PerspectiveLorenaUlloaNo ratings yet
- Understanding The Vocational Impact of Mental Health Disorders.Document65 pagesUnderstanding The Vocational Impact of Mental Health Disorders.John F. LeporeNo ratings yet
- Trauma Assessment: John Briere, PH.DDocument10 pagesTrauma Assessment: John Briere, PH.DZawawi Ibnu RosyidNo ratings yet
- Mental HygieneDocument18 pagesMental Hygienechester chesterNo ratings yet
- Crisis CounsellingDocument28 pagesCrisis CounsellingPooja varmaNo ratings yet
- A Spiders Web OutlineDocument6 pagesA Spiders Web Outlineapi-235484994No ratings yet
- Antshel2017 PDFDocument22 pagesAntshel2017 PDFCristinaNo ratings yet
- Facilitating Learning: Nature of InvolvementDocument6 pagesFacilitating Learning: Nature of InvolvementMay Eden M. MabasaNo ratings yet
- NCP For Parent and Child PDFDocument3 pagesNCP For Parent and Child PDFMariana Mikaela AlagarNo ratings yet
- Sigmund Freud Screen MemoriesDocument10 pagesSigmund Freud Screen MemoriesOlivia Spalletta0% (1)
- The Psychology of Pain: George R. Hansen, MD, Jon Streltzer, MDDocument10 pagesThe Psychology of Pain: George R. Hansen, MD, Jon Streltzer, MDRobi Maulana100% (1)
- Level of depression among elderly in old age homesDocument1 pageLevel of depression among elderly in old age homesDeepak Krishnamurthy KNo ratings yet
- Smith Metro Symp 15 ApraxiaDocument30 pagesSmith Metro Symp 15 ApraxiachamilaNo ratings yet
- Psychological TherapiesDocument146 pagesPsychological TherapiesMirela Cojocaru StetcoNo ratings yet
- Addendum PSWDocument6 pagesAddendum PSWMegha JainNo ratings yet
- Research in Developmental Disabilities: SciencedirectDocument8 pagesResearch in Developmental Disabilities: SciencedirectLaura Kata LopezNo ratings yet
- Persnality TestDocument4 pagesPersnality TestZeeshan KhanNo ratings yet
- Change MGT Pregentation (Group 1) FinalDocument40 pagesChange MGT Pregentation (Group 1) FinalAbdullah NomanNo ratings yet
- Depression PowerpointDocument32 pagesDepression PowerpointjoycechicagoNo ratings yet
- Schizophrenia NOTESDocument8 pagesSchizophrenia NOTESCamille GraceNo ratings yet
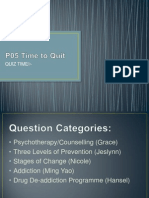
- QuizDocument15 pagesQuizGracie ChongNo ratings yet