Professional Documents
Culture Documents
Arsrgj
Uploaded by
Debasis SahooOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Arsrgj
Uploaded by
Debasis SahooCopyright:
Available Formats
[Downloaded free from http://www.joacp.org on Saturday, August 12, 2017, IP: 47.11.234.
46]
Original Article
Efficacy of the subcostal transversus abdominis plane block in
laparoscopic cholecystectomy: Comparison with conventional
port-site infiltration
S Tolchard, R Davies, S Martindale
North Bristol NHS Trust, Bristol, UK
Abstract
Background: Pain experienced following laparoscopic cholecystectomy is largely contributed by the anterior abdominal wall
incisions. This study investigated whether subcostal transversus abdominis (STA) block was superior to traditional port-site
infiltration of local anesthetic in reducing postoperative pain, opioid consumption, and time for recovery.
Materials and Methods: Forty-three patients presenting for day case laparoscopic cholecystectomy were randomly allocated
to receive either an ultrasound-guided STA block (n = 21) or port-site infiltration of local anesthetic (n = 22). Visual analog pain
scores were measured at 1 and 4 h postoperatively to assess pain severity, and opioid requirement was measured in recovery
and up to 8 h postoperatively. The time to discharge from recovery was recorded.
Results: STA block resulted in a significant reduction in serial visual pain analog score values and significantly reduced the
fentanyl requirement in recovery by >35% compared to the group that received local port-site infiltration (median 0.9 vs. 1.5
cg/kg). Furthermore, STA block was associated with nearly a 50% reduction in overall 8-h equivalent morphine consumption
(median 10 mg vs. 19 mg). In addition, STA block significantly reduced median time to discharge from recovery from 110 to
65 min.
Conclusion: The results suggest that STA block provides superior postoperative analgesia and reduces opioid requirement
following laparoscopic cholecystectomy. It may also improve theater efficiency by reducing time to discharge from the recovery
unit.
Key words: Subcostal block, laparoscopic cholecystectomy, analgesia, regional anaesthesia
Introduction local anesthetic[4-6] have been used successfully to reduce opioid
use and improve postoperative analgesia, the operation is usually
Laparoscopic cholecystectomy is a common minimally invasive performed under general anesthesia with port-site infiltration of
procedure which is increasingly performed in the day case local anesthetic and supplementary opioid analgesia.
unit.[1] Pain experienced following laparoscopic cholecystectomy
derives significantly from the incisions made in the anterior Recently, the uses of peripheral axial blocks that deliver
abdominal wall[2] which has segmental innervation provided by local anesthetic into the transversus abdominis fascial plane
nociceptor afferents in the transversus abdominis fascial plane[3] have become popular for operations that involve incision(s)
between the internal oblique and transversus abdominis muscles. of the abdominal wall. Thus, the transversus abdominis
Although neuroaxial blockade and intraperitoneal lavage of plane (TAP) block has been shown to reduce perioperative
opioid use in elective abdominal surgery,[7] including open
Address for correspondence: Dr. S Tolchard, Southmead Hospital,
appendicectomy,[8] laparotomy,[9] cesarean section,[10] and
North Bristol NHS Trust, Southmaed Road, Bristol, BS10 5NB.
E-mail: tolchard@doctors.org.uk laparoscopic cholecystectomy.[6] However, the efficacy of the
TAP block is reportedly only reliable in providing analgesia
Access this article online
below the umbilicus.[11,12] In the one study[6] in which it
Quick Response Code:
Website: was used for postoperative analgesia following laparoscopic
*** cholecystectomy, the port sites were moved to facilitate the
regional distribution of the block.
DOI:
10.4103/0970-9185.98331 The ultrasound-guided subcostal transversus abdominis
(STA) block is a recently described variation on the TAP
Journal of Anaesthesiology Clinical Pharmacology | July-September 2012 | Vol 28 | Issue 3 339
[Downloaded free from http://www.joacp.org on Saturday, August 12, 2017, IP: 47.11.234.46]
Tolchard, et al.: Sub-costal plane block and laparoscopic cholecystectomy
block which produces reliable unilateral supraumbilical Postoperatively, patients were transferred to the recovery unit.
analgesia.[12] The present study was designed to evaluate the Recovery nurses, who were blinded to the group intervention,
analgesic efficacy of STA block in reducing postoperative were however told that the patients had received local anesthetic
pain, opioid consumption, and recovery time following elective for patient safety purposes. In the recovery unit, patients
laparoscopic cholecystectomy. received intravenous fentanyl analgesia in 20 mcg boluses.
Administration of a bolus of fentanyl was triggered by pain
Materials and Methods described as moderate or severe when asked about their pain
intensity on a scale of mild, moderate, or severe. The criteria
The study was sponsored by the hospital trust and approved for discharge from the recovery unit were pain control (absent
by the local research ethics committee. Written informed or mild pain), absence of nausea and vomiting, hemodynamic
consent was gained from 43 ASA I/II adult (>16 yearsold) stability, and alert or appropriately responsive to voice. On
patients listed for elective laparoscopic cholecystectomy; discharge, all patients had achieved a modified Aldrete score
patient characteristics and details of anesthesia and surgery are of 9.[13] Following discharge from the recovery unit, the
summarized in Table 1. Emergency patients were excluded as patients were transferred to the day case ward where their
were those with allergy to local anesthetic agents, skin conditions analgesic requirements were satisfied on request with oral
precluding the block, or preoperative chronic dependence upon weak opioids and non-opioid analgesia. In the ward, analgesia
opioid medication. Based upon these exclusion criteria, only requirement was checked at 20-min intervals and moderate
one patient was not eligible for the study. to severe pain was treated.
Patients were blinded to the treatment group, as was the Outcome data were collected by a third anesthetist who was
anesthetist involved in postoperative data collection. A blind to the treatment group of individual patients. The
standardized general anesthetic regime was employed, quality of analgesia was determined by comparing visual
consisting of propofol (2.5 mg/kg), fentanyl (3 mcg/kg), pain analog scores (VPAS) preoperatively and at 1 and
and atracurium (0.6 mg/kg), with intraoperative non-opioid 4h postoperatively. Opioid requirement was examined in a
analgesia of paracetamol (1520 mg/kg) and diclofenac number of ways: the dose of fentanyl (mcg/kg) required in the
(0.5 mg/kg) [Table 1]. A sealed envelope randomization recovery unit, individual postoperative analgesic requirement
system was employed to allocate patients to receive either on the day case ward, and the overall 8-h equivalent morphine
an STA block (n = 21) or local anesthetic infiltration of dose which was calculated as the morphine dose equivalent
the laparoscopy port sites (n = 22) using a standardized
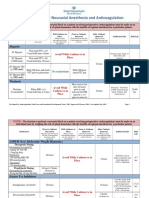
dose of 1 mg/kg bupivacaine hydrochloride (Marcain, Astra Table 1: Patient characteristics, standardized doses
Zeneca UK) using sterile technique. Three subcostal and (mean SEM) of anesthesia and analgesia, and dose and
volume (mean SEM) of local anesthesia in the port-site
one periumbilical port sites were employed in all cases. The
infiltration (n = 22) and STA block (n = 21) groups
volume and dose of local anesthetic did not differ between
Port-site Subcostal Mann
the groups [Table1]. The STA block was performed by infiltration block Whitney U
one of two anesthetists with expertise in ultrasound-guided P value
axial blocks, whereas port-site infiltration was performed by Demographic
the surgeon. The block was performed under ultrasound Age (years) 48 3 52 3 0.78
Gender (M:F) 2:0 5:16 0.24[1]
guidance (Sonosite iLook, Sonosite Inc., Bothwell, UT,
BMI 28 2 30 2 0.3
USA). The probe was placed in the midline of the abdomen
Weight (kg) 76 4 82 5 0.18
2 cm below the xiphisternum and moved right laterally Standard anesthesia/
along the subcostal margin to the anterior axillary line. The analgesia
transversus abdominis muscle was identified lying beneath Propofol (mg/kg) 2.4 0.2 2.2 0.2 0.56
and extending lateral to the rectus abdominis muscle. A Fentanyl (g/kg) 3.1 0.2 3.0 0.2 0.85
100-mm, 22-G Stimuplex block needle was then guided, Atracurium (mg/kg) 0.7 0.04 0.65 0.18
0.04
in plane, to a point just inferior to the right costal margin
Paracetamol (mg/kg) 21 2 16 1.5 0.61
at the anterior axillary line such that the tip lay between the Diclofenac (mg/kg) 0.65 0.1 0.58 0.1 0.5
transversus abdominis and internal oblique muscle within Procedural times (min)
the neurovascular fascial plane. Following aspiration, 1 mg/ Induction of anesthesia 12 1 16 2 0.38
kg bupivacaine was deposited within the plane. Port-site Operation time 76 5 68 5 0.72
infiltration was performed postoperatively in the usual manner Local anesthetic
using the same quantities and the dose of local anesthetic was Dose (mg/kg) 1.2 0.1 1.1 0.1 0.34
divided equally between port sites [Table 1]. Volume (ml) 21 1 22 1 0.85
340 Journal of Anaesthesiology Clinical Pharmacology | July-September 2012 | Vol 28 | Issue 3
[Downloaded free from http://www.joacp.org on Saturday, August 12, 2017, IP: 47.11.234.46]
Tolchard, et al.: Sub-costal plane block and laparoscopic cholecystectomy
to the opioid analgesia consumed (using opioid:morphine (median 0.9 vs. 1.5 mcg/kg, P < 0.05, MannWhitney
equivalents of 100 mcg i.v. fentanyl to 7 mg i.v. morphine; U-test) [Figure 2a]. Following discharge from the recovery
60 mg oral codeine to 6 mg i.v. morphine; 100 mg oral unit to the day case ward, there were no differences between
tramadol to 10 mg i.v. morphine).[14] These outcome measures the groups in the requirements for morphine, tramadol, or
were chosen to reflect common practice of employing opioid non-opioid analgesic medication. Two patients (one from each
analgesia of varying strengths as dictated by the WHO group) could not be satisfied by oral analgesics and they received
analgesia laddera. In order to improve the accuracy of data intramuscular morphine for breakthrough pain. However,
concerning recovery time, the time recorded was the difference overall, the 8-h equivalent morphine dose in the patients who
between admission time and the time the criteria for discharge received an STA block was significantly less than in those who
were achieved (see methods). received port-site infiltration of local anaesthetic (median 9.2 mg
vs. 16.8 mg, P < 0.01, MannWhitney U-test) [Figure 2b].
Statistical analysis was performed using SPSS software. The Significantly fewer patients in the STA group received codeine
ShapiroWilk test was employed to determine whether data phosphate postoperatively (P< 0.01, Chi-squared test) and
sets differed from a normal distribution. Normally distributed the amount of codeine required in this group was significantly
data was analyzed using a repeat-measures general linear less (P<0.01, independent t-test) [Table 2].
model analysis of variance (ANOVA), whereas non-normally
distributed data were analyzed using the MannWhitney In addition to a reduction in postoperative pain and analgesic
U-test and the Chi-squared test. The sample size of 21 per requirement, STA block was also associated with reduced
group was calculated assuming a 30% reduction in opioid use recovery time [Figure 3]. Median time to discharge from
to provide 90% power at a significance level of 5%. The 30% recovery in patients who received an STA block was 65min
assumed reduction was a conservative estimate based upon compared with 110 min in the group that received port-site
prior studies which show 4570% reductions in postoperative infiltration (P < 0.005, MannWhitney U-test). The
morphine requirement following TAP blockade.[6-11]
reduction in recovery discharge time was not offset by increased
anesthetic and operative times, which did not significantly
Results differ between the treatment groups [Table 1].
Patient data and details of the anesthesia and local anesthesia
administered to each study group are shown in Table 1. No Discussion
statistical differences were found in the parameters presented
for each group in Table 1 (NS, MannWhitney U-test). Good postoperative analgesia is an important component of
adequate perioperative care. It is associated with improved
VPAS measurements were performed in order to assess the outcome, a reduction in perioperative stress, improved
quality of analgesia achieved in the study groups. Statistical patient satisfaction, and coupled with a reduction in
comparison showed that STA block was associated with lower opioid consumption, fewer adverse side effects.[15,16] The
postoperative pain scores (P < 0.01, ANOVA) [Figure1]. present study suggests that STA block reduces pain, opioid
Lower pain scores were accompanied by lower analgesic consumption, and recovery time following elective laparoscopic
requirement in the STA group. In the recovery unit, the number cholecystectomy.
of patients in each group who required fentanyl analgesia was
not significantly different [Table 2]. However, patients who To our knowledge, this is the first report of the efficacy of STA
received the STA block required significantly less fentanyl block in elective laparoscopic cholecystectomy surgery and,
analgesia than those who received local port-site infiltration whilst the data suggest a significant benefit of the procedure
compared to conventional port-site infiltration with local
a WHO Analgesia Ladder available at http://www.who. anesthetic, the study has a number of limitations. The extent
int/cancer/palliative/painladder/en/. Last accessed on 02/12/11. of the block in each group was not tested. The anesthetists
Table 2: Opioid analgesic requirement (SEM) in the 8-h post-laparoscopic cholecystectomy in patients who received
either STA block or port-site infiltration of local anesthetic (LA)
Opioid drug (mg) Proportion receiving drug Chi-squared Mean (SEM) 8-hourly requirement (mg/kg) Independent t-test
LA STA LA STA
Morphine 3/22 1/21 P = 0.61 3 0.03 1 0.9 P = 0.3
Tramadol 8/22 6/21 P = 0.75 0.54 0.21 0.27 0.1 P = 0.27
Codeine 15/22 5/21 P < 0.01 0.77 0.16 0.22 0.1 P < 0.01
STA: Subcostal transversus abdominis, LA: Local anesthetic
Journal of Anaesthesiology Clinical Pharmacology | July-September 2012 | Vol 28 | Issue 3 341
[Downloaded free from http://www.joacp.org on Saturday, August 12, 2017, IP: 47.11.234.46]
Tolchard, et al.: Sub-costal plane block and laparoscopic cholecystectomy
and surgeons administering local anesthetic were not blind the recovery unit and the overall equivalent morphine dose
to the treatment; however, neither group was involved in postoperatively. There were no differences between groups
subsequent data collection. The study is also limited in that in either non-opioid analgesic dose or the doses of anesthetic
data were collected only up until 8 h postoperatively as it agent that might have contributed to postoperative analgesia
was envisaged at the outset that day case patients would in these patient groups.
be discharged by this point. It is also noteworthy that the
post-incisional port-site infiltration was employed in this The improved quality of the postoperative analgesia associated
study. Pre-incisional infiltration is also a recognized analgesic with STA block further supports a growing body of evidence that
technique for laparoscopic cholecystectomy; however, its TAP block is superior to traditional infiltration techniques.[6-12]
efficacy compared with STA block has not been investigated This study also showed the additional benefit of a reduced
and may be superior. recovery time in patients who received STA blocks whilst not
impacting significantly on anesthetic or operation duration.
The demonstrated analgesic efficacy of STA block in
elective laparoscopic cholecystectomy is consistent with
prior studies that demonstrate reduction in opioid analgesic
requirement and reduced pain scores following TAP block
in appendicectomy, cesarean section, and laparoscopic
cholecystectomy.[5-11] It was reported previously that the
TAP block results in similar reductions in opioid use;[6]
however, this study necessitated adjustment of the port-
site positions to facilitate the anatomical distribution of
the block[11,12] and postoperative analgesia was limited to
sufentanil. In contrast to this and other studies, [6-11] the
outcome measures in the present study were considered to
better reflect current postoperative analgesia practice where
a range of non-opioid, weak, and strong opioid analgesics
are employed, as per WHO analgesic laddera. STA block
significantly reduced intravenous fentanyl requirement in
b
Figure 2: (a) The distribution of fentanyl doses (open circles) in patients who
received STA block (n = 21) or port-site infiltration of local anesthetic (n = 22).
(b) The distribution of equivalent morphine doses (open circles) in patients who
Figure 1: STA block (open circles) significantly reduced serial VPAS (mean received STA block (n = 21) or port-site infiltration of local anesthetic (n = 22)
SEM) following laparoscopic cholecystectomy compared with patients who (Median doses shown as filled circles. The n values in parentheses indicate the
received local port-site infiltration (filled circles; P < 0.01, ANOVA) number of patients with the same values in a particular group.)
342 Journal of Anaesthesiology Clinical Pharmacology | July-September 2012 | Vol 28 | Issue 3
[Downloaded free from http://www.joacp.org on Saturday, August 12, 2017, IP: 47.11.234.46]
Tolchard, et al.: Sub-costal plane block and laparoscopic cholecystectomy
funding for this project Dr S Fitzjohn for statistical advice and
contributions.
References
1. NHS Institute for Innovation and Improvement. Delivering Quality
and Value: Focus on Laparoscopic Cholecystectomy. DH, London,
2006.
2. Wall PD, Melzack R. Pain measurements in persons in pain: In:
Wall PD, Melzak R, editors. Textbook of Pain. 4th Edition: Churchill
Livingstone, 1999. p. 409-26.
3. McMinn RH. Lasts Anatomy. 9th Edition: Churchill Livingstone,
London, 1998.
4. Boddy AP, Metha S, Rhodes M. The effect of intraperitoneal local
anaesthesia in laparoscopic cholecystectomy: A systematic review.
Anesth Analg 2006;103:62-8.
5. Erol DD, Yilmaz S, Polat C, Arikan Y. The efficacy of thoracic
epidural analgesia in laparoscopic cholecystectomy. Adv Therap
Figure 3: STA block reduces median time to discharge from the recovery unit 2008;25:45-52.
following laparoscopic cholecystectomy compared with patients who received 6. El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, DelviMB,
local port-site infiltration (***P < 0.005, MannWhitney U-test). The central Thallaj A, et al . Ultrasound guided transversus abdominis
box covers the interquartile range enclosing a line representing the median. The plane block: description of a new technique and comparison
whiskers extend to the 10th and 90th percentiles and extreme values are plotted
with conventional systemic analgesia during laparoscopic
separately (filled circles)
cholecystectomy. Br J Anaesth 2009;102:763-7.
7. Kadam RV, Field JB. Ultrasound-guided continuous transverse
This effect on efficiency is a significant finding, in particular, abdominis plane block for abdominal surgery. J Anaesthesiol Clin
in hospitals such as ours, where recovery units have limited Pharmacol 2011;27:333-6.
8. Niraj G, Searle A, Mathews M, Misra V, Baban M, Kiani S, et al.
bed spaces and that are likely to see greater numbers of day Analgesic efficacy of ultrasound-guided transversus abdominis
case laparoscopic cases in future.[1] plane block in patients undergoing open appendicectomy. Br J
Anaesth 2009;103:601-5.
Finally, it is noteworthy that there were no complications of 9. Mc Donnell JG, ODonnell B, Curley G, Heffernan A, PowerC,
LaffeyJG. The analgesic efficacy of transversus abdominis
STA block in the present study; however, the study was not
plane block after abdominal surgery: A prospective randomized
powered to investigate this. All blocks were performed under controlled trial. Anesth Analg 2007;104:193-7.
ultrasound guidance which has the advantage of visualization 10. Mc Donnell JG, Curley G, ODonnell B, Heffernan A, Power C,
of needle position in relation to the transversus neurovascular Laffey JG. The analgesic efficacy of transversus abdominis plane
block after caesarean section: A prospective randomized controlled
plane and real-time image of the site at which local anesthetic
trial. Anesth Analg 2008;106:186-91.
is deposited. In this regard, the study is in keeping with the 11. Shibata Y, Sato Y, Fujiwara Y, Komatsu T. Transversus abdominis
growing body of opinion that ultrasonic guidance may be safer plane block. Anesth Analg 2007;105:883.
in the conduction of neural blockade.[17] 12. Hebbard P. Subcostal transversus abdominal plane block under
ultrasound guidance. Anesth Analg 2008;106:674-75.
13. Aldrete JA. Modification to post anaesthesia score for use in
In summary, the present study provides further evidence ambulatory surgery. J Perianaesth Nurs 1998;13:148-55.
that STA block can produce effective analgesia for upper 14. Sasada M, Smith S. Drugs in anaesthesia and intensive care. 3rded.
abdominal laparoscopic surgery.[6-11] Furthermore, it effectively Oxford: Oxford University Press; 2003.
reduces opioid analgesic requirement in elective laparoscopic 15. Wu C.L. Correlation of post-operative pain to quality of recovery
in the immediate post-operative period. Regional Anaesth Pain
cholecystectomy and reduces the burden of these patients Med 2005;30:516-22.
on recovery services. It is noteworthy that these effects were 16. Kehlet H. Surgical stress: The role of pain and analgesia. Br J
achieved with basic ultrasound devices, unilateral blocks, and Anaesth 1989;63:189-95.
single injection STA blocks. The use of bilateral blocks, multiple 17. Marhofer P, Harrop-Griffith W, Wilksche H, Kirchmair L. Fifteen
years of ultrasound guidance in regional anaesthesia. Part2. Recent
injection sites, or implanted catheters may further improve on the developments in block techniques. Br J Anaesth 2010;104:673-83.
present findings.[11,18] Future studies to evaluate the analgesic 18. Barrington MJ, Ivanusic JJ, Rozen WM, Hebbard P. Spread of
efficacy and recovery benefits of axial blocks for all abdominal injectate after ultrasound-guided transversus abdominis plane
laparoscopic techniques would also be of interest. block: a cadaveric study. Anaesthesia 2009;64:745-50.
How to cite this article: Tolchard S, Davies R, Martindale S. Efficacy of the
Acknowledgments subcostal transversus abdominis plane block in laparoscopic cholecystectomy:
Comparison with conventional port-site infiltration. J Anaesthesiol Clin
Pharmacol 2012;28:339-43.
We are grateful to the WCLRN for providing the infrastructure Source of Support: WCLRN/NIHR, UK, Conflict of Interest: None declared.
Journal of Anaesthesiology Clinical Pharmacology | July-September 2012 | Vol 28 | Issue 3 343
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- CCBsDocument1 pageCCBsDebasis SahooNo ratings yet
- Signs and Symptoms That Suggest Specific Causes of Acute Respiratory Distress SyndromeDocument1 pageSigns and Symptoms That Suggest Specific Causes of Acute Respiratory Distress SyndromeDebasis SahooNo ratings yet
- (Tec-5631) Defibrillator - With Pacing - Specs..Document1 page(Tec-5631) Defibrillator - With Pacing - Specs..Debasis SahooNo ratings yet
- Asma 2Document1 pageAsma 2Debasis SahooNo ratings yet
- AsmaokkDocument1 pageAsmaokkDebasis SahooNo ratings yet
- Eligibility For Fellowship ProgrammesDocument6 pagesEligibility For Fellowship ProgrammesDebasis SahooNo ratings yet
- NEET - SS 2018: Personal DetailsDocument2 pagesNEET - SS 2018: Personal DetailsDebasis SahooNo ratings yet
- Alr PDFDocument1 pageAlr PDFDebasis SahooNo ratings yet
- AsmaDocument1 pageAsmaDebasis SahooNo ratings yet
- Anaesthetic Management of A Patient With Ischaemic Heart Disease Undergoing Non Cardiac SurgeryDocument72 pagesAnaesthetic Management of A Patient With Ischaemic Heart Disease Undergoing Non Cardiac SurgeryDebasis SahooNo ratings yet
- AlriteDocument1 pageAlriteDebasis SahooNo ratings yet
- General Anesthesia: Anticipated Problems/ConcernsDocument1 pageGeneral Anesthesia: Anticipated Problems/ConcernsDebasis SahooNo ratings yet
- Alr PDFDocument1 pageAlr PDFDebasis SahooNo ratings yet
- Ok PDFDocument1 pageOk PDFDebasis SahooNo ratings yet
- NsaidDocument51 pagesNsaidDebasis Sahoo100% (1)
- GoodDocument1 pageGoodDebasis SahooNo ratings yet
- Measurements.: Spirometry Is The Name of The Test, Whilst A Spirometer Is The Device That Is Used To Make TheDocument7 pagesMeasurements.: Spirometry Is The Name of The Test, Whilst A Spirometer Is The Device That Is Used To Make TheDebasis SahooNo ratings yet
- God Is Great OkDocument1 pageGod Is Great OkDebasis SahooNo ratings yet
- Document PDFDocument4 pagesDocument PDFDebasis SahooNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Microneedles A Transdermal Drug Delivery SystemDocument12 pagesMicroneedles A Transdermal Drug Delivery Systemchristin stanley100% (1)
- HydrotherapyDocument25 pagesHydrotherapyleilanurse100% (1)
- SulfonamidesDocument14 pagesSulfonamidescamzyyy30No ratings yet
- Gas / Vapour Respirators: A. Horesch 96Document11 pagesGas / Vapour Respirators: A. Horesch 96Anonymous iI88LtNo ratings yet
- Pinning Ceremony1Document55 pagesPinning Ceremony1Denisse Anne SubaNo ratings yet
- Azeem (Deef)Document4 pagesAzeem (Deef)Shabbir AlamNo ratings yet
- Johnson and Johnson Iilm FinalDocument15 pagesJohnson and Johnson Iilm FinalAayushi Pandey100% (1)
- Consumer Insight and SegmentationDocument2 pagesConsumer Insight and SegmentationDatheshNo ratings yet
- Lippincott 39 S Anesthesia Review 1001 Questions A PDFDocument429 pagesLippincott 39 S Anesthesia Review 1001 Questions A PDFPeter Kazarin50% (2)
- PDFDocument444 pagesPDFOki NurpatriaNo ratings yet
- Chemical and Biological Investigation of Erythrina Variegata (Fabaceae)Document63 pagesChemical and Biological Investigation of Erythrina Variegata (Fabaceae)zakx24x7bdNo ratings yet
- Drug Therapy in Pregnancy (Soal)Document6 pagesDrug Therapy in Pregnancy (Soal)Yola FebriyantiNo ratings yet
- Anti-Epileptic DrugsDocument7 pagesAnti-Epileptic DrugsSampada ghodkiNo ratings yet
- Pharma CompaniesDocument7 pagesPharma Companiesshaishav_86100% (2)
- Formulation Development and Evaluation of Sustained Release Tablets of AceclofenacDocument128 pagesFormulation Development and Evaluation of Sustained Release Tablets of Aceclofenacraju narayana padala0% (1)
- Memorandum and Article of Association BeximcoDocument5 pagesMemorandum and Article of Association BeximcoMd. Jakir HossainNo ratings yet
- Phenytoin Sodium 50 MG Film-Coated Tablets (Phenytoin Sodium) PL 16363/0253Document17 pagesPhenytoin Sodium 50 MG Film-Coated Tablets (Phenytoin Sodium) PL 16363/0253Mohammed shamiul ShahidNo ratings yet
- MD HOW TO InfoDocument4 pagesMD HOW TO InfoMotherboardTV92% (13)
- Toxicology and Safety Assessment: (Otc and Dangerous Drugs)Document57 pagesToxicology and Safety Assessment: (Otc and Dangerous Drugs)Sheena GagarinNo ratings yet
- Journal of Integrative MedicineDocument9 pagesJournal of Integrative MedicinerurinNo ratings yet
- Code of Ethics of Pharmaceutical ProfessionDocument3 pagesCode of Ethics of Pharmaceutical ProfessionMairre Louie David PunsalanNo ratings yet
- ##Default - Genres.article## 28341 2 10 20210116Document10 pages##Default - Genres.article## 28341 2 10 20210116cyndinurvitasariNo ratings yet
- AZN Zydus - Farxiga - 15 Oct 21Document10 pagesAZN Zydus - Farxiga - 15 Oct 21XDL1No ratings yet
- Review Article: Impact of Chinese Herbal Medicine On American Society and Health Care System: Perspective and ConcernDocument7 pagesReview Article: Impact of Chinese Herbal Medicine On American Society and Health Care System: Perspective and ConcernAnonymous 6OPLC9UNo ratings yet
- Retrosynthetic Analysis: © Ravi Divakaran, 2008Document9 pagesRetrosynthetic Analysis: © Ravi Divakaran, 2008ajaysharmacdriNo ratings yet
- Corruption Within The Pharmaceutical Supply ChainDocument96 pagesCorruption Within The Pharmaceutical Supply ChainBen SchmidtNo ratings yet
- Central Nervous System StimulantsDocument83 pagesCentral Nervous System Stimulantskiran mahal100% (1)
- Hydroxypropyl CelluloseDocument4 pagesHydroxypropyl CelluloseHani AlhelwaniNo ratings yet
- Journal Pre-ProofDocument53 pagesJournal Pre-ProofAndres Fernando Silvestre SuarezNo ratings yet
- Olainfarm Product CatalogueDocument40 pagesOlainfarm Product Catalogueeverstrong0% (1)