Professional Documents
Culture Documents
Integritas Usus Pada Anak Diberi ASI Dengan Sufor
Uploaded by
Mohamad Syaikhul IslamCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Integritas Usus Pada Anak Diberi ASI Dengan Sufor
Uploaded by
Mohamad Syaikhul IslamCopyright:
Available Formats
Paediatrica Indonesiana
Volume 56 July 2016 Number 4
Original Article
Gut wall integrity in
exclusively breastfed vs. formula-fed infants
Nur Hayati, Muzal Kadim, Irawan Mangunatmadja, Soepardi Soedibyo,
Evita Bermansyah Ifran, Hikari Ambara Sjakti
A
Abstract dequate levels of nutritional intake
Background Breast milk has bioactive substances that modulate and utilization are critical to optimize
gastrointestinal maturation and maintain mucosal integrity of the childrens ongoing growth, development,
gut in infants. Markers that are both non-invasive and reliable, and health.1-2 Breast milk is the ideal
such as fecal alpha-1 antitrypsin (AAT), calprotectin, and secretory
immunoglobulin A (sIgA) have been used to assess gut integrity in
nutrition for infants and has been recommended to
adults. Higher AAT levels may imply greater enteric protein loss be given exclusively for 6 months of life.3-5 Although
due to increase intestinal permeability of immaturity gut. breastfeeding is optimal for infants, there are few
Objective To assess and compare gut integrity of exclusively breastfed conditions under which breastfeeding may not be in
(BF) and exclusively formula fed (FF) infants aged 4-6 months. the best interest of the infant. As such, formula is an
Methods Subjects were 80 healthy infants (BF=40; FF=40), alternative type of feeding. The notion that human
aged 4-6 months who visited the Pediatric Polyclinic at St. Carolus
Hospital, and lived in Pasar Minggu or Cempaka Putih Districts, milk supplies only nutrients to the infant has been
Jakarta. The fecal AAT was analyzed by an ELISA method. rectified by the discoveries of a wide spectrum of
Mann-Whitney and unpaired T-test were used to analyze possible bioactive agents that have potential targets in the
correlations between feeding type and gut integrity. gastrointestinal tract, modifying its function and
Results The BF group had significantly higher mean fecal AAT than having profound effects on its integrity in experimental
the FF group (P=0.02). Median sIgA levels were not significantly
different between groups (P=0.104). The FF group had a higher mean animals.6-8 Infant formula provides the nutrients
fecal calprotectin level but this difference was also not significant needed for adequate growth, but not all components
(P=0.443). There was a significant correlation between breastfeeding of human milk can be duplicated in formula.8
and mean fecal AAT level (P=0.02), but no significant correlation Maturation of the gastrointestinal tract is a
with calprotectin (P=0.65) or sIgA (P=0.26).
dynamic process that continues from birth to 1 to 2
Conclusion The breastfed group shows better mucosal integrity
compared to the formula fed group. Higher mean fecal AAT years of life. Intestinal maturation may be assessed
level in the BF group is related to the AAT content of breast by its permeability, secretory immunoglobulin,
milk. Therefore AAT content of BF group is actually lower than
formula fed group which shows greater mucosal integrity in BF
group. [Paediatr Indones. 2016;56:199-204. doi: 10.14238/
pi56.4.2016.199-204]. From the Department of Child Health, University of Indonesia Medical
School/Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia.
Keywords: infants; breastfeeding; markers; gut wall Reprint request: Muzal Kadim, Department of Child Health, University
integrity; fecal; alpha-1 antitrypsin; calprotectin; of Indonesia Medical School/Dr. Cipto Mangunkusomo Hospital, Jalan
secretory IgA Diponegoro no. 71, Jakarta, 10430, Indonesia. Tel. +62-21-3907742; Fax.
+62-21-3907743. E-mail: muzalk@yahoo.com.
Paediatr Indones, Vol. 56, No. 4, July 2016 199
Nur Hayati et al: Gut wall integrity in exclusively breastfed vs. formula-fed infants
and antimicrobial peptides.9 Gut wall integrity is All infants were healthy, with histories of full term
affected by gastrointestinal maturity, as defined by pregnancy (gestational age 3742 weeks) and birth
permeability changes and intestinal inflammation.7,10 weights of 2.5-4.75 kg.
Assessment of gut wall integrity in clinical practice Birth weights, lengths, head circumferences,
is a challenge. Indirect examinations that are non- age at recruitment, gender, and mode of delivery
invasive, rapid, easy, and accurate are needed to were recorded for all subjects. Fecal specimens
assess gut wall integrity. Markers of gut wall integrity were obtained from infants diapers, put in sterile
that fulfill these criteria are fecal alpha-1 antitrypsin plastic tubes, then stored at -80oC until analysis.
(AAT), calprotectin, and secretory IgA (sIgA). Calprotectin, AAT, and sIgA levels were measured
Studies with human subjects on nutritional effects in duplicate fecal aliquots using an enzyme-linked
on the growth and development of the post-natal immunoassay (Phical, Immundiagnostik, Germany).
gastrointestinal tract have been rare because of The normal levels of fecal AAT, calprotectin, and
ethical reasons related to nutritional intervention sIgA were defined (<26.8 mg/dL, 85-988 mg/kg, and
and the need for gut specimens from healthy 510-2040 g/mL, respectively) based on the manual
subjects. Studies on differences in gut wall integrity guide of the test kits.
in breastfed (BF) and formula fed (FF) infants using Data was analyzed using SPPS version 20 and
fecal AAT, calprotectin, and sIgA levels have had expressed as medians, means and standard deviations
varying results.12-17 We aimed to assess gut maturity (SD) with 95%CI. Statistical analyses on correlations
of infants in 4-6 months age interval using fecal between two qualitative variables were performed
AAT, calprotectin, and sIgA levels on exclusively using Mann-Whitney and unpaired T-test. Cut off
BF and FF babies. point levels for fecal AAT, calprotectin, and sIgA of
this study subject population was defined using ROC
curves. The correlation of qualitative and quantitative
Methods variables was analyzed using students T-test. A P value
of < 0.05 was considered to be statistically significant.
An analytic, cross-sectional study of 80 healthy babies Informed consent was obtained from parents at
was undertaken in the Pediatric Clinic at St. Carolus the time of recruitment. Protocols were approved
Hospital, as well as Pasar Minggu and Cempaka by the Medical Research Ethics Committee of the
Putih Districts, Jakarta from June to August 2013. University of Indonesia Medical Schhool/Dr. Cipto
Infants recruited were 46 months of age and were Mangunkusumo Hospital, Jakarta, Indonesia.
divided into groups according to their diet. Infants
were eligible for inclusion as breastfed or formula
fed if the mother had either exclusively breast fed or Results
exclusively formula fed her baby (i.e., the mothers did
not combine the two or add complementary food) for The characteristics of the subjects in both groups were
the entire 4-6 months before enrolling in the study. similar (Table 1).
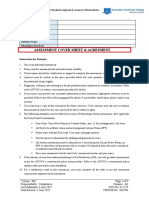
Table 1. Characteristics of subjects
Characteristics BF group FF group P value
Mean age, days 153.43 147.85 0.233b
95% CI 147.21 to 159.64 95% CI 140.83 to 154.87
Median birth weight (range), g 3,275 (2,700-3,700) 3,232.75 (2,600-4,500) 0.605a
Median birth length (range), cm 49 (47-52) 49 (47-56) 0.957a
Mean body weight, kg 7.25 7 0.249b
95% CI 6.93 to 7.58 95% CI 6.68 to 7.3
Mean body length, cm 64.79 63.58 0.083b
95% CI 64.03 to 65.56 95% CI 62.41-64.74
Mean head circumference, cm 41.93 41.41 0.078b
95% CI 41.55 to 42.3 95% CI 40.96 to 41.86
aMann-Whitney test, bunpaired T-test
200 Paediatr Indones, Vol. 56, No. 4, July 2016
Nur Hayati et al: Gut wall integrity in exclusively breastfed vs. formula-fed infants
Mean fecal AAT in the BF group was signifi- subjects less than 6 weeks of age (BF 97.66 mg/dL;
cantly higher than in the FF group, but there were no 95%CI 60.56 to 134.77 mg/dL, SF 38.4 mg/dL; 95%CI
significant differences in calprotectin and sIgA levels 0.32 to 76.39 mg/dL). In a second sampling 3 months
between groups (Table 2). later, they found the following mean levels: (BF 195.19
The marker cut-off points of the fecal level of the mg/dL; 95%CI 157.35 to 233.03 mg/dL; SF 61.7 mg/
three markers based on this study subject population dL; 95%CI 22.25 to 101.15 mg/dL).12
were AAT 133.875 mg/dL, calprotectin 205.5 mg/ A prospective, longitudinal study on 820
kg, and sIgA 777.78 g/mL. There was a significant healthy babies also had significantly higher AAT
correlation between feeding type and increased mean levels in BF babies at all age intervals. That study
AAT level, but no significant correlation between divided the subjects into six age groups, with
feeding type and mean calprotectin or median sIgA 2 groups of feeding types in subjects less than
levels (Table 3, Table 4, Table 5) 6 months of age (BF and FF), and 3 groups of
Table 2. Fecal AAT, calprotectin, and sIgA levels in the BF and FF groups
BF group FF group
Variables P value
(n=40) (n=40)
Mean AAT,mg/dL 147.43 121.84 0.02a
95% CI 135.86 to 158.99) 95% CI 103.51 to 140.17
Mean calprotectin, mg/kg 199.08 213.79 0.443a
95% CI 174.48 to 223.69 95% CI 184.08 to 243.51
Median sIgA (range), g/mL 928.81(75.1-1676.95) 530.87 (50.82-1376.95) 0.104b
aunpaired T-test, bMann-Whitney test
Table 3. Analysis of fecal AAT, calprotectin, sIgA levels and feeding types
Levels
Variables Feeding groups P value Odds ratio 95%CI
Higher* Lower*
AAT, n(%) BF (n=40) 25 (62.5) 15 (37.5) 0.02 2.78 1.12 to 6.87
FF (n=40) 15 (37.5) 25 (62.5)
Calprotectin, n(%) BF (n=40) 20 (47.6) 20 (52.6) 0.65 1.22 0.51 to 2.94
FF (n=40) 22 (52.4) 18 (47.4)
sIgA, n(%) BF (n=40) 17 (43.6) 23 (56.1) 0.26 1.65 0.68 to 4.00
FF (n=40) 22 (56.4) 18 (43.9)
*compared to cut off level in this study
Discussion feeding types in subjects more than 6 months of
age (BF, FF, and cows milk). Fecal AAT levels
The fecal AAT examination is an easy and accurate tended to be higher in the first 6 months of life
method to assess intestinal permeability and protein and tended to decrease and stabilize 6 months
enteric loss in children and adults. Higher fecal AAT later.14 In contrast, a study on 232 subjects (aged
level shows greater gut wall permeability which cause 7 days-18 months) with 5 different feeding types
greater protein enteric loss.12,18 However, using AAT (exclusively BF, non-exclusively BF, exclusively
measurements to assess gut wall integrity in infants FF, cows milk, and soy formula) reportedly
has had varied results. We found a significantly higher had higher fecal AAT level in the exclusively
mean AAT level in the BF group compared to the FF BF group at < 90 days of age, but significantly
group (P=0.02). Similar results were found in another lower at 90-179 days of age (3-6 months). Their
study that involved 160 healthy, exclusively BF results showed differences in age and feeding
babies and infants who received probiotic/prebiotic- in the concentration of alpha 1-antitrypsin
supplemented formula (SF). The BF group had a which then support the theory that human
significantly higher mean AAT level (P=0.019) in milk can modulate the maturation process
Paediatr Indones, Vol. 56, No. 4, July 2016 201
Nur Hayati et al: Gut wall integrity in exclusively breastfed vs. formula-fed infants
of gastrointestinal tract and decrease enteric Fecal calprotectin levels are relatively high in the
protein loss because the differences may reflect first few weeks in life of term or premature infants
subtle changes in gastrointestinal tract function compared to healthy children and adults. However,
in infancy.13 we found no significant difference in fecal calprotectin
In our study, elevated fecal AAT concentra- levels between the BF and FF groups (P=0.443). In
tions were found in both the BF and FF groups. The comparison, a study of 69 four-day-old infants who
comparison of higher and lower value was assessed by were healthy and exclusively BF or FF, also found
both the cut-off in the test kit module (<26.8 mg/dL) no significant difference in fecal calprotectin levels
and the cut off point from this studys subject popula- between groups. The study consisted of 3 groups:
tion (133.875 mg/dL). The higher fecal AAT level in 18 subjects on standard formula, 19 subjects on
exclusively BF babies is derived from human milk.15 prebiotic-supplemented formula, and 32 subjects were
The role of AAT is to protect human milk protein exclusively BF. The FF group showed a higher level of
content (such as immunoglobulin) escape intestinal fecal calprotectin, but it was not significantly different
degradation. The AAT only works in an intact form.15 compared to the other 2 groups. All groups showed a
One study demonstrated high AAT concentrations higher calprotectin level compared to the reference
in human milk (0.3-0.6 mg/mL) in the early weeks value in healthy adults (50 g/g). That study demon-
of lactation which persisted for the first few months strated no correlation between feeding type and fecal
of life. The AAT consumed by exclusively BF babies calprotectin level.17 Another report on 70 healthy
is excreted and significant quantities of intact AAT 3-month-old babies also revealed no difference in
(25-60%) can be found in feces.15 In our study, ev- fecal calprotectin levels between exclusively BF and
enthough we found a significant correlation between FF babies (P=0.09).18 In addition, another study on
mean fecal AAT level in both group, anyhow those 160 healthy babies who were either exclusively BF or
values were obtained without taking intact AAT from received prebiotic/probiotic supplemented formula
breastmilk in feces into account. Based on literature, revealed no significant difference in fecal calprotectin
25-60% of the fecal AAT levels in the BF group in level between the first sampling (< 6 weeks of age)
our study implied that 36.85-88.46 mg/dL AAT came and at second (3 months later) (P=0.393).12 Our
from the breast milk. Accordingly, the AAT level that study could not be compared to previous studies due
solely reflect protein entering the intestine from the to differences in age intervals of the subjects, thus
intra-vascular space was 58.97-110.88 mg/dL and that the result consistently showed a higher level of fecal
value was still lower than FF groups fecal AAT level calprotectin in FF babies.
(121.84 mg/dL). Since the FF group did not get AAT The lack of a significant difference in fecal
from formula milk so it could be concluded that the calprotectin levels in our study may be explained
high fecal AAT level of this group is caused purely by by several factors. The first factor is that human
the protein enteric loss. Similar to a previous study on milk contributed to the increasing calprotectin level
820 healthy babies, we found a significant correlation in BF babies. Human milk contains monocytes/
between fecal AAT level and exclusive breastfeeding. macrophages (59-63%) and those are known to
In that study, the exclusively BF babies had higher contain calprotectin.2,6 The second factor is that most
AAT levels at all age intervals (2-52 weeks).13 FF subjects received prebiotic/probiotic-supplemented
Calprotectin has been used as an accurate fecal formula. The acid environment that created by the
and gut inflammation marker for the last 10 years. fermentation process may increase the Bifidobacteria
Calprotectin is resistant to enzyme degradation, and Lactobacillus populations, precipitating sIgA
stabile at room temperature, and easy to measure in production. Prebiotics could also prevent pathogen
fecal specimens. High calprotectin levels are indica- attachment. Those two conditions would decrease the
tive of increased mucosal leukocyte and granulocyte inflammation process in the intestinal lumen.2,19-21 The
migration to the intestinal lumen.11 Gut inflammation first factor made the fecal calprotectin level of BF babies
is caused by several factors such as mucosal deterio- tend to increase and the second made the calprotectin
ration, or intestinal leakage related to pathological level tend to decrease because of the decreasing
processes or immaturity, as is the focus of this study. inflammation process in the intestinal lumen.
202 Paediatr Indones, Vol. 56, No. 4, July 2016
Nur Hayati et al: Gut wall integrity in exclusively breastfed vs. formula-fed infants
The normal median fecal calprotectin level for groups that could be caused by the use of prebiotic/
infants aged 3 to 6 months is 278 mg/kg (range 85- probiotic-supplemented formula in most of the
988 mg/kg).22 The mean level of both groups in our FF group subjects. Nine subjects (22.5%) had
study were in the normal range and not significantly standard formula, 26 subjects (65%) had prebiotic-
different. However, the FF group had a higher mean supplemented formula, and 5 subjects (12.5%) had
level than that of the BF group, based on the cut off probiotic-supplemented formula. While comparing
point of this study subject population. The fact was standard formula to prebiotic-supplemented formula,
revealed a higher inflammation process in FF babies a previous study demonstrated a significantly higher
compared to BF babies. fecal sIgA level in the prebiotic-supplemented group
Fecal sIgA has been known to have a strong until 4 months of age.21 Prebiotics or oligosaccharides
correlation with neutralizing ability and clearing of in the intestinal lumen undergo fermentation that
pathogenic microbes.2,6,23 Another study on infants < can increase the growth and activity of Bifidobacteria
2 months of age revealed that the level of fecal sIgA in and Lactobacillus. The acid environment caused
the BF group was significantly higher at weeks 2, 4, and by fermentation acts as a signal to the gut defense
8 compared to that of the FF group. In another report mechanism to produce sIgA. Probiotics have a role
on 34 healthy term babies, it was demonstrated that in the fermentation process.2,21
BF infants had significantly higher levels of fecal sIgA There was no significant correlation between
than FF infants at 1, 2, and 5 months of age. Fecal sIgA feeding type and increased fecal sIgA in this study. A
peaked at the age of 1 month, then gradually decreased previous study demonstrated decreased sIgA in human
until the age of 5 months in the BF group. This could milk in the first 6 months along with increased fecal
be due the mean sIgA concentration in breast milk sIgA at 1-5 months of age.24 Thus, the increased fecal
decreasing from 1 to 0.5 mg/mL between 1 month and sIgA is not only caused by human milk consumption,
6 months of age. Thus, fecal sIgA levels were markedly but also due to the maturity of GIT immunity that
influenced by the intake of breast milk.24 increases with age.
Another study on the immunological devel- In conclusion, BF infants have better mucosal
opment of the gastrointestinal system in the first 8 integrity compared to FF infants as shown by the
months of life found that fecal sIgA was detected in all significantly higher fecal AAT level in BF babies
infants from birth, with comparable levels in preterm related to the AAT from breastmilk. The FF infants
and term infants. Levels in BF infants were highest at have a higher level of calprotectin, although they do
birth, then decreased. The BF group had higher levels not get calprotectin from formula as the BF infants
compared to FF group throughout the study. We thus get from breastmilk. The BF babies have a higher
inferred that fecal IgA levels reflect breast-milk IgA fecal sIgA level, although most of the FF subjects used
content, because along with the decrease in breast prebiotic-supplemented formula.
milk IgA level, the fecal IgA level decreased. Since
fecal IgA levels were 3-9 times higher than levels in
BF infants, either breast milk may have a stimulatory Conflict of interest
effect, or breast milk IgA may be concentrated in the
colon, or both.25 None declared.
The two groups in our study had normal fecal
sIgA levels based on the literature (510-2,040 g/mL). References
However, the BF group had higher median fecal sIgA
level of based on the cut off point of this study subject 1. Diehl-Jones WL, Askin DF. Nutritional modulation of
population compared to that of the FF group. The high neonatal outcomes. AACN Clin Issues. 2004;15:83-96.
fecal sIgA level in the BF group may be explained by 2. Hegar B, Sahetapy M. Air susu ibu dan kesehatan saluran
bioactive substances in human milk such as TNF- cerna. In: Hegar B, Suradi R, Hendarto A, Partiwi IGA,
alpha, IL-1, IL-6, and IL-10 that activate both B- and editors. Bedah ASI. 1st ed. Jakarta: Balai Penerbit FKUI;
T-lymphocytes, increasing sIgA production.2,23,27 2008. p. 57-67.
We found no significant difference between 3. American Academy of Pediatrics Work Group on Breastfeed-
Paediatr Indones, Vol. 56, No. 4, July 2016 203
Nur Hayati et al: Gut wall integrity in exclusively breastfed vs. formula-fed infants
ing. Breastfeeding and the use of human milk. Pediatrics. of enteric protein loss. Acta Paediatr. 1990;79:137-41.
1997;100:1035-9. 16. Compeotto F, Butel MJ, Kalach N, Derrieux S, Aubert-Jacquin
4. Besar DS, Eveline PN. Air susu ibu dan hak bayi. In: Hegar C, Barbot L, et al. High faecal calprotectin concentrations
B, Suradi R, Hendarto A, Partiwi IGA, editors. Bedah ASI. in newborn infants. Arch Dis Child Fetal Neonatal Ed.
1st ed. Jakarta: Balai Penerbit FKUI; 2008. p. 1-16. 2004;89:F353-5.
5. Hegar B. Nilai menyusui. In: Suradi R, Hegar B, Partiwi IGA, 17. Rosti L, Braga M, Fulcieri C, Sammarco G, Manenti B, Costa
Marzuki AN, Ananta Y, penyunting. Indonesia menyusui. 1st E. Formula milk feeding does not increase the release of the
ed. Jakarta: IDAI; 2010 . p. 1-12. inflammatory marker calprotectin, compared to human milk.
6. Goldman AS. Modulation of the gastrointestinal tract of Pediatr Med Chir.2011;33:178-81.
infants by human milk. Interfaces and interactions. An 18. Strygler B, Nicar MJ, Santangelo WC, Porter JL, Fordtran JS.
evolutionary perspective. J Nutr. 2000;130:426S-31S. Alpha 1-antitrypsin excretion in stool in normal subjects and
7. Colome G, Sierra C, Blasco J, Garcia MV, Valverde E, Sanchez in patients with gastrointestinal disorders. Gastroenterology.
E. Intestinal permeability in different feedings in infancy. Acta 1990;99:1380-7.
Paediatr. 2007;96:69-72. 19. Bode L. Recent advances on structure, metabolism,
8. Le Huero-Luron, Blat S, Boudry G. Breast- vs. formula and function of human milk oligosaccharides. J Nutr.
feeding: impacts on the digestive tract and immediate and 2006;136:2127-30.
long-term health effects. Nutr Res Rev. 2010;23:23-36. 20. Gopal PK, Gill HS. Oligosaccharides and glycoconjugates in
9. Szczawinska-Poplonyk A. Development of mucosal immunity bovine milk and colostrum. Br J Nutr. 2000;84S:69-74.
in children: a rationale for sublingual immunotherapy? J 21. Bakker-Zierikzee AM, Alles MS, Knol J, Kok FK, Tolboom
Allergy. 2012;10:1-7. JJ, Bindels JG. Effects of infant formula containing a
10. Osontokun B, Kocoshis SA. Anatomy and physiology of the mixture of galacto- and fructo-oligosaccharides or viable
small and large intestine. In: Wyllie Hym JS, Kay M, editors. Bifidobacterium animalis on the intestinal microflora during
Pediatric gastrointestinal and liver disease, patophysiology, the first 4 months of life. Br J Nutr. 2005;94:783-90.
diagnosis, management. 3rd ed. Philadelphia: Elsivier Inc; 22. Fagerhol MK. Calprotectin, a faecal marker of organic
2006. p. 5-6. gastrointestinal abnormality. Lancet. 2000;356:1783-4.
11. Derikx JPM, Luyer MDP, Heineman EH, Buurman WA. Non- 23. Munasir Z, Kurniati N. ASI dan kekebalan tubuh. In: Hegar
invasive markers of gut wall integrity in health and disease. B, Suradi R, Hendarto A, Partiwi IGA, editors. Bedah ASI.
World J Gastroenterol. 2010;16:5272-79. 1st ed. Jakarta: Balai Penerbit FKUI; 2008. p. 69-81.
12. Oswari H, Prayitno L, Dwipoerwantoro PG, Firmansyah A, 24. Maruyama K, Hida M, Kohgo T, Fukunaga Y. Changes in
Makrides M, Lawley B, et al. Comparison of stool microbiota salivary and fecal secretory IgA in infants under different
composition, stool alpha 1-antitrypsin and calprotectin feeding regimen. Pediatr Int. 2009;51:342-5.
concentrations, and diarrhoeal morbidity of Indonesian 25. Kuitunen M, Savilahti E. Mucosal IgA, mucosal cows milk
infants fed breast milk or probiotic/prebiotic-supplemented antibodies, serum cows milk antibodies and gastrointestinal
formula. J Paediatr Child Health. 2013;49:1032-9. permeability in infants. Pediatr Allergy Immunol. 1995;
13. Woodruff C, Fabacher D, Latham C. Fecal alpha 1-antitrypsin 6:30-5.
and infant feeding. J Pediatr. 1985;106:228-32. 26. Hofman LF, Le T. Preliminary pediatric reference range for
14. Thomas DW, McGilligan KM, Carlson M, Azen SP, Eisenberg secretory IgA in saliva using an enzyme immunoassay. Clin
LD, Lieberman HM, et al. Fecal alpha 1-antitrypsin and Chem. 2002;48:A169-77.
hemoglobin excretion in healthy human milk-, formula-, 27. Gomela TL. Assessment of gestational age. In: Gomella
cows milk-fed infants. Pediatrics. 1986;78:305-12. TL, Cunningham MD, Eyal FG, editors. Neonatology
15. Davidson LA, Lonnerdal B. Fecal alpha 1-antitrypsin in breast- management, procedures, on-call problems, diseases, and
fed infants is derived from human milk and is not indicative drugs. 6th ed. New York: McGraw Hill; 2009. p. 23-31.
204 Paediatr Indones, Vol. 56, No. 4, July 2016
You might also like
- Endometrial StudyDocument6 pagesEndometrial StudyMohamad Syaikhul IslamNo ratings yet
- Jurnal Ginekologi 4 Menstrual PhysiologyDocument14 pagesJurnal Ginekologi 4 Menstrual PhysiologyMohamad Syaikhul IslamNo ratings yet
- Endometrial StudyDocument6 pagesEndometrial StudyMohamad Syaikhul IslamNo ratings yet
- Jurnal Kontrasepsi 1 - Injectable and Oral ContraceptiveDocument11 pagesJurnal Kontrasepsi 1 - Injectable and Oral ContraceptiveMohamad Syaikhul IslamNo ratings yet
- Bedah Digestif - Jurnal LaparotomiDocument9 pagesBedah Digestif - Jurnal LaparotomiDenny EmiliusNo ratings yet
- Determinan of Symptomatic Vulvovaginal CandidiasisDocument10 pagesDeterminan of Symptomatic Vulvovaginal CandidiasisMohamad Syaikhul IslamNo ratings yet
- Jurnal Ginekologi 1 TargetingDocument9 pagesJurnal Ginekologi 1 TargetingAndayanaIdhamNo ratings yet
- The Association Between Endometriomas and Ovarian Cancer: Preventive Effect of Inhibiting Ovulation and Menstruation During Reproductive LifeDocument10 pagesThe Association Between Endometriomas and Ovarian Cancer: Preventive Effect of Inhibiting Ovulation and Menstruation During Reproductive LifeMohamad Syaikhul IslamNo ratings yet
- Gi 3Document21 pagesGi 3Mohamad Syaikhul IslamNo ratings yet
- G1 PDFDocument8 pagesG1 PDFMohamad Syaikhul IslamNo ratings yet
- The Association Between Endometriomas and Ovarian Cancer: Preventive Effect of Inhibiting Ovulation and Menstruation During Reproductive LifeDocument10 pagesThe Association Between Endometriomas and Ovarian Cancer: Preventive Effect of Inhibiting Ovulation and Menstruation During Reproductive LifeMohamad Syaikhul IslamNo ratings yet
- Jurnal Obstetri 5 Chorioamnionits Bacteria ConfirmedDocument11 pagesJurnal Obstetri 5 Chorioamnionits Bacteria ConfirmedMohamad Syaikhul IslamNo ratings yet
- Jurding DR Dewi SPDocument11 pagesJurding DR Dewi SPMohamad Syaikhul IslamNo ratings yet
- Mantap Jurding ObgynDocument17 pagesMantap Jurding ObgynMohamad Syaikhul IslamNo ratings yet
- Jurnal Kontrasepsi 2 Worldwide Use Intrauterine ContraceptionDocument12 pagesJurnal Kontrasepsi 2 Worldwide Use Intrauterine ContraceptionMohamad Syaikhul IslamNo ratings yet
- Jurnal Obstetri 3 Air Pollution and PromDocument8 pagesJurnal Obstetri 3 Air Pollution and PromMohamad Syaikhul IslamNo ratings yet
- Mantap Jurding ObgynDocument17 pagesMantap Jurding ObgynMohamad Syaikhul IslamNo ratings yet
- Obgyn Jurding MantapDocument13 pagesObgyn Jurding MantapMohamad Syaikhul IslamNo ratings yet
- GTG 67 Endometrial HyperplasiaDocument31 pagesGTG 67 Endometrial HyperplasiaFinka Inarae100% (1)
- Jurding DR Dewi SPDocument11 pagesJurding DR Dewi SPMohamad Syaikhul IslamNo ratings yet
- Dihydropyridine Calcium Channel Blockers and Renal DiseaseDocument8 pagesDihydropyridine Calcium Channel Blockers and Renal DiseaseMohamad Syaikhul IslamNo ratings yet
- JUrnal TUberculosisDocument10 pagesJUrnal TUberculosisMohamad Syaikhul IslamNo ratings yet
- Journal Pone 0189126Document13 pagesJournal Pone 0189126Mohamad Syaikhul IslamNo ratings yet
- Jurnal Kontrasepsi 1 - Injectable and Oral ContraceptiveDocument11 pagesJurnal Kontrasepsi 1 - Injectable and Oral ContraceptiveMohamad Syaikhul IslamNo ratings yet
- Iodine and Thyroid Hormones During Pregnancy and PostpartumDocument15 pagesIodine and Thyroid Hormones During Pregnancy and PostpartumMohamad Syaikhul IslamNo ratings yet
- Bacte Ria Localizat Ion and Chorio N Thinning AmongDocument11 pagesBacte Ria Localizat Ion and Chorio N Thinning AmongBrenda Ruth PanjaitanNo ratings yet
- Case JawabanDocument3 pagesCase JawabanMohamad Syaikhul IslamNo ratings yet
- Endometrial StudyDocument6 pagesEndometrial StudyMohamad Syaikhul IslamNo ratings yet
- Jurnal Obstetri 5 Chorioamnionits Bacteria ConfirmedDocument11 pagesJurnal Obstetri 5 Chorioamnionits Bacteria ConfirmedMohamad Syaikhul IslamNo ratings yet
- Determinan of Symptomatic Vulvovaginal CandidiasisDocument10 pagesDeterminan of Symptomatic Vulvovaginal CandidiasisMohamad Syaikhul IslamNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Msae Msae2018-Arwm012 Full Dronespraying 2Document4 pagesMsae Msae2018-Arwm012 Full Dronespraying 2Muhammad Huzaifah Mohd RoslimNo ratings yet
- PerforationsDocument5 pagesPerforationsMariusNONo ratings yet
- Higuey, Dom Rep Mdpc/Puj: .Eff.23.MayDocument5 pagesHiguey, Dom Rep Mdpc/Puj: .Eff.23.MayVanessa Yumayusa0% (1)
- 004 VSL Datasheets US-ADocument22 pages004 VSL Datasheets US-Akmabd100% (1)
- ABS and Air Conditioner Wiring DiagramDocument207 pagesABS and Air Conditioner Wiring Diagramservice_00783% (30)
- Usos HummusDocument36 pagesUsos HummusAlisson FernandaNo ratings yet
- PP Ceylon Graphite Corp February 2023Document16 pagesPP Ceylon Graphite Corp February 2023Siddhant DhallNo ratings yet
- 1 s2.0 S0149763418301957 MainDocument24 pages1 s2.0 S0149763418301957 MainjackNo ratings yet
- Pre Mocks Y11 2023Document14 pagesPre Mocks Y11 2023Ahsan AhmedNo ratings yet
- 04 Refrigerated CargoDocument33 pages04 Refrigerated Cargosaurabh1906100% (1)
- SITHCCC018 Assessment 2Document9 pagesSITHCCC018 Assessment 2Taimoor Ahmed0% (1)
- Chemical Equation CalculationsDocument6 pagesChemical Equation CalculationsHera RiegoNo ratings yet
- Guidance On The 2010 ADA Standards For Accessible Design Volume 2Document93 pagesGuidance On The 2010 ADA Standards For Accessible Design Volume 2Eproy 3DNo ratings yet
- AquaNereda Brochure 1017 WebDocument4 pagesAquaNereda Brochure 1017 WebdmnNo ratings yet
- NCPDocument18 pagesNCPChristian Karl B. LlanesNo ratings yet
- Business Plan: in Partial Fulfillment For The Requirements in Entrepreneurship 2 Semester, S.Y. 2019-2020Document48 pagesBusiness Plan: in Partial Fulfillment For The Requirements in Entrepreneurship 2 Semester, S.Y. 2019-2020John Guden100% (1)
- Sister Letty G. Kuan Retirement and Role DiscontinuitiesDocument26 pagesSister Letty G. Kuan Retirement and Role DiscontinuitiesAbigail Faith Pretesto100% (1)
- Egyptian GlyphsDocument35 pagesEgyptian GlyphsDrMoor0% (1)
- Clean Room Laboratory ReportDocument6 pagesClean Room Laboratory ReportHaider IftikarNo ratings yet
- Effects of Climate Change and Global WarmingDocument14 pagesEffects of Climate Change and Global WarmingSwetal SosaNo ratings yet
- DC72D MK2 Genset Controller User Manual V1.5Document61 pagesDC72D MK2 Genset Controller User Manual V1.5Cristobal AvecillaNo ratings yet
- t-47 Residential Real Property Affidavit - 50108 ts95421Document1 paget-47 Residential Real Property Affidavit - 50108 ts95421api-209878362No ratings yet
- Tips For Establish Ball Pen Refill PlantDocument5 pagesTips For Establish Ball Pen Refill PlantSingam Sridhar100% (1)
- New Accreditation ToolsDocument52 pagesNew Accreditation ToolsLyle Guion Paguio100% (1)
- PC 4. Emulsiones Tipo MayonesasDocument10 pagesPC 4. Emulsiones Tipo MayonesasmadarahuchihaNo ratings yet
- Electro BladeDocument2 pagesElectro Bladeapi-19808945No ratings yet
- Solarizer Value, Spring & UltraDocument4 pagesSolarizer Value, Spring & UltraEmmvee SolarNo ratings yet
- Explorations in PersonalityDocument802 pagesExplorations in Personalitypolz2007100% (8)
- TPB - Questionnaire Sample PDFDocument10 pagesTPB - Questionnaire Sample PDFhaneena kadeejaNo ratings yet
- Electrical: Mep Project Progress ReportDocument11 pagesElectrical: Mep Project Progress ReportAvinash GuptaNo ratings yet