Professional Documents
Culture Documents
Surgical Safety Cheklist
Uploaded by
Edy Tahir MattoreangCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Surgical Safety Cheklist
Uploaded by
Edy Tahir MattoreangCopyright:
Available Formats
Systematic review
Systematic review and meta-analysis of the effect of the World
Health Organization surgical safety checklist on postoperative
complications
J. Bergs1 , J. Hellings2 , I. Cleemput1 , Ö. Zurel1 , V. De Troyer3 , M. Van Hiel5 , J.-L. Demeere4 ,
D. Claeys6 and D. Vandijck1,7
1
Department of Patient Safety and Health Economics, Faculty of Business Economics, and 2 Patient Safety Group, Faculty of Medicine and Life Sciences,
Hasselt University, Hasselt, 3 ICURO and 4 Department of Anaesthesiology, Kliniek St Jan, Brussels, 5 Operating Theatre, Imelda Hospital, Bonheiden,
and 6 Department of Surgery, AZ Maria Middelares, and 7 Department of Public Health and Health Economics, Faculty of Medicine and Health Sciences,
Ghent University, Ghent, Belgium
Correspondence to: Mr J. Bergs, Department of Patient Safety and Health Economics, Faculty of Business Economics, Hasselt University, Martelarenlaan
42, 3500 Hasselt, Belgium (e-mail: jochen.bergs@uhasselt.be)
Background: The World Health Organization (WHO) surgical safety checklist (SSC) was introduced to
improve the safety of surgical procedures. This systematic review evaluated current evidence regarding
the effectiveness of this checklist in reducing postoperative complications.
Methods: The Cochrane Library, MEDLINE, Embase and CINAHL were searched using predefined
inclusion criteria. The systematic review included all original articles reporting a quantitative measure of
the effect of the WHO SSC on postoperative complications. Data were extracted for postoperative compli-
cations reported in at least two studies. A meta-analysis was conducted to quantify the effect of the WHO
SSC on any complication, surgical-site infection (SSI) and mortality. Yule’s Q contingency coefficient
was used as a measure of the association between effectiveness and adherence with the checklist.
Results: Seven of 723 studies identified met the inclusion criteria. There was marked methodological
heterogeneity among studies. The impact on six clinical outcomes was reported in at least two studies. A
meta-analysis was performed for three main outcomes (any complication, mortality and SSI). Risk ratios
for any complication, mortality and SSI were 0·59 (95 per cent confidence interval 0·47 to 0·74), 0·77
(0·60 to 0·98) and 0·57 (0·41 to 0·79) respectively. There was a strong correlation between a significant
decrease in postoperative complications and adherence to aspects of care embedded in the checklist
(Q = 0·82; P = 0·042).
Conclusion: The evidence is highly suggestive of a reduction in postoperative complications and
mortality following implementation of the WHO SSC, but cannot be regarded as definitive in the
absence of higher-quality studies.
Paper accepted 23 October 2013
Published online in Wiley Online Library (www.bjs.co.uk). DOI: 10.1002/bjs.9381
Introduction Organization (WHO) patient safety programme, similar
to those used in aviation, aeronautics and product
Hospitals are not as safe as generally believed1 . Overall, manufacturing. The surgical safety checklist (SSC) consists
the incidence of in-hospital adverse events is about 10 of 19 items and is used at three critical perioperative
per cent, of which three-quarters are related to surgery. At moments: induction, incision and before the patient
least half of these adverse events are considered preventable leaves the operating theatre. The items contain an oral
within the current standards of care2 – 4 . The rate of patients confirmation by the surgical team of the completion of
experiencing an adverse event is even expected to increase some key steps for ensuring safe delivery of anaesthesia,
over time5 . The incidence of surgery-related adverse events antibiotic prophylaxis, effective teamwork and other
combined with the increasing volume of surgery6 results essential practices in surgery7 .
in an important healthcare problem. Previous studies8,9 suggested that implementation
With the aim of improving patient safety following compliance was low, despite checklist awareness by the
surgery, a checklist was developed by the World Health theatre team. The knowledge that checklists are executed
2014 BJS Society Ltd BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
Effect of World Health Organization surgical safety checklist on postoperative complications 151
incompletely makes the evaluation of a team’s compliance full-text review were screened according to the inclusion
with the checklist as important as evaluating clinical and exclusion criteria. Two independent reviewers carried
outcomes9,10 . However, to date, only one single-centre out data extraction and critical assessment of included
study11 has examined the extent to which the WHO SSC studies, with disagreements settled by a third reviewer.
effectiveness is related to checklist adherence. Study setting, design, selection and measurement bias,
The aim of this review was to assess the effectiveness baseline outcome measurements and characteristics, risk of
of the WHO SSC. The first objective was to assess contamination, data analysis, selective outcome reporting,
the effect of the checklist on postoperative complications other risks of bias, and issues relating to generalizability
and mortality following implementation; the second was and sustainability were extracted and recorded. Assessment
to assess the relationship between clinical outcome and for risk of bias and critical appraisal was conducted
adherence with the WHO SSC. using the Cochrane Collaboration’s Effective Practice and
Organisation of Care Group guidelines12 .
Methods
Data sources Data synthesis and analysis
The Cochrane Library, MEDLINE, Embase and Cumu- Data were analysed using R (a language and environment
lative Index to Nursing and Allied Health Literature for statistical computing)13 . All reported P values are
(CINAHL) databases were searched systematically for all two-sided; P < 0·050 was considered to indicate statistical
publications until February 2013. The following medi- significance.
cal subject heading (MeSH) search terms and keywords Postoperative complications discussed in at least two
were used, either individually or in combination: ‘Postop- studies were included in the narrative synthesis. Meta-
erative complications’[MeSH], ‘Checklist’[MeSH], ‘Post- analysis was performed for three main patient outcome
operative complications, prevention and control’[MeSH]. measures: occurrence of any postoperative complication,
The MEDLINE search strategy (Appendix S1, sup- surgical-site infection (SSI) and death. If a study provided
porting information) was adjusted to the dictionary of data for more than one site, data from the individual sites
the other databases as appropriate. This was accompa- were used in order to overcome the effect of aggregated
nied by a checklist-specific query using the following data reporting as well as to limit in-study heterogeneity.
keywords: ‘Safety Management’[MeSH], ‘Risk Manage- Risk ratios (RRs) with 95 per cent confidence intervals (c.i.)
ment’[MeSH], ‘Checklist’[MeSH]. In addition, biblio- were calculated as summary estimates of the effects using
graphies of included articles were hand searched for other a random-effects model, as proposed by DerSimonian and
relevant articles. During the preparation of the manuscript, Laird14 . Heterogeneity of the study results was assessed
the MEDLINE strategy was consulted weekly in order to using the Cochran Q test and the Higgins I 2 test. P < 0·100
identify potentially new relevant publications. Grey litera- in Cochran’s Q test and an I 2 value exceeding 50 per cent
ture was not considered. were considered to show significant heterogeneity.
Yule’s Q contingency coefficient was used as a measure
Study selection of association between effectiveness and adherence. Yule’s
Only English-language studies were included. Poten- Q is a transformation of the odds ratio (OR) designed to
tially included study designs were: randomized clini- vary, not from 0 to infinity with 1 indicating no effect,
cal trials, non-randomized controlled trials, controlled but from −1 to +1 with 0 indicating no effect, as the
before–after studies, interrupted time series (ITS) and Pearson correlation. Conceptually, this is the number of
repeated-measures studies. Only studies with a quantitative pairs in agreement (ad) minus the number in disagreement
evaluation regarding the impact of the WHO SSC on post- (bc) divided by the total number of paired observations15 .
operative complications, including postoperative mortality, Effectiveness of the WHO SSC was represented using a
were included. Studies were excluded if they addressed binary variable indicating the occurrence of a significant
only a particular issue or complication, such as those solely RR for any complication.
focusing on the effectiveness of surgical-site marking. All authors reviewed the measures of adherence
individually and determined whether adequate adherence
to the SSC could be expected. Adequate adherence
Data extraction
was defined as adherence to the provided measures for
After removal of duplicates, a first selection of references at least 90 per cent of all patients. Following these
was made based on title and abstract. Papers selected for individual assessments, a consensus meeting was held at
2014 BJS Society Ltd www.bjs.co.uk BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
152 J. Bergs, J. Hellings, I. Cleemput, Ö. Zurel, V. De Troyer, M. Van Hiel et al.
each site, at which consensus was sought in cases of asked to implement the WHO SSC. The checklist was
disagreement. Throughout this procedure the authors were introduced to the operating theatres over a 1-week to 1-
blinded to outcome data and study references. Agreement month interval. To facilitate implementation, the checklist
between the authors regarding their interpretation of was translated to the local language and adjusted to fit
checklist adherence was assessed using Fleiss’ κ. The into the care process at each institution. A local dedicated
resulting decision was expressed as a binary variable study team guided the introduction of the checklist to
representing presence or absence of adequate adherence to the staff. Effectiveness was measured as the reduction
the WHO SSC. in any major complication, including death, during the
postoperative hospital stay (up to 30 days) or until hospital
discharge. Weiser and co-workers19 conducted a reanalysis
Results
of a subsample of adult patients undergoing urgent, non-
In total, 723 potentially relevant articles were retained. cardiac surgery. The subsample was drawn from the data
After critical assessment of title and abstract, nine papers used by Haynes and colleagues18 .
were selected for full-text evaluation of which two16,17 were Sewell et al.20 evaluated the use of the WHO SSC before
excluded because they did not meet the inclusion criteria. and after implementation of an educational programme
Finally, seven11,18 – 23 papers were considered for further in one hospital in the UK20 . This study, with an ITS
analysis. One study19 was excluded from meta-analysis as design, considered trauma and orthopaedic surgery. The
it was a reanalysis of a subcohort of patients undergoing programme, which was designed to improve checklist use,
non-elective surgery already reported in another study consisted of the following measures: SSC forms were
(Fig. 1). placed in the operating theatre so staff members could
become more familiar with their use; a compulsory training
video was produced, detailing the correct way to fulfil
Included studies
the checklist; and educational sessions were delivered,
Haynes and colleagues18 assessed the effectiveness of the discussing the main causes of adverse events associated
WHO SSC at eight hospitals worldwide. This study, with with surgery, and explaining how to use the checklist
an ITS design, included patients aged 16 years or older appropriately. Effectiveness was measured as the reduction
undergoing non-cardiac surgery. After a first exploratory in any major complication, including death, during the
baseline measurement, each institution received feedback postoperative hospital stay, up to 30 days or until hospital
about areas of deficiencies identified and was subsequently discharge.
Records identified through initial Additional records identified through
database searching other sources
n = 555 n = 168
Records after duplicates removed
n = 440
Records screened
n = 440
Records excluded
n = 431
Full-text articles assessed for eligibility
n=9
Full-text articles excluded
n=2
Studies included in narrative data synthesis
n=7
Studies included in meta-analysis
n=6
Fig. 1 PRISMA diagram showing selection of articles for review
2014 BJS Society Ltd www.bjs.co.uk BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
Effect of World Health Organization surgical safety checklist on postoperative complications 153
Askarian and colleagues21 evaluated the effect of the Kwok and colleagues23 evaluated the effectiveness of
WHO SSC on postoperative morbidity and mortality rates the WHO SSC at a public, university-affiliated general
in a tertiary-care hospital in Iran. This study, with an and trauma hospital in Chisinau, Moldova, using an
ITS design, included patients aged at least 16 years under- ITS design. The intervention comprised a hospital-wide
going elective general surgery. End-stage and immuno- implementation of the WHO SSC. A local implementation
compromised patients were excluded. Baseline assessment team was created consisting of hospital administrators and
was carried out during the first 3 months of the study; representatives from the surgical, anaesthesia and nursing
postoperative complications were recorded in four hos- departments. The implementation team was trained during
pital wards until hospital discharge. The checklist was four weekly 30–60-min video conferences, using checklist
introduced during meetings, and an educational package, and oximetry training materials developed by the WHO,
containing the checklist and accompanying guidelines, Harvard School of Public Health, the World Federation
was provided to operating theatre personnel. Effective- of Societies of Anaesthesiologists, and the Association of
ness was measured as the reduction in postoperative Anaesthetists of Great Britain and Ireland. These materials
complications. included presentations, manuals, clinical scenarios and
van Klei and co-workers11 evaluated the effect of an videos. Thirty-day complication data were collected as
adapted version of the WHO SSC on in-hospital mortality, defined by the American College of Surgeons National
together with the impact of checklist compliance on Surgical Quality Improvement Program.
outcome, in a tertiary hospital in the Netherlands. This
retrospective cohort study included all adult patients who
Risk of bias of included studies
underwent a surgical procedure. Modifications of the
WHO SSC were made to enhance local applicability, All studies were prone to confounding and bias owing
resulting in a 22-item checklist. The entire surgical and to methodological decisions. All papers reported the
anaesthesia team briefly reviewed each surgical patient, results of non-randomized studies, resulting in potential
replacing the sign-in part of the WHO SSC. To ensure bias. As methodological information was difficult to find,
that checklist items were also available to caregivers before many questions concerning bias and confounding were
a patient entered and left the operating theatre, structured unanswered. The following potential sources of bias and
handovers were implemented from the ward to the theatre confounding could be generalized. A first source concerns
holding area as well as from the theatre to the recovery compliance with checklist use. Six studies18 – 23 reported
room. Implementation information was provided both a measure of a subgroup of safety indicators that reflect
at regular meetings and during extra meetings with the compliance with the checklist, with a range between 0
entire staff (surgeons, anaesthetists and nurses), where the and 97·3 per cent. All studies demonstrated variability
importance of the checklist was emphasized. In addition, in compliance between checklist items. This incomplete
the checklist was made available in poster format in every implementation makes it difficult to attribute the measured
operating theatre and electronically in the scheduling effect to the WHO SSC alone. A second source of bias is the
system. Effectiveness was measured as any reduction in implementation strategy used in the studies. Various, often
in-hospital mortality within 30 days of surgery. unclear, implementation approaches were used, possibly
Bliss et al.22 evaluated the effects of the Association of resulting in different levels of compliance with the WHO
Perioperative Registered Nurses Comprehensive Surgical SSC. Third, in some studies direct observation was used to
Checklist at a 600-bed tertiary-care facility and major evaluate compliance, potentially leading to a Hawthorne
teaching hospital in the USA. This checklist incorporates effect.
mandated clinical practice required by the WHO, the Joint
Commission, and the Centers for Medicare and Medicaid
Effects of checklist use on postoperative
Services. This study used an ITS design with historical
complications
controls, and included all patients aged 18 years or older
undergoing high-risk surgical procedures. Implementation Any complication
of the checklist involved a three-session team-based Six studies18 – 23 reported data on any complication within
training programme. Surgical services staff were oriented 30 days following surgery or until hospital discharge
to the use of the checklist, and barriers to checklist use (Table 1). Five studies found decreasing complication rates:
were discussed at the training session. Effectiveness was 11·0 versus 7·0 per cent (P < 0·001)18 , 18·4 versus 11·7
evaluated as any reduction in 30-day mortality and/or per cent (P = 0·001)19 , 22·9 versus 10·0 per cent
postoperative complications. (P = 0·03)21 , 23·6 versus 8 per cent (P < 0·001)22 and 21·5
2014 BJS Society Ltd www.bjs.co.uk BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
154 J. Bergs, J. Hellings, I. Cleemput, Ö. Zurel, V. De Troyer, M. Van Hiel et al.
Table 1 Summary of major clinical outcomes before and after checklist implementation
Any complication (%) Mortality (%) Surgical-site infection (%)
Before After P Before After P Before After P
Haynes et al.18 11·0 7·0 < 0·001 1·5 0·8 0·003 6·2 3·4 < 0·001
Site 1 11·6 7·0 < 0·050 1·0 0 < 0·050 4·0 2·0 < 0·050
Site 2 7·8 6·3 > 0·050 1·1 0·3 > 0·050 2·0 1·7 > 0·050
Site 3 13·5 9·7 > 0·050 0·8 1·4 > 0·050 5·8 4·3 > 0·050
Site 4 7·5 5·5 > 0·050 1·0 0·6 > 0·050 3·1 2·6 > 0·050
Site 5 21·4 5·5 < 0·050 1·4 0·0 < 0·050 20·5 3·6 < 0·050
Site 6 10·1 9·7 > 0·050 3·6 1·7 > 0·050 4·0 4·0 > 0·050
Site 7 12·4 8·0 < 0·050 2·1 1·7 > 0·050 9·5 5·8 > 0·050
Site 8 6·1 3·6 > 0·050 1·4 0·3 > 0·050 4·1 2·4 > 0·050
Weiser et al.19 18·4 11·7 0·001 3·7 1·4 0·007 11·2 6·6 < 0·001
Sewell et al.20 8·5 7·6 RR 0·89 (0·58,1·37) 1·9 1·6 RR 0·88 (0·34, 2·26) 4·4 3·5 n.a.
Askarian et al.21 22·9 10·0 0·03 n.a. n.a. n.a. 10·4 5·3 0·1
van Klei et al.11 n.a. n.a. n.a. 3·1 2·9 OR 0·91 (0·78, 1·05) n.a. n.a. n.a.
Bliss et al.22 23·6 8 < 0·001 n.a. n.a. n.a. 6·2 5 0·845
Kwok et al.23 21·5 8·8 < 0·001 4·0 3·1 0·151 14·9 4·7 < 0·001
Values in parentheses are 95 per cent confidence intervals. RR, risk ratio; n.a., not available; OR, odds ratio.
Any complication
Reference After implementation Baseline Risk ratio Risk ratio Weight (%)
18
Haynes et al.
Site 1 42 of 598 61 of 524 0·60 (0·41, 0·88) 9·2
Site 2 22 of 351 28 of 357 0·80 (0·47, 1·37) 7·3
Site 3 47 of 486 67 of 497 0·72 (0·50, 1·02) 9·5
Site 4 30 of 545 39 of 520 0·73 (0·46, 1·16) 8·2
Site 5 18 of 330 79 of 370 0·26 (0·16, 0·42) 7·9
Site 6 46 of 476 50 of 496 0·96 (0·66, 1·40) 9·1
Site 7 47 of 585 65 of 525 0·65 (0·45, 0·93) 9·4
Site 8 21 of 584 27 of 444 0·59 (0·34, 1·03) 7·1
20
Sewell et al. 37 of 485 41 of 480 0·89 (0·58, 1·37) 8·6
Askarian et al.21 15 of 150 33 of 144 0·44 (0·25, 0·77) 7·0
Bliss et al.22 6 of 73 491 of 2079 0·35 (0·16, 0·75) 5·2
Kwok et al.23 185 of 2106 428 of 1993 0·41 (0·35, 0·48) 11·5
Random-effects model 6769 8429 0·59 (0·47, 0·74) 100
Heterogeneity: I2 = 75%, t2 = 0·115, P < 0·001
0·2 0·5 1 2 5
Forest plot showing the effectiveness of the World Health Organization surgical safety checklist in reducing any complication.
Fig. 2
A random-effects model was used for meta-analysis. Risk ratios are shown with 95 per cent confidence intervals
versus 8·8 per cent (P < 0·001)23 . One study20 did not Mortality rates
demonstrate a significant difference between evaluation Thirty-day mortality was reported in five studies11,18 – 20,23
intervals (8·5 versus 7·6 per cent; RR 0·89, 95 per cent c.i. (Table 1). A significant effect on mortality following SSC
0·58 to 1·37). Meta-analysis for any complication across implementation was found in two: 1·5 versus 0·8 per cent
five studies yielded a RR of 0·59 (95 per cent c.i. 0·47 (P = 0·003)18 and 3·7 versus 1·4 per cent (P = 0·007)19 .
to 0·74; P < 0·001). There was significant heterogeneity van Klei and colleagues11 reported a decrease in crude
(Cochran’s Q = 44·07, 11 d.f., P < 0·001; I 2 = 75 (95 per mortality rates from 3·1 to 2·9 per cent, but this was
cent c.i. 56 to 86) per cent) (Fig. 2). not statistically significant (P = 0·19). After adjustment
2014 BJS Society Ltd www.bjs.co.uk BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
Effect of World Health Organization surgical safety checklist on postoperative complications 155
Mortality
Reference After implementation Baseline Risk ratio Risk ratio Weight (%)
Haynes et al.18
Site 1 0 of 598 5 of 524 0·08 (0·00, 1·44) 0·7
Site 2 1 of 351 4 of 357 0·25 (0·03, 2·26) 1·2
Site 3 7 of 486 4 of 497 1·79 (0·53, 6·07) 3·7
Site 4 3 of 545 5 of 520 0·57 (0·14, 2·38) 2·7
Site 5 0 of 330 5 of 370 0·10 (0·01, 1·84) 0·7
Site 6 8 of 476 18 of 496 0·46 (0·20, 1·05) 7·4
Site 7 10 of 585 11 of 525 0·82 (0·35, 1·91) 7·0
Site 8 2 of 584 6 of 444 0·25 (0·05, 1·25) 2·2
Sewell et al.20 8 of 485 9 of 480 0·88 (0·34, 2·26) 5·8
van Klei et al.11 318 of 11 151 450 of 14 362 0·91 (0·79, 1·05) 42·0
23
Kwok et al. 65 of 2106 80 of 1993 0·77 (0·56, 1·06) 26·4
Random-effects model 17 697 20 568 0·77 (0·60, 0·98) 100
Heterogeneity: I2 = 24%, t2 = 0·031, P = 0·216
0·01 0·1 1 10 100
Forest plot showing the effectiveness of the World Health Organization surgical safety checklist in reducing mortality. A
Fig. 3
random-effects model was used for meta-analysis. Risk ratios are shown with 95 per cent confidence intervals
for baseline differences, mortality decreased significantly Blood loss
after checklist implementation (OR 0·85; 95 per cent c.i. Two studies19,22 reported on blood loss. In the article by
0·73 to 0·98). This effect was strongly related to checklist Weiser and colleagues19 , the proportion of patients with
compliance; the OR was 0·44 (0·28 to 0·70) if the checklist estimated blood loss greater than 500 ml declined from
was completed fully, compared with 1·09 (0·78 to 1·52) 20·3 to 13·3 per cent (P < 0·001). Bliss et al.22 , however, did
and 1·16 (0·86 to 1·56) for partial and non-compliance not demonstrate a significant difference in the percentage
respectively11 . Two studies20,23 did not demonstrate a that required transfusion for bleeding (6·1 to 5·5 per cent;
significant reduction in mortality. Meta-analysis for crude P = 0·392)22 .
mortality revealed that across four studies the RR for
mortality with the use of the WHO SSC was 0·77
Unplanned return to operating theatre
(0·60 to 0·98; P = 0·035), without significant heterogeneity
Three studies18,20,23 reported details on unplanned return
(Cochran’s Q = 13·15, 10 d.f., P = 0·216; I 2 = 24 (0 to 62)
to the operating theatre. In the Haynes study18 the
per cent) (Fig. 3).
unplanned return rate dropped from 2·4 to 1·8 per cent
Surgical-site infections (P = 0·047)18 . Sewell and colleagues20 reported unplanned
return to the operating theatre after 1 per cent of
SSIs were reported in six studies (Table 1)18 – 23 . Three
procedures in both audits. Kwok and co-workers23 reported
reported a significant decrease in SSI rates follow-
that the unplanned return rate decreased from 1·9 to 1·5
ing SSC implementation: from 6·2 to 3·4 per cent
per cent (P = 0·151).
(P < 0·001)18 , 11·2 to 6·6 per cent (P < 0·001)19 and
14·9 to 4·7 per cent (P < 0·001)23 . The other studies did
not demonstrate a significant change in SSI rate after Pneumonia
implementation of the WHO SSC: 4·4 versus 3·5 per Pneumonia or lower respiratory tract infections were
cent20 , 10·4 versus 5·3 per cent (P = 0·1)21 and 6·2 versus 5 reported in five studies18,20 – 23 . One23 reported a sig-
per cent (P = 0·845)22 . Meta-analysis revealed that across nificant decrease in pneumonia rates, from 4·7 to 2·6
five studies the RR for SSI with the use of the WHO SSC per cent (P < 0·001). The others all reported a non-
was 0·57 (95 per cent c.i. 0·41 to 0·79; P < 0·001). There significant difference: 1·1 versus 1·3 per cent (P = 0·46)18 ,
was significant heterogeneity (Cochran’s Q = 41·74, 11 2·1 versus 2·5 per cent20 , 7·6 versus 3·3 per cent (P = 0·1)21
d.f., P < 0·001; I 2 = 74 (53 to 85) per cent) (Fig. 4). and 2·4 versus 0 per cent (P = 0·362)22 .
2014 BJS Society Ltd www.bjs.co.uk BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
156 J. Bergs, J. Hellings, I. Cleemput, Ö. Zurel, V. De Troyer, M. Van Hiel et al.
Surgical-site infection
Reference After implementation Baseline Risk ratio Risk ratio Weight (%)
Haynes et al.18
Site 1 12 of 598 21 of 524 0·50 (0·25, 1·01) 8·0
Site 2 6 of 351 7 of 357 0·87 (0·30, 2·57) 5·3
Site 3 21 of 486 29 of 497 0·74 (0·43, 1·28) 9·3
Site 4 14 of 545 16 of 520 0.83 (0·41, 1·69) 7·9
Site 5 12 of 330 76 of 370 0·18 (0·10, 0·32) 8·9
Site 6 19 of 476 20 of 496 0·99 (0·54, 1·83) 8·7
Site 7 34 of 585 50 of 525 0·61 (0·40, 0·93) 10·4
Site 8 14 of 584 18 of 444 0·59 (0·30, 1·18) 8·1
Sewell et al.20 17 of 485 21 of 480 0·80 (0·43, 1·50) 8·6
21
Askarian et al. 8 of 150 15 of 144 0·51 (0·22, 1·17) 7·0
Bliss et al.22 4 of 73 129 of 2079 0·88 (0·34, 2·32) 6·0
Kwok et al.23 99 of 2106 297 of 1993 0·32 (0·25, 0·39) 11·9
Random-effects model 6769 8429 0·57 (0·41, 0·79) 100
Heterogeneity: I2 = 74%, t2 = 0·219, P < 0·001
0·1 0·5 1 2 10
Fig. 4Forest plot showing the effectiveness of the World Health Organization surgical safety checklist in reducing surgical-site
infection. A random-effects model was used for meta-analysis. Risk ratios are shown with 95 per cent confidence intervals
Relationship between checklist compliance c.i. 0·47 to 0·74), mortality (RR 0·77, 0·60 to 0·98) and SSI
and effectiveness (RR 0·57, 0·41 to 0·79). The present study also suggested
that sites with adequate compliance with aspects of care
Six studies measured adherence with the SSC. Five18 – 22
embedded in the checklist were more likely to demonstrate
reported adherence to a subgroup of six safety measures
a significant reduction in postoperative complications.
as an indicator of checklist adherence. One study23
Pooled analysis showed significant improvements in
used a subset of five safety measures as an indicator of
postoperative complications following implementation of
checklist adherence (for details see Table S1, supporting
the WHO SSC. Yet, there was variability in effect sizes
information).
among the studies. The variation becomes even more
A significant RR, favouring use of the WHO SSC,
evident when the Haynes study18 is analysed at site level
was found in six of the 12 sites (Fig. 2). Within this
(Table 1). Even when a uniform implementation method
group, four reported adequate adherence with the safety
is used (as assumed in the Haynes study), variation in
measures. Of the five sites with adequate adherence,
adherence and outcome is observed. It is likely that the
four demonstrated a significant reduction in postoperative
implementation method has an impact, but it is not the
complications. In contrast, two of seven sites reporting only determinant. Haynes and colleagues17 showed that
inadequate adherence demonstrated a significant reduction improvements in postoperative outcomes were associated
in postoperative complications. These results suggest a with improved perception of teamwork and safety climate
correlation between a significant decrease in postoperative among respondents, suggesting that changes in these
complications and adequate adherence to the reported aspects may be partially responsible for the effect of the
safety measures (Q = 0·82, P = 0·042). checklist.
This study highlights that evaluation of a team’s
Discussion compliance with the checklist, which is measured by
adherence, is as important as evaluating outcomes9,10 .
The results of this meta-analysis suggest that the Hospital administrators, implementation leaders and
WHO SSC reduces postoperative complications, including researchers need to measure and report compliance with
mortality. Meta-analysis demonstrated a significant effect the checklist in association with clinical outcomes. There is
of the checklist on any complication (RR 0·59, 95 per cent a need for a reproducible method of measuring compliance
2014 BJS Society Ltd www.bjs.co.uk BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
Effect of World Health Organization surgical safety checklist on postoperative complications 157
that allows a better understanding of its potential effect as factor not included in the measures of adherence in the
a confounding variable affecting checklist efficiency10,24 . included studies. Compliance with the subgroup of safety
In addition, there is a need to identify the key barriers to measures does not necessarily imply appropriate use of the
improve adherence to the SSC8 . checklist.
One other review25 has dealt with the effectiveness of a The available evidence is supportive of a reduction
checklist during surgery. This general review by Borchard in postoperative complications and mortality following
and colleagues did not consider the WHO SSC exclusively. implementation of the WHO SSC, but cannot be regarded
The present review excluded the SURgical PAtient Safety as definitive in the absence of higher-quality studies.
System (SURPASS) checklist26 , which is conceptually Reduction in postoperative complications correlates with
different from the WHO SSC. The SURPASS is a adherence to aspects of care embedded in the WHO SSC.
comprehensive multidisciplinary checklist divided into
parts that correspond to the different phases of the entire
Disclosure
surgical pathway (preoperative, operative, recovery or
intensive care, and postoperative hospital stay); the WHO The authors declare no conflict of interest.
SSC covers only the perioperative phase. Inclusion of the
SURPASS would therefore be methodologically incorrect
here as the two instruments are different. Furthermore, References
this study used the impact of adherence with individual 1 Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human:
items singled out for measurement to explain the variation Building a Safer Health System. National Academy Press:
in effectiveness between sites. Only one other study11 Washington, DC, 2000.
demonstrated the relationship between adherence with the 2 Zegers M, de Bruijne MC, de Keizer B, Merten H,
WHO SSC and reduction in postoperative complications. Groenewegen PP, van der Wal G et al. The incidence,
In their study, van Klei and colleagues11 also showed root-causes, and outcomes of adverse events in surgical
units: implication for potential prevention strategies. Patient
a decrease in mortality related to the degree of SSC
Saf Surg 2011; 5: 13.
completeness.
3 de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ,
The present findings should be interpreted in the Boermeester MA. The incidence and nature of in-hospital
context of the included studies and their limitations. adverse events: a systematic review. Qual Saf Health Care
Several potential biasing and confounding elements must 2008; 17: 216–223.
be considered. First, considerable methodological, clinical 4 Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies
and statistical heterogeneity among studies might have C et al. Mortality after surgery in Europe: a 7 day cohort
hampered the meta-analysis. As a result of various study. Lancet 2012; 380: 1059–1065.
methodological issues and the lack of detailed information 5 Baines RJ, Langelaan M, de Bruijne MC, Asscheman H,
regarding implementation and adherence, meta-regression Spreeuwenberg P, van de Steeg L et al. Changes in adverse
event rates in hospitals over time: a longitudinal
could not be performed in order to explain statistical
retrospective patient record review study. BMJ Qual Saf
heterogeneity. Second, as mortality rates were relatively
2013; 22: 290–298.
low, some studies20 – 23 were underpowered and as such 6 Weiser TG, Regenbogen SE, Thompson KD, Haynes AB,
not able to detect a potential difference in mortality. Lipsitz SR, Berry WR et al. An estimation of the global
Third, the size of the benefit found in these low- volume of surgery: a modelling strategy based on available
quality studies, expressed as a RR, is not close to the data. Lancet 2008; 372: 139–144.
size postulated in general methodological discussions as 7 Weiser TG, Haynes AB, Lashoher A, Dziekan G, Boorman
being sufficient to rule out the need for a randomized DJ, Berry WR et al. Perspectives in quality: designing the
trial27 . Fourth, considering the different cohorts studied, WHO Surgical Safety Checklist. Int J Qual Health Care
paediatric patients were not investigated. Finally, the 2010; 22: 365–370.
interpretation of compliance with the SSC was based on 8 Fourcade A, Blache JL, Grenier C, Bourgain JL, Minvielle
E. Barriers to staff adoption of a surgical safety checklist.
the adherence to a subgroup of safety measures. This is an
BMJ Qual Saf 2012; 21: 191–197.
important distinction as these reported measures represent
9 Levy SM, Senter CE, Hawkins RB, Zhao JY, Doody K, Kao
adherence to specific aspects of care embedded in the LS et al. Implementing a surgical checklist: more than
WHO checklist. The full checklist probably functions checking a box. Surgery 2012; 152: 331–336.
in a different way to the individual items singled out 10 Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S.
for measurement. Studies emphasize the importance of A conceptual framework for implementation fidelity.
team function and communication in checklist use, a Implement Sci 2007; 2: 40.
2014 BJS Society Ltd www.bjs.co.uk BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
158 J. Bergs, J. Hellings, I. Cleemput, Ö. Zurel, V. De Troyer, M. Van Hiel et al.
11 van Klei WA, Hoff RG, Van Aarnhem EE, Simmermacher 20 Sewell M, Adebibe M, Jayakumar P, Jowett C, Kong K,
RKJ, Regli LP, Kappen TH et al. Effects of the introduction Vemulapalli K et al. Use of the WHO surgical safety
of the WHO ‘Surgical Safety Checklist’ on in-hospital checklist in trauma and orthopaedic patients. Int Orthop
mortality: a cohort study. Ann Surg 2012; 255: 44–49. 2011; 35: 897–901.
12 Cochrane Effective Practice and Organisation of Care 21 Askarian M, Kouchak F, Palenik CJ. Effect of surgical safety
Group. EPOC Author Resources. http://epoc.cochrane.org/ checklists on postoperative morbidity and mortality rates,
epoc-author-resources [accessed 15 November 2013]. Shiraz, Faghihy Hospital, a 1-year study. Qual Manag Health
13 Team RDC. R: A Language and Environment for Statistical Care 2011; 20: 293–297.
Computing. R Foundation for Statistical Computing: Vienna, 22 Bliss LA, Ross-Richardson CB, Sanzari LJ, Shapiro DS,
2012. Lukianoff AE, Bernstein BA et al. Thirty-day outcomes
14 DerSimonian R, Laird N. Meta-analysis in clinical trials. support implementation of a surgical safety checklist. J Am
Control Clin Trials 1986; 7: 177–188. Coll Surg 2012; 215: 766–776.
15 Warrens MJ. On association coefficients for 2 × 2 tables and 23 Kwok AC, Funk LM, Baltaga R, Lipsitz SR, Merry AF,
properties that do not depend on the marginal distributions. Dziekan G et al. Implementation of the World Health
Psychometrika 2008; 73: 777–789. Organization surgical safety checklist, including
16 Ziewacz JE, Arriaga AF, Bader AM, Berry WR, Edmondson introduction of pulse oximetry, in a resource-limited setting.
L, Wong JM et al. Crisis checklists for the operating room: Ann Surg 2012; 257: 633–639.
development and pilot testing. J Am Coll Surg 2011; 213: 24 Bergs J, Zurel O, Cleemput I, Hellings J, Vandijck D. The
212–217. implementation of a perioperative checklist increases
17 Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat patients’ perioperative safety and staff satisfaction. Acta
A-HS, Dellinger EP et al. Changes in safety attitude and Anaesthesiol Scand 2013; 57: 675.
relationship to decreased postoperative morbidity and 25 Borchard A, Schwappach DL, Barbir A, Bezzola P. A
mortality following implementation of a checklist-based systematic review of the effectiveness, compliance, and
surgical safety intervention. BMJ Qual Saf 2011; 20: critical factors for implementation of safety checklists in
102–107. surgery. Ann Surg 2012; 265: 925–933.
18 Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, 26 de Vries EN, Hollmann MW, Smorenburg SM, Gouma DJ,
Dellinger EP et al. A surgical safety checklist to reduce Boermeester MA. Development and validation of the
morbidity and mortality in a global population. N Engl J SURgical PAtient Safety System (SURPASS) checklist. Qual
Med 2009; 360: 491–499. Saf Health Care 2009; 18: 121–126.
19 Weiser TG, Haynes AB, Dziekan G, Berry WR, Lipsitz SR, 27 Glasziou, P, Chalmers I, Rawlins M, McCulloch P. When
Gawande AA; Safe Surgery Saves Lives Investigators and are randomised trials unnecessary? Picking signal from
Study Group. Effect of a 19-item surgical safety checklist noise. BMJ 2007; 334: 349–351.
during urgent operations in a global patient population. Ann
Surg 2010; 251: 976–980.
Supporting information
Additional supporting information may be found in the online version of this article:
Appendix S1 Search strategy (MEDLINE) (Word document)
Table S1 Adherence to a subgroup of safety measures as an indicator of checklist adherence before and after
implementation (Word document)
2014 BJS Society Ltd www.bjs.co.uk BJS 2014; 101: 150–158
Published by John Wiley & Sons Ltd
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 4 5969910185303475765 PDFDocument116 pages4 5969910185303475765 PDFEdy Tahir MattoreangNo ratings yet
- Gambaran CT SCAN: (Kasus: Edh, SDH, Ich, Sah, Infark Cerebri, IvhDocument44 pagesGambaran CT SCAN: (Kasus: Edh, SDH, Ich, Sah, Infark Cerebri, Ivhfahmi rosyadiNo ratings yet
- Empirical First Line AntibioticsDocument1 pageEmpirical First Line Antibioticsdiati zahrainiNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Sexually Transmitted InfectionsDocument110 pagesSexually Transmitted Infectionstummalapalli venkateswara raoNo ratings yet
- Obesity Exercise PrescriptionDocument34 pagesObesity Exercise Prescriptionkhushbu88% (8)
- A Mental Healthcare Model For Mass Trauma Survivors - M. Basoglu, Et. Al., (Cambridge, 2011) WW PDFDocument296 pagesA Mental Healthcare Model For Mass Trauma Survivors - M. Basoglu, Et. Al., (Cambridge, 2011) WW PDFraulNo ratings yet
- Monoclonal Antibodies and Engineered AntibodiesDocument24 pagesMonoclonal Antibodies and Engineered AntibodiesMunawar AliNo ratings yet
- Analytical Method Validation of Clopidogrel Tablets BR HPLCDocument48 pagesAnalytical Method Validation of Clopidogrel Tablets BR HPLCAman ThakurNo ratings yet
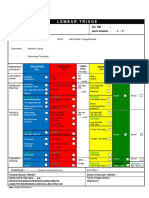
- Lembar Triage: Nama Pasien: Tanggal Lahir: No. RM: Jenis Kelamin: L / PDocument1 pageLembar Triage: Nama Pasien: Tanggal Lahir: No. RM: Jenis Kelamin: L / PEdy Tahir MattoreangNo ratings yet
- RagozineDocument28 pagesRagozineMoisés MedinaNo ratings yet
- Bergs2015 PDFDocument12 pagesBergs2015 PDFEdy Tahir MattoreangNo ratings yet
- Applied Ergonomics: Rebecca J. Mitchell, Ann Williamson, Brett MolesworthDocument11 pagesApplied Ergonomics: Rebecca J. Mitchell, Ann Williamson, Brett MolesworthEdy Tahir MattoreangNo ratings yet
- The SSI BundleDocument15 pagesThe SSI BundleEdy Tahir MattoreangNo ratings yet
- Pone 0101915Document9 pagesPone 0101915Edy Tahir MattoreangNo ratings yet
- Corp Aorn Flyer Pdf2Document1 pageCorp Aorn Flyer Pdf2Edy Tahir MattoreangNo ratings yet
- Sacks Et Al. - 2015 - Teamwork, Communication and Safety Climate A Systematic Review of Interventions To Improve Surgical CultureDocument11 pagesSacks Et Al. - 2015 - Teamwork, Communication and Safety Climate A Systematic Review of Interventions To Improve Surgical CultureEdy Tahir MattoreangNo ratings yet
- Aorn 2016 - Wound Prevalence Study - 161092 Corp Aorn Poster Pdf3Document1 pageAorn 2016 - Wound Prevalence Study - 161092 Corp Aorn Poster Pdf3Edy Tahir MattoreangNo ratings yet
- The SSI BundleDocument15 pagesThe SSI BundleEdy Tahir MattoreangNo ratings yet
- Sacks Et Al. - 2015 - Teamwork, Communication and Safety Climate A Systematic Review of Interventions To Improve Surgical CultureDocument11 pagesSacks Et Al. - 2015 - Teamwork, Communication and Safety Climate A Systematic Review of Interventions To Improve Surgical CultureEdy Tahir MattoreangNo ratings yet
- Early Warning SystemDocument5 pagesEarly Warning SystemEdy Tahir MattoreangNo ratings yet
- WHO Dengue Guidelines 2013Document160 pagesWHO Dengue Guidelines 2013Jason MirasolNo ratings yet
- Handbook: For Clinical Management of DengueDocument124 pagesHandbook: For Clinical Management of DengueraattaiNo ratings yet
- HeyDocument1 pageHeyEdy Tahir MattoreangNo ratings yet
- Tugas Perilaku OrganisasiDocument20 pagesTugas Perilaku OrganisasiEdy Tahir MattoreangNo ratings yet
- Evaluation of scales in immune-mediated polyneuropathiesDocument222 pagesEvaluation of scales in immune-mediated polyneuropathiesAngelo MalerbaNo ratings yet
- Fycompa Efficacy Adjunctive Partial SeizuresDocument20 pagesFycompa Efficacy Adjunctive Partial SeizuresoneniravNo ratings yet
- The LungsDocument6 pagesThe LungsnandaNo ratings yet
- Unit 2Document4 pagesUnit 2api-296199660No ratings yet
- Anvisa National Health Surveillance AgencyDocument52 pagesAnvisa National Health Surveillance AgencyVimarsha HSNo ratings yet
- Excerpt: "Unaccountable: What Hospitals Won't Tell You and How Transparency Can Revolutionize Health Care" by Marty MakaryDocument4 pagesExcerpt: "Unaccountable: What Hospitals Won't Tell You and How Transparency Can Revolutionize Health Care" by Marty Makarywamu885No ratings yet
- Elgabri v. Lekas, M.D., 1st Cir. (1992)Document21 pagesElgabri v. Lekas, M.D., 1st Cir. (1992)Scribd Government DocsNo ratings yet
- Ayushman Bharat - KailashDocument11 pagesAyushman Bharat - KailashKailash NagarNo ratings yet
- ReviewerDocument20 pagesReviewerYang MolosNo ratings yet
- Elphos Erald: Second Shot: Hillary Clinton Running Again For PresidentDocument10 pagesElphos Erald: Second Shot: Hillary Clinton Running Again For PresidentThe Delphos HeraldNo ratings yet
- Hyperthermia and Risk For AspirationDocument3 pagesHyperthermia and Risk For AspirationAlmyr RimandoNo ratings yet
- 64 Vital Nerve CentresDocument29 pages64 Vital Nerve CentresadinaNo ratings yet
- IRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)Document4 pagesIRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)analyn123No ratings yet
- CCMP 2020 Batch Cardiovascular MCQsDocument2 pagesCCMP 2020 Batch Cardiovascular MCQsharshad patelNo ratings yet
- Expansion Screw Activation Guidelines PDFDocument1 pageExpansion Screw Activation Guidelines PDFOsama SayedahmedNo ratings yet
- Zocor (Simvastatin)Document3 pagesZocor (Simvastatin)E100% (1)
- Sound Transduction EarDocument7 pagesSound Transduction Earhsc5013100% (1)
- Resume Jurnal-Dessy Dwi H 201720401011160Document3 pagesResume Jurnal-Dessy Dwi H 201720401011160Pratiwi UmbohNo ratings yet
- ق 4Document36 pagesق 4Zainab HasanNo ratings yet
- Makalah Bahasa InggrisDocument2 pagesMakalah Bahasa InggrisOlga RevalinaNo ratings yet
- Medical Surgical Treatments For EDDocument31 pagesMedical Surgical Treatments For EDskumar_p7No ratings yet
- AcidifiersDocument17 pagesAcidifiersKarim Khalil100% (3)
- Large Volume Parenterals: Guidelines and Quality Control TestsDocument36 pagesLarge Volume Parenterals: Guidelines and Quality Control TestsRákêsh MãttàNo ratings yet