Professional Documents
Culture Documents
Insel 1982
Uploaded by
RavennaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Insel 1982
Uploaded by
RavennaCopyright:
Available Formats
The Sleep of Patients With
Obsessive-Compulsive Disorder
Thomas R. Insel, MD; J. Christian Gillin, MD; Angela Moore, MSW;
Wallace B. Mendelson, MD; Richard J. Loewenstein, MD; Dennis L. Murphy, MD
\s=b\ Fourteen patients with obsessive-compulsive disorder the sleep of obsessional patients to investigate biological
(OCD) were studied with all-night sleep EEG recordings. Nine similarities as well.
of these patients reported abnormal sleep patterns before the
METHODS
polygraphic study. Analysis of the sleep records disclosed
significantly decreased total sleep time with more awakenings, Patients were referred from across the country to an extensive
less stage 4 sleep, decreased rapid-eye-movement (REM) research program on OCD at the Clinical Center of the National
efficiency, and shortened REM latency compared with those of Institutes of Health, Bethesda, Md. At the time of admission, in
a group of age- and sex-matched normal subjects. These addition to a psychiatric interview (which elicited subjective
abnormalities generally resembled those of an age-matched reports of sleep disturbance) and physical examination, collateral
information was obtained from the patients' families and from case
group of depressed patients, although significant differences records of previous hospitalizations. During a two-week drug-free
remained. These findings suggest that such sleep abnormali- assessment period, patients received routine clinical chemistry
ties as shortened REM latency may not be entirely specific for tests, thyroid function studies, a 16-channel EEG, projective
primary affective illness. They also point to a possible bio- psychological tests, and a battery of obsessional and other psychi-
logical link between OCD and affective illness. atric rating inventories.
(Arch Gen Psychiatry 1982;39:1372-1377) The final diagnosis was made by one of us (T. R. I.), using the data
from two psychiatric interviews as well as the results of the
assessment battery to establish that each patient satisfied both
Obsessive-compulsive
uncommon
thoughts, ideas, images,
disorder (OCD) is a severe and
illnesscharacterized by recurrent
or behavior that the patient resists
Research Diagnostic Criteria (RDC)13 and DSM-IIP4 require-
ments for OCD. The DSM-III requires either obsessions (recur-
rent, persistent ideas, thoughts, images, or impulses that are ego
and recognizes as ego dystonic. The etiology and treatment dystonic) or compulsions (repetitive and seemingly purposeful
of this disorder have confounded psychiatrists for nearly a behaviors that are performed according to certain rules or in a
century. Although the classic symptoms of this disorder, stereotyped fashion) that are a significant source of distress to the
individual and are not due to another mental disorder. Ten of our
such as washing and checking rituals, have traditionally
been interpreted psychologically, the syndrome has been patients complained chiefly of obsessional fears or doubts that led
to checking rituals. Eight patients had a chief complaint of washing
conspicuously unresponsive to psychodynamic treat- rituals resulting from contamination fears. All the patients had
ments.1,2 Investigators of various persuasions have thus been ill for at least one year (mean duration of illness, 12 years).
sought to find some "constitutional" element that would Scores on the Leyton Obsessional Inventory for symptoms (mean,
explain the disorder. Janet,3 for instance, described the 28.8), resistance (mean, 40.4), and interference (mean, 44.8) scales
disorder as a form of psychasthenia. Anna Freud4 spoke of a were comparable to those described by Cooper16 in a study
"constitutional increase in the intensity of the anal-sadistic distinguishing obsessional neurotics from housewives with obses-
tendencies." Neuropsychological data have implicated fron- sional traits and normal subjects.
In no case was the obsessional disorder secondary to affective
tal lobe dysfunction in OCD.5 Furthermore, recent thera- illness or schizophrenia. Several patients did have affective symp-
peutic success with the tricyclic antidepressant, toms. In these cases, the Schedule for Affective Disorders and
clomipramine, has led to a "serotonin hypothesis" modeled Schizophrenia16 was administered to refine the diagnosis. Seven
on the amine hypotheses of affective illness." patients would have satisfied the DSM-III criteria for major
In an effort to extend these psychobiological approaches depressive disorder, but in each case the affective symptoms were
to the disorder, we studied the sleep of obsessional patients described by the patient as explicitly resulting from a loss of
with all-night EEG recordings. While to the best of our functioning due to specific rituals or obsessions. These patients
were thus classified as having a secondary depression. Two pa-
knowledge there have been no previous comprehensive tients in whom the affective symptoms had become autonomous
studies ofthe sleep of patients with OCD, several investiga-
tors9"11 have reported sleep abnormalities in depressed (ie, no longer related to the obsessional symptoms) and one patient
with hallucinations were excluded from this study.
patients, a group that shares several clinical features with In all, 18 patients met the criteria for OCD. Four, all with
obsessive-compulsive patients.12 The clinical affinity of the cleaning rituals, refused to participate in the sleep study because
two disorders suggested to us the importance of studying of concerns with contamination. Of the remaining 14 (eight men, six
women), the mean age was 35 years, with an age range of from 18 to
71 years. All participants agreed not to nap during the course of the
Accepted for publication April 15, 1982. study.
From the Clinical Neuropharmacology Branch (Drs Insel and Murphy) Patients were studied in their hospital beds on our clinical
and the Biological Psychiatry Branch (Drs Gillin, Mendelson, and Loewen- research unit. No patient received active medication during the
stein), National Institute of Mental Health, and the Laboratory of Neuro- three weeks before the sleep study. In seven cases, the subjects
sciences, National Institute of Aging (Ms Moore), Bethesda, Md. Dr Gillin is had been taking placebo capsules. Each of these seven had begun
now with the University of California, San Diego.
Reprint requests to Clinical Neuropharmacology Branch, National Insti- receiving placebo several days before the sleep study as part of a
tute of Mental Health, National Institutes of Health Clinical Center, six-month study of drug response.
10/3D41, Bethesda, MD 20205 (Dr Insel). Between two and four all-night tracings of the EEG electromyo-
Downloaded From: http://archpsyc.jamanetwork.com/ by a New York University User on 10/13/2015
Table 1.Sample Characteristics
Primary
Obsessive- Primary
Compulsive Affective
Disorder Normal Disorder
No._14_14_14
M/F ratio_8/6_8/6_7/7
Age,yr
Mean SE_36.4 + 4.24 35.1 3.81 35.23.47
Range_18-71_23-68_21-61
Hamilton Depression
Scale state mean 17.96(n 13)
=
... 31.40(n 10)*
=
*P<.01, Student's f test.
gram, and electro-oculogram were recorded for each subject
(sample total, 46). Each night's record was scored manually using
standard criteria.1' Sleep onset was defined as the first minute of
stage 2 or rapid-eye-movement (REM) sleep, followed by at least
eight minutes of sleep in the subsequent nine minutes. The REM
efficiency, expressed as a percentage, was calculated by dividing
the actual minutes of REM time in an REM period by the total
duration of the REM period. An individual mean was then calcu-
lated from the REM efficiency of each REM period during the
night. The REM architecture was investigated by two variables.
One method for describing REM distribution across the night in
each individual correlated REM period length with all previous
non-REM (NREM) time for each night (rREM.NREM). This measure
has been previously used by Vogel et al18 in a study of depressives.
If the duration of successive REM periods increased across the
night, as is normally the case, one should see a positive correlation. Hours
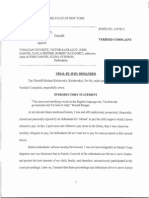
If the proportion of REM sleep was unusually high early in the Fig 1.Top, Sleep pattern of 34-year-old male normal subject.
night, a low or negative correlation should result. For the calcula- Bottom, Sleep pattern of 30-year-old subject with obsessive-com-
tion of rREM.NREM, nights with fewer than three REM periods were pulsive disorder shows reduced rapid-eye-movement (REM) la-
excluded from analysis. A group value was obtained by calculating tency (RL), reduced stage 4 sleep, and interruptions of early REM
the mean of the individual correlation coefficients. As a second sleep. His primary symptom was checking, and his Hamilton
approach to REM architecture, we tabulated REM activity, REM Depression Scale score was 13. A indicates awake, SL, sleep
time, and REM density (REM activity/REM time) for each REM latency.
period during the night. Only the second night of recording was
used for these measures of the efficiency and distribution of REM,
as this was the one postadaptation night for which data were
available on all subjects.
tailed t test for paired data comparing patients with OCD with
During the week of the sleep recordings, all patients except one normal subjects and then patients with OCD with depressed
were rated (without knowledge of the sleep results) on the 24-item
Hamilton Depression Scale,19 an obsessional subscale derived from patients. In this case, however, as the OCD data were used twice,
the Comprehensive Psychiatric Rating Scale,6 and the anxiety Bonferroni t statistics were used to render a more conservative
subscale from the Global National Institute of Mental Health interpretation of the level of significance.22 In addition, we calcu-
Scales.19 For one patient, these scales were not completed during lated linear regression coefficients for seven sleep variables
v rating scores on the depression, obsessional, and anxiety inven-
the week of the sleep study, so he was later excluded from
correlations of sleep data with rating scale scores. tories for each of the patients with OCD.
For purposes of comparison, we contrasted the findings in the RESULTS
patients with OCD with those in normal and depressed subjects Subjective Findings
previously studied in our laboratory.20 These subjects were se-
lected by matching for age and sex without reference to the sleep Of the 14 patients with OCD studied, nine reported sleep
data. As Table 1 indicates, the age means for the three groups were disturbances in the initial psychiatric assessment. In seven pa-
nearly identical. Sex matching, less important than age,21 was off tients, this was characterized as difficulty getting to sleep as well
by one subject in the depressed group. For ten of the age-matched as awakenings during the night. Two others reported hypersom-
depressed control subjects, we had Hamilton Depression Scale nia, with 12 hours of sleep per night in each case. Five patients had
scores (including the three additional items) from the week of their no symptoms related to sleep, although one of these had an earlier
polygraphic sleep studies. This group appeared to be significantly history of somnambulism. Several subjects described their awak-
more depressed than our OCD sample (Table 1). enings or difficulty falling asleep as specifically related to obses-
For both depressed and normal control groups, sleep records had sional worries, eg, arising during the night to check that gas jets or
been collected and scored in an identical fashion, except that water faucets were off. One patient linked the onset of his checking
adaptation night (ie, first night polygraphically recorded) data rituals (needing to resolve visually ambiguous stimuli) to imagery
were not available for scoring. The subsequent two nights were that began during sleep. He would awaken with a need to "resolve
used for comparisons with the OCD data. uncertainty" about the shape of a door frame or the color of a fabric
Adaptation effects for the subjects with OCD were analyzed by a and would spend much of the morning struggling with this
two-tailed t test for paired data comparing nights 1 and 2. First- dilemma. Later, this patient recovered completely with tra-
night records were not scorable in two of the subjects with OCD, nylcypromine, a drug that presumably acts like other monoamine
reducing the sample size to 12. The mean for the postadaptation oxidase inhibitors to powerfully suppress REM sleep.23
nights was calculated for each of 18 sleep-recording variables in all Another aspect of the subjective sleep complaints related to the
subjects. Again, statistical significance was determined by a two- study itself. For many of the patients, particularly those with
Downloaded From: http://archpsyc.jamanetwork.com/ by a New York University User on 10/13/2015
Table 2.Sleep Variables (Mean : SE) Obtained in Obsessive-Compulsive Patients, Normal Subjects,
and Depressed Patients
Obsessive-
Compulsive Normal Depressed
Patients Subjects Patients
(N 14)
=
(N 14)
=
(N 14)
=
Totalrecording period, min 418.27.0 439.1 7.3* 435.6 + 8.2
Sleep continuity
Sleep latency, min 32.53.0 28.8 6.7 40.87.4
Total sleep time, mln 330.9 12.6 382.6 + 8.6* 335.1 14.4
Sleep efficiency, % 79.22.7 87.2 1.8 77.53.0
Early morning awakening, mln 16.54.5 9.53.1 18.84.9
Awake-movement time, min 40.1 8.4 18.3 + 3.1* 38.29.3
Sleep architecture
Stage 1, min 21.1 2.4 13.5 1.6* 7.81.8t
Stage 1, % 6.60.9 3.60.5t 2.50.6f
Stage 2, min 194.87.9 225.28.3* 209.97.0
Stage 2, % 58.91.2 58.8 1.7 64.0 + 2.9
Stage 3, min 26.93.9 30.4 3.3 13.33.7*
Stage 3, % 8.01.2 7.8 + 0.8 3.51.0*
Stage 4, mln 12.54.2 31.86.3t 19.25.9
Stage 4, % 3.41.1 8.31.6f 5.1 1.5
Delta, % 11.61.6 16.9 + 2.2* 8.8 2.3
Rapid eye movement (REM), % 22.81.2 20.71.3 24.8 1.4
REM measures
REM latency, mln 48.48.8 80.85.5* 47.3 5.1
REM density 1.680.12 1.690.14 2.20.18
REM efficiency, %+ 83.77.9 90.47.2* 88.511.9
rfor REM time/sum previous non-REMJ ,37.16 .32 + 15
. .09.15
No. of REM periods 3.80.2 3.8 + 0.1 3.9 0.3
Total REM time, min 75.73.9 82.02.9 85.27.2
*P<.05, Bonferroni t statistics for paired data comparing obsessive-compulsive patients with either normal subjects or depressed patients.
tP<.01.
tSecond night only.
cleaning rituals, the sleep-recording procedures were a source of differences between groups, but there was a tendency for REM
considerable stress. Two patients refused to allow recordings in activity and REM density to be greater in depressed subjects,
their regular hospital bed for fear of contamination. Others in- especially early in the night. Curiously, both subjects with OCD
sisted that they shower just before and just after the sleep and depressed subjects followed a pattern of increasing REM time
recordings. One patient who reluctantly consented to the sleep until the fourth REM period, when REM time declined. In
study withdrew after two nights amid intense preoccupations that contrast, the normal subjects showed a progressive increase in
the electrode headset had contaminated her bed. REM time across all four REM periods.
Objective Findings Adaptational effects, analyzed only for the patients with OCD,
were marked for REM latency but not significant for other
Theanalysis sleep EEGs generally corroborated the sub-
of variables (Table 4). The REM latency from the first night of
jective complaints of restless, fragmented sleep (Fig 1). As Table 2 recording was nearly double that seen on the second night, thus
shows, the patients with OCD differed from their matched normal approximating the REM latency in the normal subjects from the
subjects on eight of 17 sleep variables (total recording period, the postadaptation nights.
18th variable, was not a sleep variable). Specifically, the patients A few representative sleep variables were chosen for correlation
with OCD had shorter total sleep, more awakenings, almost twice with rating data (Table 5). Sleep continuity (sleep efficiency and
as much stage 1 sleep, less stage 2 sleep, less than half the amount awake-movement time) showed a positive correlation with depres-
of stage 4 sleep, an overall decrease in the percent of delta sleep, sion and anxiety rating scale scores; however, only the correlation
and nearly a 50% reduction in REM latency compared with the with depression scores reached the P<.05 level of significance.
normal subjects. The REM efficiency, a measure of the fragmenta- Obsessional ratings, while not correlated with measures of sleep
tion within REM periods, was also reduced in the subjects with continuity, showed a trend toward an inverse relationship with
OCD. Sleep efficiency was reduced, but not to a significant level (i stage 4 sleep and a positive correlation with REM density. Of
=
2.50, P<.06). Compared with the age-matched depressed sub- interest, REM latency was not correlated with any of the three
jects, the patients with OCD differed on only two of the 17 rating scales.
variables. In this comparison, the patients with OCD had more We further divided our obsessional sample into two subgroups
stage 1 and stage 3 sleep. In addition, there was a tendency (t on the basis of the initial clinical assessment: seven with affective
=
2.40, P-C.07) for patients with OCD to have lower REM density symptoms (mean age, 39.9 years; mean Hamilton Depression Scale
than depressed patients. score, 23.4) and seven without significant affective symptoms
The correlation of REM to previous NREM sleep was equivalent (mean age, 30.3 years; mean Hamilton Depression Scale score,
for subjects with OCD and normal subjects but slightly higher in 11.7). The differences between these two subgroups were signifi-
subjects with OCD than in the depressed group. Tabulating REM cant for depression ratings ( 4.06, P<.005), but not for age or
=
time across one night (Table 3) demonstrated no significant obsessional ratings (although the more depressed subgroup was
Downloaded From: http://archpsyc.jamanetwork.com/ by a New York University User on 10/13/2015
Table 3.Distribution of Rapid-Eye-Movement (REM) Table 5.Correlation Coefficients From Sleep
Time, REM Activity, and REM Density Across REM Periods Variables v Behavioral Ratings for 13
in Night 2 (Mean SE) Obsessive-Compulsive Patients
Obsessive- Comprehensive
Compulsive Normal Depressed Hamilton Psychiatric Rating Global
_Patients_Subjects Patients Depression ScaleObsessional Anxiety
Scale Subscale Scale
REM period 1 (n 14)
=
(n 14)
=
(n 14)
=
Time, min_16.82.5_14.53.2 19.52.6 Sleep efficiency -.56* .38 -.50t
Activity, units 28.66.2 24.1 7.1_40.710.0 Awake-movement
time .55* + .37 + .53t
Density*_1.560.13 1.21 0.14 1.880.21 +
REM period 2 (n 14)
=
(n 14)
=
(n=14) Stage 1 -.34 -.25 .37
Time, min_17.62.9_19.52.9 26.24.3 Stage 4 .37 50t -.31
Activity, units 28.36.2_31.85.6_49.99.0 Rapid-eye-movement
(REM) latency -.09 .31 -.01
Density_1.560.18 1.660.22 1.94 0.14 +
REM density + .36 + .49t + .27
REM period 3 (n 12)
=
(n=14) (n=14)
REM efficiency + .04 .17 -.04
Time, min_26.25.2 24.62.2 31.1 3.4
Activity, units 41.19.8 47.27.7 62.49.31 *Ps.05.
Density_1.570.22 1.820.18 2.000.22 tPs.10.
REM period 4 (n 8)
=
(n 9)
=
(n 7)
=
Time, min_17.42.3 30.55.6 20.35.9
Activity, units 34.1
5.9_45.711.3 39.0+14.4
Density 1.91 0.14 1.92 0.31 1.77 0.28
*REM actlvity/REM time.
Table4.Comparison of Nights 1 and 2 for 12
Obsessive-Compulsive Patients (Mean SE)
Sleep Variable_Night 1_Night 2_P*
Totalsleep time, min 338.0 21.0 331.6 17.7 NS
Sleep efficiency, %_82.4 + 3.3 76.2 4.0_NS +
Awake-movement
time, min_34.78.3 46.514.0 NS
Stage 1, %_6.5 + 1.5 6.61.4 NS
Stage 4, %_3.1 1.3_2.8 1.2 + NS OCD Normal OCD Normal
Delta, %_10.1 1.8_9.3 1.6_NS (Secondary (Nondepressed)
Rapid-eye movement Depressed)
(REM) latency, min 80.9 13.4 45.412.3 <025
Total REM time, min 81.910.5 82.5 + 6.6 NS Paired r= 1.97 Paired / = 2.24
One-tailed P < .05 One-tailed P < .05
*Level of significance of f statistic for paired data, d/=1l.
(n =
7) (n 7)
=
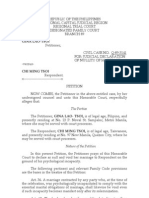
Fig 2.Mean rapid-eye-movement latency for depressed and
somewhat more obsessive). Both of these subgroups showed statis- nondepressed subgroups of patients with obsessive-compulsive
tically significant reductions in REM latency compared with age- disorder (OCD) and for age-matched normal subjects. Difference
matched normal subjects, although among the patients with OCD between OCD subgroups was not significant.
(Fig 2), the REM latency of the depressed subgroup was lower. The
difference between the depressed and nondepressed subgroups
was not statistically significant.
We considered that these findings might reflect several
COMMENT
methodological problems in the study. One difficulty, for
These subjective and objective descriptions suggest that instance, was the variability of sample size. Two of the
sleep is markedly abnormal for obsessive-compulsive pa- patients with OCD refused further sleep recordings after
tients. Earlier clinical descriptions have not mentioned the second night. Thus, for these two, only a single
sleep as impaired in this disorder,24 although a recent report postadaptation night was available for comparison with
of preliminary findings in a small group of obsessional normal and depressed subjects. To check on the validity of
adolescents described similar abnormalities of sleep effi- our findings, we reanalyzed each of the abnormal sleep
ciency, total sleep time, and REM latency.26 Both our variables for this one postadaptation night in all patients
patients' subjective reports and their EEG records dis- with OCD and normal subjects. Results were similar
closed a pattern of shallow, interrupted, inefficient, and though not identical. On this single-night comparison,
shortened sleep. These results as well as the shortened REM latency, stage 1 sleep, stage 4 sleep and awake-
REM latency suggest that the sleep of patients with OCD movement time continued to be significantly abnormal
has many similarities to that of patients hospitalized with (P<.05); total sleep and sleep efficiency showed a trend
primary depression. While the study was not directly toward being reduced in the subjects with OCD (P<.10);
designed to formally compare depressed patients and pa- and delta sleep was no longer remarkable.
tients with OCD, it appears that they differed from each Another problem was the use of placebo in half of the
other in relatively few wayspatients with OCD had more patients with OCD. Placebo effects in insomniacs are well
stage 1 and 3 sleep and tended to have less REM density known.26 The direction of these effects is opposite to the
early in the night. findings in our patients; we considered, however, that the
Downloaded From: http://archpsyc.jamanetwork.com/ by a New York University User on 10/13/2015
use of placebo might have limited the validity of treating all symptoms did not account for the short REM latency. First,
of the patients as a single group. For this reason, we depressive symptoms were not significantly correlated
compared patients with OCD who were receiving placebo with REM latency (Table 5). Second, when we divided our
with those not receiving placebo. No differences were sample into depressed and nondepressed subgroups, there
apparent on total sleep time, sleep efficiency, stage 1, stage were nonsignificant differences in REM latency between
4, REM sleep, or REM latency. Awake-movement time was the two groups, although both values were significantly
greater in subjects not taking placebo. Comparing just the shorter than that of age-matched normal subjects (Fig 2).
patients receiving placebo with matched normals continued It appears that although the patients with OCD showed a
to demonstrate differences in awake-movement time, stage reduction in REM latency that was equal in magnitude to
4 sleep, and REM latency. Patients not receiving placebo that of patients with affective disorder, there were some
had analogous mean differences from matched normals in subtle differences that warrant emphasis. For instance,
awake-movement time ( + 21.0 minutes) and REM latency Kupfer29 has shown that for patients with affective illness,
( 22 minutes), but greater variance reduced the statistical there is a significant negative correlation between the
significance of these differences. These seven patients not length of REM latency and clinical ratings of depression.
-
receiving placebo therapy did have significant increases in Such a correlation was absent in the patients with OCD.
stage 1 sleep. In a related study of 13 obsessional subjects, a Furthermore, in patients with primary affective disorder,
spectrum of clinical variables (eg, mood, obsessions, anx- REM latency is reduced on the first as well as subsequent
iety) did not change during four weeks of placebo therapy nights of laboratory sleep.30 In contrast, the patients with
(our unpublished data), also suggesting the validity of OCD showed a normal REM latency on the first night.
combining the patients with OCD as a group for analysis. Curiously, a similar "first-night effect" for REM latency has
The sleep latencies of all three groups of patients are previously been reported for patients with secondary de-
prolonged beyond those in previous reports.11 Although this pressions.30
may partly reflect our definition of sleep onset, a review of Recent formulations of the REM abnormalities in affec-
individual data disclosed that one normal subject was a tive illness have stressed not only the reduction of REM
clear outlier, with a sleep latency of 106 minutes. The mean latency (which is technically an NREM measure), but also
for the other 13 normal subjects was 22.7 minutes, which an increase in REM density and an inversion of the normal
was almost statistically shorter (P<.07) than that in the 13 REM distribution such that more REM time occurs early in
matched subjects with OCD. the night.18,31 On these two latter variables, the patients
The reduction of REM efficiency in patients with OCD with OCD did not so closely resemble patients with affec-
was consistent with the general fragmentation of sleep and tive illness. The REM density was lower in the patients with
the increase in stage 1 sleep. Reduced REM efficiency could OCD compared with the depressed patients, although this
reflect either a decrease in REM time (ie, actual number of difference did not quite reach statistical significance. Al-
minutes with REM during an REM period) or an increase in though there is no generally accepted scheme for describing
the duration of the REM periods (REM time plus interven- REM distribution, the percentage of REM time in the first
ing NREM or wakefulness). As REM time was not signifi- REM period and rREM_NREM are two variables that have been
cantly reduced in the subjects with OCD, an increase in the previously reported as abnormal in patients with primary
intrusion of NREM or awake time must have contributed to affective illness when compared with insomniacs.18 The
the lowering of REM efficiency. This fragmentation of REM subjects with OCD had 22.9% of their REM time in the first
might correspond to the subjective reports of obsessions REM period. This value lies between the normal value of
intruding into sleep, leading to brief awakenings. Unfor- 20.2% and the corresponding value in the depressed sub-
tunately, we did not record sleep mentation reports. The jects of 23.9%. On the correlational measure, the subjects
only relevant evidence we have, our correlational data with OCD appeared to be closer to the normal subjects,
(Table 5), showed no relationship between severity of obses- although the variance in each group was high. It appears,
sions and REM efficiency. There is, however, another then, that on both the percentage of REM time in the first
aspect of REM efficiency that deserves mention. This sleep REM period and the correlation of REM with previous
variable previously has been found to be reduced in absti- NREM, the subjects with OCD cannot be distinguished
nent alcoholics27 and bipolar (more than unipolar) depres- from either normal subjects or patients with primary
sives.28 In both of these earlier studies, REM efficiency was depression. The present analysis did not address whether
linked to serotonin particularly because 5-hydroxytryp- our primary depressives could indeed be separated from
tophan, a serotonin precursor, normalized the reduced age-matched normal controls on these measures.
REM efficiency of alcoholics.27 Recent pharmacologie stud- Short REM latencies have been described in other psy-
ies of OCD have likewise focused on the serotonergic chiatric entities using earlier diagnostic categories. Early
system, as clomipramine, a tricyclic antidepressant that articles reported this finding in small samples of schizo-
powerfully inhibits neuronal reuptake of serotonin, has phrenics;3234 however, these reports were later contested on
been shown to be effective in this syndrome, which the diagnostic grounds that many of these patients may
heretofore had been refractory to medications.68 While the have been schizoaffective.35 Patients with subaffective dys-
links must still be considered very tentative, it may be that thymia,36 anorexia nervosa37 (some of whom were later
the reduction in REM efficiency is another indicator of the diagnosed as depressed), and normal aging38 all may show
involvement of the serotonergic system in OCD. reduced REM latencies. Depressed subjects continue to
It was surprising to find a reduction of REM latency in show even briefer REM latencies with age.21 Whether REM
the subjects with OCD compared with normal subjects. As latency is specific for some common element in all of these
this abnormality has previously been most closely associ- syndromes remains conjectural. While the patients with
ated with primary affective illness, we considered the OCD showed very weak correlations between REM latency
possibility that our patients with OCD, many of whom were and clinical ratings, it may be that weekly ratings are less
depressed, might be suffering from primary rather than important for such a correlation than the state of the patient
secondary depressions. Two approaches using our rating just before sleep. This possibility, which is entirely hypo-
scale data, however, suggest that the severity of depressive thetical, was suggested to us because the two subjects with
Downloaded From: http://archpsyc.jamanetwork.com/ by a New York University User on 10/13/2015
OCD who had the longest REM latencies seemed the least imating the incidence of this abnormal response in affective
apprehensive about the sleep study. Future attempts at illness.44 This neuroendocrine abnormality has recently
correlating sleep measures to clinical variables might be been noted in a preliminary report of another sample of
improved by the use of ratings just before sleep. Other patients with OCD.45
variables, such as the time of going to sleep39,40 or a history of These findings, along with the recent reports of the
prior REM deprivation,41 will also need to be specified as efficacy of tricyclic antidepressants for this disorder,8 sug-
these factors can influence REM latency. gest that patients with OCD may share some of the bio-
In addition to the sleep findings, the patients with OCD logical and genetic substrates of affective illness. Retro-
shared some other similarities with those with primary spective studies have shown that even though depression is
affective disorder. For instance, one patient had a history 12 the most common complication of OCD, the disorders can be
years earlier of a circumscribed episode of major depressive distinguished on the basis of clinical course, family history,
disorder without obsessive symptoms. Three patients had and phenomenology.46"48
family histories of affective disorder in first-degree rela- More research into the psychobiological basis of this
tives; one had a family history of alcoholism. Moreover, as uncommon disorder is warranted. Our findings suggest
part of another study in a larger sample of patients, ten of that studies of biological variables that have been previ-
the patients with OCD were given the dexamethasone ously described as abnormal in affective illness may be
suppression test, which is purported to be of diagnostic particularly fruitful in studying patients with OCD. Con-
value in primary depression42 and major depressive disor- ceivably, such abnormalities could predict clinical response
der.43 Four of these patients showed no suppression, approx- to antidepressant medication.
References
1. Marks IM: Living With Fear. New York, McGraw-Hill Book Co, 1978. 26. Mendelson W: The Use and Misuse of Sleeping Pills: A Clinical
2. Mellett PG: The clinical problem, in Beech HR (ed): Obsessional Guide. New York, Plenum Press, 1980.
States. London, Methuen & Co Ltd, 1974, pp 55-94. 27. Zarcone UP, Hoddes E: Effects of 5-hydroxytryptophan on fragmen-
3. Janet P: Les obsessions et la psychasthenie. Paris, Bailliere, 1908. tation of REM sleep in alcoholics. Am J Psychiatry 1975;132:74-76.
4. Freud A: Obsessional neurosis: A summary of psychoanalytic views as 28. Duncan WC, Pettigrew KD, Gillin JC: REM architecture changes in
presented at the Congress. Int J Psychoanal 1966;47:116-122. bipolar and unipolar depression. Am J Psychiatry 1979;136:1424-1427.
5. Flor-Henry P, Yeudall LT, Koles ZJ, et al: Neuropsychological and 29. Kupfer DJ: REM latency: A psychobiologic marker for primary
power spectral EEG investigations of the obsessive-compulsive syndrome. depressive disease. Biol Psychiatry 1976;11:159-174.
Biol Psychiatry 1979;14:119-130. 30. Coble P, Foster FG, Kupfer DJ: Electroencephalographic sleep
6. Thoren P, Asberg M, Cronholm B, et al: Clomipramine treatment of diagnosis of primary depression. Arch Gen Psychiatry 1976;33:1124-1127.
obsessive compulsive disorder: A controlled clinical trial. Arch Gen Psychi- 31. Foster FG, Kupfer DJ, Coble P, et al: Rapid eye movement sleep
atry 1980;37:1281-1289. density: An objective indicator in severe medical-depressive syndromes.
7. Yaryura-Tobias JA, Bhagavan HN: L-Tryptophan in obsessive compul- Arch Gen Psychiatry 1976;33:1119-1123.
sive disorders. Am J Psychiatry 1977;123:1298-1299. 32. Feinberg I, Koresko R, Gottlieb F, et al: Sleep electroen-
8. Insel T, Murphy DL: The psychopharmacologic treatment ofobsessive cephalographic and eye movement patterns in schizophrenic patients.
compulsive disorder: A review. J Clin Psychopharmacol 1981;1:304-311. Compr Psychiatry 1964;5:44-53.
9. Chen CN: Sleep, depression and antidepressants. Br J Psychiatry 33. Stern N, Fram D, Greenspoon L, et al: All night sleep studies of acute
1979;135:385-402. schizophrenics. Arch Gen Psychiatry 1969;20:470-477.
10. Kupfer DJ, Foster FG, Goble P, et al: The application of EEG sleep for 34. Jus K, Bouchard M, Jus AK, et al: Sleep EEG studies in untreated
the differential diagnosis of affective disorders. Am J Psychiatry 1978;135: long term schizophrenic patients. Arch Gen Psychiatry 1973;29:386-390.
69-74. 35. Reich L, Weiss BL, Coble P, et al: Sleep disturbance in schizophrenia:
11. Gillin
JC, Duncan W, Pettigrew K, et al: Successful separation of A revisit. Arch Gen Psychiatry 1975;32:51-55.
depressed, normal, and insomniac subjects by EEG sleep data. Arch Gen 36. Akiskal HS, Rosenthal TL, Haykal RF, et al: Characterological
Psychiatry 199;136:85-90. depressions. Arch Gen Psychiatry 1980;37:777-783.
12. Videbech T: The psychopathology of anacastic endogenousdepres-- 37. Neal JF, Merikanges JR, Foster FG, et al: Waking and all night sleep
sion. Acta Psychiatr Scand 1975;52:336-373. EEGs in anorexia nervosa. Clin Electroencephalogr 1980;11:9-15.
13. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria: 38. Feinberg I, Koresko RL, Heller N: EEG sleep patterns as a function
Rationale and reliability. Arch Gen Psychiatry 1978;35:773. of normal and pathologic aging in man. J Psychiatr Res 1967;15:107-144.
14. Diagnostic and Statistical Manual of Mental Disorders, ed 3. 39. Czeisler CA, Weitzman ED, Moore-Ede M, et al: Human sleep: Its
Washington, DC, American Psychiatric Association, 1980. duration and organization depend on its circadian phase. Science 1980;210:
15. Cooper J: The Leyton Obsessional Inventory. Psychol Med 1970;1: 1264-1267.
48-64. 40. Karacan I, Finley WW, Williams RC, et al: Changes in stage 1, REM
16. Spitzer RL, Endicott J: Schedule for Affective Disorders and Schizo- and stage 4 sleep during naps. Biol Psychiatry 1970;2:261-265.
phrenia. New York, State Psychiatric Institute, 1975. 41. Dement W, Henry P, Cohen H, et al: Studies of the effect of REM
17. Rechtschaffen A, Kales A: A Manual of Standardized Terminology, deprivation in humans and animals. Res Publ Assoc Res Nerv Ment Dis
Techniques and Scoring System for Sleep Stages of Human Subjects, 1967;45:456-460.
publication 234. Dept. of Health, Education and Welfare, 1968. 42. Schlesser MA, Winokur G, Sherman BM: Genetic subtypes of unipo-
18. Vogel GW, Vogel F, McAbee RS, et al: Improvement of depression by lar primary depressive illness distinguished by hypothalamic-pituitary-
REM sleep deprivation: New findings and a theory. Arch Gen Psychiatry adrenal axis activity. Lancet 1979;1:739-741.
1980;37:247-253. 43. Carroll BJ, Feinberg M, Greden JF, et al: A specific laboratory test
19. Murphy DL, Pickar D, Alterman IS: Methods for the quantitative for the diagnosis of melancholia: Standardization, validation, and clinical
assessment of depressive and manic behavior, in Burdock EI, Sudilovsky A, utility. Arch Gen Psychiatry 1981;38:15-22.
Gershon S (eds): Quantitative Techniques for the Evaluation of the Behavior 44. Insel TR, Kalin NH, Guttmacher LB, et al: The dexamethasone
of Psychiatric Patients. New York, Marcel Dekker Inc, 1982, pp 355-392. suppression test in patients with obsessive compulsive disorder. Psychiatr
20. Gillin JC, Duncan WC, Murphy DL, et al: Age-related changes in Res 1982;6:153-160.
sleep in depressed and normal subjects. Psychiatr Res 1981;4:73-78. 45. Asberg M, Thoren P: Clomipramine treatment of obsessive-compul-
21. Ulrich RF, Shaw DH, Kupfer DJ: Effects on aging on EEG sleep in sive disorder: Biochemical and pharmacological aspects. Read before the
depression. Sleep 1980;3:31-40. Third World Congress of Biological Psychiatry, Stockholm, June 28, 1981.
22. Miller RG Jr: Simultaneous Statistical Inference. New York, John 46. Goodwin D, Guze S, Robins E: Follow-up studies in obsessional
Wiley & Sons Inc, 1966, p 200. neurosis. Arch Gen Psychiatry 1969;20:182-187.
23. Akindele MO, Evans JI, Oswald I: Monoamine oxidase inhibitors, 47. Coryell W: Obsessive-compulsive disorder and primary unipolar
sleep, and mood. Electroencephalogr Clin Neurophysiol 1970;29:47-56. depression: Comparisons of background, family history, course, and mor-
24. Nemiah J: Obsessive compulsive neurosis, in Freedman A, Kaplan H, tality. J Nerv Ment Dis 1981;169:220-224.
Sadock B (eds): A Comprehensive Textbook of Psychiatry. Baltimore, 48. Kendell RE, Discipio WJ: Obsessional symptoms and obsessional
Williams & Wilkins Co, 1975, pp 1241-1255. personality traits in patients with depressive illness. Psychol Med 1970;1:
25. Rapaport J, Elkins R, Langer DH, et al: Childhood obsessive 65-72.
compulsive disorder. Am J Psychiatry 1981;138:1545-1554.
Downloaded From: http://archpsyc.jamanetwork.com/ by a New York University User on 10/13/2015
You might also like
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- HHS Public Access: Hoarding Disorder: More Than Just A Problem of Too Much StuffDocument5 pagesHHS Public Access: Hoarding Disorder: More Than Just A Problem of Too Much StuffRavennaNo ratings yet
- HHS Public Access: Antidepressant Use and Cognitive Decline: The Health and Retirement StudyDocument16 pagesHHS Public Access: Antidepressant Use and Cognitive Decline: The Health and Retirement StudyRavennaNo ratings yet
- HAZMAT Happens: The Premiere Hazmat Training For The Healthcare ProfessionalDocument2 pagesHAZMAT Happens: The Premiere Hazmat Training For The Healthcare ProfessionalRavennaNo ratings yet
- Stenglerwenzke2007 PDFDocument8 pagesStenglerwenzke2007 PDFRavennaNo ratings yet
- MIlosz, Czeslaw - To Begin Where I Am (2001, FSG) PDFDocument481 pagesMIlosz, Czeslaw - To Begin Where I Am (2001, FSG) PDFRavenna100% (6)
- Immune Aberrations in Obsessive-Compulsive Disorder: A Systematic Review and Meta-AnalysisDocument9 pagesImmune Aberrations in Obsessive-Compulsive Disorder: A Systematic Review and Meta-AnalysisRavennaNo ratings yet
- 10 1016@j Jocn 2018 10 042Document11 pages10 1016@j Jocn 2018 10 042RavennaNo ratings yet
- Cassidy2013 Attachment Theory and Research PDFDocument39 pagesCassidy2013 Attachment Theory and Research PDFRavenna0% (1)
- Is A Psychodynamic Perspective Relevant To The Clinical Management of Obsessive-Compulsive Disorder?Document12 pagesIs A Psychodynamic Perspective Relevant To The Clinical Management of Obsessive-Compulsive Disorder?RavennaNo ratings yet
- Journal of Clinical Neuroscience: Fernanda B. Melo-Felippe, Leonardo F. Fontenelle, Fabiana B. KohlrauschDocument6 pagesJournal of Clinical Neuroscience: Fernanda B. Melo-Felippe, Leonardo F. Fontenelle, Fabiana B. KohlrauschRavennaNo ratings yet
- Neurotransmitters, Temperament and Social Functioning: ReviewDocument14 pagesNeurotransmitters, Temperament and Social Functioning: ReviewRavennaNo ratings yet
- Ostracism and Indirect Reciprocity: The Reproductive Significance of HumorDocument18 pagesOstracism and Indirect Reciprocity: The Reproductive Significance of HumorRavennaNo ratings yet
- Role of Psilocybin in The Treatment of Depression: Ananya Mahapatra and Rishi GuptaDocument3 pagesRole of Psilocybin in The Treatment of Depression: Ananya Mahapatra and Rishi GuptaRavennaNo ratings yet
- N-Acetylcysteine in The Treatment of Psychiatric Disorders: Current Status and Future ProspectsDocument51 pagesN-Acetylcysteine in The Treatment of Psychiatric Disorders: Current Status and Future ProspectsRavennaNo ratings yet
- A Case Series of 223 Patients With Depersonalization-Derealization SyndromeDocument11 pagesA Case Series of 223 Patients With Depersonalization-Derealization SyndromeRavennaNo ratings yet
- Bokor 2014Document15 pagesBokor 2014RavennaNo ratings yet
- Personality Disorders and Culture: Contemporary Clinical Views (Part B)Document13 pagesPersonality Disorders and Culture: Contemporary Clinical Views (Part B)RavennaNo ratings yet
- Nihms836647 PDFDocument4 pagesNihms836647 PDFRavennaNo ratings yet
- Furey2006 Antidepressant ScopolamineDocument9 pagesFurey2006 Antidepressant ScopolamineRavennaNo ratings yet
- Umr Cnrs 5249, Grenoble, France Cea, DSV, Irtsv, Grenoble, France Àuniversite Joseph Fourier, Grenoble, FranceDocument10 pagesUmr Cnrs 5249, Grenoble, France Cea, DSV, Irtsv, Grenoble, France Àuniversite Joseph Fourier, Grenoble, FranceRavennaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Case Study - Ben & Jerry'sDocument7 pagesCase Study - Ben & Jerry'sLinh Phan Thị MỹNo ratings yet
- WAH ChecklistDocument2 pagesWAH ChecklistLiko A. PaddingtoneNo ratings yet
- A Great FraudDocument38 pagesA Great FraudHorsetail Goatsfoot100% (5)
- Ancient China Lesson PlanDocument2 pagesAncient China Lesson Planburns8459No ratings yet
- Interpretation and Construction of The Indemnity Clauses: A Judicial AnalysisDocument14 pagesInterpretation and Construction of The Indemnity Clauses: A Judicial AnalysisIshwarNo ratings yet
- Gestures - Vilém FlusserDocument208 pagesGestures - Vilém FlusserrachelcocNo ratings yet
- SLCUNM PetitionerDocument32 pagesSLCUNM PetitionerAnkit Tiwari100% (1)
- Fostering Digital CitizenshipDocument15 pagesFostering Digital CitizenshipDeepak Gupta (DG)No ratings yet
- Mackie s Logical Argument from Evil ααand PDFDocument16 pagesMackie s Logical Argument from Evil ααand PDFΠαύλος ΣιλβέστροςNo ratings yet
- Complaint Supreme 2013Document58 pagesComplaint Supreme 2013SLAVEFATHERNo ratings yet
- Change Management or LeadershipDocument13 pagesChange Management or Leadershipnmmng2011100% (2)
- What Is Vote BuyingDocument10 pagesWhat Is Vote BuyingFatih GamaNo ratings yet
- Gender Equality in IslamDocument12 pagesGender Equality in IslamSyed Anwer ShahNo ratings yet
- The Filibustero and El Filibusterismo PDFDocument74 pagesThe Filibustero and El Filibusterismo PDFsvpsNo ratings yet
- Conformity Assessment Cross-Reference Table: Title Applicable Ce Marking? Notified Body Category InvolvmentDocument1 pageConformity Assessment Cross-Reference Table: Title Applicable Ce Marking? Notified Body Category InvolvmentAmit DamaNo ratings yet
- To Be Executed On Non-Judicial Stamp Paper of Appropriate Value and NotarizedDocument3 pagesTo Be Executed On Non-Judicial Stamp Paper of Appropriate Value and NotarizedKiranNo ratings yet
- Critical Review By:: Shema Sheravie Ivory F. QuebecDocument3 pagesCritical Review By:: Shema Sheravie Ivory F. QuebecShema Sheravie IvoryNo ratings yet
- Pre Job Hazard Assessment: Our Goal Is Injuries in The WorkplaceDocument1 pagePre Job Hazard Assessment: Our Goal Is Injuries in The WorkplaceNadya ShintaNo ratings yet
- 첨부5 투심위 운영규정 ENGDocument3 pages첨부5 투심위 운영규정 ENGYoung-Kwon LeeNo ratings yet
- Mangaliag V CatubigDocument1 pageMangaliag V CatubigMiguel CastricionesNo ratings yet
- Chi Ming Tsoi Sample PleadingDocument5 pagesChi Ming Tsoi Sample Pleadingbeth_afanNo ratings yet
- Strategic Management and Business Policy Bba-Vi Semester Unit-IiDocument25 pagesStrategic Management and Business Policy Bba-Vi Semester Unit-IiAmit Srivastava100% (1)
- Alt ParadigmDocument14 pagesAlt Paradigmali3800No ratings yet
- Judicial CanonsDocument7 pagesJudicial CanonsTNVTRLNo ratings yet
- Module 4 - Code of EthicsDocument14 pagesModule 4 - Code of EthicsSienna Mae AgringoNo ratings yet
- Never Despair in The Mercy of Allah - Forgiveness: Islamic PerspectiveDocument2 pagesNever Despair in The Mercy of Allah - Forgiveness: Islamic PerspectiveMohammed Abdul Hafeez, B.Com., Hyderabad, IndiaNo ratings yet
- $3.5 Billion Man With Pictures 2Document106 pages$3.5 Billion Man With Pictures 2Raymond YoungNo ratings yet
- 100 QuotesDocument24 pages100 Quotesc_abhijit468547No ratings yet
- Bar - Bar Waiter-EssDocument3 pagesBar - Bar Waiter-EssSebastia Felipe SolisNo ratings yet
- Advertisement Law in HungaryDocument8 pagesAdvertisement Law in HungaryShiroi ShichiNo ratings yet