Professional Documents
Culture Documents
Chronic Kidney Disease and Its Management: A Review
Uploaded by
Baru Chandrasekhar RaoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chronic Kidney Disease and Its Management: A Review
Uploaded by
Baru Chandrasekhar RaoCopyright:
Available Formats
IAJPS 2017, 4 (11), 3803-3805 Mehvish Adil and Mariam Zaka ISSN 2349-7750
CODEN [USA]: IAJPBB ISSN: 2349-7750
INDO AMERICAN JOURNAL OF
PHARMACEUTICAL SCIENCES
http://doi.org/10.5281/zenodo.1039860
Available online at: http://www.iajps.com Review Article
CHRONIC KIDNEY DISEASE AND ITS MANAGEMENT:
A REVIEW
Mehvish Adil *and Mariam Zaka
Lahore College for Women University, Jail Road Lahore, Pakistan
Abstract:
Chronic kidney disease (CKD) is a major public health problem worldwide and its prevalence is increasing day by
day. CKD defines as kidney damage or a decreased glomerular filtration rate of less than 60 mL/min/1.73 m 2 for 3
or more months irrespective of cause. It has deeper effects on morbidity, mortality, health care costs, as well as on
patient quality of life and on important social implications. CKD patients have several other co-morbidities such as
hypertension, diabetes mellitus, coronary artery disease and anemia , and due to these co morbidities, patients are
on multiple medications, and are higher risk of developing drug-related problems. Hypertension is a major
promoter of the decline in glomerular filtration rate (GFR) and a strong independent risk factor along with
Diabetes mellitus for CKD. Treatment of high blood pressure is recommended for all individuals with, or at risk of,
chronic kidney disease. Glycemic control can help to prevent the onset of early stages of chronic kidney disease in
individuals with diabetes. Better management of CKD can slow the progression of CKD, prevent complications, and
reduce cardiovascular-related outcomes and improve patients quality of life.
Key words: chronic kidney disease, Glomerular filtration rate, Hypertension, Diabetes mellitus, Drug related
problem, Angiotensin converting enzyme inhibitor, end stage renal disease, National Kidney Foundation, quality of
life,
Corresponding author:
Mehvish Adil, QR code
Lahore College for Women University,
Jail Road Lahore,
Pakistan
Email Id: mehvish.adil777@gmail.com
Contact no: 0302-4684319
Please cite this article in press as Mehvish Adil et al , Chronic Kidney Disease and Its Management:
A Review, Indo Am. J. P. Sci, 2017; 4(11).
www.iajps.com Page 3803
IAJPS 2017, 4 (11), 3803-3805 Mehvish Adil and Mariam Zaka ISSN 2349-7750
INTRODUCTION: The major part of this increase is caused by such
Chronic kidney disease (CKD) is a worldwide public lifestyle-related factors as hypertension and diabetic
health problem. Chronic kidney disease is a global nephropathy. The association between obesity,
threat to health for developing and under developing smoking, and physical activity and chronic kidney
countries because of an increasing incidence, poor disease (CKD) are important. It is known that
outcome, and high cost of treatment. It is a general obesity leads to ESRD through diabetes mellitus and
term for heterogeneous disorders affecting kidney hypertension, but obesity also can contribute directly
structure and function. The Kidney Disease to kidney damage through obesity-related
Outcomes Quality Initiative (K/DOQI) of the glomerulopathy, mechanical compression, and a
National Kidney Foundation (NKF) defines CKD as cascade of other hemodynamic and metabolic
kidney damage or a decreased glomerular filtration mechanisms. [6]
rate of less than 60 mL/min/1.73 m2 for 3 or more It is recommended that both diabetic and non-
months, irrespective of the cause. [1] diabetic adults with CKD and urine albumin
Chronic kidney disease is a common disorder and its excretion <30 mg/24 hours (or equivalent) whose BP
prevalence is increasing worldwide day by day.[2] is consistently >140 mm Hg systolic or >90 mm Hg
According to the World Health Report 2002 and diastolic should be treated with BP-lowering drugs to
Global Burden of Disease (GBD) project, diseases of maintain a BP that is consistently 140 mm Hg
the kidney and urinary tract contribute to the global systolic and 90 mm Hg diastolic and also
burden of diseases, with approximately 850,000 recommended that an ARB [angiotensin-receptor
deaths every year and 15,010,167 disability-adjusted blocker] or ACE-I [angiotensin-converting enzyme
life years . They are the 12th cause of death and the inhibitor] be used in both diabetic and non-diabetic
17th cause of disability, in the world. [3] adults with CKD and urine albumin excretion >300
Chronic kidney disease has profound effects on mg/24 hours .
morbidity, mortality, and health care costs, as well as Control of blood pressure and reduction of
on important social implications. Pakistan reveals an proteinuria are critical in preventing CKD
alarmingly high burden. Approximately 15 to 20 progression. The reduction of proteinuria using
percent of persons 40 years of age or older have a reninangiotensinaldosterone system (RAAS)
reduced estimated GFR. Evidence indicates that interruption slows progression of both diabetic and
chronic kidney disease develops is about a third of nondiabetic nephropathy. Lowering blood pressure
patients with diabetes. The burden of hypertension is also slows CKD progression, breaking a potentially
even higher affecting about one third of 45 years vicious cycle associating hypertension and CKD.
of age or older. Although the average Pakistani adult Evidence is insufficient to recommend combining an
visits a primary care physician four to five times each angiotensin-converting enzyme inhibitor with
year, 64 percent of adults have never had their blood angiotensin-receptor blockers to prevent CKD
pressure measured, and 70 percent of patients with progression. Although JNC 8 recommends a RAAS
hypertension and 50 percent of patients with diabetes blocker for all patients with chronic kidney disease,
are unaware of their condition. Compounding the Some chronic kidney disease patients can develop
problem of under detection are gaps in the knowledge hyperkalemia or a decreased estimated glomerular
of some Pakistani physicians about the management filtration rate after starting an ACE-I or an ARB.
of hypertension and diabetes, which lead to under Monitoring should include assessment of serum
treatment and a lack of preventive measures against potassium and estimated glomerular filtration rate
chronic kidney disease. Against this backdrop of poor approximately within several weeks after initiation or
medical practices, patients with kidney failure are dose escalation. When hyperkalemia develops,
faced with the high cost of renal-replacement outpatient management strategies include
therapy.[4] identification and restriction of dietary potassium,
Disease and management are classified according to treatment of metabolic acidosis if appropriate,
stages of disease severity, which are assessed from consideration of thiazide or loop diuretic use to
glomerular filtration rate (GFR) and albuminuria, and increase potassium excretion, and treatment with a
clinical diagnosis (cause and pathology). Chronic potassium-binding exchange resin. Discontinuation
kidney disease can be detected with routine of the RAAS blocker should be considered only if
laboratory tests, and some treatments can prevent these interventions fail.[7]
development and slow disease progression, reduce Vitamin D deficiency may also be associated with the
complications of decreased GFR and risk of progression of renal function in CKD. Vitamin D and
cardiovascular disease, and improve survival and derivatives have been widely used in the management
quality of life.[5] of CKD, for example, the control of
hyperparathyroidism. The different Vitamin D
www.iajps.com Page 3804
IAJPS 2017, 4 (11), 3803-3805 Mehvish Adil and Mariam Zaka ISSN 2349-7750
analogs have differential effects on physiological 6.Stein Hallan, Rene de Mutsert, Sven Carlsen,
function, which could be classified by the activity. Friedo W. Dekker, Knut Aasard, and Jostein
Nutritional Vitamin D25 can be supplemented by oral Holmen. Obesity, Smoking, and Physical Inactivity
intake of vitamin D rich or fortified diets is non as Risk Factors for CKD: Are Men More Vulnerable?
biological active form such as ergo calciferol, American Journal of Kidney Diseases, 2006; 47(3) :
cholecalciferol and traditionally the active forms, 396-405.
1,25(OH)2D, known as hormone are calcitriol and 7.Paul E. Stevens, Adeera Levi. Evaluation and
alfacalcidol. More recently, four Vitamin D analogs Management of Chronic Kidney Disease: Synopsis of
have been introduced in the nephrology area and play the Kidney Disease: Improving Global Outcomes
an increasingly important role in CKD treatment 2012 Clinical Practice Guideline Annals of Internal
which is doxercalciferol, paricalcitol, oxacalcitriol Medicine, 2013; 158(11):825-830.
and falecalcitriol. [8] 8.Nan Zhu, Jialin Wang, Lijie Gu, Ling Wang &
Better management of CKD can slow the progression Weijie Yuan. Vitamin D supplements in chronic
of CKD, prevent complications, and reduce kidney disease Renal Failure, 2015; 37(6): 917-924.
cardiovascular-related outcomes. Early referral to a 9.Laura C. Plantinga, ScM; L. Ebony Boulware,
nephrologist has been shown to improve outcomes Josef Coresh,Lesley A. Stevens, Edgar R. Miller III,
for those who progress to end-stage renal disease. [9] Rajiv Saran, Kassandra L. Messer, Andrew S.
Aerobic exercise in hemodialysis patients has been Levey, Neil R. Powe. Patient Awareness of Chronic
reported to enhance insulin sensitivity, improve lipid Kidney Disease Arch Intern Med. 2008; 168(20):
profile, increase hemoglobin, increase strength, 2268-2275.
decrease blood pressure, and improve quality of life. 10.Irfan Moinuddin, David J. Leehey. A Comparison
[10] of Aerobic Exercise and Resistance Training in
Patients With and Without Chronic Kidney Disease
CONCULSION: Advances in Chronic Kidney Disease, 2008;
This study revealed that that most commonly 15(1):83-96.
observed stage of chronic kidney disease was end
stage renal disease. Calcium channel blockers and
insulin was most commonly prescribed drugs for
hypertensive and diabetic patients with chronic
kidney disease. CKD leads to complications such as
anemia, bone disorders & hyperphosphatemia, to
manage these complications vitamin D supplements,
erythropoietin therapy & phosphate binders were
most commonly prescribed.
REFERENCES:
1.Chaitali S Bajait, Sonali A Pimpalkhute, Smita D
Sontakke, Kavita M Jaiswal, and Amruta V Dawri.
Prescribing pattern of medicines in chronic kidney
disease with emphasis on phosphate binders Indian
Journal of Pharmacology, 2014; 46(1):35-39.
2.Matthew T James, Brenda R Hemmelgarn, Dr
Marcello Tonelli. Early recognition and prevention of
chronic kidney disease The Lancet,2010;
375(972):12961309.
3.Arrigo Schieppati , Giuseppe Remuzzi. Chronic
renal diseases as a public health problem:
Epidemiology, social, and economic implications
Kidney International, 2005; 68( 98):7-10
4.Tazeen H. Jafar. The Growing Burden of Chronic
Kidney Disease in Pakistan The New England
Journal of Medicine, 2006; 354(10): 995.
5.Dr Andrew S Levey and Josef Coresh. Chronic
kidney disease The Lancet, 2012; 379(9811): 165-
180.
www.iajps.com Page 3805
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Assessment of Correlation Between Physical Activity and Academic Performance Among The Students of Gujranwala Medical College, GujranwalaDocument7 pagesAssessment of Correlation Between Physical Activity and Academic Performance Among The Students of Gujranwala Medical College, GujranwalaBaru Chandrasekhar RaoNo ratings yet
- Disorders of The Digestive SystemDocument108 pagesDisorders of The Digestive SystemNina Lao CamamaNo ratings yet
- Urinary Incontinence ModuleDocument103 pagesUrinary Incontinence Modulesny007No ratings yet
- Mod 7 PoisoningDocument12 pagesMod 7 Poisoningrez198767% (3)
- MaltingDocument28 pagesMaltingChristopher Garcia75% (4)
- Thyroid Function TestDocument11 pagesThyroid Function TestBookmyscansNo ratings yet
- The Role of Clinical Pharmacist in Pharmacovigilance and Drug Safety in Teritiary Care Teaching HospitalDocument11 pagesThe Role of Clinical Pharmacist in Pharmacovigilance and Drug Safety in Teritiary Care Teaching HospitalBaru Chandrasekhar RaoNo ratings yet
- Passive to Active Voice ConversionDocument3 pagesPassive to Active Voice ConversionQhaisya Binasanjaya67% (3)
- Development of Cell Culture System From Selected Tissues of Pangaius HypopthalmusDocument6 pagesDevelopment of Cell Culture System From Selected Tissues of Pangaius HypopthalmusBaru Chandrasekhar RaoNo ratings yet
- Development and Validation of Stability Indicating Assay Method For Estimation of Teriflunomide in Tablet Dosage FormDocument11 pagesDevelopment and Validation of Stability Indicating Assay Method For Estimation of Teriflunomide in Tablet Dosage FormBaru Chandrasekhar RaoNo ratings yet
- Genetic Enhancment of Groundnut (Arachis Hypogaea L.) Through Induced Muiation.Document5 pagesGenetic Enhancment of Groundnut (Arachis Hypogaea L.) Through Induced Muiation.Baru Chandrasekhar RaoNo ratings yet
- Formulation, Optimization and Evaluation Colon Targated Drug Delivery System For OrniadazoleDocument9 pagesFormulation, Optimization and Evaluation Colon Targated Drug Delivery System For OrniadazoleBaru Chandrasekhar RaoNo ratings yet
- Analytical Method Development and Validation of Stability Indicating RP-HPLC Method For Estimation of Lercanidipine Hydrochloride and Enalapril Maleate in CombinationDocument8 pagesAnalytical Method Development and Validation of Stability Indicating RP-HPLC Method For Estimation of Lercanidipine Hydrochloride and Enalapril Maleate in CombinationBaru Chandrasekhar RaoNo ratings yet
- Non-Adherence in Hyppertensive Patients of Peshawar, PakistanDocument13 pagesNon-Adherence in Hyppertensive Patients of Peshawar, PakistanBaru Chandrasekhar RaoNo ratings yet
- Gastroprotective Activity of Methanolic Extract of Phyllanthus Acidus Fruit Against Indomethacin-Induced Gastric Ulcers in RatsDocument7 pagesGastroprotective Activity of Methanolic Extract of Phyllanthus Acidus Fruit Against Indomethacin-Induced Gastric Ulcers in RatsBaru Chandrasekhar RaoNo ratings yet
- Knowledge On Antibiotics Use and Its Storage Among Saudi Arabia Residents: A Cross Sectional StudyDocument8 pagesKnowledge On Antibiotics Use and Its Storage Among Saudi Arabia Residents: A Cross Sectional StudyBaru Chandrasekhar RaoNo ratings yet
- The Bordering Areas (Nine Areas of Panjgur District) Issue of Pakistan About Human Malaria Prevalence: A Cross-Sectional Research of Malaria Parasites Identification in Blood SlidesDocument8 pagesThe Bordering Areas (Nine Areas of Panjgur District) Issue of Pakistan About Human Malaria Prevalence: A Cross-Sectional Research of Malaria Parasites Identification in Blood SlidesBaru Chandrasekhar RaoNo ratings yet
- Simultaneous Estimation of Rosuvastatin Calcium and Ezetimibe As Bulk Drug and in Tablet Dosage Form by RP-HPLC MethodDocument6 pagesSimultaneous Estimation of Rosuvastatin Calcium and Ezetimibe As Bulk Drug and in Tablet Dosage Form by RP-HPLC MethodBaru Chandrasekhar RaoNo ratings yet
- A Brief Review On YawsDocument7 pagesA Brief Review On YawsBaru Chandrasekhar RaoNo ratings yet
- Preparation of Silver Nanoparticles From Herbal PlantDocument9 pagesPreparation of Silver Nanoparticles From Herbal PlantBaru Chandrasekhar RaoNo ratings yet
- Nephroprotective Activityof Acorus Calamus Leaves Extract Against Lithium Induced Nephrotoxicity in Wistar RatsDocument12 pagesNephroprotective Activityof Acorus Calamus Leaves Extract Against Lithium Induced Nephrotoxicity in Wistar RatsBaru Chandrasekhar RaoNo ratings yet
- Relationship of Testosterone With Body Mass Index in Infertile Males in Local CommunityDocument4 pagesRelationship of Testosterone With Body Mass Index in Infertile Males in Local CommunityBaru Chandrasekhar RaoNo ratings yet
- Role of Simvastatin in Addition To Metformin in Polycystic Ovarian Syndrome Patients, A Randomized Controlled Trial On Pakistani WomenDocument4 pagesRole of Simvastatin in Addition To Metformin in Polycystic Ovarian Syndrome Patients, A Randomized Controlled Trial On Pakistani WomenBaru Chandrasekhar RaoNo ratings yet
- An Incidence of Hypertension Among People and Its Association To Consumption of Hard Water: A Cross-Sectional ResearchDocument6 pagesAn Incidence of Hypertension Among People and Its Association To Consumption of Hard Water: A Cross-Sectional ResearchBaru Chandrasekhar RaoNo ratings yet
- An Epidemiological Survey About The Infections Caused by Dengue in The Perspective of Hematological, Clinical and Demographic Risk FactorsDocument6 pagesAn Epidemiological Survey About The Infections Caused by Dengue in The Perspective of Hematological, Clinical and Demographic Risk FactorsBaru Chandrasekhar RaoNo ratings yet
- Review On: Inventory ManagementDocument8 pagesReview On: Inventory ManagementBaru Chandrasekhar RaoNo ratings yet
- Association of Socioeconomic Status, Hypertension and Treatment Modality With Diabetic Amputation - A Case Control StudyDocument4 pagesAssociation of Socioeconomic Status, Hypertension and Treatment Modality With Diabetic Amputation - A Case Control StudyBaru Chandrasekhar RaoNo ratings yet
- Pharmaceutical Sciences: IAJPS 2018, 05 (04), 3075-3081 Aneeqa Ali RaoDocument7 pagesPharmaceutical Sciences: IAJPS 2018, 05 (04), 3075-3081 Aneeqa Ali RaoBaru Chandrasekhar RaoNo ratings yet
- Study of Clinical Profile of Transfused Thalassemic Childrens With Special Reference To Hepatitis B Profile and Liver Function.Document6 pagesStudy of Clinical Profile of Transfused Thalassemic Childrens With Special Reference To Hepatitis B Profile and Liver Function.Baru Chandrasekhar RaoNo ratings yet
- After Acute Myocardial Infarction End Result of Cardiogenic Shock in Hospitalized PatientsDocument4 pagesAfter Acute Myocardial Infarction End Result of Cardiogenic Shock in Hospitalized PatientsBaru Chandrasekhar RaoNo ratings yet
- Descriptive Study Knowing The Patients Load in The Neonatal Icu at The Tertiary Care Hospital LahoreDocument4 pagesDescriptive Study Knowing The Patients Load in The Neonatal Icu at The Tertiary Care Hospital LahoreBaru Chandrasekhar RaoNo ratings yet
- C-Reactive Protein Levels Preoperatively and Postoperatively Effect On Cardiovascular Surgery ComplicationsDocument5 pagesC-Reactive Protein Levels Preoperatively and Postoperatively Effect On Cardiovascular Surgery ComplicationsBaru Chandrasekhar RaoNo ratings yet
- An Exploratory Review of The Myths and Common Beliefs About Acne and Its TreatmentDocument6 pagesAn Exploratory Review of The Myths and Common Beliefs About Acne and Its TreatmentBaru Chandrasekhar RaoNo ratings yet
- Isolation and Identification of Clostridium Perfringens Causing Enterotoxaemia in Bovine of Kacchi District Balochistan.Document8 pagesIsolation and Identification of Clostridium Perfringens Causing Enterotoxaemia in Bovine of Kacchi District Balochistan.Baru Chandrasekhar RaoNo ratings yet
- Oppertunistic Hypertension Screening in Rural Health Population of Umar Abad Tehsil Kharezat Disrtrict Pishin Balochistan. A Cross Sectional StudyDocument10 pagesOppertunistic Hypertension Screening in Rural Health Population of Umar Abad Tehsil Kharezat Disrtrict Pishin Balochistan. A Cross Sectional StudyBaru Chandrasekhar RaoNo ratings yet
- A Cross Sectional Survey Information About Weaning Process Among Mothers of Infants Above 6 Months of Age in Opd Pediatrics at Kishwer Fazal Teaching Hospital LahoreDocument8 pagesA Cross Sectional Survey Information About Weaning Process Among Mothers of Infants Above 6 Months of Age in Opd Pediatrics at Kishwer Fazal Teaching Hospital LahoreBaru Chandrasekhar RaoNo ratings yet
- Muscular TissuesDocument46 pagesMuscular TissuesDAVE CANALETANo ratings yet
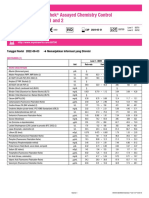
- Lyphochek Assayed Chemistry Control Levels 1 and 2: Tanggal Revisi 2022-06-03 Menunjukkan Informasi Yang DirevisiDocument2 pagesLyphochek Assayed Chemistry Control Levels 1 and 2: Tanggal Revisi 2022-06-03 Menunjukkan Informasi Yang DirevisiFahmiNo ratings yet
- Lecture 11 Nursing Care of A Family During Labor and Birth 2021Document105 pagesLecture 11 Nursing Care of A Family During Labor and Birth 2021مؤمن شطناويNo ratings yet
- Soebandiri Dept of Medicine, Division of Hematology Airlangga University School of Medicine SurabayaDocument17 pagesSoebandiri Dept of Medicine, Division of Hematology Airlangga University School of Medicine SurabayaniluhayusumbawatiNo ratings yet
- The Fundamental Unit of Life: CBSE Class 9th NCERT Solution: ScienceDocument7 pagesThe Fundamental Unit of Life: CBSE Class 9th NCERT Solution: ScienceShyamlal BairwaNo ratings yet
- L16 Animal Diversity 2Document29 pagesL16 Animal Diversity 2shadoworacleNo ratings yet
- Underground Clinical Vignettes BiochemistryDocument128 pagesUnderground Clinical Vignettes Biochemistrymartha2112No ratings yet
- jm800328v PDFDocument9 pagesjm800328v PDFVINODNo ratings yet
- Cambridge International General Certificate of Secondary EducationDocument16 pagesCambridge International General Certificate of Secondary EducationJeet JeetNo ratings yet
- Artigo RolfingDocument8 pagesArtigo RolfingIsis CalioNo ratings yet
- Identifying Amino AcidsDocument8 pagesIdentifying Amino AcidsWahyuniAntariNo ratings yet
- Passion and Deceit Part VI PDFDocument20 pagesPassion and Deceit Part VI PDFno2meNo ratings yet
- Biology Revision Essay Questions and Answers For Secondary Kusoma - Co - .KeDocument48 pagesBiology Revision Essay Questions and Answers For Secondary Kusoma - Co - .Kestevewanji0% (1)
- 9700 w01 Ms 2Document4 pages9700 w01 Ms 2Sathya Seelan0% (1)
- Anatomy of The Left EyeDocument3 pagesAnatomy of The Left EyeJaessa FelicianoNo ratings yet
- Obstructive LunDocument10 pagesObstructive Lunabenezer isayasNo ratings yet
- Blood Sugar Reg-WPS OfficeDocument8 pagesBlood Sugar Reg-WPS Officetanjidul islamNo ratings yet
- Jcpe 12206 PDFDocument17 pagesJcpe 12206 PDFrozh rasulNo ratings yet
- Guillain BarreDocument6 pagesGuillain BarreValentín PalmNo ratings yet
- An evidence-based approach to undifferentiated shockDocument1 pageAn evidence-based approach to undifferentiated shockHely ICNo ratings yet
- Pinoy Jokes!: Pupils!Document4 pagesPinoy Jokes!: Pupils!joserizal666No ratings yet
- Nursing JournalDocument10 pagesNursing JournalRenee Dwi Permata MessakaraengNo ratings yet
- Approach To The Infant or Child With Nausea and Vomiting - UpToDateDocument47 pagesApproach To The Infant or Child With Nausea and Vomiting - UpToDatemayteveronica1000No ratings yet
- Embriologi Alat Kelamin (Deferensiasi SexDocument19 pagesEmbriologi Alat Kelamin (Deferensiasi SexAdi Putra GhifariNo ratings yet